Abstract
Objective:
The aim of this study was to assess and compare the clinical, radiological, and functional results of patients treated with FITBONE or PRECICE nails due to deformity and length discrepancy in their lower extremities.
Methods:
This retrospective cohort study included 41 patients with length discrepancy and deformity in their lower extremities, who underwent limb lengthening surgery with either FITBONE (group F) or PRECICE (group P) nails between 2010 and 2020. The mean postoperative follow-up period was 15.95 ± 4.75 months in group F (20 patients) and 20.48 ± 7.57 months in group P (21 patients). Lower extremity mechanical and anatomical axes were measured on x-rays preoperatively and at the end of treatment. Consolidation and distraction indexes were also calculated to assess bone healing. Lower Extremity Functional Scale test was used to evaluate functional outcomes and quality of life.
Results:
Neither of the treatment methods caused deviations in the mechanical axes and femoral distal angles (P > .05). No statistically significant difference in consolidation and distraction indexes was found between the groups (P > .05). Postoperative complications were seen in 3 of the patients in group F and 4 of the patients from group P. There was no significant difference in Lower Extremity Functional Scale scores between groups (P = .425).
Conclusion:
This study has demonstrated that treatment with both the FITBONE and PRECICE nails resulted in improved physical and emotional functional outcomes. Both nails had similar radiographic results, complication rates, high patient compliance, and good cosmesis.
Level of Evidence: Level III, Therapeutic Study.
Keywords: FITBONE, PRECICE, Motorized lengthening nails, Magnetic lengthening nails, Length discrepancy, Deformity
Highlights
Externally controlled motorized intramedullary lengthening devices have been added to lengthening methods with external fixators and intramedullary nail-supported external fixators. The aim of this study is to describe technical and biomechanical features of lengthening and deformity correction surgery, as well as to compare the radiological functional, and clinical results of the patients treated with FITBONE and PRECİCE nails.
The results showed no significant difference between the groups, in terms of consolidation and distraction indices, the number of complications and Lower Extremity Functional Scale scores. Neither of the nails caused deviations in the mechanical axes and distal femoral angles.
The results indicate that both the FITBONE and PRECİCE lengthening nails improve physical, emotional and functional outcomes and similar radiographic results and complication rates can be achieved in treatment of lower extremity limb length discrepancy.
Introduction
Lower extremity deformity and leg length discrepancy cause limping and walking difficulties and may also affect the pelvis and spine. When left untreated, these create biomechanical problems involving the entire musculoskeletal system and the lower extremity.1,2 With developments in technology, new and better methods have been added to the treatment of these pathologies. Externally controlled motorized intramedullary lengthening devices have been added to lengthening methods with external fixators (ilizarov, monolateral external fixator) and intramedullary nail-supported external fixators.3 The most widely used lengthening intramedullary systems are Albizzia (Depuy, Villeurbanne, France), ISKD (Orthofixinc.), FITBONE (Wittenstein, Igersheim, Germany) PRECICE (Ellipse Technologies, İrvine, CA, USA) nails.3–6
The aim of this study was to discuss the technical and biomechanical features of lengthening and deformity correction surgery and compare the radiological, functional, and clinical results of patients treated with FITBONE and Precice nails.
Materials and Methods
Patients
This retrospective cohort study included all patients with leg length discrepancy and deformity, who underwent limb lengthening surgery with externally controlled motorized extendable intramedullary nails at the Orthopedics and Traumatology Clinic of S.B.U Sisli Hamidiye Etfal Training and Research Hospital between 2010 and 2020 with complaints of limping, gait disturbance, and pain. Al1 41 patients included in the study have completed the lengthening procedure. No patient was excluded from the study for any specific reason. The study was approved as a retrospective study by the Clinical Research Ethics Committee of S.B.U Sisli Hamidiye Etfal Training and Research Hospital (No: 3337). The informed consent was obtained from all patients participating in the study. No funding was received and there are no competing interests declared.
Implants
The first implant used was the second-generation Precice magnetic extension system produced by Nuvasive Specialized Orthopaedics, Inc. Ellipse Technologies (Irvine, Calif, USA) developed the PRECICE nail with a team of surgeons led by Dr. Stuart Green, using the mechanism they developed for their spine growing rods called the “MAGEC System.”7
The FITBONE® intramedullary limb lengthening system was developed in partnership with Professor Baumgart. Unlike mechanical distraction nails, the FITBONE system provides lengthening via an integrated, fully encapsulated motor. The required energy is sent from an external control unit via a transmitter to a receiver placed under the skin.8
Patient preparation and surgical technique
During the preoperative planning for the deformity and limb lengthening surgeries, clinical and radiographic evaluations of lower extremity shortness and associated varus/valgus deformities were performed. A single-level osteotomy was planned at the apex of the associated deformity to achieve acute correction during surgery. In patients with isolated limb shortness, osteotomy was planned from the diaphyseal region to prevent iatrogenic deformity.
