Abstract
Background.
This article reviews the epidemiology of polio, acute flaccid paralysis (AFP) surveillance, and the implementation of supplemental immunization activities (SIAs) in Afghanistan from 1997 thru 2013.
Methods.
Published reports and unpublished national data on polio cases, AFP surveillance, and SIAs were analyzed. Recommendations from independent advisory groups and Afghan government informed the conclusions.
Results.
From 1997 thru 2013, the annual number of confirmed polio cases fluctuated from a low of 4 in 2004 to a high of 80 in 2011. Wild poliovirus types 2 and 3 were last reported in 1997 and 2010, respectively. Circulating vaccine-derived poliovirus type 2 emerged in 2009. AFP surveillance quality in children aged <15 years improved over time, achieving rates >8 per 100 000 population. Since 2001, at least 6 SIAs have been conducted annually.
Conclusions.
Afghanistan has made progress moving closer to eliminating polio. The program struggles to reach all children because of management and accountability problems in the field, inaccessible populations, and inadequate social mobilization. Consequently, too many children are missed during SIAs. Afghanistan adopted a national emergency action plan in 2012 to address these issues, but national elimination will require consistent and complete implementation of proven strategies.
Keywords: polio, disease eradication, Afghanistan, epidemiology, strategies
Afghanistan remains 1 of 3 countries globally where endemic transmission of wild poliovirus (WPV) continues uninterrupted [1]. Afghanistan is operationally divided into 7 regions, 34 provinces, and 399 districts (Figure 1). The south and west regions are the largest in area; however, the central, east, and parts of the west and north regions are among the most densely populated. Estimates of Afghanistan’s ethnically diverse population vary, but the Global Polio Eradication Initiative (GPEI) estimates there are 8.3 million children aged <5 years and 17 million children aged <15 years [2]. In 1988, the World Health Organization (WHO) Regional Committee for the Eastern Mediterranean Region (EMR) resolved to eliminate polio from the region by the year 2000 [3]. In late 1994, supplemental immunization activities (SIAs) that included polio and other childhood vaccines began in Afghanistan [4]. Polio vaccine–specific SIAs and acute flaccid paralysis (AFP) surveillance at major health facilities to detect possible polio cases, supported by WHO and the United Nations Children’s Fund (UNICEF) staff, started in 1997 [4].
Figure 1.
Political map of Afghanistan showing regions and districts.
Challenges to interrupting poliovirus transmission in Afghanistan include limited healthcare infrastructure and personnel [5, 6], low routine vaccination coverage [7], high rates of poverty and illiteracy [8], cultural norms that may restrict caregiver interaction with vaccinators [9], and subpopulations that travel frequently to at-risk areas of Pakistan, where WPV transmission is endemic [2]. SIAs have been hampered by areas of armed conflicts, limited monitoring and evaluation of coverage, and insufficient local program accountability and effectiveness to reach all children [2, 6]. The frequent cross-border migration of ethnic groups shared with Pakistan requires close coordination of each country’s respective immunization efforts [10].
Despite these obstacles, since 1997 a team composed of the Afghan Ministry of Public Health (MoPH), WHO, and UNICEF staff and other partners has made great progress in reducing poliovirus transmission, developing new approaches, and implementing the key GPEI strategies to reach all children with polio vaccine as outlined in the 2012 National Emergency Action Plan (NEAP) [5].
This article summarizes the history of GPEI in Afghanistan since 1997, and reviews the epidemiology of wild and vaccine-derived poliovirus cases, the quality and results of national AFP surveillance, and the implementation of GPEI strategies.
BACKGROUND
AFP Surveillance System
In 1997, Afghanistan first implemented all key strategies for polio eradication. This included a sentinel system for monitoring and reporting AFP cases at 37 major health facilities in regional capitals [11] with testing supported by the WHO-accredited Regional Reference Poliovirus Laboratory in Islamabad, Pakistan [12]. By 2003, AFP surveillance became an active system that shifted the classification of cases from clinical to virological. In the ensuing years, AFP surveillance quality exceeded global targets [11].
Supplementary Immunization Activities
From 1994 to 1996, 3 multiantigen immunization campaigns, targeting about 70% of children aged <5 years, provided measles, diphtheria-pertussis-tetanus, and OPV vaccines. In April and May 1997, National Immunization Days (NIDs) replaced earlier campaigns [4]. Since late 1999, increasing numbers of NID rounds and a house-to-house vaccination strategy improved vaccination coverage [11–15]. The SIAs used trivalent OPV until monovalent and bivalent OPV vaccines became available in 2005 and 2009, respectively. As early as 2001, SIAs were coordinated with neighboring Iran and Pakistan [16]. Postcampaign coverage assessments (PCAs) using independent monitoring and market surveys were conducted beginning in 2002 [13], but results were not officially recorded until 2006. Since 2005, Afghanistan has employed additional strategies, such as vaccination posts at border crossings, to reach nomadic and mobile populations [17].
Monovalent OPV types 1 and 3 were introduced in 2005 and 2007, respectively [17, 18]. In December 2009, Afghanistan conducted the world’s first large-scale use of bivalent OPV [20]. Finger marking children at the time of vaccination was introduced in 2008 to enumerate children vaccinated during a campaign and to facilitate PCA objectivity [19]. By 2009, efforts to reach more children in insecure areas included involvement of local leaders, nongovernmental organizations (NGOs), and short-interval additional dose campaigns where 2 OPV rounds in the same populations are conducted within 2 weeks of relative security [20]. Since 2008, there have been multiple efforts to negotiate PEI staff access to conflict areas [21].
