Graphical abstract
Keywords: Cardiac cysts, Pericardial cyst, Bronchogenic cyst, Hepatic cyst, Blood cyst, Duplication cyst, Paracardiac cyst
Highlights
-
•
Paracardiac cysts (located adjacent to or inside the heart) are rarely detected.
-
•
There is a broad differential diagnosis for cysts encountered with echocardiography.
-
•
Multimodality imaging is crucial for comprehensively evaluating paracardiac cysts.
Introduction
Paracardiac cysts, or cysts located adjacent to or inside the heart, are rarely diagnosed by cardiac imaging, occurring in <0.1% of echocardiograms. Using echocardiography, computed tomography (CT), and magnetic resonance imaging (MRI), we highlight the broad differential diagnosis for these structures by presenting 5 unique types of paracardiac cysts: pericardial, esophageal duplication, bronchogenic, blood, and hepatic. Advanced echocardiographic strategies, including microbubble ultrasound enhancement agents (UEAs), are also demonstrated. This case series emphasizes the integral role of multimodality strategies for comprehensively evaluating and determining the most appropriate, personalized treatment plan for paracardiac cysts.
Case Presentations
Case 1: Pericardial Cyst
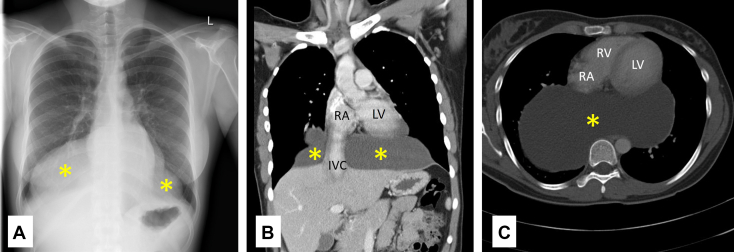
A 22-year-old woman with no medical history presented to the emergency room after an episode of loss of consciousness. The physical exam was unremarkable, and basic laboratory testing was normal. The electrocardiogram (ECG) showed normal sinus rhythm. Chest radiography demonstrated a markedly enlarged cardiac silhouette with an abnormal right heart border (Figure 1A).
Figure 1.
Pericardial cyst. (A) Chest x-ray with a markedly enlarged cardiac silhouette with an abnormal right heart border. Panels B (coronal view) and C (axial view) display chest CT imaging with iodinated contrast showing a large pericardial cyst (indicated by yellow asterisks) within the posterior mediastinum measuring 21.5 × 11.4 × 14.2 cm, contiguous with the pericardium. IVC, Inferior vena cava; LV, left ventricle; RA, right atrium; RV, right ventricle.
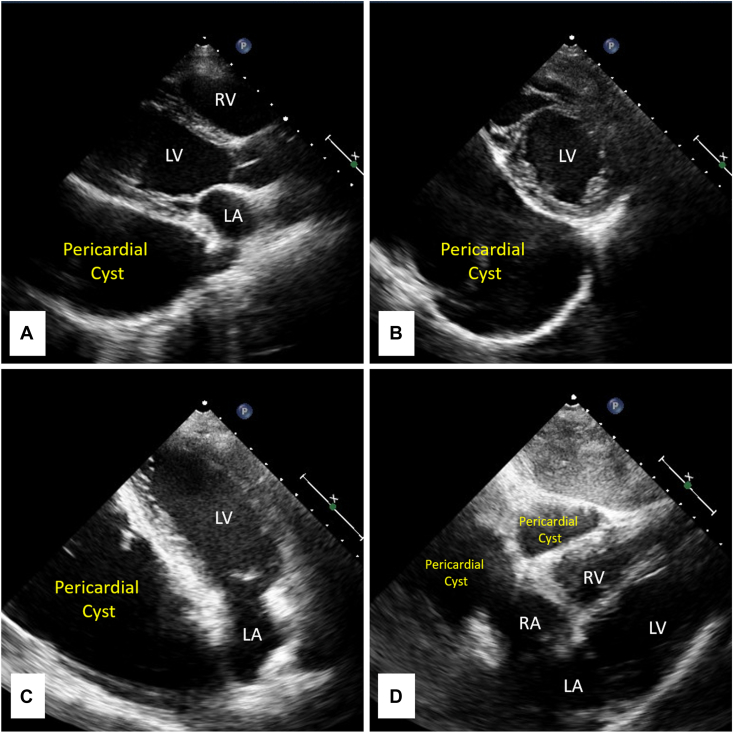
Transthoracic echocardiography (TTE), performed due to the abnormal chest x-ray, revealed normal biventricular systolic global and regional function. A round, well-circumscribed echolucent lesion was incidentally detected behind the heart (Figure 2). Chest CT imaging with iodinated contrast showed a large fluid collection within the posterior mediastinum measuring 21.5 × 11.4 × 14.2 cm, contiguous with the pericardium (Figure 1B and C). Cytology from a fine-needle aspiration found clear fluid without malignant or inflammatory cells. These findings were diagnostic of a pericardial cyst.
Figure 2.
Pericardial cyst. Transthoracic echocardiography showing a round, well-circumscribed echolucent lesion behind the heart. (A) Parasternal long-axis view. (B) Parasternal short-axis view. (C) Apical 2-chamber view. (D) Subcostal view. This figure corresponds to Video 1. LV, Left ventricle; RA, right atrium; RV, right ventricle.
Case 2: Esophageal Duplication Cyst
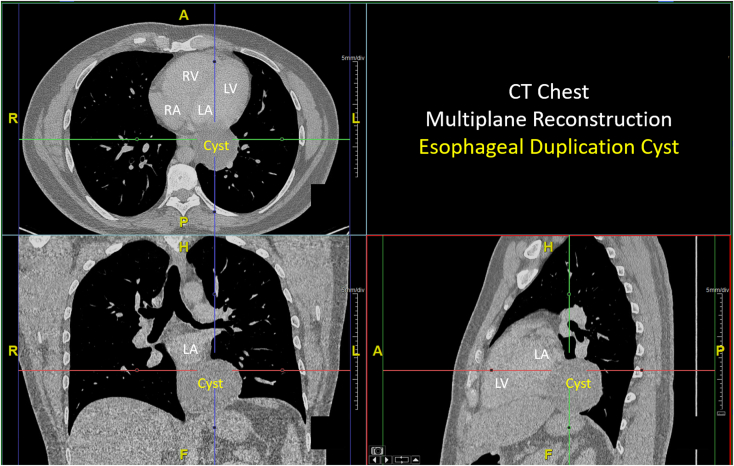
A 32-year-old man with a history of diabetes mellitus presented for a physical exam prior to enlisting in the United States Navy. An absent left testicle was noted. The physical exam was otherwise normal. Subsequently, an abdominal CT scan, performed due to the abnormal physical examination, revealed an undescended left testicle as well as an incidental finding of a large ovoid retrocardiac lesion. A dedicated chest CT with iodinated contrast showed the lesion to be a large mediastinal cyst measuring 6.3 × 7.0 × 6.0 cm (Figure 3). The cyst had a low radiodensity (27 Hounsfield units) and was inseparable from the heart, esophagus, and diaphragm.
