Abstract
Purpose
We aimed to characterize the incidence of complications regarding olecranon osteotomy, looking more specifically at the type of osteotomy and the fixation construct used to repair the osteotomy.
Methods
In accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, a comprehensive search was performed. A study was included if it was an adult clinical study, a transverse or chevron olecranon osteotomy was performed, and the study explicitly states the fixation construct used to repair the osteotomy. A quality assessment was performed in each study prior to data extraction.
Results
We included 39 studies with a total of 1,445 patients. Most studies included patients who were being treated primarily for a distal humerus fracture. The overall incidence of delayed union was 27/643 (4.2%), with a higher rate in transverse osteotomy than in chevron osteotomy (5/49 (10.2%) vs 22/595 (3.7%)). Nonunion occurred in 43/811 (5.4%) of patients, with a higher rate in transverse osteotomy (6/73 (8.2%) vs. 37/712 (5.2%)). Implant failure or loss of reduction occurred in 44/746 (5.9%) of patients, with a higher rate in transverse osteotomy (11/49 (22.4%) vs 33/688 (4.8%)). The removal of implants occurred in 236/1078 (21.9%) of all patients, with the highest rate in those studies that used plate fixation 44/99 (44.4%).
Conclusions
Compared with chevron osteotomy, patients who underwent transverse osteotomy had a higher incidence of delayed union, nonunion, and implant failure or loss of reduction requiring revision surgery. The incidence of implant removal indicates that patients should be informed that nearly half of the osteotomy fixed with a plate was removed after implantation.
Type of study/level of evidence
Therapeutic III.
Key words: Chevron, Elbow surgery, Olecranon osteotomy
Osteotomy of the olecranon allows excellent visualization and access to the elbow joint.1 Although olecranon osteotomy is most often used for exposure to intra-articular fractures of the distal humerus where anatomic reduction is of paramount importance, its use includes any surgery where direct visualization of the elbow joint is vital for success, such as contracture release.2,3 The orientation of the olecranon osteotomy varies and may be chevron, transverse, or oblique.
A large variety of fixation options exist to repair the olecranon osteotomy. Classically, the osteotomy is repaired with a tension band wiring (TBW) construct, including a stainless-steel wire in a figure-of-eight configuration secured to the bone with K-wires.4 Theoretically, the tension band construct converts tensile forces into compression forces at the opposing bony edges, thereby encouraging union.5,6 Newer techniques use a long, fully, or partially threaded cancellous screw (with or without a washer) spanning the osteotomy site.7 Adding a stainless-steel wire in a figure-of-eight configuration (ie, a tension band) to the single cancellous screw has the benefit of additional compression at the osteotomy site. The use of plate and screw constructs is becoming more common, likely due to the low-profile nature of newer plates and the strength of locking screw constructs.8,9 Complications, such as implant failure or loosening and osteotomy nonunion or delayed union, occur with each fixation construct and often require additional surgery, adding to the morbidity of the treatment.10,11 Due to their subcutaneous location, implants are often prominent and prove bothersome.
Despite its common use, there is no consensus regarding the optimal type of osteotomy or fixation construct to repair the osteotomy. This is especially important regarding the associated complications.
We aimed to systematically review the available literature to better characterize the complications associated with types of osteotomies and various fixation constructs.
Materials and Methods
Data sources
The study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. A trained clinical health sciences librarian (S.T.W.) developed a comprehensive search strategy using the following electronic databases from inception to April 22, 2022: PubMed, Cochrane Central Register of Controlled Trials, EMBASE, CINAHL via EBSCO, and Web of Science. Search terms were used to retrieve articles addressing the two main concepts of the search strategy: olecranon and variations in the term osteotomy. The search results were then downloaded to Mendeley, and duplicates were removed. All references were uploaded to the Covidence Systematic Review software,12 a web-based tool designed to facilitate and track each step of the abstraction and review process.
Study selection and data extraction
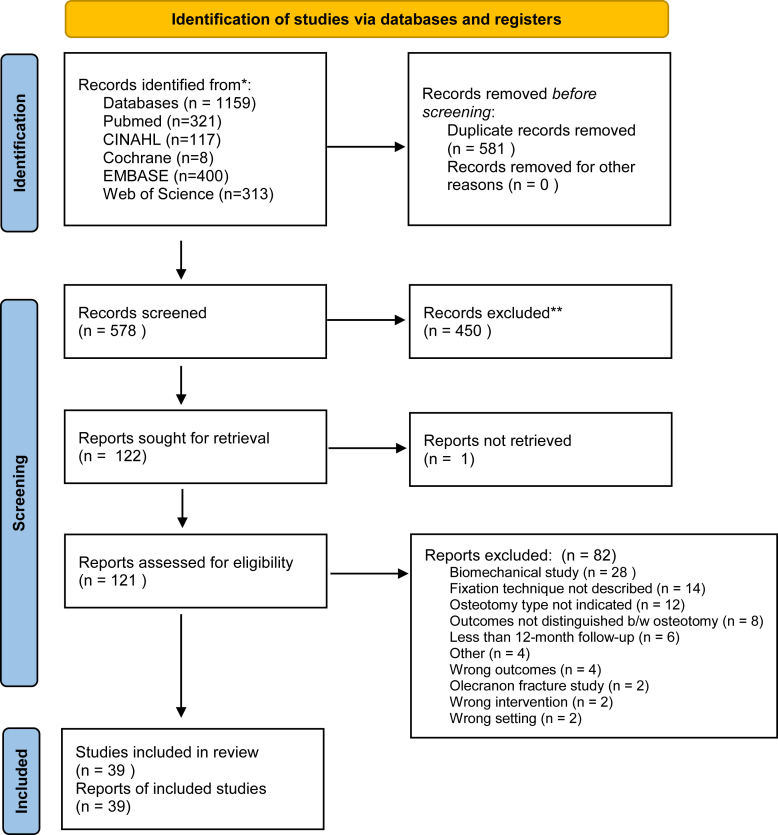
The list of potential studies identified through the database search was reviewed for inclusion by two independent reviewers. Where there was uncertainty regarding eligibility, a third reviewer was consulted. Studies were included if they were a clinical study of patients 18 years of age and older, a transverse or chevron olecranon osteotomy was performed, and the study specified a fixation construct was used to repair the osteotomy. Studies were excluded if they were case reports, technique papers, review articles, or biomechanical studies including pediatric patient population or olecranon fractures, used any osteotomy other than chevron or transverse, or did not explicitly state the fixation of the olecranon osteotomy. Details of the data extraction process are outlined in Figure 1.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses chart. ∗: all originally identified records; ∗∗: all records excluded after screening.