Subsequent to the polio resurgence in 2011, advisory groups monitoring polio eradication efforts recommended improvements to Afghanistan’s program [22–24]. Consequently, the program developed the NEAP and implemented several strategies to enhance SIA effectiveness. The President’s Office monitors national implementation of the NEAP and engages provincial and district governors in PEI efforts through a national focal point for polio eradication.
Strategies include mapping to better define inaccessible areas; increasing the number of short-interval additional dose campaigns to reach missed children; introducing dashboards (display of program indicators color coded to show stage of achievement); equipping polio control rooms to monitor pre-, intra-, and postcampaign activities; conducting lot quality assessment sampling (LQAS) to better monitor SIA quality; establishing permanent polio teams in low-performing districts, and enhancing social mobilization and communication strategies [5].
Routine Immunization
In 1978, Afghanistan started implementing the Expanded Program on Immunization (EPI) with a 3-dose OPV schedule. Since 2003, routine vaccines are administered by NGOs contracted to provide basic health services in provincial hospitals and health centers and through outreach and mobile sites [25]. These NGOs are monitored by the national EPI but are accountable to a separate department of the Afghan MoPH [5].
METHODS
Information on AFP surveillance and polio incidence was compiled from the records of PEI-Afghanistan staffed by WHO and UNICEF and reports of the Centers for Disease Control and Prevention (CDC) and the EMR Office. These records provided the number of confirmed WPV, compatible cases, and circulating vaccine-derived poliovirus (cVDPV) cases from 1997–2013, AFP surveillance results and sensitivity indicators, and the vaccination status of nonpolio AFP cases.
The CDC’s global reference laboratory genetic sequencing reports provided genetic distribution data of WPV and cVDPV from fecal samples of AFP patients. The laboratory used viral cultures, 2 intratypic differentiation methods to determine the WPVs, and nucleic acid sequencing of the entire VP1 genome region of WPVs to determine genetic relatedness.
Three different sources were used for immunization coverage data. The PEI-Afghanistan PCA reports provided estimates of the percentage of children vaccinated and the percentage missed during each SIA. The 2010–2011 Multiple Indicator Cluster Survey and the 2007–2012 WHO-UNICEF published reports provided estimates of routine immunization coverage.
The NEAP prepared by the Afghan MoPH and partners to address the 2011 surge in polio cases provided information on current strategies and initiatives. Situation analyses of children missed during 2012 and 2013 SIAs were obtained from the PEI team report and a presentation by staff of the president’s focal point for polio eradication.
Social data were collected through independent monitoring, detailed case investigations, and Knowledge Attitude and Practices (KAP) surveys conducted in 2009 and 2012. The 2012 KAP surveyed caregivers of children aged <5 years in >2000 randomly selected households in 13 southern high-risk districts.
RESULTS
WPV Incidence and Genetic Clusters
In 1997 and 1998, there were 19 (7 laboratory confirmed) and 59 (27 laboratory confirmed) reported WPV cases, respectively, that met the pre-2001 criterion of residual paralysis for confirmed cases (Table 1). The last reported case of WPV type 2 was in 1997 [4].
Table 1.
Wild Poliovirus Confirmed Cases, Total Cases of Confirmed Polio, Circulating Vaccine-Derived Poliovirus, and Third-Dose Oral Polio Vaccine Coverage, 1997–2013
| Year | WPV1 | WPV2 | WPV3 | Total Confirmed Casesa | cVDPV2b | OPV3 Coverage (%)c |
|---|---|---|---|---|---|---|
| 1997 | 4 | 2 | 0 | 19 | . . . | 28 |
| 1998 | 15 | 0 | 12 | 59 | . . . | 28 |
| 1999 | 45 | 0 | 18 | 150 | . . . | 27 |
| 2000 | 18 | 0 | 10 | 120 | . . . | 24 |
| 2001 | 10 | 0 | 1 | 11 | . . . | 35 |
| 2002 | 5 | 0 | 5 | 10 | . . . | 36 |
| 2003 | 5 | 0 | 3 | 8 | . . . | 41 |
| 2004 | 2 | 0 | 2 | 4 | . . . | 50 |
| 2005 | 5 | 0 | 4 | 9 | . . . | 58 |
| 2006 | 29 | 0 | 2 | 31 | . . . | 58 |
| 2007 | 6 | 0 | 11 | 17 | . . . | 63 |
| 2008 | 25 | 0 | 6 | 31 | . . . | 64 |
| 2009 | 15 | 0 | 23 | 38 | 1 | 63 |
| 2010 | 17 | 0 | 8 | 25 | 5 | 66 |
| 2011 | 80 | 0 | 0 | 80 | 1 | 66 |
| 2012 | 37 | 0 | 0 | 37 | 11 | 71 |
| 2013 | 14 | 0 | 0 | 14 | 3d |
Abbreviations: avb,; cVDPV2, circulating vaccine-derived poliovirus; OPV, oral polio vaccine; WPV, wild poliovirus.
From 1997 through most of 2000, the number of total confirmed polio cases included clinical and WPV cases. After 2000, the total includes only WPV confirmed cases. Total does not include cVDPV cases.
Before September 2009, vaccine-derived poliovirus could not be differentiated from Sabin-like virus.
World Health Organization–United Nations Children’s Fund best estimates.
One case immunodeficiency-associated VDPV also detected in Northern region.
Following the peak in reported cases in 1999, total confirmed polio cases decreased substantially, reaching a nadir of 4–9 WPV cases during 2003–2005. From 2006 to 2010, an average of 28 cases occurred annually (range, 17–38) with 85% reported from the south region. However, in 2011, 80 confirmed WPV1 cases from 34 districts were the most laboratory-confirmed cases ever reported in Afghanistan, and 4 provinces reported their first case in ≥10 years. Since 2004, 2–13 compatible cases have been recorded annually.
