Abstract
Purpose:
Respirators are simple and efficient in protecting workers against toxic airborne substances; however, their use may limit the physical performance of workers. The purpose of this study was to determine the effect of inspiratory resistance on physical performance and breathing perception in normobaric hypoxia.
Method:
Nine healthy men wore a tight-fitting respiratory mask outfitted with one of four different inspiratory resistors (R) (0, 1.5, 4.5, 7.5 cm H2O/L/Sec) while exercising at normobaric hypoxia (17% O2) at submaximal exercise workloads of 50, 100, and 150 W on a cycle ergometer for 10 minutes each, followed by a maximal oxygen uptake (VO2max) test to exhaustion.
Results:
Maximal power output at R7.5 was significantly lower than R0 (p = 0.016) and R1.5 (p = 0.035). Respiration rate was significantly reduced at R4.5 (p = 0.011) and R7.5 (p ≤ 0.001) compared with R0. Minute ventilation was significantly decreased in R7.5 compared with R0 (p = 0.003), R1.5 (p = 0.010), and R4.5 (p = 0.016), whereas VO2 was not significantly changed. Breathing comfort (BC) and breathing effort (BE) were significantly impaired in R7.5 (BC: p = 0.025, BE: p = 0.001) and R4.5 (BC: p = 0.007, BE: p = 0.001) compared with R0, but rating of perceived exertion (RPE) remained unchanged.
Conclusions:
Added inspiratory resistance limited maximal power output and increased perceptions of BC and BE in normobaric hypoxia. However, low-to-moderate inspiratory resistance did not have a deleterious effect on VO2 or RPE at submaximal or maximal exercise. Perceptual and physiological characteristics of respirators of varying inspiratory resistances should be considered by manufacturers and end users during design and respirator selection processes.
Keywords: breathing comfort, breathing effort, exercise performance, inspiratory resistance, normobaric hypoxia
Introduction
Various respirators are used in private industries and healthcare settings, and reduce the exposure to airborne contaminants when used properly. Consequently, adequate respiratory protection helps protect against respiratory diseases, including asthma, bronchitis, lung cancer, and chronic obstructive pulmonary disease (COPD) (Beckett, 2000; Fukakusa et al., 2011). However, the use of respirators has been shown to have adverse effects on physiological and psychological responses (Louhevaara et al., 1984; Johnson et al., 1995). Respirator filters and canisters create breathing resistance, which can reduce maximal work performance ~10% (Raven et al., 1977; Stemler and Craig, 1977; Deno et al., 1981) and produce breathing discomfort (Roberge et al., 2013). Prior investigation also reported that increased inspiratory resistance resulted in excessive respiratory fatigue that significantly reduced maximal working time (Heus et al., 2004).
It is common for occupational and military activities to be performed at locales (e.g., Denver, CO) with moderately high altitude (1500 m). High altitude produces low partial pressures of oxygen (O2) in the blood, which can cause alterations of physiological (Laciga and Koller, 1976) and psychological functions (Crow and Kelman, 1973). Furthermore, poorly controlled pulmonary diseases, such as COPD, asthma, and bronchitis limit O2 delivery to vital organs and initiate hypoxemia (Khatri and Ioachimescu, 2016).
While much is known regarding the role of breathing resistance on physical performance in normobaric normoxia, the interaction between inspiratory resistance and physical performance in environmental hypoxia has not been definitively determined. As aforementioned, hypoxic conditions can be induced by environmental and pathophysiological factors; this can possibly have a negative impact on workers who perform their duties at high altitude or those who have poorly controlled mild-to-moderate pulmonary disease. Therefore, the purpose of this study was to evaluate the effects of inspiratory resistances on physical performance during submaximal and maximal efforts in environmental hypoxia. It was hypothesized that added inspiratory resistance would limit cardiopulmonary function and consequently impair physical performance and subjective perception linearly with resistance level.
Materials and Methods
Participants
Nine healthy men (25 ± 2 years of age, height 181.4 ± 6.1 cm, weight = 92.5 ± 2.6 kg, and body mass index = 28.0 ± 5.3 kg/m2) participated in the current study between April and August, 2016. All subjects were residents of the state of Ohio (mean state elevation 259 m) and had not been exposed to normobaric hypoxia or hypobaric hypoxia within 2 months of the study. Subjects were screened through a health history questionnaire before participation and were excluded if they reported the presence or history of smoking, respiratory disease, cardiovascular disease, or metabolic disorder. The Institutional Review Board of Kent State University (16–176) approved this study and all subjects provided signed, informed consent.
Experimental design
The present study employed a single blind, repeated measures design with counterbalanced order. Subjects reported to the Exercise Physiology Laboratory at Kent State University on five occasions, separated by at least 3 days between individual trials. Experimental trials consisted of breathing through a respiratory mask outfitted with one of four custom-built inspiratory resistors (R) [(0, 1.5, 4.5, 7.5 cm H2O/L/Sec) at air flow rate of 85 L/min] (model 7400 V-mask; Hans-Rudolph, Shawnee, KS) while exercising at various work rates on a cycle ergometer. These resistors span the inspiratory resistance levels permitted in the current National Institute for Occupational Safety and Health standard for air purifying respirators, such as filtering facepiece respirators and half-mask elastomeric respirators (Shykoff and Warkander, 2011). The maximum allowable inhalation resistance for various types of respirators range from 1.5 to 8.5 cm H2O/L/Sec with constant air flow rate of 85 L/min. Experimental trials were conducted in a normobaric hypoxic chamber (Colorado Altitude Training, Louisville, CO) at 21% normobaric normoxia (NN21) and 17% O2 normobaric hypoxia (NH17).
