Graphical abstract

Keywords: Endocarditis, Leukocytoclastic vasculitis, Echocardiography
Highlights
-
•
IE is rarely associated with multisystem vasculitis.
-
•
A high index of suspicion is required to ensure proper treatment of IE.
-
•
Mistaking IE for vasculitis and treating with immunosuppressives can be fatal.
Introduction
Subacute infective endocarditis (IE) has various presentations and rarely can present as a cutaneous leukocytoclastic vasculitis. This can be problematic when directly competing etiologies are in the differential diagnosis. Misdiagnosing a patient with bacterial IE and initiating immunosuppressive therapy can lead to detrimental outcomes. A high index of suspicion for IE is imperative when manifestations of vasculitis are seen in a patient with sepsis.
Case Presentation
A 71-year-old man with a 4-month history of anemia, thrombocytopenia, fatigue, weight loss, and night sweats and multiple prior episodes of transient painless left-eye vision loss was admitted to the hospital for worsening of these symptoms in addition to increasing pedal edema and the development of a purpuric rash (Figure 1).
Figure 1.
Photograph of the lower extremities demonstrating the purpuric rash and mild edema.
The patient’s prior outpatient work up included colonoscopy, endoscopy, and bone marrow biopsy, which were all nonrevealing of an etiology for the patient’s constellation of symptoms. A computed tomographic scan of the chest, abdomen, and pelvis revealed splenomegaly with evidence of splenic infarct. A biopsy of the rash demonstrated leukocytic vasculitis. Physical examination on the first day of hospital admission demonstrated clear lungs and a regular heart rate and rhythm with a 2/4 holosystolic murmur best appreciated at the apex, a soft 3/6 diastolic murmur at the aortic valve position radiating to the apex, mild jugular venous pressure, and 1+ bilateral pitting edema of the legs. The patient developed paroxysmal atrial fibrillation with a rapid ventricular rate of 132 beats/min with a systolic blood pressure of 90 mm Hg. Laboratory analysis revealed chronic anemia with a hemoglobin level of 7.6 g/dL, a platelet count of 76,000/μL, and an elevated ferritin value of 1,864 ng/mL with positive serum results for cryoglobulins and B2-microglobulin. On hospital day 2, transthoracic echocardiography was performed because of the results of physical examination and showed a 1.1 × 1.25 cm echogenic mass on the ventricular aspect of the aortic valve (Figure 2A; Video 1, Video 2, Video 3). The patient was started on empiric ceftriaxone at this time. Subsequent transesophageal echocardiography on hospital day 4 was conducted for better visualization of the echogenic mass and confirmed a valvular vegetation with a mobile component and severe aortic (vena contracta > 0.65 cm with a pressure half-time of 180 msec) and mitral regurgitation (effective regurgitant orifice area > 0.5 cm and a regurgitant volume of 70 mL; Figures 2B-D; Video 4). Subsequent blood cultures were positive for streptococcal mitis. The patient’s rash resolved shortly after treatment with antibiotics.
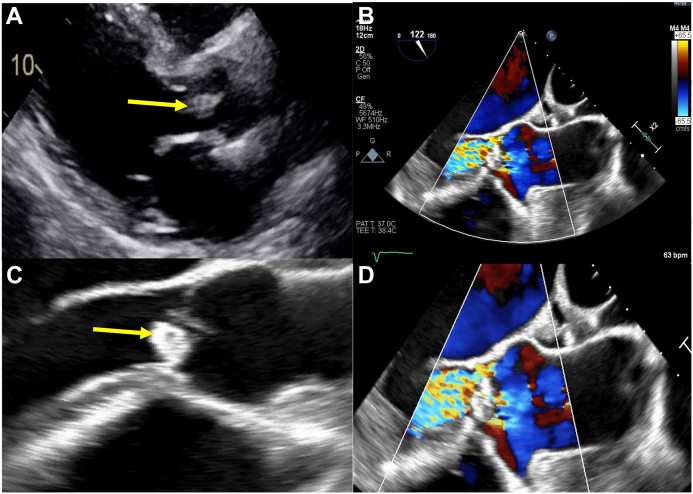
Figure 2.
