Abstract
The experience of rejection and disconnection reliably amplifies pain. Yet, little is known about the impact of enduring feelings of closeness, or social connectedness, on experiences of chronic pain. The current secondary analysis tested the hypothesis that greater social connectedness would predict lower chronic pain ratings, mediated by lower depression and anxiety. In addition, based on the social-affective effects of deeper pressure, and our previous finding that deeper pressure from a weighted blanket reduced chronic pain ratings, we examined whether deeper pressure from a weighted blanket would induce greater pain relief in socially disconnected chronic pain patients. We assessed social connectedness, anxiety, and depression at baseline and pain levels before and after a remote, seven-day randomized-controlled trial of a heavy or light (control) weighted blanket in a predominately White (86%) and female (80%) sample of 95 chronic pain patients. Results revealed that lower social connectedness was associated with higher chronic pain ratings, which was mediated by anxiety, but not depression. Pressure level (light vs. deep) moderated associations between social connectedness and pain reductions, such that deeper pressure was necessary for pain relief in the most socially disconnected participants. Our findings suggest a close relationship between social connectedness and chronic pain through a mechanistic pathway of anxiety. Further, our findings demonstrate that sensory-affective interventions such as a weighted blanket may be a beneficial tool for chronic pain sufferers who are prone to social disconnection, potentially by activating embodied representations of safety and social support.
Keywords: chronic pain, social connectedness, deep pressure, affective touch, anxiety
Introduction
Humans exhibit a profound need to belong, relying on others for survival and well-being throughout the lifespan (Baumeister & Leary, 1995; Taylor, 2007). Multiple sources of evidence suggest that basic homeostatic mechanisms may have evolved to monitor and maintain social relationships. For example, threats to social inclusion are often described as “painful” (Eisenberger, 2012a; 2012b; MacDonald & Leary, 2005) and recruit hunger-like craving mechanisms in the midbrain (Tomova et al., 2020). In fact, there is significant overlap in the neural circuitry subserving the affective components of physical pain and the pain of disrupted social connections (Eisenberger, 2012a; Eisenberger et al., 2003; Inagaki et al., 2016; Inagaki et al., 2020), revealing close linkages between experiences of pain and human (dis)connectionIndeed, a growing body of evidence shows that negative social factors, including social isolation (Karayannis et al., 2019; Oliveira et al., 2015), social exclusion (Bungert et al., 2015; Eisenberger et al., 2003), and loneliness (Jaremka et al., 2014; Wolf & Davis, 2014; Wolf et al., 2015) co-vary with and amplify both acute and chronic pain (Karayannis et al., 2019; Oliveira et al., 2015). Similarly, adults who were abused or neglected in childhood are at increased risk of chronic pain (Davis et al., 2005; Lampe et al., 2003).
Much less is known about the impact of positive social factors on pain. A fundamental benefit of connecting with others is the opportunity to receive tangible, emotional, and appraisal support in the face of threatening situations, like pain. For example, pain has motivational aspects that signal the need for help from others to remove the self from threat (Wiech & Tracey 2013; Krahe et al., 2013). In turn, receiving social support during potentially threatening exposures reduces subjective pain ratings (Brown et al., 2003; Reddan et al., 2020; Lopez-Sola et al., 2019). Evidence also suggests that chronic pain patients that engage in meaningful social connections (Koebner et al., 2019) and have a close, expansive social network (Mitchinson et al., 2008; Hughto et al., 2021) report lower pain and are less likely to abuse opiate mediations.
Social connectedness is defined as an attribute of the self that reflects cognitions of enduring interpersonal closeness with others (Lee et al., 2001; Lee & Robbins, 1995). In contrast to negative social constructs, social connectedness focuses on the independent self in relation to others, providing a stable phenomenological sense of connectedness or social closeness that is not susceptible to vacillations in relationships, social network size, or exclusions from others. People with high social connectedness tend to feel close with other people, identify with them, and readily engage in social activities and groups. In contrast, socially disconnected persons tend to view themselves as outsiders, feel misunderstood by others, and have difficulty engaging in social interactions, characteristic of people with insecure or anxious attachment styles (Lee et al., 2001; Lee & Robbins, 1995). A greater appreciation of the psychosocial style by which one navigates their environment should provide a more comprehensive understanding of the differential trajectories of a person living with chronic pain.
There is widespread agreement that a lack of social connectedness is a leading determinant of anxiety and depression (Lee et al.,, 2001; Santini et al., 2020; Wickramaratne et al., 2022; Schmidt et al., 2022; Karayannis et al., 2019; Jaremka et al., 2014). The elevated negativity inherent in self-other evaluations by those prone to social disconnection may reflect pervasive differences in negative appraisals and emotionality (Cacioppo & Hawkley, 2009; Watson & Clark, 1984) that heighten this risk. Of note, anxiety and depression also reliably exacerbate acute and chronic pain perceptions (Adler-Neal et al., 2019; Leino & Magni, 1993; Ploghaus et al., 2001; Rhudy & Meagher, 2000; van den Hout et al., 2001) and pain-related ruminations (Kucyi et al., 2014), suggesting potential mechanistic pathways whereby social connectedness might influence pain. In support of this idea, heightened periods of social disconnection in fibromyalgia patients are associated with increases in ruminative, negative cognitions related to pain, which in turn intensifies pain perceptions over time (Wolf et al., 2015; Jaremka et al., 2014). A generalized proclivity toward feelings of disconnection should increase the tendency toward anxiety and depression, amplifying the appraisal and rumination of chronic pain sensations.
Touch is integral to human relationships and social connection (Cascio et al., 2018; Dunbar, 2010; 2012; Suvilehto, 2015). Just as C-fiber nociceptive input is a peripheral trigger of the central experience of pain, the Social Affective Touch Hypothesis (Morrison et al., 2010; Olausson et al., 2008) posits that the C-tactile (CT) afferent pathway is a specialized sensory pathway underlying positively valanced social and affective components of touch. CT sensory afferents respond optimally to slow, gentle stroking of hairy skin (Morrison et al 2010; Vallbo et al., 1999; Watkins et al., 2021), which induces positive affect, reduces anxiety (Case et al 2020; Loken et al., 2011; Loken et al., 2009; Pawling, Cannon et al., 2017; Pawling, Trotter et al., 2017; Vallbo et al., 1999), and activates neural regions involved in the descending modulation of pain (Schweinhardt & Bushnell, 2010). Our recent research calls for an expansion of this hypothesis to consider the sensory pathways initiating the experience of pleasant deep pressure, as found in hugging, cuddling, hand holding, and massage (Case et al., 2020). Like CT touch, oscillating deep pressure – even when delivered by a mechanical compression sleeve – is perceived as pleasant and calming (Case et al., 2021; Diego et al., 2004; Field et al., 2010; Grandin, 1992), and activates neural substrates involved in interception and nociceptive processing (secondary somatosensory cortex; insula) (Case et al., 2021). Both deep pressure and CT optimal touch have been shown to reduce acute and chronic pain (Di Lernia et al., 2020; Fidanza et al., 2021; Field et al., 2002; Honigman et al., 2016; Law et al., 2008; Liljencrantz et al., 2017; von Mohr et al., 2018), beyond distraction and expectancy-related effects (Baumgartner et al., 2021; Liljencrantz et al., 2017). We recently demonstrated that deeper pressure delivered by 15-pound weighted blanket reduced ratings of chronic pain more than a 5-pound weighted blanket, particularly for individuals high in trait anxiety (Baumgartner et al., 2021), suggesting a pain modulatory mechanism for deep pressure that involves both sensory and psychosocial factors. The fact that touch therapies can be effective even when delivered in a non-social, mechanical format is of particular relevance to socially disconnected individuals who, by their disposition, are less likely to respond positively to therapies that include social interactions (Lee et al., 2001). Indeed, attachment styles have been shown to moderate associations between pleasant touch on pain, such that early pain-related neural processing is attenuated by pleasant touch in those who desire closeness from others (Krahé et al., 2016).
It is possible that C-tactile and deep pressure inputs could activate social-affective touch pathways capable of reducing pain in individuals low in social connectedness by implicitly activating embodied representations of social closeness, support, and safety (Baumgartner et al., 2021; Hertenstein et al., 2006; Krahe et al., 2013; Morrison et al., 2010). During a social exclusion manipulation, C-tactile optimal touch buffers against reduction in feelings of belongingness and other aspects of social closeness (von Mohr et al., 2017), possibly suggesting that disconnection motivates a need for touch (Tai et al., 2011). Across three studies (Master et al., 2009; Eisenberger et al., 2011; Younger et al., 2010), viewing pictures of a romantic partner reduced pain ratings, relative to a stranger or acquaintance and was positively associated with activation in areas associated with safety-signaling in response to threat (ventromedial prefrontal cortex) and reward processing (caudate; nucleus accumbens), not due to mere distraction effects (Eisenberger et al., 2011). Interestingly, the augmentation of safety-related neural mechanisms was stronger in those with more long-standing social connections (i.e., those in longer-term relationships) (Eisenberger et al., 2011). Taken together, these findings suggest that the conditioned social schemas or expectancies that touch may communicate (e.g., safety; closeness; social support) may alter the value, salience, and subjective experience of nociceptive signals in those who are prone to negatively appraise the status of their social relationships.