Experimental procedure
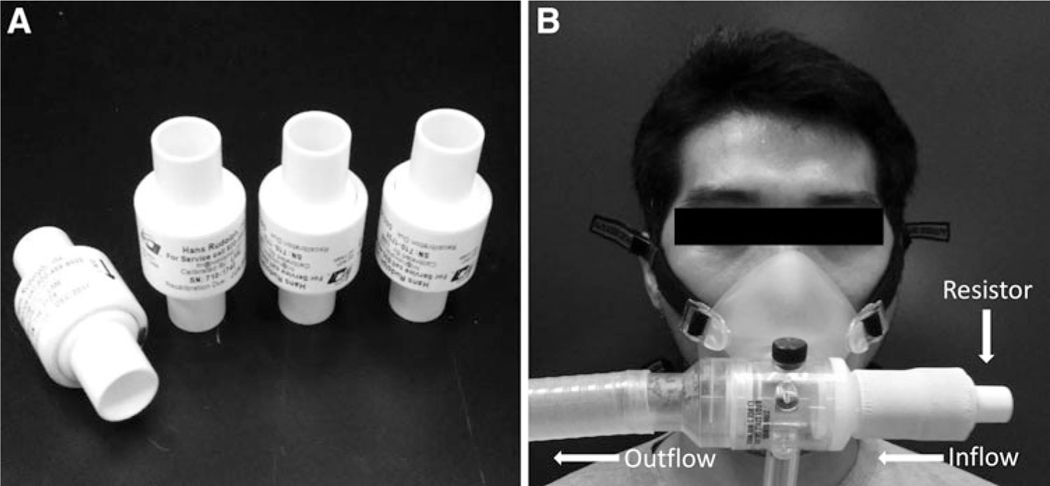
On the days of experimental trials, subjects were clothed in T-shirts, shorts, and athletic shoes. They were equipped with a silicone–rubber oronasal facemask that was outfitted with one of the aforementioned custom-built inspiratory resistors (Fig. 1). Expired air samples were analyzed by a Parvo-Medics TrueOne 2400 Metabolic System (Parvo, Sandy, UT) for oxygen uptake (VO2), respiratory rate (RR), tidal volume (VT), minute ventilation (VE), and respiratory exchange ratio (RER). The heart rate (HR) was monitored with a HR monitor (Polar RS800 CS; Polar Electro Oy, Kempele, Finland), and the pulse-derived oxygen saturation (oxygen saturation as measured by pulse oximetry [SpO2]) was measured with a digital pulse oximeter (Oxy-Go, Roslyn, NY). Subjective impressions of exertion were obtained using the Borg Perceived Exertion Scale (Borg, 1982) ranging from “no exertion at all” to “maximal exertion.” Inspiratory breathing comfort (BC), and inspiratory breathing effort (BE) were measured by 7-point scales (Roberge et al., 2013) ranging from “no discomfort” to “intolerable discomfort” and “not noticeable” to “intolerable,” respectively. Subjective impressions were measured simultaneously with SpO2 and HR at the last minute of each stage. All measurements were averaged for the last minute of each time point.
FIG. 1.
Custom-built inspiratory resistors (A) and experimental mask setup (B).
Subjects sat in a chair for 10 minutes in NN21 ambient conditions, whereas baseline measurements of VO2, HR, SpO2, and subjective scales were obtained immediately before exercise trials. Subjects then rested in the NH17 chamber for 30 minutes and had the same measurements taken as in the NN21 baseline state, after which they performed submaximal and maximal exercise consecutively on an automatically braked cycle ergometer (Lode Excalibur Sport; Lode, Groningen, Netherlands). The submaximal cycling included three stages of absolute workloads at 50, 100, and 150 W for 10 minutes each. Thereafter, the workload increased 25 W every minute until volitional fatigue. Verbal encouragement was given by staff during the maximal cycling exercise.
Statistical analyses
All statistical analyses were conducted using a statistical software package (SPSS v.19.0). The overall study used a two-way repeated measure analyses of variance (ANOVA) to compare physiological and subjective measurements between normoxia and hypoxia as well as four different inspiratory resistances. When the ANOVA indicated a significant main effect and interaction, post-hoc paired sample t-test and pair-wise comparisons with the least significant difference were utilized to identify the effect of hypoxia and inspiratory resistance on physiological and subjective measurements. One-way repeated measures ANOVA was also used to determine if there were significant differences at each time point between the four conditions and to determine maximal workload at the four different inspiratory resistances. A simple linear regression was used to identify any association between maximal power output and dependent variables of interest (SpO2, VO2, VE, RR, HR, VT). The level of statistical significance was set at α ≤ 0.05 and all data are presented as mean ± standard deviation.