Studies that reported a minimum follow-up of fewer than 12 months were excluded prior to data extraction because this time period is insufficient to accurately detect the outcomes of interest of this study. Data were analyzed and presented descriptively.
Results
Data synthesis
Summing all studies amounted to 1,445 patients who underwent olecranon osteotomy (Table 1). The average age of these patients was 44.5 ± 10.3 years. Two studies did not report the age of their study population.9,13 Twenty-three of the studies indicated the sex of the patients, of which 53.6% were male and 46.4% were female.
Table 1.
Data Extraction From 39 Included Studies
| Author | Year | Indication(s) | No. of Osteotomy Patients | Type of Osteotomy | Osteotomy Fixation Construct | Delayed Union, n/N (%) | Nonunion, n/N (%) | Implant Failure/ Revision, n/N (%) | Implant Removal, n/N (%) | Infection, n/N (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Atalar et al29 | 2009 | Complex distal humerus fracture | 19 | Chevron | Screw and TBW | 0/21 (0) | 0/21 (0) | 0/21 (0) | 5/21 (23.8%) | |
| Sané et al28 | 2009 | Distal humerus fracture | 14 | Transverse | TBW | 2/14 (14.3) | 1/14 (7.1) | 14/14 (100) | ||
| Woods et al11 | 2015 | Distal humerus fracture | 160 | Chevron | TBW, plate, screw and TWB, and screw | 21/160 (13.1) | 15/160 (9.4) | 41/160 (26.9) | 14/160 (8.8) | |
| Gainor et al30 | 1995 | Complex distal humerus fracture | 10 | Transverse | Screw and TBW or TBW | 3/10 (30) | ||||
| Holdsworth & Mossad19 | 1990 | Displaced distal humerus fracture | 27 | Chevron or Transverse | Screw and TBW | 3/27 (11.1) | 4/27 (14.8) | |||
| Babhulkar & Babhulkar13 | 2011 | Intra-articular distal humerus fracture | 184 | Chevron | TBW | 3/94 (3.2) | 1/94 (1.1) | 1/90 (1.1) | ||
| Wu15 | 2003 | Traumatic elbow contracture | 20 | Transverse | TBW ("modified") | 0/20 (0.0%) | ||||
| Coles et al31 | 2006 | Distal humerus fracture | 67 | Chevron | Screw and TBW or plate | 1/67 (1.5) | 0/67 (0) | 2/67 (3.0) | 18/67 (26.9) | |
| Zhang et al32 | 2014 | Intercondylar distal humerus fracture | 36 | Chevron | TBW | 2/36 (5.6) | 1/36 (2.8) | 5/36 (13.9) | 15/36 (41.7) | 2/36 (5.6) |
| Ring et al33 | 2004 | Distal humerus fracture or nonunion | 47 | Chevron | TBW | 0/45 (0) | 0/45 (0) | 1/45 (2.2%) | 12/45 (27) | 1/45 (2.2) |
| Tian et al17 | 2013 | Distal humerus fracture | 25 | Chevron | TBW | 0/25 (0) | 0/25 (0) | 0/25 (0%) | 0/25 (0) | 0/25 (0) |
| Daroch et al34 | 2016 | Distal humerus fracture | 40 | Chevron | TBW | 1/40 (2.5) | 3/40 (7.5) | |||
| Hewins et al9 | 2007 | Distal humerus fracture | 17 | Chevron | Plate | 0/17 (0) | 0/17 (0) | 1/17 (5.9) | 1/17 (5.9) | |
| Kinik et al25 | 1999 | Intra-articular distal humerus fracture | 4 | Chevron | TBW ("self-locking") | 0/4 (0) | 0/4 (0) | 0/4 (0) | 0/4 (0) | |
| Henley35 | 1987 | Intercondylar distal humerus fracture | 28 | Transverse | Screw and TBW or TBW | 1/28 (3.6) | 2/28 (7.1) | 6/28 (21.4) | 6/28 (21.4) | 2/33 (6.1) |
| Azboy et al36 | 2016 | Intra-articular distal humerus fracture | 18 | Chevron | Screw and TBW | 2/18 (11.1) | 0/18 (0) | 4/18 (22.2) | ||
| Schmidt- Horlohe et al21 | 2011 | Distal humerus fracture | 31 | Chevron | Plate | 2/31 (6.4) | 2/31 (6.4) | 1/31 (3.2) | 15/31 (48.4) | 0/31 (0) |
| Cannada et al37 | 2011 | Supracondylar or intercondylar distal humerus fracture | 67 | Chevron | Screw and TBW or TBW | 3/67 (5.2) | 8/67 (11.9) | 8/71 (11.3) | ||
| Eralp et al20 | 2001 | Intra-articular distal humerus fracture | 17 | Chevron or Transverse | TBW | 1/17 (5.9) | 0/17 (0) | |||
| McKee et al27 | 2000 | Displaced intercondylar distal humerus fracture | 11 | Chevron | TBW | 3/11 (27.3) | 1/11 (9.1) | |||
| Tyllianakis et al38 | 2004 | Intra-articular distal humerus fracture | 26 | Chevron | TBW or screw and TBW | 0/26 (0) | 3/24 (12.5) | 3/24 (12.5) | 1/24 (4.2) | |
| Tak et al39 | 2009 | Intra-articular distal humerus fracture | 89 | Chevron | Screw and TBW | 4/89 (4.5) | 0/94 (0) | 29/89 (32.6) | 8/89 (8.9) | |
| Jung et al40 | 2016 | Intercondylar distal humerus fracture | 38 | Chevron | TBW | 1/38 (2.6) | 0/38 (0) | 3/38 (7.9) | ||
