Abstract
Background:
In October 2012, an open-access, multimedia digital cleft simulator was released. Its purpose was to address global disparities in cleft surgery education, providing an easily accessible surgical atlas for trainees globally. The simulator platform includes a three-dimensional surgical simulation of cleft care procedures, intraoperative videos, and voiceover. This report aims to assess the simulator's demographics and usage in its tenth year since inception. Finally, we also aim to understand the traction of virtual reality in cleft surgical education.
Methods:
Usage data of the simulator over 10 years were retrospectively collected and analyzed. Data parameters included the number of users, sessions, countries reached, and content access. An electronic survey was emailed to registered users to assess the benefits of the simulator.
Results:
The total number of new and active simulator users reached 7687 and 12,042. The simulator was accessed an average of 172.9.0 ± 197.5 times per month. Low- to middle-income regions accounted for 43% of these sessions. The mean session duration was 11.4 ± 6.3 minutes, yielding a total screen time of 3022 hours. A total of 331 individuals responded to the survey, of whom 80.8% found the simulator to be very useful or extremely useful. Of those involved in education, 45.0% implemented the simulator as a teaching tool.
Conclusions:
Global utilization of the simulator has been sustained after 10 years from inception with an increased presence in low- to middle-income nations. Future similar surgical simulators may provide sustainable training platforms to surgeons in low- and high-resource areas.
Takeaways
Question: Is digital surgical simulation viable for achieving global use and supporting education in high- and low-income settings?
Findings: The total number of new and active simulator users reached 7687 and 12,042. Low- to middle-income regions accounted for 43% of these sessions. A total of 331 individuals responded to the survey, of whom 80.8% found the simulator to be very useful or extremely useful.
Meaning: Global utilization of the simulator has been sustained after 10 years from inception with an increased presence in low- to middle-income nations, providing sustainable training platforms to surgeons in low- and high-resource areas.
INTRODUCTION
Cleft lip and palate (CLP) is the most common congenital anomaly affecting the face. As uncorrected CLP can lead to impaired speech development, failure to thrive, recurrent otitis media, and dental complications, timely reconstruction is paramount to normal development.1 Yet, although access to cleft care is largely equitable in high-income countries, rates of uncorrected CLP are still high in middle- and low-income nations, leading to higher morbidity associated with craniofacial anomalies in the latter.2
Differences in global patient access to cleft care are multifold. The sparsity of reconstructive surgeons is a common challenge in low- and middle-income countries. For instance, in certain areas of Asia, the incidence of unilateral cleft is 6.51 per 10,000 births, but there are only 1.5 plastic surgeons per one million people. This is in stark comparison with North American countries that have approximately one provider per 57,000 individuals.3,4 To mitigate this discrepancy, the development of local surgical training has been pursued. However, in developing nations, due to an already diminished plastic surgery workforce, surgical training programs can be less formalized with students exposed to a smaller number of cases.5 Compared to programs in more developed nations, medical students and residents in low-resource regions may have limited educational learning modalities and opportunities.5 This impacts the surgical quality and safety practices offered to patients in such regions. The culmination of these variables may lead to care disparities between developed and developing nations.
To address these global disparities existing in cleft care, in partnership with Smile Train, Inc. (New York, N.Y.) and BioDigital (New York, N.Y.), the senior author developed an educational, freely available, multidevice-friendly, internet-based cleft surgery simulator which demonstrates the cardinal procedures in cleft care within an interactive multimedia platform. Available in five languages, the platform includes a three-dimensional digital surgical simulation, voiceover, textbox, and high-definition intraoperative video footage of all major steps of the operation. The purpose of this tool is to empower local surgeons to supplement their training in a safe and approachable environment. Although early reports on the utilization of this cleft simulator demonstrate favorable engagement, long-term analysis of international use is lacking.6,7
In this study, we report the demographics of users and patterns of use of the described cleft simulator over a 10-year period. We hypothesize that the simulator has had sustained use over a decade and, therefore, may serve as a model for other surgical education resources which can be deployed on a national to international scale. Finally, we aim to elucidate the potential traction of implementing virtual reality (VR) as an additional tool to support cleft surgical education.
