Abstract
Background.
Accumulation of susceptible children whose caregivers refuse to accept oral poliovirus vaccine (OPV) contributes to the spread of poliovirus in Nigeria.
Methods.
During and immediately following the OPV campaign in October 2012, polio eradication partners conducted a study among households in which the vaccine was refused, using semistructured questionnaires. The selected study districts had a history of persistent OPV refusals in previous campaigns.
Results.
Polio risk perception was low among study participants. The majority (59%) of participants believed that vaccination was either not necessary or would not be helpful, and 30% thought it might be harmful. Religious beliefs were an important driver in the way people understood disease. Fifty-two percent of 48 respondents reported that illnesses were due to God’s will and/or destiny and that only God could protect them against illnesses. Only a minority (14%) of respondents indicated that polio was a significant problem in their community.
Conclusions.
Caregivers refuse OPV largely because of poor polio risk perception and religious beliefs. Communication strategies should, therefore, aim to increase awareness of polio as a real health threat and educate communities about the safety of the vaccine. In addition, polio eradication partners should collaborate with other agencies and ministries to improve total primary healthcare packages to address identified unmet health and social needs.
Keywords: assessment, OPV, oral polio vaccine, refusals, noncompliance
Nigeria is one of only 3 countries globally that is yet to interrupt endemic circulation of wild poliovirus (WPV). Polio cases in Nigeria increased steadily from 2009 to 2012. In 2012, Nigeria accounted for 50% of total global polio cases [1] and contributed 95% of cases in the World Health Organization (WHO) African Region [2]. In 2013 ( provisionally as of 11 March 2014), Nigeria contributed 13.1% of the 406 global case burden and 33.1% of cases from polio-endemic countries [3]. Ongoing WPV transmission in northern Nigeria is the main source of WPV infections elsewhere in the country and in neighboring countries [4]. The current strategy to achieve global polio eradication requires the vaccination of every eligible child in all parts of the world [5]. In polio-endemic countries such as Nigeria, supplementary immunization activities (SIAs) for the house-to-house delivery of oral poliovirus vaccine (OPV) remain the major strategy to deliver OPV to all eligible children [4, 5]. Because multiple doses of OPV are needed to develop adequate immunity in countries in which polio is highly endemic, every child <5 years of age has to be reached with OPV during each SIA, irrespective of immunization history. SIAs are intended to complement, not replace, routine immunization against polio [5–7].
OPV refusals during SIAs are a major impediment to polio eradication efforts. A June 2012 study in the Democratic Republic of the Congo showed that, of the children who did not receive OPV during SIAs in the first quarter of 2012, 46% were missed because of vaccine refusal by caregivers [8]. Similarly, a retrospective analysis of the 2012 polio case investigation forms in Nigeria revealed that vaccination refusals were a major contributor to the continued spread of poliovirus [1]. Overt refusals accounted for 24% of missed children in high-risk areas of Nigeria, and more than one third of polio case patients were from families that refused OPV. Furthermore, in the northern states of Sokoto and Kano, more than two thirds of polio cases were from households in which OPV was refused (hereafter, “refusal households”). Similarly, 57% of all polio cases in 2012 were reported from 3 states with the highest rate of refusals (Sokoto, Kano, and Katsina) [9]. As was seen previously, if not adequately addressed, a rise in polio cases in states with high rates of OPV refusal has the potential to put the polio-free status of surrounding African countries at risk [10].
OPV refusal in northern Nigeria became pronounced in 2003, when community leaders ( predominantly Muslim clerics) rejected the OPV [11]. Five northern states in Nigeria banned the administration of the polio vaccine, alleging that the vaccine was a Western plot to sterilize women in Nigeria, contained human immunodeficiency virus, and was contaminated with chemicals. The ban, which was supported by the Sharia Council of Nigeria, forced the WHO to cancel several planned national polio SIAs in the affected states. The 1996 Pfizer-Meningitis study in Nigeria that led to a class action lawsuit from 20 participants was implicated as a reason for the rejection, mistrust, and subsequent ban. Concerted dialogue with Muslim leaders later abated the crisis, which lasted for 16 months. By the end of the ban, polio cases had risen from <50 in 2000 to >250 in 2003 [11]. By 2013, the virus had been exported from Nigeria to 25 previously polio-free countries [12, 13]. A residual effect of this experience is that a proportion of the northern Muslim population has yet to approve delivery of OPV to their children.
