Introduction
Although uncommonly the subject of surgical planning and possibly considered an afterthought by trainees, surgical positioning has been described in itself as “a subspecialty of surgery” that comprises management of patient risks by the entire operating room team. 14 Positioning for a given procedure necessitates careful communication and may require a compromise between optimal surgical access and the potential iatrogenic risks or consequential anesthetic challenges. The topic of positioning in orthopaedic surgery is relatively understudied with scant literature available for review, leaving surgeons subject to their clinical anecdotes and training by mentors in positioning their patients.
Although positioning is a critical portion of any orthopaedist’s practice, the variety of approaches to the foot and ankle requires a solid understanding of the indications, risks, and best practices for the different patient positions. This contemporary review will focus on common positioning in foot and ankle surgery including the supine, traditional lateral, and prone positions, as well as lateral decubitus variations, pearls for arthroscopy, and considerations for procedures at the heel. Additionally, patient-specific risk factors and positioning complications will be discussed.
Supine Positioning
Supine positioning remains the most common positioning for any surgical procedure including foot and ankle surgery (Table 1). With respect to surgery in the lower extremity, this position offers ease for both anesthesia and the surgeon. Theoretically, it poses the least risk of iatrogenic injury to any flaccid, spheroid joints (eg, such as iatrogenic shoulder dislocation or acute rotator cuff insult) during transfers to and from the operating room table. A “hip-bump” or insert under the ipsilateral trochanter can be employed to internally rotate the hip and ensure that the patient’s foot is directed toward the ceiling.
Table 1.
Positioning Pearl Quick Reference: Supine.
| Indications: |
| • Forefoot • Midfoot • Procedures of ankle/hindfoot requiring lateral, anterior, anterolateral, anteromedial, medial approaches only (including those but not limited to ankle fractures without posterior malleolus component requiring open reduction internal fixation, ankle spanning external fixation, etc) |
| Advantages: |
| Ease for anesthesia + surgical team |
| Ease in increasing bump size to account for poor hip internal rotation; approximate IR per thickness |
| Good for polytrauma patient or in patients requiring multiple panels |
| Disadvantages: |
| Poor access to posterior malleolus and posterior structures |
| Many patients have poor hip IR, which precipitate a large hip bump and which may confer postoperative pain. |
| General pearls/tips: |
| Airplane can accommodate for 10-20 degrees of internal rotation but may be limited by patient habitus and C-arm positioning |
| Contralateral hip bump can extenuate hip ER of operative leg for limited posteromedial approaches |
| Radiolucent bed ought to be used when imaging is anticipated |
| If no indication for use of fluoroscopy (eg, simple irrigation and debridement and simple forefoot procedures), consider using stretcher vs OR table to expedite total OR time. |
| Unanswered questions: |
| Does hip bump confer any associated morbidity? |
Abbreviations: ER, external rotation; IR, internal rotation; OR, operating room.
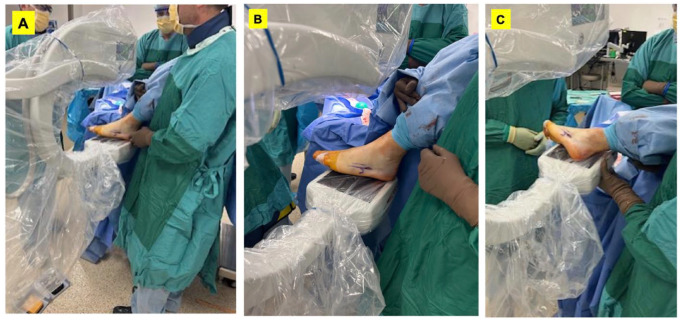
A larger support, such as a bean bag positioner that helps support the spine, can also be used to increase the internal rotation of the hip beyond neutral for lateral/posterolateral approaches. It should also be noted that a contralateral hip bump can extenuate hip external rotation of the operative leg for limited posteromedial approaches—such as required in Haglund’s resection. Another surgical application warranting adjustments to supine positioning can be seen in the fixation of Jones fractures. In the operative treatment of these injuries, it is imperative to obtain a perfect anteroposterior and lateral of the foot intraoperatively to achieve an appropriate start point for intramedullary fixation.1,21 The image intensifier of the C-arm can be used as a base for the foot for anteroposterior radiographs (Figure 1A, B). Then, when obtaining lateral radiograph, the leg and hip can be rotated internally, and a sterile bump may be placed under the operative leg to elevate the foot over the contralateral foot (Figure 1C).
Figure 1.
(A) Jones fracture positioning. The patient is positioned to the far edge of the bed so the operative leg can be dangled onto the mini-C arm image intensifier, which is used as a stable platform. (B) Adequate anteroposterior views can be obtained in this position as well as (C) perfect lateral views.
We have not observed a substantial clinical difference between placing a hip bump directly under the patient’s skin vs underneath a drawsheet that the patient is laying on. For the purposes of mitigating skin irritation to the buttock, we prefer to place a hip bump under the sheet.
