Abstract
Background:
Geographic variability in esophageal cancer has been reported in China, but data are lacking at the local level. We aimed to investigate changes in disparities in esophageal cancer–related mortality among Chinese counties and whether county-level socioeconomic status was associated with this variation.
Methods:
We used data from a nationwide survey and population-based cancer registries to calculate esophageal cancer–related mortality rates for 782 Chinese counties for the periods of 1973–1975 and 2015–2017. We performed hotspot analysis to identify spatial clusters. We used a multivariable negative binomial regression model to estimate the associations between county-level socioeconomic factors and mortality.
Results:
From 1973–1975 to 2015–2017, the age-standardized esophageal cancer–related mortality rate decreased from 27 to 8 per 100,000 person-years in China. By county, 577 (74%) of 782 counties experienced decreasing mortality. Geographic disparities in mortality substantially narrowed, with the gap in mortality rates between 90th and 10th percentile counties decreasing from 55 per 100,000 person-years in 1973–1975 to 16 in 2015–2017. However, clusters of elevated rates persisted across north-central China. Rurality [adjusted mortality rate ratio (MRR) 1.15; 95% confidence interval (CI), 1.10–1.21], per capita gross domestic product (adjusted MRR, 0.95; 95% CI, 0.91–0.98), and percentage of people with a high-school diploma (adjusted MRR, 0.86; 95% CI, 0.84–0.87) in a county were significantly associated esophageal cancer–related mortality rates.
Conclusions:
China has made substantial progress in reducing esophageal cancer–related mortality and disparities, but the intercounty differences remain large.
Impact:
Continued efforts are needed to address the geographical and socioeconomic disparities in esophageal cancer.
Introduction
Esophageal cancer is the sixth most common cause of cancer-related death worldwide, with an estimated 544,000 deaths in 2020 (1). China has the world's largest esophageal cancer–related burden and alone contributes 55.3% of global deaths (2). In the 1970s, the first nationwide survey on causes of death revealed substantial geographic variations in esophageal cancer–related mortality rates in China, with more than 100 times variation across counties. In particular, the esophageal cancer–related mortality rate can change more than 5 times within 200 kilometers (3, 4).
Considering that the esophageal cancer–related mortality rate can sharply change over short geographic distances (3, 4), county-level data are valuable because they can reveal patterns that are masked at the national level. Understanding patterns and changes of county-level differences in mortality may not only help guide public health interventions at the local and national levels but also provide important clues to generate etiologic hypotheses. Moreover, local information can aid in identifying cancer hotspots that need further investigation. However, because of limited data availability, most previous studies on geographic differences in esophageal cancer–related mortality in China focused on variations by geographical area or counties in a single province (5–7), with less national information available at the county level. In addition, the association between county-level socioeconomic status and esophageal cancer–related mortality has not yet been well studied in China.
To fill the data gap, the primary aim of our study was to characterize changes in geographic disparities of esophageal cancer–related mortality at the county level from 1973 to 2017 using the most updated data from nationwide population-based cancer registries and data from the first national survey on causes of death in China. The second aim was to explore whether county-level socioeconomic factors were associated with esophageal cancer–related mortality in 2015–2017. Such results may contribute to the understanding of the effectiveness of esophageal cancer control at the national and local levels over the past decades and may further guide precise interventions to reduce disparities.
Materials and Methods
Data sources
Esophageal cancer–related mortality data in 1973–1975
During the 1970s, the Chinese National Office for Cancer Prevention and Control (NOCPC) conducted the first national retrospective survey on causes of mortality from 56 diseases with special emphasis on cancers in China. This survey has been described in detail previously (4). Briefly, it was conducted in 2,392 counties (from a total of 2,429 counties in China) across 29 provinces, covering 850 million people (96.7% of the population of the country). Only Taiwan, Hong Kong, Macau, and 35 remote counties in Tibet and Sichuan Provinces were excluded. The cause of death was determined retrospectively for deaths in the 3-year period of 1973–1975. International Classification of Diseases, 9th Revision (ICD-9) was used to classify the cause of death. To ensure data accuracy and completeness, this survey used a uniform questionnaire and organized advisory and quality control groups at the county, provincial, and national levels. The results for the first time provided the national profiles of cancer-related mortality and are one of the main data sources of information on the burden of cancer in China (8, 9). Given that this survey and the original Chinese population–based cancer registries were both organized by NOCPC and used the same data source and methods of quality control (8), they have been widely combined to estimate the long-term trend of cancer burden in China (9–11).
Esophageal cancer–related mortality data in 2015–2017
We obtained county-level esophageal cancer–related mortality data in 2015–2017 from the National Central Cancer Registry (NCCR) of China. Established in 2002, the NCCR is the national bureau for the collection and management of data from population-based cancer registries in China (9). In 2020, a total of 821 cancer registries from 31 provinces submitted cancer data to NCCR, covering a population of 564 million (45.57% of the Chinese population; ref. 12). All cancer-related deaths were coded according to ICD-10. On the basis of the criteria of the Chinese Guideline for Cancer Registration (13) and the International Association of Cancer Registries data quality criteria (14, 15), the NCCR checks and evaluates the quality of submitted data for each local registry. The indicators of quality include the mortality to incidence ratio, the percentage of cases that are morphologically verified, the percentage of death certificate-only cases, and the stability of cancer trends over years. Only registries with data met the quality of NCCR were included in this study (Supplementary Table S1). The cancer registries that were accepted for inclusion slightly varied by year of submission. To estimate reliable mortality rates across as many counties as possible, we aggregated data between 2015 and 2017.
For consistency, in this study, we only included counties that have reliable mortality data in both the 1973–1975 and 2015–2017 periods. Consequently, we included 782 counties (379 urban, 403 rural) from 31 provinces, covering a population of 455 million (32.9% of the Chinese population). The distribution and population coverage of each county was shown in Supplementary Fig. S1. We extracted esophageal cancer–related data using the ICD-9 (150) for the 1973–1975 period and ICD-10 (C15) for the 2015–2017 period. The variable of place of residence from the two periods was harmonized using the county-level administrative division code of China, a unique six-digit geocode assigned to each county (National Bureau of Statistics of China, RRID:SCR_023863).
