Abstract
This article takes stock of the research work carried out in Europe over the period 2020-2022 by a multidisciplinary consortium of specialists in psychiatry and mental health that brings together university research laboratories, psychiatric hospitals, universities, and training centers. Our work focuses on the difficulties encountered by care and psycho-social support professionals during the COVID-19 period. These difficulties are individual and organizational to ensure a service of accompaniment and follow-up of psychiatric users. What synthesis can we achieve of our successes, our failures, our limitations, and for which avenues of work for the future?
After presenting the methodological protocol, we conduct a self-critical reflection of the achievements in 3 main axes of analysis: 1. Evolution of working conditions in a context of uncertainty, 2. Organizational dimensions and hindered care, 3. Digital technologies.
From these results emerges a set of controversies and ethical questions relating to the legitimacy of remote care, confidentiality and protection of personal data, and equity in access to care. It appears that the professional practices deployed during the COVID-19 health crisis question the way in which the organization of care and social support integrate the possibilities offered by digital applications. They are about promoting the autonomy and empowerment of mental health service users and professionals.
From this perspective, the extension of this work develops a forward-looking approach included in Community digitization policies for new European projects. It appears necessary to carry out multidisciplinary in-depth work, by 2030 on hospital psychiatry and "outside the walls", the care pathway of the user, social support, digitalization, data management, and the training of professionals in technological changes.
Keywords: COVID-19, organization of care, professionals, psychiatry, digital technologies
Time for balance sheets...
As part of a research project, we conducted a study of the practices of psychiatric professionals, the management of their psychological consequences, and their organizational challenges. What lessons can be learned now from this research project entitled Psy-Gipoc, carried out during COVID-19, for the field of psychiatry and mental health in Europe? What have we learned from our experience about analyzing professional practices in and out of the hospital during the pandemic? What synthesis can we achieve of our failures, our limitations, and for which avenues of work for the future? Like State institutions and agencies that have drawn up observations, prospective analysis reports (HAS, 2023), it is time for assessments for the world of research in public health and psychiatric medicine. The following text constitutes a form of self-criticism of the work undertaken by a European and multidisciplinary team of researchers and clinicians over the period 2020-2022. It proposes research and development axes to extend the work undertaken during the Covid period based on the results of work carried out in 2020-2022 and their shortcomings. The Psy-Gipoc research project consists of a preliminary study in 2020, at the beginning of the pandemic, and in-depth European research in 2022, in the midst of a health crisis. We will take stock of the results and limitations of our results to propose a prospective vision for scientific input work on the evolution of professional practices in psychiatry and mental health.
In 2020, a consortium and a preliminary investigation
For the past ten years, a European consortium of specialists in psychiatry and mental health has brought together university research centres, psychiatric hospitals, universities and training centres to carry out European projects. In this collaboration, several countries are represented from Western Europe: France, Italy, Belgium, Luxembourg... from the East: Poland, Romania, and from the South: Greece, Malta, Spain... Effective multidisciplinarity, collaborative trust and friendship have made it possible from the beginning of the pandemic to quickly mobilize a network of 23 researchers, teachers, European clinicians, social sciences, public health, as well as psychiatric medicine and mental health, to launch a study, in real-time, on the practice of professionals to cope with the sudden COVID-19 crisis.
Our work focuses on the difficulties encountered by care and psycho-social support professionals during the COVID-19 period. These difficulties are individual and organizational to ensure a support and follow-up service for particularly vulnerable psychiatric patients.
Carried out in 2020, a preliminary survey work allowed us "to identify the main transnational challenges across Europe faced by psychiatric and mental health professionals: an ad hoc survey was conducted among 23 experts, from 23 different countries on psychiatry and mental health services, barriers to service delivery. Several key issues were reported by colleagues, even though they were at different stages of their national outbreaks (Thome et al., 2021). This research was carried out with local actors, and psychiatric professionals in the participating countries, and produced an "intercultural unifying perspective for sharing knowledge and multisectoral experiences" (Fond-Harmant & Tal Dia, 2008).
In 2021, the Psy-Gipoc research project
From this first survey at the beginning of the pandemic, we designed a research project entitled "Psy-Gipoc", to deepen the avenues of work (L. Fond-Harmant et al., 2021).
Psy-Gipoc Study Protocol
A research protocol was designed (L. Fond-Harmant et al., 2021) with the prospect of providing insight into the impact of the COVID-19 pandemic on the field of mental health professionals in 23 countries. The objective of Psy-Gipoc was to propose a model of recommendations of good practices and proposals of methods and digital tools to improve the well-being at work of mental health professionals and the quality of services offered in times of crisis and post-crisis. The dimension of an in-depth ethical review of the evaluation of the use of digital tools for psychiatric professionals and patient support, including teleconsultation, had been considered.