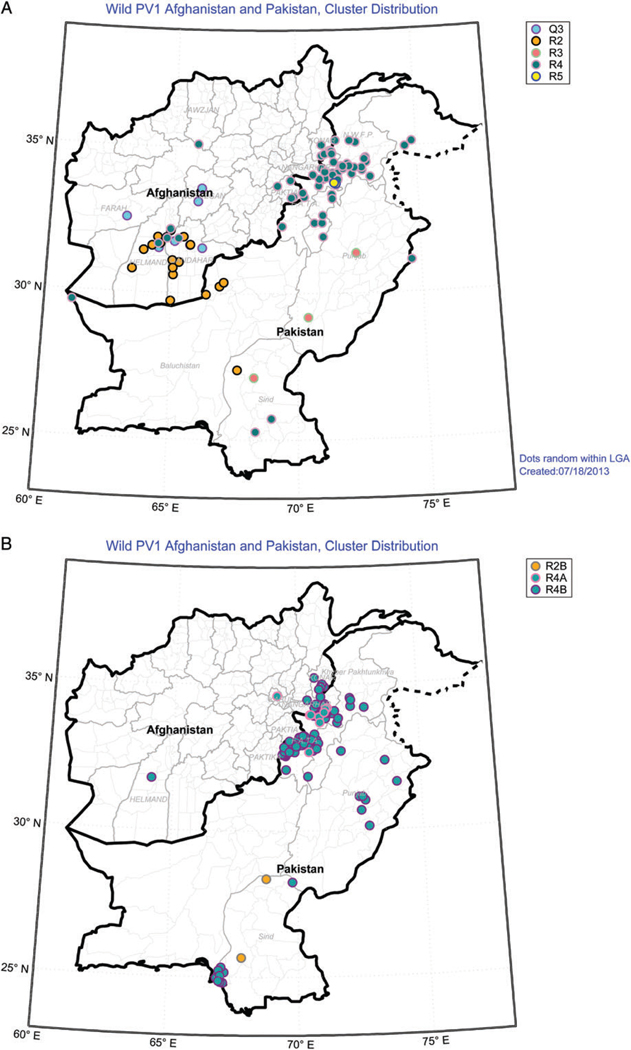
In 2012, 37 WPV type 1 (WPV1) cases from 21 districts were reported. Twenty-four cases (65%) were from the south, 2 from the west, and 11 from the east and southeast regions. In the south, 13 cases were from known high-risk districts and 2 cases were from families who refused vaccination. Virus genotyping data indicate that in 2012, polio transmission originated from index cases in both Pakistan and Afghanistan with shared transmission across the border (Figure 2). In 2013, only 14 WPV1 cases were reported from eastern (12), southern (1) and central (1) regions.
Figure 2.
Genetic profile of wild poliovirus cases in Afghanistan and Pakistan, 2012 (A) and 2013 (B). Abbreviation: PV1, poliovirus type 1.
Cases of type 3 WPV (WPV3) decreased steadily in the early 2000s; however, in 2007, there was a resurgence of WPV3 associated with the reduced use of type 3–containing OPV. WPV3 cases reached their peak in 2009 at 23, and none have been reported since April 2010.
Since 2001, when the distribution and genetic sequences of the cases were first analyzed, the main WPV reservoir has been in the south region, which forms an epidemiologic block with southwest Pakistan. Over the past 13 years, the biodiversity of the WPVs isolated from Afghanistan has varied but is now decreasing. Between 2000 and 2006, the number of virus lineages for WPV1 decreased from 10 to 5, and the number of WPV3 lineages decreased from 6 to 2. In 2010, 4 WPV1 and 1 WPV3 genetic linkages circulated in Afghanistan, but by 2012, only 4 WPV1 linkages were found: R2A, R2B, R4B, and Q3. Of these, Q3 and R2 are considered indigenous and continued to circulate in the south region through November 2012. However, almost all R4B viruses, which primarily circulate in the east and southeast regions, have direct genetic linkages to Pakistan. In late 2013 Afghanistan detected its first case of the R4A virus usually found in Pakistan (Figure 2).
cVDPV Incidence and Genetic Clusters
In 2009–2010, Afghanistan reported its first cVDPV cases [14]. Six type 2 cVDPV (cVDPV2) isolates were identified during June 2010–January 2011 in the south, where routine coverage was low and WPV1 was circulating. After response with 2 rounds of trivalent OPV, no additional cVDPV cases were detected until October–December 2012, when 11 cVDPV2 cases were reported in the southern provinces, representing a new emergence (4 cases) linked to southwest Pakistan and continued circulation of the lineage previously present in this region (7 cases). These patients had a median age of 18 months and vaccination history of 2 OPV doses. In 2013, 3 additional cVDPV2 cases were reported from the southern region with latest onset in March 2013.
AFP Surveillance
Since initiation, the sensitivity of AFP surveillance has improved steadily, first meeting all WHO performance indicators in 2002. Since 2003, the national program has exceeded the 80% target of proportion of adequate stools, and since 2007, the adequacy of the stool samples has been >90% (Table 2). At the subnational level, all regions have met or exceeded the 80% target since 2008, although the south region consistently has the lowest performance. Beginning in 2006, the nonpolio AFP rate has been >6 per 100 000 population.
Table 2.
