Abstract
Aim of the study
To investigate the role of the novel adipokines visfatin and vaspin in hepatitis C virus (HCV)-cirrhotic patients with and without hepatocellular carcinoma (HCC) and their association with tumour characteristics and liver dysfunction.
Material and methods
This case-control study was carried out between March 2021 and September 2021. Serum visfatin and vaspin were measured in 67 HCV-cirrhotic patients (37 had HCC, and 30 did not) and 20 healthy individuals using enzyme-linked immunosorbent assay (ELISA).
Results
Serum visfatin and vaspin were substantially elevated in HCC patients compared to those without HCC and healthy controls (p = 0.001, < 0.0001, respectively) and significantly associated with hepatic dysfunction. At a cut-off value of 12.1 ng/ml, the sensitivity and specificity of the serum visfatin in detecting HCC were 67.6% and 83.3%, respectively. Serum vaspin at a cut-off value of 321 ng/dl had a sensitivity of 94.6% and specificity of 66.7%. In multivariate regression analysis, serum vaspin and albumin were independent risk factors for HCC development. Patients with Barcelona Clinic Liver Cancer (BCLC) stage D had significantly the highest serum levels of visfatin and vaspin (p = 0.03, 0.008, respectively).
Conclusions
Serum visfatin and vaspin were substantially higher in HCC patients, associated with tumour stage, and might be considered as potential biomarkers of HCC, but this should be confirmed in larger independent cohorts of patients with liver cirrhosis. Serum vaspin and albumin were independent risk factors for HCC development. There was a substantial association between visfatin, vaspin, and the severity of the underlying liver dysfunction.
Keywords: hepatocellular carcinoma, visfatin, vaspin, novel adipokines
Introduction
Hepatocellular carcinoma (HCC) is the sixth most common cancer (4.7%) and the third major cause of cancer-related mortality (8.3%) worldwide. Most HCC cases globally are attributable to chronic infection with hepatitis B (HBV) and C (HCV) viruses. Moreover, HCV is the leading virus-related cause of HCC in many countries including Egypt [1]. Therefore, it is important to study the factors that increase the risk of HCC in those with HCV infection [2].
Although the relationship between HCV and HCC is well established, it is still unclear and poorly understood how directly HCV causes cancer. The interaction between environmental, viral, and host cofactors may result in multiple genetic alterations which gradually accumulate in hepatocytes leading to the development of HCC [3]. It is well known that metabolic derangements, such as adipokine imbalance, are associated with the development of cancer, including HCC [2]. Adipokines are thought to encourage cancer cell progression by enhancing growth, inflammation, migration, and anti-apoptotic mechanisms which can facilitate cancer metastasis [4].
Visfatin is a pro-inflammatory cytokine abundantly produced in human visceral fat. It is positively correlated with body mass index (BMI) and associated with a variety of clinical disorders, including type 2 diabetes mellitus (DM) and obesity [5, 6]. Furthermore, there is a relationship between elevated serum levels of visfatin and the development and spread of various cancers, including colorectal, gastric, pancreatic, breast, ovarian, prostate, and oral cancers [4].
Vaspin has been isolated from subcutaneous and visceral white adipose tissue. Significant associations have been established between vaspin, BMI, and the percentage of body fat [7]. Furthermore, in chronic HCV (CHC) patients, vaspin is associated with significant liver fibrosis [8]. Few studies have been conducted to explore the link between vaspin and cancer; these studies demonstrated a stimulatory effect of vaspin on colorectal cancer cells and inhibitory effects on endometrial cancers [4, 9, 10].
To date, few studies have been conducted to investigate the role of serum visfatin and vaspin in HCC patients with inconclusive results. Moreover, their relevance in the diagnosis of HCC is not fully elucidated [2, 6, 11, 12]. Therefore, this study aimed to assess the potential role of serum visfatin and vaspin in HCV-cirrhotic patients with and without HCC on top and their possible association with tumour characteristics and liver dysfunction.
Material and methods
Patients
From March 2021 to September 2021, we enrolled 67 consecutive patients with HCV-related liver cirrhosis, of whom 37 (55.22%) had HCC, and 30 (44.78%) cirrhotic patients without HCC. In addition, we enrolled 20 healthy controls. All participants in this case-control study were enrolled from the Tropical Medicine and Gastroenterology Departments of Sohag and Assiut University Hospitals. The study protocol was revised and approved by the Ethics Committee of Sohag Faculty of Medicine (under IRB number Soh-Med-21-02-04 and ClinicalTrials.gov ID NCT04763707). Informed written consent was provided by all participants before enrolment. All patients were seropositive for anti-HCV and the diagnosis of liver cirrhosis was based on clinical data, sonographic, and laboratory characteristics. The diagnosis of HCC was established by the presence of the characteristic pattern of arterial phase hyperenhancement followed by washout in the venous phase on triphasic computed tomography (CT) [13].
We excluded patients with hepatocellular injury due to causes other than HCV; patients diagnosed with other malignancies; or with a history of prior local or systemic HCC-specific treatment.
Methods
All participants were subjected to complete medical history, clinical examination, abdominal ultrasound, and laboratory investigations. The presence of HCC was suspected by the presence of a hepatic focal lesion on abdominal ultrasound examination which was then confirmed by triphasic abdominal CT scan. We calculated the Child-Turcotte-Pugh (CTP) [14] and model for end-stage liver disease (MELD) scores [15] to evaluate the degree of liver dysfunction. HCC staging was established based on the Barcelona Clinic Liver Cancer (BCLC) staging system [16].