County-level socioeconomic factors
To investigate the association between county-level socioeconomic status and esophageal cancer–related mortality in 2015–2017, we used three county attributes that reflect socioeconomic status based on prior knowledge and data availability (16), including areas (urban and rural), gross domestic product (GDP) per capita, and education level. We categorized each county into rural or urban based on the classification in 2015 from the National Bureau of Statistics of China (RRID: SCR_023863). We used county-level GDP per capita in 2015 from the Chinese Statistical Yearbook (17). GDP per capita are presented in Chinese Yuan (¥). Education level, defined as the proportion of people with an education level of high school or higher, was extracted from the Chinese National Population Census in 2010 (18). We used 2010 data for education level because it was the most recent available indicator data at the county level. The study was conducted in accordance with recognized ethical guidelines (Declaration of Helsinki and CIOMS) and approved by the institutional review board of the Cancer Hospital, Chinese Academy of Medical Sciences (22/324–3526). The written informed consent was waived owing to its retrospective study design and use of deidentified patient data.
Statistical analysis
We calculated county-level, age-standardized esophageal cancer–related mortality rates for the periods 1973–1975 and 2015–2017 by the direct standardization method using the Segi standard population in 5-year age groups. To quantify temporal changes in the age-standardized mortality rate, we calculated the absolute and relative change in the age-standardized mortality rate between 1973–1975 and 2015–2017 for each county. We tested the changes for significance using negative binomial regression models adjusted for age. Negative binomial regression was chosen due to overdispersion of deaths from esophageal cancer. We mapped counties showing significant increases, decreases, or no significant change in mortality. We further conducted a Supplementary Analysis to compare the change in mortality rates between screening and non-screening counties. A county covered by the population-based endoscopic screening program for esophageal cancer before 2017 was defined as a screening county.
We quantified geographic disparities by comparing age-standardized mortality rates between 90th and 10th percentile counties (19, 20). We considered absolute and relative disparities. We quantified absolute disparities using the difference between age-standardized mortality rates in the 90th and 10th percentile counties. We quantified relative inequality using the ratio of age-standardized mortality rates in the 90th and 10th percentile counties.
We tested the spatial distributions of the county-level mortality rate for global spatial autocorrelation using the Moran's I statistic (21). This measure tests whether spatial clustering of the county-level mortality rate exists across the whole study area. A positive value of the Moran's I statistic indicates clustering, a negative value indicates dispersal, and 0 indicates complete spatial randomness (no clustering). We then identified areas with local spatial clustering using the Gi* statistic based on local Getis-Ord Gi* hotspot analysis (22). The Gi* statistic calculates a Z-score and a P value for each county to indicate the presence or absence of significant local clustering, by comparing county-specific Moran's I statistic with corresponding values in neighboring counties. Clusters were considered statistically significant at a P value of <0.05 and Z-score of 1.96 (corresponding to the 95% confidence level). High–high clusters indicate counties with high mortality surrounded by neighboring areas with high mortality. Low–low clusters indicate counties with low mortality surrounded by neighboring areas with low mortality. We identified the distance band used for analysis based on incremental spatial autocorrelation. We analyzed each period separately.
We used multivariable negative binomial regression models to investigate the associations between county-level socioeconomic factors and esophageal cancer–related mortality in 2015–2017. The dependent variable was the number of deaths from esophageal cancer in each county by sex and age group. The log of person years was included as an offset variable to estimate mortality rates. GDP per capita and education level were included in models as continuous variables. Model coefficients were converted to mortality rate ratios (MRR). We reported MRRs and 95% confidence intervals (CI) only adjusting for age (5-year age group). We further reported adjusted MRRs and 95% CIs adjusting for the age group, GDP per capita, education level, and rurality. As a collinearity diagnostic metric, we calculated the variance inflation factor (VIF) among the independent variables.
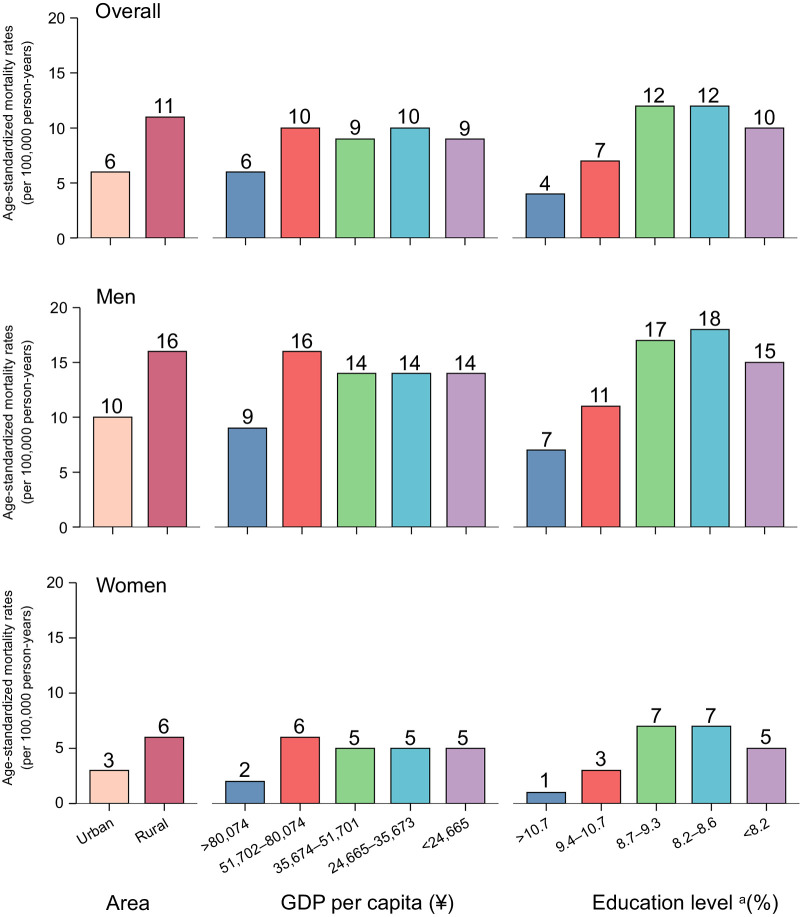
To further quantify the socioeconomic difference in mortality rate, we then categorized counties into quintiles on the basis of GDP per capita (<¥24,665, ¥24,665–35,673, ¥35,674–51,701, ¥51,702–80,074 and >¥80,074), the percentage of people with an education level of high school or higher (<8.2%, 8.2%–8.6%, 8.7%–9.3%, 9.4%–10.7%, and >10.7%), and rurality (urban and rural). We then estimated the age-standardized mortality rate for each category. We conducted separate analyses by sex.