Acute Flaccid Paralysis Surveillance, Afghanistan, 1997–June 2013
| Year | No. of AFP Cases | Met Specimen Standards, %a | Nonpolio AFP Rate per 100 000 Children Aged <15 yb |
|---|---|---|---|
| 1997 | 28 | 46.4 | 0.1 |
| 1998 | 122 | 48.4 | 0.7 |
| 1999 | 231 | 51.9 | 0.7 |
| 2000 | 253 | 49.4 | 1.1 |
| 2001 | 214 | 73.8 | 1.7 |
| 2002 | 335 | 79.7 | 2.3 |
| 2003 | 600 | 88.2 | 4.0 |
| 2004 | 687 | 90.8c | 4.5 |
| 2005 | 827 | 91.7 | 5.3 |
| 2006 | 989 | 89.2 | 6.2 |
| 2007 | 1116 | 91.8 | 6.9 |
| 2008 | 1383 | 92.2d | 8.2 |
| 2009 | 1477 | 92.5 | 8.8 |
| 2010 | 1572 | 92.6 | 9.2 |
| 2011 | 1830 | 92.1 | 10.5 |
| 2012 | 1829 | 92.3 | 9.9 |
| 2013 | 1879 | 93.0 | 9.9 |
Abbreviation: AFP, acute flaccid paralysis.
Quality of AFP surveillance is evaluated by 3 key indicators established by the World Health Organization (WHO): sensitivity of reporting (target: nonpolio AFP rate of ≥2 cases per 100 000 children aged <15 years; completeness of stool specimen collection (target: 2 adequate stool specimens from ≥80% of all persons with AFP); and proportion of stool specimens processed in a WHO-accredited laboratory.
United Nations population figures used to calculate rates.
In 2004, the global community changed the target for the sensitivity of reporting from 1 to 2 cases per 100 000 children aged <15 years, and the second indicator was modified to “the completeness and timeliness of stool specimen collection”—at least 80% of AFP cases with 2 adequate stool specimens collected >24 hours apart, both within 14 days of paralysis onset and shipped on ice or frozen packs to a WHO-accredited laboratory and arriving at the laboratory in good condition.
In 2008, the third indicator, the proportion of stools and specimens processed in a WHO accredited laboratory, was added as a separate measure of surveillance quality.
OPV Vaccination Coverage
In 1997, coverage with 3 doses of OPV (OPV3) at 1 year of age administered through the routine program was estimated at 28%. Estimated coverage consistently increased, with the WHO-UNICEF–estimated OPV3 coverage reaching 66% in 2010 and 2011 and 71% in 2012 (Table 1). However, the 2010–2011 Multiple Indicator Cluster Survey household survey found only 48% OPV3 coverage at 1–2 years of age, with coverage varying from 8% in the south region to 45%–58% in the other regions.
From 2010 to 2013, estimates of regional OPV3 vaccination coverage based on vaccination histories (with and without records) of children with nonpolio AFP show that most regions report 60%–90% routine OPV3 coverage, and >80% of nonpolio AFP cases reported >7 OPV doses (routine and SIA). The south region, however, maintained a low reported routine OPV coverage rate in nonpolio AFP cases that has decreased to <20% during the past 3 years. It also has the highest proportion of zero-dose nonpolio AFP children and the most reported cVDPV cases in the country.
Supplementary Immunization Activities
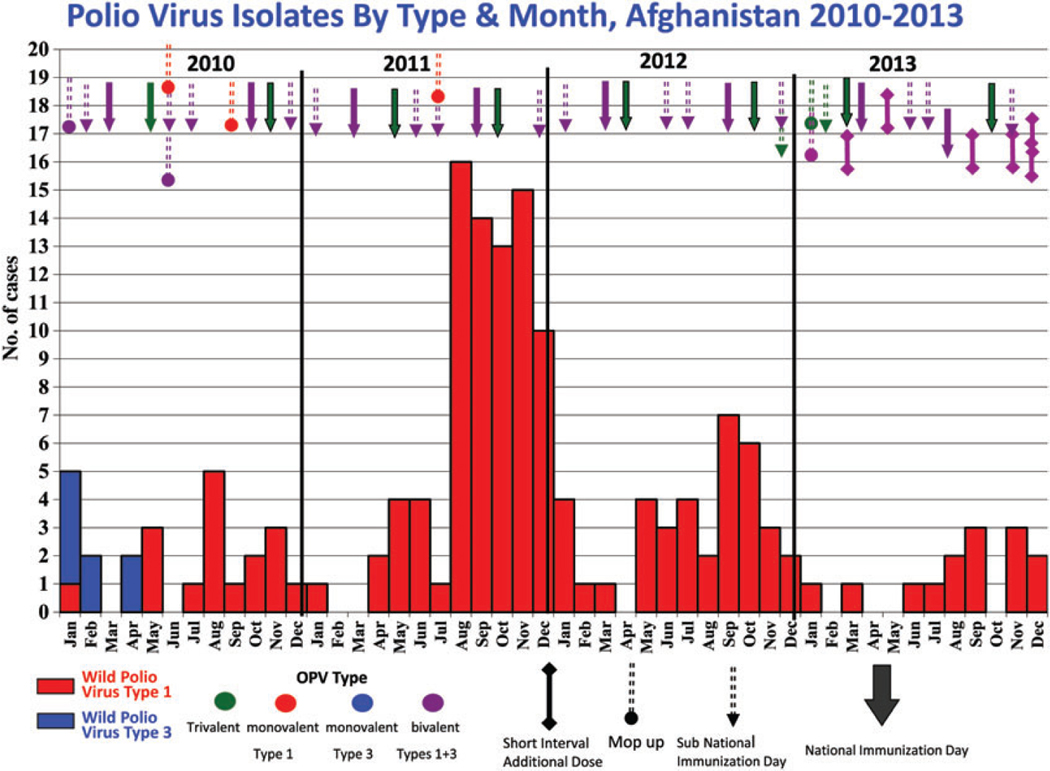
Since 1997, Afghanistan has conducted multiple rounds of NIDs and the geographically more targeted sub-NIDs annually (Table 3). In 2001, the introduction of house-to-house vaccinations reached 5.8 million children, compared to 4 million at fixed sites in 1999. SIA PCA results, first recorded officially in 2006, estimated OPV coverage of at least 80% of targeted children and often >90% (Table 3). Depending on the epidemiology of the most recent WPV and cVDPV cases, the SIA schedule used different configurations of OPVs and targeted either all or only specific areas of the country (Figure 3).