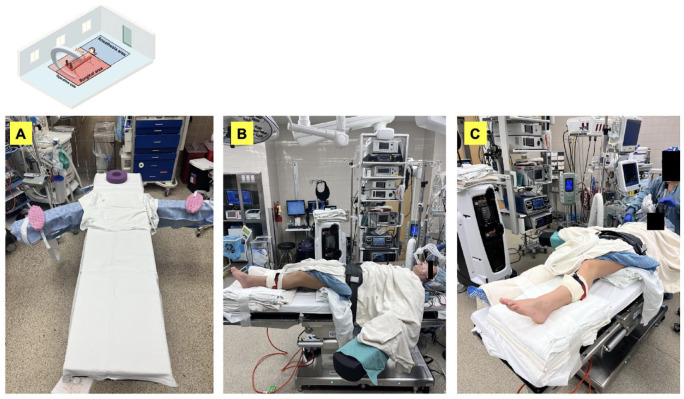
Imaging Pearls
Patients who require intraoperative fluoroscopy should be positioned such that the operative heel is at the foot of the bed. This allows anterior-posterior imaging access of the midfoot to hindfoot without significant need for manipulation. Care should also be taken to place the patient’s arms in an abducted position to mitigate any blocks to free canting of the C-Arm beam (Figure 2A). Additionally, we find that the operative extremity is best visualized fluoroscopically when an elevated platform is used to position the extremity above the contralateral leg (Figure 2B, C). This allows not only for easier surgical access but also for improved lateral imaging. Corresponding monitors displaying fluoroscopy should be positioned in a comfortable position for both the primary surgeon and first assist.
Figure 2.
(A) Supine positioning OR table layout with arm board attachments. (B) Operative extremity can be elevated with a nonsterile towel platform. (C) View of anterolateral foot/ankle.
Complications relating to supine positioning are relatively few and can often be traced to compression-related injuries. We agree with the common teaching that compression neuropraxia most often results from poorly padded bony prominences or mechanical injury when transitioning from stretcher to OR table.
It is also important to ensure the patient is securely fastened to the bed. With larger hip bumps, the patient can slide and become unstable. We choose to tape the padded nonoperative extremity after the standard safety belt is placed more proximally. With larger patients, other positioners may be employed to ensure the patient is not at risk of falling off the bed, including lateral posts and bed extenders attached to the side of the bed.
What About Procedures at the Heel?
There is a paucity of literature describing best practices for performing procedures requiring direct access to the plantar heel. Though these are often performed in supine position, technical challenges for performing plantar heel procedures exist and are exaggerated when there is not a first assist available. One technique used to perform plantar heel procedures is to simply have an assistant lift the leg. If using a sterile fenestrated extremity drape, we advocate draping out the leg proximally at least to the level of the thigh to prevent the drape tenting toward the operative field. Another common technique is to elevate the foot with a wedge, towel-bump, or equivalent while leaving the heel free floating. The latter allows for easier access to the surgical site while rendering intraoperative imaging more convenient, as a stable platform is preferred over manually holding up the foot and ankle.
Lateral Positioning
Traditional lateral positioning utilizing a bean bag inflated with a patient held in the lateral decubitus position allows for reliable access during anterolateral, lateral, posterolateral ankle procedures in addition to lateral (eg, extensile or sinus tarsi) approaches to the calcaneus (Table 2). The bean bag should be centered and deflated on the OR table to allow for ease in patient transfer and intubation/preoperative anesthetic measures (Figure 3A). If possible, the bean bag should be positioned just inferior to the axilla prior to intubation with the arms in a comfortable position. Prior to setting up in a lateral decubitus position, patients can be repositioned toward the cranial or caudal end of the OR table by simply sliding the bean bag as necessary. Coordination and communication lead by the surgical team should outline the order of events for rolling the patient onto one side with or without the need for slight lateral translations of the patient prior to positioning the patient centrally within the bean bag centered on the table. Once the patient has been placed laterally, a pad or roll is placed carefully in the axilla while team members elevate the patient’s thorax in conjunction with anesthesia elevating the patient’s head. Next, prompt deflation of the bean bag should be performed by a separate OR staff member that is not holding the patient. It is important that the bean bag, axillary roll, and nonoperative extremities are carefully inspected, with ample padding placed under bony prominences. Peripheral nerves may also be vulnerable to compression, such as the well-leg common peroneal nerve. To modulate the height of the operative leg, stacked blankets or foam can be taped to the caudal end of the OR table (Figure 3B).
Table 2.
Positioning Pearl Quick Reference: Lateral and Lateral Variants
| Indications: |
| Procedures of ankle/hindfoot requiring lateral, anterior, anterolateral; posterolateral and posterior |
| Advantages: |
| Relative ease for anesthesia + surgical team |
| Direct access to posterolateral ankle |
| Gravity may assist in maintaining graft in lateral approaches to nonunion care or arthrodesis (eg, transfibular approaches) |
| Disadvantages: |
| Poor for polytrauma patient |
| Greater risk of iatrogenic compression-related complications (pressure injury, compression neuropraxia) |
| Access to medial structures significantly decreased and related to hip mobility |
| General pearls/tips: |
| Prior to draping, trial capture anticipated fluoroscopic views |
| If more than 1 incision is required, ensure that the patient’s surgical leg can be mobilized/rotated appropriately with ample space for retractor placement and instrumentation prior to draping |
| Communication between all perioperative team members is crucial; would recommend institutional “all hands-on deck” approach to avoid iatrogenic injury to patient- and work-related injuries of staff |
| Unanswered questions: |
| Is an axillary roll necessary? |
Figure 3.