In the current study, we inquire about the relationship between social connectedness and chronic pain, and about the impact of social connectedness on the effects of deep pressure. The current study is a secondary analysis of our previously conducted remote, double-blind, between-subjects randomized controlled trial of weighted blankets for chronic pain (Baumgartner et al., 2021). A heterogeneous sample of adult chronic pain patients across the U.S. were randomly assigned to use a deeper or lighter pressure (placebo control) weighted blanket overnight for seven nights, with validated assessments collected remotely at baseline and post-intervention. Previously, we analyzed data from pain and selected psychological measures; additional measures of social connectedness and loneliness were collected, which are analyzed and reported in the present study. We hypothesized that social connectedness would exhibit a negative association with chronic pain at baseline, mediated by anxiety and depression. Given research on the social-affective effects of touch (Case et al., 2021; Goldstein et al., 2018; López-Solà et al., 2019; Reddan et al., 2020; von Mohr et al., 2017), we also tested whether individual differences in social connectedness would alter the modulation of pain by pressure; we hypothesized that socially disconnected individuals would experience greater pain relief from the deeper pressure weighted blanket.
Method
The study was conducted during the COVID-19 pandemic (June-November 2020).
Participants
Participants who self-reported having chronic pain before the study were recruited using ResearchMatch, a secure national registry that connects research volunteers with studies. Individuals were eligible if they were at least 18 years of age, fluent in English, diagnosed with chronic pain prior to study recruitment, willing to sleep with a weighted blanket for one week, able to safely lift at least 15 pounds, and willing to use their personal smartphone to complete study assessments. Individuals were excluded if they were pregnant, had a major medical condition, were current or previous users of a weighted blanket, or were claustrophobic. The UC San Diego Institutional Review Board approved all study procedures. All participants provided informed consent digitally via Research Electronic Data Capture (REDCap) software. In compensation for their time and effort, participants were offered to keep the weighted blanket and fitness tracker (used for exploratory sleep analyses) and received a $20.00 gift card for study completion.
Sample size determination was based on the primary outcomes of our original study. Based on the effect size of Cohen’s d = 0.75 estimated a published study demonstrating improvements in sleep quality (Ackerley et al., 2015), two independent groups, α = 0.05, and power = 0.80, we determined the study would require 48 participants in each blanket group for a total of N = 96. However, the IRB approved N = 135 to account for study dropout; the trial was stopped once we reached a planned sample size of 100 completed participants.
Sample characteristics
After exclusions and drop-outs, 95 adults with chronic pain constituted the final sample, with 47 in the light pressure blanket group and 48 in the heavy/deep pressure blanket group. Participants were 43.8 years of age on average (SD = 12.8; range = 19-69), and were predominantly female (n = 75, 80%) and White (White n = 81, 86%; Black n = 8, 9%; Hispanic and/or Latino n = 4, 4%; other n = 1, 1%). Most participants self-reported a diagnosis consistent with chronic primary pain (n = 57, 61%) and/or secondary musculoskeletal pain (n = 57, 61%), followed by neuropathic pain (n = 18, 19%). A smaller proportion of participants reported secondary visceral pain (n = 7, 7%), cancer-related pain (n = 2, 2%), posttraumatic / post-surgical pain (n = 1, 1%), and/or secondary headache / orofacial pain (n = 1, 1%). Forty-two percent of participants were taking opioid medications. Additional details including CONSORT diagram, subject BMI, baseline pain levels, and ratings of blanket pleasantness are reported in Baumgartner et al., 2021.
Randomization and Blinding
Randomization with allocation concealment was performed to assign participants to two weighted blanket groups of equal size. Males and females were randomized with replacement across a list of 200 codes using an Excel-based random number generator. Both investigators and participants were blinded, except for the research coordinator who performed random assignment. Investigators were unblinded before data analysis. While it was impossible to conceal the heaviness of either blanket from participants, all participants were told they would be receiving a “weighted blanket” and that various weights would be used in the study.
Weighted Blankets
Participants were randomly assigned to receive a 15-pound [lb; 6.8 kilograms (kg)], “deep pressure” weighted blanket or a 5-lb (2.3 kg) “light pressure” weighted blanket to use at home overnight for 7 nights. The light pressure weighted blanket served as an active control for widespread body sensation and blanket-related positive outcome expectancies. All blankets were twin-size, grey, cotton-polyester-blend, and weighted with hypoallergenic glass beads that distributed pressure across the body (SensaCalm, Chattanooga, TN).
Ecological Momentary Assessment (EMA)
A smartphone-based EMA application remotely guided participants through the study and captured self-report ratings (see EMA items) (Depp et al., 2016; Kaufmann et al., 2016; Moore et al., 2017). EMA assessments were conducted in the LifeData® System (www.lifedatacorp.com), a HIPAA compliant web-based system designed for human subjects research.
Self-Report Measurements
Sociodemographic and Health Variables
Age, sex, race, height, weight, chronic pain diagnosis, and medication use were assessed in REDCap. Three physicians at UC San Diego categorized diagnoses of chronic pain and medications based on published standards (Di Lernia et al., 2020; Treede et al., 2015; Treede et al., 2019).
Social Connectedness
Social connectedness – a measure of how individuals tend to cognitively appraise interpersonal closeness and belongingness with others in their social world – was measured using the Social Connectedness Scale - Revised (SCS-R) (Lee et al., 2001). The SCS-R consists of 20 items, including “I am able to connect with other people,” and “I feel comfortable in the presence of strangers,” (positively worded items), as well as “I don’t feel related to most people,” and “I feel disconnected from the world around me” (negatively worded items). Responses were made on a 6-point Likert scale ranging from 1 (strongly disagree) to 6 (strongly agree). A composite sum was calculated with higher values indicating greater social connectedness (Baseline α = .96, Post-intervention α = .97). A SCS-R sum of 70 or lower is considered “low” in social connectedness, or more socially disconnected (Lee et al., 2001).
Chronic Pain Intensity and Interference
The Pain, Enjoyment of Life, and General Activity Scale (PEG) (Krebs et al., 2009) is a three-item questionnaire derived from the Brief Pain Inventory (Cleeland & Ryan, 1994) that measures global chronic pain intensity (“What number best describes your pain on average in the past week”), as well as pain interference with enjoyment of life (“What number best describes how, during the past week, pain has interfered with your enjoyment of life”) and general activities (“What number best describes how, during the past week, pain has interfered with your general activity”). Participants made responses based on the last week using an 11-point scale ranging from 0 = no pain / does not interfere to 10 = pain as bad as you can imagine / completely interferes, respectively. Items were averaged into a total score with higher values indicating chronic greater pain intensity and interference (Baseline α = .89, Post-intervention α = .90).
Anxiety and Depression
The Patient-Reported Outcomes Measurement Information System (PROMIS) (Gershon et al., 2010) developed by the National Institutes of Health provides a brief (29-items) and comprehensive assessment of general physical and mental health and functioning across 7 domains. Participants rated items on a 5-point scale based on their experience during the past 7 days. The domains included in the present study were anxiety (“I felt fearful”; Baseline α = .90, Post-intervention α = .89) and depression (“I felt worthless”; Baseline α = .91, Post-Intervention α = .93). Items are summed into a composite score with higher values indicating worse anxiety or depressive symptoms.
Loneliness
The UCLA Loneliness Scale (Russell, 1996; Russell et al., 1978) is a 20-item scale that measures subjective feelings of loneliness and social isolation. Participants rated items such as “I have nobody to talk to” and “I feel completely alone” on a 4-point scale ranging from 0 = I never feel this way to 3 = I often feel this way. The total score is the sum of all items with higher scores indicating greater loneliness (Baseline α = .96, Post-intervention α = .96). Loneliness was used as a covariate in analyses due to its common association with the social connectedness construct, in that both measure a subjective experience of social relationships. Both constructs have been found to be highly correlated in past research (r = −.80) (Lee et al., 2001), as well as in the current sample (r = −.71, p < .01 at baseline; r = −.52, p < .01 over time). Thus, we attempted to isolate the unique features of social connectedness on outcomes above and beyond the effects of loneliness.
EMA item
EMA item measuring blanket-related expectations for pain relief (“Please rate how you expect the weighted blanket will affect your pain, if at all”) was sent to participants’ personal smartphones using the LifeData® System. The item was displayed on a 100-point visual analog scale (VAS) ranging from 1 = “increase pain a lot / not at all” to 100 = “decrease pain a lot / all of the night,” respectively. Visual analog scales appeared on participants’ smartphone devices and moved horizontally via tapping from left to right. Numerical values were not visible to participants. Additional ratings were collected that were not included in the present analyses.
Procedure
The present study reports measures from the Baseline session (originally “session 1”) and 7-day Post-intervention session (originally “session 3”) of the original study.
Baseline
During the Baseline session, participants self-reported sociodemographic information, and completed social connectedness, chronic pain, anxiety, depression, and loneliness measures. Upon completion, the research coordinator randomized participants to receive a deeper or a lighter pressure weighted blanket by mail. Participants were instructed to sleep normally for three nights of baseline data collection (ratings and fitness tracker sleep measure; data reported in Baumgartner et al., 2021) while awaiting their blanket. After receiving their blanket, they were instructed to provide an EMA rating of their expectation of pain relief from its use. They then rated pain intensity, anxiety and blanket pleasantness while lying down for 15min with and without the weighted blanket, wearing the fitness tracker (data elsewhere in Baumgartner et al., 2021).
Post-intervention
Immediately after completing the seventh day of overnight blanket use, participants were asked to complete Post-intervention assessments, which included the same measures of social connectedness, chronic pain, anxiety, depression, and loneliness as in the Baseline session, as well as pain medication use. Debriefing was conducted one week after study completion and included study purpose, blanket weights, and summary of study findings.
Statistical Analyses
Normality assumptions were affirmed using the skewness and kurtosis indices for continuous variables of interest. All variables were within normal ranges, justifying the use of parametric tests. Assumptions for ordinary least squares regression (OLS; i.e., normality; linearity; absence of multicollinearity; homoscedasticity) were met. A significance criterion of p < .05 was employed for all analyses.
