Abstract
The world is on the verge of achieving global polio eradication. During >25 years of operations, the Global Polio Eradication Initiative (GPEI) has mobilized and trained millions of volunteers, social mobilizers, and health workers; accessed households untouched by other health initiatives; mapped and brought health interventions to chronically neglected and underserved communities; and established a standardized, real-time global surveillance and response capacity. It is important to document the lessons learned from polio eradication, especially because it is one of the largest ever global health initiatives. The health community has an obligation to ensure that these lessons and the knowledge generated are shared and contribute to real, sustained changes in our approach to global health. We have summarized what we believe are 10 leading lessons learned from the polio eradication initiative. We have the opportunity and obligation to build a better future by applying the lessons learned from GPEI and its infrastructure and unique functions to other global health priorities and initiatives. In so doing, we can extend the global public good gained by ending for all time one of the world’s most devastating diseases by also ensuring that these investments provide public health dividends and benefits for years to come.
Keywords: polio eradication, lessons learned, legacy
The world is on the verge of achieving global polio eradication [1]. In May 2013, the 66th World Health Assembly endorsed the Polio Eradication and Endgame Strategic Plan 2013–2018 [2]. The new plan provides a concrete timeline for the completion of the Global Polio Eradication Initiative (GPEI) by eliminating all paralytic polio due to both wild and vaccine-related polioviruses. The 4 principal objectives of the plan are to (1) detect and interrupt all poliovirus transmission, (2) strengthen immunization systems and withdraw all oral polio vaccine from use, (3) contain poliovirus and certify interruption of transmission, and (4) plan the polio eradication initiative’s legacy.
In the context of these objectives, particularly objective 4, it is important to document the lessons learned from polio eradication, especially considering that it is one of the largest ever global health initiatives. The health community has an obligation to ensure that these lessons and the knowledge generated are shared and contribute to real, sustained changes in our approach to global health. There is no time to lose. We have a time-limited opportunity to exploit the lessons learned and the capacity and resources of GPEI before momentum to do so dissipates, as can occur when large projects are winding up and proper planning is not in place. In fact, most countries that have already eradicated polio are already well into the legacy transition. India is an excellent example that is described in depth in a separate article [3]. The experience from smallpox eradication demonstrates that the assets from a global health initiative can disappear very quickly; fortunately, the global Expanded Programme on Immunization (EPI) emerged from among the lessons learned and legacy of smallpox eradication and has proven its value, and the power of vaccines, many times over during the 40 years of EPI’s existence [4–6]. Consequently, attention must be directed toward extending the GPEI program capacities, lessons learned, and legacy for other purposes as we move forward into the future, so that these lessons do not have to be rediscovered and reinvented later at the price of substantial additional cost and lost momentum.
GPEI LEGACY PLANNING
What Is Meant by “Legacy Planning”?
During >25 years of operations, the GPEI has mobilized and trained millions of volunteers, social mobilizers, and health workers; accessed households untouched by other health initiatives; mapped and brought health interventions to chronically neglected and underserved communities; and established a standardized, real-time global surveillance and response capacity [2, 7]. As the initiative nears completion, the GPEI’s primary goals of legacy planning are both to protect a polio-free world and to ensure that the investments made, designed to eradicate polio, contribute to broader health goals after the completion of polio eradication.
What Are the Main Guiding Principles of the Polio Legacy Planning Process?
The Polio Legacy Planning Working Group asserted 4 guiding principles of polio legacy planning [8]:
Polio legacy planning will aim to benefit all countries and the global community, not only those countries in which polio resources are currently concentrated.
Legacy planning will ensure the innovations that have helped tip the world to eradication can be adapted and applied to expanded immunization and other health programs.
Enabling long-term transitions to country ownership of basic public health functions, wherever possible, will be a priority for the polio legacy planning process.
Beginning the process of polio legacy planning early represents the GPEI’s desire to plan carefully and responsibly for the future.
What Work Needs to Be Done?
