Abstract
Klebsiella oxytoca 1731, which showed a wide spectrum of resistance to β-lactams, including cefoxitin, was isolated in 1994 from a patient in Genoa, Italy. This strain contained a plasmid-mediated AmpC β-lactamase with a pI of 7.25. Sequencing of the corresponding DNA of K. oxytoca 1731 revealed 96 and 97% identities of the deduced amino acid sequence with FOX-1 and FOX-2, respectively.
Chromosomal group 1 β-lactamases (class C of Ambler) produced by gram-negative bacteria such as Enterobacter spp., Serratia spp., Citrobacter spp., and Morganella spp. can hydrolyze many β-lactam antibiotics, including cephamycins and extended broad-spectrum cephalosporins (8). In recent years ampC genes have been found mainly in conjugative plasmids and among Klebsiella pneumoniae isolates and occasionally among Escherichia coli isolates. ampC genes encode a variety of enzymes, including MIR-1 (20), CMY-1 (5), CMY-2 (4), BIL-1 (21, 28), MOX-1 (12), LAT-1 (25), FOX-1 (10), LAT-2 (9), FOX-2 (6), and ACT-1 (7); some of them are highly related to chromosomal AmpC of Citrobacter freundii, such as BIL-1, LAT-1, LAT-2, and CMY-2, or of Enterobacter cloacae, such as MIR-1 and ACT-1. Bacteria that harbor AmpC plasmids have antibiotic susceptibility patterns which are similar to those of strains overproducing chromosomally encoded β-lactamase (15).
In this study we characterize an AmpC-type plasmid-mediated β-lactamase isolated from Klebsiella oxytoca 1731 in Italy. This strain was isolated from a vaginal swab of one patient and was collected in 1994 during a European multicenter survey of the incidence of Klebsiella spp. carrying extended-spectrum β-lactamases in intensive care units (16). Furthermore, a strain of K. pneumoniae 1734 with the same resistance pattern was isolated from a urine specimen of another patient. Both patients were admitted to the same intensive care unit at the University Hospital of Genoa at the end of 1994. For treatment these patients received piperacillin, and one patient received in addition imipenem.
The minimal inhibitory concentrations (MICs) of β-lactams alone or in combination with clavulanate (4 μg/ml) were determined by the agar dilution technique recommended by the National Committee for Clinical Laboratory Standards (19). The antibiotic resistance phenotypes of the donor strains K. oxytoca 1731 and K. pneumoniae 1734 are shown in Table 1. The MICs of cefoxitin, cefotaxime, ceftazidime, and aztreonam remained unchanged despite the addition of clavulanate, whereas the MICs of the two penicillins (amoxicillin and ticarcillin) were substantially reduced.
TABLE 1.
In vitro β-lactam susceptibilities of K. oxytoca 1731 and K. pneumoniae 1734 and their transconjugants and the E. coli J53-2 recipient
| β-Lactam | MIC ( μg/ml) for:
|
||||
|---|---|---|---|---|---|
| K. oxytoca 1731 | E. coli J53-2 R+ (EC1731) | K. pneumoniae 1734 | E. coli J53-2 R+ (EC1734) | E. coli J53-2 R− | |
| Amoxicillin | 1,024 | 1,024 | 1,024 | 1,024 | 2 |
| + Clavulanate | 32 | 32 | 32 | 32 | 2 |
| Ticarcillin | ≥1,024 | ≥1,024 | ≥1,024 | ≥1,024 | 2 |
| + Clavulanate | 32 | 32 | 32 | 32 | 2 |
| Cefoxitin | 64 | 64 | 64 | 64 | 4 |
| + Clavulanate | 64 | 64 | 64 | 64 | 4 |
| Cefotaxime | 1 | 1 | 1 | 1 | ≤0.06 |
| + Clavulanate | 1 | 1 | 1 | 1 | ≤0.06 |
| Ceftazidime | 16 | 16 | 16 | 16 | 0.25 |
| + Clavulanate | 16 | 16 | 16 | 16 | 0.25 |
| Aztreonam | 4 | 1 | 4 | 1 | ≤0.06 |
| + Clavulanate | 4 | 1 | 2 | 1 | ≤0.06 |
| Cefepime | 0.12 | ≤0.06 | 0.12 | ≤0.06 | ≤0.06 |
| + Clavulanate | ≤0.06 | ≤0.06 | 0.12 | ≤0.06 | ≤0.06 |
| Imipenem | 0.12 | 0.12 | 0.12 | 0.12 | 0.12 |
Several E. coli J53-2 rif-R transconjugants were selected on MacConkey agar plates supplemented with rifampin (200 μg/ml) and cefoxitin (10 μg/ml) or ceftazidime (2 μg/ml) or ticarcillin (100 μg/ml). Because of the multiresistance profile of the two donor strains, plates supplemented with tetracycline (15 μg/ml) or kanamycin (25 μg/ml) were also prepared (18). All the transconjugants selected on these antibiotics showed a resistance phenotype similar to that of their respective donor strains. These profiles were characterized by resistance to expanded-spectrum cephalosporins and cefoxitin alone or in combination with clavulanate (Table 1) and to tetracycline and kanamycin.