(A) Supine positioning operating room table layout with arm board attachments. (B) Operative extremity can be elevated with a nonsterile towel platform.
Once the patient has been positioned appropriately, a safety belt may be secured around the bean bag as a fall-safe in the event of air leakage and deflation. Furthermore, it is advisable to simulate C-arm placement for anticipated views. If a bean bag is utilized for lateral or lateral-variant positioning, a thorough inspection of the bean bag should be performed by operating room staff in advance. A faulty bean bag that cannot hold suction may lead to increased procedure difficulty and operative time delays. Our institution recommends inclusion of preoperative bean bag function testing as part of a “Room-Ready Checklist.”
Imaging Caveats
The C-arm should be placed on the opposite side of the OR table across from the surgeon. When using a traditional lateral position, the image intensifier must be moved to acquire standard or special views of the foot/ankle, whereas sloppy lateral positioning favors movement of the operative site over movement of the image intensifier.
Axial images of the heel in the lateral decubitus position can be challenging to obtain. A “Magneto view” is described by Newman et al, where the surgeon can drape both the x-ray source and the image intensifier while standing in the center of the “C.” This improves the ability to adjust the angle of projection for axial views of the calcaneus while maintaining unfettered access to the surgical field. This method requires a knowledgeable surgical team and radiography technician. Sterility can easily be compromised while switching between lateral and Harris views of the calcaneus. Repeated draping of the C-arm may be expected. 27
Care must also be taken to position the patient’s extremities in a scissored position to avoid radiographic distortion by the well extremity (Figures 3B, and 4A and B). One method is to bring the operative leg to a flexed position while the nonoperative leg is kept extended. Ample padding should be placed between the legs to cushion the prominences and create an operative table. Lateral fluoroscopic views of the calcaneus can be obtained with the C-arm image intensifier aiming straight down toward the floor. 27 Marsh et al have described their technique for obtaining Harris view images in the lateral decubitus position. The C-arm is cantilevered nearly 45 degrees parallel to the floor, the tube is positioned flush underneath the OR table, and the beam is aimed down the center of the heel while the foot is dorsiflexed. 26 In either case, it is critical to be able to obtain reliable biplanar fluoroscopic images of the heel without the need to manipulate the foot especially when fractures are held with provisional fixation.
Figure 4.
(A) Sloppy lateral positioning with operative extremity scissored from the well leg. (B, C) Sloppy lateral with the bean bag inflated and patient appropriately positioned. The arm is brought across the chest and secured. (D, E) Postdraping demonstration of anteroposterior and lateral access in the sloppy lateral position.
Advantages, Disadvantages, and Variations
Numerous modifications have been described in the literature pertaining to lateral positioning.13,23,24 One such variation described by Lees et al has been coined the “Floppy Lateral Position.” This was motivated by the challenges of capturing lateral fluoroscopic views with traditional lateral. 23 These authors describe a technique in which the leg can be rotated for anteroposterior and lateral views with minimal image intensifier movement and with dynamic access to all aspects of the foot and ankle. Specifically, the patient is placed into a semilateral position where the pelvis is rolled 45 degrees posteriorly with an anterior support placed at the pubic symphysis. This provides ample rotation of the operative leg. The operative leg is elevated by a thick radiolucent pad secured to the table that is high enough to allow for a lateral view of the foot/ankle clear of the contralateral leg. If a more supine position is required for any portion of the case, the hip bump can be easily removed/deflated intraoperatively to allow increased medial access (Figure 4). If a bump is used, care should be taken to keep the spine in neutral position and avoid overrotation. In their technique tip, Lees et al 23 underscore the need to not too rigidly fix the pelvis either anteriorly or posteriorly to allow for dynamic rotation of the operative leg and to use OR table tilt as needed.
Liu et al 24 describe a variation on the floppy lateral positioning utilizing an additional orthogonal radiolucent table adjacent to the operative extremity. These authors describe a technique in which a very large hip bump is placed under the operative hip and with knee flexion, the foot is placed onto the orthogonal table for posterolateral or lateral approaches to the ankle. Furthermore, they report statistically significant differences between the use of an additional table and traditional positioning in terms of duration of surgery, fluoroscopy time, and overall time for positioning without changes to postoperative AOFAS scores for a small series of patients with bimalleolar and trimalleolar ankle fractures. This technique may be difficult to perform in patients with hip and knee stiffness because of the need for internal rotation of the operative leg, extension of the hip, and flexion of the knee. Also, the extra radiolucent table may be challenging to use in small operative theaters. 24
Lateral positioning confers increased risk compared to supine positioning despite its relative ease in setup. Inherently, body contact area is decreased, resulting in increased pressure at those points where the body contacts the OR table. It is therefore imperative that bony prominences and superficial nerves be cushioned. One commonly overlooked site of possible pressure injury when using lateral positioning is the sequential compression device pneumatic cords on the nonoperative leg. It is important to rotate these in such a manner that they are not between the patient and OR table once the final position has been established. At our institution, we position these upside-down or rotated 90 degrees from conventional orientation prior to induction.