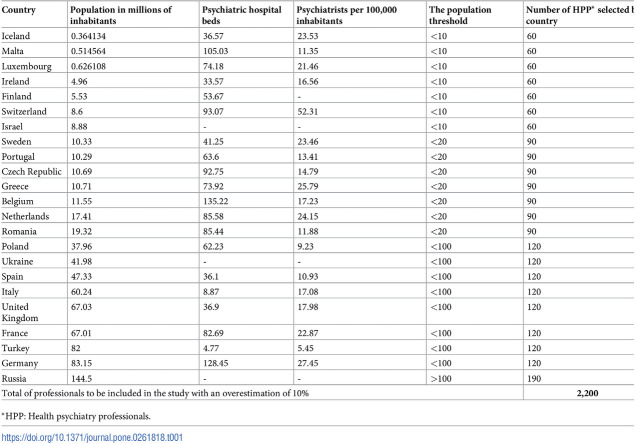
This is a large international survey conducted in 23 countries over a 12-month period. The survey is based on 30 individual interviews and 20 focus group sessions, and a digital questionnaire was sent to 2,000 professionals based on gender, age, professional experience, psychiatric specialty, psychiatric work context, and geographical location (table 1/inclusion criteria). Regarding the development of telepsychiatry, during the COVID-19 pandemic, a pilot study on the use of digital tools is being conducted among 100 psychiatric users in France and Belgium.
Table 1.
Selection criteria for the questionnaires among countries
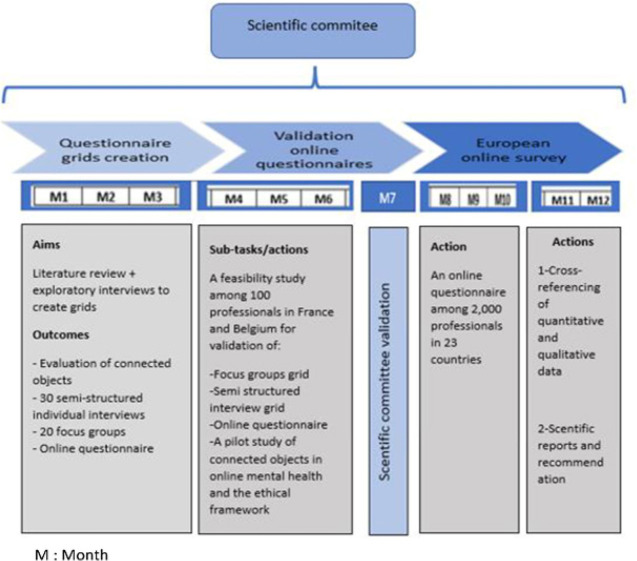
This is how Psy-Gipoc was born. Led by the University of Tours (Health Ethics Education Laboratory, EES-EA7505), co-funded by the National Research Agency and the Centre-Val de Loire Region – this project documented and questioned the adaptations implemented in this unprecedented context of an international health crisis. Operationally, Psy-Gipoc is led by 2 Research and Research Engineers (University of Tours-Laboratory-EES) and 2 scientific supervisors, one of whom is external (Sorbonne Paris Nord University, LEPS, and ACSEA-Luxembourg). Figure 1 presents over 12 months, the schedule of the Psy-Gipoc project and its methodological steps (Fond-Harmant and al., 2021)
Figure 1.
Psy-Gipoc project schedule and work stages
Intentions and objectives of Psy-Gipoc
This one-year project (2022) aims to design tools for remote medicine and to develop the use of digital applications to monitor and support professionals and help them build the conditions for satisfactory operational work in crisis and post-crisis situations, using adapted organizational methods. Psy-Gipoc supports professionals in the search for concrete existing solutions to deal with urgent work situations while maintaining an optimal quality of life. France, as coordinator of the project, is the pilot country for the design of methods and tools, including remote medicine (e-medicine) and the development of the use of connected electronic tools for monitoring and supporting professionals and users. These digital tools are initially intended to prevent psychological suffering and its consequences while accompanying staff and by targeting signs of discomfort.
Our research must support professionals in the search for concrete solutions so that they can cope with emergency work situations while maintaining an optimal quality of life. In connection with the deployment of artificial intelligence and psychiatry 3.0 (Briffault, 2017) open to the city, the Psy-Gipoc project will produce reflections and operational and concrete proposals. They will emerge from the working group, a specialist in psychiatry and mental health and work organizations, set up in March 2020. The research will mobilize this collective of 23 international experts in psychiatry and mental health on ethical and valorial issues of management practices in the context of the crisis and post-COVID-19 crisis (Chanut et al., 2015). The overall focus of the project is part of a 21st century public health vision and will help describe the impact of COVID-19 on work organizations and guide psychiatric professionals.
