Abstract
Objectives
Xylazine has emerged as a consistent part of the unregulated drug supply in recent months. We discuss major domains of xylazine’s harm, current knowledge deficits, clinical and harm reduction strategies for minimizing harm, and xylazine’s public health and policy context. As an interdisciplinary team from across the USA, we have pooled our knowledge to provide an overview of xylazine’s current and emerging contexts.
Methods
To inform this essay, the pertinent literature was reviewed, clinical knowledge and protocols were shared by multiple clinicians with direct expertise, and policy and public health context were added by expert authors.
Results
We describe xylazine’s major harm domains—acute poisoning, extended sedation, and wounds, along with anemia and hyperglycemia, which have been reported anecdotally but lack as clear of a connection to xylazine. Current successful practices for xylazine wound care are detailed. Understanding xylazine’s epidemiology will also require greater investment in drug checking and surveillance. Finally, approaches to community-based wound care are discussed, along with an orientation to the larger policy and public health context.
Conclusions
Addressing the harms of xylazine requires interdisciplinary participation, investment in community-based harm reduction strategies, and improved drug supply surveillance. The relatively unique context of xylazine demands buy-in from public health professionals, harm reduction professionals, clinicians, basic science researchers, policymakers and more.
Keywords: Xylazine, Harm reduction, Wounds, Drug injection
Background
Xylazine was originally developed in the 1960s to treat hypertension in humans, but this application was abandoned due to excessive sedative effects [1]; today, it is routinely used as a surgical anesthetic and procedural sedative in veterinary medicine, either alone or in combination with other medications. It is supplied as an injectable solution and sold under multiple brand names. Xylazine’s primary mechanism of action is agonism of alpha-2 adrenergic receptors (α2-ARs) leading to inhibition of presynaptic norepinephrine release [2], however new data suggests there may be alternative targets [3].
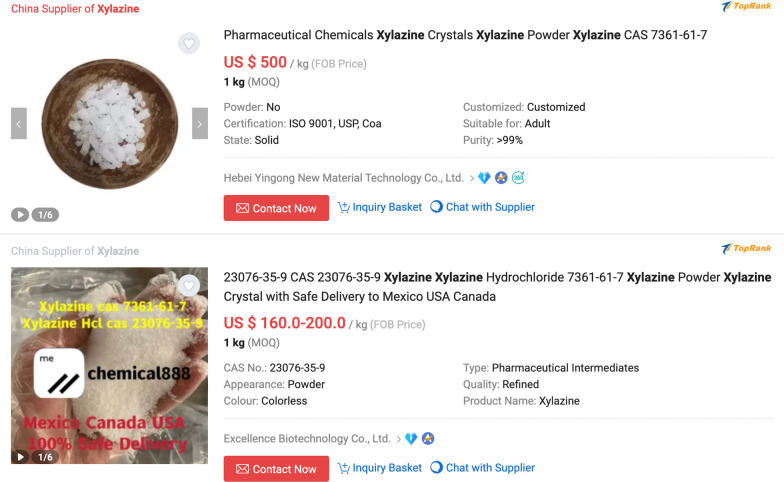
Xylazine was detected intermittently in the North American unregulated drug supply for decades, and case reports of poisonings were noted as early as the 1970s and 1980s [4]. It became common in the Puerto Rican drug supply in the 2000s, where it was primarily used alongside heroin and cocaine, and where its association with skin lesions was first identified [5, 6]. Xylazine has become increasingly prevalent in the North American unregulated opioid supply in recent years, but full extent of this increase is likely under-appreciated given xylazine is not routinely assayed in post-mortem toxicology, urine drug screens, and other common modes of supply monitoring [7]. Surveillance studies are hampered because vital statistics data do not have distinct codes to identify xylazine, so xylazine would not be noted on death certificates even if detected. It is unclear whether xylazine primarily comes from the veterinary pharmaceutical supply or is synthesized clandestinely, although the presence of empty discarded vials of xylazine (specifically AnaSed®, Akorn Pharmaceuticals) in areas of Philadelphia known for drug sales suggests that the former is at least contributory [8]. (Fig. 1) Xylazine sold as a hydrochloride salt can be purchased on Chinese online research chemicals marketplaces, constituting another potential source (Fig. 2).
Fig. 1.