Table 3.
Supplementary Immunization Activities at National and Provincial Levels and Postcampaign Assessments, Afghanistan, 1997–2012
| Year | National Immunization Days | Subnational Immunization Days | Short-Interval Additional Dose | Othersa | Postcampaign Assessment Range |
|---|---|---|---|---|---|
| 1997 | 2 | Not done | |||
| 1998 | 2 | Not done | |||
| 1999 | 4 | Not done | |||
| 2000 | 4 | Not done | |||
| 2001 | 5 | 1 | 1 | Not done | |
| 2002 | 5 | 2 | 1b | Data not availableb | |
| 2003 | 4 | 3 | Data not available | ||
| 2004 | 4 | 2 | 2 | Data not available | |
| 2005 | 4 | 5 | 2 | Data not available | |
| 2006 | 5 | 5 | 4 | 93–98 | |
| 2007 | 4 | 3 | 4 | 95–98 | |
| 2008 | 4 | 6 | 4 | 95–98 | |
| 2009 | 6 | 4 | 5 | 88–93 | |
| 2010 | 4 | 4 | 83–98 | ||
| 2011 | 4 | 4 | 4 | 5 | 80–97 |
| 2012 | 4 | 4 | 3 | 86–92 | |
| 2013 | 4 | 4 | 11 | 2 | 93–96 |
Special rounds for nomadic children.
Postcampaign assessments begun in 2002, but not reported officially until 2006.
Figure 3.
Wild poliovirus polio cases types 1 and 3 and Supplementary Immunization Activities, Afghanistan, 2010–2013.
District-level PCAs demonstrated pockets of missed children. PCA data obtained March 2013 from 10 high-risk districts indicated about 11% of targeted children were missed, with 2% due to inaccessibility. This compares to the average of 16% reported missed in 13 high-risk districts during 2012 campaigns. Nationally in August 2013, 8% and 2% of children were missed in accessible and inaccessible areas, respectively. The data also documented that the majority (62%–100%) of children in these provinces were missed because they were outside the house, or because children were sick, newborn, or sleeping when the vaccinators arrived. Overt refusals accounted for <3% of children not vaccinated, except for the southern provinces where overt refusals accounted for up to 9.4% of missed children. Also, in the south and in 1 western province, the PCA data showed that the failure of vaccination teams visiting homes accounted for 7.6%–56.6% of missed children. Of concern is that results of LQAS assessments, first conducted in April 2013, are often substantially lower than PCA estimates.
Current Strategies
Following the 2011 surge of polio cases, MoPH and key stakeholders developed the NEAP to close the gaps in the following core areas: management and accountability, accessibility, communications and demand, and routine immunization.
In May 2012, the WHO’s Technical Advisory Group (TAG) on Polio Eradication in Afghanistan recommended that the PEI team focus on districts with demonstrated poor SIA performance and high polio risk (designated as low-performing districts [LPDs]). Accordingly, 13 southern districts were identified for special efforts, Specific criteria, which included polio cases within the past 2 years, zero-dose AFP cases within 2 years, <90% finger marking coverage in the last 3 SIAs, and awareness levels <50% in the last 3 SIAs, were developed to identify these LPDs. In late 2012, 11, districts in the south met criteria (Table 4); in mid-2013, 30 districts (9 southern, 21 eastern) were designated LPDs.
Table 4.
Districts in Afghanistan’s South Region That Met the Country’s Criteriaa for Low Performance of Polio Eradication Activities in 2012
| Region | Province | District | Target Population, 0–59 mo | No. of Wild Poliovirus Cases |
No. of Children With AFP and No History of OPV |
Average Coverage With OPV During SIAsb (%) | Average Parental Awareness Levelsc | District Accessible to Vaccinators | ||
|---|---|---|---|---|---|---|---|---|---|---|
| 2011 | 2012 | 2011 | 2012 | |||||||
| South | Helmand | Bust/Lashkarga | 71 028 | 1 | 1 | 4 | 3 | 88 | 74 | Yes |
| Nahr-e saraj | 76 768 | 5 | 6 | 4 | 2 | 87 | 63 | Yes | ||
| Sarban Qala (Sangin) | 29 589 | 0 | 1 | 0 | 1 | 88 | 85 | Yes | ||
| Nad-e Ali | 113 922 | 8 | 2 | 7 | 9 | 79 | 64 | Yes | ||
| Kandahar | Kandahar/Dand | 188 087 | 13 | 2 | 8 | 5 | 93 | 79 | Yes | |
| Shah Wali Kot | 35 000 | 3 | 0 | 6 | 0 | 55 | 5 | Yes | ||
| Arghandab | 23 244 | 1 | 0 | 2 | 1 | 82 | 35 | Yes | ||
| Khakrez | 9191 | 1 | 1 | 1 | 1 | 44 | 25 | Yes | ||
| Maiwand | 42 893 | 8 | 7 | 10 | 9 | 78 | 67 | Yes | ||
| Panjwai | 32 608 | 4 | 0 | 3 | 1 | 56 | 63 | Yes | ||
| Spin Boldak | 48 313 | 3 | 0 | 0 | 1 | 81 | 61 | Yes | ||
| Total | 2 | 11 | 670 643 | 47 | 20 | 45 | 32 | |||
Abbreviations: AFP, acute flaccid paralysis; OPV, oral polio vaccine; SIAs, Supplementary Immunization Activities.