Results
Drawing on the international network of experts from the preliminary study, Psy-Gipoc was able to articulate important lessons learned from the early stages of the European COVID-19 pandemic and highlight key considerations for mental health services in all countries as the pandemic develops. For our self-critical synthesis of achievements, we have gathered 3 main lines of analysis:
Evolution of working conditions in a context of uncertainty,
Organizational dimensions and hampered care,
Digital technologies: Uses, challenges, and opportunities
1-Evolution of working conditions and uncertainties
As part of an approach based on documentary analysis and the implementation of the protocol validated by all partners, this work aims to understand the maintenance, in the best possible conditions, and medical follow-up of a patient with psychiatric disorders in the event of a health crisis while integrating the individual dimensions of professionals and the organizational dimensions of institutions and services Psychiatric. Concerning health isolation, this stage of research "highlights the deployment of common strategies within European mental health services, including the adoption of distancing measures, the reduction of hospitalizations, and the use of telepsychiatry. It documents the experience of professionals in these services in the face of reorganizations, changes in their working conditions, and uncertainties related to the adoption of new practices and, more broadly, the health crisis. It shows that the adaptations made in an emergency have often been built outside of "good practice" frameworks, placing professionals in the face of ethical dilemmas and controversies" (Gourret Baumgart et al., 2022).
New configurations, chaos, confusion, complexity, lack of harmonization of spontaneous practices developed in an emergency... These are the new working conditions studied during the pandemic and confinement.
Under tension for several years, the psychiatry and mental health sectors have adapted to manage the new needs generated by the crisis. Professionals have been subjected to strong and sometimes contradictory demands. Their knowledge gained through experience must be taken into consideration to rethink the organization of mental health care
2-Organizational and transformative dimensions
2-1 Experience of care hampered by health measures
"The covid-19 epidemic has pushed psychiatric and mental health services to adopt health measures to limit the risk of contamination. These measures have hindered the continuation of certain therapeutic activities, limited the possibilities of communication, and prohibited physical contact, preventing gestures of welcome and reassurance.
Based on 31 individual interviews and 5 group interviews conducted with health professionals working in psychiatric departments in France and Belgium, Psy-Gipoc examines how these professionals lived this experience of care hampered by sanitary measures, in particular physical distancing.
Shadow of them described a feeling of deterioration in the quality of care. They explained that they were faced with a transformation of their usual role. They have invested in videoconferencing, faced with the impossibility of continuing certain face-to-face care, which has clashed with their conceptions of care giving an important place to the meeting of the patient/user. The lockdown has reactivated the imaginary of psychiatric hospitalization conceived in the mode of isolation, contradicting efforts to co-construct rehabilitation, social reintegration, and recovery pathways" (Kane et al., 2020).
2.1.1. Renonciations, resistances and adaptations...
Faced with the dual challenge of managing the epidemic and ensuring continuity of care and patient support, health professionals have adopted postures of renunciation, resistance, and adaptation. The distancing measures have led them to live in relational and organizational situations through which they have reconsidered the importance of bodily co-presence in care, but also of the opening of services to the outside world. This experience questioned their roles and missions as caregivers, touching the limits of their values and ethics. As a result of a shared experience of the constraints of the pandemic, they apprehended with particular sensitivity what their patients were experiencing. Faced with situations reminiscent of asylum confinement, they implemented strategies of innovation and resistance to preserve the dignity and mental health of their patients.
2-2 Recomposition of territories and industrial relations
From the point of view of work organization, in this phase of research, the impacts of COVID-19 management on relations between health service professionals were questioned. The researchers focused on the situation of mental health professionals in this time of pandemic. These data were collected from 57 Belgian and French professionals through individual and group interviews. The analysis shows that professionals identify types of devices that are related to their practical effects in everyday work. Professionals give the devices put in place an "agency", the power to act, which implies that they act "against and with" these devices (Absil et al., 2022). "Agency" is that process that "enables individuals to play a role in their own development, adaptation and personal transformation in the face of change" (Bandura, 2001).
For researchers, the agency of work arrangements is particularly revealed by the mobilization of the concept of "geographical border", experienced or symbolic. The devices act on the boundaries that structure the work of professionals, make them obsolete or blur them; They create new frontiers, which supplant or overlap them. The action of work arrangements has consequences on roles and functions and thus makes it possible to analyze the reorganization of industrial relations in the context of a crisis (Absil et al., 2022).
3- Digital technologies
3-1-Use of digital tools
"The COVID-19 pandemic has forced mental health professionals to modify their practices to limit the risk of transmission of SARS-CoV-2, in particular by favouring remote monitoring via digital tools. We have delved deeper into the impact of this health crisis on their professional practices.
As before, in addition to an international literature review, the methodology adopted combines quantitative and qualitative methods with individual and group interviews and questionnaires among 2,000 European mental health professionals.
The research documents the evolution of the use of digital tools by mental health and psychiatric professionals in the face of the COVID-19 pandemic. It reveals a heterogeneous integration of these tools, depending on the country, context, regulations, and care modalities. Notwithstanding these variations, the use of videoconferencing has increased, affecting working conditions and therapeutic relationships. The pandemic has been an opportunity for professionals to build an experience of remote care and, thus, to better understand the possibilities and limitations of digital tools.
From these results emerges a set of controversies and ethical questions relating to the legitimacy of remote care, confidentiality and protection of personal data, and equity in access to care. In fact, the use of digital tools essentially corresponds to a transfer from the traditional consultation model to teleconsultation: it makes less use of artificial intelligence, for example. Thus, COVID-19 questions the way in which the organization of care integrates the possibilities offered by digital technology, specifically in order to promote the autonomy and empowerment of users of mental health services" (Kane, Gourret Baumgart, Fond-Harmant, et al., 2022).