Figure 3.
Esophageal cyst. Multiplanar reconstruction of chest CT imaging with iodinated contrast showing a large mediastinal cyst measuring 6.3 × 7.0 × 6.0 cm. The cyst has a low radiodensity (27 Hounsfield units) and is inseparable from the heart, esophagus, and diaphragm. LV, Left ventricle; RA, right atrium; RV, right ventricle.
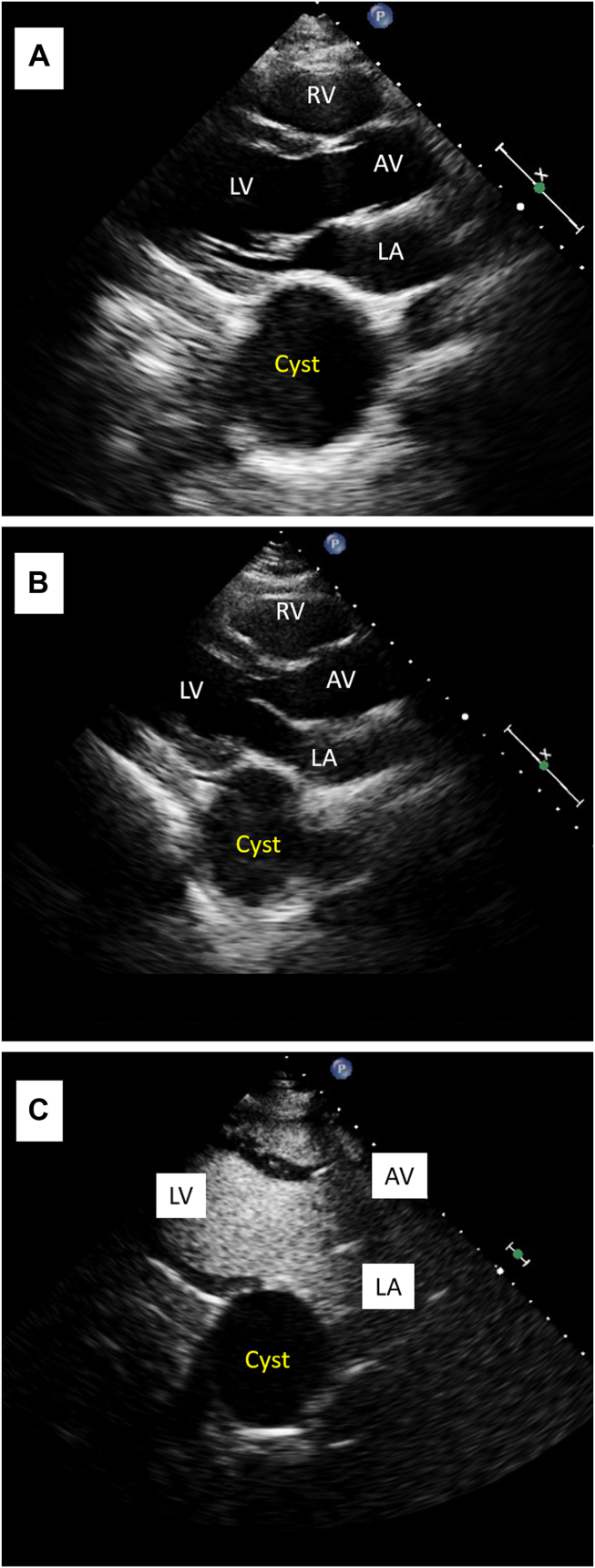
A TTE demonstrated normal biventricular systolic global and regional function and anatomy. However, posterior to the left atrium (LA), there was a large globular, echolucent cystic structure (Figure 4A, Video 2). After the patient drank a carbonated beverage, no bubbles were seen in the cystic structure, supporting the conclusion that the cyst was not in communication with the upper gastrointestinal tract (Figure 4B). After intravenous (IV) injection of activated perflutren lipid microsphere UEA, no bubbles appeared in the cyst, indicating that it was not a vascular structure (Figure 4C, Video 3). Overall CT and TTE findings were suggestive of either an enterogenic duplication cyst or a bronchogenic cyst.
Figure 4.
Esophageal cyst. (A) Transthoracic echocardiography in the parasternal long-axis view showing a large globular, echolucent cystic structure posterior to the LA. (B) The same view immediately after the patient drank a carbonated beverage. No bubbles were seen in the cystic structure, supporting the conclusion that the cyst was not in communication with the upper gastrointestinal tract. (C) The same view immediately after an IV injection of activated perflutren lipid microsphere UEA. No bubbles appeared in the cyst, indicating that it was not a vascular structure. This figure corresponds to Video 3. AV, Aortic valve; LV, left ventricle; RV, right ventricle.
Given the cyst’s potential for future esophageal compression and malignant transformation, the patient then underwent a resection of the cyst with regional lymph node biopsy. Surgical pathology revealed normal lymph nodes and a benign, epithelium-lined cyst with partial denudation, wall fibrosis, and chronic inflammation, consistent with esophageal duplication cyst. They are now doing well and preparing to reapply to the navy.
Case 3: Bronchogenic Cyst
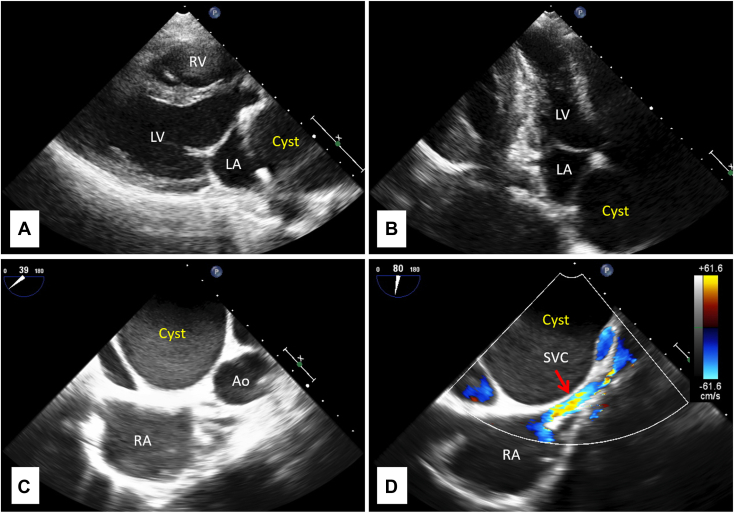
A 29-year-old woman with a history of Hashimoto’s thyroiditis presented with new-onset palpitations. The physical exam was normal except for an irregular heart rhythm. An ECG demonstrated atrial fibrillation. Transthoracic and transesophageal echocardiography (TEE) imaging done in preparation of cardioversion of atrial fibrillation demonstrated normal biventricular systolic global and regional function and anatomy. Additionally, there was a round, well-circumscribed echolucent extracardiac lesion measuring 5.5 cm in diameter and extrinsically compressing the LA (Figure 5, Videos 4 and 5).