Consideration for designation as a low-performing district are the following: any district that has confirmed polio cases in each of the last 2 years, or (1) any district with a polio case in 1 of the last 2 years; (2) zero-dose AFP in 1 or both of the last 2 years, plus (3) <90% finger marking coverage in the last 3 rounds of SIA, plus (4) an average level of awareness <50% in the last 3 rounds of SIAs plus significant continuous inaccessibility in the last 3 rounds of SIAs.
SIA coverage determined through postcampaign assessments of children with finger markings indicative of recent polio vaccination.
Awareness levels are the percentage of parents interviewed in a postcampaign assessment who knew of a scheduled SIA before the vaccinators arrived.
Management and Accountability
Over the past few years, the government reinforced its already strong political commitment to polio elimination in Afghanistan. A presidentially appointed senior advisor and PEI focal point provides oversight to NEAP implementation, liaises with the governors of provinces with LPDs, and reports progress directly to the president. In addition, the government formed an interministerial task force to better coordinate PEI efforts and a Polio High Council, which includes government and donors to address planning, implementation, and coordination strategy.
Although a reasonably strong management system exists at the national and regional levels, the program faces considerable difficulties and challenges in the field. Some of the salient issues in both accessible and inaccessible areas are the lack of permanent support and oversight of SIA implementation and assessments, lack of reliable financial and accountability mechanisms, and lack of human resources capacity, including female vaccinators and social mobilizers in areas where male–female interaction is extremely limited. Since 2012, all southern LPDs have established permanent district EPI management teams, supported by the MoPH, WHO, UNICEF, and NGOs. Their responsibilities include microplanning, training, and administrative and budgetary supervision. Additionally, a human resources surge continues to strengthen the number and quality of staff at the various administrative levels, especially in LPDs. Finally, as recommended in 2012 by the TAG, the program is establishing polio control rooms at the national level and in key provinces and districts, implementing dashboards, and using mobile technology to improve real-time data dissemination and decision making.
Inaccessibility
Areas are considered “inaccessible” if there are overt or perceived threats of violence to polio vaccinators. Most of Afghanistan is accessible to vaccinators, but in some regions, particularly the south and east, the mobility of staff during SIAs is seriously compromised because of control by nongovernmental forces. In the LPDs of the south region, 5%–6% of targeted children are reported as missed during each SIA because of inaccessibility.
Differences in district definitions of “accessibility,” unpredictable changes in local permission for vaccinator access, and the lack of verification of reported inaccessible areas make it difficult to compare district estimates of inaccessible children. Data from 2012 show that 8 of the 50 districts in the south region reported that >5% of children were missed during SIAs because of inaccessibility, and an additional 15 districts reported 1%–4.9% missed children for the same reason. In the east region where there has been less success brokering access, 5 districts reported missing >5% of children because of inaccessibility, and there were no SIAs in 1 district. In the southeast and west regions, ≤3 districts in each region reported inaccessibility problems during different SIAs. An assessment of children missed in 2012 and 2013 SIAs shows that the security situation improved but concluded that many more children were missed during SIAs because of reasons unrelated to accessibility, such as poor field management and accountability or societal attitudes and demand.
Beginning in April 2012, the program employed an innovative strategy of permanent polio teams (PPTs) to reach more children, especially in LPDs facing conflict and insecurity. The PPTs comprise 2 local community members who provide at least 1 dose of OPV to every child aged <5 years once every 3 months in a cluster or catchment area. By the end of 2012, 49 PPT teams were working in 10 LPDs. Data from September 2012 show that the teams in 8 LPDs had vaccinated almost 195 000 children, including approximately 10 000 who received their first dose of OPV.
Transit vaccination teams established at border crossings into Pakistan and Iran have proven successful, vaccinating >1 million children per year. This concept has now been applied to the borders of inaccessible districts. Other successful innovations to reach missed children included proactive local negotiations and special fixed vaccination sites.
Communications and Demand
Polio eradication efforts require a strong communications component that enlists parental and community support for routine immunizations and numerous SIAs. Among 22 cases in 2012 for whom data are available, 64% of caregivers knew what polio was, but only half knew it could be prevented. None of the mothers and only 14% of the fathers of these children were literate, emphasizing some of Afghanistan’s larger communication challenges.
Communication strategies have gained traction over the last year. Caregiver awareness of campaign dates, shown to improve coverage, has increased recently from the lowest in the world to almost 85% in the 11 LPDs. Public service announcements of upcoming campaign dates air monthly on southern television and radio programs with largely female audiences. The number of social mobilizers increased in all regions, primarily in the south by almost 100%. Mobilizers who visit homes prior to SIAs are present in >90% of targeted low-performing communities in the south. These mobilizers identify all eligible children and mark their homes so that vaccinators know how many children in a household need vaccine, decreasing the likelihood of missed children.