Bivariate correlation analyses examined basic relationships of social connectedness with chronic pain, anxiety, and depression at baseline and at 1-week (“Post-intervention”). OLS regression further examined the contribution of baseline social connectedness to baseline pain, as well as to two potential mediators (anxiety and depression, in separate models). Regression models were run both with and without important sociodemographic and health variables including age, gender, race, opioid medication use, and loneliness. To assess the relative importance of social connectedness compared to the other tested covariates, we also implemented a Shapley value regression. A Shapley value regression computes all possible combinations of the independent variables within a model, and then measures the extent of contribution of each variable to the total R2 by observing changes associated with the addition or subtraction of each variable (Budescu, 1993). An advantage of this technique is that it determines the percentage of variance attributed to each independent variable after accounting for multicollinearity. See the following papers for further description and applications (Covert & Lee, 2021; Israeli, 2007; Lipovetsky & Conklin, 2001; Okhrati & Lipani, 2021; Smith & Alvarez, 2021).
Mediation models tested for an indirect effect of social connectedness on pain via anxiety and depression, tested in separate models. Models were estimated with an OLS regression path analytic framework implemented in the SPSS PROCESS Macro Version 3.4 (Model 4) (Hayes & Rockwood, 2017; Preacher & Hayes, 2004). Significance of indirect effects was predicated on bias-corrected bootstrapped approximations with 5,000 iterations and 95% bias-corrected confidence intervals. We controlled for anxiety or depression when considering either mediator, to determine the unique contribution of each mediator in supporting social connectedness and pain linkages. Additionally, the model was run both with and without controlling for relevant sociodemographic, health, loneliness, and baseline variables.
Finally, we tested the moderation of the effect of blanket on pain reductions by baseline social connectedness. Moderation analysis was implemented in SPSS in the PROCESS extension (Model 1) to explore the boundary conditions by which blanket pressure influenced PEG pain reductions (i.e., Δ = Baseline - Post-intervention) as a function of baseline social connectedness, adjusting for baseline pain (PEG) scores. The model was tested both with and without the inclusion of covariates for blanket-related pain expectations (i.e., placebo effects), sociodemographic and health variables, and loneliness. The Johnson-Neyman technique (Hayes & Rockwood, 2017) identified the cutoff value below which social connectedness played a significant conditional role in the effect of blanket pressure on pain reductions. We report the results of analyses with the inclusion of all covariates described above; all results were maintained when covariates were excluded.
Transparency and Openness
All analyses were conducted in SPSS Version 26 (IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp). The original study purpose, targeted condition, study design, and primary and secondary outcomes were pre-registered in ClinicalTrials.gov (NCT04447885: “Weighted Blankets and Chronic Pain”). The present study is a secondary analysis of this previously published work (Baumgartner et al., 2021), and thus was not pre-registered. Sample size determination was based on previous studies of weighted blankets for anxiety (Chen et al., 2013) and sleep (Ackerley et al., 2015) and was calculated using G*power version 3.1.9.7 as further described in the original study (Baumgartner et al., 2021). A version of the dataset and syntax used to produce the results in the current study can be found on the following link from Open Science Framework (OSF): tinyurl.com/SCSBlanket.
Results
Higher social connectedness is associated with lower chronic pain, anxiety, and depression
At baseline, higher social connectedness ratings were significantly correlated with lower chronic pain scores (PEG) (r = −.26, p < .05; see Figure 1), anxiety (r = −.61, p < .01), and depression (r = −.63, p< .01) (moderate to large effect sizes; Table 1). The predictive utility of baseline social connectedness on pain (see appendix Table A2), anxiety (appendix Table A4), and depression (appendix Table A6) remained significant after controlling for age, gender, race, opioid use, and baseline loneliness, with social connectedness accounting for 42.9% of the variance in PEG scores, 55% in anxiety scores, and 51% in depression scores relative to the other independent variables in each respective model. This same pattern of results was maintained at Post-intervention (moderate to large effect sizes; see appendix tables A1, A3, A5 and A7).
Figure 1. Negative correlation between baseline social connectedness and chronic pain.
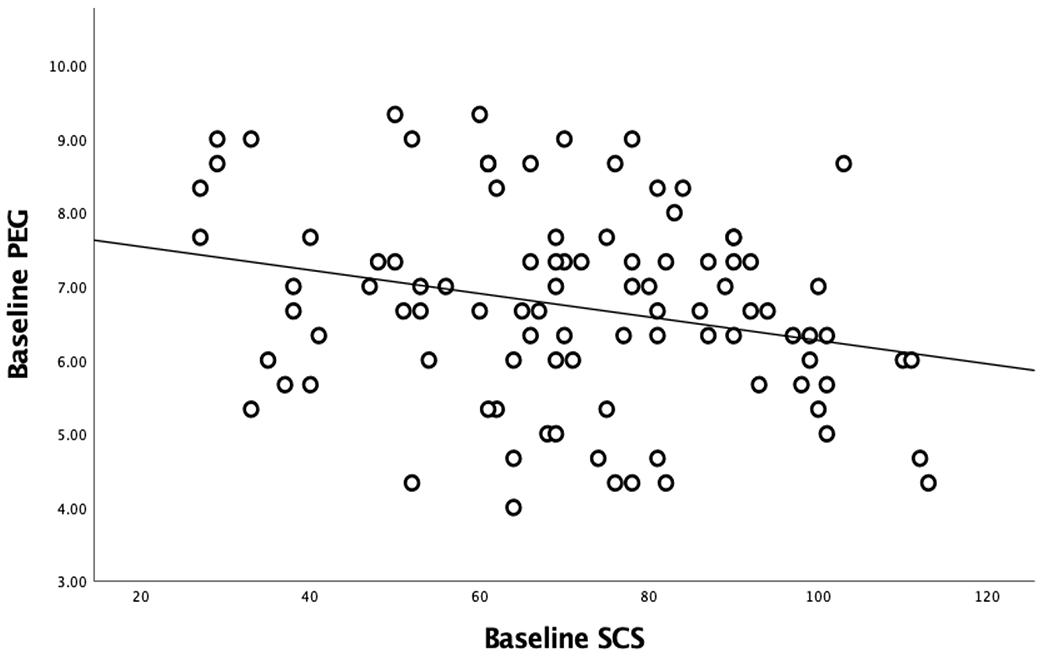
Bivariate correlation analysis revealed that greater social connectedness ratings were significantly associated with lower PEG pain scores, r = −.26, p < .05.
Table 1.
Descriptive statistics and bivariate correlations among Baseline variables.
| Variable | M | SD | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|---|
| 1. SCS | 71.08 | 21.57 | – | |||
| 2. PEG | 6.73 | 1.33 | −.26 * | – | ||
| 3. Anxiety | 6.92 | 3.45 | −.61 ** | −.56** | – | |
| 4. Depression | 6.46 | 4.21 | −.63 ** | .45** | .74** | – |
Note.
p < .05,
p < .01.
SCS = Social Connectedness Scale, PEG = Pain, Enjoyment of Life and General Activity Scale.
Anxiety, but not depression, mediates the association between baseline social connectedness and chronic pain
Mediation analyses tested for an indirect effect of social connectedness on chronic pain (PEG scores) via anxiety and depression, separately. As can be seen in Figure 2A, at Baseline, the hypothesized indirect effect of social connectedness on pain via anxiety was significant, such that greater social connectedness was associated with lower anxiety, which in turn predicted lower PEG pain scores. In contrast, depression did not emerge as a significant mediator in our models (indirect effects, p > .05; Figures 2B). The same pattern of results was obtained when no baseline or demographic covariates were included in the model.
Figure 2. Mediation analyses between social connectedness and pain.
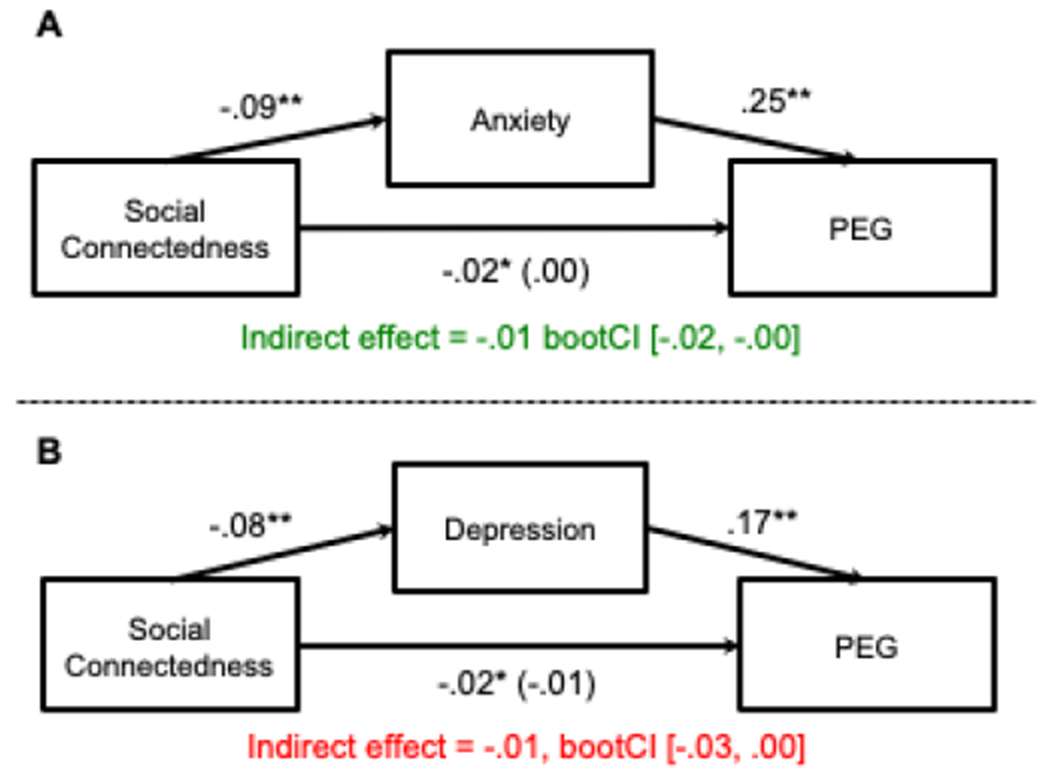
(A) The hypothesized negative association between baseline social connectedness ratings and PEG pain scores was significantly mediated by anxiety, as indicated by a non-zero bootstrapped confidence interval. Greater levels of social connectedness were associated with lower anxiety, which in turn, predicted lower pain. Values are unstandardized coefficients from OLS regression after controlling for age, sex, race, opioid medication use, baseline loneliness, and baseline depression. Standard errors are represented in parentheses. Significance of indirect effects was predicated on bias-corrected bootstrapped approximations with 5,000 iterations and 95% bias-corrected confidence intervals. Asterisks indicate significance paths at the *p < .05 and **p < .01 levels. (B) The hypothesized negative association between baseline social connectedness ratings and PEG pain scores was not significantly mediated by depression, as indicated by a bootstrapped confidence interval that included zero.