Figure 5.
Bronchogenic cyst. (A) Transthoracic echocardiography parasternal long-axis view showing a round, well-circumscribed echolucent extracardiac lesion measuring 5.5 cm in diameter and extrinsically compressing the LA. (B) Apical 2-chamber view from TTE again demonstrating the lesion. (C) Transesophageal echocardiography midesophageal short-axis view at the level of the aortic valve showing the cyst’s proximity to the right atrium. (D) Transesophageal echocardiography midesophageal bicaval view with color Doppler demonstrating the cyst compressing the SVC. This figure corresponds to Videos 4 and 5. Ao, Aorta; LV, left ventricle; RA, right atrium; RV, right ventricle.
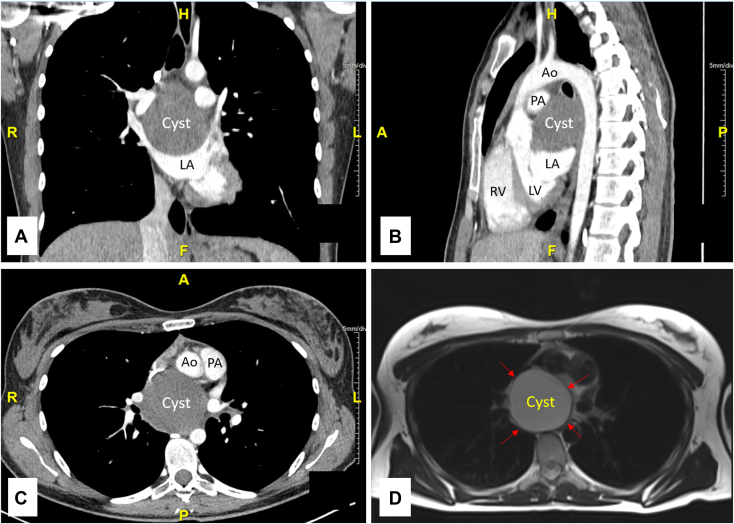
Chest CT imaging with iodinated contrast showed a hypodense, subcarinal, middle mediastinal mass causing extrinsic compression of the superior wall of the LA, right inferior pulmonary vein, superior vena cava (SVC), and right main pulmonary artery (Figure 6A-C). A magnetic resonance scan was obtained for tissue characterization and demonstrated the lesion to be without internal enhancement but with mild peripheral rim enhancement on T2 sequences (Figure 6D). Based on the above multimodality imaging, the differential diagnosis included a bronchogenic cyst or an esophageal or enterogenic duplication cyst.
Figure 6.
Bronchogenic cyst. (A, B, C) Multiplanar reconstructions of chest CT imaging with iodinated contrast in the coronal, sagittal, and axial views, respectively, showing a hypodense, subcarinal, middle mediastinal mass causing extrinsic compression of the superior wall of the LA, right inferior pulmonary vein, SVC, and right main PA. (D) Chest MRI T2 imaging demonstrating the lesion to be without internal enhancement but with mild peripheral rim enhancement as indicated by the red arrows. Ao, Aorta; LV, left ventricle; PA, pulmonary artery; RV, right ventricle.
Given the LA compression and resulting atrial arrhythmia, a surgical resection of the lesion with regional lymph node biopsy was performed. During surgery, the cyst was noted to be productive of white milky fluid. Fluid analysis from the cyst found macrophages, amorphous material, degenerated nonviable cellular debris, and occasional detached cilia tufts. Histologic evaluation was consistent with inflamed walls of a bronchogenic cyst. Atrial fibrillation resolved 2 weeks later, and the patient is now doing well.
Case 4: Blood Cyst
A 45-year-old woman with no medical history presented with new-onset exertional dyspnea. Aside from a faint systolic murmur along their left upper sternal border, the physical exam was normal. An ECG showed normal sinus rhythm. Laboratory testing was unremarkable.
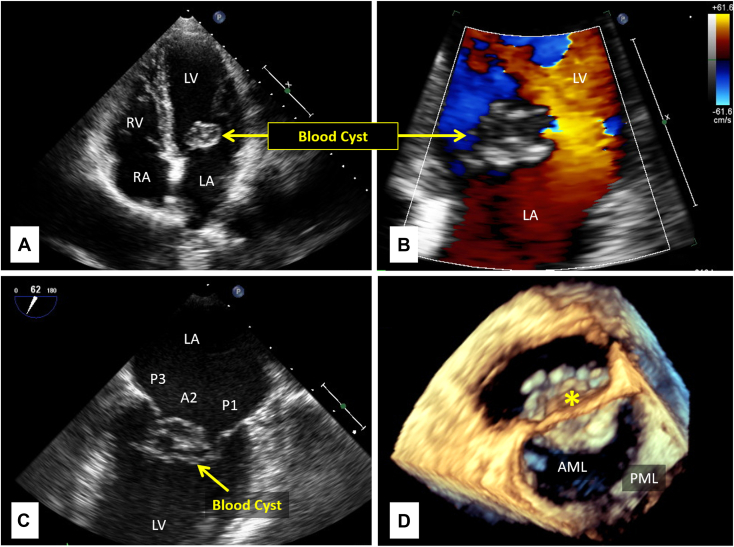
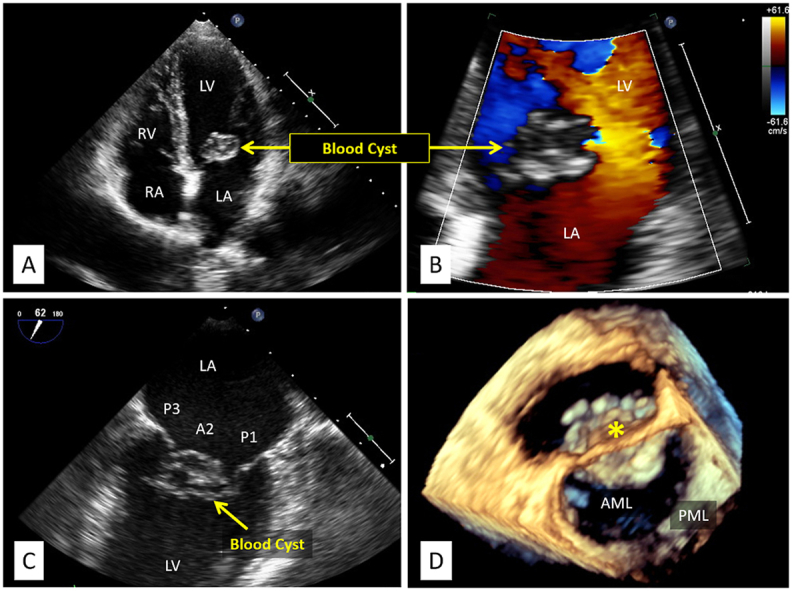
Transthoracic echocardiography demonstrated mild mitral regurgitation as well as a 2.0 × 1.4 cm septated, cystic structure associated with the anterior mitral valve (MV) leaflet. There was no evidence of left ventricular outflow tract obstruction or other valvular pathology (Figure 7A and B, Video 6). Two- and three-dimensional TEE imaging further assisted in characterizing the cyst (Figure 7C and D, respectively; Video 7). Transesophageal echocardiography imaging with IV injection of activated perflutren lipid microsphere UEA demonstrated delayed filling of the lesion, indicating its limited communication with the blood pool. Overall TTE and TEE findings were suggestive of a blood cyst.