3-2 Digital opportunities and challenges
This fieldwork and investigation led the researchers to conduct a systematic literature review. Its objective was to study the evolution of digital uses during the COVID-19 pandemic.
"Conducted in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, the MEDLINE (i.e. PubMed) and Cairn databases were searched, as well as a specialized mental health platform, Ascodocpsy. A total of 558 articles were selected for 2020. After applying inclusion and exclusion criteria, first on titles and abstracts, and then on full texts, 61 articles were included.
The literature review revealed a heterogeneous integration of digital technologies, not only across countries, contexts, and local regulations but also across care modalities. Despite these variations, the use of videoconferencing has grown considerably, affecting working conditions and therapeutic relationships. For many psychiatric and mental health professionals, the pandemic has been an opportunity to strengthen their experience with telecare and thus better understand the possibilities and limitations of these digital technologies".
Recommendations...
Documenting the experience of these professionals in the face of the COVID-19 health crisis and the suffering it has caused, has allowed the Psy-Gipoc research team to formulate recommendations in favor of the occupational health of these professionals (Kane, Gourret Baumgart, El-Hage, et al., 2022).
It is important to promote well-being at work and to prevent burnout and psychological distress among these professionals.
As the relational dimension is central to the care of people affected by mental disorders, it is essential to preserve the psychic availability of these professionals, which can be impaired when their own mental health is affected in the context of crisis.
It would be appropriate to develop, in addition to the psychological support systems already available to them, devices allowing them to decompress and recharge their batteries. This could involve the implementation of landscaped and equipped spaces so that each professional who feels the need can take time for himself. Because of the importance of sociability between colleagues, highlighted by the research, the establishment of spaces dedicated to sharing conviviality time, promoting the sharing of experiences and mutual assistance between colleagues, can be recommended. It is important that the professionals concerned are involved in the design and implementation of these devices.
In addition, it also seems relevant to recommend:
The accompaniment of psychiatric professionals in their process of appropriation of digital tools for professional purposes.
The implementation of awareness programs on the ethical uses of digital devices that can be used in professional practice in psychiatry and mental health to promote reflexivity on practices and the search for optimal local solutions.
It also seems appropriate to add to the content of initial and continuing training a module on the ethical uses of digital devices in the context of remote care and follow-up in psychiatry and mental health.
Lessons learned and limitations
It is clear that in the 23 countries of the PSY-Gipoc study, organizational complexity has paralyzed decisions and the ability to implement them during the pandemic. In these contexts of uncertain situations, the usual modes of organization and decisions could not be maintained and new work organizations emerged with varying degrees of success.
From the point of view of Public Health and crisis management by decision-makers and politicians, the complexity of situations has been unprecedented during the pandemic: multiplicities of structures, actors... The biomedical and epidemiological dimensions were privileged in the emergency to the detriment of an interdisciplinary approach... The psychiatry and mental health sector has remained the forgotten one, the poor relation... The medical world has expressed its concern about the complications of COVID and the collateral effects of the pandemic, such as the impact on mental health, especially among young people, the most precarious people, the great fatigue and burnout of healthcare staff, a source of absenteeism and resignations (Henrard et al., 2021).
Given the funding and limited duration of the project, Psy-Gipoc was unable to work on these important issues despite proposing "digital methods and tools to improve the well-being of mental health professionals at work and the quality of services offered in times of crisis and post-crisis" (L. Fond-Harmant et al., 2021). These digital tools were initially intended to prevent psychological suffering and its consequences, while accompanying staff and targeting their signs of ill-being. Our project was to help professionals build the conditions for satisfactory operational work, during crises and post-crisis, by adapted organizational methods. It aimed to contribute to the co-construction of an international organization and a monitoring system that take into account psychiatric health professionals as major resources to fight the COVID-19 pandemic. It seemed to us that it would be possible to develop effective crisis preparedness and anticipation processes by minimizing psychosocial risks (L. Fond-Harmant et al., 2021). However, the one-year funding of our project did not allow us to achieve these goals.
In France, the High Authority for Health, HAS, in its prospective analysis report on public expertise in health in crisis situations, insists on the need for multidisciplinary expertise integrating experiential knowledge. It points to the fact that research in the humanities and social sciences, while it has been active, has not been sufficiently integrated at the same time as knowledge of experience from the field of actors: professionals and users (HAS, 2023). The multidisciplinary research team of the Psy-Gipoc project has contributed well to informing public decisions. It has made known the ascent and descent of information from and to the ground by communicating at international congresses and publishing its results of work...