Deep pressure provides greater pain relief than light pressure in socially disconnected individuals
Social connectedness significantly moderated the effect of the weighted blanket on PEG pain reductions, even after loneliness was included as a covariate (−1SD = 49.45, b = −1.18, SEM = .42, p = .01, 95% CI [−2.01, −0.35]). As shown in Figure 3, within participants who reported the lowest social connectedness at baseline, the deeper pressure blanket induced greater pain relief than the light pressure weighted blanket. In contrast, the deep and light pressure blankets provided comparable levels of pain relief for individuals higher in social connectedness. The Johnson-Neyman cutoff value for social connectedness was 66.55 (b = −.60, SEM = .30, p = .05). In the current sample, 41.49% of participants had social connectedness ratings below this value. The same pattern of results was obtained when no baseline or demographic covariates were included in the model.
Figure 3. Baseline social connectedness significantly moderates the association between blanket pressure and chronic pain reductions.
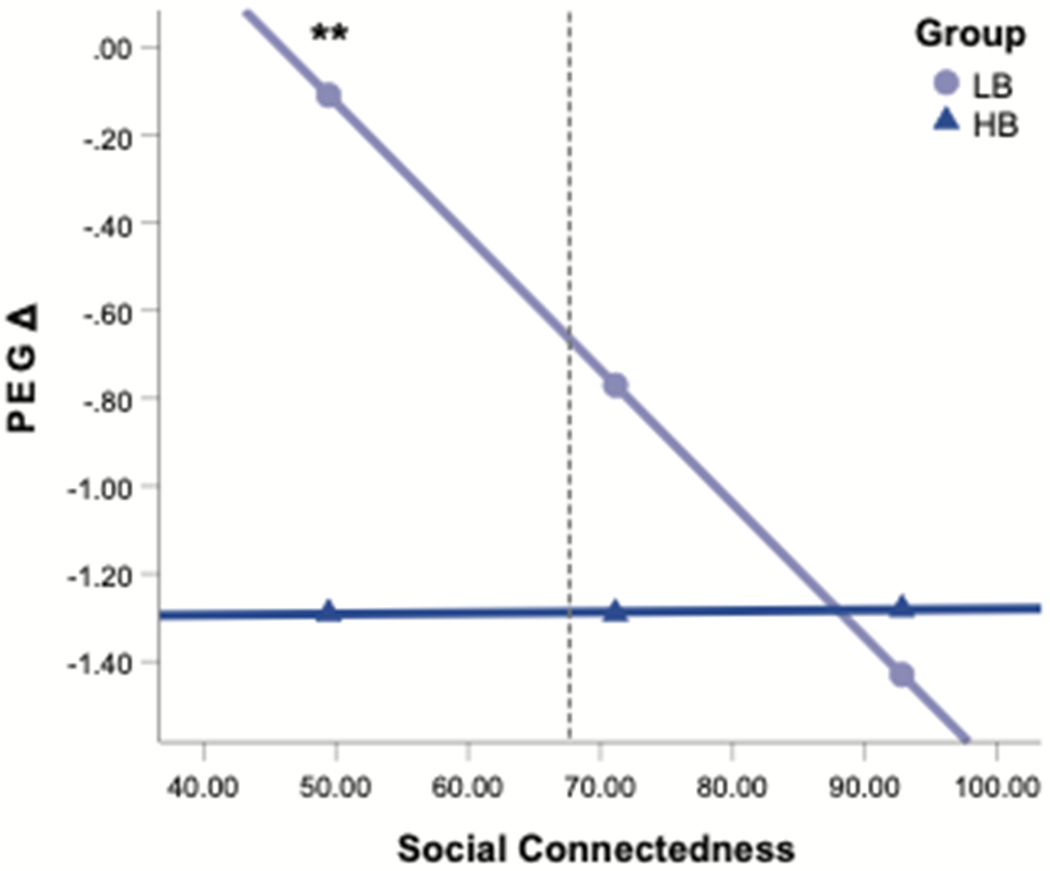
There was a significant interaction between weighed blanket group and baseline social connectedness reductions in predicting PEG pain reductions from Baseline to Post-intervention. Post hoc tests revealed that PEG reductions were significantly greater in the deep pressure weighted blanket group [“heavy blanket” (HB); dark blue line] for chronic pain patients who reported a “low” level of social connectedness (−1SD = 49.45) at baseline. PEG reductions were relatively unchanged in the light pressure weighted blanket group [“light blanket” (LB); light blue line) in those who reported low social connectedness at baseline. The dotted grey line represents the exact value (66.55) of social connectedness where the conditional effect was no longer significant. Values are displayed after adjusting for age, sex, race, opioid use, loneliness, blanket-related pain expectations, and baseline PEG scores. Asterisks indicate significance difference at the **p < .01 level.
Discussion
Social isolation, rejection, and loneliness are known to amplify pain, but the effect of individual differences in social connectedness – a tendency to perceive closeness and belongingness with others – on chronic pain has not been rigorously studied. The current study conducted a secondary analysis of social connectedness and pain ratings in patients with chronic pain and assessed the role of social connectedness in the pain-reducing effects of deep pressure after 1-week overnight use of a weighted blanket. Our previous study demonstrated greater pain reduction from the deep pressure (15-lb.) weighted blanket relative to the light pressure (5-lb.) placebo control weighted blanket (Baumgartner et al., 2021). The current analysis demonstrates a significant negative association between social connectedness and chronic pain scores, as well a greater effect of the deeper pressure blanket on pain relief for individuals who were most socially disconnected. These effects reveal close linkages between pain and the tendency to feel connected or close with other people, as well as the relevance of social connectedness in the outcome of sensory-affective interventions for chronic pain.
The present study contributes to a growing appreciation of the relevance of social processes to pain and provides the first evidence to our knowledge of associations between individual differences in social connectedness and the experience of pain. At baseline, chronic pain patients who reported higher social connectedness provided lower ratings of chronic pain, anxiety, and depression. Importantly, social connectedness consistently accounted for the majority of variance in our models predicting pain, anxiety, and depression, compared to other baseline variables, including loneliness – a construct strongly negatively correlated with social connectedness – situating itself as a robust predictor of pain and mental health. This suggests a need for broader inclusion of measures that capture both positive and negative social factors in research attempting to elucidate affective contributions to the experience of chronic pain, capturing both pain amplifying and pain buffering effects.
Our results contribute to an emerging understanding of psychosocial context on pain by demonstrating anxiety as a mediator for the association between social connectedness and pain. This finding is consistent with previous research demonstrating positive correlations between pain and trait anxiety (Cioffi et al., 2016; James & Hardardottir, 2002; Tang & Gibson, 2005), state anxiety (Tang & Gibson, 2005), and experimentally induced anxiety (Rhudy & Meagher 2000), as well as research showing negative correlations between social connectedness and anxiety (Lee & Robbins, 1995; Malaquias et al., 2015). Anxiety is a future-oriented emotion characterized by negative affect and anticipation of potential threats, resulting in hypervigilance, tension, and environmental and interoceptive scanning that facilitates sensory receptivity. Anxiety is thought to augment pain through mechanisms such as enhanced attention (hypervigilance) and monitoring for salient events like pain (Rhudy & Meagher 2000). It is possible that social connectedness provides a schema by which chronic pain patients may allocate attentional resources to somatic processes associated with enhanced well-being, environmental predictability, and homeostatic processes (Khalsa & Lapidus, 2016). Moreover, social connectedness is known to have a reciprocal relationship with positive affect leading to an “upward spiral” of positive affect and close connections (Ramsey & Gentzler, 2015). It is possible that the propensity toward disconnection increases anxiety, initiating a “downward spiral” that increases the difficulty of developing and maintaining social connections. The increased anxiety produced from this downward spiral could then result in further increases in the perception and maintenance of pain. Recent work showing trait anxiety as a mediator between clinical pain and health-related quality of life in fibromyalgia (Galvez-Sánchez et al., 2020) additionally points to a broad role of anxiety in mediating relationships between pain and well-being. The influence of social connectedness on pain via anxiety may also be due to the role of social connectedness in assuaging threat appraisals generally, thereby reducing feelings of anxiety that amplify pain-related appraisals (Cacioppo & Hawkley, 2009; Watson & Clark, 1984; Adler-Neal et al., 2019; Leino & Magni, 1993; Ploghaus et al., 2001; Rhudy & Meagher, 2000; van den Hout et al., 2001). The fact that depression did not emerge as a significant mediator in the current study is noteworthy, and further suggests a threat and arousal-related regulatory or monitoring mechanism may mediate associations between perceptions of closeness and chronic pain specifically.