Laboratory investigations
Sample collection
About 12 ml of venous blood was withdrawn from the patients and controls by a clean venipuncture and immediately delivered to 4 tubes: 2 ml in an EDTA tube (ethylene diamine tetra-acetic acid) for a complete blood picture (CBC), 2 ml in a sodium citrate tube for prothrombin time (PT) and concentration (PC), and 8 ml of blood was delivered into two plain tubes for other investigations.
The following investigations were performed for all participants at admission:
a complete blood count (CBC) was performed by CELL-DYN 3700 (Abbott Laboratories, Diagnostic division, IL, USA);
prothrombin time and concentration were determined using a Dade Innovin, Thromborel S Kit on a Sysmex CS 1600 automated blood coagulation analyser (Sysmex Corporation, Kobe, Japan);
liver function tests (albumin, bilirubin, alanine aminotransferase [ALT] and aspartate aminotransferase [AST]), serum creatinine, blood urea, fasting blood glucose, and lipid profile (cholesterol and trigly- cerides) were performed using the Cobas c311 Chemistry Analyzer System (Roche Diagnostics, GmbH, Mannheim, Germany);
serum electrolyte (sodium and potassium) measurements were performed with the ISE Module Diastro (Diastro, Argentina);
hepatitis markers: hepatitis B surface antigen (HBsAg) and hepatitis C antibody (HCVAb) were determined using the Architect i1000SR System (Abbott Laboratories, Diagnostic division, Abbott Park, IL, USA);
α-fetoprotein (AFP) was determined only in patients with HCC using the Architect i1000SR System (Abbott Laboratories, Diagnostic division, Abbott Park, IL, USA).
Detection of vaspin and visfatin in serum
Vaspin and visfatin were assayed in serum samples using an enzyme-linked immunosorbent assay (ELISA) kit (Glory Science Co., Ltd USA, Catalogue #: 94785, Glory Science Co., Ltd USA, Catalogue #: 17539, respectively). Patient samples were diluted at 1 : 5 prior to the assay, and 10 µl of each sample was added to 40 µl of prediluted sample buffer in a polystyrene tube and mixed well. Controls and calibrators are ready to use and do not need to be diluted. One hundred µl of prediluted patient samples, controls, and calibrators were pipetted into the wells and incubated at room temperature for 60 minutes. Then, the microwells were washed 5 times with a previously prepared wash solution (300 ml). In each well, 50 µl of Chromogen solution A and 50 µl of Chromogen solution B were added. The plate was then incubated for 15 minutes at room temperature and protected from light. In each well, 50 µl of stop solution was added and incubated for 15 minutes at room temperature. The colour of the wells turned from blue to yellow. A Thermo Fisher Scientific Multiskan EX Microplate Reader (Thermo Fisher Scientific Oy, FI-01621 Vantaa, Finland) was used to measure the absorbance OD at 450 nm. By comparing the OD of the samples to a standard curve, the vaspin and visfatin concentrations were identified. The sensitivity of this assay was 10 pg/ml and was in the range 75-2400 pg/ml.
Statistical analysis
STATA program version 14.2 (Stata Statistical Software: Release 14.2 College Station, TX: Stata Corp LP.) was used. The mean ± standard deviation (SD), median, range, and interquartile range (IQR) were used to describe quantitative data. For normally distributed data the means were compared by the ANOVA or Student’s t-test. For non-parametric data, the medians were compared by the Kruskal-Wallis or the Mann-Whitney U test. Chi-square (χ2) or Fisher’s exact test was used to compare qualitative data that were presented as numbers and percentages. Receiver operating characteristics (ROC) curve analysis was used to detect the best cut-off value of serum visfatin and vaspin for the diagnosis of HCC. Pearson’s correlation and linear regression analysis tests were applied to study the correlations and associations of serum visfatin and vaspin with the study variables. Logistic regression analysis was applied to test the risk factors for the development of HCC. Graphs were prepared using STATA or Excel programs. The p-value < 0.05 was considered statistically significant.
Results
Baseline characteristics of the studied population
The baseline demographic and clinical characteristics of the studied cohort are summarized in Tables 1 and 2. HCC patients were older and had a significant male predominance and less advanced liver disease than those without HCC (45.95% were Child A, compared to 10%, p = 0.006). Furthermore, they had a significantly lower prevalence of upper gastrointestinal bleeding (UGIB), hepatic encephalopathy, ascites, anaemia, thrombocytopenia, hypoalbuminaemia, blood glucose and urea, and significantly higher levels of ALT, PC, and cholesterol. Also, serum visfatin and vaspin were significantly higher in the HCC group compared to liver cirrhosis and control groups. Other clinical and laboratory features were comparable between the three subgroups.
Table 1.
Baseline demographic and clinical characteristics of the studied patients
| Variable | LC with HCC n = 37 |
LC n = 30 |
P-value | |
|---|---|---|---|---|
| Age (years) | ||||
| Mean ±SD | 64.11 ±8.09 | 61.63 ±6.91 | 0.86 | |
| Median (range) | 64 (48-84) | 61.5 (43-77) | ||
| Gender, n (%) | ||||
| Female | 9 (24.32) | 15 (50) | 0.03 | |
| Male | 28 (75.68) | 15 (50) | ||
| BMI | ||||
| Mean ±SD | 32.66 ±4.79 | 31.22 ±5.7 | 0.88 | |
| Median (range) | 32 (24-44) | 31.6 (23-44.7) | ||
| Diabetes mellitus, n (%) | 8 (21.62) | 13 (43.33) | 0.06 | |
| Hypertension, n (%) | 7 (18.92) | 9 (30) | 0.29 | |
| Smoking, n (%) | 12 (32.43) | 5 (16.67) | 0.14 | |
| UGIB, n (%) | 7 (18.92) | 18 (60) | 0.001 | |
| Hepatic encephalopathy, n (%) | 7 (18.92) | 16 (53.33) | 0.003 | |
| Jaundice, n (%) | 10 (27.03) | 11 (36.67) | 0.39 | |
| Ascites, n (%) | 12 (32.43) | 16 (53.33) | 0.09 | |
| History of DAAs, n (%) | 30 (81.08) | 29 (96.67) | 0.07 | |
| Child class, n (%) | ||||
| A | 17 (45.95) | 3 (10) | 0.006 | |
| B | 12 (32.43) | 16 (53.33) | ||
| C | 8 (21.62) | 11 (36.67) | ||
| MELD score | ||||
| Mean ±SD | 14 ±7.15 | 15.06 ±6.72 | 0.35 | |
| Median (range) | 11 (6-36) | 13 (7-30) | ||
LC – liver cirrhosis, HCC – hepatocellular carcinoma, BMI – body mass index, UGIB – upper gastrointestinal bleeding, DAAs – direct-acting antivirals, MELD – model for end-stage liver disease
Table 2.