Figure 7.
Blood cyst. (A) Transthoracic echocardiography apical 4-chamber view showing a 2.0 × 1.4 cm septated, cystic structure associated with the anterior MV leaflet. (B) Apical 2-chamber view with color Doppler showing the cystic structure’s disruption of laminar flow into the left ventricle. (C) Transesophageal echocardiography in the midesophageal bicommissural view again demonstrating the cystic lesion’s association with the anterior MV leaflet. (D) Three-dimensional TEE zoomed-in approximate surgical view of the MV showing the morphology of the cyst as indicated by the yellow asterisk. This figure corresponds to Videos 6 and 7. A2, Anterior MV second scallop; AML, anterior mitral leaflet; LV, left ventricle; P1, posterior MV first scallop; P3, posterior MV third segment; PML, posterior mitral leaflet; RA, right atrium; RV, right ventricle.
A year later, a repeat TTE showed no interval change to the blood cyst. They continue to follow up with a cardiologist and are doing well.
Case 5: Hepatic Cyst
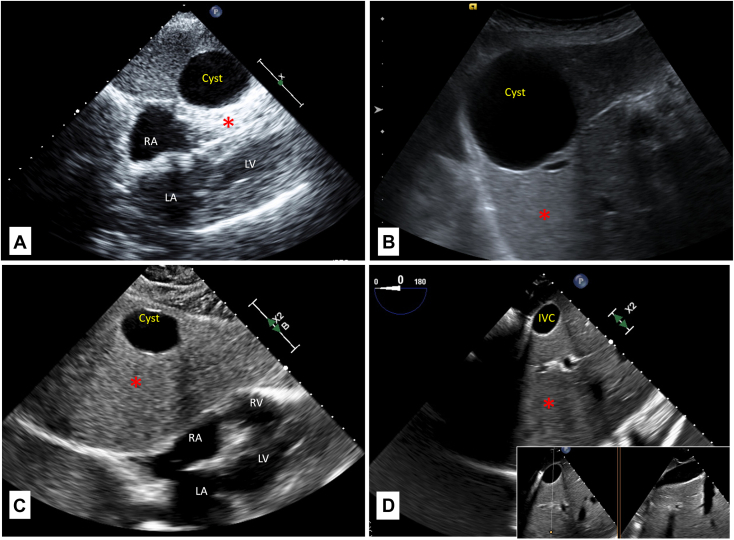
An 83-year-old woman with a history of diverticulitis and chronic obstructive pulmonary disease presented with shortness of breath and was referred for TTE, which revealed normal biventricular systolic global and regional function and anatomy. The physical exam was normal. On subcostal views there was an incidental finding of an anechoic, unilocular, circumferential structure along the superior aspect of the liver. It measured 4.0 cm in diameter and demonstrated characteristic acoustic enhancement artifact in the far field. The findings were consistent with a hepatic cyst (Figure 8A, Video 8). The cyst did not encroach on the heart or result in right atrial inflow obstruction.
Figure 8.
Hepatic cyst. (A) Transthoracic echocardiography subcostal view from the presented patient showing an anechoic, unilocular, circumferential structure along the superior aspect of the liver. It measured 4 cm in diameter and demonstrated characteristic acoustic enhancement artifact in the far field (red asterisks). This panel corresponds to Video 8. (B) Dedicated abdominal ultrasound from the presented patient showing a simple cyst measuring 3.7 × 4.0 × 4.5 cm. (C) Example of a simple hepatic cyst detected with TTE with clearly demonstrated posterior acoustic enhancement. This panel corresponds to Video 9. (D) Short axis of IVC with posterior acoustic enhancement (red asterisk), which should not be confused with a hepatic cyst. The insert is a simultaneous biplane view through the IVC demonstrating that the circular structure in the left panel corresponds to the long axis of IVC in the right panel. This panel corresponds to Video 10. IVC, Inferior vena cava; LV, left ventricle; RA, right atrium; RV, right ventricle.
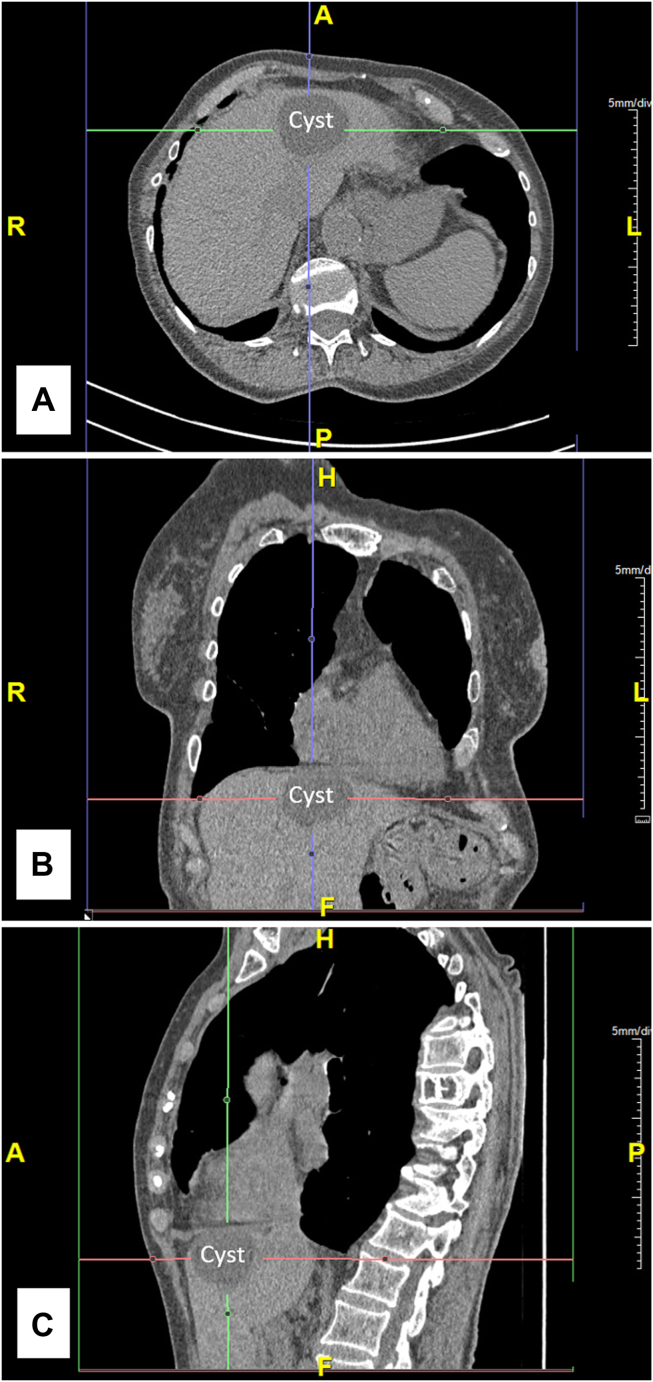
A dedicated abdominal ultrasound found a simple cyst measuring 3.7 × 4.0 × 4.5 cm (Figure 8B). The liver was enlarged with normal overall echotexture and a patent main portal vein. Multiple kidney cysts were also detected. The hepatic cyst was also noted on chest CT imaging, and its contents measured 3 Hounsfield units, consistent with hypodense fluid with attenuation similar to water (Figure 9).