Another novel contribution of the present research is the finding that chronic pain patients in the current sample that reported the highest level of social disconnection required greater pressure from the weighted blanket to experience pain relief. The effect of the weighted blanket contributes to findings showing that deep pressure is associated with reductions in anxiety and increases in positive affect (Case et al., 2020; Field et al., 2010; Chen et al., 2013; Champagne et al., 2015), reductions in pain (Baumgartner et al., 2021; Field et al., 2002; Law et al., 2008; Honigman et al., 2016), and the effects of social-affective touch inputs in reducing negative social experiences generally (Heatley Tejada et al., 2020; Tai et al., 2011; von Mohr et al., 2017).
Touch is thought to serve, in a large part, to communicate discrete emotions (Morrison et al., 2010; Hertenstein et al., 2006), and can also serve as a source of semantic meaning for abstract concepts (Gibbs Jr et al., 2004). For example, the act of carrying physical weight is associated with processing the concept of “importance” (Zhang & Li, 2012). It is possible that deep pressure from a weighted blanket fosters an embodied, symbolic form of social support that communicates concepts and emotions associated with safety, security, and closeness (Eisenberger et al., 2011; Hertenstein et al., 2006; von Mohr et al., 2017), thereby reducing pain-related appraisals in individuals that feel the greatest disconnection within their social environment. Individuals who lack social connection may be most receptive to these processes as they are more likely to attempt to compensate for a lack of closeness by creating connection with inanimate objects (Epley et al., 2008), some of which have been shown to mitigate the negative effects of social disconnection (Tai et al 2011). Interestingly, social disconnection evoked by a social exclusion manipulation is also associated with the phenomenological experience of “coldness” and increased desire for warmth (Zhong & Leonardelli, 2008). Conversely, social connection manipulations evoke feelings of warmth (Inagaki & Eisenberger, 2013) and engage neural circuitry overlapping both representations of CT-optimal and deep pressure touch (mid and posterior insula; somatosensory cortices: Case 2020). CT afferents respond optimally to dynamic touch around 32°C (Ackerley et al., 2014; Vallbo et al., 1999), further supporting the idea that social-affective touch – perhaps including deep pressure – may provide a kind of “warm” social support in this context, and potentially in those who feel the greatest disconnection. It will be important for future research to distinguish between pain reduction effects attributed to the direct sensory experience of physical weight or deep pressure compared to effects generated from predictable and stable signatures of symbolic associations, or the upregulation of positive affect and other hedonic feelings and their psychosocial consequences.
Constraints on generalizability
We note several study limitations in the original report (see Baumgartner et al., 2021) that apply to the current secondary analysis. In addition to these limitations, it is noteworthy that the current sample consisted predominately of female and White persons, which limits generalizability to other gender, racial, and ethnicity groups who may be more susceptible to feelings of social disconnection, resulting in part from stigma and isolation from structural racism, discrimination, and other social determinants of health in pain management (Todd et al., 1994; Todd et al., 1993; Hoffman et al., 2016; Mossey, 2011). We maintain that weighted blankets are a relatively inexpensive and accessible tool for chronic pain relief that have the potential to benefit the unique needs of numerous people in an equitable manner. Future research should strive for more inclusive samples to better distinguish who may (or may not) benefit from such complementary interventions.
Conclusion
In conclusion, the present secondary analysis revealed a negative correlation between social connectedness and chronic pain, mediated by anxiety. We further demonstrated that chronic pain patients with a tendency toward low social connection benefited more from deeper pressure provided by a weighted blanket. These findings have important implications in the fields of health psychology, pain medicine, and rehabilitation science by providing additional evidence that individual differences in social processes are fundamental, not peripheral, to the experience and expression of pain. Psychosocial interventions that target the social-affective consequences of pleasant touch may make a meaningful contribution to chronic pain sufferers, especially those most vulnerable.
Disclosures:
This work was supported by UC San Diego Health and the National Center for Complementary and Integrative Health – National Institutes of Health (R00-AT009466, F32-AT010843). The authors have no conflicts of interest to disclose. A version of the dataset and syntax used to produce the results in the current study can be found on the following link from Open Science Framework (OSF): https://osf.io/rujah/?view_only=3702d451ebf74ec9a21f695ce3dbd26f
Table A1.
Descriptive statistics and bivariate correlations among Post-intervention ratings.
| Variable | M | SD | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|---|
| 1. SCS | 73.48 | 23.08 | – | |||
| 2. PEG | 5.71 | 1.79 | −.36 ** | – | ||
| 3. Anxiety | 6.31 | 3.47 | −.53 ** | .38** | – | |
| 4. Depression | 5.64 | 4.33 | −.54 ** | .45** | .73** | – |
Note.
p < .05,
p < .01.
SCS = Social Connectedness Scale, PEG = Pain, Enjoyment of Life and General Activity Scale.
Table A2.
Results of the multiple regression analysis for variables predicting baseline chronic pain intensity and interference (PEG) scores.
| Variable | B | β | t | Shapley R2 | p |
|---|---|---|---|---|---|
| Age | .00 | .02 | .16 | .29% | .88 |
| Gender | .38 | .14 | 1.33 | 8.52% | .19 |
| Race | −.30 | −.16 | −1.59 | 14.35% | .12 |
| Opioid use | .55 | .20 | 1.96 | 19.63% | .05 |
| Baseline loneliness | −.01 | −.05 | −.35 | 14.30% | .73 |
| Baseline social connectedness | −.02 | −.35 | −2.40 | 42.90% | .02 |
Note. R2 for the full model = .14 (N = 94, p = .03).
PEG = Pain, Enjoyment of Life and General Activity Scale.
Gender was coded as 1 = female, 2 = male, 3 = unspecified. Opioid use was coded as 0 = not currently taking opioid medications, 1 = currently taking opioid medications.
Table A3.
Results of the multiple regression analysis for variables predicting Post-intervention chronic pain intensity and interference (PEG) scores.
| Variable | B | β | t | Shapley R2 | p |
|---|---|---|---|---|---|
| Age | .02 | .13 | 1.37 | 5.82% | .18 |
| Gender | .24 | .07 | .67 | .70% | .50 |
| Race | −.57 | −.23 | −2.38 | 14.89% | .02 |
| Opioid use | .87 | .24 | 2.51 | 17.52% | .01 |
| Group | −.32 | −.09 | −.94 | 2.09% | .35 |
| Post-intervention loneliness | .00 | .00 | .03 | 14.36% | .98 |
| Post-intervention social connectedness | −.03 | −.44 | −3.57 | 44.61% | .00 |
Note. R2 for the full model = .27 (N = 94, p < .001).
PEG = Pain, Enjoyment of Life and General Activity Scale.
Gender was coded as 1 = female, 2 = male, 3 = unspecified. Opioid use was coded as 0 = not currently taking opioid medications, 1 = currently taking opioid medications. Group was coded as 0 = light pressure weighted blanket, 1 = deeper pressure weighted blanket.
Table A4.
Results of the multiple regression analysis for variables predicting baseline anxiety scores.
| Variable | B | β | t | Shapley R2 | p |
|---|---|---|---|---|---|
| Age | −.05 | −.17 | −1.99 | 7.29% | .05 |
| Gender | .78 | .11 | 1.34 | 3.70% | .19 |
| Race | −.70 | −.14 | −1.77 | 3.05% | .08 |
| Opioid use | .72 | .10 | 1.24 | 1.28% | .22 |
| Baseline loneliness | .03 | .13 | 1.07 | 29.67% | .29 |
| Baseline social connectedness | −.09 | −.54 | −4.60 | 55.00% | .00 |
Note. R2 for the full model = .45 (N = 94, p < .001).
Gender was coded as 1 = female, 2 = male, 3 = unspecified. Opioid use was coded as 0 = not currently taking opioid medications, 1 = currently taking opioid medications.
Table A5.
Results of the multiple regression analysis for variables predicting Post-Intervention anxiety scores.
| Variable | B | β | t | Shapley R2 | p |
|---|---|---|---|---|---|
| Age | −.04 | −.14 | −1.54 | 5.91% | .13 |
| Gender | .40 | .06 | .62 | 1.20% | .54 |
| Race | −.76 | −.15 | −1.70 | 5.49% | .09 |
| Opioid use | .31 | .04 | .48 | 1.10% | .63 |
| Group | −.45 | −.07 | −.74 | 1.71% | .46 |
| Post-intervention loneliness | .06 | .28 | 2.40 | 39.69% | .02 |
| Post-intervention social connectedness | −.06 | −.37 | −3.20 | 44.90% | .00 |
Note. R2 for the full model = .39 (N = 90, p < .001).
Gender was coded as 1 = female, 2 = male, 3 = unspecified. Opioid use was coded as 0 = not currently taking opioid medications, 1 = currently taking opioid medications. Group was coded as 0 = light pressure weighted blanket, 1 = deeper pressure blanket.
Table A6.