Optimal nail sizes were determined based on the preoperative bone length and canal diameter measurements taken using a calibrated digital radiography system ([Picture Archiving and Communication System (PACS)]. According to the manufacturer’s recommendations, the length of the nail was selected so that at the end of the lengthening, at least a 2-3 cm thicker nail fragment was located within the distraction bone segment. In order to prevent avascular necrosis of the femoral head in pediatric patients, 10° proximal inclined nails were selected, and for adults, straight antegrade nails. In retrograde femoral nail applications, 10° angled or straight nails were selected according to procurvatum or recurvatum deformity in the distal femur.
All patients were administered 2 g cefazolin 1 hour preoperatively, and 600 mg clindamycin iv antibiotherapy was given to patients with allergies. For antegrade femoral intramedullary nail application, the tip of the greater trochanter level was marked on the skin under fluoroscopy. A Steinmann pin was placed in the piriformis fossa.
For retrograde nailing, measurements were made 1 cm proximal to the intercondylar notch. After making a 1 cm lateral incision at the osteotomy level, holes were made in the bone using a 4.8 mm drill bit. A Steinmann pin was placed in the middle of the intercondylar notch and laterally at the distal end of the Blumensaat line on the anteroposterior (AP) image.
The guidewire was removed, and the nail was inserted into the canal up to the planned osteotomy level. Two parallel Steinmann pins were inserted into the femur, both proximally and distally, to avoid rotation during osteotomy. The femur was fixed with the help of an assistant, and an osteotomy was performed using a drill on the previously determined osteotomy line. The osteotomy was then completed using a thin osteotome.
If the FITBONE nail was to be applied, a tunnel was prepared for the cable between the motor unit and the subcutaneous antenna using a drill and guide at this stage. The nail was then advanced manually and checked under fluoroscopy that it was placed at the desired level. After the FITBONE nail was placed carefully without resistance, it was locked distally and proximally. The cable unit was passed through the tunnel and connected to the subcutaneous antenna.
After locking, the distraction area of the nail was determined and marked under fluoroscopy guidance. The procedure was terminated by making a 1-2 mm distraction, which was checked with fluoroscopy to ensure that the nails were working before the patient woke up.
When applying intramedullary nails to the tibia, a 4.5 mm syndesmotic screw was inserted at the distal syndesmosis level to protect the distal tibiofibular joint. A 1 cm incision was then made on the fibula from the 1/3 mid-level lateral, and the fibula was osteotomized using a drill and osteotome, and a 1 cm block was resected.
While the knee was in hyperflexion, the entry point was enlarged using a reamer. The predetermined osteotomy line was entered with a 1 cm incision, the periosteum was removed, and multiple drilling was performed with a drill. If the deformity was to be corrected, blocking screws were placed in the predetermined locations under fluoroscopy guidance. The nail was advanced and sent distally. Then, the aforementioned stages on the femur were completed, and the operation was terminated (Figure 1).
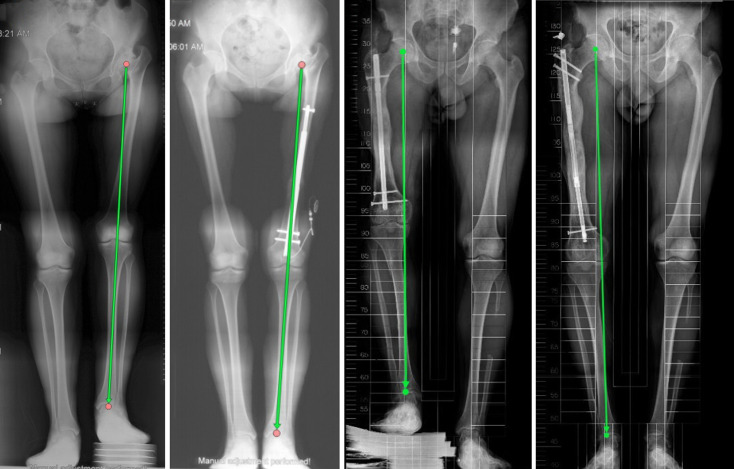
Figure 1.
(A) 35-year-old female patient had shortness (45 mm) and a lateral mechanical axis deviation in her left lower extremity due to DDH. (B) The patient’s lower extremity was lengthened with a femoral FITBONE nail application. (C) A 36-year-old male patient was operated on 6 times for a femur fracture after a motor vehicle accident. (D) The patient had shortness of 80 mm and was lengthened with the PRECICE nail.
Postoperative care
Active hip, knee, and ankle exercises were started 1 day after surgery. When the latent period after osteotomy ended, daily lengthenings were started (femur: 7 days; tibia: 5-7 days). The use of the devices, the frequency, and the amount of lengthening was explained to the patients in detail, and it was ensured that they learned the process. In femur and tibia lengthenings, 1 mm/day distraction was started at 0.25 mm/day 4 times. In the distraction phase, the patients were called for follow-up every 2 weeks and evaluated with x-rays. During the consolidation period, follow-up examinations were every 6 weeks.