Laboratory parameters of the studied cohort
| Variable | LC with HCC n = 37 |
LC n = 30 |
Controls n = 20 |
P-value | P1 | P2 | P3 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total bilirubin (mg/dl) | |||||||||||||||
| Mean ±SD | 3.33 ±4.87 | 2.95 ±4.87 | 0.57 ±0.19 | 0.0001 | 0.66 | 0.0001 | 0.0001 | ||||||||
| Median (range) | 1.5 (0.2-23) | 1.65 (0.3-27) | 0.55 (0.2-1) | ||||||||||||
| ALT (IU/l) | |||||||||||||||
| Mean ±SD | 72.7 ±130.58 | 27.17 ±29.35 | 15.95 ±7.26 | 0.0001 | 0.001 | 0.0001 | 0.12 | ||||||||
| Median (range) | 38 (10-636) | 18 (6-160) | 13.5 (9-32) | ||||||||||||
| AST (IU/l) | |||||||||||||||
| Mean ±SD | 96.95 ±151.58 | 55.83 ±44.44 | 21.05 ±12.94 | 0.0001 | 0.06 | 0.0001 | 0.0001 | ||||||||
| Median (range) | 54 (12-885) | 43 (14-208) | 18.5 (12-70) | ||||||||||||
| Albumin (g/dl) | |||||||||||||||
| Mean ±SD | 3.3 ±0.79 | 2.62 ±0.61 | 3.74 ±0.44 | < 0.0001 | < 0.0001 | 0.06 | < 0.0001 | ||||||||
| Median (range) | 3.5 (1.4-4.6) | 2.65 (1.5-4) | 3.8 (3-4.5) | ||||||||||||
| PT (sec) | |||||||||||||||
| Mean ±SD | 15.58 ±3.37 | 16.08 ±2.13 | 12.06 ±1.67 | < 0.0001 | 1.0 | < 0.0001 | < 0.0001 | ||||||||
| Median (range) | 15 (12-26) | 16 (13-21) | 11.85 (10-16) | ||||||||||||
| PC (%) | |||||||||||||||
| Mean ±SD | 74.94 ±18.14 | 61.85 ±14.25 | 96.40 ±18.01 | < 0.0001 | 0.007 | < 0.0001 | < 0.0001 | ||||||||
| Median (range) | 76.7 (35-98) | 61.25 (41-88) | 97.6 (66.3-124) | ||||||||||||
| INR | |||||||||||||||
| Mean ±SD | 1.23 ±0.3 | 1.33 ±0.22 | 0.96 ±0.15 | < 0.0001 | 0.31 | 0.001 | < 0.0001 | ||||||||
| Median (range) | 1.1 (0.9-2.09) | 1.3 (1-1.8) | 0.95 (0.7-1.2) | ||||||||||||
| WBCs (103/ul) | |||||||||||||||
| Mean ±SD | 7.04 ±4.4 | 8.93 ±7.69 | 8.9 ±4.06 | 0.07 | 0.3 | 0.02 | 0.21 | ||||||||
| Median (range) | 6 (2-26) | 6.6 (2.6-40) | 9.4 (3-20) | ||||||||||||
| Haemoglobin (gm/dl) | |||||||||||||||
| Mean ±SD | 11.42 ±2.46 | 10.03 ±2.60 | 12.02 ±1.27 | 0.008 | 0.048 | 1.00 | 0.01 | ||||||||
| Median (range) | 12 (6.6-16) | 10.6 (5.5-15) | 12 (9.5-14) | ||||||||||||
| Platelets (103/ul) | |||||||||||||||
| Mean ±SD | 174.59 ±104.05 | 116.26 ±57.84 | 302.9 ±90.08 | < 0.0001 | 0.01 | 0.0001 | 0.0001 | ||||||||
| Median (range) | 153 (40-561) | 107.5 (40-246) | 307 (152-500) | ||||||||||||
| Na (mEq/l) | |||||||||||||||
| Mean ±SD | 134.05 ±5.14 | 134.4 ±6.4 | 138.65 ±2.5 | 0.005 | 1 | 0.006 | 0.02 | ||||||||
| Median (range) | 134 (121-146) | 135.5 (112-142) | 139 (134-143) | ||||||||||||
| Creatinine (mg/dl) | |||||||||||||||
| Mean ±SD | 1.48 ±1.01 | 1.53 ±0.93 | 0.69 ±0.23 | 0.0001 | 0.55 | 0.0001 | 0.0001 | ||||||||
| Median (range) | 1.2 (0.5-5) | 1.2 (0.7-5) | 0.65 (0.4-1.4) | ||||||||||||
| Urea (mg/dl) | |||||||||||||||
| Mean ±SD | 49.42 ±23.77 | 68.53 ±25.28 | 33.7 ±11.63 | 0.0001 | 0.0009 | 0.01 | 0.0001 | ||||||||
| Median (range) | 42 (20-123) | 59 (20-124) | 33.5 (16-55) | ||||||||||||
| Cholesterol (mg/dl) | |||||||||||||||
| Mean ±SD | 142.56 ±63.2 | 113.3 ±38.58 | 169.5 ±32.65 | 0.0001 | 0.04 | 0.03 | 0.0001 | ||||||||
| Median (range) | 145 (37-320) | 101 (49-230) | 172 (108-223) | ||||||||||||