Results
Effects of normobaric hypoxia
Baseline measurements of SpO2, VO2, HR, and RER were similar between conditions (NN21 and NH17). SpO2, VO2, HR, and RER demonstrated a significant interaction (F = 7.868, p ≤ 0.001), (F = 38.042, p ≤ 0.001), (F = 6.459, p ≤ 0.001), and (F = 22.948, p ≤ 0.001), respectively. Subsequent paired sample t-tests revealed that SpO2 was significantly lower in NH17 than NN21 during the graded cycling exercise compared with baseline and rest (p ≤ 0.05, respectively). VO2 was significantly lower in NH17 than NN21, and was significantly increased during graded cycling exercise compared with baseline and rest (all, p ≤ 0.001, respectively). RER was significantly higher in NH17 compared with NN21 at 100 W (p = 0.009), 150 W (p ≤ 0.001), and maximal cycling exercise (p ≤ 0.001) (Table 1). HR was also significantly higher at 100 W (p = 0.43) and 150 W (p = 0.026) of submaximal cycling exercise in NH17 than NN21 (Table 1). Maximal power output and maximal oxygen uptake (VO2max) were signify cantly decreased in NH17 (p = 0.007, p ≤ 0.001, respectively). Maximal power output was significantly lower in NH17 (272 ± 44 W) than NN21 (300 ± 54 W). The average of the VO2max values was reduced 30 ± 9.6% in NH17 (Table 1).
Table 1.
Effect of Normobaric Hypoxia
| NN21 |
NH17 |
|||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| VO2 (mL/kg/min) | ||||
| Baseline | 3.5 | 0.4 | 3.7 | 0.4 |
| Rest | 4.0 | 0.7 | 3.8 | 0.5 |
| 50 W | 12.7 | 1.5 | 12.1 | 1.2 |
| 100 W | 19.0 | 2.7 | 17.9* | 2.4 |
| 150 W | 28.9 | 4.9 | 24.4* | 3.9 |
| Max | 46.1 | 8.9 | 31.8* | 4.1 |
| RER | ||||
| Baseline | 0.86 | 0.04 | 0.86 | 0.11 |
| Rest | 0.85 | 0.08 | 0.87 | 0.06 |
| 50 W | 0.88 | 0.03 | 0.91 | 0.05 |
| 100 W | 0.92 | 0.04 | 1.01* | 0.05 |
| 150 W | 0.95 | 0.03 | 1.12* | 0.08 |
| Max | 1.08 | 0.05 | 1.37* | 0.13 |
| SpO2 (%) | ||||
| Baseline | 98.0 | 0.5 | 97.9 | 0.8 |
| Rest | 98.0 | 1.2 | 93.3* | 3.3 |
| 50 W | 96.9 | 2.1 | 91.2* | 2.1 |
| 100 W | 97.3 | 0.7 | 91.6* | 2.4 |
| 150 W | 97.6 | 1.0 | 89.9* | 2.5 |
| Max | 97.0 | 1.5 | 92.8* | 3.2 |
| HR (bpm) | ||||
| Baseline | 69.7 | 10.0 | 71.2 | 7.6 |
| Rest | 67.7 | 5.9 | 72.7 | 9.1 |
| 50 W | 91.7 | 7.5 | 96.0 | 6.8 |
| 100 W | 112.7 | 10.2 | 121.7* | 4.9 |
| 150 W | 144.8 | 13.6 | 155.6* | 7.5 |
| Max | 178.4 | 16.7 | 174.3 | 10.9 |
p ≤ 0.05 versus NN21.
NN21, normobaric normoxia; NH17, normobaric hypoxia; VO2, oxygen uptake, RER, respiratory exchange ratio; SpO2, oxygen saturation as measured by pulse oximetry; HR, heart rate; bpm, beats per minute; SD, standard deviation.
Effects of inspiratory resistance in NH17
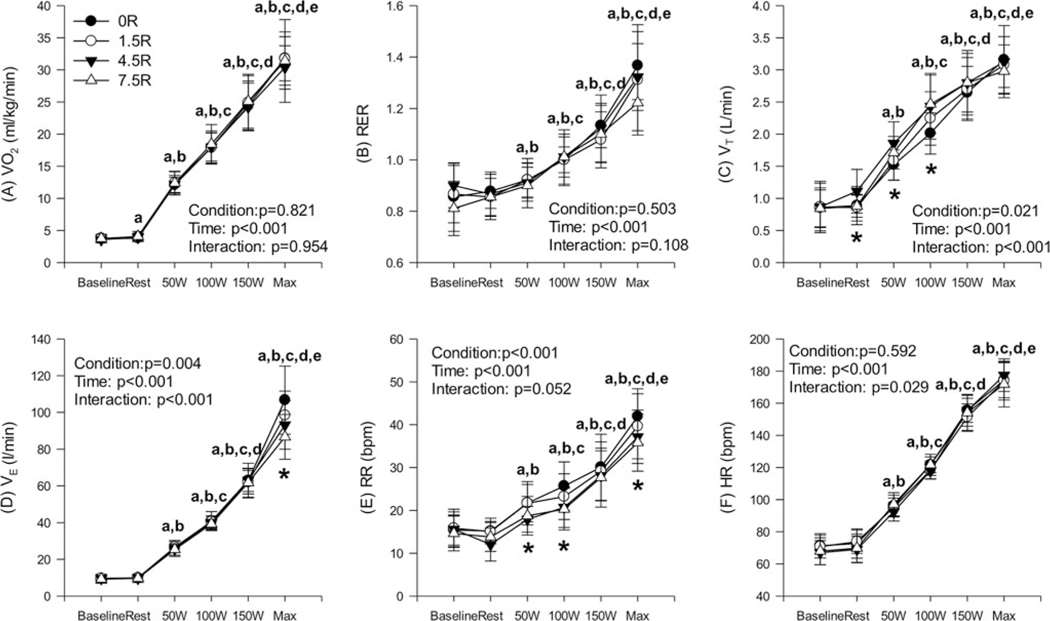
Physiological measurements were similar between the four inspiratory resistance conditions (R0, R1.5, R4.5, and R7.5) (p ≥ 0.05), respectively, at baseline. Also, there were no significant differences between baseline and resting parameters (p ≥ 0.05), except for VO2 (p = 0.047) and SpO2 (p ≤ 0.001) (Figs. 2 and 3).