Patients with congenital shortness of the femur and insufficient cruciate ligaments were closely monitored for early knee luxation throughout the distraction phase and for the first 2 months after completion of lengthening. It was also recommended to use a knee orthosis to keep the knee in full extension for 22 hours a day. Full weight bearing was allowed when radiographs showed consolidation in at least 3 cortices of the regeneration.7
Radiological evaluation and parameters
The demographic characteristics of the 2 groups of patients were evaluated as age, gender, weight, height, comorbidity, smoking, etiology, operated bone, presence of deformity, and operation method (Tables 1 and 2).
Table 1.
Demographic characteristics of the patients (Pearson chi-square test)
| FITBONE | PRECİCE | P | |||
|---|---|---|---|---|---|
| Gender | Male | 8 (40%) | Male | 12 (57.1%) | |
| Female | 12 (60%) | Female | 9 (42.9%) | .272 | |
| Side | Right | 9 (45%) | Right | 11 (52.4%) | |
| Left | 11 (55%) | Left | 10 (47.6%) | .636 | |
| Etiology | Posttraumatic | 6 (30%) | Posttraumatic | 10 (47.6%) | |
| DHD sequelae | 4 (20%) | DHD sequelae | 2 (9.5%) | ||
| Hemihypertrophy | 4 (20%) | Hemihypertrophy | 2 (9.5%) | ||
| Congenital | 2 (10%) | Congenital | 5 (23.8%) | ||
| Polio sequelae | 2 (10%) | Polio sequelae | 1 (4.8%) | ||
| Fibula hemimelia | 1 (5%) | Achondroplasia | 1 (4.8%) | ||
| Achondroplasia | 1 (5%) | Fibula hemimelia | 0 (0%) | .553 | |
| Nail application | Retrograde femoral nail | 13 (65%) | Retrograde femoral nail | 3 (14.29%) | |
| Antegrade femoral nail | 5 (25%) | Antegrade femoral nail | 12 (57.14%) | ||
| Tibial nail | 2 (10%) | Tibial nail | 6 (28.57%) | .040 | |
| Surgical purpose | Isolated lengthening | 11 (55%) | Isolated lengthening | 16 (76.2%) | |
| Varus correct. + lengt. | 5 (25%) | Varus correct. + lengt. | 3 (14.3%) | ||
| Valgus correct. + lengt. | 4 (20%) | Valgus correct. + lengt. | 2 (9.5%) | .355 | |
Table 2.
Descriptive statistics calculated from the radiological measurements of the patients
|
|
FITBONE | PRECICE | P | ||||
|---|---|---|---|---|---|---|---|
| Mean ± SD | Minimum–maximum | Median | Mean ± SD | Minimum–maximum | Median | ||
| Age* | 27.3 ± 9.25 | 14-46 | 25 | 23.57 ± 9.69 | 14 to 45 | 20 | .123 |
| Weight (kg) | 66.55 ± 10.7 | 51-89 | 65.50 | 66.9 ± 7.22 | 52 to 86 | 66 | .027 |
| Height (cm) | 165.65 ± 9.8 | 150-186 | 162.50 | 164.4 ± 7.8 | 150 to 181 | 163 | .080 |
| Shortness (mm)* | 59.10 ± 22.4 | 35-130 | 55 | 65.6 ± 35.9 | 38 to 210 | 58 | .480 |
| Lengthening amount (mm)* | 54.35 ± 13.79 | 35-80 | 48 | 56.7 ± 14.99 | 38 to 80 | 52 | .564 |
| Preoperative MAD (mm) | 6.6 ± 15 | -20-22 | 13.5 | 8.29 ±17.7 | -15 to 50 | 5 | .874 |
| Postoperative MAD (mm) | 4.2 ± 6.8 | -9-19 | 5 | 5.2 ± 14.8 | -27 to 35 | 8 | .012 |
| Preoperative MNSA (°) | 130.50± 8.05 | 110-145 | 130.5 | 127.45 ± 8.65 | 103 to 140 | 127 | .558 |
| Postoperative MNSA (°) | 127.58 ± 8.46 | 107-139 | 128.8 | 126.66 ± 5.95 | 108 to 136 | 126 | .049 |
| Preoperative aMPFA (°)* | 84.70±7.63 | 73-99 | 86.5 | 83.95 ±10.54 | 52 to 98.8 | 87 | .906 |
| Postoperative aMPFA (°)* | 78.66 ±12.8 | 36-95.7 | 81.35 | 82.99 ± 8.71 | 57 to 94.3 | 85 | .175 |
| Preoperative mLPFA (°)* | 88.55± 6.32 | 74-100 | 90 | 89.56 ± 13.99 | 74.5 to 135 | 85 | .396 |
| Postoperative mLPFA (°)* | 94.61 ± 16.82 | 72.3-141 | 89.35 | 91.18 ± 11.23 | 78.9 to 122 | 86.6 | .382 |
| Preoperative aLDFA (°) | 80.50± 4.57 | 70-89 | 80.5 | 84.76 ± 6.01 | 73 to 99 | 85.20 | .455 |
| Postoperative aLDFA (°) | 84.93 ± 4.22 | 77.6-95.5 | 85.2 | 83.4 ± 7.85 | 60 to 96.8 | 82.6 | .071 |
| Preoperative mLDFA (°) | 88.7 ± 5.59 | 79-96 | 90 | 89.8 ± 5.2 | 81 to 102 | 88 | .434 |
| Postoperative mLDFA (°) | 88.5 ± 5 | 79.3-100 | 88.5 | 89.2 ± 5.43 | 79.7 to 100 | 89 | .879 |