The use of an axillary roll remains controversial, with little literature or quantitative data to support its use. Though the indications for an axillary roll with the concomitant use of a bean bag is debated, lateral positioning under general anesthesia can lead to upper extremity neuropathies due to dependent shoulder position and traction of the brachial plexus, arm ischemia, and compartment syndrome.12,15 The need for axillary rolls in patients who are under deep sedation as opposed to general anesthesia is debated. There is some controversy on whether judicious placement of the cranial-most bean bag is sufficient to function as an axillary roll, or if axillary rolls are necessary in cases with brief operative times. Given the lack of strong clinical or biomechanical data available, we recommend the use of an axillary roll whenever possible to mitigate risk of plexopathy and other complications.
Prone Positioning
Prone positioning is frequently used across multiple disciplines in orthopaedic surgery (Table 3). Given the relatively longer surgical times in spinal deformity correction and fusion as well as open pelvis reduction and fixation, literature describing complications from prone positioning is abundant.
Table 3.
Positioning Pearl Quick Reference: Prone.
| Indications: |
| • Procedures of ankle/hindfoot requiring posterior, posterolateral, posteromedial approaches • Ankle fractures with a posterior malleolar component • Achilles tendon pathology • Arthroscopic procedures requiring access to posterior structures |
| Advantages: |
| Direct visualization of posterior malleolus fragment for anatomic reduction of ankle fractures |
| Simultaneous access to posterior tibia and fibula fractures through a single incision (posterolateral) |
| Adequate restoration of PITFL can obviate the need for syndesmotic screw or tightrope placement |
| Disadvantages: |
| Medial malleolus fractures are less accessible |
| Difficulty for anesthesia + surgical team |
| Approach is not extensile distally and anterior ankle structures cannot be addressed |
| General pearls/tips: |
| Place a bump under the ankle and use gravity as a natural aid for posterior malleolus fracture reduction |
| Flex the knee to 90 degrees to access medial structures |
Abbreviation: PITFL, posteroinferior talofibular ligament.
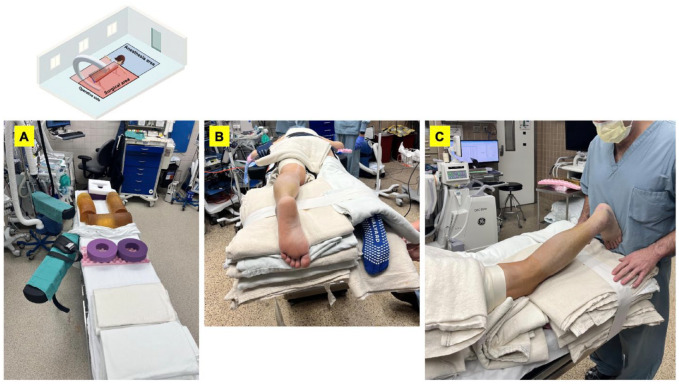
At our institution, we begin by placing cushioned foam pillows and gel pads onto the OR table to relieve pressure on the chest, pelvis, distal thighs, and knees once the patient is flipped prone (Figure 5A). Anesthesia intubates and secures the patient’s airway supine on the stretcher before placing a pillow-mask in preparation for prone positioning. The OR staff may be reminded to avoid placing electrocardiogram leads or Bovie pads on anterior bodily surfaces. When ready for positioning, the stretcher should be brought immediately adjacent to the OR table. With the patient laying supine arms by their side, we recommend that the assistant standing on the stretcher side of the patient place one hand under the patient’s shoulder blade, and another hand under the posterior supior illiac spine (PSIS) while maintaining that arm superior to the patient’s arm, which prevents arm flailing during log roll. The assistant standing on the operating table side should guide the patient down gently to complete the log roll, making sure bony prominences are centered appropriately over the padded cushions.
Figure 5.
(A) Prone positioning table setup, with gel foam rolls centered from the iliac crests to the clavicles. A third horizontally oriented gel foam pad elevates the hemi pelvis. Foam pads offload pressure from the knees. (B, C) Nonsterile towel platform underneath the operative extremity with the knee flexed to about 20 degrees allows for convenient surgical site access.
The gel foam should be centered longitudinally from the clavicle to the iliac crest on each side. A third gel foam oriented horizontally is centered across the iliac crests and elevates the pelvis. Care must be taken to avoid compression of male genitalia and breast tissue by the gel foams. The arms can be positioned cranially with the shoulder abducted less than 90 degrees, elbow flexed to 90 degrees, and forearms neutral with the palms facing down in the surrender position (Figure 5B). Elbow and wrist foam pads should be applied bilaterally. We prefer to place a thigh tourniquet while the patient is still supine, taking care to ensure the tube is rotated away from the anterior position. This eases placement and avoids extension of the hip, which can place tension on the femoral nerve. The operative ankle is placed over a towel bump after prepping and draping and the ipsilateral knee is flexed to about 20 degrees using a gel foam roll or blanket ramp under the tibia (Figure 5C). C-arm is positioned on the opposite side of the table from the operative extremity and an assistant internally rotates the leg at the knee to obtain lateral radiographs.