Plasmid DNAs from K. oxytoca 1731 and two transconjugants were prepared by the alkaline extraction method (14). Analysis of plasmid DNA by electrophoresis in 0.8% agarose gels with Tris-borate-EDTA buffer revealed one large plasmid of about 130 kb common to all strains (data not shown). Analytical isoelectric focusing was performed in polyacrylamide gels with sonicated crude cell extracts as described previously (18). Two bands of β-lactamase activity (pI 5.4 and 7.25, respectively) were detected in K. oxytoca 1731 and its transconjugants.
The molecular characterization of the pI 5.4 β-lactamase produced by K. oxytoca 1731 was performed by PCR-restriction fragment length polymorphism, as previously described (3). With Sau3AI, BclI, BpmI, HpaII, HphI, and MseI as endonucleases, no point mutations were detected in comparison with the β-lactamase tem-1 gene (pBR322). Therefore, this enzyme was identified as a TEM-1 β-lactamase and was probably responsible for the resistance to ticarcillin and amoxicillin and explains the reduction of the MICs of these two penicillins observed in the presence of clavulanate.
The characterization of the β-lactamase with a pI of 7.25 from the transconjugant EC1731 was determined after purification as described by Iaconis and Sanders (13). The substrate profile of the pI 7.25 β-lactamase of the transconjugant EC1731 was assessed by the spectrophotometric method (26) by using a Biochrom 4060 spectrophotometer (Pharmacia LKB Biotechnology) at 37°C and freshly prepared antibiotic solutions in 0.05 M phosphate buffer (pH 7.0). The molecular extinction coefficients were calculated as previously described (24), and the maximum rate of hydrolysis (Vmax) was determined by the Lineweaver-Burk plot of initial velocity (v) at six different substrate concentrations. The maximal change in absorbance of the substrates was monitored as follows (in nm): cephaloridine, 260; cephalothin, 270; cefoxitin, 265; cefotaxime, 254; ceftazidime, 254; aztreonam, 292; benzylpenicillin, 232; and nitrocefin, 482. Specific activity was defined as micromoles of nitrocefin hydrolyzed per minute per microgram of protein. Protein concentration was determined by the method of Lowry et al. (17). The purified β-lactamase of pI 7.25 from EC1731 showed high rates of hydrolysis for cephaloridine and cephalothin and low rates of hydrolysis for benzylpenicillin, cefoxitin, cefotaxime, ceftazidime, and aztreonam (Table 2). The susceptibility to inhibition was determined by preincubating the enzyme with various concentrations of inhibitors for 10 min. Nitrocefin was then added as the substrate, and residual enzyme activity was measured. The concentration of inhibitors required for 50% inhibition of enzyme activity was defined as the IC50. The purified β-lactamase of pI 7.25 from EC1731 was strongly inhibited by cloxacillin (IC50 = 0.02 μM) and aztreonam (IC50 = 0.0015 μM) and by relatively high concentrations of clavulanate (IC50 = 3 μM). The enzyme from EC1731 had kinetic parameters (Km and Vmax values) that were very similar to those of FOX-1 variants (10). The Vmaxs for cefoxitin, cefotaxime, ceftazidime, and aztreonam were very low. However, the high affinity of the enzyme for these antibiotics might compensate for the slow hydrolysis rates, and this might result in resistance as observed with K. oxytoca 1731. Very low values of Vmax for cefoxitin (0.008 and 0.003) have also been described for FOX-1 variants (10). The IC50s of clavulanate, cloxacillin, and aztreonam were in agreement with values reported for other plasmid-mediated AmpC-type β-lactamases (12, 20, 25) and were similar to values reported for FOX-1 (10).