| Preoperative mMPTA (°) | 89.50 ± 3.00 | 83-96 | 90 | 88.35 ± 3.45 | 81 to 96 | 89 | .734 |
| Postoperative mMPTA (°) | 87.95 ± 2.37 | 82.9-94 | 88.3 | 88.46 ± 3.69 | 81.2 to 94.9 | 87.8 | .036 |
| Follow-up time (months) | 15.95 ± 4.75 | 9-29 | 15.50 | 20.48 ± 7.57 | 12 to 39 | 18 | .027 |
| Distraction index* total (days/mm) | 1.11 ± 0.13 | 0.92-1.4 | 1.1 | 1.29 ± 0.35 | 1 to 2.1 | 1.18 | .097 |
| Distraction index* femur (days/mm) | 1.09 ± 0.12 | 0.92-1.4 | 1.1 | 1.14 ± 0.2 | 1 to 1.75 | 1.1 | .486 |
| Distraction index* tibia (days/mm) | 1.28 ± 0.18 | 1.15-1.4 | 1.28 | 1.65 ± 0.4 | 1.2 to 2.1 | 1.65 | .241 |
| Consolidation index—total (day/cm) | 30.9 ± 3.7 | 24-38.25 | 31 | 32.3 ± 4.7 | 23.5 to 37.4 | 30.6 | .088 |
| Consolidation index—femur (days/cm) | 30.56 ± 3.45 | 24-37 | 30.75 | 31.4 ± 5 | 23.5 to 39.4 | 29.4 | .070 |
| Consolidation index—tibia (days/cm) | 34.38 ± 5.48 | 30.5 -38.2 | 34.385 | 34.7 ± 2.7 | 30.6 to 38.6 | 34.7 | .167 |
| LEFS | 78.5 ± 12.5 | 59-99 | 78.8 | 78.75 ± 13.7 | 60 to 99 | 81.3 | .425 |
aLDFA, anatomic lateral distal femoral angle; aMPFA, anatomic medial proximal femoral angle; LEFS, Lower Extremity Functional Scale; mLPFA, mechanical lateral distal femoral angle; mMPTA, mechanical medial proximal tibial angle.
*Indicates abnormal distribution (Mann–Whitney U test), and others are normally distributed (independent t-test).
The PACS (EXTREMPACS #2015-001) system was used to view the x-rays and calculate the measurements. The anatomic and mechanical axes of the extremities operated on with the Precice nail and FITBONE nail included in the study were calculated. Medial neck shaft angle (MNSA), mechanical axis deviation (MAD), mechanical lateral proximal femoral angle (mLPFA), anatomic medial proximal femoral angle (aMPFA), mechanical lateral distal femoral angle (mLDFA), anatomic lateral distal femoral angle (aLDFA), and mechanical medial proximal tibial angle (mMPTA) values were recorded from preoperative and end-of-treatment radiographs (Table 2).
Consolidation and distraction indexes were calculated to evaluate bone healing. The distraction index was accepted as the ratio of lengthening in millimeters to the number of days extended, while the consolidation index was considered as the ratio of bone healing time (the period when 3 of the 4 cortices became visible on anterior-posterior and direct lateral radiographs) to the amount of lengthening in centimeters. The follow-up time was calculated as the time between the date of osteotomy and the date when consolidation was seen in 3 cortices on the x-rays.
Translated version of the Lower Extremity Functional Scale (LEFS) test was applied to the patients to evaluate functional outcomes and quality of life.9 The test results were calculated as percentages (%). The Paley criteria modified by (the Association for the Study and Application of the Methods of İlizarov) ASAMİ were used for functional and bone outcome assessment.
Statistical analysis
Data obtained in the study were analyzed statistically using Statistical Package for Social Sciences (SPSS) version 26.0 software (IBM SPSS Corp.; Armonk, NY, USA). Descriptive statistics were stated as mean, SD, median, minimum, maximum values, frequency, and ratios. When comparing numerical data, the independent t-test, a parametric test, was used if the data were normally distributed, and the Mann–Whitney U test, a non-parametric test, was used if the data were abnormally distributed. For the comparisons of dependent variables within groups, the parametric dependent t-test was used if the data were normally distributed, and the Wilcoxon paired-pairs test was used if the data were abnormally distributed. Pearson’s chi-square test was used to compare categorical data. The level of statistical significance was set at P < .05.