Though typically assessed by anesthesia staff, we recommend that the surgeon also ensure that the neck is stable in a neutral position. Additionally, direct pressure on the abdomen should be minimized as blood pressure and cardiac strain are both associated with increased afterload.
Advantages, Disadvantages, and Variations
Prone positioning allows for excellent access to posterior approaches of the hindfoot and distal tibia. Both the posteromedial and posterolateral approach to the ankle and distal tibia can be efficiently executed with prone positioning especially in ankle fractures requiring posterior fixation. Talbot et al 30 contend that the posterolateral approach allows not only for direct visualization and anatomical reduction of the posterior malleolar fragment in ankle fractures, but also concurrent reduction of the lateral malleolus because of the respective bony attachments of the posterior inferior tibiofibular ligament (PITFL). An additional benefit is that the same incision and intermuscular plane between the peroneal tendons and posterior border of the fibula can be used to reduce both the posterior malleolus and the distal fibula fractures. Because of the importance of the PITFL regarding syndesmotic stability, adequate fixation of both the posterior and lateral malleolus often restores the natural syndesmosis, reducing the need for additional syndesmotic screw or tightrope fixation. 29
Compared with indirect reduction of the posterior malleolus using anterior-to-posterior screws in the supine position, the likelihood of anatomic reduction of the posterior malleolus from the posterolateral approach in the prone position is significantly higher. 19 Posterior malleolus fractures rarely occur in isolation. We advocate for prone positioning in isolated posterior malleolus fractures or ankle fractures with both posterior malleolar and lateral malleolar fragments. That being said, many surgeons would advocate for lateral positioning using a posterolateral approach for direct access to the posterior malleolus.
When syndesmotic fixation is required, a well-planned posterolateral incision using the plane anterior to the peroneal tendons allows for adequate exposure. Additionally, posterior or posterolateral placement of a fibular plate tends to require less exposure than direct lateral plating. Accordingly, increased vigilance is required to avoid irritation to the peroneal tendons, particularly with distal fibula fractures. The main limitation for prone positioning in trimalleolar ankle fractures is the ability to address the medial malleolus. After reduction of the posterior and/or lateral malleolar fractures, access to the medial side may be accomplished by flexing the knee. 9 An assistant may be required to internally rotate the tibia to access the medial malleolus because of the leg’s proclivity for external rotation. Alternatively, a small bump may be placed under the hip on the contralateral side. In the prone position, fluoroscopy using the image intensifier can be especially challenging. To address this problem, Hamid et al 16 discuss securing the operative leg down with the anterior ankle at the edge of the table with the toes hanging over the edge. The knee of the well-leg is flexed to an obtuse angle and a padded radiolucent triangle elevates the tibia. This allows for improved access to medial, lateral, and posterior structures in addition to unimpeded fluoroscopy of the operative leg.
Prone positioning requires full communication between the surgical and anesthesia teams. Case reports have described unintentional endotracheal tube extubation in the prone position, which can be life threatening as it is challenging for the anesthesia team to reestablish the airway. 7 Patients may complain of postoperative numbness in the anterior thighs from compression neuropathy of the lateral femoral cutaneous nerve while laying prone for long periods. However, this is usually mild and self-limiting. 6 More serious considerations from prone positioning include brachial plexus injuries, intraabdominal compartment syndrome, pressure sores, cortical blindness, and oropharyngeal swelling.
Ankle Arthroscopy/Hindfoot Endoscopy
Arthroscopic access to the ankle can be achieved either through supine or prone positioning, though literature describing either positioning is scant (Table 4). When only anterior portals are necessary, it is advisable to utilize the supine position, although access to posterior portals is achievable with both supine and prone positioning.
Table 4.
Positioning Pearl Quick Reference: Ankle Arthroscopy.
| Indications: |
| • Intra-articular and periarticular procedures of ankle and subtalar joint; consider prone positioning for posterior-pathology • For extra-articular procedures involving posterior talus including os trigonum syndrome, FHL, or peroneal stenosing tenosynovitis; consider prone positioning 18 |
| General pearls/tips: |
| Prior to draping, trial capture anticipated fluoroscopic views |
| Prior to draping, trial method of hand-less means of ankle dorsiflexion/plantarflexion |
| Thoughtful consideration must be paid to well-leg and avoidance of compression-related complications due to caudal positioning on OR table to enable |
| If a noninvasive traction device is to be used, care should be taken to avoid using tape to secure the patient along the rail in which the device to be placed |
| Supine positioning puts neurovascular structures at risk when placing posteromedial and posterolateral portals. |
Abbreviations: FHL, flexor hallucis longus; OR, operating room.