From a socio-anthropological point of view (link with multidisciplinarity), we wonder how to apprehend this complexity. Admittedly, on the one hand, research should be anchored in the paradigm of complexity sciences. The latter makes multidisciplinarity necessary. It invites an epistemological posture of conjunction where social phenomena are considered from the angle of their systemic relations. It makes way for the "ET" against the simplifications of the "OR". On the other hand, the survey mobilizes many concepts and quasi-concepts. This mobilization is necessary to designate social phenomena and to agree on them. At the same time, they constitute theoretical tests. Beyond questions of ideology, which should not be dismissed for the cause, the project is an opportunity to test concepts and then propose them as an analytical framework for professionals, users, and institutions. These concepts often form the basis of our analytical and evaluation frameworks. Should we think of the use of digital technology in terms of resilience? What about an analysis based on the concepts of repair and recovery? Have not digital tools become, by their actions, the discreet organizers of reality and everyday life? (Bennett, 2004): Dealing with uncertainty, certainly, but uncertainty is now an analytical concept in the humanities (Barthe et al., 2014; Becker, 2013). According to Dousset's anthropology of uncertainty (Dousset, 2019; Fond-Harmant et al., 2022; Fond-Harmant et al., 2023). Experts, building expertise, Paris 1690-1790, was the uncertainty related to the crisis existential because professionals and organizations had no "precedent" to refer to to deal with? Has it been systemic in calling into question collective modes of judgment? Does it hold both?
As a response to our shortcomings...
To bridge the gap between the project's aims and achievements in one year of fieldwork and analysis, the research team initiated new partnerships with consortium colleagues for the development of 4 new research projects, in continuity, of Psy-Gipoc, in particular for European funding research: COST, Interreg North-West and Erasmus +. Two projects are underway and the other two are awaiting funding agreements.
Table 2 (Appendix 1) presents a summary of the program of 4 ongoing and pending projects, as a response to our limitations and shortcomings. These projects and their lines of research as an extension of Psy-Gipoc work fill our gaps. Table 2 shows the main thematic axes, the partners, the target audiences, the types of partnership, and funding. These projects are extensions of the issues raised in our work. They take into account the significant gaps and difficulties pointed out by professionals in the field of psychiatry during the Covid period. They are all oriented towards the use of digital tools because, concomitantly with the health crisis and the development of remote work, European policies have developed legal and infrastructure development community frameworks (Mitchell, 2016; OMS, 2021). European digitalisation policies, within Community frameworks, have set objectives for infrastructure development but also connectivity, digital transformation of the economy, intensification of digital human capital, and increased governance (security/ trust/transparency) of digital ecosystems (Commission Européenne, 2022; DESI, 2022).
Table 2.
Summary of the program of ongoing and pending projects in the continuity of Psy-Gipoc work
| Projects | IT 4 Anxiety | DLIS | Let IT Care | EE-Mental Health : European Expertise, Public Policies and Practices |
|---|---|---|---|---|
| Main lines of research | Creation and evaluation of digital tools to combat anxiety | Dematerialization of society and transformation of social work Social inequality, literacy | Digital tools and wellbeing at work for health professionals (psychiatry) and social support |
|
|
Partner Disciplines |
Digital, Psychiatrists, social sciences, training, education | Social Work Engineering, Social sciences and humanities, training, teaching | Digital technology, Social sciences and humanities, Psychiatry, training, teaching. | Clinical medicine, Psychiatry, Sociologie, Psychology Economics and business Health Sciences , Digital engineering |
| Profiles of partner structures | Start Ups, Universities, Psychiatric Hospitals Higher Education | Institutes of Social Work, Universities Research Laboratory, Social Work Associations | Start Ups, Universities: Research Laboratory, Psychiatric Hospitals | ated Organisations ,Private Non-Profit without market revenues, NGO,Government/ Intergovernmental Organisations except Higher Education Standards Organisation |
| ____________ | ____________ | ____________ | ____________ | ____________ |
| Pays partenaires | Belgium, France, Luxembourg, Ireland, Germany | Belgique, France, Luxembourg, Greece, Roumanie | Belgium, France, Luxembourg, Ireland | Belgium , Croatia , France , Germany , Greece , Italy , Luxembourg , Poland, Portugal , Romania , Spain , Turkey |
| Target audience | Users of psychiatry | Users of psychiatry and recipients of social benefits | Health professionals (psychiatry + mental health) and professionals in the social sector | Psychiatric users and professionals |
| Status of the project | Ongoing project | Ongoing project | Awaiting validation for funding | Awaiting validation for funding |
| Type of European fund | Interreg Nord-Ouest | Erasmus + | Interreg Nord-Ouest | COST Association |
| Project start and end years | 2019-2023 | 2021-2024 | 2024-2028 | 2024-2028 |
The Psy-Gipoc project has observed, analyzed, and proposed courses of action in the context of a health crisis long unprecedented in Western countries. The health crisis has had effects in relation to fragile economic, social, and environmental contexts. Adhoc arrangements, professional and institutional tinkering, pragmatism, "save who can" and heroism in the face of the crisis should be put into perspective with a reflection on the capacity of our social organizations to face crises, to survive them, to repair themselves and to prepare themselves. Issues are emerging, such as the resilience of structures and infrastructures (Centemeri et al., 2021).