Results
This study included 2 separate patient groups. A total of 41 patients were operated on as 20 with FITBONE nails (group F) and 21 with Precice nails (group P).
Group F (FITBONE) patients comprised 8 (40%) males and 12 (60%) females with a mean age of 27.3 ± 9.25 years, mean weight of 66.55 ±10.7 kg, and mean height of 165.65 ± 9.8 cm.
The group P (Precice) patients comprised 12 (57.14%) males and 9 (42.86%) females, with a mean age of 23.57 ± 9.69 years, mean weight of 66.9 ± 7.22 kg, and mean height of 164.4 ± 7.8 cm (Table 2).
A total of 7 (4 F group, 3 P group) patients were smokers. In group F, 1 patient was diagnosed with hypertension, and in group P, 1 patient had diabetes mellitus, and 1 patient was diagnosed with hypertension. Of the 41 surgical procedures performed, 33 (group F: 18, group P: 15) were applied to the femur, and 8 (group F:2, group P: 6) were applied to the tibia bone. Femoral antegrade nailing was performed in 5 patients in group F and 12 patients in group P, and retrograde nailing was performed in 13 patients in group F and in 3 patients in group P.
The patients in both groups showed a similar distribution in terms of gender, side, etiology, and surgical purpose and were heterogeneous in terms of nail application (Table 1).
While the mean postoperative follow-up period was 15.95 ± 4.75 months in group F and 20.48 ± 7.57 months in group P, the difference between the 2 groups was statistically significant (P = .027).
The 2 patient groups were determined to be similar in respect of age, height, shortness, amount of lengthening, all preoperative angle measurements, distraction, and consolidation indexes (Table 2).
Alignment, malalignment, and lengthening
There was no difference between the P and F groups in respect of the preoperatively measured angles. A statistically significant difference was determined between the groups in respect of the postoperative MAD, MNSA, and mMPTA values (P < .05) (Table 2).
Nails were applied to 14 patients after osteotomy and acute correction. There were 8 varus and 6 valgus deformities, and their distribution was similar in groups P and F. The MAD parameter decreased from 29.6 to 12 in patients with varus deformity and improved from −14.7 to 7 mm in patients with valgus deformity. Similarly, the mLDFA values regressed to normal limits (P < .05) (Table 3).
Table 3.
Comparison of the preoperative and postoperative deformity values of the patients using Wilcoxon test
| Shortness | Lengthening | P | ||
|---|---|---|---|---|
| Intended elongation | F | 59.10 (35-130) | 54.35 (35-80) | .109 |
| P | 65.6 (38-210) | 56.7 (38-80) | .050 | |
| Preoperative | Postoperative | P | ||
| Acute axial correction after osteotomy (n = 14) | ||||
| MAD (mm) | Varus |
|
12 (−7 to 35) | .012 |
| Valgus | −14.7 (−20 to −10) | 7 (0-14) | .028 | |
| mLDFA (°) | Varus | 93.5 (84-99) | 90.5 (84.5-94.1) | .017 |
| Valgus | 83.4 (79-89) | 89 (79.3-100.8) | .027 | |
| Isolated lengthening (n = 27) | ||||
| MAD (mm) | F(11) | 8.5 (−16 to 19) | 3.5 (−9 to 19) | .056 |
| P(16) | 3.8 (−15 to 18) | 0.8 (−27 to 16) | .079 | |
| MNSA (°) | F(11) | 128 (110-136) | 127 (107-138) | .529 |
| P(16) | 129 (116-140) | 129 (121-136) | .593 | |
| mLDFA (°) | F(11) | 90 (81-96) | 88 (81-95) | .695 |
| P(16) | 89 (81-102) | 89 (78-100) | .518 | |
| MPTA (°) | F(11) | 90 (85-96) | 88 (83-90) | .100 |
| P(16) | 89 (84-96) | 89 (81-95) | .977 | |
MAD, mechanical axis deviation; mLDFA, mechanical lateral distal femoral angle; MNSA, medial neck shaft angle; MPTA, medial proximal tibial angle.
The MAD, MNSA, mLDFA, and mPTA values of 27 patients with isolated shortness were evaluated with the suspicion that malalignment might occur during elongation. It was observed that the nails did not cause deviations in the mechanical axis and femoral distal angles during extension (P > .05) (Table 3).
In group F, the mean preoperative shortness was 59.10 ± 22.4 mm, and the lengthening in the postoperative follow-up period was 54.35 ± 13.79 mm. In evaluating the relationship between the preoperative shortness and the amount of postoperative lengthening, no significant difference was found (P = .109). In group P, these values were 65.6 ± 35.9 mm and 56.7 ± 14.99 mm with no significant difference determined (P = .05) (Table 3). These results show that the lengthenings were completed as intended, and the extremity shortness was adequately corrected. These shortness and elongation values were found to be similar between the 2 groups (P = .480 for shortness; P = .564 for lengthening) (Table 2).
The distraction indexes were calculated as 1.11 ± 0.13 for the FITBONE and 1.29 ± 0.35 for the PRECICE. It was also calculated for the femur and tibia in isolation. No statistically significant difference was found between the groups (P > .05) (Table 2).