Routine Immunization
Despite improvements in routine vaccination coverage, injection safety, data and supply management, and the introduction of new vaccines made possible by substantial outside funding, a 2012 independent review found insufficient infrastructure and financing, suboptimal cold chain, low data quality, and lack of community engagement and awareness. As estimated by WHO, routine coverage of childhood vaccines has never exceeded 71%. Accordingly, the program introduced a 3-month accelerated routine immunization plan as part of the NEAP, with the first phase focusing on strengthening routine immunization services in LPDs.
DISCUSSION
Despite many challenges, Afghanistan continues its progress toward interrupting polio transmission. AFP surveillance has consistently improved, meeting global performance standards for timeliness and exceeding criteria for completeness. During the last 5 years, 14 provinces have remained polio-free and in 2013, 30 provinces have reported no cases including most in the historically polio-endemic southern region. Implementation of innovative strategies in 2012 indicates stronger national commitment, multiorganizational teamwork, and continued donor support. It remains encouraging that during 2013, only 14 WPV1 cases were reported.
Phylogenetic analyses have provided important information regarding virus transmission pathways and helped inform SIA vaccine decisions. In addition, the data highlight the importance of cross-border and coordinated vaccination campaigns, as cases linked to importations, particularly in the eastern region the last 3 years, pose a continued threat to polio eradication in both Pakistan and Afghanistan and a risk to neighboring polio-free countries. These analyses also demonstrate that 2 WPV1 genetic lineages and 1 cVPDV2 lineage were endemic in Afghanistan during 2011–2013 and highlight challenges to AFP surveillance, as evidenced by failure to detect cVDPV for almost 2 years and the continued occurrence of compatible cases. No cases associated with the Afghanistan WPV1 endemic lineages have been reported in 2013, but these may still be circulating and could persist and pose a risk to both Afghanistan and Pakistan. Improving national trends can mask present difficulties reaching pockets of children in LPDs. Periodic PEI assessments over the past few years, summarized in reports from the Independent Monitoring Board, the WHO TAGs in May and November 2012, and the NEAP, consistently identify the same areas of program weakness: management and accountability, accessibility, communications and demand creation, and routine immunization.
Some children remain unvaccinated because of overt or passive refusals by their caregivers. The reasons for this are not well understood, but a recent KAP found that the most common concerns cited for overt refusal were that the vaccine was unsafe, could cause sterility, or was not permitted under Islamic law. The lack of female vaccinators likely contributes to mothers’ refusals to interact with male vaccination teams and to instead provide excuses as to why she cannot present a child for vaccination.
At the core, however, an unacceptable number of children are missed during SIAs for reasons that can and should be addressed, and the majority of the missed children reside in areas accessible to vaccinators. A presentation from the office of the President’s PEI focal point aptly highlights that efforts to reduce the number missed have not met expectations and the results obtained have been disproportionate to the resources expended.
Another concern, as evident in years of low routine coverage and the continued detection of cVDPV2, is that EPI is also missing the most vulnerable children, threatening the successful interruption of cVDPV transmission and future implementation of IPV introduction. The NEAP is recognized for its cross-cutting innovations, such as PPTs to help address the program limitations; however, official endorsement at all levels of government took time and implementation of the strategies has been incremental. For example, the majority of polio control rooms in key areas are not fully functional, and about 24% of the southern LPDs remain without a PPT.
Vaccinating hard-to-reach children requires sustained commitment and monitoring at the district and cluster levels. Innovative methods to access all households, including those in highly conservative areas where only 10% of the current vaccinators are women, are extremely important if polio elimination is to succeed. However, it is in these areas where trained personnel and program dedication may be most lacking and supervision most difficult. The Afghanistan PEI program requires increased scrutiny of vaccination campaigns both to evaluate strategy effectiveness in LPDs and other at-risk areas and to ensure that other districts continue to improve. The development and use of district and provincial dashboards and polio control rooms, improved field management and accountability, and increased use of LQAS to monitor SIA coverage can prove valuable in these monitoring efforts.
Afghanistan is at a critical juncture in eliminating polio. Success is within reach, but time is of the essence. The government, in coordination with its partners, must implement proven strategies, particularly in the eastern and southern regions, if the interruption of both WPV and cVDPV transmission is to succeed.
Acknowledgments.
The authors thank the Provincial EPI Management teams who implement, supervise, and monitor PEI activities in their province, and all the vaccinators in Afghanistan, especially those who go from house to house in insecure districts. We also thank the many nongovernmental organizations that provide routine vaccinations throughout the country as part of the Basic Package of Healthcare Services. The authors thank the WHO Afghanistan PEI staff, especially Dr Mehmet Akif Saatcioglu and Ms Laurance Chabirand, who provided much of the data reviewed in this paper, and Brian Kaplan at the CDC, who created the maps presented in this article.
Financial support.
Donor organizations that have funded PEI activities in Afghanistan include Rotary International, the Bill & Melinda Gates Foundation, Australian Government Overseas Aid Program, Canadian International Development Agency, Japan International Cooperation Agency, US Agency for International Development, US Department of Health and Human Services, CDC, and World Bank.
Supplement sponsorship.
This article is part of a supplement entitled “The Final Phase of Polio Eradication and Endgame Strategies for the Post-Eradication Era,” which was sponsored by the Centers for Disease Control and Prevention.
Footnotes
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Centers for Disease Control and Prevention. Progress toward poliomyelitis eradication—worldwide, January 2011–March 2012. MMWR Morb Mortal Wkly Rep 2012; 61:353–7.22592275 [Google Scholar]
- 2.Ministry of Public Health, Islamic Republic of Afghanistan. Annual report 2012, Polio Eradication Initiative, Afghanistan. http://www.polioeradication.org/Portals/0/Document/InfectedCountries/Afghanistan/AnnualPEIReport2012_Afghanistan.pdf. Accessed 23 June 2013.