There are 3 principal aspects of the polio legacy work [2]:
Mainstreaming essential polio eradication functions, such as immunization, surveillance, communication, response, and containment, into ongoing public health programs
Ensuring that the knowledge generated and lessons learned during 25 years of polio eradication activities are documented and shared with other health initiatives
Where feasible, desirable, and appropriate, transitioning the capacities, processes, and assets, including human resources, that the GPEI has created and engaged to support other health priorities
Relationship Between Lessons Learned and the Polio Legacy
There is a close interrelationship between the GPEI lessons learned and the transition of GPEI assets as a component of the polio legacy planning process. GPEI has both tangible assets (eg, the global surveillance/laboratory network) and more-intangible accumulated knowledge, best practices, functions, processes, systems, activities, and methods of work that represent lessons learned over >25 years of experience that have made it possible for those assets to exist and function properly. These lessons have the potential to benefit other health priorities above and beyond the transfer of existing tangible assets.
WHAT ARE THE LESSONS LEARNED?
The lessons of GPEI fall into 5 general categories: (1) mobilizing political and social support, (2) strategic planning and policy development, (3) partnership management and donor coordination, (4) program operations and tactics, and (5) oversight and independent monitoring. A more detailed characterization of these categories can be found in Table 1. We have summarized here what we believe are the 10 leading lessons learned from the polio eradication initiative.
Table 1.
Lessons Learned: A Listing of Major Categories
| Mobilizing political and social support • Social mobilization and advocacy • Communications and community engagement |
| Policy development and strategic planning • Multiyear strategic plans and planning processes • Technical advisory bodies and policy processes (national, regional, and global) • National, state, and subnational task forces to guide and implement strategy |
| Partnership management and donor coordination • The Global Polio Eradication Initiative architecture—managing a global public-private partnership • Interagency coordinating committees • Financial resource requirements and cash flow management • Resource mobilization and advocacy |
| Program operations and tactics • Global surveillance and response capacity, including global laboratory network • Mapping communities (microplans) • Evidence-based decision making • Accountability frameworks • Research and development • Outreach • Surveys—monitoring and evaluation • Data management • Vaccination teams—recruitment, training, monitoring, payment • Precampaign and in-process monitoring of activities • Workforce development—building a trained and motivated health workforce |
| Oversight and independent monitoring • Performance indicators • Global and regional certification commissions • Independent monitoring board |
Lesson 1. Communications and Community Engagement: Mobilizing Social and Community Support for Vaccination
This major achievement perhaps stands at the pinnacle of the lessons learned and knowledge gained by the program [3, 9–11], insofar as “[t]he success of any disease eradication initiative depends strongly on the level of societal and political commitment” [12]. Among India and the remaining 3 polio-endemic countries, >20 000—predominantly female—social mobilizers engage with parents, community, religious, and traditional leaders daily to enlist expansive and targeted social support for polio vaccination.
For decades leading up to eradication, building social support for vaccination has begun with a comprehensive and wide-reaching approach to generate mass public support for polio eradication. As vaccination rates increased and the proportion of missed children became increasingly confined to discrete social and socioeconomic groups, communication and social mobilization strategies were refined and targeted to reach the most vulnerable families. More than any other global health program in history, “GPEI has accessed the chronically unreached, marginalized and most vulnerable populations in the world” [9]. Through this process of mobilizing communities large and small, the polio program has developed the expertise to overcome the logistic, geographic, social, political, cultural, ethnic, gender, and other barriers to working with the most-marginalized, most-deprived, and, often, most–security-compromised children and communities [9]. The characteristics and innovations developed to build social support for vaccination, include the following:
Coordinating communications to support a global and national public health goal, as well as the “relentless pursuit of the missed child” at local levels
Identifying individuals, themes, and social pillars that could unify and motivate diverse population groups for a common goal
Engaging with the media as a critical partner in raising awareness, holding stakeholders publically accountable for vaccination, and motivating leaders and communities for greater progress
Mobilizing communities house-by-house on a grand scale to accept oral poliovirus vaccine (OPV) and other health interventions, including vitamin A supplementation, measles vaccination, antihelminthic administration, and soap, bed net, and oral rehydration solution packet distribution
Creating detailed neighborhood vaccination team microplans and maps, including the identification of so-called pro-OPV influencers and supporters to help address vaccine hesitancy or resistance at the point of care
Tracking of mobile and migrant groups and communicating to these groups while they are in transit
Reaching families with information and vaccine, even when they are out of the house during campaign days; mobilizing parents at social, cultural and religious events such as weddings, mazars, shrines, and melas (festivals)
Using traditional, religious, community and civil society leaders and structures for community mobilization
Lesson 2. Communications and Community Engagement: Using Targeted Disease Initiatives as a Springboard for Broader Health Communication
The collection and analysis of social data at the most-local levels have enabled the eradication initiative to understand and engage effectively with the population it serves [3, 9–11]. Evidence-based communication insights have enabled GPEI to direct limited resources to the most-vulnerable areas and families, focus on critical messages that clarify specific knowledge gaps, and understand the remaining barriers preventing OPV from reaching children.