Healing and regeneration
The mean consolidation index was calculated as 30.94 ± 3 (days/cm) in group F and 32 ± 4 (days/cm) in group P. The consolidation indices for the isolated femur and tibia are shown in Table 2. No statistically significant difference in consolidation indices was found between the groups (P > .05) (Table 2).
Consolidation was completed in all patients. Delayed union was observed in 1 patient in group F and 2 in group P. Union was achieved by replacing the nail with grafting and rigid nails. Paley’s limb lengthening bone outcome measures on intramedullary nails modified by ASAMI were calculated in both groups. In group F, the bone score was found to be very good in 90% of the patients, and good in 10%. In group P, 85.71% were evaluated as very good and 14.29% as good.
Complications and functional results
During the follow-up period, 4 complications occurred in 3 patients (20%) in group F. Perioperative fracture developed in 1 patient who underwent femoral surgery, and osteosynthesis was performed with a plate and screw. Delayed union was detected in the follow-up period, so autograft was applied to the osteotomy area with autograft from the iliac crest. In the second patient who underwent femoral surgery, premature union and joint contracture developed. Re-osteotomy was performed after manipulation was applied to the patient under anesthesia. Tibia lengthening surgery was performed in the third patient due to hemihypertrophy. A fracture around the implant was detected during follow-up, and osteosynthesis was performed with a plate and screw.
In group P, the delayed union was detected in 2 (1 femur, 1 tibia) of 4 (19.05%) patients who developed complications, and nail replacement was performed with autograft and rigid nails. In 1 of the other 2 patients who underwent femoral surgery, the proximal locking screw came back and was reinserted in the operating room under local anesthesia and sedation. In the second patient, the premature union developed, so a re-osteotomy was performed. The full union was determined in the final follow-up examinations of the patients in both groups.
The mean LEFS value in group F patients was calculated as 78.50 ± 12.5%. The LEFS values of 3 patients who underwent lengthening surgery because of hemihypertrophy, polio sequelae, and developmental dysplasia of the hip (DDH) were significantly lower than those of the other patients [Table 2]. In Group P, the mean LEFS score was 78.75 ± 13.7%. The lowest values in this group were seen in one patient with a diagnosis of osteogenesis imperfecta, who was operated on for posttraumatic shortness, and in another patient who underwent lengthening surgery for fibular hemimelia. No significant difference was found between the 2 groups (P = .425)
Discussion
There is more experience with traditional methods for limb lengthening and deformity correction surgery. However, experience with externally controlled motorized extendable intramedullary nail surgery, which has been used for the past 20 years, still needs to be improved. Disadvantages such as pain, infection, joint stiffness, and low patient compliance have been frequently mentioned in the literature in surgeries performed with circular external fixators and monolateral fixators combined with nails.9-11 Developing technologies in deformity correction and limb lengthening surgery have led to fewer complications and more predictable results making expandable nails advantageous.
From previous studies, it can be seen that the patient groups are mostly in the second and third decades of life.3,4,12,13 The patients in the current study were also in this age group. The patient groups of this study were similar in terms of many demographic, etiological, and radiological parameters, enabling a more objective evaluation.
There were differences between the 2 groups in respect of implant and surgical technique.
When comparing the 2 implants based on their specifications, the PRECICE nail offers more size and thickness options than the FITBONE. Additionally, the Precice nail has a winding and rewinding feature that provides the advantage of retraction in cases of excessive lengthening or distraction-compression in non-union cases. On the other hand, using the FITBONE nail may result in problems with antenna placement, and there is a risk of perioperative fracture due to the free driving of the locking screws.
From this perspective, the PRECICE nail appears to be more advantageous for application. However, our study did not yield any data to support this claim. It is important to note that further research and analysis may be necessary to fully evaluate the effectiveness and safety of these implants in clinical practice.
In the results of nail lengthening surgery reported in the literature, there is often no difference between the planned and final lengthening amounts. Some studies have reported residual shortness of ±5 mm.3,7,12,14 This was also the case in some of the current study patients with remaining subclinical shortness.
In a study of 50 patients in 2018, Horn et al did not detect a significant difference between preoperative and postoperative MAD values in patients who underwent isolated lengthening. However, a difference was found in those who underwent acute correction and lengthening. The same article mentioned that there might be deviations in MNSA values in extremity surgery performed with antegrade femoral nails.13 In the current study, the MAD and mLDFA parameters were seen to be within the normal range in 13 patients with acute correction. The main reason for the difference in postoperative MAD, postoperative MNSA, and postoperative mMPTA values between the 2 groups was due to the patients being corrected for deformity. In addition, there were only minor changes of 1-2° in the MAD, MNSA, mLDFA, and MPTA parameters of 28 patients on whom isolated lengthening was performed.