METHODS
In partnership with the nonprofit organization Smile Train and industry partners, the senior author developed a freely available cleft simulator to augment surgical training in 2012. The purpose of the simulator was to provide a freely available and easily accessible digital resource for cleft surgery to low- to middle-income regions of the world, available at www.cleftsim.org (available on Google Chrome and Mozilla Firefox web browsers) and with no additional need for specialized software platforms or hardware tools.
Since its inception, the simulator has undergone progressive updates to include new training modules, translation of all content into five languages (English, Spanish, Portuguese, French, and Mandarin), and requisite platform modifications to maintain compatibility with internet browser updates.8 Furthermore, to increase accessibility to the index of individuals in developing countries, a smartphone application available through iPhone and Android devices was developed and launched in 2017.
Data regarding the patterns of the simulator users were collected from a database embedded in the platform. Available data included the number of hours accessed, users’ countries of origin, new users per month, number of active and recurrent users, user session duration, and most accessed simulator modules. Here, new users are defined as the number of new simulator registrations, whereas active users include both new and previous users. To create a temporal narrative of parameters collected, retrospective data from previous years and published studies were also measured and compared to currently available data.6,7
Finally, to identify subjective parameters of use, a survey was created and distributed to the host list of users that have accessed the platform. Questions asked included user demographics, preferred methods of learning, preferred mediums of accessing the simulator, the perceived value of the tool for cleft education, and opinions on possible simulator improvements. As a prelude to future developments of the platform, users’ experience with VR, whether VR would be an optimizing addition to the learning experience, and what barriers they would face if VR were to be included as an option in the simulator platform were also assessed.
RESULTS
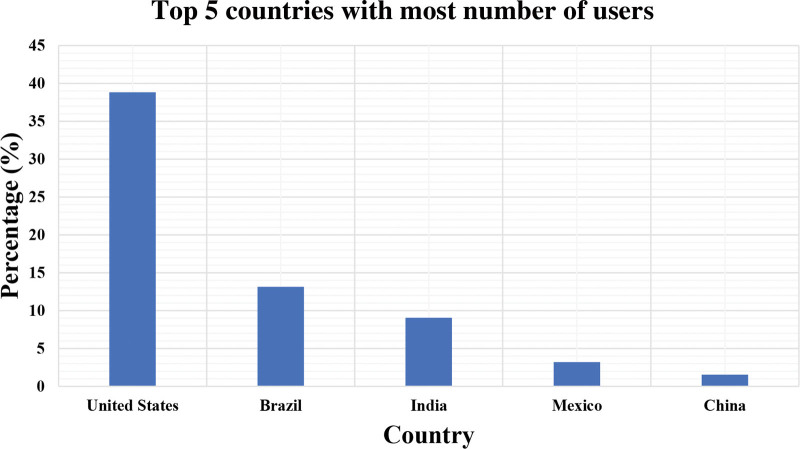
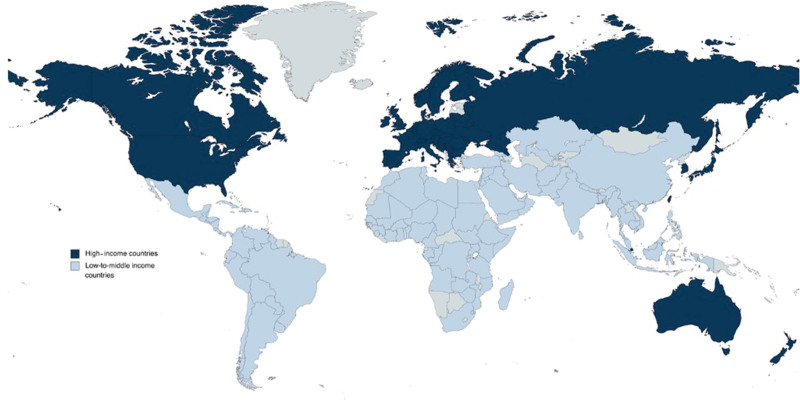
Users from 148 countries accessed the simulator, a substantial increase from 78, and 136 were identified in 1- and 5-year reports, respectively. The proportion of users from developing nations increased substantially from 35% in the 5-year report to 46% in this 10-year study. The five countries with the most frequent simulator access remained the same between the 5-year landmark and now and included the United States (46.4%), Brazil (14.3%), India (10.3%), Mexico (2.9%), and China (1.7%) (Fig. 1). The presence of the surgical simulator in different countries in the world can be found in Figure 2, stratified between Global North and Global South nations.