| Iorio et al41 | 2013 | Intra-articular distal humerus fracture, revision ORIF, or TEA | 14 | Chevron | Olecranon sled | 0/14 (0) | 0/14 (0) | 2/14 (14.3) | ||
| Wagener et al26 | 2015 | Intra-articular distal humerus fracture | 19 | Chevron | Screw and TBW (fibrewire) | 0/19 (0) | 0/19 (0) | 0/19 (0) | 0/19 (0) | |
| Aksoy et al42 | 2010 | Intra-articular distal humerus fracture | 21 | Chevron | Screw and TBW | 0/21 (0) | 0/21 (0) | 0/21 (0) | ||
| Edwards et al16 | 2017 | Posttraumatic elbow contracture | 35 | Chevron | Intramedullary nail | 0/35 (0) | 0/35 (0) | 0/35 (0) | 0/35 (0) | |
| Habib et al24 | 2014 | Intra-articular distal humerus fracture | 10 | Chevron | TBW | 0/10 (0) | 0/10 (0) | 0/10 (0) | 0/10 (0) | 0/10 (0) |
| Kamrani et al14 | 2018 | Distal humeral nonunion | 6 | Chevron | TBW | 0/6 (0) | 1/6 (16.7) | 0/6 (0) | 1/6 (16.7) | 1/6 (16.7) |
| Wagner et al22 | 2018 | Distal humerus fracture | 11 | Chevron | Hook plate | 0/11 (0) | 0/11 (0) | 1/11 (9.1) | 4/11 (36.4) | 2/11 (18.2) |
| Li & Zhao18 | 2017 | Distal humerus fracture | 18 | Chevron | TBW | 0/18 (0) | 0/18 (0) | 0/18 (0) | 0/18 (0) | 1/18 (5.6) |
| Guo et al43 | 2017 | Distal humerus fracture | 34 | Chevron | TBW | 0/34 (0) | ||||
| Kumar44 | 2017 | Distal humerus fracture | 21 | Transverse | TBW | 3/21 (14.3) | 0/21 (0) | 5/21 (23.8) | 5/21 (23.8) | 0/21 (0) |
| Meldrum et al45 | 2021 | Distal humerus fracture | 91 | Chevron | TBW, plate, screw and TWB, and screw | 3/91 (3.3) | 34/91 (37.4) | 3/91 (3.3) | ||
| Cañete San Pastor7 | 2021 | Distal humerus fracture | 26 | Chevron | Screw | 2/26 (7.7) | 1/26 (3.8) | 8/26 (30.8) | 1/26 (3.8) | |
| Rollo et al46 | 2018 | Intra-articular distal humerus fracture | 46 | Chevron | Plate | 0/46 (0) | ||||
| Singh et al47 | 2019 | Complex distal humerus fracture | 24 | Chevron | TBW | 0/24 (0) | 2/24 (8.3) | |||
| Ansari et al48 | 2020 | Intra-articular distal humerus fracture | 28 | Chevron | TBW | 1/28 (3.6) | 1/28 (3.6) | 3/28 (10.7) | ||
| Haglin et al8 | 2020 | Distal humerus fracture | 48 | Chevron | TBW or plate | 2/48 (4.2) | 2/48 (4.2) | 3/48 (6.3) | 1/48 (2.1) | |
| 1445 | 27/642 (4.2) | 43/789 (5.4) | 44/742 (5.9) | 236/1076 (21.9) | 54/772 (7.0) |
If more than one fixation construct was used in a study, they are listed in order of frequency used within that study. Blank cells represent those that were not explicitly stated in the study. Incidences listed are aggregates for all fixation constructs used.
ORIF, open reduction internal fixation; TEA, total elbow arthroplasty.
Of the 39 studies included, 36 included patients with distal humerus fractures. One study included only patients with distal humerus nonunion,14 whereas two studies that did not include distal humerus fractures included only patients with an elbow joint contracture.15,16
The average follow-up time period of all the included studies was 30.9 ± 14.0 months. The range of follow-up for all patients was 1.5–156 months. Five studies did not report an average follow-up time period but rather included a minimum follow-up time period for patients included in their study.7,11,13,17,18
Regarding the type of osteotomy used, 34 studies included a total of 1,308 patients who underwent chevron osteotomy, whereas five studies included a total of 93 patients who underwent transverse osteotomy. Two studies had a total of 44 patients who underwent either transverse or chevron osteotomy, but these studies did not specify the number of each osteotomy type; therefore, these studies were excluded from any analysis of osteotomy type.19,20
Fixation options varied greatly among the included studies. Tension band wiring using K-wires and a stainless-steel wire was the most frequently used option, involving 761 patients used exclusively in 19 studies. The next most frequently used fixation construct was a 6.5 mm cancellous screw with TBW, involving 382 patients and used exclusively in six studies. Only three studies exclusively used plate and screw fixation, two of which used only hook plate fixation.21,22 One study exclusively used a multiplanar locking intramedullary nail (OlecraNail; Mylad Orthopedic Solutions); this study had 35 patients.16 The remaining studies involved patient populations with more than one fixation construct.