A study published by Morrison et al15 in 2020 discussed the specific complications that may occur in lengthening surgery with motorized nails, such as failure of nail distraction, insufficient regenerate and non-union, device breakage, iatrogenic deformity, joint contracture, joint subluxation, and neurovascular complications. In a systematic literature review of complications following surgery performed with motor nails on 983 segments, published in 2021, Frost et al reported a generally high complication rate. In 1 of every 4 segments, complications were said to have a major impact, leading to significant changes in treatment (15%), failure to achieve the lengthening goal (5%), or the onset of a new pathology or permanent sequelae (3%).16 In the current study, the complication rates of both groups of patients were found to be close to the literature and did not affect the final treatment or cause any permanent sequelae. Among the F group patients, 4 complications developed in 3 patients (20%), and complications developed in 4 patients (19.05%) in group P. The complications encountered were non-union, premature union, preoperative fracture, and screw backout.
It is noteworthy that the follow-up period of the P group patients was statistically longer. There was no significant difference between the groups in respect of the number of complications. However, the follow-up time of the patients with complications in the PRECİCE group was longer. In 1 patient in group F, who had a perioperative fracture and later underwent grafting due to non-union, the follow-up period was 29 months. In contrast, all the remaining patients had a follow-up period of 21 months or less. The follow-up period of 4 patients with complications in the P group was calculated as 24–27–30–39 months.
In a study published by Landge et al17 in 2015, a 12-item patient questionnaire was created to evaluate the satisfaction of patients who underwent lengthening surgery with an external fixator and lengthening nails and the results showed that nails were preferred in terms of pain, esthetics, and ease of rehabilitation. In 2009, Schep et al6 reported a mean LEFS score of 75% for the long-term functional results of lengthening surgery with limb reconstruction system (LRS) in 15 patients. This was similar to the LEFS scores calculated in the current study. The number of studies in the literature that have evaluated postoperative functional outcomes is very limited.18 In general, although it is thought that extendable nails provide significant patient comfort during lengthening but do not make a significant functional difference at the end of the treatment, this idea needs to be clarified and is open to discussion. Preoperative and postoperative functional scoring could be considered to be more valuable in revealing the functional results of deformity correction and lengthening surgery with motorized nails. The success of motorized extension nails depends on critical factors such as appropriate surgical training, correct preoperative planning, minimally invasive surgery, mechanical integrity of the structure, and control of the ideal distraction rate and rhythm.
The positive aspect of this study was that the groups were similar in terms of age, gender, side, and etiology distribution. A negative aspect was the heterogeneous distribution of the femoral antegrade and retrograde nails between the groups. Another negative aspect of the study is the retrospective investigation of the patients. In addition, the implant applied to the patients was chosen in accordance with the conditions and accessibility of that day. Therefore, the implants were not selected according to the characteristics of the patients, and controlled randomization was not applied at the same time. A further limitation was that as all the measurements were made on the orthoroentgenogram, sagittal measurements such as posterior proximal tibial angle (PPTA) were insufficient, and the sagittal plane could not be thoroughly evaluated.
Lower extremity deformities and length differences are problems that have social, economic, cosmetic, and psychological effects on patients and are difficult to treat for both the patient and the surgeon. Treatment methods for this pathology that have been applied for many years are progressing further with new developments in technology.
The motorized intramedullary lengthening nail is essential for limb length and deformity correction surgery. Using these implants allows correction even in patients with multiplane deformities. It can be considered that the success of this procedure depends on the implant, meticulous preoperative planning, and correct application.
Lower extremity limb length discrepancy can be effectively treated with both the FITBONE and PRECİCE fully implantable motorized lengthening nails, resulting in improved physical and emotional functional outcomes, similar radiographic results and complication rates, high patient compliance, and good cosmesis.
Footnotes
Ethics committee approval: This study was approved by Ethics Committee of University of Health Sciences Sisli Hamidiye Etfal Training and Research Hospital (Approval No: 3337, Date: November 23, 2021).
Informed consent: Written informed consent was obtained from the patients who agreed to take part in the study.
Peer-review: Externally peer-reviewed.
Author contributions: Consept – İ.K.A.S., M.K.; Design – F.S., İ.K.A.S.; Supervision – İ.K.A.S., M.K.; Resoruces – M.K., H.M.Ö.; Materials – F.S., İ.T.; Data Collection – F.S., İ.T.; Analysis – İ.K.A.S., F.S.; Literature Search – İ.K.A.S., İ.T.; Writing – İ.K.A.S., F.S.; Critical Review – M.K., H.M.Ö.
Declaration of interests: The authors have no conflict of interest to declare.
Funding: The authors declared that this study has received no financial support.