FIG. 2.
Ventilatory and heart rate responses during graded cycling exercise with graded inspiratory resistance in normobaric hypoxia. ap ≤ 0.05 versus baseline; bp ≤ 0.05 versus rest in hypoxia; cp ≤ 0.05 versus 50 W; dp ≤ 0.05 versus 100 W; ep ≤ 0.05 versus 150 W. *p ≤ 0.05, a significant difference between conditions at given work load.
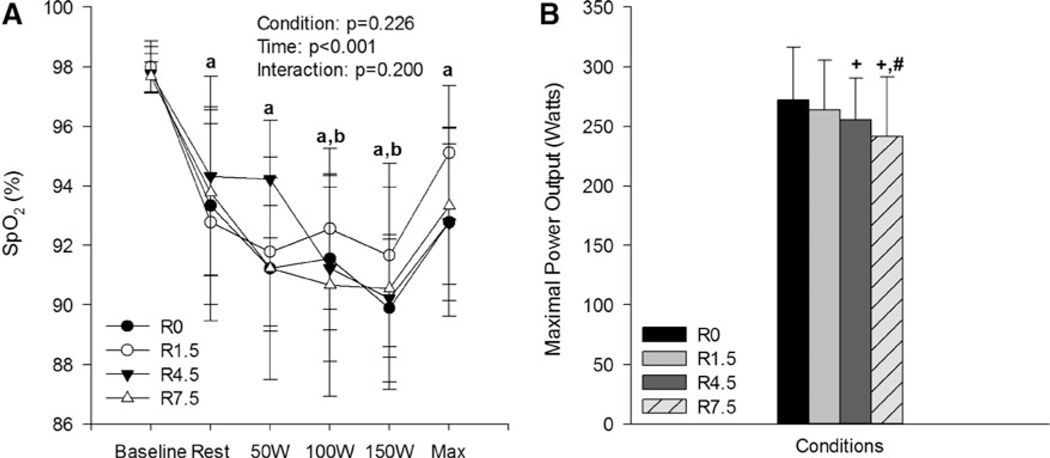
FIG. 3.
(A) SpO2 and (B) Maximal power outputs during graded cycling exercise with inspiratory resistance in normobaric hypoxia. ap ≤ 0.05 versus baseline; bp ≤ 0.05 versus rest in normobaric hypoxia. +p ≤ 0.05 versus R0; #p ≤ 0.05, versus R1.5 at maximal exercise in normobaric hypoxia. SpO2, oxygen saturation as measured by pulse oximetry.
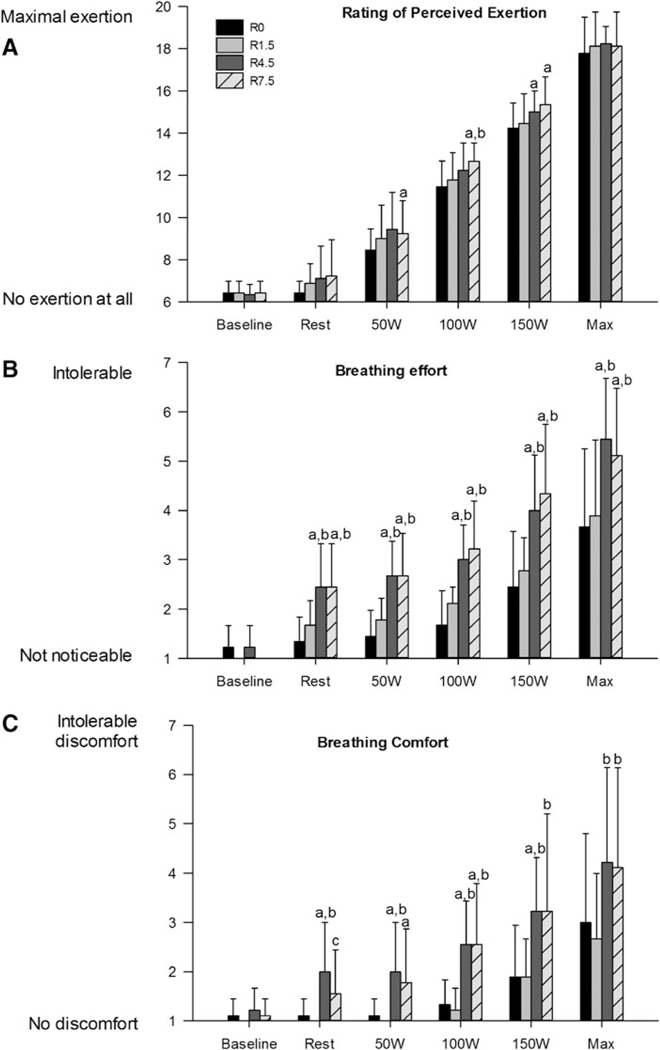
VO2, RER, VE, VT, RR, and HR increased during the graded cycling exercise compared with baseline and rest (p ≤ 0.05, respectively) (Fig. 2). Also, subjective measurements of RPE, BC, and BE were significantly higher during the graded cycling exercise compared with baseline and rest (p ≤ 0.05, all) (Fig. 4).