All significance tests were two-sided, and P values less than 0.05 were considered to be statistically significant. We mapped county-level mortality data and conducted hotspot analysis using ESRI ArcGIS 10.2 software. We performed other statistical analyses in R software (version 3.2.5).
Data availability
Because of Chinese legal restrictions, raw data are not publicly available to share, but the research group can provide the data dictionary, study protocol, and descriptive data in table form. Requests can be made to W. Wei (weiwq@cicams.ac.cn).
Results
Changes in geographic variability in mortality
Nationally, the age-standardized esophageal cancer–related mortality rate decreased by 69% between 1973–1975 and 2015–2017, from 27 to 8 per 100,000 person-years. At the individual county level, the median age-standardized mortality rate decreased from 16 per 100,000 person-years [interquartile range (IQR), 8–30] in 1973–1975 to 6 (IQR, 3–10) in 2015–2017 (Table 1).
Table 1.
Overall and sex-stratified national and county-level esophageal cancer–related mortality in China.
| National-level mortality | County-level age-standardized mortality rate (per 100,000 person-years) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Time period | Crude mortality rate (per 100,000 person-years) | Age-standardized mortality rate (per 100,000 person-years) | Min | 10th | Median | 90th | Max | 90th minus 10th percentile (deaths/100,000 population) | 90th/10th (percentile ratio) | |
| 1970–1973 | Overall | 20 | 27 | 0 | 3 | 16 | 58 | 220 | 55 | 20 |
| Men | 24 | 37 | 0 | 4 | 23 | 78 | 273 | 74 | 18 | |
| Women | 15 | 19 | 0 | 2 | 10 | 41 | 177 | 39 | 22 | |
| 2015–2017 | Overall | 15 | 8 | 0 | 2 | 6 | 18 | 66 | 16 | 8 |
| Men | 21 | 13 | 0 | 4 | 9 | 27 | 93 | 23 | 7 | |
| Women | 8 | 4 | 0 | 1 | 2 | 10 | 46 | 9 | 19 | |
We observed substantial geographic variation in changes in esophageal cancer–related mortality. From 1973–1975 to 2015–2017, the absolute change in the age-standardized mortality rate across counties ranged from −190 per 100,000 person-years in Qibin County, Henan Province to 11 per 100,000 person-years in Zhangwu County, Liaoning Province (Fig. 1A). Among 782 counties, 577 (74%) showed significant declines in mortality rates. Conversely, 19 counties experienced statistically significant increases in the mortality rate, and 186 counties showed no significant change (Fig. 1B and C). Of note, counties with higher mortality rates in 1973–1975 experienced larger absolute decreases in mortality rates (P < 0.0001; Supplementary Fig. S2). Screening counties experienced a larger decrease in mortality rates compared with non-screening counties (absolute change: −46 vs. −14 per 100,000 person-years; relative change: −84% vs. −74%; Supplementary Table S2).
Figure 1.
Change in county-level age-standardized esophageal cancer–related mortality rates in China from 1973–1975 to 2015–2017. The figure contains three panels. A, Shows the absolute change in mortality rates. B, Shows the relative change in mortality rates. C, Shows counties with significant increases, decreases, or no significant change in mortality. Legend categories for A and B are based on the 1st, 5th, 10th, 25th, 50th, 75th, 90th, 95th, and 99th percentiles of change in mortality rates.
Geographic variability in esophageal cancer–related mortality narrowed over time. From 1973–1975 to 2015–2017, the absolute difference in age-standardized mortality rates between the 90th and 10th percentile counties declined from 55 to 16 per 100,000 person-years. The ratio of age-standardized mortality rates between 90th and 10th percentile counties declined from 20 to 8 (Table 1, Fig. 2A and B).
Figure 2.
County-level variability in esophageal cancer–related mortality rates in China in 1973–1975 and 2015–2017. The figure contains four panels. A, Shows county-level age-standardized esophageal cancer–related mortality rates in 1973–1975. B, Shows county-level, age-standardized, esophageal cancer–related mortality rates in 2015–2017. Legend categories of A and B are based on 1st, 5th, 10th, 25th, 50th, 75th, 90th, 95th, and 99th percentiles of mortality. C, Shows within-province variability in age-standardized, county-level, esophageal cancer–related mortality rates in 1973–1975. The red horizontal line indicates the average mortality rate across China in 1973–1975. D, Shows within-province variability in county-level age-standardized esophageal cancer–related mortality rates in 2015–2017. The red horizontal line indicates the average mortality rate across China in 2015–2017. The blue horizontal line indicates the average mortality rate across the world in 2018 (2). Only provinces with 10 or more counties with available data were included in C and D. The mortality rate in C and D was plotted on a semi-log scale.
Variability in the county-level mortality rate also narrowed within provinces. The absolute difference in age-standardized mortality rates between the 90th and 10th percentile counties ranged from 2 per 100,000 person-years in Heilongjiang Province to 24 per 100,000 person-years in Henan Province in 2015–2017, compared with ranges from 3 per 100,000 person-years in Yunnan Province to 94 per 100,000 person-years in Henan Province in 1973–1975 (Fig. 2C and D; Supplementary Table S3).
Spatial analysis showed that the age-standardized esophageal cancer–related mortality rate was consistently highly spatially correlated over time (1973–1975: Moran's I statistic = 0.4, P < 0.001; 2015–2017: Moran's I statistic = 0.3, P < 0.001). From 1973–1975 to 2015–2017, clusters of elevated rates were persistently identified across the Taihang Mountain tri-provincial range (Henan, Hebei, and Shanxi), Jiangsu Province, northern Anhui Province, and northern Sichuan Province (Fig. 3A and B).
Figure 3.