Fig. 1.
Countries with the most users.
Fig. 2.
Countries with users, stratified according to high, middle, and low income.
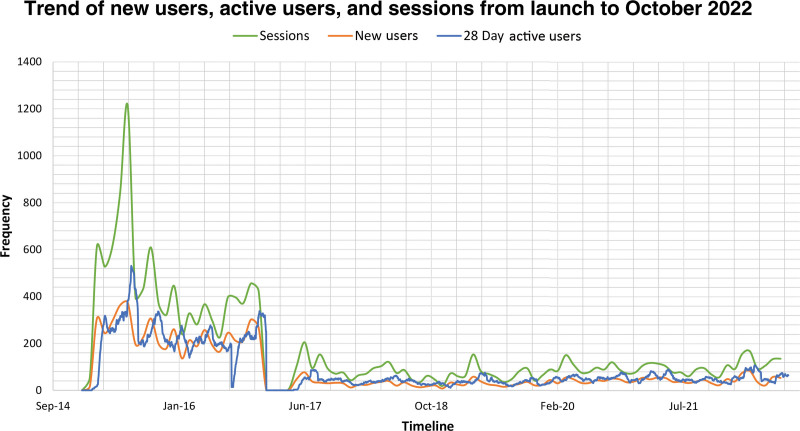
The number of new users per month has gradually increased from 51 to 83.6 on average. Although the number of sessions per month decreased from an average of 399 in 2017 to 172.9 in 2022, the number of minutes spent per session increased from 9.0 to 11.4 (Table 1). A trend of active and new users, and average sessions per month, can be found in Figure 3.
Table 1.
Simulator Use Parameters
| Parameter | Average (STDV), 2017 | Average (STDV), 2022 |
|---|---|---|
| New users per month | 51 (22) | 83.6 (95.7) |
| Active users per month | 104 (119) | 90.0 (95.1) |
| Sessions per month | 399 (190) | 172.9 (197.5) |
| Session duration (min) | 9.0 (7.3) | 11.4 (6.3) |
Fig. 3.
The trend of new users, active users, and sessions from simulator launch to October 2022.
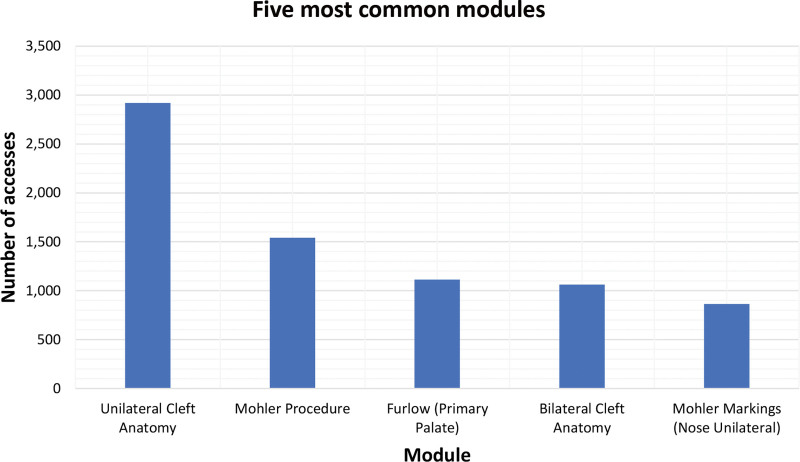
In August 2022, the total number of new and active simulator users reached 7687 and 12,042, respectively. There was a large relative increase in monthly users and sessions when the simulator was first launched, followed by a decrease and a relatively steady state of continued use. In total, 15,908 sessions and 3022 hours of simulator use were recorded since inception. The most common device used was the desktop (83.4%), followed by mobile (12.3%), and tablet (4.3%). Since the implementation of the smartphone option, it has been steadily increasing as an access platform. Further parameters collected are summarized in Table 2. In addition, the most accessed learning modules were “Unilateral Cleft Anatomy” followed by the “Mohler Cleft Lip Procedure,” “Furlow (Primary Palate),” and “Bilateral Cleft Anatomy” (Fig. 4).