Throughout the eradication effort, community demands for additional services beyond OPV have affected vaccine uptake in varying degrees of intensity. In India, the 107 Block Plan promoted and delivered routine immunization, zinc, oral rehydration salts, and sanitation services to the final bastions of virus transmission, in Uttar Pradesh and Bihar. After more than a decade of offering OPV and little else, the 107 Block Plan was a critical strategy to maintaining the hard-won trust and motivation of communities to finish the job. In Pakistan and Nigeria, similar strategies are proving to be the linchpin to gaining access to hesitant or staunchly opponent households and even communities.
Promoting the promise of additional health and water services has opened new doors, leading to additional children now vaccinated against polio and to the discovery of those children most invisible to all social services. Both doors offer a promise of better health outcomes for children who need them most.
Communicating for polio vaccination has served as a springboard for broader public health outcomes by
Investing in interpersonal skills, management, and motivation of all frontline workers
Tracking and counseling pregnant mothers on prenatal health and following up on 0-dose polio vaccination and neonatal health and routine immunization
Conducting targeted communication and outreach for routine immunization sessions and advocating for the improvement of sessions that were poorly attended, managed, and stocked
Advocating for better delivery of health services that meet social, cultural, and gender-based needs of communities they target
Promoting and delivering additional health interventions besides OPV to strengthen trust where feasible, including deworming medicines, vitamin A supplements, measles vaccine, sanitation services, bed nets, and routine immunization
Building trust for OPV in inaccessible or insecure communities through the hosting of health camps
Lesson 3. The Value of an Advanced, State-of-the-Art Global, Regional, and National Laboratory Network
Over a nearly 30-year period, a sophisticated, state-of-the-art poliovirus laboratory network has been built, which currently consists of 145 national laboratories, regional reference laboratories, and global specialized laboratories [13, 14]. The global polio laboratory network demonstrates that it is possible to build an efficient global surveillance system in resource-poor countries at relatively minimal cost, compared with the cost of the intervention itself [14–17]. Other laboratory networks for vaccine-preventable diseases (eg, measles and rubella) have been based on this platform [15–17] (Figure 1). A large army of laboratory professionals has been trained and supported over a sustained period through the capacity and workforce development efforts of GPEI. Among the characteristics and innovations are the following:
Figure 1.