Results of the multiple regression analysis for variables predicting baseline depression scores.
| Variable | B | β | t | Shapley R2 | p |
|---|---|---|---|---|---|
| Age | −.03 | −.09 | −1.08 | 2.04% | .29 |
| Gender | −.07 | −.01 | −.09 | .69% | .93 |
| Race | .67 | .11 | 1.40 | 3.52% | .17 |
| Opioid use | .19 | .02 | .27 | 1.43% | .79 |
| Baseline loneliness | .09 | .31 | 2.65 | 41.31% | .01 |
| Baseline social connectedness | −.08 | −.40 | −3.41 | 51.01% | .00 |
Note. R2 for the full model = .46 (N = 94, p < .001).
Gender was coded as 1 = female, 2 = male, 3 = unspecified. Opioid use was coded as 0 = not currently taking opioid medications, 1 = currently taking opioid medications.
Table A7.
Results of the multiple regression analysis for variables predicting Post-Intervention depression scores.
| Variable | B | β | t | Shapley R2 | p |
|---|---|---|---|---|---|
| Age | −.02 | −.07 | −.77 | 1.44% | .44 |
| Gender | −.18 | −.02 | −.23 | .31% | .82 |
| Race | −.23 | −.04 | −.41 | .61% | .68 |
| Opioid use | −.11 | −.01 | −.14 | 2.08% | .89 |
| Group | −.22 | −.02 | −.28 | .63% | .78 |
| Post-intervention loneliness | .10 | .36 | 3.06 | 49.52% | .00 |
| Post-intervention social connectedness | −.06 | −.31 | −2.68 | 45.41% | .01 |
Note. R2 for the full model = .38 (N = 90, p < .001).
Gender was coded as 1 = female, 2 = male, 3 = unspecified. Opioid use was coded as 0 = not currently taking opioid medications, 1 = currently taking opioid medications. Group was coded as 0 = light pressure weighted blanket, 1 = deep pressure weighted blanket.
References
- Ackerley R, Badre G, & Olausson H (2015). Positive effects of a weighted blanket on insomnia. Journal of Sleep Medicine & Disorders, 2(3), 1–7. [Google Scholar]
- Ackerley R, Wasling HB, Liljencrantz J, Olausson H, Johnson RD, & Wessberg J (2014). Human C-tactile afferents are tuned to the temperature of a skin-stroking caress. Journal of Neuroscience, 34(8), 2879–2883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adler-Neal AL, Emerson NM, Farris SR, Jung Y, Coghill RC, & Zeidan F (2019). Brain moderators supporting the relationship between depressive mood and pain. Pain, 160(9), 2028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Åsbring P, & Närvänen A-L (2002). Women’s experiences of stigma in relation to chronic fatigue syndrome and fibromyalgia. Qualitative health research, 12(2), 148–160. [DOI] [PubMed] [Google Scholar]
- Bannon S, Greenberg J, Mace RA, Locascio JJ, & Vranceanu A-M (2021). The role of social isolation in physical and emotional outcomes among patients with chronic pain. General Hospital Psychiatry, 69, 50–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumeister RF, & Leary MR (1995). The need to belong: desire for interpersonal attachments as a fundamental human motivation. Psychological bulletin, 117(3), 497. [PubMed] [Google Scholar]
- Baumgartner JN, Haupt MR, & Case LK (2022). Social Connectedness & Weighted Blanket Study. Retrieved from https://osf.io/rujah/?view_only=3702d451ebf74ec9a21f695ce3dbd26f [Google Scholar]
- Baumgartner JN, Quintana D, Leija L, Schuster NM, Bruno KA, Castellanos JP, & Case LK (2021). Widespread Pressure Delivered by a Weighted Blanket Reduces Chronic Pain: A Randomized Controlled Trial. The Journal of Pain. [DOI] [PubMed] [Google Scholar]
- Bowlby J (1973). Attachment and loss: Volume II: Separation, anxiety and anger. In Attachment and loss: Volume II: Separation, anxiety and anger (pp. 1–429). London: The Hogarth press and the institute of psycho-analysis. [Google Scholar]
- Brown JL, Sheffield D, Leary MR, & Robinson ME (2003). Social support and experimental pain. Psychosomatic medicine, 65(2), 276–283. [DOI] [PubMed] [Google Scholar]
- Budescu DV (1993). Dominance analysis: a new approach to the problem of relative importance of predictors in multiple regression. Psychological bulletin, 114(3), 542. [Google Scholar]
- Bungert M, Koppe G, Niedtfeld I, Vollstädt-Klein S, Schmahl C, Lis S, & Bohus M (2015). Pain processing after social exclusion and its relation to rejection sensitivity in borderline personality disorder. PLoS One, 10(8), e0133693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, & Hawkley LC (2009). Perceived social isolation and cognition. Trends in cognitive sciences, 13(10), 447–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cascio CJ, Moore D, & McGlone F (2019). Social touch and human development. Developmental cognitive neuroscience, 35, 5–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case LK, Liljencrantz J, McCall MV, Bradson M, Necaise A, Tubbs J, … Bushnell MC (2021). Pleasant deep pressure: expanding the social touch hypothesis. Neuroscience, 464, 3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Champagne T, Mullen B, Dickson D, & Krishnamurty S (2015). Evaluating the safety and effectiveness of the weighted blanket with adults during an inpatient mental health hospitalization. Occupational Therapy in Mental Health, 31(3), 211–233. [Google Scholar]
- Chen HY, Yang H, Chi HJ, & Chen HM (2013). Physiological effects of deep touch pressure on anxiety alleviation: The weighted blanket approach. Journal of Medical and Biological Engineering, 33(5), 463–470. [Google Scholar]
- Chester DS, DeWall CN, & Pond RS (2016). The push of social pain: Does rejection’s sting motivate subsequent social reconnection? Cognitive, Affective, & Behavioral Neuroscience, 16(3), 541–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covert I, & Lee SI (2021, March). Improving KernelSHAP: Practical Shapley value estimation using linear regression. In International Conference on Artificial Intelligence and Statistics (pp. 3457–3465). PMLR. [Google Scholar]
- Cioffi I, Michelotti A, Perrotta S, Chiodini P, & Ohrbach R (2016). Effect of somatosensory amplification and trait anxiety on experimentally induced orthodontic pain. European journal of oral sciences, 124(2), 127–134. [DOI] [PubMed] [Google Scholar]
- Cleeland C, & Ryan K (1994). Pain assessment: global use of the Brief Pain Inventory. Annals, academy of medicine, Singapore. [PubMed] [Google Scholar]
- Csupak B, Sommer JL, Jacobsohn E, & El-Gabalawy R (2018). A population-based examination of the co-occurrence and functional correlates of chronic pain and generalized anxiety disorder. Journal of anxiety disorders, 56, 74–80. [DOI] [PubMed] [Google Scholar]
- Davis DA, Luecken LJ, & Zautra AJ (2005). Are Reports of Childhood Abuse Related to the Experience of Chronic Pain in Adulthood?: A Meta-analytic Review of the Literature. The Clinical Journal of Pain, 21(5), 398–405. [DOI] [PubMed] [Google Scholar]
- Depp CA, Moore RC, Dev SI, Mausbach BT, Eyler LT, & Granholm EL (2016). The temporal course and clinical correlates of subjective impulsivity in bipolar disorder as revealed through ecological momentary assessment. Journal of affective disorders, 193, 145–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Lernia D, Lacerenza M, Ainley V, & Riva G (2020). Altered interoceptive perception and the effects of interoceptive analgesia in musculoskeletal, primary, and neuropathic chronic pain conditions. Journal of Personalized Medicine, 10(4), 201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diego MA, Field T, Sanders C, & Hernandez-Reif M (2004). Massage therapy of moderate and light pressure and vibrator effects on EEG and heart rate. International Journal of Neuroscience, 114(1), 31–44. [DOI] [PubMed] [Google Scholar]
- Dunbar RI (2010). The social role of touch in humans and primates: behavioural function and neurobiological mechanisms. Neuroscience & Biobehavioral Reviews, 34(2), 260–268. [DOI] [PubMed] [Google Scholar]
- Dunbar RI (2012). Bridging the bonding gap: the transition from primates to humans. Philosophical Transactions of the Royal Society B: Biological Sciences, 367(1597), 1837–1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberger NI (2012a). Broken hearts and broken bones: A neural perspective on the similarities between social and physical pain. Current Directions in Psychological Science, 21(1), 42–47. [Google Scholar]
- Eisenberger NI (2012b). The pain of social disconnection: examining the shared neural underpinnings of physical and social pain. Nature Reviews Neuroscience, 13(6), 421–434. [DOI] [PubMed] [Google Scholar]
- Eisenberger NI, Lieberman MD, & Williams KD (2003). Does rejection hurt? An fMRI study of social exclusion. Science, 302(5643), 290–292. [DOI] [PubMed] [Google Scholar]
- Eisenberger NI, Master SL, Inagaki TK, Taylor SE, Shirinyan D, Lieberman MD, & Naliboff BD (2011). Attachment figures activate a safety signal-related neural region and reduce pain experience. Proceedings of the National Academy of Sciences, 108(28), 11721–11726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epley N, Akalis S, Waytz A, & Cacioppo JT (2008). Creating social connection through inferential reproduction: Loneliness and perceived agency in gadgets, gods, and greyhounds. Psychological science, 19(2), 114–120. [DOI] [PubMed] [Google Scholar]
- Fidanza F, Polimeni E, Pierangeli V, & Martini M (2021). A better touch: C-tactile fibers related activity is associated to pain reduction during temporal summation of second pain. The Journal of Pain, 22(5), 567–576. [DOI] [PubMed] [Google Scholar]
- Field T, Diego M, Cullen C, Hernandez-Reif M, Sunshine W, & Douglas S (2002). Fibromyalgia pain and substance P decrease and sleep improves after massage therapy. JCR: Journal of Clinical Rheumatology, 8(2), 72–76. [DOI] [PubMed] [Google Scholar]