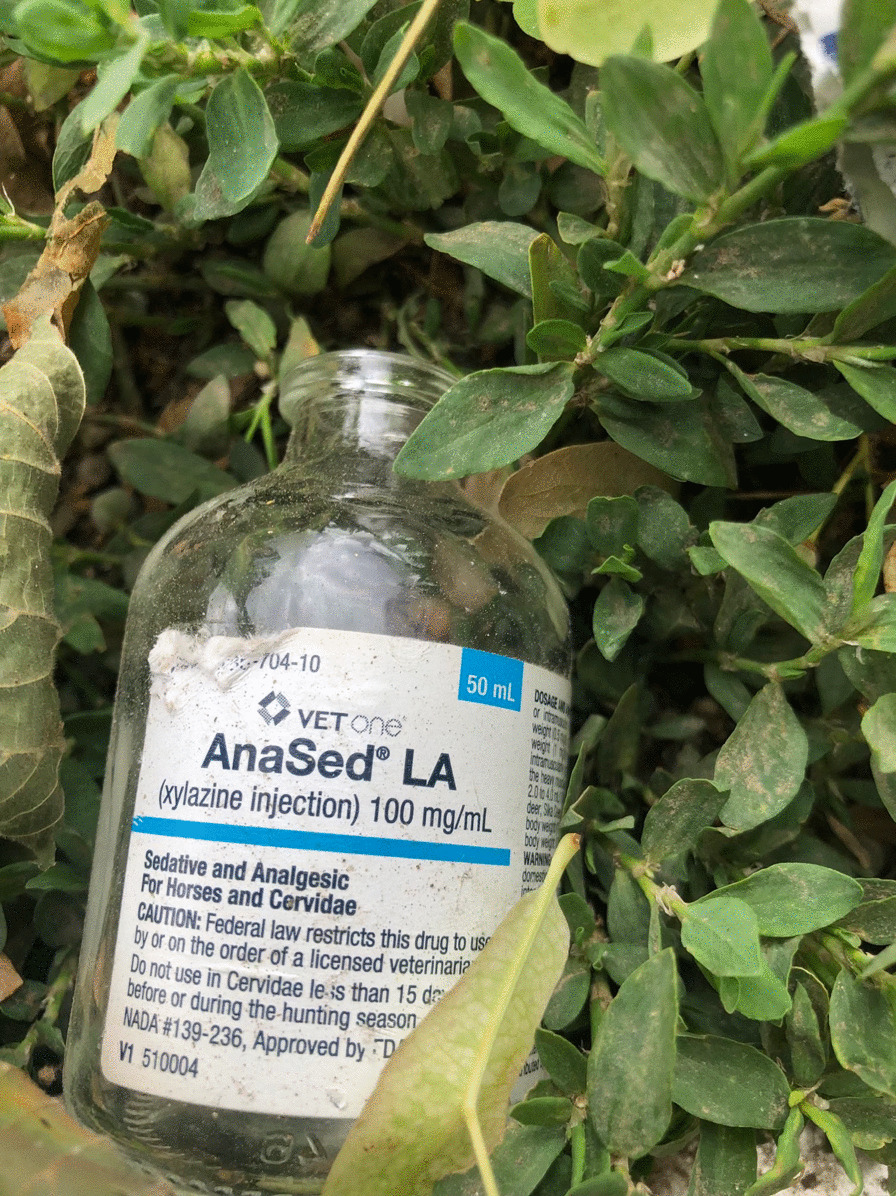
Photo of a discarded bottle of AnaSed® xylazine found in a shrubby area in Kensington, Philadelphia, Pennsylvania. Courtesy Christopher Moraff
Fig. 2.
Screengrabs from an online retailer offering xylazine for purchase
There are conflicting theories about why xylazine has been introduced into the unregulated drug supply [9]. On one hand, negative subjective feelings reported by people who use drugs about xylazine suggest incidental addition in a manner that could hamper sales. It is unclear at this point if xylazine is being sold as a pre-mixed cut, and there is likely regional variation to the specific manner in which xylazine is being processed and sold. Xylazine is found as a primary constituent in retail street samples, but also in trace quantities, further complicating whether this is from incidental inclusion or systematic addition. On the other hand, xylazine may be intentionally selected as a bulking agent given its sedative properties to allow for the inclusion of less opioid with the goal of inducing less severe respiratory depression. Given its pharmacological similarity to clonidine and lofexidine—effective treatments for opioid withdrawal syndrome—it is possible that xylazine may be intentionally selected for potential to mitigate these symptoms between opioid doses. Reports from people who use both fentanyl and xylazine support these propositions as they note xylazine increases the duration of effect from fentanyl and delays withdrawal symptoms [10]. Prior literature has demonstrated that increasing prevalence of fentanyl in the drug supply is associated with increased frequency of use [11], which is likely a response to fentanyl’s short half-life relative to that of heroin.
Harm reduction strategies
Three primary domains of harm have emerged in relation to xylazine exposure via the unregulated drug supply—acute poisoning, prolonged sedation, and skin wounds. While there is a dearth of clinical research evaluating acute and chronic xylazine exposure in humans, collected reports from across North America reveal actionable strategies which can be employed quickly to reduce harms related to xylazine use. Given the considerable stigma people who use drugs experience in conventional healthcare settings [12, 13], identifying harm reduction strategies that empower them to self-manage symptoms and to seek support from trusted sources in their community is critical.