- 3.World Health Organization. Regional Office for the Eastern Mediterranean Region. Polio Eradication Initiative http://www.emro.who.int/polio/about/. Accessed 23 June 2013.
- 4.Centers for Disease Control and Prevention. Progress toward poliomyelitis eradication—Afghanistan, 1994–1999. MMWR Morb Mortal Wkly Rep 1999; 48:825–9. [PubMed] [Google Scholar]
- 5.Ministry of Public Health, Islamic Republic of Afghanistan. Afghanistan emergency action plan for polio eradication 2012–2013. http://www.polioeradication.org/Portals/0/Document/Aboutus/Governance/IMB/6IMBMeeting/3.4_6IMB.pdf. Accessed 23 June 2013.
- 6.Islamic Republic of Afghanistan. Ministry of Public Health, DG of Preventive Medicine, National Immunization Program. Comprehensive multi-year plan for National Immunization Program 2011–2015 update. 2012:6. http://www.irinnews.org/pdf/cmyp-afghanistan_immunization.pdf. Accessed 23 June 2013.
- 7.World Health Organization. Afghanistan: WHO and UNICEF estimates of immunization coverage: 2011 revision. http://www.who.int/immunization_monitoring/data/afg.pdf. Accessed 23 June 2013.
- 8.United Nations Statistics Division. World Statistics Pocket Book. Afghanistan. http://data.un.org/CountryProfile.aspx. Accessed 23 June 2013.
- 9.Mashal T, Nakamura K, Kizuki M, Seino K, Takano T. Impact of conflict on infant immunization coverage in Afghanistan: a countrywide study 2000–20003. Int J Health Geo 2007; 6:23. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1899486/pdf/1476-072X-6-23.pdf. Accessed 23 June 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. Progress towards eradicating poliomyelitis: Afghanistan and Pakistan, January 2011–August 2012. Wkly Epidemiol Rec 2012; 87:381–8. [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Progress toward poliomyelitis eradication—Pakistan and Afghanistan, January 2000–April 2002. MMWR Morb Mortal Wkly Rep 2002; 51:521–4. [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. Progress toward poliomyelitis eradication – Pakistan and Afghanistan, January 2006– February 2007. MMWR Morb Mortal Wkly Rep 2003; 56:340–3. [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Progress toward poliomyelitis eradication –Afghanistan and Pakistan, January 2002–May 2003. MMWR Morb Mortal Wkly Rep 2003; 52:683–5. [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Assessment of risks to the Global Polio Eradication Initiative (GEPI) strategic plan 2010–2012. Page 41. http://www.who.int/immunization/sage/2_CDC_risk_analysis_final_14Sept10.pdf. Accessed 23 June 2013.
- 15.Centers for Disease Control and Prevention. Progress toward poliomyelitis eradication—Pakistan and Afghanistan, January 2004–February 2005. MMWR Morb Mortal Wkly Rep 2005; 54:276–9. [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Progress toward poliomyelitis eradication—Afghanistan, 1999–2000. MMWR Morb Mortal Wkly Rep 2002; 50:144–7. [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. Progress toward poliomyelitis eradication—Pakistan and Afghanistan, January 2005–May 2006. MMWR Morb Mortal Wkly Rep 2006; 55:679–82. [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Progress toward poliomyelitis eradication—Pakistan and Afghanistan, 2007. MMWR Morb Mortal Wkly Rep 2008; 57:315–9. [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. Progress toward poliomyelitis eradication—Pakistan and Afghanistan, 2008. MMWR Morb Mortal Wkly Rep 2009; 58:198–201. [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. Progress toward poliomyelitis eradication—Pakistan and Afghanistan, 2009. MMWR Morb Mortal Wkly Rep 2010; 59:268–72. [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Progress toward poliomyelitis eradication—Pakistan and Afghanistan, January 2010–September 2011. MMWR Morb Mortal Wkly Rep 2011; 60:1523–7. [PubMed] [Google Scholar]
- 22.World Health Organization, Regional Office for the Eastern Mediterranean. Meeting of the Technical Advisory Group on Polio Eradication in Afghanistan, Kabul, Afghanistan, 6–7 May 2012. http://www.polioeradication.org/Portals/0/Document/Aboutus/Governance/IMB/7IMBMeeting/3.5_7IMB.pdf. Accessed 23 June 2013. [Google Scholar]
- 23.World Health Organization, Regional Office for the Eastern Mediterranean. Second meeting of the Technical Advisory Group on Poliomyelitis Eradication in Afghanistan, Kabul, Afghanistan, 27–28 November 2012. http://www.polioeradication.org/Portals/0/Document/Aboutus/Governance/IMB/8IMBMeeting/3.4_8IMB.pdf. Accessed 23 June 2013. [Google Scholar]
- 24.World Health Organization. Regional Office for the Eastern Mediterranean: independent review of the Afghanistan Polio Eradication Programme. 29 June–5 July 2012. http://www.polioeradication.org/Portals/0/Document/Aboutus/Governance/IMB/7IMBMeeting/3.6_7IMB.pdf. Accessed 23 June 2013.
- 25.Islamic Republic of Afghanistan. Ministry of Public Health, General Directorate of Health Care and Promotion, National EPI Office, Expanded Program on Immunization financial sustainability plan 2004–2009. Pages 1 and 15. http://www.who.int/immunization_financing/countries/afg/AFG_FSP.pdf. Accessed 23 June 2013.