| Triglycerides (mg/dl) | |||||||||||||||
| Mean ±SD | 164.84 ±64.21 | 147.27 ±70.59 | 131.05 ±51.82 | 0.12 | 0.21 | 0.04 | 0.51 | ||||||||
| Median (range) | 156 (55-356) | 136.5 (39-343) | 122.5 (65-262) | ||||||||||||
| Blood glucose (mg/dl) | |||||||||||||||
| Mean ±SD | 114.76±39.16 | 149.77±63.94 | 93.4±29.17 | 0.0009 | 0.04 | 0.004 | 0.002 | ||||||||
| Median (range) | 100 (73:243) | 135 (56:260) | 84.5 (70:200) | ||||||||||||
| Serum visfatin (ng/dl) | |||||||||||||||
| Mean ±SD | 14.18 ±5.4 | 10.88 ±2.54 | 10.12 ±4.81 | 0.001 | 0.0001 | 0.0001 | 0.03 | ||||||||
| Median (range) | 13.19 (8.21-39.11) | 10.39 (7.63-18.68) | 9.16 (0.54-26.16) | ||||||||||||
| Serum vaspin (ng/dl) | |||||||||||||||
| Mean ±SD | 408.19 ±68.24 | 304.47 ±55.7 | 216.1 ±55.07 | < 0.0001 | < 0.0001 | < 0.0001 | < 0.0001 | ||||||||
| Median (range) | 394 (313-588) | 301 (190-410) | 206.5 (81-316) | ||||||||||||
P-value compared the three groups, P1 compared HCC & LC, P2 compared HCC & controls, and P3 compared LC & controls. ALT – alanine transaminase, AST – aspartate transaminase, PT – prothrombin time, PC – prothrombin concentration, INR – international normalized ratio, WBCs – white blood cells
Most (59.46%) HCC patients had a single nodule, and the right lobe was affected in 64.86% of patients. The mean tumour size was 6.08 ±3.28 cm (range 2-17 cm). Portal vein thrombosis (PVT) was detected in 24.32% of HCC patients, abdominal lymph nodes (LN) in 5.41%, and none had distant metastases. The highest proportion (35.14%) of HCC patients was noted for BCLC stage B, and the median (IQR) of AFP was 526 (26.5-3628) ng/ml (Table 3).
Table 3.
Clinical features of HCC patients
| Variable | Summary statistics |
|---|---|
| HFL number, n(%) | |
| Single | 22 (59.46) |
| Multiple | 15 (40.54) |
| Maximum HFL size (cm) | |
| Mean ±SD | 6.08 ±3.28 |
| Median (range) | 5 (2-17) |
| Site of HFL, n(%) | |
| Right lobe | 24 (64.86) |
| Left lobe | 3 (8.11) |
| Both lobes | 10 (27.03) |
| Portal vein thrombosis, n(%) | 9 (24.32) |
| Abdominal lymph nodes | 2 (5.41) |
| AFP (ng/ml) | |
| Mean ±SD | 20968.64 ±75148 |
| Median (IQR) | 526 (26.5-3628) |
| BCLC stage, n(%) | |
| A | 8 (21.62) |
| B | 13 (35.14) |
| C | 8 (21.62) |
| D | 8 (21.62) |
HFL – hepatic focal lesion, AFP – α-fetoprotein, IQR – interquartile range,
BCLC – Barcelona Clinic Liver Cancer
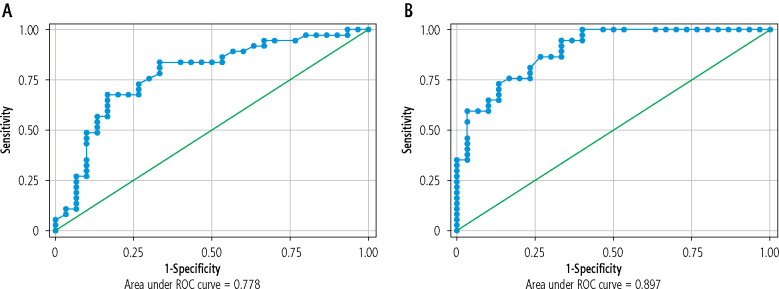
ROC curve study of the diagnostic accuracy of serum visfatin and vaspin for detection of hepatocellular carcinoma
When comparing HCC patients vs. cirrhotic patients without HCC we observed that at a cut-off value of 12.1 ng/ml, serum visfatin had a sensitivity of 67.6% and a specificity of 83.3% for the diagnosis of HCC (AUC = 0.778, 95% CI: 0.662-0.895), with a negative predictive value (NPV) of 67.6% and a positive predictive value (PPV) of 83.3%. Serum vaspin at a cut-off value of 321 ng/dl had a sensitivity of 94.6%, a specificity of 66.7% (AUC = 0.897, 95% CI: 0.824-0.97), with NPV of 90.9%, and PPV of 77.8% (Table 4, Fig. 1).
Table 4.