Recognizing the persistent problem of OPV refusals in northern Nigeria, the 24th Polio Expert Review Committee, at its September 2012 meeting, recommended that social research be conducted to better understand the reasons for OPV refusal, to provide well-informed and tailored solutions to counter OPV refusals [14]. We conducted an assessment of the extent and reasons for OPV refusal in northern Nigeria to assist the Nigeria polio eradication program in developing new tailored communication and programmatic strategies to address OPV refusals in specific communities.
METHODS
Study Period
The OPV refusal study was conducted during the polio SIAs that were conducted during 6–12 October 2012.
Study Sites
The study was conducted in 9 local government areas (LGAs), equivalent to districts, in the Northwest geopolitical zone of Nigeria (comprising Kaduna, Kano, Katsina, Jigawa, and Zamfara states). Analysis of data for the January–August 2012 OPV SIAs had shown that these 5 study states contributed the highest OPV refusal burden in 2012. In addition, although these states make up only 20.6% of the 140, 420, 142 individuals living in Nigeria, they contributed 75 (74%) of 102 WPV cases in Nigeria at the time of our study, with 25 cases from Katsina, 24 from Kano, 13 from Kaduna, 7 from Jigawa, and 6 from Zamfara. The selected states predominantly speak Hausa or Fulani, and Islam is the major religion.
Study Design
We conducted a cross-sectional study using interviewer-administered semistructured questionnaires. Interviewers were trained on the data tools prior to the study. We purposely selected 2 LGAs (1 rural and 1 urban) at high risk for polio from each of the 5 preselected states. However, only one LGA, Batsari (a rural LGA), participated in the study in Katsina. The urban LGA, Katsina LGA, selected for the study did not participate, because of its inability to meet the polio dashboard indicators necessitating the postponement of SIA in the LGA by 2 weeks. Data collection was performed over a 5-day period, including the 4 implementation days of the polio SIA and the mop-up day.
We selected wards and settlements with the highest reported numbers of refusals during the ongoing campaign. These were identified from 2 sources: the daily campaign tally sheets and the reports of immunization staff in the LGAs (ie, ward focal persons, field volunteers, vaccination team supervisors, and monitors) obtained at evening review meetings. From the selected wards and settlements, we generated a list of refusal households. These households were visited on the following campaign day, and caregivers were requested to participate in the study. Consenting households were recruited consecutively on the basis of the previously generated list. Using the standard questionnaire, trained interviewers collected data from persons responsible for health decisions in refusal households. Interviews were most often conducted at the entrance to the respondents’ homes. Interviewers determined whether participants/households were either first-time or second-time refusers, based on history of previous attempts by local campaign supervisors to resolve noncompliance. No economic incentive was provided to respondents. Most of the interviews were conducted in Hausa because most interviewers were fluent speakers of Hausa. On average, the interviews lasted 45 minutes per respondent.
Data Management and Analysis
The semistructured questionnaires were administered in Hausa by trained interviewers. Questionnaire answers were then translated to English and entered into EpiInfo, version 3.4.5. Qualitative analysis was conducted on the responses to open-ended questions. Frequencies were calculated from categorical responses and variables (eg, yes/no answers, education level, and race). In addition, after completing the qualitative analysis of responses to open-ended questions, the frequency of themes was quantified for most questions (eg, perceived polio threat, reasons for OPV refusal, and perception of campaigns and vaccination teams). Prior to analyzing the qualitative data, a coding list and structure was developed using the framework of themes and topics that were central to the objective of the study as described in the study protocol. The analysis used open coding [15] and was conducted separately by 2 investigators in the analysis team. The assigned codes from the 2 investigators were compared for consistency. The codes were then applied to responses from the questionnaire. To reflect the nuances of the data, the coding list and structure were modified in an iterative process after consensus discussions by the analysis team. Excel 2010 (Microsoft) was used to tabulate and calculate frequencies for each response and to create graphs from selected questionnaire data.