Acute poisoning
Xylazine reduces level of consciousness while lowering heart rate and blood pressure. Human case reports have also identified decreased respiratory rate and the need for mechanical ventilation in instances of very high dose xylazine administration [14]. However, reports of fatalities from xylazine alone are extremely rare. From 2015–2020, the proportion of poisoning deaths in the USA involving xylazine increased substantially, but illicitly-manufactured fentanyls were present in 98.4% of xylazine-involved poisonings [15]. While xylazine may have additive or potentiating effects, this potential synergism is not yet clearly evidenced, and it is likely that fentanyls were the primary drivers of respiratory depression and death. Thus, even though naloxone does not directly and significantly antagonize the sedative effects of xylazine [3], it can nonetheless effectively treat many poisonings resulting from concomitant opioid and xylazine use, and naloxone remains a critical tool for anyone who may experience or respond to a drug poisoning. An acute reversal agent specific for xylazine has not been approved for use in humans, and whether such a drug would be helpful to reduce xylazine-associated poisoning deaths is unclear. While reversal of opioid poisoning with naloxone is generally safe even in a person with physical dependence to opioids, this is not true for all reversal agents which have been deployed in a drug poisoning context. For example, administration of flumazenil—a competitive antagonist of benzodiazepines—has resulted in death in polysubstance poisonings and induced seizures when administered to people with physical dependence to benzodiazepines [16]. Given that sudden discontinuation of other α2-AR agonists may induce rebound hypertension, it is plausible that rapid reversal of xylazine’s effects with an α2-AR receptor antagonist in a person chronically exposed to xylazine could result in a dangerous acute elevation in blood pressure [17]. Even in the absence of deployment of a specific reversal agent, clinicians must recognize that chronic exposure to xylazine may complicate withdrawal management in patients with opioid use disorder and treatment with α2-AR agonists may be warranted alongside opioid agonists [18].
Prolonged sedation
Extended periods of sedation and immobility have been reported by people exposed to xylazine through the unregulated opioid supply [10]. While “nodding” has long been a well-known effect of opioids such as fentanyl, the sedation attributed to xylazine appears distinct in some ways. The sedation produced by xylazine is lengthier, and associated with long periods of immobility. Reports have emerged of people using xylazine and subsequently nodding in awkward positions, such as hyperflexed at the waist or slouched against a wall, for several hours. Immobility is associated with several harms that are preventable via simple and very well-studied strategies. Traditional nursing interventions to prevent harms associated with immobility (such as pressure ulcers) include padding, regular turning (every 2 h), laying people on flat surfaces free of wrinkles or other irritating prominences, avoiding skin friction while moving or turning, and ensuring that skin remains dry [19, 20]. These are all practices that laypersons can easily learn and perform. Additionally, some positions in which people may nod, such as kneeling or hyperflexion at the waist, may theoretically present a risk of distal tissue injury from arterial kinking [21] and acute compartment syndrome [22]. Moving people who have nodded in awkward positions onto their side should be encouraged.
Further, people who use drugs, harm reduction professionals, and individuals working in related fields should be vigilant for other foreseeable harms of xylazine’s prolonged sedation. For example, increased rates of sexual assault, physical assault, and theft are likely to emerge as a significant xylazine-related harm. While xylazine is too new of a drug supply component for there to be literature on this issue at this time, the context of xylazine use and prolonged sedation may be reasonably compared to that of alcohol use, which has long been known to be associated with sexual assault [23]. Additionally, particularly for people experiencing homelessness, extended periods of sedation outdoors reasonably pose a heightened risk for traumatic injury if occurring on or near streets, sidewalks, train tracks, and similar contexts.
Skin wounds
While severe and at times limb and life-threatening skin and soft tissue infections (SSTIs) (usually attributed to Staphylococcus ssp. [24]) are commonly seen among people who inject drugs, the presentation of skin wounds attributed to xylazine exposure are distinct. While bacterial SSTIs are commonly seen at or near the site of injection, usually due to the introduction of bacteria by injection and associated local tissue trauma causing an abscess and/or cellulitis, one of the common hallmarks of xylazine-associated wounds is their emergence at sites other than those used for injection. These wounds are often described as large (greater than 10 cm in diameter), heterogeneous in appearance, granular and “burn-like”, and severe. An area of central necrosis is frequently observed, and a common course of progression is one of several small “punch-hole” wounds appearing in a cluster, which then coalesce into a single larger wound. Further, while wounds are often colonized with bacteria from skin/environment, they are not typically purulent, and in the absence of clear symptoms of infection do not require antibiotics. While xylazine-associated wounds are dramatic in appearance, it is important to note that they do often respond well to appropriate wound care, which should be implemented and exhausted before considering more radical options such as limb amputation. The cellular mechanisms underlying the atypical appearance and progression of these skin lesions are as-yet unknown, and basic science investigation is needed to illuminate these mechanisms.
While evidence is currently not yet sufficient to recommend standardized clinical guidelines on xylazine-related wound care the authors have a combined experience of caring for dozens of people with likely or confirmed xylazine-related skin lesions, over a period of several months, with many successes. We offer our cumulative recommendations both as a starting point for others in need of this information, and to prompt further research to help clarify and identify best practices.