ROC curve analysis of the diagnostic performance of serum visfatin and vaspin for the detection of HCC
| Variable | Serum visfatin | Serum vaspin |
|---|---|---|
| Cut-off (ng/dl) | > 12.1 | > 321 |
| AUC (95% CI) | 0.778 (0.662-0.895) | 0.897 (0.824-0.97) |
| Sensitivity (%) | 67.6 | 94.6 |
| Specificity (%) | 83.3 | 66.7 |
| NPV (%) | 67.6 | 90.9 |
| PPV (%) | 83.3 | 77.8 |
| P-value | < 0.0001 | < 0.0001 |
AUC – area under the curve, PPV – positive predictive value, NPV – negative predictive value
Fig. 1.
ROC curve study to evaluate the performance of A) visfatin, and B) vaspin in the diagnosis of HCC in comparison to cirrhotic patients without HCC
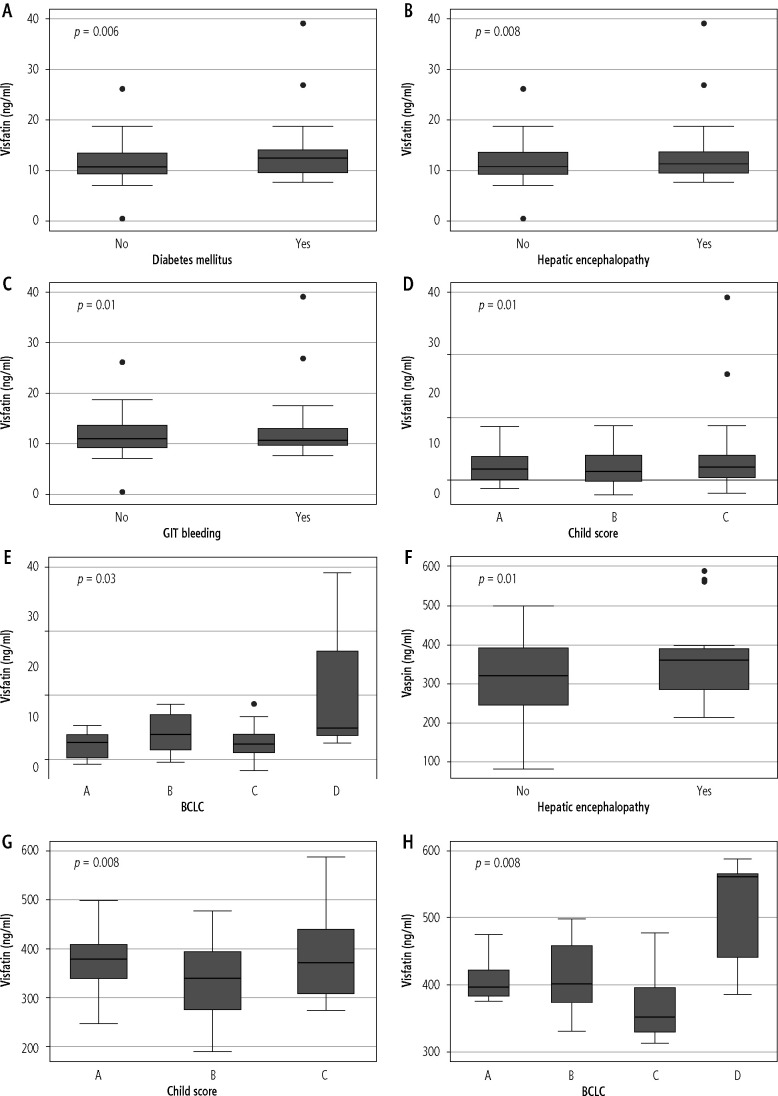
Associations between serum visfatin and vaspin levels, and clinical and laboratory parameters of study patients
In patients with HCC, serum visfatin showed a significant positive correlation with international normalized ratio (INR) and a significant negative correlation with platelet count, while serum vaspin exhibits a significant positive correlation with MELD score and a significant negative correlation with platelet count (Table 5). Additionally, serum visfatin level was substantially higher in diabetic patients, in those presenting with hepatic encephalopathy, UGIB, and as the Child class increased (p = 0.006, 0.008, 0.01, 0.01, respectively) (Fig. 2A-D). Serum vaspin was significantly higher in hepatic encephalopathy patients, and as the Child class increased (p = 0.008, 0.01, respectively) (Fig. 2F, G).
Table 5.
Correlation between serum visfatin and vaspin levels and clinical and laboratory parameters in HCC patients
| Variable | Serum visfatin | Serum vaspin | ||
|---|---|---|---|---|
| rho | p-value | rho | p-value | |
| Age (years) | –0.04 | 0.8 | –0.13 | 0.43 |
| BMI | –0.07 | 0.7 | –0.16 | 0.35 |
| Platelets (103/ul) | –0.33 | 0.048 | –0.39 | 0.02 |
| Total bilirubin (mg/dl) | –0.02 | 0.91 | 0.1 | 0.55 |
| ALT (IU/l) | –0.01 | 0.94 | –0.03 | 0.88 |
| AST (IU/l) | –0.04 | 0.81 | 0.03 | 0.87 |
| Albumin (g/dl) | –0.23 | 0.18 | –0.32 | 0.053 |
| PT (s) | 0.3 | 0.07 | 0.27 | 0.1 |
| INR | 0.36 | 0.03 | 0.32 | 0.051 |
| AFP (ng/ml) | 0.07 | 0.69 | 0.08 | 0.65 |
| Creatinine (mg/dl) | –0.18 | 0.29 | 0.13 | 0.44 |
| Cholesterol (mg/dl) | –0.24 | 0.15 | –0.24 | 0.16 |
| Triglycerides (mg/dl) | –0.23 | 0.16 | –0.08 | 0.62 |
| Random blood sugar (mg/dl) |
0.31 | 0.07 | 0.04 | 0.81 |
| MELD score | 0.09 | 0.6 | 0.33 | 0.04 |
| HFL size (cm) | –0.02 | 0.89 | 0.05 | 0.77 |
BMI – body mass index, ALT – alanine transaminase, AST – aspartate transaminase, PT – prothrombin time, INR – international normalized ratio, AFP – α-fetoprotein, MELD – model for end-stage liver disease, HFL – hepatic focal lesion
Fig. 2.