Figure 9.
Hepatic cyst. Multiplanar reconstruction CT chest imaging with iodinated contrast showing a cystic structure within the liver. The cyst did not encroach on the heart or inflow vessels. Its contents measured 3 Hounsfield units, consistent with bland fluid. (A) Axial view. (B) Coronal view. (C) Sagittal view.
The patient is planned for repeat surveillance abdominal imaging.
Discussion
Paracardiac cysts, or cysts located adjacent to or inside the heart, can originate from any structure within or near the mediastinum. They are rarely diagnosed on clinical echocardiograms, with a reported rate of <0.1% of studies, and the differential diagnosis is broad.1,2 Many are benign but occasionally present within a variety of clinical settings including arrhythmias, signs of structural heart disease, SVC syndrome, and post–obstructive pneumonia.3 This case series includes examples of pericardial, esophageal duplication, bronchogenic, blood, and hepatic cysts and discusses strategies for characterizing these findings on TTE with comparisons to other imaging modalities.
Differential Diagnosis
Pericardial cysts are congenital lesions that occur due to incomplete fusion of the mesenchymal lacunae that form the pericardium during fetal development.4,5 Their estimated prevalence is 1 in 100,000 people, and they are usually found in the right anterior cardiophrenic angle.4,6 They are often incidentally identified on chest radiography and appear as an enlarged contour of the right heart border but may alter other cardiac borders as well.5, 6, 7 Sometimes pericardial cysts resolve spontaneously, although, similar to the other paracardiac cysts, they can also enlarge and eventually result in compromise of other mediastinal structures.
Enterogenic (including esophageal) duplication and bronchogenic cysts are frequently classified under the umbrella of foregut duplication cysts, given their similar embryologic origins. The foregut forms both the upper gastrointestinal tract from the mouth to the duodenum as well as the lower respiratory tract via the respiratory bud.8,9 Frequently, these cysts do not communicate with their respective structures of origin. While infrequent, these cysts can undergo malignant conversion or become a nidus of infection.6,8,9 Distinguishing between foregut duplication cysts is challenging, and the diagnosis is often not determined until surgical resection and histopathologic analysis.
Blood cysts are sometimes found on heart valves during postmortem examinations of newborns and seldom persist beyond childhood.10,11 As such, there are scarce reports of these structures in adult patients. They are thought to be formed by trapped blood during valve development in utero but may also be acquired following surgery or trauma.10,11 Histologically, these cysts are composed of fibromyxoid walls with an internal lining of endothelial cells and filled with nonorganized blood.10,12 They occasionally result in incomplete coaptation of MV leaflets, causing severe mitral regurgitation or left ventricular outflow tract obstruction.11
Hepatic cysts are common, usually benign malformations within the liver that are found in 2% to 18% of the general population.13 Most are considered simple, which are characterized by thin, smooth walls and up to 2 septa.14 Simple cysts are frequently congenital and formed by biliary ducts that do not communicate with the rest of the biliary system.14 They may also be associated with disorders like polycystic kidney disease.14 Malignancies and parasitic infections also result in hepatic cysts, although these tend to have complex features like multiple septa and mural thickening.13,14 While usually located within the liver parenchyma, hepatic cysts can sometimes encroach into the thorax and directly neighbor the pericardium or interfere with other cardiac structures, including compression of the right atrium.13 Hepatic cysts are often an incidental finding on TTE using limited liver views. For complete evaluation of hepatic cysts, including their number and location as well as the frequency of imaging follow-up, dedicated liver imaging with abdominal ultrasound or advanced tomographic imaging tools should be considered.
While this case series highlights 5 different types of paracardiac cysts, the differential diagnosis is extensive and additionally includes, but is not limited to, thymic cysts, meningoceles, lymphovascular malformations, and neoplasms.15
Imaging Characterization
In the majority of the presented cases, patients were referred for TTE following the detection of paracardiac lesions on other imaging modalities. In the remainder of cases, patients presented with nonspecific chest symptoms.
Transthoracic echocardiography is often considered the initial imaging modality of choice when attempting to characterize paracardiac cystic structures in addition to comprehensively assessing cardiac structure and function in a noninvasive, real-time manner.11 Upon detection of cystic structures, it is important to describe not only their size but also their location, echogenicity, and whether there is communication with surrounding structures (Table 1).
Table 1.
Characteristics of paracardiac cysts
| Pericardial cysts | Foregut duplication cysts | Blood cysts | Hepatic cysts | |
|---|---|---|---|---|
| Location | On any pericardial surface | Usually behind the heart | On any endocardial surface of the heart | Inferior to the heart |
| Echogenicity | Anechoic | Variable | Anechoic | Variable |
| Communication | None | None | Variable | None |
| Additional Characteristics | Frequently detected by abnormal right heart border on chest x-ray. | Frequently filled with proteinaceous fluid. | May have communication with general blood pool through microchannels in cyst walls. | Simple cysts are anechoic, while complex ones are hazy. |
Location
Correct localization assists in the appropriate identification of a paracardiac cyst. An understanding of both normal anatomy and basic embryology is crucial given that cysts typically arise as malformations during development. Cysts detected posterior to the left ventricle tend to originate from either the heart itself or the adjacent organs of the middle and posterior mediastinum (i.e., bronchi and esophagus).16 Cysts found in front of the heart are more likely from a cardiac structure or an anterior mediastinal structure, although a large cyst in another space may displace normal anatomy. During echocardiography, cysts can be difficult to differentiate from loculated pericardial effusions, with the distinction being a thin wall separating the cyst from the main pericardial space.7 Cardiac imagers may also encounter cysts outside of the chest, including hepatic cysts, which are frequently found on comprehensive TTE exams while scanning through the liver to acquire subcostal views.