Wound treatment and care for xylazine induced wounds in the outpatient setting relies on existing evidence-based practices, but must be approached with a harm reduction lens; typical or best practice treatment regimens may not be possible in the outpatient, street-based setting. Providing access to low barrier wound care with easily accessible supplies through a team-based approach (i.e., care provider and patient) may prove most beneficial. Interviewing the person with wounds in a non-judgmental, compassionate way allows for an in-depth understanding of the severity and timeline of the wound and may give way for relevant history [25]. It is important to document any previous treatments for the wound, as well as information about how the patient takes care of the wound; this interview will directly influence the type of treatments used during the visit and any upcoming appointments.
Regimens should be individualized for each patient, but can follow these major steps: 1) assess the wound and affected area, 2) cleanse wound with soap and water, wound cleanser, or saline solution depending on patient preference, product availability and potential allergy indication, 3) prepare supplies with necessary ointments or enzymatic or autolytic debriding agents (per prescribing provider order or clinic protocol), 4) dress the wound [26]. Hydrogen peroxide should not be used because it may delay wound healing via oxidative toxicity to fibroblasts [27]. In addition to these steps, motivational interviewing should be utilized to create a treatment plan in collaboration with the patient. Information about how to continue to care for the wound should be provided to the patient in a way that works for them; pre-made information sheets with symbols may be helpful, others may prefer recording the care provider's voice onto their phone with simple, replicable instructions to listen to when changing the dressing on their own.
When assessing the wound, documentation on measurements, tissue types (percent granulation, eschar, slough, presence of biofilm), signs of infection (erythema, edema, purulence) should be noted as well as systemic signs of infection (fever, chills, tachycardia) [28]. This assessment will guide the treatment course and care provision; if the wound has eschar, medical grade honey (often found as brand MediHoney® (Integra LifeSciences, Princeton, NJ)) wound gel or enzymatic collagen debridement ointments such as SANTYL (Smith + Nephew, Watford, England) may be used per protocol and indications, taking into consideration any potential allergies and contraindications [29, 30]. Mupirocin ointment, active against methicillin-resistant Staphylococcus aureus (MRSA), may be utilized as well [31]. These treatments, if indicated, can be applied directly to skin or a dressing such as petroleum gauze or nonadherent gauze. Before applying the impregnated gauze to the skin, care should be taken to cut the dressing to fit the wound area, while sparing any intact skin. For example, if there are areas of eschar among a greater area of slough and granulation tissue, the dressing with any enzymatic debridement should be applied to just the area indicated for treatment (eschar only), while another dressing with any indicated treatments, such as mupirocin on petroleum gauze or a nonadherent gauze, should be cut appropriately for the other types of tissue. This method prevents maceration of the wound bed while treating the most damaged tissue. Enzymatic debridements should be used with caution; it is necessary to ask the patient how often they are able to change their dressing. Enzymatic debridement will break down tissue and bacteria and if left on, can provide an ideal environment for continued bacterial growth and further infection and damage [30]. If the patient cannot change their dressing within twenty-four hours, enzymatic debridement [32] should be reconsidered. Depending on the amount of purulence, the patient's housing situation, and how long they may need to wait until their next dressing change, an ABD pad may be applied before wrapping the dressing with rolled gauze, tape, and/or elastic self-adhesive wrap.
Lesions may be present at individuals’ preferred injection locations, so education about why injection into or near lesions is harmful—in addition to general safer injection technique education—may be helpful for some patients. As venous access sites may be limited for some, a concern is a patient injecting through or alongside a xylazine-associated wound. Patients may want to inject into or near the wound in an effort to treat pain from the wound, or because prior intravenous drug use has scarred over other potential venous sites, leaving them with few options. Injecting into a wound increases the risk of bacterial superinfection of the wound and delayed healing, so alternatives to this should be explored as necessary. While non-ideal for concerns of infection and tissue injury, both subcutaneous and intramuscular injection (“skin popping” and “muscling”, respectively) are alternatives to injecting into or near a wound for people with limited points of venous access. These types of injection are also preferable to a patient accessing central veins, which carries a high risk of vessel and nerve injury [33] and systemic infection [34]. Other fruitful options include helping the patient locate new alternative points of venous access with aid of a tourniquet and/or a vein finder and encouraging use of the smallest feasible needle gauge in order to minimize local tissue injury and make use of smaller veins. Coaching the patient to drink plenty of water, apply a warm compress to the skin, and exercise the limb musculature prior to injection (e.g., performing push-ups) are also good options for increasing the intravascular volume of superficial limb veins, making these sites easier to access. Additionally, alternatives to injection altogether bypass many infection concerns. Fentanyl, which is the most-common opioid in the illegal supply at this time, may be consumed when heated on uncoated foil or in a glass pipe and the resulting vapor inhaled (“smoking”), insufflated (“snorting”) or administered rectally as a solution (“boofing”, “booty bumping”, among others). However, regional variation of the unregulated drug supply may make some routes of administration more acceptable and achievable than others, so collaboration with the patient and consideration for their experience is key. Additionally, it is not known if xylazine presents additional or more severe harms when consumed via varying routes, and so relative safety of using xylazine via a given route is unknown. As such, no specific route of administration can reasonably be described as “safer” at this time. Future research should explore the relative safety of these various routes of administration in the context of xylazine (Table 1).