Overall, there was a 27/643 (4.2%) incidence (27 reported cases) of delayed union of olecranon osteotomy (Table 2). Delayed union was defined by the individual papers and aggregated for the purposes of this review. The incidence of a delayed union in transverse osteotomy 5/49 (10.2%) was higher than in chevron osteotomy 22/595 (3.7%). Considering the fixation construct, the incidence of delayed union was the lowest in TBW alone 11/355 (3.2%) and the highest with cancellous screw alone 2/26 (7.7%) (Table 2).
Table 2.
Delayed Union
| Delayed Union | Cases (n) | Incidence (%) |
|---|---|---|
| Overall | 27 | 4.2 |
| Osteotomy | ||
| Transverse | 5 | 10.2 |
| Chevron | 22 | 3.7 |
| Fixation | ||
| TBW alone | 11 | 3.1 |
| Cancellous screw and TBW | 15 | 7.5 |
| Cancellous screw alone | 2 | 7.7 |
| Plate and screw | 3 | 5.1 |
Includes only outcomes explicitly stated in studies.
TBW, tension band wire.
Overall, there was a 43/796 (5.4%) incidence (43 reported cases) of nonunion of olecranon osteotomy (Table 3). In all studies, the incidence of nonunion was higher in transverse osteotomy 6/73 (8.2%) than in chevron osteotomy 37/712 (5.2%). Considering the fixation construct, the incidence of nonunion was the lowest with cancellous screw and TBW 12/308 (3.9%) and the highest with cancellous screw alone 5/72 (6.9%).
Table 3.
Nonunion
| Nonuinon | Cases (n) | Incidence (%) |
|---|---|---|
| Overall | 43 | 5.4 |
| Osteotomy | ||
| Transverse | 6 | 8.2 |
| Chevron | 37 | 5.2 |
| Fixation | ||
| TBW alone | 21 | 6.8 |
| Cancellous screw and TBW | 12 | 3.9 |
| Cancellous screw alone | 5 | 6.9 |
| Plate and screw | 5 | 5.0 |
Includes only outcomes explicitly stated in studies.
TBW, tension band wire.
Overall, there was a 44/746 (5.9%) incidence (44 reported cases) of implant failure and loss of reduction of the olecranon osteotomy, including those requiring revision surgery (Table 4). In all studies, the incidence of implant failure in transverse osteotomy 11/49 (22.4%) was higher than in chevron osteotomy 33/688 (4.8%). Considering the fixation construct, the incidence of implant failure and loss of reduction were the lowest for cancellous screw and TBW 8/178 (4.5%) and the highest for cancellous screw alone 3/39 (7.7%).
Table 4.
Implant Failure or Loss of Reduction, Including Those Requiring Revision Surgery
| Implant Failure | Cases (n) | Incidence (%) |
|---|---|---|
| Overall | 44 | 5.9 |
| Osteotomy | ||
| Transverse | 11 | 22.4 |
| Chevron | 33 | 4.8 |
| Fixation | ||
| TBW alone | 29 | 6.1 |
| Cancellous screw and TBW | 8 | 4.5 |
| Cancellous screw alone | 3 | 7.7 |
| Plate and screw | 4 | 7.4 |
Includes only outcomes explicitly stated in studies.
TBW, tension band wire.
Overall, there was a 236/1078 (21.9%) incidence (236 reported cases) of the removal of olecranon osteotomy implants (Table 5). Considering the fixation construct, the incidence of implant removal was the highest with plate fixation 44/99 (44.4%) and similarly low for all other constructs, as shown in Table 5.
Table 5.
Implant Removal
| Implant Removal | Cases (n) | Incidence (%) |
|---|---|---|
| Overall | 236 | 21.9 |
| Fixation | ||
| TBW alone | 110 | 19.8 |
| Cancellous screw and TBW | 68 | 19.4 |
| Cancellous screw alone | 14 | 19.4 |
| Plate and screw | 44 | 44.4 |
Includes only outcomes explicitly stated in studies.
TBW, tension band wire.
Overall, there was a 54/771 (7.0%) incidence (54 reported cases) of infection (Table 6). Considering those cases where a fixation construct was identified, the incidence of infection was the lowest associated with TBW alone 17/459 (3.7%) and the highest associated with plate fixation 6/44 (13.6%).
Table 6.
Infection
| Infection | Cases (n) | Incidence (%) |
|---|---|---|
| Overall | 54 | 7.0 |
| Fixation | ||
| TBW alone | 17 | 3.7 |
| Cancellous screw and TBW | 13 | 7.0 |
| Cancellous screw alone | 3 | 4.6 |
| Plate and screw | 6 | 13.6 |
Includes only outcomes explicitly stated in studies.
TBW, tension band wire.
Discussion
The fact that most included studies involved patients who had experienced a distal humerus fracture, either immediately prior or in the past (ie, revision surgery or nonunion), is expected, given the frequency of use of the olecranon osteotomy in extensile exposure of the elbow joint. However, because of its access to the elbow joint, olecranon osteotomy use has other applications, including exposure for elbow joint contracture release.