Association between serum visfatin (A-E), and vaspin levels (F-H) with the clinical parameters in HCC patients. GIT – gastrointestinal, BCLC – Barcelona Clinic Liver Cancer
We noted that HCC patients with BCLC stage D had substantially higher serum visfatin and vaspin levels (p = 0.03, 0.008, respectively). However, the mean levels of serum visfatin and vaspin did not consistently increase along with the stage of BCLC, being lowest in stage C (Fig. 2E, H). We found no association between visfatin and vaspin serum levels and HCC characteristics (Table 5 and Supplementary Table 1).
Logistic regression analysis for risk factors of HCC development among cirrhotic patients
In univariate analysis, male gender, serum visfatin, serum vaspin, albumin, cholesterol, and Child class B and C were substantially associated with HCC development. Multivariate regression analysis was conducted on significant factors in the univariate model and revealed that serum vaspin (OR = 1.05, 95% CI: 1.01-1.1, p = 0.009) and albumin (OR = 3.34, 95% CI: 1.06-8.26, p = 0.02) were independent risk factors for the development of HCC (Table 6).
Table 6.
Univariate and multivariate logistic regression analysis of risk factors predicting the presence of HCC in cirrhotic patients
| Variable | Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Age (years) | 1.05 (0.98-1.12) | 0.19 | 1.15 (0.97-1.38) | 0.11 |
| Male gender | 3.11 (1.1-8.78) | 0.03 | 1.31 (0.1-16.81) | 0.83 |
| Serum visfatin | 1.43 (1.13-1.81) | 0.003 | 1.16 (0.72-1.86) | 0.54 |
| Serum vaspin | 1.03 (1.02-1.05) | < 0.0001 | 1.05 (1.01-1.1) | 0.009 |
| DAAs | 0.15 (0.02-1.28) | 0.08 | 0.006 (0.00002-16.51) | 0.21 |
| Total bilirubin | 1.02 (0.92-1.13) | 0.75 | 1.24 (0.97-1.57) | 0.08 |
| Albumin | 3.61 (1.67-7.82) | 0.001 | 3.34 (1.06-8.26) | 0.02 |
| PT | 0.94 (0.79-1.11) | 0.48 | 1.18 (0.73-1.9) | 0.51 |
| Cholesterol | 1.01 (1.001-1.02) | 0.035 | 1.02 (0.99-1.04) | 0.12 |
| Triglyceride | 1.004 (0.996-1.01) | 0.29 | 1.001 (0.98-1.02) | 0.9 |
| MELD score | 0.977 (0.91-1.05) | 0.53 | 0.94 (0.7-1.27) | 0.7 |
| Child score | ||||
| A | Ref | Ref | ||
| B | 0.13 (0.03-0.56) | 0.006 | 1.04 (0.03-1.27) | 0.98 |
| C | 0.13 (0.03-0.59) | 0.008 | 0.18 (0.002-18.75) | 0.47 |
OR – odds ratio, 95% CI – 95% confidence interval, DAAs – direct-acting antivirals, PT – prothrombin time, MELD – model for end-stage liver disease
Discussion
The major outcome of the current study is that cirrhotic patients with HCC had substantially higher serum visfatin and vaspin levels than patients without HCC and healthy controls, and ROC curve analysis showed that both markers could serve as potential biomarkers of HCC, although further confirmation is required in larger independent cohorts of patients with liver cirrhosis. Additionally, serum vaspin and albumin were found to be independent risk factors for HCC development.
There is sufficient evidence that metabolic abnormalities, including adipokine imbalance, may raise the risk of HCC in those with viral hepatitis. HCV can cause insulin resistance in two different ways: directly by disrupting insulin signalling pathways and indirectly by promoting the production of pro-inflammatory cytokines. In patients with CHC, insulin resistance raises the risk of HCC. Furthermore, HCV enhances steatohepatitis, which may exacerbate inflammation, oxidative stress, and fibrosis and ultimately lead to the development of HCC [17, 18]. Substantial evidence revealed that in patients with viral hepatitis adipokines such as adiponectin and leptin could enhance steatohepatitis and subsequently the development of HCC [4]. At present, few studies have addressed the relationship between the novel adipokines visfatin, vaspin, and HCC risk. We found that serum visfatin and vaspin levels were substantially higher in cirrhotic patients with HCC than those with liver cirrhosis and healthy controls. This is consistent with earlier studies that found significantly higher serum levels of visfatin [11, 12, 19] and vaspin [6, 18] in HCC patients, and this could be linked to more advanced inflammation and higher HCC risk [2]. Ninomiya et al. [20] stated that visfatin had a significant role in the induction of HCC cell growth and it may be directly associated with the progression of this cancer.
Early diagnosis of HCC is important, as it is associated with better outcomes and improved survival. Currently, there is no definite effective tumour biomarker with optimal diagnostic accuracy and prognostic significance for HCC detection and diagnosis [21]. To investigate the diagnostic performance of serum visfatin and vaspin in HCC patients in comparison to cirrhotic patients without HCC, we performed ROC curve analysis. At a cut-off value of 12.1 ng/ml, serum visfatin had a sensitivity of 67.6% and specificity of 83.3% for the detection of HCC, with NPV of 67.6%, and PPV of 83.3%. The sensitivity and specificity in our study were lower than the values observed by El-Daly et al. [11] and higher than those reported by Sun et al. [12]. We observed that serum vaspin at a cut-off value of 321 ng/dl had a sensitivity of 94.6%, specificity of 66.7%, NPV of 90.9%, and PPV of 77.8%. To date, there have been no studies that evaluated the diagnostic role of vaspin in HCC patients, so further research is needed on larger independent cohorts of patients with liver cirrhosis to carefully validate its significance.