FIG. 4.
Subjective measurements of (A) rating of perceived exertion, (B) breathing effort, (C) breathing comfort during graded cycling exercise with inspiratory resistance in normobaric hypoxia. ap ≤ 0.05 versus R0; bp ≤ 0.05 versus R1.5; cp ≤ 0.05 versus R4.5 in normobaric hypoxia.
SpO2 was significantly decreased during graded cycling exercise compared with baseline. Also, SpO2 was significantly reduced at 100 W (p = 0.029) and 150 W (p ≤ 0.001) compared with rest in normobaric hypoxia (Fig. 3A).
There were significant changes on VT, VE, RPE, BE, and BC by conditions over time, but not RR (Figs. 2 and 4). At exhaustion, maximal power output was shown to be lowest in R7.5 followed by R4.5, R1.5, and R0 with maximal power output at R7.5 being significantly lower than R0 (p = 0.016) and R1.5 (p = 0.035) (Fig. 3B).
RR was significantly lower in R4.5 (p = 0.011) and R7.5 (p ≤ 0.001) compared with R0. Also, RR of R4.5 (p = 0.015) and R7.5 (p = 0.007) were significantly lower than R1.5. VT was only statistically higher in R4.5 compared with R1.5. (p = 0.041). However, VT trended toward significance in R4.5 (p = 0.06) and R7.5 (p = 0.054) compared with R0. VE was significantly lower in R7.5 compared with R0 (p = 0.003), R1.5 (p = 0.010), and R4.5 (p = 0.016), respectively). Furthermore, VE was significantly lower in R4.5 than R0 (p = 0.044).
RPE was significantly higher in R7.5 (p = 0.005) and R4.5 (p = 0.003) compared with R0. BC was significantly higher both in R7.5 (p = 0.025) and R4.5 (p = 0.007) compared with R0. Also, BC was significantly higher both in R7.5 (p = 0.001) and R4.5 (p = 0.013) compared with R1.5. BE was significantly higher both in R7.5 (p = 0.001) and R4.5 (p = 0.001) compared with R0. Also, BE was significantly higher both in R7.5 (p ≤ 0.001) and R4.5 (p ≤ 0.001) compared with R1.5.
A simple linear regression analysis for maximal power output with cardiopulmonary variables indicated a significant negative correlation with SpO2 (p = 0.021) and positive correlation with VE (p = 0.021), HR (p = 0.003), and VT (p = 0.025) in R0. VE (p = 0.015) and HR (p = 0.024) showed a significant positive correlation in R1.5, whereas HR showed a significant positive correlation in R7.5 condition (p = 0.025) (Table 2).
TABLE 2.
Correlation with Maximal Power Outputs in Four Different Conditions
| SpO2 | VE | VO2 | RR | HR | VT | |
|---|---|---|---|---|---|---|
| R0 | r = −0.747 | r =0.875 | r =0.270 | r =0.215 | r =0.891 | r = 0.730 |
| p = 0.021* | p = 0.021* | p = 0.483 | p = 0.578 | p = 0.003* | p = 0.025* | |
| R1.5 | r = 0.214 | r = 0.773 | r = 0.027 | r = 0.322 | r = 0.776 | r = 0.407 |
| p = 0.581 | p = 0.015* | p = 0.946 | p = 0.399 | p = 0.024* | p = 0.277 | |
| R4.5 | r = −0.155 | r = 0.570 | r = 0.122 | r =0.355 | r = 0.576 | r = 0.295 |
| p = 0.691 | p = 0.109 | p = 0.755 | p = 0.388 | p = 0.104 | p = 0.478 | |
| R7.5 | r = −0.283 | r = 0.450 | r =0.609 | r =0.521 | r = 0.773 | r = 0.287 |
| p = 0.460 | p = 0.224 | p = 0.082 | p = 0.150 | p = 0.025* | p = 0.454 |
p ≤ 0.05 significantly correlated with maximal power output. VE, minute ventilation; RR, respiratory rate; VT, tidal volume.