(A) Two-dimensional transthoracic echocardiography, parasternal long-axis view, mid-diastolic phase, demonstrating the echogenic mass on the aortic valve (arrow). (B) Two-dimensional transesophageal echocardiography (TEE), midesophageal, long-axis (122°) view, diastolic phase with color flow Doppler, demonstrating severe aortic regurgitation. (C) Two-dimensional TEE, midesophageal, zoomed long-axis view, diastolic phase, demonstrating the echogenic mass (arrow) and with color flow Doppler (D) demonstrating severe aortic regurgitation.
On hospital day 6, head computed tomography revealed bilateral hematomas and a subarachnoid hemorrhage, raising the possibility of septic or mycotic embolism. The hospital course was further complicated by worsening renal function, with the serum creatinine level rising to 6.1 mg/dL (baseline, 1.0 mg/dL) over the course of 2 weeks. A renal biopsy revealed postinfectious glomerulonephritis with crescent formation. After clearance from neurology, nephrology, and the infectious disease teams, the patient underwent successful mitral valve and aortic valve replacement by the cardiothoracic department.
Discussion
Although uncommon, IE presenting with cutaneous vasculitis has been reported in the literature. A 2015 study by Loricera et al.1 revealed that among 766 patients presenting with cutaneous vasculitis, 27 had underlying bacterial infections. The study showed that the median delay from admission to diagnosis of infection was 4 days. Long diagnostic delays were noted in two patients (32 and 45 days, respectively). Neither patient had typical signs of IE at admission. Both patients went into acute heart failure and required the implantation of prosthetic valves. A report published in 2017 described a patient who was suspected to have an idiopathic autoimmune cutaneous vasculitis but was found to have IE with aortic involvement. The delay in diagnosis led the patient to deteriorate and require intubation for respiratory failure. Transesophageal echocardiography showed complete destruction of the aortic valve with dissection into the left ventricle.2 Another example is a 2021 report of a 71-year-old woman with a dual-chamber automatic implantable cardioverter-defibrillator who presented with septic shock, acute renal failure, and purpuric rash with scattered bullae. Cultures were negative at the time. Biopsy of the cutaneous lesions confirmed leukocytoclastic vasculitis, but immune suppression treatment was delayed because of hemodynamic instability. Echocardiography was performed because of acute decompensation and revealed a mobile mass adjacent to the patient’s cardiac device, providing a major criterion for the diagnosis of IE. The patient was given ceftriaxone for coverage of native and prosthetic valve endocarditis, leading to eventual hemodynamic stability and resolution of the vasculitis.3 Early identification of the cutaneous manifestations associated with IE is crucial because of the prognostic importance of an early diagnosis and therapeutic management.
The gold standard of treatment for most types of vasculitis is immunosuppression with corticosteroids. However, immunosuppressive therapy can be detrimental in patients with IE. Therefore, it is imperative to differentiate between the two diseases.
In the patient described here, the presentation of weight loss, night sweats, leg swelling, purpuric rash with decreased red blood cell count, and thrombocytopenia in conjunction with a leukocytoclastic vasculitis on skin biopsy led to an initial differential diagnosis of a primary vasculitis, systemic lupus erythematous, and malignancy such as spleen lymphoma. However, the patient’s abnormal echocardiographic findings led to the diagnosis of IE with embolic phenomena, likely due to underlying abnormal heart valves instead of an underlying rheumatic etiology.
The clinical manifestations of are highly variable. Fever is the most common symptom, along with headache, myalgias, night sweats, pleuritic pain, and dyspnea. In rare instances, IE can present as leukocytoclastic vasculitis. In retrospect, this patient presented with several signs of IE such as septic emboli (splenic infarct, worsening renal function, and transient ischemic attack), leukocytoclastic vasculitis, and a subacute prodrome of fatigue, lower extremity swelling, and night sweats. The accepted criteria for diagnosis of IE are the modified Duke criteria, which require a certain number of major or minor clinical criteria. Major criteria seen in this patient included positive blood cultures for viridans organisms and evidence of endocardial involvement on echocardiogram. Minor criteria met in this patient included fever, vascular phenomena (possibly the patient’s blindness and intracranial hemorrhages), and immunologic phenomena (glomerulonephritis).