Table 1.
Xylazine harm domains and clinical approaches
| Harm domain | Mechanism | Clinical implications | Harm reduction strategies |
|---|---|---|---|
| Heavy sedation | Alpha-2 receptor agonism |
Continued sedation after naloxone administration Pressure ulcers and skin breakdown likely Elevated risk for DVT Elevated risk of compartment syndrome Nerve, muscle, and soft tissue injury Rhabdomyolysis |
Encourage using drugs with a friend Roll people nodding onto their side Move people nodding every two hours Pad under bony areas (sacrum, heels, shoulders, etc.) Avoid wrinkled or hard surfaces under nodding person |
| Skin wounds | Unknown |
Bacterial superinfection possible Ensure adequate longitudinal wound care Can cause shame and reduced care-seeking Individuals may be deemed ineligible for in-patient substance use disorder care due to untreated wounds |
Coach to avoid injecting into or near wounds Facilitate wound care access Teach individual and friends/family how to care for wounds Provide wound care supplies Teach on signs of worsening condition |
| Anemia | Unknown; perhaps sympathetic antagonism |
Vague symptoms may delay care-seeking Important to rule out dietary or other causes |
Coach communities on signs and symptoms; when care-seeking is necessary Encourage and facilitate community support to identify changes in health status in self and others |
| Dysglycemia | Unknown |
Vague symptoms may delay care-seeking Important to rule out other causes of metabolic derangement Potential to worsen skin wound progress |
Coach communities on signs and symptoms; when care-seeking is necessary Encourage and facilitate community support to identify changes in health status in self and others |
Anemia and hyperglycemia
Transient anemia and hyperglycemia have been observed with xylazine administration in animals [35, 36]. Whether these may be observed in humans and progress to a level of severity warranting specific intervention in humans as a result of chronic exposure is unknown. Further research in this area is needed. While specific harm reduction strategies for addressing anemia and hyperglycemia are unclear, the larger-picture fundamentals of harm reduction are still very apt. Many of the early signs and symptoms of these two disease conditions—weakness, fatigue, dizziness, dry mouth—are non-specific and easily ignored. Thus, a fruitful harm reduction strategy may include providing education about signs and symptoms in case these conditions appear, supporting community cohesion among people who use drugs to encourage the observation of changes in health status in self and others, and offering to accompany potentially ill people to the hospital or clinic to advocate and help buffer against hostility and stigmatizing interactions from health care staff.
Awareness and engagement
The relatively rapid ascendance of xylazine as a component of the illegal drug supply, and the near-total lack of informative research on xylazine in humans, speaks to an under-appreciated danger of continued and expanded drug prohibition: the acceleration of the drug market away from well-understood substances such as heroin, to less-familiar substances which are relatively unknown to people who use drugs, clinicians, researchers, and policymakers, and which pose unknown health risks. While xylazine is an excellent example of this, so too are ascendant drug supply components such as the nitazene opioids and novel benzodiazepines such as flualprazolam. We urge rapid attention to xylazine in the basic sciences to illuminate its cellular mechanisms of action, and in the clinical context to inform best practices for management of xylazine-related health harms—in the etiologic sense of preventing xylazine-related wounds, and in the larger policy and social science context. Without these insights, comprehensive and scientifically rigorous care for people who use xylazine cannot be achieved.
Harm reduction leadership
Considering that one of xylazine’s hallmarks is severe wound formation, resources should be moved to harm reduction organizations, street outreach groups, and mutual aid organizations with close and preexisting relationships with people who use drugs in their community. For people who use drugs, a major barrier to seeking medical attention is maltreatment in the medical setting. This is particularly true for people seeking care for skin and soft tissue infections [13]. Since wounds such as those associated with xylazine use often require wound care over the course of several weeks, if this care was only offered in a traditional clinical setting it would likely fail to be broadly accepted and utilized as appropriate. Alternatively, organizations which have already built trusting relationships with people who use drugs are in an ideal position to provide necessary care, and so should be funded and empowered to do so for best results at the community level. The incorporation of wound care services into traditional harm reduction settings like syringe access programs can alleviate stigma, provide low barrier access to high quality care for participants, and help establish a point of care for individuals to receive basic treatment and share information with healthcare staff and each other [37].
Drug checking
Drug checking is one strategy to lessen the harms of xylazine. This approach involves testing drug samples for the presence of specific substances via methodologies such as immunoassay test strips and spectroscopy. People who use drugs may be unknowingly using xylazine, particularly when its presence in the drug supply is new to a region, and given its common commingling with opioids in the drug supply. In the case of xylazine, knowing of its presence can help people who use drugs make informed decisions guided by harm reduction practices. At the population level, comprehensive drug checking data can be aggregated to understand spatiotemporal trends in xylazine prevalence. Toxicology testing is another potential source of information about xylazine trends [15]. This information can also be a complement to drug checking information, however, there are limitations in this context. Toxicology testing is typically limited in its timeliness as it often occurs post-mortem, and due to common lags in data reporting. Additionally, xylazine is not yet a standard component of toxicology panels, making reporting from this domain imprecise for population-level insights.