Echogenicity
Another characteristic feature of paracardiac cysts is their echogenicity. Cysts filled with low-density fluids like water or unclotted blood will appear anechoic, whereas proteinaceous fluid that is more viscous will look hazy with ultrasound imaging. Fluid-filled structures, such as cysts and blood vessels, may also exhibit posterior acoustic enhancement (Figure 8C and D, Videos 9 and 10). Pericardial and blood cysts usually appear as anechoic.11,12 However, the contents of bronchogenic duplication and enterogenic cysts vary, and they are occasionally filled with protein- or calcium-rich fluids that appear hazy during echocardiography.17 Fluid echogenicity also helps differentiate simple from complex hepatic cysts: simple cysts are anechoic, while complex cysts may have very proteinaceous contents or contain debris.14
Communication With Surrounding Structures
A comprehensive TTE examination should also attempt to discern whether a cyst communicates with its surrounding structures. It is important to include both color-flow and spectral Doppler to confirm the cyst is intact and does not show blood flow.3,11 Microbubble UEAs have also been demonstrated to assist in the differentiation between cardiac masses.18 Unlike tumors or other vascularized structures, walled-off cysts that do not communicate with the circulatory system will not enhance with the addition of contrast.18 Blood cysts, which are thought to contain microchannels within their walls that serve as conduits to the chambers of the heart, may demonstrate delayed microbubble contrast enhancement.11 Another simple and effective maneuver is to have the patient drink a carbonated beverage. In cases where there is communication between the cyst and the gastrointestinal tract, the anechoic lesion will fill with bubbles, an approach first described in 1985 to differentiate diaphragmatic hernias mimicking intra-atrial masses.19
Other Imaging Modalities
Two- and three-dimensional TEE, including biplane imaging, often supplements TTE findings. It is especially helpful when cysts are located in atypical locations or transthoracic windows are inadequate.7 Transesophageal echocardiography can also assist in further delineating the impact of lesions on cardiac structures like assessing for valvular dysfunction. However, disruption of normal anatomy by the cyst and the relationship of the esophagus to the other structures in the mediastinum may result in difficulty performing TEE or interpreting images.3
Computed tomography and MRI are often used to further characterize cysts given their improved spatial resolution.6 Margin shape, attenuation, intensity, and degree of enhancement may assist in appropriately identifying the etiology of the cyst.6,20 However, CT cannot reliably distinguish malignant tissue from nonmalignant fluid-filled cysts.21 Similarly, T1-and T2-weighted MRI may be inconclusive when cysts contain nonserous, proteinaceous fluid.21 Diffusion-weighted imaging on MRI can further characterize cysts as the diffusion of protons within a simple cyst is less restricted in comparison with complex cysts.21
Management
Appropriate management of paracardiac cysts is unknown. All cysts described here present the possible risk of compromising normally functioning cardiac structures. Surgical resection is often performed when patients start developing symptoms or when imaging demonstrates that the cyst significantly interferes with the shape and/or size of the surrounding structures.6,7,22 Otherwise, patients frequently undergo surveillance TTE, with intervals determined on an individual basis depending on cyst size and location.7 Given the relative rarity of paracardiac cysts, there appear to be no general guidelines on how frequently to perform follow-up imaging, which is often determined based on recurrence of signs and symptoms. There is no clear guidance to suggest that patients with paracardiac cysts should be pharmacologically treated with antiplatelet agents or given antibiotic prophylaxis prior to dental procedures, unless otherwise indicated by the presence of other diseases.
Conclusion
Paracardiac cysts are rare and can arise from the multitude of structures both within and proximal to the heart. Cardiac imagers should be aware of the broad differential diagnosis for cysts around the heart to best recommend appropriate additional workup and management for patients with these findings.
Ethics Statement
The authors declare that the work described has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans.
Consent Statement
The authors declare that since this was a non-interventional, retrospective, observational study utilizing de-identified data, informed consent was not required from the patient under an IRB exemption status.
Funding Statement
The authors declare that this report did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure Statement
The authors report no conflict of interest.
Acknowledgments
We thank the NYU Langone Noninvasive Cardiology Laboratory team for their tireless efforts in caring for patients with cardiovascular disease.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.case.2023.05.006.
Supplementary Data
Pericardial cyst. A composite of 4 separate video segments obtained by TTE in the parasternal long-axis view (segment 1), parasternal short-axis view (segment 2), apical 2-chamber view (segment 3), and subcostal view (segment 4). They all demonstrate a round, well-circumscribed echolucent lesion behind the heart. The parasternal long-axis view also demonstrates pseudodyskinesis of the inferolateral wall, suggesting that, during diastole, the pressure inside the cyst exceeds the diastolic left ventricular pressure. This video corresponds to Figure 2. LV, Left ventricle; RA, right atrium; RV, right ventricle.
Esophageal duplication cyst. A composite of 2 separate video segments obtained by TTE. They demonstrate normal internal cardiac anatomy and function with a large globular, echolucent cystic structure posterior to the LA. Segment 1 is a parasternal long-axis view. Segment 2 is a parasternal short-axis view with color Doppler showing no evidence of flow within the cyst to suggest communication with outside structures. This video corresponds to Figure 4A. AV, Aortic valve; LV, left ventricle; RV, right ventricle.
Esophageal duplication cyst. A composite of 2 separate video segments obtained by TTE with contrast after IV injection of activated perflutren lipid microsphere UEA showing no bubbles within the cyst, indicating that it was not a vascular structure. Segment 1 is a parasternal long-axis view. Segment 2 is a parasternal short-axis view. This video corresponds to Figure 4C. Ao, Aorta; LV, Left ventricle; RA, right atrium; RV, right ventricle.
Bronchogenic cyst. A composite of 2 separate video segments obtained by TTE showing normal internal cardiac anatomy and function as well as a round, well-circumscribed echolucent extracardiac lesion measuring 5.5 cm in diameter and extrinsically compressing the LA. Segment 1 is in the parasternal long-axis view, and segment 2 is in an apical 2-chamber view. This video corresponds to Figure 5. Ao, Aorta; LV, Left ventricle; RA, right atrium; RV, right ventricle.
Bronchogenic cyst. A composite of 2 separate video segments obtained by TEE showing the cyst’s proximity to the right atrium. Segment 1, obtained at the midesophageal short-axis view at the level of the aortic valve, shows the cyst’s proximity to the right atrium. Segment 2, obtained at the midesophageal bicaval view with color Doppler, demonstrates the cyst compressing the SVC. This video corresponds to Figure 5. Ao, Aorta; RA, right atrium.