Ethical Considerations
This study was assessed as a nonresearch public health activity. Prior to conducting interviews, all participants provided verbal consent. Participants received information about the project and its procedures and benefits and were assured that their responses would be confidential. Participants were aware that their participation was voluntary and would not affect their future access to healthcare and other social services.
RESULTS
A total of 148 respondents participated in the refusal study in 9 high-risk LGAs, with 13–22 respondents per LGA (Table 1). Most of the refusal households that were invited to participate accepted to be interviewed; however, the precise participation rate was unrecorded.
Table 1.
Distribution of 148 Participants in a Study of Oral Poliovirus Vaccine Refusal in Northern Nigeria, by Selected Local Government Area (LGA) and State—October 2012
| State, LGA | Respondents, No. (%) |
|---|---|
| Jigawa | |
| Birnin Kudu | 16 (10.8) |
| Dutse | 18 (12.2) |
| Kaduna | |
| Igabi | 14 (9.5) |
| Birnin Gwari | 18 (12.2) |
| Kano | |
| Bebegi | 16 (10.8) |
| Sumaila | 16 (10.8) |
| Katsina | |
| Batsari | 15 (10.1) |
| Zamfara | |
| Bugundu | 13 (8.8) |
| Gusau | 22 (14.9) |
Demographic Characteristics
Of the 148 study participants, 82% were male (Table 2). The median age was 39.5 years (range, 17–75 years). All respondents were Muslim. Tribal distributions were 86% Hausa and 9% Fulani; other tribes composed 5%. The level of education was low, with 38% indicating they only had a Qur’anic education and 34% having no formal education; only 28% had a primary education level or higher.
Table 2.
Demographic Characteristics of 148 Participants in a Study of Oral Poliovirus Vaccine Refusal in Northern Nigeria—October 2012
| Characteristic | Value |
|---|---|
| Age, y, median (range) | 39.5 (17–75) |
| Sex | |
| Male | 122 (82.4) |
| Female | 26 (17.6) |
| Tribe | |
| Hausa | 123 (83.1) |
| Fulani | 13 (8.8) |
| Other | 12 (8.1) |
| Religion, Islam | 148 (100) |
| Educational level | |
| None | 51 (34.5) |
| Qur’anic only | 56 (37.8) |
| Primary or higher | 41 (27.7) |
Data are no. (%) of respondents, unless otherwise indicated.
Polio Risk Perception and Understanding of Polio Among Refusal Households
Of the 148 respondents, 21 (14%) agreed that polio was a significant health threat in their community, 39 (26%) thought their child was at risk, and only 50 (34%) were willing to have their children vaccinated. While malaria was identified by most respondents (85%) as one of the most significant health problems in their community, polio was not perceived as a priority health concern. Religious beliefs were an important driver in the way people understood disease. When asked to comment about polio risks, 25 (52%) of 48 respondents reported that illnesses were due to God’s will and/or destiny (ie, the risk was out of their hands “because everything good or bad comes from God”). When asked whether they knew how to protect themselves from polio, “God and prayers” was mentioned by 40 (46%) of 86 respondents, whereas vaccination was mentioned by less than one quarter (Figure 2). The majority of participants (87 [59%] of 148) believed that vaccination was either not necessary or would not be helpful.
Figure 2.