- Field T, Diego M, & Hernandez-Reif M (2010). Moderate pressure is essential for massage therapy effects. International Journal of Neuroscience, 120(5), 381–385. [DOI] [PubMed] [Google Scholar]
- Galvez-Sánchez CM, Montoro CI, Duschek S, & Del Paso GAR (2020). Depression and trait-anxiety mediate the influence of clinical pain on health-related quality of life in fibromyalgia. Journal of affective disorders, 265, 486–495. [DOI] [PubMed] [Google Scholar]
- Gershon RC, Rothrock N, Hanrahan R, Bass M, & Cella D (2010). The use of PROMIS and assessment center to deliver patient-reported outcome measures in clinical research. Journal of applied measurement, 11(3), 304. [PMC free article] [PubMed] [Google Scholar]
- Gibbs RW Jr, Lima PLC, & Francozo E (2004). Metaphor is grounded in embodied experience. Journal of pragmatics, 36(7), 1189–1210. [Google Scholar]
- Goldstein P, Weissman-Fogel I, Dumas G, & Shamay-Tsoory SG (2018). Brain-to-brain coupling during handholding is associated with pain reduction. Proceedings of the national academy of sciences, 115(11), E2528–E2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandin T (1992). Calming effects of deep touch pressure in patients with autistic disorder, college students, and animals. Journal of child and adolescent psychopharmacology, 2(1), 63–72. [DOI] [PubMed] [Google Scholar]
- Hayes AF, & Rockwood NJ (2017). Regression-based statistical mediation and moderation analysis in clinical research: Observations, recommendations, and implementation. Behaviour research and therapy, 98, 39–57. [DOI] [PubMed] [Google Scholar]
- Heatley Tejada A, Dunbar R, & Montero M (2020). Physical contact and loneliness: being touched reduces perceptions of loneliness. Adaptive human behavior and physiology, 6(3), 292–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hertenstein MJ, Keltner D, App B, Bulleit BA, & Jaskolka AR (2006). Touch communicates distinct emotions. Emotion, 6(3), 528–533. doi: 10.1037/1528-3542.6.3.528 [DOI] [PubMed] [Google Scholar]
- Hoffman KM, Trawalter S, Axt JR, & Oliver MN (2016). Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc Natl Acad Sci U S A, 113(16), 4296–4301. doi: 10.1073/pnas.1516047113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honigman L, Bar-Bachar O, Yarnitsky D, Sprecher E, & Granovsky Y (2016). Nonpainful wide-area compression inhibits experimental pain. Pain, 157(9), 2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughto JM, Restar AJ, Wolfe HL, Gordon LK, Reisner SL, Biello KB, … & Mimiaga MJ. (2021). Opioid pain medication misuse, concomitant substance misuse, and the unmet behavioral health treatment needs of transgender and gender diverse adults. Drug and alcohol dependence, 222, 108674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inagaki TK, & Eisenberger NI (2013). Shared neural mechanisms underlying social warmth and physical warmth. Psychological science, 24(11), 2272–2280. [DOI] [PubMed] [Google Scholar]
- Inagaki TK, Hazlett LI, & Andreescu C (2020). Opioids and social bonding: Effect of naltrexone on feelings of social connection and ventral striatum activity to close others. Journal of Experimental Psychology: General, 149(4), 732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inagaki TK, Ray LA, Irwin MR, Way BM, & Eisenberger NI (2016). Opioids and social bonding: naltrexone reduces feelings of social connection. Social Cognitive and Affective Neuroscience, 11(5), 728–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israeli O (2007). A Shapley-based decomposition of the R-square of a linear regression. The Journal of Economic Inequality, 5(2), 199–212. [Google Scholar]
- James JE, & Hardardottir D (2002). Influence of attention focus and trait anxiety on tolerance of acute pain. British journal of health psychology, 7(2), 149–162. [DOI] [PubMed] [Google Scholar]
- Jaremka LM, Andridge RR, Fagundes CP, Alfano CM, Povoski SP, Lipari AM, … Yee LD (2014). Pain, depression, and fatigue: loneliness as a longitudinal risk factor. Health Psychology, 33(9), 948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karayannis NV, Baumann I, Sturgeon JA, Melloh M, & Mackey SC (2019). The impact of social isolation on pain interference: a longitudinal study. Annals of Behavioral Medicine, 53(1), 65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufmann CN, Gershon A, Eyler LT, & Depp CA (2016). Clinical significance of mobile health assessed sleep duration and variability in bipolar disorder. Journal of psychiatric research, 81, 152–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalsa SS, & Lapidus RC (2016). Can interoception improve the pragmatic search for biomarkers in psychiatry?. Frontiers in psychiatry, 7, 121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koebner IJ, Fishman SM, Paterniti D, Sommer D, Witt CM, Ward D, & Joseph JG (2019). The art of analgesia: A pilot study of art museum tours to decrease pain and social disconnection among individuals with chronic pain. Pain Medicine, 20(4), 681–691. [DOI] [PubMed] [Google Scholar]
- Krahé C, Drabek MM, Paloyelis Y, & Fotopoulou A (2016). Affective touch and attachment style modulate pain: a laser-evoked potentials study. Philosophical Transactions of the Royal Society B: Biological Sciences, 371(1708), 20160009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krahé C, Springer A, Weinman JA, & Fotopoulou A (2013). The social modulation of pain: others as predictive signals of salience–a systematic review. Frontiers in human neuroscience, 7, 386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krebs EE, Lorenz KA, Bair MJ, Damush TM, Wu J, Sutherland JM, … Kroenke K (2009). Development and initial validation of the PEG, a three-item scale assessing pain intensity and interference. Journal of general internal medicine, 24(6), 733–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kucyi A, Moayedi M, Weissman-Fogel I, Goldberg MB, Freeman BV, Tenenbaum HC, & Davis KD (2014). Enhanced medial prefrontal-default mode network functional connectivity in chronic pain and its association with pain rumination. Journal of Neuroscience, 34(11), 3969–3975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lampe A, Doering S, Rumpold G, Sölder E, Krismer M, Kantner-Rumplmair W, Schubert C, & Söllner W (2003). Chronic pain syndromes and their relation to childhood abuse and stressful life events. Journal of Psychosomatic Research, 54(4), 361–367. [DOI] [PubMed] [Google Scholar]
- Law LAF, Evans S, Knudtson J, Nus S, Scholl K, & Sluka KA (2008). Massage reduces pain perception and hyperalgesia in experimental muscle pain: a randomized, controlled trial. The Journal of Pain, 9(8), 714–721. [DOI] [PubMed] [Google Scholar]
- Lee RM, Draper M, & Lee S (2001). Social connectedness, dysfunctional interpersonal behaviors, and psychological distress: Testing a mediator model. Journal of counseling psychology, 48(3), 310. [Google Scholar]
- Lee RM, & Robbins SB (1995). Measuring belongingness: The social connectedness and the social assurance scales. Journal of counseling psychology, 42(2), 232. [Google Scholar]
- Leino P, & Magni G (1993). Depressive and distress symptoms as predictors of low back pain, neck-shoulder pain, and other musculoskeletal morbidity: a 10-year follow-up of metal industry employees. Pain, 53(1), 89–94. [DOI] [PubMed] [Google Scholar]
- Liljencrantz J, Strigo I, Ellingsen DM, Krämer H, Lundblad LC, Nagi SS, … Olausson H (2017). Slow brushing reduces heat pain in humans. European Journal of Pain, 21(7), 1173–1185. [DOI] [PubMed] [Google Scholar]
- Lipovetsky S, & Conklin M (2001). Analysis of regression in game theory approach. Applied Stochastic Models in Business and Industry, 17(4), 319–330. [Google Scholar]
- Löken LS, Evert M, & Wessberg J (2011). Pleasantness of touch in human glabrous and hairy skin: order effects on affective ratings. Brain research, 1417, 9–15. [DOI] [PubMed] [Google Scholar]
- Löken LS, Wessberg J, McGlone F, & Olausson H (2009). Coding of pleasant touch by unmyelinated afferents in humans. Nature neuroscience, 12(5), 547–548. [DOI] [PubMed] [Google Scholar]
- López-Solà M, Geuter S, Koban L, Coan JA, & Wager TD (2019). Brain mechanisms of social touch-induced analgesia in females. Pain, 160(9), 2072–2085. [DOI] [PubMed] [Google Scholar]
- MacDonald G, & Leary MR (2005). Why does social exclusion hurt? The relationship between social and physical pain. Psychological bulletin, 131(2), 202. [DOI] [PubMed] [Google Scholar]
- Malaquias S, Crespo C, & Francisco R (2015). How do adolescents benefit from family rituals? Links to social connectedness, depression and anxiety. Journal of child and Family Studies, 24(10), 3009–3017. [Google Scholar]
- Maner JK, DeWall CN, Baumeister RF, & Schaller M (2007). Does social exclusion motivate interpersonal reconnection? Resolving the” porcupine problem.”. Journal of personality and social psychology, 92(1), 42. [DOI] [PubMed] [Google Scholar]
- Master SL, Eisenberger NI, Taylor SE, Naliboff BD, Shirinyan D, & Lieberman MD (2009). A picture’s worth: Partner photographs reduce experimentally induced pain. Psychological science, 20(11), 1316–1318. [DOI] [PubMed] [Google Scholar]
- McWilliams LA, Cox BJ, & Enns MW (2003). Mood and anxiety disorders associated with chronic pain: an examination in a nationally representative sample. Pain, 106(1-2), 127–133. [DOI] [PubMed] [Google Scholar]
- Mitchinson AR, Kim HM, Geisser M, Rosenberg JM, & Hinshaw DB (2008). Social connectedness and patient recovery after major operations. Journal of the American College of Surgeons, 206(2), 292–300. [DOI] [PubMed] [Google Scholar]