Table 2.
Simulator Parameters Since Launch
| Parameter | Total Number (2017) | Total Number (2022) |
|---|---|---|
| New users | 2865 | 7687 |
| Active users | 4086 | 12042 |
| Sessions | 11,176 | 15,908 |
| Total session hour (h) | 1676 | 3022 |
| Sessions in | ||
| Desktop | 8282 | 13,264 |
| Mobile | 1382 | 1966 |
| Tablet | 552 | 678 |
| Countries | 136 | 146 |
| Languages available in modules | 5 | 5 |
Fig. 4.
Most common modules accessed in the simulator.
The study survey was distributed to 6413 enlisted users, and 331 (5.20%) responded. The majority of users were attendings (67.1%), followed by residents/fellows (30.5%), and a minority represented by medical students (2.4%). Respondents were predominantly plastic surgery trained (45.3%), followed by maxillofacial surgery (40.2%), pediatric surgery (5.7%), general surgery (4.00%), and otolaryngology (3.3%). The remaining 1.5% did not disclose their specialty of practice. The majority of users found the simulator to be very useful (45.2%) and extremely useful (35.6%).
When asked to compare the simulator with traditional education tools, the majority of users found the simulator more useful than other resources, including textbooks, seminars, and lectures. On a scale of one to 10, with one being the most useful, the STVSS averaged the highest at 2.37 followed by textbooks at 2.44. In addition, approximately half the of respondents (46.7%) mentioned being involved in resident education, and, of these, 45.0% mentioned actively implementing the simulator as a teaching tool. Users’ suggestions for improvement included videos teaching how to use the platform and similar content for other plastic surgery subspecialties.
Finally, when questioned on the possibility of introducing VR to the simulator, approximately half (49.2%) of users denied previous experience using VR while 50.8% affirmed prior experience, including 34.0% as learners, 14.4% as educators, and 2.4% as content creators. Many respondents (41.2%) agreed that the addition of VR to the platform would be extremely helpful and would largely augment their training. Yet, when asked about barriers that would hinder VR implementation, users answered that lack of formal VR training (20.8%), lack of strong internet connection (7.6%), and financial barriers (57.2%) would have to be addressed to facilitate the use of VR in the intended educational setting. A minority of users (13.2%) responded that they would not face any barriers to implementation.
DISCUSSION
This study investigates the global utilization of an internet-based, freely accessible, multimedia educational cleft simulator in its tenth year since inception. This study demonstrates that this freely available simulator has sustained widespread acceptance among individuals from under-resourced countries and high-income countries. Application use within developing nations grew steadily between the 5- and 10-year study periods, despite the potential limitations of internet access in these regions. Although criticism of internet-dependent resources emphasized how the need for the internet could further widen disparities between high and low socio-economic disparities in developing nations, a recent report from the UN indicated that among the global youth population, more than 70% of individuals have current internet access.9,10 Furthermore, even in low-income countries, surgeons are among those with a higher likelihood of internet accessibility. This report demonstrates that internet-based educational modules can be successfully leveraged to be deployed to provide valued training resources to low- and high-income regions of the world.