Nothing about us without us
The empowerment of people who use drugs to check, disseminate, and act upon information about the unregulated drug supply is central to successfully mitigating the risks of xylazine and other contaminants. Both drug-using and selling communities (often one and the same) have the ability to rapidly communicate critical information obtained through empirical observation in an actionable and beneficial way to drug-using communities [38]. For this reason, people who use drugs must be empowered to engage in and lead self-determinant practices such as confidential drug checking, and should be employed whenever possible in testing settings [39]. Working directly with people who use drugs to form and implement drug checking and harm reduction strategies illustrates the scientific value of parsimony, and works to mitigate biases against people who use drugs. Bias against people who use drugs is a significant and omnipresent potential confounder which threatens valid conclusions in research. Through the meaningful inclusion and empowerment of people who use drugs in research relevant to this population, we confront threats to the validity of this research and create a richer and more insightful research community around drug use, while providing employment and pathways to career advancement to experts that are often excluded from the workforce owing to their drug use.
Drug war failure
Xylazine is unscheduled at the federal level, and to date is illegal only in Florida, where it was banned in 2018 [40]. Increased attention to xylazine and its harms has recently prompted a call for xylazine to be federally scheduled. However, we urge caution in such an approach. Scheduling xylazine would only control the licit supply, creating barriers to needed research on the health impacts, toxicology, and safety profile of the drug. Further, xylazine is used very commonly as a surgical anesthetic for animals used in pre-clinical research, including cancer research. Scheduling xylazine would disrupt these research areas and slow progress. Additionally, the ban of xylazine in Florida serves as a test case of sorts, and the results are wanting. Despite making xylazine illegal in 2018, the Drug Enforcement Agency (DEA) reports a 1127% increase in xylazine-involved overdose deaths in Florida’s field division [41] from 2020 to 2021. And finally, increasing prohibitions on substances has been shown repeatedly to prompt a less-safe drug market. With greater prohibition, the supply side of the unregulated drug market is motivated to invest in more potent substances which are logistically easier to conceal [42], clouding our understanding of the safety of the drug market and moving the drug supply away from one of consistency. An inconsistent and more-potent drug supply heightens health risks to people who use drugs.
Acknowledgements
The authors would like to thank Kastalia Medrano, Alex Krotulski, John Weems, Colin Miller, Louise Vincent, Don Jackson, and Maryalice Nocera
Author contributions
CZ conceptualized the article, wrote several sections, developed the table, edited for clarity, and managed the process. RH and SA wrote the portions on wound care, medical concerns, and helped create the table. CM contributed portions on xylazine epidemiology and potential scheduling of xylazine. AF contributed writing on the broader social context of xylazine and the drug war. MF contributed to the introduction and contributed and organized several references. NS confirmed accuracy and precision of medical context and recommendations, and verified the accuracy of the table. ZM contributed to the pharmacological discussion, and added context on xylazine’s use in pre-clinical research. LH contributed a discussion of the pharmacology of potential xylazine reversal drugs, and edited for clarity and ease of comprehension. ND supervised and led the development of this manuscript, offered guidance on themes, and offered insight from drug checking.