- Moore RC, Kaufmann CN, Rooney AS, Moore DJ, Eyler LT, Granholm E, … Scott J (2017). Feasibility and acceptability of ecological momentary assessment of daily functioning among older adults with HIV. The American Journal of Geriatric Psychiatry, 25(8), 829–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison I, Löken LS, Olausson H. The skin as a social organ. Exp Brain Res. 2010. Jul;204(3):305–14. doi: 10.1007/s00221-009-2007-y. Epub 2009 Sep 22. [DOI] [PubMed] [Google Scholar]
- Mossey JM (2011). Defining racial and ethnic disparities in pain management. Clin Orthop Relat Res, 469(7), 1859–1870. doi: 10.1007/s11999-011-1770-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson EE, & Panksepp J (1998). Brain substrates of infant–mother attachment: contributions of opioids, oxytocin, and norepinephrine. Neuroscience & Biobehavioral Reviews, 22(3), 437–452. [DOI] [PubMed] [Google Scholar]
- Okhrati R, & Lipani A (2021, January). A multilinear sampling algorithm to estimate shapley values. In 2020 25th International Conference on Pattern Recognition (ICPR) (pp. 7992–7999). IEEE. [Google Scholar]
- Olausson H, Cole J, Rylander K, McGlone F, Lamarre Y, Wallin BG, … & Vallbo Å. (2008). Functional role of unmyelinated tactile afferents in human hairy skin: sympathetic response and perceptual localization. Experimental brain research, 184(1), 135–140. [DOI] [PubMed] [Google Scholar]
- Oliveira VC, Ferreira ML, Morso L, Albert HB, Refshauge KM, & Ferreira PH (2015). Patients’ perceived level of social isolation affects the prognosis of low back pain. European Journal of Pain, 19(4), 538–545. [DOI] [PubMed] [Google Scholar]
- Pawling R, Cannon PR, McGlone FP, & Walker SC (2017). C-tactile afferent stimulating touch carries a positive affective value. PloS one, 12(3), e0173457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pawling R, Trotter PD, McGlone FP, & Walker SC (2017). A positive touch: C-tactile afferent targeted skin stimulation carries an appetitive motivational value. Biological Psychology, 129,186–194. [DOI] [PubMed] [Google Scholar]
- Ploghaus A, Narain C, Beckmann C, Wise R, Bantick S, Clare S, … Tracey I (2001). Anxiety increases perceived pain intensity: A hippocampal mechanism. Neuroimage, 13(6). [Google Scholar]
- Preacher KJ, & Hayes AF (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior research methods, instruments, & computers, 36(4), 717–731. [DOI] [PubMed] [Google Scholar]
- Ramsey MA, & Gentzler AL (2015). An upward spiral: Bidirectional associations between positive affect and positive aspects of close relationships across the life span. Developmental review, 36, 58–104. [Google Scholar]
- Rayner L, Hotopf M, Petkova H, Matcham F, Simpson A, & McCracken LM (2016). Depression in patients with chronic pain attending a specialised pain treatment centre: prevalence and impact on health care costs. Pain, 157(7), 1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddan MC, Young H, Falkner J, López-Solà M, & Wager TD (2020). Touch and social support influence interpersonal synchrony and pain. Social Cognitive and Affective Neuroscience, 15(10), 1064–1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhudy JL, & Meagher MW (2000). Fear and anxiety: divergent effects on human pain thresholds. Pain, 84(1), 65–75. [DOI] [PubMed] [Google Scholar]
- Russell D, Peplau LA, & Ferguson ML (1978). Developing a measure of loneliness. Journal of personality assessment, 42(3), 290–294. [DOI] [PubMed] [Google Scholar]
- Russell DW (1996). UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of personality assessment, 66(1), 20–40. [DOI] [PubMed] [Google Scholar]
- Santini ZI, Jose PE, Cornwell EY, Koyanagi A, Nielsen L, Hinrichsen C, … & Koushede V (2020). Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. The Lancet Public Health, 5(1), e62–e70. [DOI] [PubMed] [Google Scholar]
- Schmidt RD, Feaster DJ, Horigian VE, & Lee RM (2022). Latent class analysis of loneliness and connectedness in US young adults during COVID-19. Journal of clinical psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schweinhardt P, & Bushnell MC (2010). Pain imaging in health and disease—how far have we come?. The Journal of clinical investigation, 120(11), 3788–3797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith M, & Alvarez F (2021). Identifying mortality factors from Machine Learning using Shapley values–a case of COVID19. Expert Systems with Applications, 176, 114832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suvilehto JT, Glerean E, Dunbar RI, Hari R, & Nummenmaa L (2015). Topography of social touching depends on emotional bonds between humans. Proceedings of the National Academy of Sciences, 112(45), 13811–13816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tai K, Zheng X, & Narayanan J (2011). Touching a teddy bear mitigates negative effects of social exclusion to increase prosocial behavior. Social Psychological and Personality Science, 2(6), 618–626. [Google Scholar]
- Tang J, & Gibson SJ (2005). A psychophysical evaluation of the relationship between trait anxiety, pain perception, and induced state anxiety. The Journal of Pain, 6(9), 612–619. [DOI] [PubMed] [Google Scholar]
- Taylor CT, Pearlstein SL, Kakaria S, Lyubomirsky S, & Stein MB (2020). Enhancing social connectedness in anxiety and depression through amplification of positivity: preliminary treatment outcomes and process of change. Cognitive therapy and research, 44(4), 788–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor SE (2007). Social support.
- Tesarz J, Eich W, Treede R-D, & Gerhardt A (2016). Altered pressure pain thresholds and increased wind-up in adult patients with chronic back pain with a history of childhood maltreatment: A quantitative sensory testing study. PAIN, 157(8), 1799–1809. [DOI] [PubMed] [Google Scholar]
- Todd KH, Lee T, & Hoffman JR (1994). The effect of ethnicity on physician estimates of pain severity in patients with isolated extremity trauma. Jama, 271(12), 925–928. [PubMed] [Google Scholar]
- Todd KH, Samaroo N, & Hoffman JR (1993). Ethnicity as a risk factor for inadequate emergency department analgesia. Jama, 269(12), 1537–1539. [PubMed] [Google Scholar]
- Tomova L, Wang KL, Thompson T, Matthews GA, Takahashi A, Tye KM, & Saxe R (2020). Acute social isolation evokes midbrain craving responses similar to hunger. Nature neuroscience, 23(12), 1597–1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treede R-D, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, … First MB (2015). A classification of chronic pain for ICD-11. Pain, 156(6), 1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treede R-D, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, … First MB (2019). Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain, 160(1), 19–27. [DOI] [PubMed] [Google Scholar]
- Vallbo ÅB, Olausson H, & Wessberg J (1999). Unmyelinated afferents constitute a second system coding tactile stimuli of the human hairy skin. Journal of neurophysiology, 81(6), 2753–2763. [DOI] [PubMed] [Google Scholar]
- van den Hout JH, Vlaeyen JW, Houben RM, Soeters AP, & Peters ML (2001). The effects of failure feedback and pain-related fear on pain report, pain tolerance, and pain avoidance in chronic low back pain patients. Pain, 92(1-2), 247–257. [DOI] [PubMed] [Google Scholar]
- von Mohr M, Kirsch LP, & Fotopoulou A (2017). The soothing function of touch: affective touch reduces feelings of social exclusion. Scientific reports, 7(1), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Mohr M, Krahé C, Beck B, & Fotopoulou A (2018). The social buffering of pain by affective touch: a laser-evoked potential study in romantic couples. Social Cognitive and Affective Neuroscience, 13(11), 1121–1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins RH, Dione M, Ackerley R, Backlund Wasling H, Wessberg J, & Löken LS (2021). Evidence for sparse C-tactile afferent innervation of glabrous human hand skin. Journal of Neurophysiology, 125(1), 232–237. [DOI] [PubMed] [Google Scholar]
- Watson D, & Clark LA (1984). Negative affectivity: the disposition to experience aversive emotional states. Psychological bulletin, 96(3), 465. [PubMed] [Google Scholar]
- Wickramaratne PJ, Yangchen T, Lepow L, Patra BG, Glicksburg B, Talati A, … & Weissman MM (2022). Social connectedness as a determinant of mental health: A scoping review. Plos one, 17(10), e0275004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiech K, & Tracey I (2013). Pain, decisions, and actions: a motivational perspective. Frontiers in neuroscience, 7, 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf LD, & Davis MC (2014). Loneliness, daily pain, and perceptions of interpersonal events in adults with fibromyalgia. Health Psychology, 33(9), 929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf LD, Davis MC, Yeung EW, & Tennen HA (2015). The within-day relation between lonely episodes and subsequent clinical pain in individuals with fibromyalgia: Mediating role of pain cognitions. Journal of psychosomatic research, 79(3), 202–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Younger J, Aron A, Parke S, Chatterjee N, & Mackey S (2010). Viewing pictures of a romantic partner reduces experimental pain: Involvement of neural reward systems. PloS one, 5(10), e13309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang M, & Li X (2012). From physical weight to psychological significance: The contribution of semantic activations. Journal of Consumer Research, 38(6), 1063–1075. [Google Scholar]
- Zhong CB, & Leonardelli GJ (2008). Cold and lonely: Does social exclusion literally feel cold?. Psychological Science, 19(9), 838–842. [DOI] [PubMed] [Google Scholar]