Discussion
We hypothesized that added inspiratory resistance would impair physical performance as measured by cardiorespiratory and perceptual responses. The main findings of this study were: (1) additional inspiratory resistance in a hypoxic environment limited the maximal power output (shorter time to exhaustion), whereas VO2max was not significantly impacted; (2) subjective measurement of BC and BE were significantly influenced by inspiratory resistance, whereas RPE did not significantly differ across four resistors.
NN21 versus NH17
Well-documented literature has shown that the stress of high altitude or hypoxia significantly limits physiological function and exercise performance (Pandolf et al., 1988). The present findings confirm a previous conclusion that SpO2, VO2max, and RER were significantly decreased during NH17, as well as maximal power output and VO2max were significantly decreased during NH17. Previous literature indicated that the onset of reduction in VO2max begins at an altitude of 589 m and linearly decreases approximately at a rate of 10% per 1000 m (Young et al., 1985; Pandolf et al., 1988; McArdle et al., 2001). Consequently, at an altitude of 4300 m or breathing 12.5% O2 gas mixture, VO2max decreases an average of 27%–28%, with individual variability from 9% to 54% decrement (Young et al., 1985). HR was also significantly higher in NH17 compared with NN21, which is in agreement with previous findings (Lhuissier et al., 2012) in that the maximal power output was relatively lower in hypoxia compared with normoxia for the same HR during submaximal exercise (20% and 40% maximal aerobic power).
Considering the current findings, in agreement with the previous work, it is important to note that occupational work performance at submaximal and maximal work rates in mild hypoxia, commonly experienced in some high-altitude cities, can potentially affect individuals negatively. Increased HR to complete the same absolute, submaximal task would likely result in earlier fatigue over time. Additionally, in an emergency or high-stress occupational environment requiring maximal effort, absolute work performance and ability may be compromised, potentially decreasing the workers’ health and safety.
Added inspiratory resistance in normobaric hypoxia
Baseline (normoxic) measurements were not different between applied resistances because subjects were not actively exercising, so that O2 requirements were low. The same is true for resting (hypoxic) conditions because SpO2 levels were sufficient to meet body requirements (Fig. 2). Furthermore, baseline and resting parameters did not differ because the resting body requirement for O2 is easily met at 17% O2 as observed in the SpO2 responses.
The lack of significant impact of inspiratory resistance on VO2 during exercise is interesting given that the addition of a resistive load increases ventilatory work (Powell and Williams, 2012). However, similar findings were reported in other studies addressing the effect of inspiratory resistance at various levels of fixed and staggered exercise in normobaric, normoxic conditions (Gee et al., 1968; Demedts and Anthonisen, 1973; Dressendorfer et al., 1977; Lerman et al., 1983; Jette et al., 1990; and Powell and Williams, 2012) and normobaric, hypoxic conditions (Mazzeo, 2008; Moon et al., 2016). This has led to the proposition by some researchers that inspiratory resistance does not negatively impact the performance of submaximal work in healthy individuals (Jette et al., 1990) and that the respiratory muscles must play a very minor role in limiting VO2 (Harber et al., 1984).
The fact that O2 consumption is constant at any given power output of submaximal exercise, irrespective of barometric pressure (Hill et al., 2011), implies that maintenance of energy requirement for the work of breathing under different inspiratory resistances is brought about through compensatory physiological responses. One suggested adaptation includes changes in the respiratory duty cycle (ratio of inspiratory time to total time of the respiratory cycle) that allows for prolonged retention time of inspired air in the lungs and subsequent enhanced O2 extraction (Jette et al., 1990), a premise that the increase in VT and decrease in RR in the present study potentially supports. Additional adaptations include increased anaerobic work to compensate for decreased levels of O2, and hypoventilation resulting in decreased respiratory work toward normal levels (Gee et al., 1968). Increases in HR to compensate for hypoxic conditions’ effects on O2 delivery and utilization have been put forth (Moon et al., 2016), but reduction in O2 delivery by beta-blockade of HR was compensated for by enhanced tissue O2 extraction during submaximal exercise (Mazzeo, 2008). Indeed, in the current study, HR was not significantly impacted by the increased inspiratory resistances (Fig. 2F), so that enhanced O2 extraction rather than increased cardiac output, may have been responsible for the maintenance of comparable VO2 among the various resistances during submaximal exercise.
On the other hand, the maximal power output (and thereby time to exhaustion) was adversely impacted by the increased inspiratory resistance, as reported similarly in other studies (Jette et al., 1990; Heus et al., 2004). This may result from the redistribution of available energy brought on by the recruitment of additional muscles of respiration to compensate for the effects of inspiratory resistance at higher work rates, as well as achievement of the lactate threshold prematurely (Jette et al., 1990; Heus et al., 2004). Energy distribution to the exercising muscles may be compromised by the additional burden of metabolic requirement to the respiratory musculature. It is also feasible that significantly impaired perceptual breathing responses may have limited the participants’ mental ability to reach their highest maximal power output potential. Decreased BC and increased BE at the higher two resistances may have resulted in a discomfort, thereby influencing early time to exhaustion.