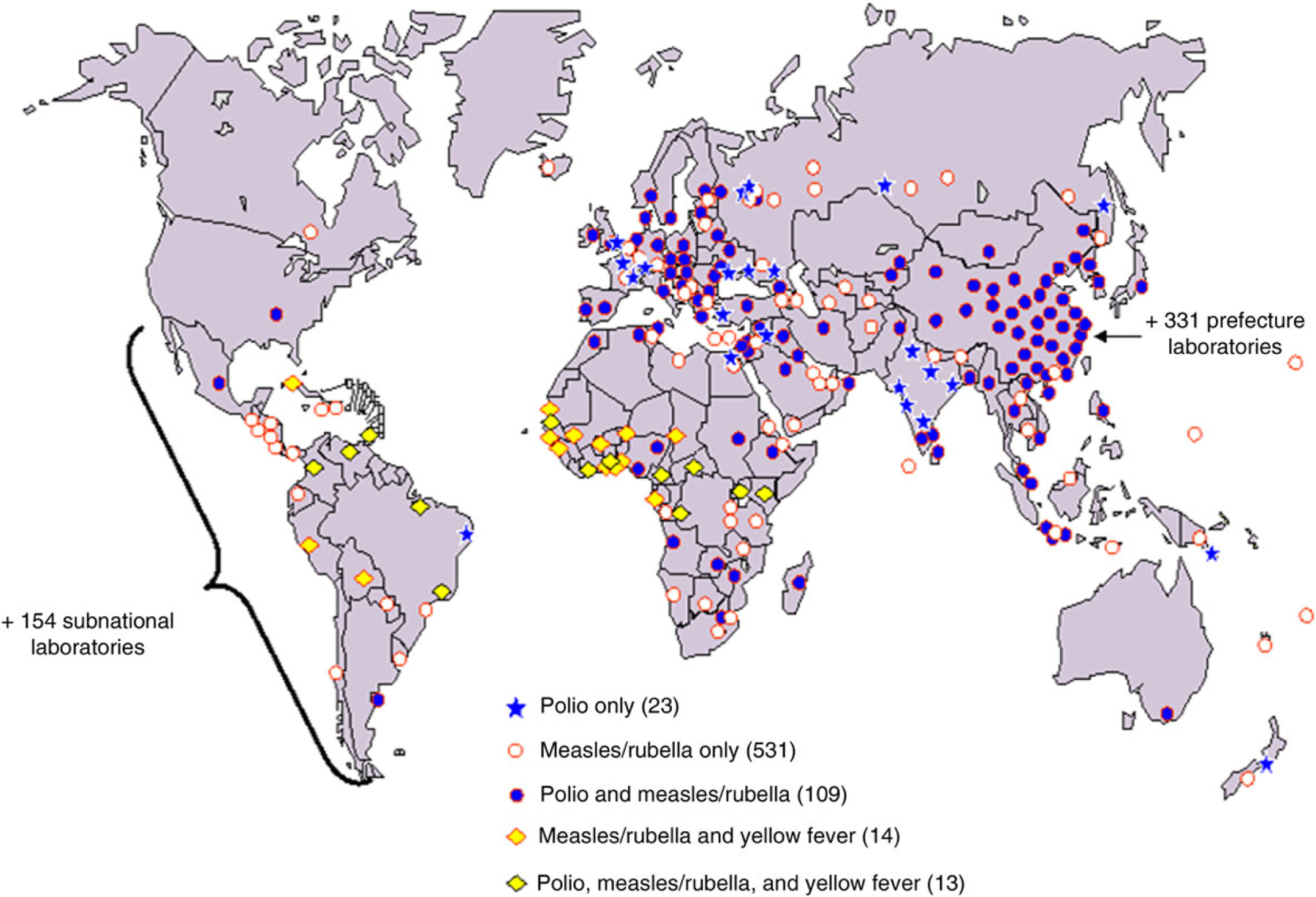
Building on the Polio Laboratory and Surveillance Network (>700 laboratories).