Compared to the 5-year report, session numbers and time spent per session have continuously increased. Furthermore, average screen time is higher than the calculated average webpage visit dwell times, defined as the time the user stays on the same page. For instance, one study calculated dwell time to be as low as 30 seconds in commercial webpages containing relevant information to participants, indicating that an average in the range of minutes suggests users’ engagement in the presented content.11 When compared to metrics published in the 5-year report, we found an increase of over 2 minutes in time spent on the simulator, implying the engagement with the simulator has increased. Although it is true that new users may skew the average to a higher value, the fact that recurrent users increased at a higher rate in the past 5 years suggests recurrence of use and better user interface interaction. Similarly, based on survey results, there has been an increased interest in the use of the simulator as an educational tool.6,7 In fact, the simulator was considered more useful than traditional methods of learning, including textbooks. Furthermore, approximately half of the responders involved in education mention using the simulator as a didactic support.
Previous randomized controlled trials on educational outcomes using simulators have highlighted their benefits compared to traditional medicine learning methods, namely lectures and textbooks.12,13 A common limitation to traditional surgical training resources such as a textbook is the lack of multidimensional imaging describing and showcasing surgical methods. These constraints of print can limit the effectiveness of preoperative preparation and postoperative supplementation, potentially impacting patient care and surgical outcomes.14 The presented simulator combines dynamic three-dimensional digital surgical models, videos, text, and guided assessments, addressing many of the shortcomings of traditional surgical education resources.15 In settings where textbook access may be a financial or linguistic barrier, a free simulator may overcome educational constraints by providing a multilingual, internet- and smartphone-available platform.16
Cleft surgery is an anatomically complex and technically elaborate surgery in which seemingly minor shortcomings can have profound implications for the patient. As is the case with many surgical procedures, proficiency is dependent on adequate preparation and sufficient surgical exposure. With required resident work-hour limitations in developed nations and limited resources and case exposure in low- and middle-income countries, proper education of the intricacies of cleft surgery may not be properly interiorized before later stages of training and career when unattended operations are performed.17 It is notable that cleft surgeons treat conditions that are uncommon in occurrence. In high-resource nations, mitigations to such limitations might occur through high-fidelity training models, as no appropriate cadaver model exists. Yet, these can be unavailable in developing countries due to financial or geographic constraints.18 Thus, the simulator can emerge as a complement to hands-on training in both developed and developing nations by creating a learning environment outside of operative work hours that augments and compliments learning inside the operating room. Numerous studies have demonstrated accelerated learning through animation and simulation resources which can result in a more efficient pathway to proficiency and safer surgery.12,13,16,19,20
As the disease burden associated with orofacial clefting is highest among low-and-middle-income countries, the increased traction of the simulator in lower-income settings has aligned with decreases in the burden of orofacial clefting measured by disability-adjusted life-years (DALYs). For example, since 1990, Latin American countries have experienced, on average, a 71.0% decrease in DALYs which aligns with the continuous growth of users in nations belonging to this world region.21 Such patterns are also found for the usage of countries in East Asia, which has experienced an 83.58% DALY decrease, and South Asia, with a 60.55% DALY decrease.21 Although there are different variables affecting the decrease in disease burden, quality of surgical training and provider experience have been identified as major drivers of improved patient safety and better surgical outcomes.22 As such, the simulator may positively impact the microlevel by introducing avenues of technique improvement without possible patient harm.
In addition, the analytics report detailed in this study provides a potential opportunity for financial sustainability for this educational resource. At this time, all costs of maintenance are provided through philanthropic support. However, the user base detailed in this report almost entirely consists of reconstructive surgeons. Industry partners could capitalize on the viewer profile to promote services and products similar to what is normally done in most internet sites and smartphone applications.23 The opportunity to use this and other simulators as a platform for corporate sponsorship provides a pathway to sustainable use outside philanthropic support, the method by which the described simulator is currently supported.