TABLE 2.
Kinetic constants of the FOX-3 β-lactamase produced by EC1731
| Substrate | Relative Vmax (%) | Km (μM) | Vmax (μmol/min/μg of protein) |
|---|---|---|---|
| Cephaloridine | 100 | 363 | 1.11 |
| Cephalothin | 320 | 187 | 3.53 |
| Benzylpenicillin | 1.2 | 36 | 0.013 |
| Cefoxitin | <1 | <0.01 | |
| Cefotaxime | <1 | <0.01 | |
| Ceftazidime | <1 | <0.01 | |
| Aztreonam | <1 | <0.01 |
To amplify the ampC gene of K. oxytoca 1731, degenerate oligonucleotide primers were designed from consensus sequences from the ampC genes of E. coli, E. cloacae, and C. freundii (A1, A2) and from the ampC genes of Serratia marcescens and those encoding MOX-1 and FOX-1 (B1, B2). The sequences of the primers are as follows: ampC A1, 5′ GGAATTCCTWTGCTGCGCBCTGCTGCT 3′; ampC A2, 5′ CGGGATCCCTGCCAGTTTTGATAAAA 3′; ampC B1, 5′ GGAATTCCTCASCGAGCAGACSCTGTT 3′; and ampC B2, 5′ CGGGATCCCCCGCACMTKAYRTAGGTGTGG 3′ (W = A or T; B = C, G, or T; S = G or C; M = A or C; K = G or T; Y = C or T; R = A or G). DNA sequencing was performed by the procedure of Sanger et al. (23) by using oligonucleotide primers, fluorescent dye-labeled dideoxynucleotides, Taq polymerase, and an ABI 373A DNA sequencer (Applied Biosystems, Foster City, Calif.).
The BLAST (1, 2) and FASTA programs were used to search databases for similar nucleotide and amino acid sequences. The Clustal V program (11) was used for the alignment of multiple protein sequences.
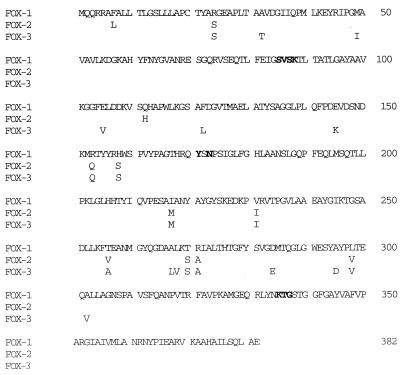
A fragment of 410 bp was obtained from K. oxytoca by PCR with ampC B1 and ampC B2 primers, and its sequence was determined. Comparison to sequences in the databases showed high sequence identities with the genes encoding FOX-1 and FOX-2 β-lactamases. Subsequent DNA amplifications of the ampC gene of K. oxytoca 1731 were performed with the new primer UT7 FOX (5′ TAATACGACTCACTATAGGGAAATGCAACAACGACGTGCG 3′) and LT3 FOX (5′ ATTAACCCTCACTAAAGGGAAATCACTCGGCCAACT GACT 3′). These primers contained the T7 (UT7 FOX) and the T3 (LT3 FOX) RNA polymerase promoter sequences. The DNA amplified by these primers encoded the entire mature protein of the FOX-1 β-lactamase. Two different PCR products, obtained from two separate PCRs, were sequenced by using the T7 and T3 primers and revealed a 1,149-bp open reading frame that had 96% nucleotide sequence identity to the plasmid-mediated β-lactamase FOX-1. The putative amino acid sequence was 96 and 97% identical to the amino acid sequences of plasmid-encoded FOX-1 and FOX-2, respectively (6, 10), and 75 to 74% identical to Aeromonas sobria chromosomal β-lactamases (22, 27) (Table 3). Comparison with sequences of eight plasmid-mediated class C β-lactamases revealed the presence of conserved motifs characteristic of serine β-lactamases, such as the box II (SVSK) and the box VII with a KTG domain, and the class C typical motif YXN (Fig. 1). These results confirmed that this β-lactamase was of the AmpC type and was homologous to the FOX-1 β-lactamase isolated in Argentina (10) and the FOX-2 originating from Guatemala (6). We propose that this enzyme should be named FOX-3.