Several previous studies have reported breathing discomfort and difficulty with common low resistance filtering facepiece respirators, such as N95 respirators (Bryce et al., 2008; Baig et al., 2010; Mitchell et al., 2012). Another study showed only minimal subjective differences in prototype respirators with 3, 6, and 9 mm H2O resistances at a low-moderate work rate for 60 minutes (Roberge et al., 2013). However, the current study found deteriorated perceptual measurements of BC and effort at high inspiratory resistances. This is in agreement with a previous study showing lower ratings of comfort with increasing inspiratory resistance from 0.78 to 7.64 cm H2O/L/Sec while walking at 80%–85% VO2max (Johnson et al., 1999). These data, taken together, suggest that breathing discomfort and difficulty may be positively related to inspiratory resistance level. While various studies have shown impaired subjective comfort at differing resistances and workloads, it remains clear that the negative practical impact of added inspiratory resistance to the end user exists, which may impact respirator use and standard conformity. It is important to consider such perceptions when recommending respirators for use or designing new and improved respirators with varying acceptable levels of inspiratory resistance.
Limitations of the study
Several limitations to this study should be noted. First, the low sample size of nine subjects, although large enough to detect significant differences in the main outcomes, may have limited this study in its ability to detect smaller changes in secondary outcome variables. Second, the subject population was limited to only young, healthy males. As such, the external validity of these findings to a coed work force is limited. Lastly, a level of environmental hypoxia implemented in this study is quite moderate, although covering a significant number of the population in high-altitude cities; therefore, the current results should be interpreted with caution when applied to workers at higher altitudes.
Additionally, several strengths of this analysis must be considered. This study provided a novel experimental design, allowing the experimentation of both the effects of environmental hypoxia as well as inspiratory resistance, independently and concurrently. Second, the use of several different inspiratory resistances allowed for the current study to examine and compare physiological and perceptual differences within levels of inspiratory resistances rather than just compared with no resistance.
While the current literature is compelling, future research is warranted to further investigate physiological and perceptual effects of varying inspiratory/expiratory resistances. Especially, deeper investigation into the seemingly complex perceptual threshold and comfort responses to the addition of breathing resistance in severe environmental and pathologic (e.g., asthma) hypoxic conditions is warranted.
Conclusion
The effect of low-to-moderate inspiratory resistance in situations with moderately reduced normobaric, ambient oxygen content does not have a deleterious effect on human oxygen consumption at submaximal work rates over short periods of time. However, added inspiratory resistance of greater than 4.5 cm H2O/L/Sec at maximal work rates significantly decreases the time to exhaustion and maximal power output. While limiting maximal power output and impairing perceived BC and effort with increased inspiratory resistance, respiratory protection of high, but acceptable, inspiratory resistance, may reduce the likelihood of an individual using the respirator properly or as often. Therefore, perceptual and physiological characteristics of different respirators of varying acceptable levels of inspiratory resistances should be considered by manufacturers and end users during design and respiratory selection processes.
Acknowledgments
The authors would like to acknowledge the study participants who generously volunteered their time to participate in this study, and are much appreciated. This research was supported by contract from the National Institute for Occupational Safety and Health, and Centers for Disease Control and Prevention (200-2016-M88553).
The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health. Mention of commercial products does not constitute endorsement by the National Institute for Occupational Safety and Health.
Footnotes
Author Disclosure Statement
No competing financial interests exist.
References
- Baig AS, Knapp C, Eagan AE, and Radonovich LJ Jr (2010). Health care workers’ views about respirator use and features that should be included in the next generation of respirators. Am J Infect Control 38:18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckett WS. (2000). Occupational respiratory diseases. N Engl J Med 342:406–413. [DOI] [PubMed] [Google Scholar]
- Borg GA. (1982). Psychophysical bases of perceived exertion. Med Sci Sports Exerc 14:377–381. [PubMed] [Google Scholar]
- Bryce E, Forrester L, Scharf S, and Eshghpour M. (2008). What do healthcare workers think? A survey of facial protection equipment user preferences. J Hosp Infect 68:241–247. [DOI] [PubMed] [Google Scholar]
- Crow TJ, and Kelman GR. (1973). Psychological effects of mild acute hypoxia. Br J Anaesth 45:335–337. [DOI] [PubMed] [Google Scholar]
- Demedts M, and Anthonisen NR. (1973). Effects of increased external airway resistance during steady-state exercise. J Appl Physiol 35:361–366. [DOI] [PubMed] [Google Scholar]