Funding
This article was produced without any funding.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable: this article does not include human or animal research.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
The original online version of this article was revised: the paragraph under the section “Drug War Failure" has been updated.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
11/27/2023
A Correction to this paper has been published: 10.1186/s12954-023-00903-w
References
- 1.Greene SA, Thurmon JC. Xylazine—a review of its pharmacology and use in veterinary medicine. J Vet Pharmacol Ther. 1988;11(4):295–313. doi: 10.1111/j.1365-2885.1988.tb00189.x. [DOI] [PubMed] [Google Scholar]
- 2.Kitano T, Kobayashi T, Yamaguchi S, Otsuguro K. The alpha(2A) -adrenoceptor subtype plays a key role in the analgesic and sedative effects of xylazine. J Vet Pharmacol Ther. 2019;42(2):243–247. doi: 10.1111/jvp.12724. [DOI] [PubMed] [Google Scholar]
- 3.Bedard M, Murray J, et al. Xylazine is an agonist at kappa opioid receptors and exhibits sex-specific responses to naloxone administration. Preprint. Posted September 9, 2023. 10.1101/2023.09.08.556914
- 4.Ruiz-Colon K, Chavez-Arias C, Diaz-Alcala JE, Martinez MA. Xylazine intoxication in humans and its importance as an emerging adulterant in abused drugs: a comprehensive review of the literature. Forensic Sci Int. 2014;240:1–8. doi: 10.1016/j.forsciint.2014.03.015. [DOI] [PubMed] [Google Scholar]
- 5.Reyes JC, Negron JL, Colon HM, et al. The emerging of xylazine as a new drug of abuse and its health consequences among drug users in Puerto Rico. J Urban Health. 2012;89(3):519–526. doi: 10.1007/s11524-011-9662-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rodriguez N, Vargas Vidot J, Panelli J, Colon H, Ritchie B, Yamamura Y. GC-MS confirmation of xylazine (Rompun), a veterinary sedative, in exchanged needles. Drug Alcohol Depend.2008;96(3):290–3. 10.1016/j.drugalcdep.2008.03.005 [DOI] [PMC free article] [PubMed]
- 7.Alexander RS, Canver BR, Sue KL, Morford KL. Xylazine and overdoses: trends, concerns, and recommendations. Am J Public Health. 2022;112(8):1212–1216. doi: 10.2105/AJPH.2022.306881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moraff C. "“Tranq Dope”—The Heroin Combo That’s Been Putting Philly to Sleep." Filter Magazine. 2 April 2019. Online. https://filtermag.org/tranq-dope-the-heroin-combo-thats-been-putting-philly-to-sleep/
- 9.Krishnan M. A Horrifying Drug Called ‘Tranq Dope’ Is Spreading in the US. Vice News. Nov 15, 2022. https://www.vice.com/en/article/akeqje/tranq-dope-in-united-states
- 10.Montero F, Bourgois P, Friedman J. Potency-enhancing synthetics in the drug overdose epidemic: Xylazine (“Tranq”), fentanyl, methamphetamine, and the displacement of heroin in Philadelphia and Tijuana. J Illicit Econ Dev. 2022;4(2):204–222. 10.31389/jied.122 [DOI] [PMC free article] [PubMed]
- 11.Lambdin BH, Bluthenthal RN, Zibbell JE, Wenger L, Simpson K, Kral AH. Associations between perceived illicit fentanyl use and infectious disease risks among people who inject drugs. Int J Drug Policy. 2019;74:299–304. 10.1016/j.drugpo.2019.10.004. [DOI] [PMC free article] [PubMed]
- 12.Ahern J, Stuber J, Galea S. Stigma, discrimination and the health of illicit drug users. Drug Alcohol Depend. 2007;88(2–3):188–196. doi: 10.1016/j.drugalcdep.2006.10.014. [DOI] [PubMed] [Google Scholar]
- 13.Figgatt MC, Salazar ZR, Vincent L, et al. Treatment experiences for skin and soft tissue infections among participants of syringe service programs in North Carolina. Harm Reduct J. 2021;18:80. doi: 10.1186/s12954-021-00528-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ball NS, Knable BM, Relich TA, Smathers AN, Gionfriddo MR, Nemecek BD, Montepara CA, Guarascio AJ, Covvey JR, Zimmerman DE. Xylazine poisoning: a systematic review. Clin Toxicol. 2022;60(8):892–901. doi: 10.1080/15563650.2022.2063135. [DOI] [PubMed] [Google Scholar]
- 15.Friedman J, Montero F, Bourgois P, Wahbi R, Dye D, Goodman-Meza D, Shover C. Xylazine spreads across the US: a growing component of the increasingly synthetic and polysubstance overdose crisis. Drug Alcohol Depend. 2022;233:109380. doi: 10.1016/j.drugalcdep.2022.109380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sivilotti ML. Flumazenil, naloxone and the 'coma cocktail'. Br J Clin Pharmacol. 2016;81(3):428–436. doi: 10.1111/bcp.12731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giovannitti JA, Thoms SM, Crawford JJ. Alpha-2 adrenergic receptor agonists: A review of current clinical applications. Anesth Prog. 2015;62(1):31–38. doi: 10.2344/0003-3006-62.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ehrman-Dupre R, Kaigh C, Salzman M, Haroz R, Peterson LK, Schmidt R. Management of Xylazine withdrawal in a hospitalized patient: a case report. J Addict Med. 2022;16(5):595–598. 10.1097/ADM.0000000000000955 [DOI] [PubMed]
- 19.Lyder CH, Ayello EA. Pressure ulcers: a patient safety issue. In: Hughes RG, editor. Patient safety and quality: an evidence-based handbook for nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); 2008 Apr. Chapter 12. https://www.ncbi.nlm.nih.gov/books/NBK2650/ [PubMed]