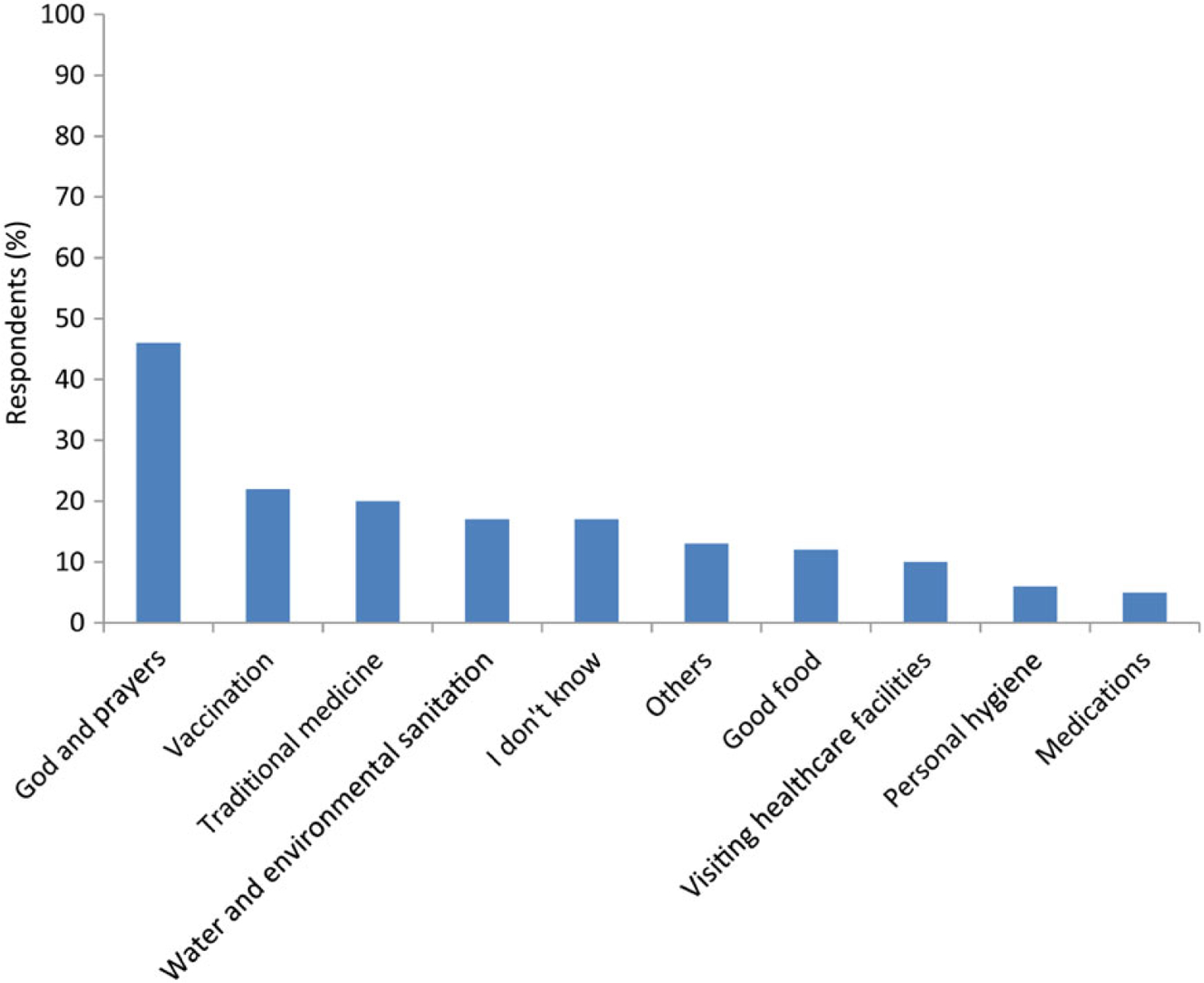
Perception of 146 questionnaire respondents on how to protect their children from polio—October 2012. Respondents could give >1 answer.
Reasons for OPV Refusal
The reasons most frequently mentioned for refusing vaccination during the current campaign were the belief that vaccination was unnecessary (49%; Figure 1), as respondents often believed that polio infection was an act of God; the perception that the vaccine was not helpful (40%); and the lack of trust in government (35%). Other reasons frequently mentioned included the belief that the government should address other neglected health and social needs (33%) and concerns regarding the safety of the vaccine (30%). Of those who were concerned about vaccine safety, more than half mentioned they were concerned that the polio vaccine might cause infertility in their children.
Figure 1.