For arthroscopy in the supine position wherein only anterior portals are anticipated, the patient is placed on a regular OR table with slight elevation of the ipsilateral buttock to ensure vertical alignment of the ankle, as previously described. If the surgeon requires external traction, the operative leg is then placed into a “well” leg thigh holder (Figure 6). This should be placed just proximal to the popliteal fossa to avoid venous congestion during exsanguination. The leg should be elevated to a point in which the foot is off the bed to allow the noninvasive traction device to be placed about the ankle in varying positions to optimize exposure. The heel of the operative foot should rest on the very end of the operation table, thus making it possible for the surgeon to fully dorsiflex and plantarflex the ankle joint by leaning against the patient’s foot or have their assistant do so. 32 If access to posterior portals is anticipated, then it is recommended the patient be positioned such that their knee can bend with lowering of the leg extension apparatus on the bed. In these circumstances, the standard arthroscopy knee holder can be positioned to restrict thigh motion but permit ankle motion and allow access to the posterior hindfoot. It is imperative that the well-leg be placed in a well-padded pillow to mitigate compression of the common peroneal nerve. As some arthroscopic procedures require fluoroscopy, we recommend that surgeons experiment with acquisition of possible views prior to draping.
Figure 6.

Arthroscopy with a leg holder for the operative extremity.
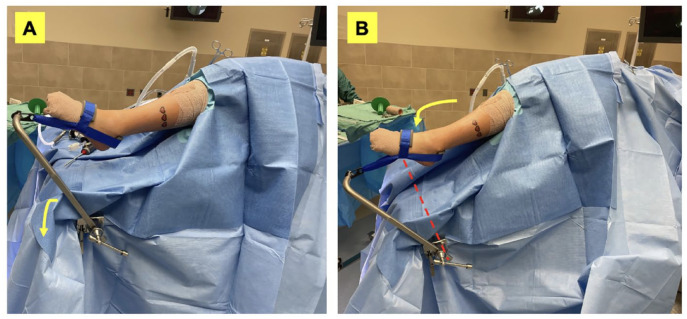
Because of the convex shape of the talar dome and morphology of the tibiotalar joint, ankle arthroscopy is considered one of the most difficult joints to perform safely. 5 As such, numerous invasive and noninvasive ankle distraction methods have been described that aid in the visualization and manipulation of instruments within the ankle joint.2,4,8,25,31,34 Unangst and Martin describe an ankle arthroscopy distraction technique utilizing an actuating external positioning arm, either the Spider (Smith & Nephew, Andover, MA) or Trimono (Arthrex, Naples, FL), attached to the ipsilateral surgical side of the bedrail. A subsequent attachment of a standard padded ankle distraction strap (Arthrex) can be positioned as needed for facilitation of joint distraction either anteriorly or posteriorly. 31 These authors suggest that this technique may help prevent traction injuries to the ankle as the treating surgeon can safely modulate tension applied to the joint and maintain the established guideline threshold. Application of less than 30 lb is considered safe for ankle arthroscopy. 31 The technique employed by one of the senior authors of this review uses a controlled traction system wherein a traction arm and leg holder are both positioned on the surgical side of the bed draped into the field (Figure 7). Dynamic manipulation of the traction arm incline plantarflexes the foot and places a traction moment onto the ankle.
Figure 7.
Controlled traction device draped into the operative field. Dynamic traction illustrated through in A and B, with B demonstrating position in traction, can allow for traction and plantarflexion of the ankle.
For surgeons who routinely perform diagnostic arthroscopy followed by open procedures requiring lateral positioning, Harbach et al 17 describe a novel, versatile lateral decubitus position to allow for ankle or subtalar arthroscopy. These authors suggest that this technique decreases surgical time and increases the ease of surgery, specifically in the context of anatomic lateral ligament repair (modified Brostrom technique).
Although access to the posterior ankle is possible via anterior portals, numerous authors recommend posterior-based portals instead. This is largely due to the inherent tightness of the ankle precipitating risk of cartilage injury.18,20,28 Nevertheless, posteromedial and posterolateral approaches prompt their own relative risks by placing the neurovascular structures at risk.3,10,11,20,22,28,33 Prone positioning for posterior ankle arthroscopy is believed by some to provide a more direct approach to the posterior aspect of the ankle and subtalar joint. Not only does prone positioning allow safer means of posterior portal placement, visualization of the posterior aspect of the talus is greatly improved—the field of view is as medial as the flexor hallucis longus, as lateral as the peroneal sheath, as cranial as the tibiotalar joint, and as caudal as the subtalar joint.18,28 In their technical article outlining their technique on prone ankle and subtalar arthroscopy, Phisitkul et al 28 briefly describe additional elements to positioning for prone arthroscopy. They advise positioning the ankle just beyond the end of the bed to allow the establishment of anterior portals for the ankle and subtalar joint as needed. This way the surgeon can lean on the foot to dorsiflex the ankle when an assistant is unavailable. Beyond these recommendations, there is a paucity of literature on positioning pearls specifically with prone positioning with posterior arthroscopy. The same general safety precautions and techniques described in the prone positioning section should be adhered.
Conclusion
Positioning is not only critical in managing the variety of approaches and pathologies required for foot and ankle surgery, but also requires a solid understanding of the indications, risks, and best practices for patient safety while maximizing surgical exposure. This contemporary review focuses on common positioning in foot and ankle surgery including supine and traditional lateral positions with discussion on lateral decubitus variations, prone positioning, pearls for arthroscopy, and considerations for procedures at the heel. Patient-specific risk factors and positioning complications are discussed, including airway complications, pressure injuries, compression neuropraxia, and others.