Blood cyst. A composite of 3 separate video segments obtained by TTE in the apical 4-chamber view. Segment 1 shows a 2.0 × 1.4 cm septated, cystic structure associated with the anterior MV leaflet. Segment 2 is a zoomed view of the cyst. Segment 3 demonstrates a zoomed view with color Doppler added showing the cystic structure’s disruption of laminar flow into the left ventricle. This video corresponds to Figure 7A and B. LV, Left ventricle; RA, right atrium; RV, right ventricle.
Blood cyst. A composite of 2 separate video segments obtained by TEE demonstrating the cystic lesion’s association within the anterior MV leaflet. Segment 1 is a two-dimensional midesophageal bicommissural view, and segment 2 is a three-dimensional zoom in approximate surgical view of the MV. This video corresponds to Figure 7C and D, respectively. A2, Anterior MV second scallop; AML, anterior mitral leaflet; LV, left ventricle; P1, posterior MV first scallop; P3, posterior MV third segment; PML, posterior mitral leaflet; RA, right atrium; RV, right ventricle.
Hepatic cyst. Transthoracic echocardiography subcostal view from the presented patient showing an anechoic, unilocular, circumferential structure along the superior aspect of the liver. It measured 4 cm in diameter and demonstrated characteristic acoustic enhancement artifact in the far field (red asterisks). This video corresponds to Figure 8A. IVC, Inferior vena cava; LV, Left ventricle; RA, right atrium; RV, right ventricle.
An example of a simple hepatic cyst detected with TTE with clearly demonstrated posterior acoustic enhancement (red asterisk). This video corresponds to Figure 8C. LV, Left ventricle; RA, right atrium; RV, right ventricle.
A composite of 2 separate video segments of a liver cyst obtained by TEE at the level of the IVC. Segment 1 demonstrates a short axis of IVC with posterior acoustic enhancement (red asterisk), which should not be confused with a hepatic cyst. Segment 2 is a simultaneous biplane view through the IVC demonstrating that the circular structure in the left panel corresponds to the long axis of IVC in the right panel. This video corresponds to Figure 8D. IVC, Inferior vena cava; LV, Left ventricle; RA, right atrium; RV, right ventricle.
References
- 1.Alkhouli M., Sandhu P., Wiegers S.E., Patil P., Panidis J., Pursnani A. Extracardiac findings on routine echocardiographic examinations. J Am Soc Echocardiogr. 2014;27:540–546. doi: 10.1016/j.echo.2014.01.026. [DOI] [PubMed] [Google Scholar]
- 2.Khosa F., Warraich H., Khan A., Mahmood F., Markson L., Clouse M.E., et al. Prevalence of non-cardiac pathology on clinical transthoracic echocardiography. J Am Soc Echocardiogr. 2012;25:553–557. doi: 10.1016/j.echo.2012.01.022. [DOI] [PubMed] [Google Scholar]
- 3.Liu Q., Vainrib A.F., Aizer A., Dodson J.A., Reynolds H.R., Cerfolio R.J., et al. Multimodality imaging of a rare case of bronchogenic cyst presenting as new-onset atrial fibrillation in a young woman. CASE (Phila) 2018;2:254–257. doi: 10.1016/j.case.2018.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Michelotto E., Tarantino N., Ostuni V., Pedote P., Colonna P., Guglielmi R. An uncommon pericardial cyst in the central mediastinum: incremental diagnosis with contrast-enhanced three-dimensional transesophageal echocardiography. J Cardiovasc Echogr. 2013;23:106–110. doi: 10.4103/2211-4122.127412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thanneer L., Saric M., Perk G., Mason D., Kronzon I. A giant pericardial cyst. J Am Coll Cardiol. 2011;57:1784. doi: 10.1016/j.jacc.2010.06.068. [DOI] [PubMed] [Google Scholar]
- 6.Verhaert D., Gabriel R.S., Johnston D., Lytle B.W., Desai M.Y., Klein A.L. The role of multimodality imaging in the management of pericardial disease. Circ Cardiovasc Imaging. 2010;3:333–343. doi: 10.1161/CIRCIMAGING.109.921791. [DOI] [PubMed] [Google Scholar]
- 7.Najib M.Q., Chaliki H.P., Raizada A., Ganji J.L., Panse P.M., Click R.L. Symptomatic pericardial cyst: a case series. Eur J Echocardiogr. 2011;12:E43. doi: 10.1093/ejechocard/jer160. [DOI] [PubMed] [Google Scholar]
- 8.Jakopovic M., Slobodnjak Z., Krizanac S., Samarzija M. Large cell carcinoma arising in bronchogenic cyst. J Thorac Cardiovasc Surg. 2005;130:610–612. doi: 10.1016/j.jtcvs.2004.12.022. [DOI] [PubMed] [Google Scholar]
- 9.Park J., Cho G.Y., Park K.H., Oh I.Y. Intracardiac bronchogenic cyst: report of a growing lesion. Circulation. 2014;130:1107–1109. doi: 10.1161/CIRCULATIONAHA.114.010992. [DOI] [PubMed] [Google Scholar]
- 10.Madhavan S., Jayaprakash K., Jayaprasad N., Sathish G., George R. Blood cyst of the anterior mitral leaflet causing severe mitral regurgitation. Proc (Bayl Univ Med Cent) 2015;28:363–364. doi: 10.1080/08998280.2015.11929275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beale R.A., Russo R., Beale C., Levin W., Atalay M.K., Fingleton J., et al. Mitral valve blood cyst diagnosed with the use of multimodality imaging. CASE (Phila) 2021;5:173–176. doi: 10.1016/j.case.2021.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yamamoto H., Nakatani S., Niwaya K., Ohnishi T., Uematsu M., Kitakaze M. Images in cardiovascular medicine. Giant blood cyst of the mitral valve: echocardiographic and intraoperative images. Circulation. 2005;112:e341. doi: 10.1161/CIRCULATIONAHA.105.546390. [DOI] [PubMed] [Google Scholar]
- 13.Panchal M., Alansari A., Wallack M., Visco F., Williams S., Sy A.M. Hepatic cyst compressing the right atrial and ventricular inflow tract: an uncommon cardiac complication. Ann Hepatol. 2018;17:165–168. doi: 10.5604/01.3001.0010.7549. [DOI] [PubMed] [Google Scholar]
- 14.Mavilia M.G., Pakala T., Molina M., Wu G.Y. Differentiating cystic liver lesions: a review of imaging modalities, diagnosis and management. J Clin Transl Hepatol. 2018;6:208–216. doi: 10.14218/JCTH.2017.00069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jeung M.Y., Gasser B., Gangi A., Bogorin A., Charneau D., Wihlm J.M., et al. Imaging of cystic masses of the mediastinum. Radiographics. 2002;22(Spec No):S79–S93. doi: 10.1148/radiographics.22.suppl_1.g02oc09s79. [DOI] [PubMed] [Google Scholar]