Provision of timely data on a weekly basis via the tiered structure (national, regional reference, and global specialized reference laboratories) of the network, which has become the model for other laboratory networks
Integration of case-based epidemiologic and laboratory information
Performance of environmental surveillance to supplement case-based data
Extension of the model to include networks for measles, rubella, yellow fever, Japanese encephalitis, rotavirus infection, invasive bacterial disease infections, and influenza
Inclusion of an annual accreditation process; proficiency testing; tracking of laboratory surveillance performance standards; standardized surveillance data collection, formatting, compilation, analysis, and feedback; quality assurance/quality control; supplying laboratories with reagents and testing kits; extensive technology transfer of new diagnostic testing procedures (eg, genetic sequencing and real-time polymerase chain reaction [PCR] analysis); periodic technical meetings for coordination and to share knowledge and findings; and periodic regional and national staff training to maintain and enhance capacity
Lesson 4. Real-time Disease Surveillance and Response Capacity, Data Analysis, and Immunization Program Monitoring
GPEI has developed and sustained a high-performance disease surveillance and program monitoring system that has enabled rapid detection of polio cases and outbreak response throughout the world, including in low-income countries. The extensive polio surveillance system composed of people, transport, Internet connections and communications, and data management facilities has enabled expansion to include surveillance of other vaccine-preventable diseases, support of measles mortality-reduction activities, and limited additional immunization program monitoring activities, including routine immunization [3, 5, 8, 15–18]. The GPEI has trained, deployed, and employed tens of thousands of health workers for >2 decades whose skills have cumulatively contributed not only to polio eradication but also to other health programs and who represent a substantial human resource capacity for the future. Recognizing this synergistic relationship, the Strategic Advisory Group of Experts on Immunization (SAGE), the technical advisory group of the WHO and the GPEI, noted the following: “Closer linkages between measles and rubella program activities and the GPEI has well-recognized benefits. As GPEI elaborates its legacy planning as a component of its endgame strategic plan, SAGE recommended that countries and global immunization partners assess the potential synergies and take active steps, where appropriate, to adapt and apply the polio infrastructure and lessons learnt to support achievement of measles and rubella elimination targets and strengthening of routine immunization programs” [19]. These resources should remain an important component of achieving the Decade of Vaccines’ goals, outlined in the Global Vaccine Action Plan [20]. Among the characteristics and innovations are the following:
Performance of case-based, rapid clinical and epidemiologic case investigation and reporting
Creation of a weekly global, regional and country World Wide Web–based reporting system with mapping of individual cases that is publicly available and unprecedented in scope
Unparalleled global surveillance and response capacity
Integration of case-based epidemiologic and laboratory information
Provision of data-driven guidance on allocation of resources, outbreak investigations, measurement of program progress, adjustments/improvements in program strategy, and implementation
Lesson 5. Addressing Strategy Implementation in Conflict-Affected Areas and the Risks of International Spread to Previously Polio-Free Countries
The GPEI is often cited for its success in implementing strategies in conflict-affected areas, and, through its experience, the GPEI has developed a range of tactics to access children and boost immunity more rapidly in these areas [21–23]. Complicating these challenges has been the regular international spread during the past decade of poliovirus from polio-endemic countries to previously polio-free countries, reemphasizing the principle of and need for global cooperation in creating a polio risk-free world and a right to health. Among the characteristics and innovations of GPEI’s polio-eradication strategy are the following:
It is an example of a global public good that should be pursued in the name of global equity and social justice and on behalf of future generations [24–26].
It reaffirms the importance of coordinating global efforts to minimize the risk of re-infecting polio-free countries and areas.
It mobilizes and deploys human and financial resources to protect at risk polio-free regions and countries (especially through SIAs).
It uses the World Health Assembly, other forums, and (recently) the International Health Regulations to persuade low-performing countries to increase their commitments and improve the quality of program performance [27].
Lesson 6. Essential Need for a Program of Research and Innovation
The GPEI has maintained an active ongoing research agenda, driven by the need to adapt and optimize strategies that had been developed in the Americas to other contexts and cultures [21, 22]. Over >2 decades, the research agenda has been able to exploit new scientific and technological developments in areas such as diagnostic tests (eg, PCR), vaccinology, and cold-chain technology (eg, vaccine vial monitors) to enhance program effectiveness and reduce cost. The research agenda also allowed for investigating and adapting to unexpected scientific findings concerning poliovirus or its control that were unrecognized at the outset of the initiative (eg, circulating vaccine-derived polioviruses) [28]. This experience has demonstrated the central and important role of research and innovation in any initiative for overcoming program setbacks and leading to a successful outcome of the initiative [29]. Innovative problem solving is required both from the bottom up as well as the top down. Among the characteristics and innovations are the following:
Recognition of constant, ongoing need to adapt and optimize strategies
Embracing of research as an essential, critical part of the program
Fast-tracked development, testing, and licensure of new tools (eg, monovalent and bivalent poliovirus vaccines and diagnostic tests) [30]
Appreciation that operational research is a key element for the success of an eradication or elimination program because “the standard of success in an eradication program is unambiguous and uncompromising” [31].