Supplemental Material
Supplemental material, sj-pdf-1-fao-10.1177_24730114231201833 for Positioning Pearls in Foot and Ankle Surgery: A Contemporary Review by Kempland C. Walley, Davin C. Gong, Thomas M. Hearty, James R. Holmes, Paul G. Talusan and Davin M. Walton in Foot & Ankle Orthopaedics
Footnotes
Ethical Approval: Ethical approval was not sought for the present study because it is a Contemporary Review.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Kempland C. Walley, MD,  https://orcid.org/0000-0003-4488-0663
https://orcid.org/0000-0003-4488-0663
Davin C. Gong, MD,  https://orcid.org/0000-0002-7532-0346
https://orcid.org/0000-0002-7532-0346
References
- 1. Aynardi M, Walley KC, Wisbeck JM. Intramedullary screw fixation of Jones fracture: the crucial starting point and minimizing complications. Orthop J Harv Med Sch. 2019;20:42-45. [Google Scholar]
- 2. Baer TE, Stolley MP, Thedens DR, Brown TD, Saltzman CL. Clinical tip: development of an ankle distraction device compatible with MRI and radiography. Foot Ankle Int. 2006;27(6):472-474. doi: 10.1177/107110070602700615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Balcı Hİ, Polat G, Dikmen G, Atalar A, Kapıcıoğlu M, Aşık M. Safety of posterior ankle arthroscopy portals in different ankle positions: a cadaveric study. Knee Surg Sports Traumatol Arthrosc. 2016;24(7):2119-2123. doi: 10.1007/s00167-014-3475-6 [DOI] [PubMed] [Google Scholar]
- 4. Ball L, Hawken R, Davis J. Distraction of the ankle joint during arthroscopy. Ann R Coll Surg Engl. 2009;91(3):266. doi: 10.1308/RCSANN.2009.91.3.266A [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Burman MS. Arthroscopy or the direct visualization of joints: an experimental cadaver study. 1931. Clin Orthop Relat Res. 2001;390:5-9. doi: 10.1097/00003086-200109000-00003 [DOI] [PubMed] [Google Scholar]
- 6. Cho KT, Lee HJ. Prone position-related meralgia paresthetica after lumbar spinal surgery: a case report and review of the literature. J Korean Neurosurg Soc. 2008;44(6):392. doi: 10.3340/JKNS.2008.44.6.392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. de Cosmo G, Congedo E. Unintentional tracheal extubation during prone position: what is the best rescue airway device? J Emerg Trauma Shock. 2017;10(1):2. doi: 10.4103/0974-2700.199525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dowdy PA, Watson BV, Amendola A, Brown JD. Noninvasive ankle distraction: relationship between force, magnitude of distraction, and nerve conduction abnormalities. Arthroscopy. 1996;12(1):64-69. doi: 10.1016/S0749-8063(96)90221-2 [DOI] [PubMed] [Google Scholar]
- 9. Easley M, Wiesel S. Operative Techniques in Foot and Ankle Surgery; 2011. Accessed August 30, 2022. https://books.google.com/books?hl=en&lr=&id=A9q0gg3Sv4YC&oi=fnd&pg=PA115&dq=Operative+Techniques+in+Foot+and+Ankle+Surgery+-+Wiesel&ots=Wd0praeyVn&sig=dURgUfIyixuHQNn7DmRLL1l8GuY
- 10. Feiwell LA, Frey C. Anatomic study of arthroscopic portal sites of the ankle. Foot Ankle. 1993;14(3):142-147. doi: 10.1177/107110079301400306 [DOI] [PubMed] [Google Scholar]
- 11. Ferkel RD, Small HN, Gittins JE. Complications in foot and ankle arthroscopy. Clin Orthop Relat Res. 2001;391:89-104. doi: 10.1097/00003086-200110000-00010 [DOI] [PubMed] [Google Scholar]
- 12. Furnas H, Canales F, Buncke GM, Rosen JM. Complications with the use of an axillary roll. Ann Plast Surg. 1990;25(3):208-209. doi: 10.1097/00000637-199009000-00011 [DOI] [PubMed] [Google Scholar]
- 13. Garala K, Patil S. Reinventing the floppy lateral position for dual approaches in COVID-19 times. Orthop Trauma. 2021;35(2):76-79. doi: 10.1016/J.MPORTH.2021.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gefen A, Creehan S, Black J. Critical biomechanical and clinical insights concerning tissue protection when positioning patients in the operating room: a scoping review. Int Wound J. 2020;17(5):1405-1423. doi: 10.1111/IWJ.13408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Haldar R, Bhagat H, Toshniwal G, Dash H. Conventional axillary rolls in prolonged neurosurgical procedures: time for reconsideration. Asian J Neurosurg. 2017;12(3):583. doi: 10.4103/1793-5482.145538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hamid KS, Dekker TJ, White PW, Adams SB. Radiolucent triangle as a positioning tool to simplify prone ankle fracture surgery. Foot Ankle Spec. 2017;10(1):51-54. doi: 10.1177/1938640016675411 [DOI] [PubMed] [Google Scholar]