Discussion: digital health... Research projects focused on
Digital health is defined as "the combined use of the internet and information technology for clinical, educational, administrative purposes both locally and remotely" (Barthe et al., 2014). It includes a broad spectrum that includes:
e-health: Health Information System (IS) Digital hospital, clinical IS, electronic medical records, vigilance IS, orientation,
telehealth: e-health service, information, training, digital social networks, serious games, etc.
robotics,
M-health: connected objects, sensors, smart textiles...
telemedicine: teleconsultation, remote home automation monitoring, connected home, home support technologies, etc.,
Artificial Intelligence
Like the major economic powers, such as the USA and China, digital Europe is preparing with major projects for 2030, based on the dematerialisation of administrative society, already developed e-commerce and digital health... Health represents both an issue of social rights and a vast market to conquer for the actors of the digital economy. If the COVID-19 pandemic has allowed the emergence of new practices, somewhat improvised, to face the new territories of social distance imposed by the health, the Psy-Gipoc research project has shown their limits, not to mention all the ethical, security, data protection, and data management issues on which the vigilance of politicians and researchers must focus.
The discourse of Europe's policies focuses on its ability to transform and embrace the digital and ecological transitions. This requires bold investments in both the public and private sectors. This is why research funds prioritize these lines of work. Digital Europe is moving forward, and it is our responsibility as researchers to make it capable of: lutter contre les inégalités sociales de santé et les fractures numériques (accès, matériel et compétences techniques) (Brotocorne & Marien, 2022) provide a protective framework for human rights, work towards destigmatization in mental health (OMS, 2021),
participate in the creation of healthy working conditions for the physical and mental health of mental health professionals and psychiatry.
involve audiences in debates and decisions about the digitalisation of health.
A forward-looking approach to European digitalisation policies
The Digital Europe Agenda (2021-2027), the European Pillar of Social Rights and the 2030 Action Plan, the 2030 Digital Compass with the deployment of quantum computers are all signs of political will for European digitalisation. Since 2014, a European evaluation programme (DESI, Digital Economy and society Index -2022) has been taking stock of progress in Europe. This index integrates 4 interrelated dimensions and 33 individual indicators (Mitchell, 2016): Human capital (digital skills and specialization), Connectivity (broadband coverage and infrastructure), Integration of digital technologies (private sectors: digital intensity: e-commerce, SMEs, industries...) digital public services (governance). On all these criteria and indicators, there are strong numerical inequalities between Community states, and strong disparities between Northern Europe and South and East with impacts on the development of digital health (Barthe et al., 2014).
For its part, "The Geneva Charter for Well-being", (OMS, 2021), defends a positive vision of mental health by advocating for the creation of "healthy environments" based on the Ottawa Charter of 1986 and "equitable access to digital technology and the exploitation of its full potential for human flourishing and well-being". It advocates "a society that promotes well-being" that "evaluates and neutralizes the harmful effects of digital tools and their attacks on the power to act... » (Fond-Harmant et al., 2023).
In addition, the issue of securing and protecting medical data and respecting medical confidentiality are of concomitant and paramount importance. All these elements are indicators of a world of health that is transforming and accelerating its transformation since the COVID-19 health crisis. Digital technologies offer a number of opportunities for monitoring, preventing and controlling people's health.
Advances in digital technologies for public health surveillance can help make analysis faster and increase monitoring capabilities, while new data mining techniques and artificial intelligence can help detect the warning signs of mental health disorders (stress, anxiety, addiction, burnout, etc.). exhaustion...). Perhaps we will be able to develop complex models for public health, aggregating a variety of data, to support policy decisions? Certainly, we will have to take the time to evaluate in concert, in a pluralistic and democratic way, the consequences of this option.
Our research programs (table 2), as an extension of the work of Psy-Gipoc, aim to create a multidisciplinary pan-European network composed of computer engineers, researchers in social and medical sciences, clinical scientists, professionals in psychiatry and the psychosocial world and user representatives. The aim will be to advance work on the study of virtuous and harmonious conditions for the development of e-mental health for users with psychological disorders in Europe. It will create an internationally validated ethical framework for standardised recommendations to address social inequalities in health and develop e-mental health literacy.
The general aim of the proposed projects is to make a public health of e-mental health and psychiatry that produces a science capable of contributing to describing and guiding the social uses of e-mental health. Producing concepts, theories, methods and analytical tools is useful in order to determine the economic scientific technical causes that positively accelerate the evolution of e-mental health in Europe. Our programmes consist of mobilising young Ph.D. students and young European professionals in a collective of international experts on the multidisciplinary dimensions of e-mental health (Brotocorne & Marien, 2022).
As an extension of the Psy-Gipoc project, our research program is structured in 4 main areas of expertise:
1-E-mental health Social inequalities in health, literacy, and ethics of use,
2-E-mental health, indirect impacts, expected benefits/users, professionals and researchers in public health,
3-E-mental health and training of actors: clinical professionals, professionals in the psychosocial sector, and research training of PhD students,
4- E-mental health and democratic evaluation of the use of digital tools.