TABLE 3.
Amino acid sequence identities of FOX-3, eight plasmid-encoded β-lactamases, and the A. sobria class C β-lactamases AER14 and CEPSa
| β-Lactamase | % Identity with:
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| FOX-3 | FOX-2 | FOX-1 | CEPS | AER14 | CMY-1 | MOX-1 | ACT-1 | CMY-2 | BIL-1 | LAT-1 | |
| FOX-3 | 100 | 97 | 96 | 75 | 74 | 72 | 64 | 40 | 40 | 40 | 39 |
| FOX-2 | 100 | 97 | 77 | 75 | 74 | 68 | 42 | 41 | 40 | 41 | |
| FOX-1 | 100 | 76 | 74 | 72 | 64 | 40 | 41 | 41 | 40 | ||
| CEPS | 100 | 74 | 73 | 65 | 43 | 43 | 42 | 42 | |||
| AER14 | 100 | 73 | 65 | 37 | 43 | 43 | 42 | ||||
| CMY-1 | 100 | 89 | 40 | 41 | 40 | 40 | |||||
| MOX-1 | 100 | 32 | 37 | 36 | 36 | ||||||
| ACT-1 | 100 | 75 | 74 | 73 | |||||||
| CMY-2 | 100 | 99 | 98 | ||||||||
| BIL-1 | 100 | 97 | |||||||||
| LAT-1 | 100 | ||||||||||
FIG. 1.
Alignment of the deduced amino acid sequences of FOX-1, FOX-2, and FOX-3 β-lactamases. Only amino acid substitutions are reported for FOX-2 and FOX-3. Boldface letters indicate conserved amino acid motifs for the active site of serine β-lactamases and AmpC β-lactamases.
Because of the possibly related origins of such enzymes, the gene encoding the FOX-3 β-lactamase was detected in K. pneumoniae 1734 by using the same degenerate oligonucleotides (ampC B1 and ampC B2 primers). One hundred percent identity (410 bp) was observed with the corresponding sequence of K. oxytoca. The two patients from which the bacteria were isolated had no contact with Argentina or Guatemala or with people from those countries.
Nucleotide sequence accession number.
The EMBL accession number for the nucleotide sequence reported in this paper is Y11068.
Acknowledgments
This investigation was supported in part by a FATMA grant (17/93.00241) from the Italian National Research Council.