Geospatial hot analysis of esophageal cancer–related mortality in China in 1973–1975 and 2015–2017. The figure contains two panels. A, Shows geospatial hotspot analysis of esophageal cancer–related mortality in 1973–1975. B, Shows geospatial hotspot analysis of esophageal cancer–related mortality in 2015–2017. Hotspot analysis identified clusters with significantly increased mortality on the basis of county-level Z scores and P values (P < 0.05 and P < 0.01).
Association between county-level socioeconomic status and mortality
We used multivariable negative binomial regression models to assess the association between county-level socioeconomic factors and esophageal cancer–related mortality rates in 2015–2017. County rurality was associated with increased esophageal cancer–related mortality (adjusted MRR, 1.15; 95% CI, 1.10–1.21; P < 0.001). A 100,000¥ increase in GDP per capita in a county was associated with a 5% decline in esophageal cancer–related mortality rates (adjusted MRR, 0.95; 95% CI, 0.91–0.98; P = 0.002). Every 1-point increase in the percentage of people with an education level of high school or higher was associated with a 14% decline (adjusted MRR, 0.86; 95% CI, 0.84–0.87; P < 0.001) in esophageal cancer–related mortality rates. In the stratified analyses, similar patterns were observed in both sexes, with a stronger association in women than in men (Table 2). There was no collinearity between the independent variables (VIF < 2).
Table 2.
Overall and sex-stratified multivariable negative binomial regression models evaluating factors associated with county-level esophageal cancer–related mortality rates.
| Model 1a | Model 2b | ||||
|---|---|---|---|---|---|
| County-level variable | MRR (95% CI) | P | MRR (95% CI) | P | |
| Overall | Area | ||||
| Urban | Reference | Reference | |||
| Rural | 1.49 (1.43–1.55) | <0.001 | 1.15 (1.10–1.21) | <0.001 | |
| GDP per capitac | 0.79 (0.76–0.81) | <0.001 | 0.95 (0.91–0.98) | 0.002 | |
| Education leveld | 0.83 (0.82–0.84) | <0.001 | 0.86 (0.84–0.87) | <0.001 | |
| Men | Area | ||||
| Urban | Reference | Reference | |||
| Rural | 1.41 (1.36–1.47) | <0.001 | 1.11 (1.06–1.16) | <0.001 | |
| GDP per capitac | 0.81 (0.78–0.84) | <0.001 | 0.95 (0.92–0.99) | 0.007 | |
| Education leveld | 0.85 (0.84–0.86) | <0.001 | 0.87 (0.86–0.88) | <0.001 | |
| Women | Area | ||||
| Urban | Reference | Reference | |||
| Rural | 1.90 (1.79–2.02) | <0.001 | 1.31 (1.21–1.41) | <0.001 | |
| GDP per capitac | 0.67 (0.64–0.71) | <0.001 | 0.93 (0.88–0.98) | 0.007 | |
| Education leveld | 0.74 (0.73–0.76) | <0.001 | 0.79 (0.77–0.81) | <0.001 | |
Abbreviations: GDP, gross domestic product; MRR, mortality rate ratio.
aModels were adjusted for the age group.
bModels were adjusted for the age group, area (rural and urban), GDP per capita, and education level.
c100,000 Chinese Yuan (¥), included in models as a continuous variable.
dThe proportion of people with an education level of high school or higher, included in models as a continuous variable.
To further quantify the socioeconomic differences in mortality, by county-level quintiles of per capita GDP, education level, and rurality. The esophageal cancer–related mortality rate was higher in the counties with the lowest per capita GDP (9 vs. 6 per 100,000 person-years) and lowest education level (10 vs. 4 per 100,000 person-years) compared with the counties with the highest per capita GDP and education level, and higher in rural counties than in urban counties (11 vs. 6 per 100,000 person-years; Fig. 4).
Figure 4.
Overall and sex-stratified age-standardized esophageal cancer–related mortality rates by county-level socioeconomic factors. The figure shows the age-standardized mortality rates by county-level quintiles of per capita GDP, education level, and rurality; GDP, gross domestic product. a, The proportion of people with an education level of high school or higher.
Discussion
Using data from a national survey and population-based cancer registries, this study for the first time provided the most up-to-date and comprehensive changes and disparities in esophageal cancer–related mortality at the county level in China. From 1973–1975 to 2015–2017, the esophageal cancer–related mortality rates declined in 74% of our counties. Intercounty differences in mortality rates substantially narrowed over time, but clusters of elevated rates persisted. Rurality, lower GDP per capita, and lower education levels were associated with increased county-level esophageal cancer–related mortality. Our findings indicated success in reducing the mortality and disparities in esophageal cancer in China and have important implications for targeted interventions to further reduce disparities.
The finding of a substantial decrease in esophageal cancer–related mortality in China is consistent with the findings of previous studies (23, 24). In this study, we further revealed that the decrease occurred across most Chinese counties. This geographically widespread decline may be largely attributable to the nationwide elimination or minimization of risk factors for esophageal cancer over past decades in China due to rapid socioeconomic development. Esophageal squamous cell carcinoma (ESCC) accounts for more than 90% of all esophageal cancer–related cases in China (25). Previous cohort studies in the 2000s indicated that tobacco use and alcohol consumption, which are the major risk factors for ESCC in Western countries (26), were less common and had a small role in ESCC etiology in high-risk regions of China (27–29). Conversely, combined factors related to lower socioeconomic status have been suggested to be responsible for the high burden of esophageal cancer in China, including low intake of fresh fruits and vegetables (28), poor nutritional status (28), indoor air pollution (27), lack of access to piped water (28, 29), poor oral health (27, 29), and consumption of pickled vegetables (30). These factors have been largely minimized in China. For instance, studies using nationally representative data from the China National Nutrition Surveys showed that the average vegetable intake in the Chinese population increased from 252.6 g/d in 1977 to 323.8 g/d in 2011 (31), and the overall fruit intake increased from 18.2 g/d to 69.6 g/d (31). During the same period, the consumption of pickled vegetables decreased from 23.7% to 18.3% (31). Moreover, access to piped water in the rural population increased from 43.2% in 1993 to 57.2% in 2008 (32, 33). In addition, with the decreased use of solid fuels and improved stoves, which have higher combustion efficiencies and are coupled with chimneys, indoor pollutant concentrations have declined in rural China (34–37). Furthermore, the widespread decrease in esophageal cancer–related mortality could partly be attributed to improved survival trends. The 5-year survival for esophageal cancer increased from 20.9% in 2003–2005 to 30.3% in 2012–2015 in China (38).