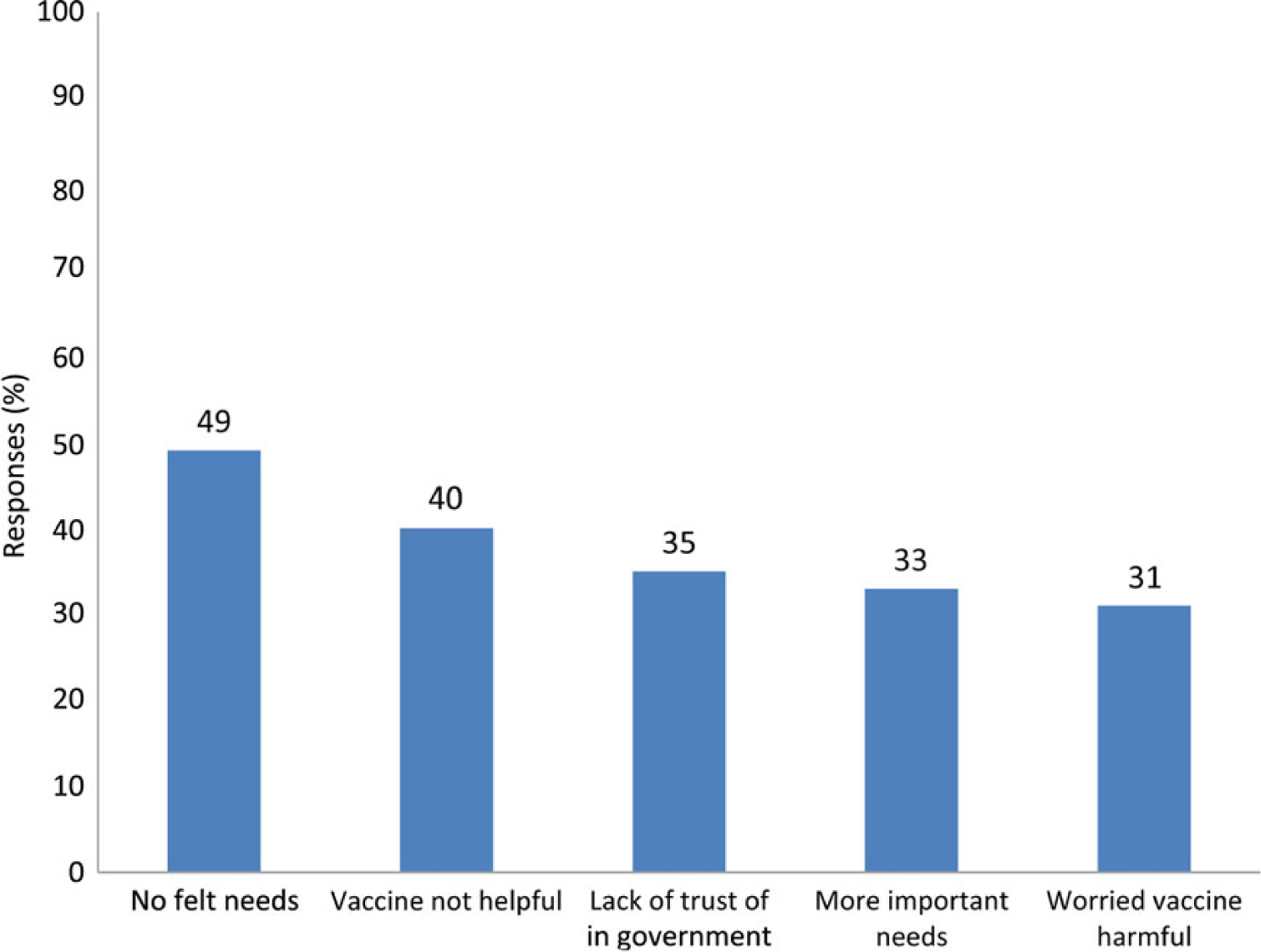
Major reasons given by 148 questionnaire respondents for refusing oral poliovirus vaccine during the October 2012 campaign. Respondents could give >1 answer.
Influencers and Motivation
When asked about possible ways that respondents could be persuaded to accept polio vaccine, about one third (of 112 respondents) stated that nothing or nobody could persuade them. Providing education/increasing awareness and government help with other health and social priorities (“If government provides other drugs free and take care of our welfare”) were the other most frequent responses. About one third of respondents indicated that they felt pressure to accept the vaccine and that this pressure was mostly from the government.
In terms of influencers, about half of respondents had received some advice about receiving polio vaccine; these were largely positive messages and usually came from community leaders. The female participants expressed concern that their husbands were very influential in the decision on whether their children could receive the vaccine.