REFERENCES
- 1.Altschul S F, Gish W, Miller W, Myers E W, Lipman D J. Basic local alignment search tool. J Mol Biol. 1990;215:403–410. doi: 10.1016/S0022-2836(05)80360-2. [DOI] [PubMed] [Google Scholar]
- 2.Altschul S F, Madden T L, Schäffer A A, Zhang J, Zhang Z, Miller W, Lipman D J. Gapped BLAST and PSI-BLAST: a new generation of protein database search programs. Nucleic Acids Res. 1997;25:3389–3402. doi: 10.1093/nar/25.17.3389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arlet G, Brami G, Decré D, Flippo A, Gaillot O, Lagrange P H, Philippon A. Molecular characterisation by PCR-RFLP of TEM β-lactamases. FEMS Microbiol Lett. 1995;134:203–208. doi: 10.1111/j.1574-6968.1995.tb07938.x. [DOI] [PubMed] [Google Scholar]
- 4.Bauernfeind A, Stemplinger I, Jungwirth R, Giamarellou H. Characterization of the plasmidic β-lactamase CMY-2, which is responsible for cephamycin resistance. Antimicrob Agents Chemother. 1996;40:221–224. doi: 10.1128/aac.40.1.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bauernfeind A, Stemplinger I, Jungwirth R, Wilhelm R, Chong Y. Comparative characterization of the cephamycinase blaCMY-1 gene and its relationship with other β-lactamase genes. Antimicrob Agents Chemother. 1996;40:1926–1930. doi: 10.1128/aac.40.8.1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bauernfeind A, Wagner S, Jungwirth R, Schneider I, Meyer D. A novel class C β-lactamase (FOX-2) in Escherichia coli conferring resistance to cephamycins. Antimicrob Agents Chemother. 1997;41:2041–2046. doi: 10.1128/aac.41.9.2041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bradford P A, Urban C, Mariano N, Projan S J, Rahal J J, Bush K. Imipenem resistance in Klebsiella pneumoniae is associated with the combination of ACT-1, a plasmid-mediated AmpC β-lactamase, and the loss of an outer membrane protein. Antimicrob Agents Chemother. 1997;41:563–569. doi: 10.1128/aac.41.3.563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bush K, Jacoby G A, Medeiros A A. A functional classification scheme for β-lactamases and its correlation with molecular structure. Antimicrob Agents Chemother. 1995;39:1211–1233. doi: 10.1128/aac.39.6.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gazouli M, Tzouvelekis L S, Prinarakis E, Miriagou V, Tzelepi E. Transferable cefoxitin resistance in enterobacteria from Greek hospitals and characterization of a plasmid-mediated group 1 β-lactamase (LAT-2) Antimicrob Agents Chemother. 1996;40:1736–1740. doi: 10.1128/aac.40.7.1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gonzalez Leiza M, Perez-Diaz J C, Ayala J, Casellas J M, Martinez-Beltran J, Bush K, Baquero F. Gene sequence and biochemical characterization of FOX-I from Klebsiella pneumoniae, a new AmpC-type plasmid-mediated β-lactamase with two molecular variants. Antimicrob Agents Chemother. 1994;38:2150–2157. doi: 10.1128/aac.38.9.2150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Higgins D G, Bleasby A J, Fuchs R. Clustal V: improved software for multiple alignments. Cabios. 1992;8:189–191. doi: 10.1093/bioinformatics/8.2.189. [DOI] [PubMed] [Google Scholar]
- 12.Horii T, Arakawa Y, Ohta M, Ichiyama S, Wacharotayankun R, Kato N. Plasmid-mediated AmpC-type β-lactamase isolated from Klebsiella pneumoniae confers resistance to broad-spectrum β-lactams, including moxalactam. Antimicrob Agents Chemother. 1993;37:984–990. doi: 10.1128/aac.37.5.984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Iaconis J P, Sanders C C. Purification and characterization of inducible lactamases in Aeromonas spp. Antimicrob Agents Chemother. 1990;34:44–51. doi: 10.1128/aac.34.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kado C I, Liu S T. Rapid procedure for detection and isolation of large and small plasmids. J Bacteriol. 1981;145:1365–1373. doi: 10.1128/jb.145.3.1365-1373.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lawrence E B, Godfrey A J. β-lactam antibiotics: mode of action and bacterial resistance. In: Lorian V, editor. Antibiotics in laboratory medicine. Baltimore, Md: Williams and Wilkins; 1991. p. 646. [Google Scholar]