With the increase in studies on the benefits of VR in residency training in the United States, the implementation of VR in the simulator is the next step in augmenting operative reality before operative exposure.24 VR systems are a low-risk and potentially high-impact approach to training and assessing clinicians and patients. The resource may be useful to medical students and residents in low-resource regions who would not otherwise have access to such equipment, and training and can enhance both technical (ie, surgical) and nontechnical (ie, teamwork) skills training.25 Although acknowledging the innate limitations of local environments, when questioned whether VR in cleft simulation would be beneficial, recipients largely agreed its addition would augment their surgical training. VR allows for more immersive interaction with the surgical field and develops key surgical motor skills that would otherwise not have been allowed in an application-based simulator.26 As VR addition has been successful in other surgical subspecialties in the United States with demonstrated benefits towards patient safety, transition to a VR model would most likely improve outcomes and support further interaction between educators in major academic centers to learners in low-resource settings.27
Our investigation is not without limitations, including its descriptive nature and the inherent limitations associated with survey studies, such as respondent selection bias. This study reports on utilization and user-reported outcomes and does not test the benefit to training or patient safety. The details of the practice patterns and surgical experience of the user base are not known other than what is reported. National and international utilization does not prove beneficial to patient outcomes. The sustained use demonstrated in this report may not be reproducible by other types of simulators in other surgical fields; however, this 10-year study does provide supportive evidence that digital surgical simulators can be a valued training resource in the national and international setting.
CONCLUSIONS
A freely available internet-based and smartphone application-based multimedia cleft simulator has sustained use and subjective benefit over a 10-year period, suggesting that this resource is a globally valued education tool that is accessible and used in both low-resource and high-resource settings.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Footnotes
Published online 29 September 2023.
Disclosure statements are at the end of this article, following the correspondence information.
Declarations of interest: none to declare.
Dr Chaya and Laspro contributed equally to this work.
REFERENCES
- 1.Zaluzec RM, Rodby KA, Bradford PS, et al. Delay in cleft lip and palate surgical repair: an institutional review on cleft health disparities in an urban population. J Craniofac Surg. 2019;30:2328–2331. [DOI] [PubMed] [Google Scholar]
- 2.Lanteri AC, Parcells BW, Lizarraga AK, et al. A cross-sectional comparison of cleft lip severity in 3 regional populations. Eplasty. 2012;12:e10. [PMC free article] [PubMed] [Google Scholar]
- 3.Semer NB, Sullivan SR, Meara JG. Plastic surgery and global health: how plastic surgery impacts the global burden of surgical disease. J Plast Reconstr Aesthet Surg. 2010;63:1244–1248. [DOI] [PubMed] [Google Scholar]
- 4.Zhu Y, Miao H, Zeng Q, et al. Prevalence of cleft lip and/or cleft palate in Guangdong province, China, 2015-2018: a spatiotemporal descriptive analysis. BMJ Open. 2021;11:e046430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Borrelli MR. What is the role of plastic surgery in global Health? A review. World J Plast Surg. 2018;7:275–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kantar RS, Plana NM, Cutting CB, et al. Internet-based digital simulation for cleft surgery education: a 5-year assessment of demographics, usage, and global effect. J Surg Educ. 2018;75:1120–1126. [DOI] [PubMed] [Google Scholar]
- 7.Plana NM, Diaz-Siso JR, Culnan DM, et al. The first year of global cleft surgery education through digital simulation: a proof of concept. Cleft Palate-Craniofac J. 2018;55:626–629. [DOI] [PubMed] [Google Scholar]
- 8.McKechnie T, Levin M, Zhou K, et al. Virtual surgical training during COVID-19: operating room simulation platforms accessible from home. Ann Surg. 2020;272:e153–e154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.James J. Confronting the scarcity of digital skills among the poor in developing countries. Dev Policy Rev. 2021;39:324–339. [Google Scholar]
- 10.United Nations International Telecommunication Union. Global connectivity report 2022. 2022.