- 16.Odev K., Aribas B.K., Nayman A., Aribas O.K., Altinok T., Kucukapan A. Imaging of cystic and cyst-like lesions of the mediastinum with pathologic correlation. J Clin Imaging Sci. 2012;2:33. doi: 10.4103/2156-7514.97750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lyon R.D., McAdams H.P. Mediastinal bronchogenic cyst: demonstration of a fluid-fluid level at mr imaging. Radiology. 1993;186:427–428. doi: 10.1148/radiology.186.2.8421745. [DOI] [PubMed] [Google Scholar]
- 18.Kirkpatrick J.N., Wong T., Bednarz J.E., Spencer K.T., Sugeng L., Ward R.P., et al. Differential diagnosis of cardiac masses using contrast echocardiographic perfusion imaging. J Am Coll Cardiol. 2004;43:1412–1419. doi: 10.1016/j.jacc.2003.09.065. [DOI] [PubMed] [Google Scholar]
- 19.Nishimura R.A., Tajik A.J., Schattenberg T.T., Seward J.B. Diaphragmatic hernia mimicking an atrial mass: a two-dimensional echocardiographic pitfall. J Am Coll Cardiol. 1985;5:992–995. doi: 10.1016/s0735-1097(85)80446-0. [DOI] [PubMed] [Google Scholar]
- 20.McAdams H.P., Kirejczyk W.M., Rosado-de-Christenson M.L., Matsumoto S. Bronchogenic cyst: imaging features with clinical and histopathologic correlation. Radiology. 2000;217:441–446. doi: 10.1148/radiology.217.2.r00nv19441. [DOI] [PubMed] [Google Scholar]
- 21.Raja A., Walker J.R., Sud M., Du J., Zeglinski M., Czarnecki A., et al. Diagnosis of pericardial cysts using diffusion weighted magnetic resonance imaging: a case series. J Med Case Rep. 2011;5:479. doi: 10.1186/1752-1947-5-479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cianciulli T.F., Ventrici J.F., Marturano M.P., Saccheri M.C., Medus M.J., Redruello M.F. Blood cyst of the mitral valve: echocardiographic and magnetic resonance imaging diagnosis. Circ Cardiovasc Imaging. 2015;8 doi: 10.1161/CIRCIMAGING.114.002729. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Pericardial cyst. A composite of 4 separate video segments obtained by TTE in the parasternal long-axis view (segment 1), parasternal short-axis view (segment 2), apical 2-chamber view (segment 3), and subcostal view (segment 4). They all demonstrate a round, well-circumscribed echolucent lesion behind the heart. The parasternal long-axis view also demonstrates pseudodyskinesis of the inferolateral wall, suggesting that, during diastole, the pressure inside the cyst exceeds the diastolic left ventricular pressure. This video corresponds to Figure 2. LV, Left ventricle; RA, right atrium; RV, right ventricle.
Esophageal duplication cyst. A composite of 2 separate video segments obtained by TTE. They demonstrate normal internal cardiac anatomy and function with a large globular, echolucent cystic structure posterior to the LA. Segment 1 is a parasternal long-axis view. Segment 2 is a parasternal short-axis view with color Doppler showing no evidence of flow within the cyst to suggest communication with outside structures. This video corresponds to Figure 4A. AV, Aortic valve; LV, left ventricle; RV, right ventricle.
Esophageal duplication cyst. A composite of 2 separate video segments obtained by TTE with contrast after IV injection of activated perflutren lipid microsphere UEA showing no bubbles within the cyst, indicating that it was not a vascular structure. Segment 1 is a parasternal long-axis view. Segment 2 is a parasternal short-axis view. This video corresponds to Figure 4C. Ao, Aorta; LV, Left ventricle; RA, right atrium; RV, right ventricle.
Bronchogenic cyst. A composite of 2 separate video segments obtained by TTE showing normal internal cardiac anatomy and function as well as a round, well-circumscribed echolucent extracardiac lesion measuring 5.5 cm in diameter and extrinsically compressing the LA. Segment 1 is in the parasternal long-axis view, and segment 2 is in an apical 2-chamber view. This video corresponds to Figure 5. Ao, Aorta; LV, Left ventricle; RA, right atrium; RV, right ventricle.
Bronchogenic cyst. A composite of 2 separate video segments obtained by TEE showing the cyst’s proximity to the right atrium. Segment 1, obtained at the midesophageal short-axis view at the level of the aortic valve, shows the cyst’s proximity to the right atrium. Segment 2, obtained at the midesophageal bicaval view with color Doppler, demonstrates the cyst compressing the SVC. This video corresponds to Figure 5. Ao, Aorta; RA, right atrium.
Blood cyst. A composite of 3 separate video segments obtained by TTE in the apical 4-chamber view. Segment 1 shows a 2.0 × 1.4 cm septated, cystic structure associated with the anterior MV leaflet. Segment 2 is a zoomed view of the cyst. Segment 3 demonstrates a zoomed view with color Doppler added showing the cystic structure’s disruption of laminar flow into the left ventricle. This video corresponds to Figure 7A and B. LV, Left ventricle; RA, right atrium; RV, right ventricle.
Blood cyst. A composite of 2 separate video segments obtained by TEE demonstrating the cystic lesion’s association within the anterior MV leaflet. Segment 1 is a two-dimensional midesophageal bicommissural view, and segment 2 is a three-dimensional zoom in approximate surgical view of the MV. This video corresponds to Figure 7C and D, respectively. A2, Anterior MV second scallop; AML, anterior mitral leaflet; LV, left ventricle; P1, posterior MV first scallop; P3, posterior MV third segment; PML, posterior mitral leaflet; RA, right atrium; RV, right ventricle.
Hepatic cyst. Transthoracic echocardiography subcostal view from the presented patient showing an anechoic, unilocular, circumferential structure along the superior aspect of the liver. It measured 4 cm in diameter and demonstrated characteristic acoustic enhancement artifact in the far field (red asterisks). This video corresponds to Figure 8A. IVC, Inferior vena cava; LV, Left ventricle; RA, right atrium; RV, right ventricle.
An example of a simple hepatic cyst detected with TTE with clearly demonstrated posterior acoustic enhancement (red asterisk). This video corresponds to Figure 8C. LV, Left ventricle; RA, right atrium; RV, right ventricle.
A composite of 2 separate video segments of a liver cyst obtained by TEE at the level of the IVC. Segment 1 demonstrates a short axis of IVC with posterior acoustic enhancement (red asterisk), which should not be confused with a hepatic cyst. Segment 2 is a simultaneous biplane view through the IVC demonstrating that the circular structure in the left panel corresponds to the long axis of IVC in the right panel. This video corresponds to Figure 8D. IVC, Inferior vena cava; LV, Left ventricle; RA, right atrium; RV, right ventricle.