Of note, we found that historically high-risk areas experienced greater reductions, resulting in the narrowing geographic disparity in esophageal cancer–related mortality in China. The steeper decrease in high-risk areas may reflect the effectiveness of the comprehensive cancer control work that has been performed in those areas. Since 1959, extensive epidemiological studies on esophageal cancer have been conducted in high-risk areas around the Taihang Mountains (39), such as the US-China collaborative studies of the Linxian Nutritional Intervention Trial (40). On the basis of those studies, various preventive measures have been undertaken, including the use of molybdenum fertilizer, prevention of mold contamination, removal of nitrosamines, elimination of undesirable eating habits, improvement of nutritional status, and treatment of precancerous lesions (39). After the nationwide survey in 1973–1975 identified high-risk areas for cancers across China, extensive research and control work on cancer expanded to more than 60 high-risk areas (41).
Furthermore, a larger decline in esophageal cancer–related mortality rates was observed in screening counties than in non-screening counties. This observation aligns with previous studies that indicated a more favorable stage distribution and a higher survival rate among patients with esophageal cancer in screening areas than those in non-screening areas (42, 43). The early detection of esophageal cancer started in the 1950s in Linzhou (44). From 1959 to 1979, approximately 500,000 people underwent balloon cytologic examinations of the esophagus (45). In 2005, the Ministry of Health of China initiated a population-based endoscopy screening program for esophageal cancer in eight high-risk areas, such as Linzhou and Cixian (46). Population-based and community-based cohort studies have indicated that this program could decrease esophageal cancer–related mortality in high-risk areas of China (47–50). By 2018, the program was expanded to 194 sites in 31 provinces. A total of 2,166,245 people were screened, and 34,607 cancers were detected (51). Recently, the effectiveness of endoscopic screening programs in reducing esophageal cancer–related mortality has been reported at local sites (50, 52–57). These findings may suggest the contribution of the screening programs to the decline in esophageal cancer–related mortality in China.
Despite the decline in most counties, there was a significant increase in esophageal cancer–related mortality observed in 19 counties. Most of these counties were located in non–high-risk northeast and southwest regions, such as the provinces of Liaoning and Yunnan. These increases may be associated with the rise in the prevalence of smoking and alcohol use in those areas (58). For example, between 1990 and 2017, the prevalence of alcohol use increased from 7.82% to 12.46% in Liaoning Province and from 6.81% to 9.74% in Yunnan Province (58). Furthermore, studies have indicated that the relative contribution of drinking to the esophageal cancer–related burden in China is expected to increase (31). It may suggest that the increased consumption of alcohol is expected to compromise the beneficial effect of economic development on esophageal cancer in China, which offers further evidence to support the importance of a healthy lifestyle in future esophageal cancer control.
Although we observed a marked decline in mortality over time, the geographic disparities in esophageal cancer–related mortality remained significant in China. The geographic variation in esophageal cancer has been widely reported across countries, with the mortality rate approximately 5 times higher in China than in the United States (59). In this study, we further revealed that the esophageal cancer–related mortality was 8 times higher in the 90th percentile counties than the 10th percentile counties in China. Notably, clusters of elevated rates were persistently identified in North China, similar to previous findings using data from a single province (7). These persisted geographic disparities highlight the need for continued and expanded screening programs for esophageal cancer in these high-risk areas (51). Furthermore, despite extensive research, the main causative factors that contribute to esophageal cancer in high-risk areas have not yet been fully elucidated (16). More epidemiologic studies are warranted to uncover the underlying reasons for these persisted esophageal cancer hotspots.
We further revealed that rurality, lower per capita GDP, and lower level of education were significantly associated with higher county-level esophageal cancer–related mortality. Of note, we found that the associations were stronger in women than in men, which suggested that esophageal cancer–related mortality among women might be more sensitive to socioeconomic status. These findings were consistent with the existing finding that individual-level formal education was a protective factor for ESCC (28). This area socioeconomic difference in esophageal cancer may be related in several respects. First, in China, residents living in developed counties are less exposed to many risk factors for ESCC, such as poor nutritional status and polluted drinking water (31, 33, 60). Second, people residing in areas with high educational attainment and GDP per capita have an increased awareness of cancer and increased adoption of healthy diet habits and lifestyles (60, 61). For example, studies showed that compared with urban areas, rural areas had a higher rate of cigarette smoking (50% vs. 45%) and a lower rate of smoking cessation (5.8% vs. 6.9%) in 2003 (60). Furthermore, regional disparities in access to health services may also play an important role in producing socioeconomic disparities in esophageal cancer–related mortality. Studies revealed remarkable geographic inequalities in health system coverage in China and showed that GDP per capita was a significant predictor of both hospital delivery and composite coverage (60, 62). Therefore, by improving diet, nutrition, quality of water, and oral hygiene in less developed regions, the targeted poverty alleviation strategies in China may offer opportunities to address these socioeconomic inequalities in esophageal cancer (63). Government initiatives to proportionally allocate more health-care resources to rural areas can also help reduce these inequalities (64). In addition, the improving insurance coverage for patients with cancer, especially for those in rural and remote areas in China, has the potential to further narrow these inequalities (65).
There are several strengths of our study. First, this study combined the two national, large-scale, and reliable population-based data sources for information on cancer in China, enabling analyzing the changes in cancer-related mortality at the county level. These trends and patterns have important implications for China's national and local strategies in esophageal cancer control, allowing us to borrow lessons from successful counties and place more emphasis on persistently high-risk counties. Second, through a combination of national cancer mortality and socioeconomic data, this is the first study to our knowledge to assess the association between esophageal cancer–related mortality and county-level socioeconomic factors.