- 11.Guo Q, Agichtein E. Beyond dwell time: estimating document relevance from cursor movements and other post-click searcher behavior. Paper presented at: WWW’12—Proceedings of the 21st Annual Conference on World Wide Web 2012. [Google Scholar]
- 12.Plana NM, Rifkin WJ, Kantar RS, et al. A prospective, randomized, blinded trial comparing digital simulation to textbook for cleft surgery education. Plast Reconstr Surg. 2019;143:202–209. [DOI] [PubMed] [Google Scholar]
- 13.Kantar RS, Alfonso AR, Ramly EP, et al. Knowledge and skills acquisition by plastic surgery residents through digital simulation training: a prospective, randomized, blinded trial. Plast Reconstr Surg. 2020;145:184e–192e. [DOI] [PubMed] [Google Scholar]
- 14.Mughal M, Din AH, O’Connor EF, et al. Breaking down training barriers: a novel method of delivering plastic surgery training through augmented reality. J Plast Reconstr Aesthet Surg. 2021;74:1101–1160. [DOI] [PubMed] [Google Scholar]
- 15.Waltzman JT, Tadisina KK, Zins JE. The rise of technology in plastic surgery education: is the textbook dead on arrival (DOA)? Aesthet Surg J. 2016;36:237–243. [DOI] [PubMed] [Google Scholar]
- 16.Diaz-Siso JR, Plana NM, Stranix JT, et al. Computer simulation and digital resources for plastic surgery psychomotor education. Plast Reconstr Surg. 2016;138:730e–738e. [DOI] [PubMed] [Google Scholar]
- 17.Zbar RIS, Rai SM, Dingman DL. Establishing cleft malformation surgery in developing nations: a model for the new millennium. Plast Reconstr Surg. 2000;106:886–889. [PubMed] [Google Scholar]
- 18.Habicht JL, Kiessling C, Winkelmann A. Bodies for anatomy education in medical schools: an overview of the sources of cadavers worldwide. Acad Med. 2018;93:1293–1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kantar RS, Alfonso AR, Ramly EP, et al. Educational resources in craniofacial surgery: the case for user-friendly digital simulators. J Craniofac Surg. 2020;31:931–933. [DOI] [PubMed] [Google Scholar]
- 20.Flores RL, Demoss P, Klene C, et al. Digital animation versus textbook in teaching plastic surgery techniques to novice learners. Plast Reconstr Surg. 2013;132:101e–109e. [DOI] [PubMed] [Google Scholar]
- 21.Massenburg BB, Hopper RA, Crowe CS, et al. Global burden of orofacial clefts and the world surgical workforce. Plast Reconstr Surg. 2021;148:568e–580e. [DOI] [PubMed] [Google Scholar]
- 22.Stulberg JJ, Huang R, Kreutzer L, et al. Association between surgeon technical skills and patient outcomes. JAMA Surg. 2020;155:960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Compton B, Barash DM, Farrington J, et al. Access to medical devices in low-income countries: Addressing sustainability challenges in medical device donations: NAM Perspectives. Discussion Paper. Washington, DC: National Academy of Medicine; 2018. [Google Scholar]
- 24.Seymour NE, Gallagher AG, Roman SA, et al. Virtual reality training improves operating room performance. Ann Surg. 2002;236:458–463; discussion 463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Palter VN, Grantcharov TP. Virtual reality in surgical skills training. Surg Clin North Am. 2010;90:605–617. [DOI] [PubMed] [Google Scholar]
- 26.Hasan LK, Haratian A, Kim M, et al. Virtual reality in orthopedic surgery training. Adv Med Educ Pract. 2021;12:1295–1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cevallos N, Zukotynski B, Greig D, et al. The utility of virtual reality in orthopedic surgical training. J Surg Educ. 2022;79:1516–1525. [DOI] [PMC free article] [PubMed] [Google Scholar]