Regarding the follow-up time period, an average of 31 months is sufficient to identify most postoperative complications. Studies that reported an average or maximum follow-up time period of fewer than 12 months were excluded from this study since most complications occur within the first 12 months after surgery, and the inclusion of these studies could have led to understating the incidence of complications.
Chevron osteotomy was used far more often than transverse osteotomy. In performing the chevron osteotomy, most studies used a sagittal saw to cut through the bone only to the far cortex and then used an osteotome to complete the osteotomy, thereby creating an irregular surface. This irregular cortical surface allowed the fragments to key into one another when the osteotomy was repaired. This way, the increased surface area from the “V-shaped” bone ends fits together efficiently. This also had the effect of increasing rotational stability compared with transverse osteotomy. Patients who underwent transverse osteotomy showed a higher incidence of delayed union, nonunion, and implant failure or loss of reduction than chevron osteotomy. In their patient series in which the authors used both chevron- and transverse-type osteotomy, Holdsworth and Mossad19 had three osteotomies with a delayed union, all of which were transverse osteotomies. Similarly, Eralp et al20 had only one nonunion following transverse osteotomy. Based on the experiences in these mixed osteotomy technique patient series, each study concluded that the chevron osteotomy is more reliable and produces superior results regarding osteotomy healing. This conclusion is supported by other clinical and biomechanical studies.23
The anconeus pedicle olecranon flip osteotomy, used by Habib et al,24 represents a variation in the chevron technique. In their patient series, the authors described an additional osteotomy to remove a section of bone from the olecranon that measures approximately 2.5 cm long, 1.5 cm wide, and 3 mm to 4 mm thick, along with the attached triceps tendon and pedicle of the anconeus muscle. In their 10-patient series, they reported no cases of loss of reduction and that all osteotomies healed in an average of seven weeks.24
Tension band wiring effectively converts tension forces into compression forces to assist in fracture healing. This is indicated in the repair of an olecranon osteotomy since this is essentially an eccentrically loaded articular fracture that requires absolute stability and interfragmentary compression for direct bone healing to occur. Several studies have used variations of the traditional TBW technique. Wu et al15 used a modified TBW technique where wires were inserted from the olecranon and directed through the length of the intramedullary canal to the ulnar styloid distally. In their series of 20 patients with posttraumatic elbow contracture treated with transverse osteotomy, they did not report any complications.15 Kinik et al25 used a self-locking TBW technique where the stainless-steel cerclage wires were passed through loops formed in the proximal ends of the wires prior to tightening in a figure-of-eight fashion. This modification serves to lock the wires, thereby preventing their proximal migration. In their series, which includes four patients with olecranon chevron osteotomy, they reported no postoperative complications or implant failures.25
As with TBW, there is considerable variation within the cancellous screw and TBW groups. Screw diameter varied, with studies using 4.5 mm, 6.5 mm, or 7.3 mm screws. The use of a washer to augment the screw also varied, with some surgeons using it only in cases of poor bone quality, whereas others used it routinely without considering the bone quality. Wagener et al26 used Fibrewire (Arthrex), a high-strength suture, instead of a stainless-steel wire in the same figure-of-eight configuration for the TBW in their fixation construct. Although our analysis grouped these 19 patients with the other cancellous screw and TBW constructs, it is important to note that there are no reported complications in this patient cohort.
Plate construct fixation also demonstrated variety between and within studies. Of the 145 patients who underwent plate fixation, at least five different types or uses of plates were represented. Schmidt-Horlohe et al21 created a hook plate by cutting the terminal plate link of a one-third tubular plate, leaving two spikes that were then bent into a hook. In their series of 31 patients, two patients (6.5%) with delayed union went on to nonunion, one patient (3.2%) had implant failure (screw loosening), and 15 patients (48.4%) had their implants removed.21 Wagner et al22 used a limited-contact hook plate (Synthes Holding AG) in their study. Their series of 11 patients who underwent chevron osteotomy reported no delayed or nonunion, one case (9.1%) of implant failure/loss of osteotomy reduction and four cases (36.4%) of subsequent implant removal.22 The analysis in these reviews combined the older plate fixation techniques with modern precontoured plates.
Edwards et al16 used a multiplanar locking intramedullary nail (OlecraNail; Mylad Orthopedic Solutions) for olecranon osteotomy repair in their series of 35 patients with refractory posttraumatic elbow contracture. This implant is sufficiently rigid to withstand deforming forces encountered during rehabilitation, incorporates proximal and distal fixation with the ability to compress across the osteotomy site, and is not prominent. The authors reported no cases of nonunion, loss of reduction, or removal of hardware due to irritation.
The postoperative rehabilitation protocol nearly always involved a brief period of immobilization with a splint or cast, and the range of motion exercises started between postoperative days one and five in the 22 studies that reported their protocol. As exceptions, Babhulkar and Babhulkar13 and McKee et al27 slightly delayed the start for the range of motion exercises, beginning between postoperative days five and seven13 and on postoperative day seven,27 respectively. Habib et al24 maintained immobilization for approximately 14 days postoperatively before beginning the range of motion associated with daily activities. Sané et al28 kept immobilization in place for an average of 28 days postoperatively (range, 19–60 days) prior to beginning range of motion exercises. Conversely, Wagener et al26 allowed active and passive range of motion exercises to begin immediately after surgery. Despite the similarities in starting range of motion exercises postoperatively, there was no consensus on the use of support devices or braces after the initial cast or brace was removed. Many studies have recommended a removable splint or brace, whereas others recommended no support device.