Community Perception of OPV Campaigns and Vaccination Teams
The reported attitude of refusal households revealed that only 36% and 48% of participants had a positive impression of polio campaigns and the vaccination teams, respectively. When asked to make suggestions to make polio campaigns more successful and improve their impression of the vaccination teams, the most common category of response was “no comment/I don’t know.” The second and third most common suggestions to make polio campaigns more successful were to educate the community/increase awareness and for the government to address other healthcare and social needs. The most common suggestion to improve the perception of polio teams was for the polio program to enhance team attitude/team selection.
DISCUSSION
Our assessment of beliefs and attitudes of refusal households showed that caregivers refused polio vaccine for their children mainly because of a low risk perception of the disease, religious beliefs, and distrust of government, in part because perceived health and social priorities were not being addressed. Respondents frequently believed that the vaccine was unnecessary, unhelpful, and might be harmful. Religious belief was an important driver of how people understood health and disease. This religious perception of OPV by some participants may be related to the erroneous teachings by certain religious sects in northern Nigeria, which led to the total suspension of polio campaigns in some northern Nigerian states in 2003.
The results of this study agree with findings in a similar study conducted in 5 provinces of the Democratic Republic of the Congo in October 2011 [8]. In our study, most respondents indicated that they were much more concerned about other health priorities affecting their community and less worried about polio. Respondents were more concerned about malaria, which they see every day in their communities, and wondered about the emphasis on polio rather than malaria. Some suggested that if more education was provide, awareness was increased, and the government paid more attention to improving their lives or providing better healthcare when they need it, then they would be more likely to accept the vaccine. The unfavorable or indifferent view of polio campaigns and vaccination teams is probably attributable to their OPV refusal stance. In general, the respondents were not concerned about improving the campaigns/campaign teams, nor did they suggest ways of making it better.
These data suggest that more education at the community and household levels needs to be conducted regarding OPV. We recommend increased dialogue with community and religious leaders to increase their engagement with OPV campaigns and to enhance local campaign ownership and vaccine acceptance. Increasing dialogue with the community would also help the government and polio eradication partners to better understand the issues about which people are most concerned. Furthermore, the national polio program should consider collaborating with other health programs and services (eg, vitamin A supplementation, other vaccination campaigns, malaria programs, nutritional supplementation programs) to provide health packages that have been identified as valued by the communities.
Efforts should be made by government and Global Polio Eradication Initiative (GPEI) partners to increase awareness of polio as a real health threat and improve perception of the vaccine. This could be done by engaging religious leaders to provide precampaign and ongoing information through communications in a religious context. Because most household decision makers are men, more education on the importance of the polio vaccine should specifically target men, both in content and method of delivery. Where possible, the polio program should also consider engaging the Federation of Muslim Women Association of Nigeria and religious leaders to be part of teams that visit refusal households, as this has been a successful strategy in certain areas. Another option that could be explored is to involve the Association of Polio Survivors (APS) during precampaign information sessions. The APS could also be integrated into teams that revisit refusal households. A strategy to increase community engagement and ownership is to have community members fully involved in campaign activities (eg, by becoming members of planning committees, social mobilization committees, and vaccination teams).
CONCLUSION
Caregivers refuse OPV largely because of poor polio risk perception, religious beliefs, and distrust of government programs and intentions. Communication strategies should, therefore, aim to increase awareness of polio as a real health threat and educate communities about the safety of the vaccine. In addition, polio eradication partners should collaborate with other agencies and ministries to improve total primary healthcare packages to address identified unmet health and social needs.
Since this study was conducted, the data have been presented to the key players at the national level, and the results have been used by the national program and GPEI partners to modify and improve communication and implementation strategies for polio eradication. Although these measures are yielding positive results, more-tailored activities identified during this study should be implemented in the future to get us over the finish line.
Acknowledgments.
Members of the NSTOP OPV refusal study team are as follows: David Newberry, Adamu Sule, Olaniran Alabi, Hassana Ibrahim, Badaru SOS, Salifu Musa, Abdulaziz Mohammed, Saheed Gidado, Milkhail Abubakar, Aisha Sadiq Abubakar, Luka Ibrahim, and Maryam Buba.