- Deno NS, Kamon E, and Kiser DM. (1981). Physiological responses to resistance breathing during short and prolonged exercise. Am Ind Hyg Assoc J 42:616–623. [DOI] [PubMed] [Google Scholar]
- Dressendorfer RH, Wade CE, and Bernauer EM. (1977). Combined effects of breathing resistance and hyperoxia on aerobic work tolerance. J Appl Physiol Respir Environ Exerc Physiol 42:444–448. [DOI] [PubMed] [Google Scholar]
- Fukakusa J, Rosenblat J, Jang B, Ribeiro M, Kudla I, and Tarlo S. (2011). Factors influencing respirator use at work in respiratory patients. Occup Med 61:576–582. [DOI] [PubMed] [Google Scholar]
- Gee J, Burton G, Vassallo C, and Gregg J. (1968). Effects of external airway obstruction on work capacity and pulmonary gas exchange. Am Rev Respir Dis 98:1003–1012. [DOI] [PubMed] [Google Scholar]
- Harber P, Tamimie J, Emory J, Bhattacharya A, and Barber M. (1984). Effects of exercise using industrial respirators. Am Ind Hyg Assoc J 45:603–609. [DOI] [PubMed] [Google Scholar]
- Heus R, den Hartog EA, Kistemaker LJ, van Dijk WJ, and Swenker G. (2004). Influence of inspiratory resistance on performance during graded exercise tests on a cycle ergometer. Appl Ergon 35:583–590. [DOI] [PubMed] [Google Scholar]
- Hill NE, Stacey MJ, and Woods DR. (2011). Energy at high altitude. J R Army Med Corps 157:43–48. [DOI] [PubMed] [Google Scholar]
- Jette M, Thoden J, and Livingstone S. (1990). Physiological effects of inspiratory resistance on progressive aerobic work. Eur J Appl Physiol Occup Physiol 60:65–70. [DOI] [PubMed] [Google Scholar]
- Johnson AT, Dooly CR, and Dotson CO. (1995). Respirator mask effects on exercise metabolic measures. Am Ind Hyg Assoc J 56:467–473. [DOI] [PubMed] [Google Scholar]
- Johnson AT, Scott WH, Lausted CG, Benjamin MB, Coyne KM, Sahota MS, and Johnson MM. (1999). Effect of respirator inspiratory resistance level on constant load treadmill work performance. Am Ind Hyg Assoc J 60:474–479. [DOI] [PubMed] [Google Scholar]
- Khatri SB, and Ioachimescu OC. (2016). The intersection of obstructive lung disease and sleep apnea. Cleve Clin J Med 83:127–140. [DOI] [PubMed] [Google Scholar]
- Laciga P, and Koller EA. (1976). Respiratory, circulatory, and ECG changes during acute exposure to high altitude. J Appl Physiol 41:159–167. [DOI] [PubMed] [Google Scholar]
- Lerman Y, Shefer A, Epstein Y, and Keren G. (1983). External inspiratory resistance of protective respiratory devices: Effects on physical performance and respiratory function. Am J Ind Med 4:733–740. [DOI] [PubMed] [Google Scholar]
- Lhuissier FJ, Brumm M, Ramier D, and Richalet JP. (2012). Ventilatory and cardiac responses to hypoxia at submaximal exercise are independent of altitude and exercise intensity. J Appl Physiol (1985) 112:566–570. [DOI] [PubMed] [Google Scholar]
- Louhevaara V, Tuomi T, Korhonen O, and Jaakkola J. (1984). Cardiorespiratory effects of respiratory protective devices during exercise in well-trained men. Eur J Appl Physiol Occup Physiol 52:340–345. [DOI] [PubMed] [Google Scholar]
- Mazzeo RS. (2008). Physiological responses to exercise at altitude: An update. Sports Med 38:1–8. [DOI] [PubMed] [Google Scholar]
- McArdle WD, Katch FI, and Katch VL. (2001). Exercise Physiology: Energy, Nutrition, and Human Performance. Lippincott Williams and Wilkins, Philadelphia, PA. [Google Scholar]
- Mitchell R, Ogunremi T, Astrakianakis G, Bryce E, Gervais R, Gravel D, Johnston L, Leduc S, Roth V, Taylor G, et al. (2012). Impact of the 2009 influenza A (H1N1) pandemic on Canadian health care workers: A survey on vaccination, illness, absenteeism, and personal protective equipment. Am J Infect Control 40:611–616. [DOI] [PubMed] [Google Scholar]
- Moon H-W, Sunoo S, Park H-Y, Lee D-J, and Nam S-S. (2016). Effects of various acute hypoxic conditions on metabolic parameters and cardiac function during exercise and recovery. SpringerPlus 5:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandolf KB, Sawka MN, and Gonzalez RR. (1988). Human Performance Physiology and Environmental Medicine at Terrestrial Extremes. Brown and Benchmark Press, Indianapolis, IN. [Google Scholar]
- Powell T, and Williams EM. (2012). Effect of resistive load on the inspiratory work and power of breathing during exertion. PLoS One 7:e49681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raven PB, Davis TO, Shafer CL, and Linnebur AC. (1977). Maximal stress test performance while wearing a self-contained breathing apparatus. J Occup Med 19:802–806. [DOI] [PubMed] [Google Scholar]
- Roberge RJ, Kim J-H, Powell JB, Shaffer RE, Ylitalo CM, and Sebastian JM. (2013). Impact of low filter resistances on subjective and physiological responses to filtering facepiece respirators. PLoS One 8:e84901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shykoff BE, and Warkander DE. (2011). Physiologically acceptable resistance of an air purifying respirator. Ergonomics 54:1186–1196. [DOI] [PubMed] [Google Scholar]
- Stemler F, and Craig F. (1977). Effects of respiratory equipment on endurance in hard work. J Appl Physiol Respir Environ Exerc Physiol 42:28–32. [DOI] [PubMed] [Google Scholar]
- Young AJ, Cymerman A, and Burse RL. (1985). The influence of cardiorespiratory fitness on the decrement in maximal aerobic power at high altitude. Eur J Appl Physiol Occup Physiol 54:12–15. [DOI] [PubMed] [Google Scholar]