Implant failure or loss of reduction occurred in 5.9% of all cases of olecranon osteotomy. Again, the incidence was higher in patients who underwent transverse osteotomy (22.4% vs 4.8% in chevron osteotomy). In their study of the 15 patients who experienced a loss of reduction, Woods et al11 found that those patients were significantly older than those who did not lose reduction (71.4 vs 48.5 years). Additionally, they found the incidence to be exceptionally high in postmenopausal women, who accounted for 10 (66.7%) cases. Additionally, TBW migration is a known complication in TBW and a consideration for constructs that do not use wires, such as a cancellous screw instead of wires in a TBW construct.
Implant removal occurred in 21.9% of all cases of olecranon osteotomy. These include cases in which the osteotomy implants were routinely removed (in 100% of patients in one study28) or as part of another surgery unrelated to the osteotomy itself; therefore, it is unclear whether the implants were indeed symptomatic at the time of their removal.
There are several important limitations to this systematic review. First, this study was designed to be primarily descriptive. Because of the vast heterogeneity in multiple areas of study design, we did not set out to do an analytic analysis (ie, meta-analysis) of these studies. Although we combined similar groups to calculate incidence in order to demonstrate trends, these results should be interpreted with appropriate caution. Although it is likely that the incidence figures approach accuracy when considering the groups with a large sample size, they may be less reliable when considering the groups with smaller sample sizes. Second, we excluded biomechanical studies and those studies with patients who experienced an olecranon fracture rather than osteotomy. Indeed, biomechanical studies offer valuable information that cannot be obtained from patient cohort studies. However, our aim in this study was to examine clinical outcomes. There was also heterogeneity among the groups. For example, tension band constructs included wire and sutures, different types of plates were grouped together in the plate group, and different screw sizes were grouped. In the interest of limiting variables, we also excluded olecranon fracture studies since each fracture is unique and typically not reproducible in a surgical setting. Third, we were limited by the information reported in each study, thus limiting the numbers used for calculations. When counting patients and making calculations, patients were omitted if it was not immediately clear how to categorize them. In our attempt to make no assumptions to minimize the risk of miscategorizing patients, the number of patients included in certain analyses decreased. Although this may decrease the applicability of the finding, we balance it with the risk of skewing results with inaccurate assumptions. As an example, in one study, one patient experienced nonunion, but that patient was not included in the osteotomy type subgroup analysis as the authors used both transverse and chevron osteotomies in their study and did not specify to which group this failure belongs. However, this patient was included in the overall incidence calculation and the fixation type subgroup analysis but excluded from specific osteotomy incidence calculations.
Overall, chevron olecranon osteotomy was used far more often and with superior clinical results than transverse osteotomy. This includes lower rates of delayed union, nonunion, and implant failure or loss of reduction. Although various fixation constructs were used, TBW alone and in conjunction with a single cancellous screw (with or without a washer) was used more often than other fixation constructs. Considering all fixation constructs, the incidence of delayed union, nonunion, and implant failure or loss of reduction were all acceptably low. However, the incidence of implant removal was decidedly higher with the use of plate fixation, and patients should be properly counseled regarding this, as it involves the morbidity of an additional procedure.
Footnotes
Declaration of interests: No benefits in any form have been received or will be received related directly to this article.
References
- 1.Wilkinson J.M., Stanley D. Posterior surgical approaches to the elbow: a comparative anatomic study. J Shoulder Elbow Surg. 2001;10(4):380–382. doi: 10.1067/mse.2001.116517. [DOI] [PubMed] [Google Scholar]
- 2.Perez E. In: Campbell’s Core Orthopaedic Procedures. Canale S.T., Beaty J.H., Azar F.M., editors. Elsevier; 2016. Open reduction and internal fixation of the humerus with olecranon osteotomy; pp. 293–296. [Google Scholar]
- 3.McKee M.D., Nauth A. In: Morrey’s The Elbow and Its Disorders. Morrey B.F., Sanchez-Sotelo J., Morrey M.E., editors. Elsevier; 2018. Fractures of the distal humerus; pp. 1347–1387. [Google Scholar]
- 4.Fuller D.A. Olecranon osteotomy with tension band wire repair. J Orthop Trauma. 2016;30(2):S15–S16. doi: 10.1097/BOT.0000000000000585. [DOI] [PubMed] [Google Scholar]
- 5.Prayson M.J., Williams J.L., Marshall M.P., Scilaris T.A., Lingenfelter E.J. Biomechanical comparison of fixation methods in transverse olecranon fractures: a cadaveric study. J Orthop Trauma. 1997;11(8):565–572. doi: 10.1097/00005131-199711000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Morrey B.F. Current concepts in the treatment of fractures of the radial head, the olecranon, and the coronoid. Instr Course Lect. 1995;44:175–185. [PubMed] [Google Scholar]
- 7.Cañete San Pastor P. Lopez Valenciano J, Copete I, Prosper Ramos I. Fixation of olecranon osteotomy only with 6′5 mm partially trheaded cancellous screw is a safe an effective method used in surgical management of distal humerus fractures. J Exp Orthop. 2021;(1):8. doi: 10.1186/s40634-020-00317-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haglin J.M., Lott A., Kugelman D.N., et al. Olecranon osteotomy fixation following distal humerus open reduction and internal fixation: clinical results of plate and screws versus tension band wiring. Orthopedics. 2020;44(1):E107–E113. doi: 10.3928/01477447-20201007-03. [DOI] [PubMed] [Google Scholar]
- 9.Hewins E.A., Gofton W.T., Dubberly J., MacDermid J.C., Faber K.J., King G.J. Plate fixation of olecranon osteotomies. J Orthop Trauma. 2007;21(1):58–62. doi: 10.1097/01.bot.0000246467.32574.fe. [DOI] [PubMed] [Google Scholar]
- 10.Jupiter J.B. Complex fractures of the distal part of the humerus and associated complications. Instr Course Lect. 1995;44:187–198. [PubMed] [Google Scholar]
- 11.Woods B.I., Rosario B.L., Siska P.A., Gruen G.S., Tarkin I.S., Evans A.R. Determining the efficacy of screw and washer fixation as a method for securing olecranon osteotomies used in the surgical management of intraarticular distal humerus fractures. J Orthop Trauma. 2015;29(1):44–49. doi: 10.1097/BOT.0000000000000131. [DOI] [PubMed] [Google Scholar]
- 12.Covidence Systematic Review Software, Veritas Health Innovation, Melbourne, Australia. Accessed May 1, 2022. https://www.covidence.org.