Development of special strategies to reach underserved and migrant populations
Universal use of finger-marking and independent monitoring technologies, including lot quality assurance sampling to monitor supplementary immunization activity (SIA) quality
Lesson 7. Partnership Coordination, Advocacy, and Resource Mobilization
An essential best-practices component of the GPEI has been the cross-agency coordination of an effective advocacy agenda that was central to the eventual endorsement of and crucial support to the GPEI by political bodies such as the African Union, the Organization of Islamic Cooperation, the Commonwealth, and especially the Group of Eight [21]. This effort was often lead by Rotary International as the pivotal member among the GPEI’s4 spearheading partners and also mobilized key persons, including UN leaders, business magnates, and international personalities and local political, community, religious, and traditional leaders in support of the eradication effort. Partnership coordination, input, and participation in strategy development, planning, and operations is facilitated by an extensive set of advisory, monitoring, and technical groups to inform the decision-making process. A large number and diversity of partner organizations have contributed to program success. Among the characteristics and innovations are the following:
Professionally planned and guided advocacy and resource mobilization infrastructure encompassing the global, national, and subnational (in large federated countries) contexts
Interagency coordination committee use at regional and national levels, first used in the Americas/Pan American Health Organization for their regional polio eradication initiative during 1985–1991
Extensive infrastructure and experience for conducting partner coordination of resource mobilization and advocacy, policy and strategy development, management and oversight, planning, communications and community engagement, and implementation and service delivery
Methods and infrastructure for tracking financial resource requirements and cash flow management
Lesson 8. Strategic Planning and Policy Development
After many years of developing and implementing a series of strategic plans and learning lessons regarding how to eradicate polio in the toughest settings, the GPEI has been able to put together its most comprehensive approach for completing polio eradication through global certification. New elements included the longest yet (6 years; from 2013 to 2018) budget and time line with measures taken to successfully raise most of the needed funds up front—specifically, $4.1 billion of the $5.5 billion estimated cost, an urgent emphasis on improving immunization systems in key geographic areas, and the most extensive monitoring framework in its history. Among the characteristics and innovations are the following:
Multiyear strategic plans and planning processes throughout the life of the GPEI
Elaborated national emergency action plans for the 3 remaining polio-endemic countries (Afghanistan, Nigeria, and Pakistan)
Technical advisory groups and policy development at a global (SAGE), regional, and national level in key countries
National, state, and subnational task forces in key countries to guide and implement strategy
Lesson 9. Oversight and Independent Monitoring and Evaluation
The GPEI has learned the fundamental need for a strong oversight framework to support the program, monitoring, and management of the collaborative process and for communicating with and sustaining the commitments of a diverse group of stakeholders. Among the characteristics and innovations are the following:
An independent body of respected and competent leaders should be formed as an independent monitoring group to assess progress toward the eradication goal for all stakeholders. Such a group, the GPEI Independent Monitoring Board, was established in 2011 and continues to play a strong role in guiding the initiative [32].
A strong central technical advisory body consisting of highly qualified and experienced people should provide ongoing technical guidance and direction for a global initiative such as GPEI. This function has been performed by the SAGE, which advises the WHO and the GPEI.
The WHO Executive Board and World Health Assembly provide the highest level of governance of the GPEI and secure the commitment of all WHO member states to support the full implementation of the GPEI strategic plan.
Global and regional certification commissions are independent bodies appointed by the Director-General of the WHO to oversee the process of certifying individual regions and the world as free of polio.
The global Polio Partners Group serves as the stakeholder voice for the GPEI.
Many surveillance and program performance indicators exist to objectively monitor country and global performance.
Lesson 10. Monitoring of Program Accountability and Performance
The GPEI learned that technical solutions could not compensate for basic management and accountability shortcomings in key countries and areas [2]. In large, federated countries with weak health systems, it became necessary to engage political leaders at the subnational level and put in place systems for greater staff and financial accountability [22]. Among the characteristics and innovations are the following:
National emergency action plans were established for the 3 remaining polio-endemic countries (Afghanistan, Nigeria, and Pakistan), creating oversight bodies at the country level reporting to heads of state, to intensify political and administrative accountability for the quality of key eradication activities.