Our study has some limitations. First, we obtained data of the two periods from two different sources. Even though they were organized by the same department and used the same data source and quality control methods (8, 9), the differences in quality of health care and diagnostic techniques between the two periods may limit data comparability. Second, our dataset included 782 counties, which may cannot fully represent the whole population of China. However, the 782 counties were selected on the basis of Chinese population-based cancer registries, which covered both urban and rural areas, representing different socioeconomic statuses and lifestyles in the country (9). Third, because of the high percentage of unspecified histology diagnoses (40%; ref. 6), we did not differentiate our analysis by histological subtype. Even though a study using data from high-quality registries reported that ESCC still accounted for more than 90% of all esophageal cancer–related cases in China in 2018 (66), future studies are needed to investigate the local-level rates by histological subtype, particularly for those areas showing increases in mortality.
In summary, the study results contributed to the understanding of geographical and socioeconomic inequalities in esophageal cancer at the county level in China and demonstrated that major advances have been made in reducing the esophageal cancer–related mortality and disparities over the past 40 years in the country. However, intercounty differences in esophageal cancer remain significant. This result highlights a need for continued effort to discover the underlying reasons for the geographic and socioeconomic inequalities in esophageal cancer and provide scientific evidence for interventions to narrow these disparities.
Supplementary Material
Supplementary Table 1 shows three major measures of data quality of cancer registries included in this study.
Supplementary Table 2 shows the change in esophageal cancer mortality rates in counties with and without screening programs.
Supplementary Table 3 shows the difference in age-standardized esophageal cancer mortality rates between 90th and 10th percentile counties by province and time period.
Supplementary Figure 1 shows the geographic distribution and population coverage of 782 counties included in final analyses, along with the population density of China.
Supplementary Figure 2 was a scatter diagram of the age-standardized esophageal cancer mortality rate in 1973-1975 and the absolute change in mortality rates from 1973–1975 to 2015–2017.
Acknowledgments
We gratefully thank the staff of the population-based cancer registries for providing cancer records. We sincerely acknowledge the cooperation of all involved in data collection, verification, and database creation in the first national retrospective surveys on causes of death. W. Wei was funded by the Major State Basic Innovation Program of the Chinese Academy of Medical Sciences (2021-I2M-1–010) and the National Natural Science Foundation of China (81974493).
The publication costs of this article were defrayed in part by the payment of publication fees. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
This article is featured in Selected Articles from This Issue, p. 1273
Footnotes
Note: Supplementary data for this article are available at Cancer Epidemiology, Biomarkers & Prevention Online (http://cebp.aacrjournals.org/).
Authors' Disclosures
No disclosures were reported.
Authors' Contributions
X. Ran: Conceptualization, data curation, formal analysis, validation, visualization, methodology, writing–original draft, writing–review and editing. R. Zheng: Resources, data curation, formal analysis, validation, investigation, methodology, writing–review and editing. H. Zeng: Resources, formal analysis, investigation, writing–review and editing. S. Zhang: Resources, validation, investigation, writing–review and editing. K. Sun: Resources, investigation, methodology, writing–review and editing. B. Han: Resources, investigation, methodology, writing–review and editing. S. Wang: Resources, investigation, methodology, writing–review and editing. R. Chen: Resources, investigation, writing–review and editing. L. Li: Resources, investigation, writing–review and editing. W. Wei: Conceptualization, resources, supervision, funding acquisition, validation, project administration, writing–review and editing. J. He: Conceptualization, resources, supervision, investigation, project administration.
References
- 1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021;71:209–49. [DOI] [PubMed] [Google Scholar]
- 2. Arnold M, Abnet CC, Neale RE, Vignat J, Giovannucci EL, McGlynn KA, et al. Global burden of 5 major types of gastrointestinal cancer. Gastroenterology 2020;159:335–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. The Editorial Committee. Atlas of cancer mortality in the People's Republic of China. Shanghai: China Map Press; 1979. p. 1–99. [Google Scholar]
- 4. Liu B. Esophageal cancer. In: The National Cancer Control Office of the Ministry of Health. China cancer death survey. Beijing: People's Medical Publishing House; 1980. p. 73–103. [Google Scholar]
- 5. Zhou MG, Wang XF, Hu JP, Li GL, Chen WQ, Zhang SW, et al. Geographical distribution of cancer mortality in China, 2004–2005. Chinese J Preventive Med 2010;44:303–8. [PubMed] [Google Scholar]
- 6. Zeng H, Zheng R, Zhang S, Zuo T, Xia C, Zou X, et al. Esophageal cancer statistics in China, 2011: estimates based on 177 cancer registries. Thorac Cancer 2016;7:232–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kou K, Guo X, Baade P, Lu Z, Fu Z, Chu J, et al. Spatial analysis of esophageal cancer mortality in a high-risk population in China: consistent clustering pattern in 1970–74 and 2011–13. Asian Pac J Cancer Prev 2018;19:3161–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yang L, Parkin DM, Li L, Chen Y. Sources of information on the burden of cancer in China. Asian Pac J Cancer Prev 2003;4:23–30. [PubMed] [Google Scholar]
- 9. Wei W, Zeng H, Zheng R, Zhang S, An L, Chen R, et al. Cancer registration in China and its role in cancer prevention and control. Lancet Oncol 2020;21:e342–9. [DOI] [PubMed] [Google Scholar]
- 10. Huang TR, Zhang SW, Chen WQ, Deng W, Zhang CY, Zhou XJ, et al. Trends in nasopharyngeal carcinoma mortality in China, 1973–2005. Asian Pac J Cancer Prev 2012;13:2495–502. [DOI] [PubMed] [Google Scholar]