We found a significant association between serum visfatin and vaspin levels and hepatic dysfunction, as evidenced by their association with hepatic encephalopathy, and higher Child score grades. Furthermore, serum vaspin levels exhibit a significant positive correlation with the MELD score, and serum visfatin shows a significant positive correlation with INR. Contrary to our results Pazgan et al. [6] reported that there was no considerable variation in visfatin and vaspin serum levels among HCC patients regarding the Child score.
We observed that in patients with HCC, serum visfatin levels were substantially higher in diabetic patients than in those without DM. There are conflicting results regarding the relationship between serum visfatin and DM; some studies support our findings [2, 22, 23], whereas others contradict them [6, 24, 25]. The negative correlation observed in our study between platelet count and serum visfatin and vaspin, together with the significant association between serum visfatin and UGIB, raises the possibility of association of these markers with portal hypertension, which requires further validation in future studies.
We noted that patients with BCLC stage D showed the highest serum visfatin and vaspin levels (statistically significant). However, the mean levels of serum visfatin and vaspin did not consistently increase along with the grade of BCLC. However, we did not find any association between serum visfatin, vaspin, and other characteristics of HCC (tumour size, number, portal vein, nodal infiltration, or AFP level). Ninomiya et al. [20] found that the progression of the clinical stage of HCC was correlated with serum visfatin concentration. Furthermore, Tsai et al. [2] and Sun et al. [12] observed that plasma visfatin was associated with AFP, tumour size, and stage, and may play a role in HCC progression and prognosis. Pazgan et al. [6] found no association between visfatin and vaspin levels and the stage of HCC according to the BCLC staging system or tumour characteristics. These conflicting observations warrant further validation in larger cohorts of patients in well-designed studies.
In the current study, univariate regression analysis revealed that male gender, serum vaspin, serum visfatin, albumin, cholesterol, and Child classes B and C were significantly associated with HCC development. On the application of multivariate regression analysis on significant factors in the univariate model, serum vaspin and albumin were independent risk factors of HCC development. Previous research demonstrated that low albumin level is linked to a higher risk of developing HCC after the elimination of HCV infection [26], and in cirrhotic patients without HBV or HCV infection [27]. Carr et al. [28] reported that albumin is associated with HCC aggressiveness. Furthermore, Nojiri et al. [29] and Bağırsakçı et al. [30] concluded that albumin inhibits cell growth, hence inhibiting HCC proliferation.
To our knowledge, this is the first report to demonstrate the potential role of serum vaspin as a risk factor for HCC development independently of other factors. Several mechanisms have been suggested that may explain how vaspin contributes to tumour development, including insulin resistance, stimulation of the growth of cells with malignant potential, and prevention of apoptosis through cellular pathways [10]. However, vaspin seems to have anti-inflammatory properties through similar cellular mechanisms; therefore, it is hard to anticipate whether vaspin acts as a tumour promoter or inhibitor in different types of cancer [9]. Hence, more research is necessary to fully understand its role as a risk factor for the development of HCC.
There were some limitations in our study. The first limitation is the small sample size. Second, the study was conducted exclusively in HCV patients with a lack of comparison of the results with other aetiologies of liver disease. Third, we did not monitor the levels of both markers (serum visfatin and serum vaspin) after treating patients with HCC.
Conclusions
Serum visfatin and vaspin were substantially increased in cirrhotic patients with HCC, associated with tumour stage, and might be considered as potential biomarkers of HCC, but this should be confirmed in larger independent cohorts of patients with liver cirrhosis. Furthermore, serum vaspin and albumin were independent risk factors for HCC development. There was a substantial association between visfatin, vaspin, and the severity of the underlying liver dysfunction.
Acknowledgments
The authors express their deep gratitude and thanks to the patients and Prof. Mohamed Omar, Professor of Tropical Medicine and Gastroenterology, Faculty of Medicine, Assiut University, for their valuable help and support throughout this work.
Disclosure
The authors declare no conflict of interest.
Supplementary material is available on journal’s website.