Microplans were created, and mapping of communities (including use of global positioning systems) was performed.
Accountability frameworks were created and implemented.
SIA coverage surveys, SIAs independent monitoring teams, lot quality assurance sampling, and seroprevalence surveys were performed to link accountability with objective monitoring data.
PREPARING FOR THE FUTURE
We have the opportunity and obligation to build a better future by applying the lessons learned from the GPEI and its infrastructure and unique functions to other global health priorities and initiatives. Chief among these prospects is the opportunity to strengthen overall immunization programs, especially routine immunization systems, in low-income countries, including India, through the use and redirection of GPEI resources and innovative approaches that have been outlined in this article. In so doing, we can extend the global public good gained by ending for all time one of the world’s most devastating diseases by also ensuring that these investments provide public health dividends and benefits for years to come.
Financial support.
This work was supported by the Centers for Disease Control and Prevention, United Nations Children’s Fund, and World Health Organization.
Footnotes
Disclaimer. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention, World Health Organization, or United Nations Children’s Fund.
Supplement sponsorship. This article is part of a supplement entitled “The Final Phase of Polio Eradication and Endgame Strategies for the Post-Eradication Era,” which was sponsored by the Centers for Disease Control and Prevention.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Global Polio Eradication Initiative. WHO polio weekly global surveillance update http://www.polioeradication.org/. Accessed 15 May 2014.
- 2.Global Polio Eradication Initiative. Polio eradication & endgame strategic plan 2013–2018 World Health Organization. http://www.polioeradication.org/. Accessed 15 May 2014. [Google Scholar]
- 3.Jafari H, Bahl S. Eradication of polio in India: major lessons learned and implications for global eradication. Jafari H and Bahl S, written communication, 2014. [Google Scholar]
- 4.Henderson DA. The eradication of smallpox—an overview of the past, present, and future. Vaccine 2011; 29(suppl 4):D7–9. [DOI] [PubMed] [Google Scholar]
- 5.Okwo-Bele JM, Cherian T. The expanded programme on immunization: a lasting legacy of smallpox eradication. Vaccine 2011; 29(suppl 4):D74–9. [DOI] [PubMed] [Google Scholar]
- 6.Chan M Beyond expectations: 40 years of EPI. Lancet 2014; 383: 1697–8. [DOI] [PubMed] [Google Scholar]
- 7.Chatterjee P Added benefits of polio eradication. BMJ 2013; 346:f3378. [DOI] [PubMed] [Google Scholar]
- 8.Polio Legacy Planning Working Group. Legacy planning process for the Global Polio Eradication Initiative: frequently asked questions Geneva: World Health Organization, 2014. http://www.polioeradication.org/. Accessed 15 May 2014. [Google Scholar]
- 9.Global Polio Eradication Initiative. Polio eradication & endgame strategic plan 2013–2018 Geneva: World Health Organization, 2014. p.76. http://www.polioeradication.org/. Accessed 15 May 2014. [Google Scholar]
- 10.Obregon R, Chitnis K, Morry C, et al. Achieving polio eradication: a review of health communication evidence and lessons learned in India and Pakistan. Bull World Health Organ 2009; 87:624–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bates J, Guirguis S, Moran T, Desomer L. Disease eradication as a springboard for broader public health communication. In: Cochi SL, Dowdle WR, eds. Disease eradication in the 21st century: implications for global health Cambridge, MA: MIT Press, 2011:255–70. [Google Scholar]
- 12.Dowdle WR. The principles of disease elimination and eradication. In: Global disease elimination and eradication as public health strategies. MMWR 1999; 48(suppl):23. http://www.cdc.gov/mmwr/preview/mmwrhtml/su48a7.htm. Accessed 18 May 2014. [Google Scholar]