- 11. Xia C, Ding C, Zheng R, Zhang S, Zeng H, Wang J, et al. Trends in geographical disparities for cervical cancer mortality in China from 1973 to 2013: a subnational spatio-temporal study. Chin J Cancer Res 2017;29:487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. National Cancer Center, Disease Prevention and Control Bureau, Ministry of Health. Chinese cancer registry annual report 2020. Beijing: Ministry of Health; 2022. p. 3–5. [Google Scholar]
- 13. Wang N, Zhou J. Data quality control. In: He J, Chen W, editors. Chinese Guideline for Cancer Registration. Beijing: People's Medical Publishing House Co., LTD.; 2016. p. 59–75. [Google Scholar]
- 14. Bray F, Parkin DM. Evaluation of data quality in the cancer registry: principles and methods. Part I: comparability, validity and timeliness. Eur J Cancer 2009;45:747–55. [DOI] [PubMed] [Google Scholar]
- 15. Parkin DM, Bray F. Evaluation of data quality in the cancer registry: principles and methods Part II. Completeness. Eur J Cancer 2009;45:756–64. [DOI] [PubMed] [Google Scholar]
- 16. Abnet CC, Arnold M, Wei WQ. Epidemiology of esophageal squamous cell carcinoma. Gastroenterology 2018;154:360–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. National Bureau of Statistics of of the People's Republic of China. Chinese statistical yearbook, 2015. Beijing: China Statistics Press; 2015. p. 3–402. [Google Scholar]
- 18. Population Census Office under the State Council Department of Population and Employment Statistics National Bureau of Statistics. Tabulation on the 2010 population census of the People's Republic of China by county. Beijing: China Statistics Press, 2012. p. 408–510. [Google Scholar]
- 19. Mokdad AH, Dwyer-Lindgren L, Fitzmaurice C, Stubbs RW, Bertozzi-Villa A, Morozoff C, et al. Trends and patterns of disparities in cancer mortality among US counties, 1980–2014. JAMA 2017;317:388–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ma C, Congly SE, Chyou DE, Ross-Driscoll K, Forbes N, Tsang ES, et al. Factors associated with geographic disparities in gastrointestinal cancer mortality in the United States. Gastroenterology 2022;163:437–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Moran PAP. The interpretation of statistical maps. J Royal Stat Soc. Series B 1948;10:243–51. [Google Scholar]
- 22. Ord JK, Getis A. Local spatial autocorrelation statistics: distributional issues and an application. Geographical Analysis 1995;27:286–306. [Google Scholar]
- 23. Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer statistics in China, 2015. CA Cancer J Clin 2016;66:115–32. [DOI] [PubMed] [Google Scholar]
- 24. Zheng R, Zhang S, Zeng H, Liu G, Jian Y, Zhou H, et al. Cancer incidence and mortality in China, 2016. J Nat Cancer Center 2022;2:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Arnold M, Soerjomataram I, Ferlay J, Forman D. Global incidence of oesophageal cancer by histological subtype in 2012. Gut 2015;64:381–7. [DOI] [PubMed] [Google Scholar]
- 26. Wang SM, Katki HA, Graubard BI, Kahle LL, Chaturvedi A, Matthews CE, et al. Population attributable risks of subtypes of esophageal and gastric cancers in the United States. Am J Gastroenterol 2021;116:1844–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wei WQ, Abnet CC, Lu N, Roth MJ, Wang GQ, Dye BA, et al. Risk factors for oesophageal squamous dysplasia in adult inhabitants of a high risk region of China. Gut 2005;54:759–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tran GD, Sun XD, Abnet CC, Fan JH, Dawsey SM, Dong ZW, et al. Prospective study of risk factors for esophageal and gastric cancers in the Linxian general population trial cohort in China. Int J Cancer 2005;113:456–63. [DOI] [PubMed] [Google Scholar]
- 29. He Z, Zhao Y, Guo C, Liu Y, Sun M, Liu F, et al. Prevalence and risk factors for esophageal squamous cell cancer and precursor lesions in Anyang, China: a population-based endoscopic survey. Br J Cancer 2010;103:1085–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lin S, Wang X, Huang C, Liu X, Zhao J, Yu IT, et al. Consumption of salted meat and its interactions with alcohol drinking and tobacco smoking on esophageal squamous-cell carcinoma. Int J Cancer 2015;137:582–9. [DOI] [PubMed] [Google Scholar]
- 31. Wu Y, Li Y, Giovannucci E. Potential impact of time trend of lifestyle risk factors on burden of major gastrointestinal cancers in China. Gastroenterology 2021;161:1830–41. [DOI] [PubMed] [Google Scholar]
- 32. Ministry of Health of China. Analysis report of national health services survey 1993. Beijing: Beijing Chinese Academy of Medical Sciences Press; 1994. p. 9. [Google Scholar]
- 33. Ministry of Health of China. Analysis report of national health services survey 2008. Beijing: BeijingChinese Academy of Medical Sciences Press; 2009. p. 10. [Google Scholar]
- 34. Zhao B, Zheng H, Wang S, Smith KR, Lu X, Aunan K, et al. Change in household fuels dominates the decrease in PM2.5 exposure and premature mortality in China in 2005–2015. Proc Natl Acad Sci USA 2018;115:12401–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Tao S, Ru MY, Du W, Zhu X, Zhong QR, Li BG, et al. Quantifying the rural residential energy transition in China from 1992 to 2012 through a representative national survey. Nat Energy 2018;3:567–73. [Google Scholar]
- 36. Zhang J, Mauzerall DL, Zhu T, Liang S, Ezzati M, Remais JV. Environmental health in China: progress towards clean air and safe water. Lancet 2010;375:1110–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Chen Y, Shen H, Smith KR, Guan D, Chen Y, Shen G, et al. Estimating household air pollution exposures and health impacts from space heating in rural China. Environ Int 2018;119:117–24. [DOI] [PubMed] [Google Scholar]
- 38. Zeng H, Chen W, Zheng R, Zhang S, Ji JS, Zou X, et al. Changing cancer survival in China during 2003–15: a pooled analysis of 17 population-based cancer registries. Lancet Glob Health 2018;6:e555–67. [DOI] [PubMed] [Google Scholar]
- 39. Yang CS. Research on esophageal cancer in China: a review. Cancer Res 1980;40:2633–44. [PubMed] [Google Scholar]
- 40. Wang SM, Taylor PR, Fan JH, Pfeiffer RM, Gail MH, Liang H, et al. Effects of nutrition intervention on total and cancer mortality: 25-year post-trial follow-up of the 5.25-year linxian nutrition intervention trial. J Natl Cancer Inst 2018;110:1229–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Dong ZW, Qiao YL, Li LD, Wang GQ, Zhang SW, Meng QZ, et al. A report of cancer high incidence scene in China. China Cancer 2009;18:4–9. [Google Scholar]