In the context of the digitization of society as a whole with the dematerialization of many social and medical services, understanding emerging digital technologies could help improve situational awareness in the ambulatory psychiatry sector: that of care networks in living environments.
It would also shed light on the coordination of the monitoring of mental disorders affecting professionals, in response to individual and/or collective crisis situations in the work organizations of this sector of activity, which has been particularly suffering for more than a decade.
At the same time, these same technologies are profoundly modifying the ecosystems of care and support work in psychiatry, confronting professionals with new practices and new forms of work organization that generate insecurity, stress, and value conflicts.
In Europe, the COVID-19 health crisis has highlighted that the professions of health, psychiatry, and mental health are in great difficulty: lack of resources, crisis of vocations. The pandemic has exacerbated this situation. In a political context where mental health services are more community-based, the demand for quality and the regulation of the system requires a rethinking of the forward-looking management of jobs and skills and the improvement of working conditions, and the quality of human resources in the sector.
It is about understanding how to better anticipate the changes that all these mental health specialists are facing, in terms of services offered with new emerging professional practices. The latter increasingly integrates the digital dimension, because modern psychiatry opens its doors to social and community life and promotes the remote for "user and professional" exchanges.
This transforms the lives of patients of course, but also gradually the place and role of medical or social companions: they have to face new work contexts, new places that are not those of the hospital, and that induce new interpersonal relationships. As our work (Absil et al., 2022), these changes are profound and destabilize the professions learned by disrupting the traditional benchmarks acquired throughout the training curriculum and the daily experiential professional life: the links and communications with the hierarchy and with the users of psychiatry are changing with new relational forms, especially with the introduction of mobile phones, the use of Internet network, among professionals and users... Indeed, users are also increasingly using new digital technologies (telephones connected to the Internet, games, electronic applications for everyday life, electronic health records, diagnoses and therapeutic follow-ups, etc.). This is not unrelated to the societal and systemic transformations of our institutional symbols: hospitals, schools, work... However, the research is still in its infancy. The literature review shows that most studies had a small number of participants and more high-quality studies are needed to assess whether the apps have significant benefits for users. But this information gathered allows us to guide the development of future AI mental health studies and applications (Brotocorne & Marien, 2022; Milne-Ives et al., 2022).
The prevention of burnout among mental health professionals, and more broadly of the conditions of well-being at work, is a pillar of the quality of care and support for users of mental health services. It contributes to the resilience of services faced with the increase in unrest in the general population and the difficulties of organizing a collective response in terms of public health.
Since the COVID-19 health crisis, the Pys-Gopic project, and our planned programs shed light on the different priority areas of action for the psychiatry and mental health sector in Europe. It appears necessary to carry out in-depth work, by 2030 on hospital psychiatry and psychiatry outside the walls, the care pathway of the user, digitalization, data management, and the training of professionals to the mutations and technological transitions that are being prepared.
References
- Absil, G., Kane, H., Gourret Beaumgart, J., Deloyer, J., Denis, F., & Fond Harmant, L. (2022). Dispositifs de gestion de la Covid-19 et recomposition des relations professionnelles dans les services de psychiatrie et santé mentale.
- Bandura, A. (2001). Social cognitive theory: an agentic perspective. Annu Rev Psychol, 52, 1-26. 10.1146/annurev.psych.52.1.1 [DOI] [PubMed] [Google Scholar]
- Barthe, Y., Callon, M., & Lascoumes, P. (2014). Agir dans un monde incertain. Essai sur la démocratie technique. Le Seuil. https://www.cairn.info/agir-dans-un-monde-incertain-essai-sur-la-democrat--9782020404327.htm
- Becker, H. S. (2013). How Much Is Enough? Public Culture, 25(3 (71)), 375-386. 10.1215/08992363-2144670 [DOI]
- Bennett, J. (2004). The Force of Things: Steps toward an Ecology of Matter. Political Theory, 32(3), 347-372. http://www.jstor.org/stable/4148158 [Google Scholar]
- Briffault, X. (2017). Singularisations, contextualisations, interconnexions. Quelques grandes évolutions de la recherche en santé mentale et leurs conséquences sur les prises en charge. Perspectives Psy, 56(2), 133-141. 10.1051/ppsy/2017562133 [DOI] [Google Scholar]
- Brotocorne, P., & Marien, I. (2022). Nouveau Baromètre de l’inclusion numérique.
- Centemeri, L., Topçu, S., & Burgess, J. P. (2021). Rethinking post-disaster recovery: Socio-anthropological perspectives on repairing environments. Routledge. [Google Scholar]
- Chanut, V., Chomienne, H., & Desmarais, C. (2015). Pratiques valorielles et management public. Revue Internationale des Sciences Administratives, 81(2), 235-242. 10.3917/risa.812.0235 [DOI] [Google Scholar]
- Commission Européenne. (2022). L’indice de l’économie et de la société numériques (DESI). Façonner l’avenir numérique de l’Europe. https://digital-strategy.ec.europa.eu/fr/policies/desi
- DESI. (2022). Digital Economy ans society Index.