References
- 1.Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021; 71: 209-249. [DOI] [PubMed] [Google Scholar]
- 2.Tsai IT, Wang CP, Yu TH, et al. Circulating visfatin level is associated with hepatocellular carcinoma in chronic hepatitis B or C virus infection. Cytokine 2017; 90: 54-59. [DOI] [PubMed] [Google Scholar]
- 3.Galal GM, Abudeif A, Ahmed NS, et al. Vitamin D receptor gene polymorphisms and risk of hepatocellular carcinoma in hepatitis C-related liver cirrhosis. Egyptian Liver Journal 2021; 11: 3. [Google Scholar]
- 4.Booth A, Magnuson A, Fouts J, et al. Adipose tissue, obesity and adipokines: role in cancer promotion. Horm Mol Biol Clin Investig 2015; 21: 57-74. [DOI] [PubMed] [Google Scholar]
- 5.Stastny J, Bienertova-Vasku J, Vasku A. Visfatin and its role in obesity development. Diabetes Metab Syndr 2012; 6: 120-124. [DOI] [PubMed] [Google Scholar]
- 6.Pazgan-Simon M, Kukla M, Zuwała-Jagiełło J, et al. Serum visfatin and vaspin levels in hepatocellular carcinoma (HCC). PLoS One 2020; 15: e0227459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kukla M, Zwirska-Korczala K, Gabriel A, et al. Chemerin, vaspin and insulin resistance in chronic hepatitis C. J Viral Hepat 2010; 17: 661-667. [DOI] [PubMed] [Google Scholar]
- 8.Kukla M, Waluga M, Sawczyn T, et al. Serum vaspin may be a good indicator of fibrosis in chronic hepatitis C and is not altered by antiviral therapy. Pol J Pathol 2012; 63: 213-220. [DOI] [PubMed] [Google Scholar]
- 9.Erdogan S, Sezer S, Baser E, et al. Evaluating vaspin and adiponectin in postmenopausal women with endometrial cancer. Endocr Relat Cancer 2013; 20: 669-675. [DOI] [PubMed] [Google Scholar]
- 10.Fazeli MS, Dashti H, Akbarzadeh S, et al. Circulating levels of novel adipocytokines in patients with colorectal cancer. Cytokine 2013; 62: 81-85. [DOI] [PubMed] [Google Scholar]
- 11.El-Daly UM, Saber MM, Abdellateif MS, et al. The possible role of adipokines in HCV associated hepatocellular carcinoma. Asian Pac J Cancer Prev 2020; 21: 599-609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sun Y, Zhu S, Wu Z, et al. Elevated serum visfatin levels are associated with poor prognosis of hepatocellular carcinoma. Oncotarget 2017; 8: 23427-23435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sherman M. Hepatocellular carcinoma: screening and staging. Clin Liver Dis 2011; 15: 323-334, vii-x. [DOI] [PubMed] [Google Scholar]
- 14.Pugh RN, Murray-Lyon IM, Dawson JL, et al. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg 1973; 60: 646-649. [DOI] [PubMed] [Google Scholar]
- 15.Kamath PS, Wiesner RH, Malinchoc M, et al. A model to predict survival in patients with end-stage liver disease. Hepatology 2001; 33: 464-470. [DOI] [PubMed] [Google Scholar]
- 16.Reig M, Forner A, Rimola J, et al. BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update. J Hepatol 2022; 76: 681-693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim JH, Sinn DH, Gwak GY, et al. Insulin resistance and the risk of hepatocellular carcinoma in chronic hepatitis B patients. J Gastroenterol Hepatol 2017; 32: 1100-1106. [DOI] [PubMed] [Google Scholar]
- 18.Pazgan-Simon M, Zuwała-Jagiełło J, Kukla M, et al. Serum concentrations of selected adipokines in virus-related liver cirrhosis and hepatocellular carcinoma. Clin Exp Hepatol 2020; 6: 235-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liang N, Chen Y, Yang L, et al. Visfatin increases miR-21 to promote migration in HCC. Cell Mol Biol (Noisy-le-grand) 2018; 64: 48-52. [PubMed] [Google Scholar]
- 20.Ninomiya S, Shimizu M, Imai K, et al. Possible role of visfatin in hepatoma progression and the effects of branched-chain amino acids on visfatin-induced proliferation in human hepatoma cells. Cancer Prev Res (Phila) 2011; 4: 2092-2100. [DOI] [PubMed] [Google Scholar]
- 21.Zhang Y, Gao J, Bao Y, et al. Diagnostic accuracy and prognostic significance of osteopontin in liver cirrhosis and hepatocellular carcinoma: A meta-analysis. Biomarkers 2021; 27: 13-21. [DOI] [PubMed] [Google Scholar]
- 22.Chang YH, Chang DM, Lin KC, et al. Visfatin in overweight/obesity, type 2 diabetes mellitus, insulin resistance, metabolic syndrome and cardiovascular diseases: a meta-analysis and systemic review. Diabetes Metab Res Rev 2011; 27: 515-527. [DOI] [PubMed] [Google Scholar]
- 23.Alnoggah SA, Zeid AF, Salem HM, et al. Study of serum levels of visfatin amongst pre-diabetic obese patients. Egypt J Hosp Med 2022; 86: 306-311. [Google Scholar]
- 24.Schindler K, Vila G, Hoppichler F, et al. The impact of type 2 diabetes on circulating adipokines in patients with metabolic syndrome. Obes Facts 2012; 5: 270-276. [DOI] [PubMed] [Google Scholar]
- 25.Karimi H, Nezhadali M, Mahdavi M, et al. Association of visfatin with blood glucose, insulin resistance and body mass index in patients with type 2 diabetes/pre-diabetes. J Adv Biomed Sci 2021; 11: 3984-3992. [Google Scholar]
- 26.Sato A, Sata M, Ikeda K, et al. Clinical characteristics of patients who developed hepatocellular carcinoma after hepatitis C virus eradication with interferon therapy: current status in Japan. Intern Med 2013; 52: 2701-2706. [DOI] [PubMed] [Google Scholar]
- 27.Yamada S, Kawaguchi A, Kawaguchi T, et al. Serum albumin level is a notable profiling factor for non-B, non-C hepatitis virus-related hepatocellular carcinoma: A data-mining analysis. Hepatol Res 2014; 44: 837-845. [DOI] [PubMed] [Google Scholar]
- 28.Carr BI, Guerra V, Giannini EG, et al. A liver index and its relationship to indices of HCC aggressiveness. J Integr Oncol 2016; 5: 178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nojiri S, Joh T. Albumin suppresses human hepatocellular carcinoma proliferation and the cell cycle. Int J Mol Sci 2014; 15: 5163-5174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bağırsakçı E, Şahin E, Atabey N, et al. Role of albumin in growth inhibition in hepatocellular carcinoma. Oncology 2017; 93: 136-142. [DOI] [PubMed] [Google Scholar]