- 42. Guan CT, Song GH, Li BY, Gong YW, Hao CQ, Xue LY, et al. Endoscopy screening effect on stage distributions of esophageal cancer: a cluster randomized cohort study in China. Cancer Sci 2018;109:1995–2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. An L, Zheng R, Zeng H, Zhang S, Chen R, Wang S, et al. The survival of esophageal cancer by subtype in China with comparison to the United States. Int J Cancer 2023;152:151–61. [DOI] [PubMed] [Google Scholar]
- 44. Yang CS, Chen XL. Research on esophageal cancer: with personal perspectives from studies in China and Kenya. Int J Cancer 2021;149:264–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Shu YJ. Cytopathology of the esophagus. an overview of esophageal cytopathology in China. Acta Cytol 1983;27:7–16. [PubMed] [Google Scholar]
- 46. Dong ZW, Qiao YL, Kong LZ, Wang GQ, Meng XZ. The strategy and implementation for early detection of cancer in China. China Cancer 2008;17:263–5. [Google Scholar]
- 47. Wei WQ, Chen ZF, He YT, Feng H, Hou J, Lin DM, et al. Long-term follow-up of a community assignment, one-time endoscopic screening study of esophageal cancer in China. J Clin Oncol 2015;33:1951–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Chen R, Liu Y, Song G, Li B, Zhao D, Hua Z, et al. Effectiveness of one-time endoscopic screening programme in prevention of upper gastrointestinal cancer in China: a multicentre population-based cohort study. Gut 2020;70:251–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Liu M, He Z, Guo C, Xu R, Li F, Ning T, et al. Effectiveness of intensive endoscopic screening for esophageal cancer in China: a community-based study. Am J Epidemiol 2019;188:776–84. [DOI] [PubMed] [Google Scholar]
- 50. Zhang N, Li Y, Chang X, Lei F, Ma H, Liu J, et al. Long-term effectiveness of one-time endoscopic screening for esophageal cancer: a community-based study in rural China. Cancer 2020;126:4511–20. [DOI] [PubMed] [Google Scholar]
- 51. Wang GQ, Wei WW. A new transition of the screening, early diagnosis and early treatment project of the upper gastrointestinal cancer: opportunistic screening. Chinese J Preventive Med 2019;53:1084–7. [DOI] [PubMed] [Google Scholar]
- 52. Hao CQ, Liu ZC, Li BY, Wang JW, Guo GZ, Wang ZH, et al. Assessment of upper gastrointestinal cancer screening in Linzhou City. Chinese J Preventive Med 2020;27:1464–569. [Google Scholar]
- 53. Zhao T, Li YY, Chen R, Zhang N, Wang JL, Wei WQ, et al. Long-term effects of endoscopic screening for upper gastrointestinal cancer in Feicheng. Chinese J Preventive Med 2020;27:1470–5. [Google Scholar]
- 54. Feng X, Hua ZL, Qian DF, Zhou Q, Shi AW, Song TQ, et al. Analysis on the effectiveness of endoscopic screening in high risk population of upper gastrointestinal cancer in Yangzhong City. Chinese J Preventive Med 2020;27:1476–82. [Google Scholar]
- 55. Wang XZ, Cui WF, Chen R, Wei WQ, Wang GQ, Zhang YZ. Prospective cohort analysis of endoscropic screening for upper gastrointestinal cancer in Yangcheng county. Chinese J Preventive Med 2020;27:1483–91. [Google Scholar]
- 56. Li J, Chen R, Wei WQ, Wang GQ, Li B, Qiao L. Influence of endoscroic screening on upper gastrointestinal cancer mortality in Yanting County. Chinese J Preventive Med 2020;27:1492–7. [Google Scholar]
- 57. Song GH, Meng FS, Chen C, Gong YW, Gao ZG, Bai WL, et al. Cohort study in area with high incidence of upper gastrointestinal cancer in Cixian, China. Chinese Journal of Preventive Medicine 2020;27:1455–63. [Google Scholar]
- 58. Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet 2019;394:1145–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Piñeros M, et al. Global cancer observatory: cancer today. Lyon, France: International Agency for Research on Cancer; 2020. [cited 2022 Jun 4]. Available from: https://gco.iarc.fr/today/home. [Google Scholar]
- 60. Liu Y, Rao K, Wu J, Gakidou E. China's health system performance. Lancet 2008;372:1914–23. [DOI] [PubMed] [Google Scholar]
- 61. Liao Y, Chen X, Tang J. Differences of cigarette smoking and alcohol consumption by sex and region in China: a population-based, multi-stage, cluster sampling survey. Lancet 2017;390:S54. [Google Scholar]
- 62. National Health Commission. China health statistical yearbook. Beijing: China Union Medical University Press; 2022. p. 4–118. [Google Scholar]
- 63. Sun Z, Zhao L, Wang S, Zhang H, Wang X, Wan Z. Targeted poverty alleviation and households' livelihood strategy in a relation-based society: evidence from northeast China. Int J Environ Res Public Health 2021;18:1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Meng Q, Xu L, Zhang Y, Qian J, Cai M, Xin Y, et al. Trends in access to health services and financial protection in China between 2003 and 2011: a cross-sectional study. Lancet 2012;379:805–14. [DOI] [PubMed] [Google Scholar]
- 65. Dong H, Duan S, Bogg L, Wu Y, You H, Chen J, et al. The impact of expanded health system reform on governmental contributions and individual copayments in the new Chinese rural cooperative medical system. Int J Health Plann Manage 2016;31:36–48. [DOI] [PubMed] [Google Scholar]
- 66. Arnold M, Ferlay J, van Berge Henegouwen MI, Soerjomataram I. Global burden of oesophageal and gastric cancer by histology and subsite in 2018. Gut 2020;69:1564–71. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1 shows three major measures of data quality of cancer registries included in this study.
Supplementary Table 2 shows the change in esophageal cancer mortality rates in counties with and without screening programs.
Supplementary Table 3 shows the difference in age-standardized esophageal cancer mortality rates between 90th and 10th percentile counties by province and time period.
Supplementary Figure 1 shows the geographic distribution and population coverage of 782 counties included in final analyses, along with the population density of China.
Supplementary Figure 2 was a scatter diagram of the age-standardized esophageal cancer mortality rate in 1973-1975 and the absolute change in mortality rates from 1973–1975 to 2015–2017.
Data Availability Statement
Because of Chinese legal restrictions, raw data are not publicly available to share, but the research group can provide the data dictionary, study protocol, and descriptive data in table form. Requests can be made to W. Wei (weiwq@cicams.ac.cn).