We thank all of the participants who agreed to be interviewed for this study; all of the people who contributed to this study, particularly the vaccination staff at the LGAs, wards, and settlements where the interviews were conducted, staff at the WHO Nigeria office, and staff at the United Nations Children’s Fund Nigeria office.
Financial support.
This work was supported by the Centers for Disease Control and Prevention.
Footnotes
Disclaimer. The views expressed are those of the authors and are not the official policy of the Centers for Disease Control and Prevention or the institutions with which the authors are affiliated.
Supplement sponsorship. This article is part of a supplement entitled “The Final Phase of Polio Eradication and Endgame Strategies for the Post-Eradication Era,” which was sponsored by the Centers for Disease Control and Prevention.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Situation analysis–polio situation worldwide: the game changer. UNICEF Quarterly Newsletter on Polio Eradication Initiative in Nigeria, 2012. [Google Scholar]
- 2.Update of poliomyelitis as at 30th November, 2012. Weekly Epidemiology Report Vol 2, no 47. Abuja, Nigeria: NCDC, Federal Ministry of Health, 2012. [Google Scholar]
- 3.GPEI. Wild poliovirus (WPV) cases: case breakdown by country as of 11 March 2014 http://www.polioeradication.org/Dataandmonitoring/Poliothisweek.aspx. Accessed 13 August 2014.
- 4.GPEI. Nigeria http://www.polioeradication.org/Infectedcountries/Nigeria.aspx. Accessed 11 March 2014.
- 5.WHO. 10 facts on polio eradication http://www.who.int/features/factfiles/polio/facts/en/index7.html. Accessed 11 March 2014.
- 6.Global polio emergency action plan 2012–13: getting Nigeria, Pakistan and Afghanistan back on track Geneva: World Health Organization, 2012. http://www.who.int/immunization/sage/meetings/2012/april/Working_draft_Global_PolioEmergencyActionPlan_04_April_v2.pdf. Accessed 10 August 2012. [Google Scholar]
- 7.Supplementary immunization [Internet] Geneva: Global Polio Eradication Initiative, World Health Organization, 2010. http://www.polioeradication.org/Aboutus/Strategy/Supplementaryimmunization.aspx. Accessed 10 August 2012. [Google Scholar]
- 8.GPEI. Root causes of refusals revealed through DR Congo study—examining one of the reasons children are missed during vaccination. Media room new story, 2012. http://www.polioeradication.org/tabid/461/iid/223/Default.aspx. Accessed 7 June 2014. [Google Scholar]
- 9.Update of poliomyelitis as of 25th January 2013. Weekly Epidemiology Report Vol 3, no 3. Abuja, Nigeria: NCDC, Federal Ministry of Health, 2013. [Google Scholar]
- 10.Larson HJ, Smith D, Paterson P, et al. Measuring vaccine confidence: analysis of data obtained by a media surveillance system used to analyse public concerns about vaccines. Lancet Infect Dis 2013; 13:606–13. [DOI] [PubMed] [Google Scholar]
- 11.Davidson M Impacts of vaccine refusal on the global efforts to eradicate polio: the case of Nigeria. Presented at: The Canadian Public Health Conference, Edmonton, Canada, 2012. http://resources.cpha.ca/CPHA/Conf/Data/2012/A12-019e.pdf. Accessed 20 March 2014. [Google Scholar]
- 12.Roberts L The art of eradicating polio. Science 2013; 342:28–35. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Progress toward poliomyelitis eradication–Nigeria, January 2012–September 2013. MMWR Morb Mortal Wkly Rep 2013; 62:1009–13. [PMC free article] [PubMed] [Google Scholar]
- 14.GPEI. 24th Meeting of the Expert Review Committee (ERC) on Polio Eradication and Routine Immunization in Nigeria Abuja, Nigeria. 10–11 September, 2012. http://www.polioeradication.org/Portals/0/Document/Resources/AdvisoryCertification/TAG/24ERCMeeting_Report_2012091011.pdf. Accessed 20 March 2013. [Google Scholar]
- 15.Strauss AL, Corbin JM. Basics of qualitative research: grounded theory procedures and techniques London: Sage Publications, 1990. [Google Scholar]