References
- 1. Gurney B. Leg length discrepancy. Gait Posture. 2002;15(2):195 206. ( 10.1016/S0966-6362(01)00148-5) [DOI] [PubMed] [Google Scholar]
- 2. Delacerda FG, Wikoff OD. Effect of lower extremity asymmetry on the kinematics of gait. J Orthop Sports Phys Ther. 1982;3(3):105 107. ( 10.2519/jospt.1982.3.3.105) [DOI] [PubMed] [Google Scholar]
- 3. Kirane YM, Fragomen AT, Rozbruch SR. Precision of the PRECICE® internal bone lengthening nail. Clin Orthop Relat Res. 2014;472(12):3869 3878. ( 10.1007/s11999-014-3575-0) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Calder PR, McKay JE, Timms AJ, et al. Femoral lengthening using the Precice intramedullary limb-lengthening system: outcome comparison following antegrade and retrograde nails. Bone Joint J. 2019;101-B(9):1168 1176. ( 10.1302/0301-620X.101B9.BJJ-2018-1271.R1) [DOI] [PubMed] [Google Scholar]
- 5. Shabtai L, Specht SC, Standard SC, Herzenberg JE. Internal lengthening device for congenital femoral deficiency and fibular hemimelia. Clin Orthop Relat Res. 2014;472(12):3860 3868. ( 10.1007/s11999-014-3572-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schep NWL, van Lieshout EMM, Patka P, Vogels LMM. Long-term functional and quality of live assessment following post-traumatic distraction osteogenesis of the lower limb. Strateg Trauma Limb Reconstr. 2009;4(3):107 112. ( 10.1007/s11751-009-0070-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Paley D. PRECICE intramedullary limb lengthening system. Expert Rev Med Devices. 2015;12(3):231 249. ( 10.1586/17434440.2015.1005604) [DOI] [PubMed] [Google Scholar]
- 8. Baumgart R, Zeiler C, Kettler M, Weiss S, Schweiberer L. Der voll implantierbare Distraktionsmarknagel bei Verkürzungen, Deformitäten und Knochendefekten. Orthopade. 1999;28(12):1058 1065. ( 10.1007/s001320050431) [DOI] [PubMed] [Google Scholar]
- 9. Çankaya M, Karakaya İÇ, Karakaya MG. Reliability and validity of the Turkish version of the lower extremity Functional Scale in patients with different lower limb musculoskeletal dysfunctions. Int J Ther Rehabil. 2019;26(9):1 14. ( 10.12968/ijtr.2018.0137) [DOI] [Google Scholar]
- 10. García-Cimbrelo E, Curto de la Mano A, García-Rey E, Cordero J, Marti-Ciruelos R. The intramedullary elongation nail for femoral lengthening. J Bone Joint Surg Br. 2002;84(7):971 977. ( 10.1302/0301-620X.84B7.12984) [DOI] [PubMed] [Google Scholar]
- 11. Baumgart R. The reverse planning method for lengthening of the lower limb using a straight intramedullary nail with or without deformity correction. A new method. Oper Orthop Traumatol. 2009;21(2):221 233. ( 10.1007/s00064-009-1709-4) [DOI] [PubMed] [Google Scholar]
- 12. Dinçyürek H, Kocaoğlu M, Eralp IL, Bilen FE, Dikmen G, Eren I. Functional results of lower extremity lengthening by motorized intramedullary nails. Acta Orthop Traumatol Turc. 2012;46(1):42 49. ( 10.3944/AOTT.2012.2671) [DOI] [PubMed] [Google Scholar]
- 13. Horn J, Hvid I, Huhnstock S, Breen AB, Steen H. Limb lengthening and deformity correction with externally controlled motorized intramedullary nails: evaluation of 50 consecutive lengthenings. Acta Orthop. 2019;90(1):81 87. ( 10.1080/17453674.2018.1534321) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Laubscher M, Mitchell C, Timms A, Goodier D, Calder P. Outcomes following femoral lengthening: an initial comparison of the Precice intramedullary lengthening nail and the LRS external fixator monorail system. Bone Joint J. 2016;98-B(10):1382 1388. ( 10.1302/0301-620X.98B10.36643) [DOI] [PubMed] [Google Scholar]
- 15. Morrison SG, Georgiadis AG, Huser AJ, Dahl MT. Complications of limb lengthening with motorized intramedullary nails. J Am Acad Orthop Surg. 2020;28(18):e803 e809. ( 10.5435/JAAOS-D-20-00064) [DOI] [PubMed] [Google Scholar]
- 16. Frost MW, Rahbek O, Traerup J, Ceccotti AA, Kold S. Systematic review of complications with externally controlled motorized intramedullary bone lengthening nails (FITBONE and PRECICE) in 983 segments. Acta Orthop. 2021;92(1):120 127. ( 10.1080/17453674.2020.1835321) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Landge V, Shabtai L, Gesheff M, Specht SC, Herzenberg JE. Patient satisfaction after limb lengthening with internal and external devices. J Surg Orthop Adv. 2015;24(3):174 179. ( 10.3113/JSOA.2015.0174) [DOI] [PubMed] [Google Scholar]
- 18. Wagner P, Burghardt RD, Green SA, Specht SC, Standard SC, Herzenberg JE. PRECICE® magnetically-driven, telescopic, intramedullary lengthening nail: pre-clinical testing and first 30 patients. SICOT J. 2017;3:19. ( 10.1051/sicotj/2016048) [DOI] [PMC free article] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a