- 17. Harbach GP, Stewart JD, Lambert EW, Anderson C. Ankle arthroscopy in the lateral decubitus position. Foot Ankle Int. 2003;24(8):597-599. doi: 10.1177/107110070302400805 [DOI] [PubMed] [Google Scholar]
- 18. Hsu AR, Gross CE, Lee S, Carreira DS. Extended indications for foot and ankle arthroscopy. J Am Acad Orthop Surg. 2014;22(1):10-19. doi: 10.5435/JAAOS-22-01-10 [DOI] [PubMed] [Google Scholar]
- 19. Huber M, Stutz PM, Gerber C. Open reduction and internal fixation of the posterior malleolus with a posterior antiglide plate using a postero-lateral approach—a preliminary report. Foot Ankle Surg. 1996;2(2):95-103. doi: 10.1046/J.1460-9584.1996.00012.X [DOI] [Google Scholar]
- 20. Kashuk KB, Harmelin E, Holcombe R, Goggin J. Arthroscopy of the ankle and subtalar joint. Clin Podiatr Med Surg. 2000;17(1):55-79, vi. Accessed August 29, 2022. https://europepmc.org/article/med/10652655 [PubMed] [Google Scholar]
- 21. Le M, Anderson R. Zone II and III fifth metatarsal fractures in athletes. Curr Rev Musculoskelet Med. 2017;10(1):86-93. doi: 10.1007/S12178-017-9388-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lee TH, Berlet GC, Amendola A, Sitler DF, Thain LMF, Spouge A. Placement of the posteromedial portal in posterior ankle arthroscopy [2] (multiple letters). J Bone Joint Surg Am. 2003;85(1):164-165. doi: 10.2106/00004623-200301000-00026 [DOI] [PubMed] [Google Scholar]
- 23. Lees D, Rankin K, Marriott A, Murty A. Floppy lateral position: technique tip. Foot Ankle Int. 2013;34:1460-1463. [DOI] [PubMed] [Google Scholar]
- 24. Liu B, Jin R, Rai S, Liu R, Hong P. Additional table for easier access to ankle fracture: a retrospective study of traditional positioning versus modified positioning. Medicine. 2020;99(45):e23146. doi: 10.1097/MD.0000000000023146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lozano-Calderón SA, Samocha Y, McWilliam J. Comparative performance of ankle arthroscopy with and without traction. Foot Ankle Int. 2012;33(9):740-745. doi: 10.3113/FAI.2012.0740 [DOI] [PubMed] [Google Scholar]
- 26. Marsh JL, Boyer JS, Sullivan J, Phisitkul P, Karam MD. A percutaneous technique for reduction and internal fixation of displaced intra-articular calcaneal fractures. JBJS Essent Surg Tech. 2011;1(2):e9. doi: 10.2106/JBJS.ST.K.00016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Newman ET, Kelly BA, Rodriguez EK. The “magneto view”: a simple method for obtaining intraoperative axial radiographs of the calcaneus. Surg Tech. 2015;16:116-120. [Google Scholar]
- 28. Phisitkul P, Junko JT, Femino JE, Saltzman CL, Amendola A. Technique of prone ankle and subtalar arthroscopy. Tech Foot Ankle Surg. 2007;6(1):30-37. doi: 10.1097/01.BTF.0000235419.53662.95 [DOI] [Google Scholar]
- 29. Pilskog K, Gote TB, Odland HEJ, et al. Traditional approach vs posterior approach for ankle fractures involving the posterior malleolus. Foot Ankle Int. 2021;42(4):389-399. doi: 10.1177/1071100720969431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Talbot M, Steenblock TR, Cole PA. Surgical technique: posterolateral approach for open reduction and internal fixation of trimalleolar ankle fractures. Can J Surg. 2005;48(6):487. Accessed August 30, 2022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3211728/ [PMC free article] [PubMed] [Google Scholar]
- 31. Unangst A, Martin KD. Simple 1-step ankle arthroscopy distraction. Arthrosc Tech. 2015;4(6):e873. doi: 10.1016/J.EATS.2015.08.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. van Dijk CN, Scholte D. Arthroscopy of the ankle joint. Arthroscopy. 1997;13(1):90-96. doi: 10.1016/S0749-8063(97)90215-2 [DOI] [PubMed] [Google Scholar]
- 33. Voto SJ, Ewing JW, Fleissner PR, Alfonso M, Kufel M. Ankle arthroscopy: neurovascular and arthroscopic anatomy of standard and trans-Achilles tendon portal placement. Arthroscopy. 1989;5(1):41-46. doi: 10.1016/0749-8063(89)90089-3 [DOI] [PubMed] [Google Scholar]
- 34. Young BH, Flanigan RM, DiGiovanni BF. Complications of ankle arthroscopy utilizing a contemporary noninvasive distraction technique. J Bone Joint Surg Am. 2011;93(10):963-968. doi: 10.2106/JBJS.I.00977 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-fao-10.1177_24730114231201833 for Positioning Pearls in Foot and Ankle Surgery: A Contemporary Review by Kempland C. Walley, Davin C. Gong, Thomas M. Hearty, James R. Holmes, Paul G. Talusan and Davin M. Walton in Foot & Ankle Orthopaedics