- Dousset, L. (2019). De l’incertitude au risque: un outil heuristique. Moussons. Recherche en sciences humaines sur l’Asie du Sud-Est(34), 21-48.
- Fond-Harmant, L., Denis, F., Deloyer, J., Lebas, M.-C., & Thome, J. (2021). Psychiatrie et lutte contre la COVID-19 : gestion de l’impact psychologique et organisation de crise et post-crise. In Maia M., Réal B., & Louis-Paul W. (Eds.), Penser la Covid-19, et penser le monde. Réflexion critique sur les effets de la pandémie du printemps 2020. JFD Editeur. [Google Scholar]
- Fond-Harmant, L., Kane, H., Gourret Baumgart, J., Rusch, E., Breton, H., El-Hage, W., Deloyer, J., Lebas, M. C., Marazziti, D., Thome, J., & Denis, F. (2021). International professional practices in mental health, organization of psychiatric care, and COVID-19: A survey protocol. PLOS ONE, 16(12), e0261818. 10.1371/journal.pone.0261818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fond-Harmant, L., Philippart, A., Megherbi, S., & Pereaux, P. (2022). Numérisation de la société : contextes européens et défis pour le travail social.
- Fond-Harmant, L., Philippart, A., Megherbi, S., Pereaux, P., & Gavrila-Ardelean, M. (2023). Digitalization of the European Society: Challenges for Social Work. Social Work Review/ Revista de Asistenta Sociala(1).
- Fond-Harmant, L., & Tal Dia, A. (2008). Public health and the North-South transfer of skills: conditions for an intercultural approach. Santé Publique, 20(1), 59-67. 10.3917/spub.081.0059 (Santé publique et transfert de compétences Nord-Sud : les conditions d'une approche interculturelle.) [DOI] [PubMed] [Google Scholar]
- Gourret Baumgart, J., Kane, H., Denis, F., & Fond-Harmant, L. (2022). Travailler en contexte d’incertitudes : l’expérience des professionnels de la santé mentale face à la COVID-19. Santé Publique, 34(HS1), 9e-9e. 10.3917/HASspub.220.0009eHAS (2023). L’expertise publique en Santé en situation de crise. Rapport d’analyse prospective 2022. https://www.has-sante.fr/jcms/p_3410771/fr/l-expertise-publique-en-sante-en-situation-de-crise-rapport-d-analyse-prospective-202236102096 [DOI] [Google Scholar]
- Henrard, J.-C., Arborio, S., Fond-Harmant, L., & Kane, H. (2021). Santé publique : les réponses aux défis de la pandémie de la COVID-19. Santé Publique, 33(6), 785-788. 10.3917/spub.216.0785 [DOI] [PubMed] [Google Scholar]
- Kane, H., Gourret Baumgart, J., El-Hage, W., Deloyer, J., Maes, C., Lebas, M. C., Marazziti, D., Thome, J., Fond-Harmant, L., & Denis, F. (2022). Opportunities and Challenges for Professionals in Psychiatry and Mental Health Care Using Digital Technologies During the COVID-19 Pandemic: Systematic Review. JMIR Hum Factors, 9(1), e30359. 10.2196/30359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane, H., Gourret Baumgart, J., Fond-Harmant, L., Absil, G., Deloyer, J., El-Hage, W., Maes, C., & Denis, F. (2020). L’expérience professionnelle de soins entravés par les mesures de distanciation physique en psychiatrie Les sciences sociales face à la pandémie de la covid-19. État des connaissances et propositions d’actions,
- Kane, H., Gourret Baumgart, J., Fond-Harmant, L., & Denis, F. (2022). Usages des outils numériques en psychiatrie et santé mentale face à la COVID-19 en Europe. Santé Publique, 34(HS1), 2c-2c. 10.3917/spub.220.0002c [DOI] [Google Scholar]
- Milne-Ives, M., Selby, E., Inkster, B., Lam, C., & Meinert, E. (2022). Artificial intelligence and machine learning in mobile apps for mental health: A scoping review. PLOS Digital Health, 1(8), e0000079. 10.1371/journal.pdig.0000079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell, P. (2016). E-santé : la médecine à l’ère du numérique. Science et santé(29).
- OMS. (2021). Charte de Genève pour le bien-être.
- Thome, J., Deloyer, J., Coogan, A. N., Bailey-Rodriguez, D., da Cruz, E. S. O. A. B., Faltraco, F., Grima, C., Gudjonsson, S. O., Hanon, C., Hollý, M., Joosten, J., Karlsson, I., Kelemen, G., Korman, M., Krysta, K., Lichterman, B., Loganovsky, K., Marazziti, D., Maraitou, M., Fond-Harmant . . ., L. (2021). The impact of the early phase of the COVID-19 pandemic on mental-health services in Europe. World J Biol Psychiatry, 22(7), 516-525. 10.1080/15622975.2020.1844290 [DOI] [PubMed] [Google Scholar]