Because of the abnormal findings on transthoracic echocardiography, the suspicion of IE was entertained. Subsequent transesophageal echocardiography and blood cultures confirmed the diagnosis. Rapid alleviation of the patient’s rash and other symptoms after antibiotic therapy further supported the diagnosis of a leukocytoclastic vasculitis due to underlying IE. Immunosuppression remains the gold standard treatment for most types of vasculitis; however, misdiagnosing a patient with IE and initiating immunosuppressive therapy can lead to detrimental outcomes. Several cases have been reported in which patients with undiagnosed subacute IE present with leukocytoclastic vasculitis and renal failure and deteriorate because of delays in treatment.1,2 A high index of suspicion is required to ensure prompt and necessary treatment of IE.
Conclusion
A differential diagnosis of IE should be considered in a patient with sepsis with symptoms of vasculitis. Despite overlapping characteristics, a misdiagnosis between the two disease states can have fatal consequences.
Ethics Statement
The authors declare that the work described has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans.
Consent Statement
The authors declare that since this was a non-interventional, retrospective, observational study utilizing de-identified data, informed consent was not required from the patient under an IRB exemption status.
Funding Statement
The authors declare that this report did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure Statement
The authors report no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.case.2023.05.002.
Supplementary Data
Two-dimensional transthoracic echocardiography, basal parasternal short-axis view, demonstrating the trileaflet, thickened aortic valve leaflets with focal echogenic material on the right coronary cusp.
Two-dimensional transthoracic echocardiography, apical long-axis view, demonstrating the abnormal aortic valve leaflets with thickening and small mobile mass within the left ventricular outflow tract.
Two-dimensional transthoracic echocardiography, apical long-axis view with color Doppler, demonstrating the severe aortic regurgitation and eccentric, posterior-directed severe mitral regurgitation.
Two-dimensional transesophageal echocardiography, midesophageal long-axis (120°) view, demonstrating the echogenic mass on the left ventricular outflow tract side of the right coronary cusp with small mobile component, the abnormal coaptation of the aortic valve leaflets directing the aortic regurgitation toward the mitral valve, and focal thickening of the anterior mitral valve leaflet with abnormal coaptation directing the mitral regurgitation posteriorly. Also noted is a dilated left atrium with a prominent Eustachian valve and a small effusion within the transverse sinus.
References
- 1.Loricera J., Blanco R., Hernández J.L., Pina T., González-Vela M.C., Fernández-Llaca H., et al. Cutaneous vasculitis associated with severe bacterial infections. A study of 27 patients from a series of 766 cutaneous vasculitis. Clin Exp Rheumatol. 2015;33:36–43. [PubMed] [Google Scholar]
- 2.El Chami S., Jibbe A., Shahouri S. Bacterial endocarditis presenting as leukocytoclastic vasculitis. Cureus. 2017;9:e1464. doi: 10.7759/cureus.1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spindel J., Parikh I., Terry M., Cavallazzi R. “Leucocytoclastic vasculitis due to acute bacterial endocarditis resolves with antibiotics”. BMJ Case Reports CP14. 2021;1:e239961. doi: 10.1136/bcr-2020-239961. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Two-dimensional transthoracic echocardiography, basal parasternal short-axis view, demonstrating the trileaflet, thickened aortic valve leaflets with focal echogenic material on the right coronary cusp.
Two-dimensional transthoracic echocardiography, apical long-axis view, demonstrating the abnormal aortic valve leaflets with thickening and small mobile mass within the left ventricular outflow tract.
Two-dimensional transthoracic echocardiography, apical long-axis view with color Doppler, demonstrating the severe aortic regurgitation and eccentric, posterior-directed severe mitral regurgitation.
Two-dimensional transesophageal echocardiography, midesophageal long-axis (120°) view, demonstrating the echogenic mass on the left ventricular outflow tract side of the right coronary cusp with small mobile component, the abnormal coaptation of the aortic valve leaflets directing the aortic regurgitation toward the mitral valve, and focal thickening of the anterior mitral valve leaflet with abnormal coaptation directing the mitral regurgitation posteriorly. Also noted is a dilated left atrium with a prominent Eustachian valve and a small effusion within the transverse sinus.