- 13.Babhulkar S., Babhulkar S. Controversies in the management of intra-articular fractures of distal humerus in adults. Indian J Orthop. 2011;45(3):216–225. doi: 10.4103/0019-5413.80039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kamrani R.S., Farhadi L., Farhoud A.R. Forearm as a valuable source of vascularized bone graft for the distal humerus. J Shoulder Elbow Surg. 2018;27(3):435–443. doi: 10.1016/j.jse.2017.09.018. [DOI] [PubMed] [Google Scholar]
- 15.Wu C.C. Posttraumatic contracture of elbow treated with intraarticular technique. Arch Orthop Trauma Surg. 2003;123(9):494–500. doi: 10.1007/s00402-003-0519-7. [DOI] [PubMed] [Google Scholar]
- 16.Edwards S.G., Rhodes D.A., Jordan T.W., Sietsema D.L. The olecranon osteotomy-facilitated elbow release (OFER) J Bone Joint Surg Am. 2017;99(21):1859–1865. doi: 10.2106/JBJS.16.00715. [DOI] [PubMed] [Google Scholar]
- 17.Tian D., Jing J., Qian J., Li J. Comparison of two different double-plate fixation methods with olecranon osteotomy for intercondylar fractures of the distal humeri of young adults. Exp Ther Med. 2013;6(1):147–151. doi: 10.3892/etm.2013.1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li Y., Zhao W. Perpendicular double-locking plating system for the internal fixation of type C distal humerus fractures through two kinds of postcubital approaches. Chin J Tissue Eng Res. 2017;21(27):4324–4329. [Google Scholar]
- 19.Holdsworth B.J., Mossad M.M. Fractures of the adult distal humerus. Elbow function after internal fixation. J Bone Joint Surg Br. 1990;72(3):362–365. doi: 10.1302/0301-620X.72B3.2341427. [DOI] [PubMed] [Google Scholar]
- 20.Eralp L., Kocaoglu M., Sar C., Atalar A.C. Surgical treatment of distal intraarticular humeral fractures in adults. Int Orthop. 2001;25(1):46–50. doi: 10.1007/s002640000198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schmidt-Horlohé K., Wilde P., Bonk A., Becker L., Hoffmann R. One-third tubular-hook-plate osteosynthesis for olecranon osteotomies in distal humerus type-C fractures: a preliminary report of results and complications. Injury. 2012;43(3):295–300. doi: 10.1016/j.injury.2011.06.418. [DOI] [PubMed] [Google Scholar]
- 22.Wagner F.C., Hölz T., Hohloch L., Suedkamp N.P., Reising K. Neues Hakenplattensystem für Olekranonfrakturen und -osteotomien. Obere Extremität. 2018;13(1):38–44. [Google Scholar]
- 23.Jupiter J.B., Neff U., Holzach P., Allgöwer M. Intercondylar fractures of the humerus. An operative approach. J Bone Joint Surg Am. 1985;67(2):226–239. [PubMed] [Google Scholar]
- 24.Habib M., Tanwar Y.S., Jaiswal A., Singh S.P., Sinha S., Lal H. Anconeus pedicle olecranon flip osteotomy: an approach for the fixation of complex intra-articular distal humeral fractures. Bone Joint J. 2014;96-B(9):1252–1257. doi: 10.1302/0301-620X.96B9.33343. [DOI] [PubMed] [Google Scholar]
- 25.Kinik H., Us A.K., Mergen E. Self-locking tension band technique. A new perspective in tension band wiring. Arch Orthop Trauma Surg. 1999;119(7–8):432–434. doi: 10.1007/s004020050015. [DOI] [PubMed] [Google Scholar]
- 26.Wagener M.L., Dezillie M., Hoendervangers Y., Eygendaal D. Clinical results of the re-fixation of a Chevron olecranon osteotomy using an intramedullary cancellous screw and suture tension band. Strateg Trauma Limb Reconstr. 2015;10(1):1–4. doi: 10.1007/s11751-015-0211-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McKee M.D., Wilson T.L., Winston L., Schemitsch E.H., Richards R.R. Functional outcome following surgical treatment of intra-articular distal humeral fractures through a posterior approach. J Bone Joint Surg Am. 2000;82(12):1701–1707. doi: 10.2106/00004623-200012000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Sané A.D., Dakouré P.W.H., Diémé C.B., et al. L’ostéotomie de l’olécrâne dans le traitement des fractures de la palette humérale de l’adulte : évaluation anatomique et fonctionnelle du coude à propos de 14 cas. Chirurgie de la Main. 2009;28(2):93–98. doi: 10.1016/j.main.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 29.Atalar A.C., Demirhan M., Salduz A., Kiliçoğlu O., Seyahi A. Functional results of the parallel-plate technique for complex distal humerus fractures. Acta Orthop Traumatol Turc. 2009;43(1):21–27. doi: 10.3944/AOTT.2009.021. [DOI] [PubMed] [Google Scholar]
- 30.Gainor B.J., Moussa F., Schott T. Healing rate of transverse osteotomies of the olecranon used in reconstruction of distal humerus fractures. J South Orthop Assoc. 1995;4(4):263–268. [PubMed] [Google Scholar]