- 16.Livermore D M, Yuan M. Antibiotic resistance and production of extended spectrum β-lactamases amongst Klebsiella spp. from intensive care units in Europe. J Antimicrob Chemother. 1996;38:409–424. doi: 10.1093/jac/38.3.409. [DOI] [PubMed] [Google Scholar]
- 17.Lowry O H, Rosebrough N J, Farr A L, Randall R J. Protein measurement with the Folin phenol reagent. J Biol Chem. 1951;193:265–275. [PubMed] [Google Scholar]
- 18.Marchese A, Arlet G, Schito G C, Lagrange P H, Philippon A. Detection of SHV-5 extended-spectrum beta-lactamase in Klebsiella pneumoniae strains isolated in Italy. Eur J Clin Microbiol Infect Dis. 1996;15:245–248. doi: 10.1007/BF01591363. [DOI] [PubMed] [Google Scholar]
- 19.National Committee for Clinical Laboratory Standards. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically, 3rd ed. Approved standard M7-A3. Villanova, Pa: National Committee for Clinical Laboratory Standards; 1995. [Google Scholar]
- 20.Papanicolaou G A, Medeiros A A, Jacoby G A. Novel plasmid-mediated β-lactamase (MIR-1) conferring resistance to oxyimino- and α-methoxy β-lactams in clinical isolates of Klebsiella pneumoniae. Antimicrob Agents Chemother. 1990;34:2200–2209. doi: 10.1128/aac.34.11.2200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Payne D J, Woodford N, Amyes S G B. Characterization of the plasmid-mediated β-lactamase BIL-1. J Antimicrob Chemother. 1992;30:119–127. doi: 10.1093/jac/30.2.119. [DOI] [PubMed] [Google Scholar]
- 22.Rasmussen B A, Keeney D, Yang Y, Bush K. Cloning and expression of a cloxacillin-hydrolyzing enzyme and a cephalosporinase from Aeromonas sobria AER 14M in Escherichia coli: requirement for an E. coli chromosomal mutation for efficient expression of the class D enzyme. Antimicrob Agents Chemother. 1994;38:2078–2085. doi: 10.1128/aac.38.9.2078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sanger F, Nicklen S, Coulson A R. DNA sequencing with chain-terminating inhibitors. Proc Natl Acad Sci USA. 1977;74:5463–5467. doi: 10.1073/pnas.74.12.5463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seeberg A H, Tolxdorff-Neutzling R M, Wiedemann B. Chromosomal β-lactamases of Enterobacter cloacae are responsible for resistance to third-generation cephalosporins. Antimicrob Agents Chemother. 1983;23:918–925. doi: 10.1128/aac.23.6.918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tzouvelekis L S, Tzelepi E, Mentis A F, Tsakris A. Identification of a novel plasmid-mediated β-lactamase with chromosomal cephalosporinase characteristics from Klebsiella pneumoniae. J Antimicrob Chemother. 1993;31:645–654. doi: 10.1093/jac/31.5.645. [DOI] [PubMed] [Google Scholar]
- 26.Waley S. A spectrophotometric assay of β-lactamase action on penicillins. Biochem J. 1984;139:789–790. doi: 10.1042/bj1390789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Walsh T R, Hall L, MacGowan A P, Bennett P M. Sequence analysis of two chromosomally mediated inducible beta-lactamases from Aeromonas sobria, strain 163a, one a class D penicillinase, the other an AmpC cephalosporinase. J Antimicrob Chemother. 1995;36:41–52. doi: 10.1093/jac/36.1.41. [DOI] [PubMed] [Google Scholar]
- 28.Woodford N, Payne D J, Johnson A P, Weinbren M J, Perinpanayagam R M, George R C, Cookson B D, Amyes S G B. Transferable cephalosporin resistance not inhibited by clavulanate in Escherichia coli. Lancet. 1990;336:253. doi: 10.1016/0140-6736(90)91784-8. [DOI] [PubMed] [Google Scholar]