- 13.Hull BP, Dowdle WR. Poliovirus surveillance: building the global polio laboratory network. J Infect Dis 1997; 175(suppl 1):S113–6. [DOI] [PubMed] [Google Scholar]
- 14.de Gourville E, Duintjer Tebbens RJ, Sangrujee N, Pallansch MA, Thompson KM. Global surveillance and the value of information: the case of the global polio laboratory network. Risk Anal 2006; 26:1557–69. [DOI] [PubMed] [Google Scholar]
- 15.Dabbagh A, Eggers R, Cochi S, Dietz V, Strebel P, Cherian T. A new global framework for immunization monitoring and surveillance. Bull World Health Organ 2007; 85:904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.WHO. Global framework for immunization monitoring and surveillance. WHO/IVB/07.06 Geneva: World Health Organization, 2007:1–54. http://www.who.int/immunization/documents/. Accessed 15 May 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Featherstone DA, Rota PA, Icenogle J, et al. Expansion of the global measles and rubella laboratory network 2005–2009. J Infect Dis 2011; 204(suppl 1):S491–8. [DOI] [PubMed] [Google Scholar]
- 18.Nsubuga P, McDonnell S, Perkins BA, et al. Polio eradication initiative in Africa: influence on other infectious disease surveillance development. BMC Public Health 2002; 2:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.WHO. Meeting of the Strategic Advisory Group of Experts on immunization, November 2012 – conclusions and recommendations. Wkly Epidemiological Rec 2013; 88:12. [PubMed] [Google Scholar]
- 20.WHO. Global vaccine action plan, 2011–2020 Geneva: World Health Organization, 2013. http://www.who.int/immunization/global_vaccine_action_plan/en/. Accessed 15 May 2014. [Google Scholar]
- 21.Aylward B, Tangermann R. The global polio eradication initiative: lessons learned and prospects for success. Vaccine 2011; 29(suppl 4): D80–5. [DOI] [PubMed] [Google Scholar]
- 22.Aylward RB. Lessons from the late stages of the global polio eradication initiative. In: Cochi SL, Dowdle WR, eds. Disease eradication in the 21st century: implications for global health Cambridge, MA: MIT Press, 2011:13–23. [Google Scholar]
- 23.Tangermann R, Hull HF, Jafari H, et al. Eradication of poliomyelitis in countries affected by conflict. Bull World Health Organ 2000; 78:330–8. [PMC free article] [PubMed] [Google Scholar]
- 24.Barrett S Polio eradication: strengthening the weakest links. Health Affairs 2009; 28:1079–90. [DOI] [PubMed] [Google Scholar]
- 25.Emerson C, Singer P. Is there an ethical obligation to complete polio eradication? Lancet 2010; 375:1340–1. [DOI] [PubMed] [Google Scholar]
- 26.Emerson CI. The moral case for eradication. In: Cochi SL, Dowdle WR, eds. In: Disease eradication in the 21st century: implications for global health Cambridge, MA: MIT Press, 2011:103–13. [Google Scholar]
- 27.Rutter PD, Donaldson LJ. Mandatory polio vaccination for travelers: protecting global public health. Lancet 2014; 383:1695–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kew OM, Sutter RW, de Gourville EM, Dowdle WR, Pallansch MA. Vaccine-derived polioviruses and the endgame strategy for global polio eradication. Annual Rev Microbiol 2005; 59:587–635. [DOI] [PubMed] [Google Scholar]
- 29.Jacobson J The role of research. In: Cochi SL, Dowdle WR, eds. The eradication of infectious diseases: understanding the lessons and advancing experience. In: Disease eradication in the 21st century: implications for global health Cambridge, MA: MIT Press, 2011:63–86. [Google Scholar]
- 30.Sutter RW, John TJ, Jain H, et al. Trial of bivalent type 1 and type 3 oral poliovirus vaccine. Lancet 2010; 376:1682–8. [DOI] [PubMed] [Google Scholar]
- 31.Recommendations of the International Task Force for Disease Eradication. MMWR Recomm Rep 1993; 42(RR-16):3. [PubMed] [Google Scholar]
- 32.Rutter P, Donaldson L. Oversight role of the independent monitoring board of the global polio eradication initiative. J Infect Dis 2014; 210 (suppl 1):S16–22. [DOI] [PubMed] [Google Scholar]