- 31.Coles C.P., Barei D.P., Nork S.E., Taitsman L.A., Hanel D.P. Bradford Henley M. The olecranon osteotomy: a six-year experience in the treatment of intraarticular fractures of the distal humerus. J Orthop Trauma. 2006;20(3):163–170. doi: 10.1097/00005131-200603000-00002. [DOI] [PubMed] [Google Scholar]
- 32.Zhang C., Zhong B., Luo C.F. Comparing approaches to expose type C fractures of the distal humerus for ORIF in elderly patients: six years clinical experience with both the triceps-sparing approach and olecranon osteotomy. Arch Orthop Trauma Surg. 2014;134(6):803–811. doi: 10.1007/s00402-014-1983-y. [DOI] [PubMed] [Google Scholar]
- 33.Ring D., Gulotta L., Chin K., Jupiter J.B. Olecranon osteotomy for exposure of fractures and nonunions of the distal humerus. J Orthop Trauma. 2004;18(7):446–449. doi: 10.1097/00005131-200408000-00010. [DOI] [PubMed] [Google Scholar]
- 34.Daroch M., Sreen S., Vashisht D., Puri P. Management of intra-articular fractures of distal humerus with two column fixation with orthogonal plate construc. Int J Med Res Health Sci. 2016;5(10):159–165. [Google Scholar]
- 35.Henley M.B. Intra-articular distal humeral fractures in adults. Orthop Clin North Am. 1987;18(1):11–23. [PubMed] [Google Scholar]
- 36.Azboy I., Bulut M., Ancar C., et al. The comparison of triceps-reflecting anconeus pedicle and olecranon osteotomy approaches in the treatment of intercondylar fractures of the humerus. Ulus Travma Acil Cerrahi Derg. 2016;22(1):58–65. doi: 10.5505/tjtes.2015.42948. [DOI] [PubMed] [Google Scholar]
- 37.Cannada L., Loeffler B., Zadnik M.B., Eglseder A.W.A. Treatment of high-energy supracondylar/intercondylar fractures of the distal humerus. J Surg Orthop Adv. 2011;20(4):230–235. [PubMed] [Google Scholar]
- 38.Tyllianakis M., Panagopoulos A., Papadopoulos A.X., Kaisidis A., Zouboulis P. Functional evaluation of comminuted intra-articular fractures of the distal humerus (AO type C). Long term results in twenty-six patients. Acta Orthop Belg. 2004;70(2):123–130. [PubMed] [Google Scholar]
- 39.Tak S.R., Dar G.N., Halwai M.A., Kangoo K.A., Mir B.A. Outcome of olecranon osteotomy in the trans-olecranon approach of intra-articular fractures of the distal humerus. Ulus Travma Acil Cerrahi Derg. 2009;15(6):565–570. [PubMed] [Google Scholar]
- 40.Jung S.W., Kang S.H., Jeong M., Lim H.S. Triangular fixation technique for bicolumn restoration in treatment of distal humerus intercondylar fracture. Clin Orthop Surg. 2016;8(1):9–18. doi: 10.4055/cios.2016.8.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Iorio T., Wong J.C., Patterson J.D., Rekant M.S. Olecranon osteotomy fixation using a novel device: the olecranon sled. Tech Hand Up Extrem Surg. 2013;17(3):151–157. doi: 10.1097/BTH.0b013e318298b39d. [DOI] [PubMed] [Google Scholar]
- 42.Aksoy S.M., Izdeş S., Kömürcü M., Bozkurt M., Başbozkurt M. Utilization of axillary brachial plexus block in the postoperative rehabilitation of intra-articular fractures of the distal humerus. Acta Orthop Traumatol Turc. 2010;44(2):111–116. doi: 10.3944/AOTT.2010.2128. [DOI] [PubMed] [Google Scholar]
- 43.Guo XW, Fan J, Yuan F. [Treatment of coronal shear fracture of the distal end of the humerus by the olecranon osteotomy approach]. 2017;30(1):14–18. [DOI] [PubMed]
- 44.Kumar J. Dual plating osteosynthesis technique used for fixation of inter - condylar distal humerus fractures via transolecranon approach. J Liaquat Uni Med Health Sci. 2017;16(03):139–144. [Google Scholar]
- 45.Meldrum A., Kwong C., Archibold K., Cinats D., Schneider P. Olecranon osteotomy implant removal rates and associated complications. J Orthop Trauma. 2021;35(5):265–670. doi: 10.1097/BOT.0000000000001979. [DOI] [PubMed] [Google Scholar]
- 46.Rollo G., Rotini R., Eygendaal D., et al. Effect of trochleocapitellar index on adult patient-reported outcomes after noncomminuted intra-articular distal humeral fractures. J Shoulder Elbow Surg. 2018;27(7):1326–1332. doi: 10.1016/j.jse.2018.02.073. [DOI] [PubMed] [Google Scholar]
- 47.Singh R., Singh H., Kanodia N. Olecranon osteotomy approach for complex AO-13C fractures of distal humerus: a prospective analysis of 24 cases. Malays Orthop J. 2019;13(1):30–35. doi: 10.5704/MOJ.1903.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ansari M.F., Khan N.A. Atif AMd. Management of type 13C2 distal humerus fractures by olecranon osteotomy approach versus triceps sparing approach—our experience with sixty cases. Int Orthop. 2020;44(12):2735–2742. doi: 10.1007/s00264-020-04785-6. [DOI] [PubMed] [Google Scholar]