- 20.Mitchell A. Adult pressure area care: Preventing pressure ulcers. Br J Nurs 2018;27(18), 1050–1052. 10.12968/bjon.2018.27.18.1050 [DOI] [PubMed]
- 21.Ramondou P, Hersant J, Bernardeau E, Moumneh T, Feuilloy M, Henni S, Abraham P. Kneeling-induced calf ischemia: a pilot study in apparently healthy European young subjects. Eur J Appl Physiol. 2021;121(11):3031–3040. doi: 10.1007/s00421-021-04764-8. [DOI] [PubMed] [Google Scholar]
- 22.Clarke D, Mullings S, Franklin S, Jones K. Well leg compartment syndrome. Trauma Case Rep. 2017;11:5–7. doi: 10.1016/j.tcr.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abbey A, Zawacki T, Buck PO, Clinton AM, McAuslan P. Alcohol and sexual assault. Alcohol Res Health. 2001;25(1):43–51. [PMC free article] [PubMed] [Google Scholar]
- 24.Chambers HF. Skin and soft tissue infections in persons who inject drugs. Infect Dis Clin N Am. 2021;35(1):169–181. doi: 10.1016/j.idc.2020.10.006. [DOI] [PubMed] [Google Scholar]
- 25.Biancarelli DL, Biello KB, Childs E, Drainoni M, Salhaney P, Edeza A, Bazzi AR. Strategies used by people who inject drugs to avoid stigma in healthcare settings. Drug Alcohol Depend. 2019;198:80–86. doi: 10.1016/j.drugalcdep.2019.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Powers J, Higham C, Broussard K, Phillips TJ. Wound healing and treating wounds. J Am Acad Dermatol. 2016;74(4):607–625. doi: 10.1016/j.jaad.2015.08.070. [DOI] [PubMed] [Google Scholar]
- 27.Wilkins RG, Unverdorben M. Wound cleaning and wound healing: a concise review. Adv Skin Wound Care. 2013;26(4):160–163. doi: 10.1097/01.ASW.0000428861.26671.41. [DOI] [PubMed] [Google Scholar]
- 28.Brown G. Wound documentation: managing risk. Adv Skin Wound Care. 2006;19(3):155–165. doi: 10.1097/00129334-200604000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Majtan J. Honey: an immunomodulator in wound healing. Wound Repair Regen. 2014;22(2):187–192. doi: 10.1111/wrr.12117. [DOI] [PubMed] [Google Scholar]
- 30.Bryant RA, Nix DP. Chapter 17: wound debridement. In Acute & chronic wounds: current management concepts (pp. 295–305). 2017. Elsevier.
- 31.Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, Chambers HF. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin infect Dis. 2011;52(3):e18–e55. doi: 10.1093/cid/ciq146. [DOI] [PubMed] [Google Scholar]
- 32.Smith+Nephew. How to apply Collagenase SANTYL◊ Ointment. Accessed 12 April 2023. https://santyl.com/how-to-apply
- 33.Mackenzie AR, Laing RB, Douglas JG, Greaves M, Smith CC. High prevalence of iliofemoral venous thrombosis with severe groin infection among injecting drug users in North East Scotland: successful use of low molecular weight heparin with antibiotics. Postgrad Med J. 2000;76(899):561–565. doi: 10.1136/pmj.76.899.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hoda Z, Kerr T, Li K, Montaner JS, Wood E. Prevalence and correlates of jugular injections among injection drug users. Drug Alcohol Rev. 2008;27(4):442–446. doi: 10.1080/09595230802089701. [DOI] [PubMed] [Google Scholar]
- 35.Ambrosio AM, Keila Kazue IDA, Souto MTDMR, Claudio L, da Silva LC, Soares PB, Marcelo T. Significant hematocrit decrease in healthy horses during clinical anesthesia. Braz J Vet Res Anim Sci. 2012;49(2):139–145. [Google Scholar]
- 36.Xiao YF, Wang B, Wang X, Du F, Benzinou M, Wang YX. Xylazine-induced reduction of tissue sensitivity to insulin leads to acute hyperglycemia in diabetic and normoglycemic monkeys. BMC Anesthesiol. 2013;13(1):33. doi: 10.1186/1471-2253-13-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sanchez DP, Tookes H, Pastar I, Lev-Tov H. Wounds and skin and soft tissue infections in people who inject drugs and the utility of syringe service programs in their management. Adv Wound Care (New Rochelle) 2021;10(10):571–582. doi: 10.1089/wound.2020.1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kolla G, Strike C. Practices of care among people who buy, use, and sell drugs in community settings. Harm Reduct J. 2020;17(1):27. doi: 10.1186/s12954-020-00372-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dasgupta N, Figgatt MC. Invited commentary: drug checking for novel insights into the unregulated drug supply. Am J Epidemiol. 2022;191(2):248–252. doi: 10.1093/aje/kwab233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.03—Standards and schedules. The Florida Senate. Accessed 12 April 2023. https://www.flsenate.gov/laws/statutes/2018/893.03
- 41.Drug Enforcement Administration. The Growing Threat of Xylazine and its Mixture with Illicit Drugs. DEA Joint Intelligence Report. October 2022. https://www.dea.gov/sites/default/files/2022-12/The%20Growing%20Threat%20of%20Xylazine%20and%20its%20Mixture%20with%20Illicit%20Drugs.pdf
- 42.Beletsky L, Davis CS. Today's fentanyl crisis: prohibition's iron law, revisited. Int J Drug Policy. 2017;46:156–159. doi: 10.1016/j.drugpo.2017.05.050. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.