Abstract
Background
Physician–nurse task shifting, a process of delegation whereby tasks are moved to other specialized healthcare workers, is used in primary care in many countries to improve access, efficiency and quality of care. One such task is the prescription of medicines.
Objectives
To identify nurse independent prescriber (NIP) and GP numbers in England, the proportions and types of NIP and GP antibiotic prescriptions dispensed in the community, and the impact of COVID-19 on the volume, rate and types of antibiotic prescriptions dispensed.
Methods
Descriptive population-based retrospective cohort study using routinely collected data on prescriptions for antibiotics dispensed in the community in England between January 2014 and October 2021.
Results
Between 2014 and 2021, numbers (headcount) of NIPs whose prescriptions were dispensed in the community rose by 146% to 34 997. GP numbers (headcount) rose by 10% to 44 681. Of the 25.373 million antibiotic prescriptions dispensed between 2014 and 2021, NIPs were responsible for 8.6%. The rate of dispensed antibiotic prescriptions per prescriber per calendar year decreased (by 50% for NIPs and by 21% for GPs) between 2014 and 2020. This decreasing trend continued following the onset of the COVID-19 pandemic across both groups. Narrow-spectrum antibiotics (penicillins, macrolides, tetracyclines) were the most frequently dispensed across both NIPs and GPs.
Conclusions
NIPs are an increasing contributory influence on total antibiotic prescribing and should be included in antimicrobial stewardship efforts. Interventions for this group need to be tailored to the population and context in which they work.
Introduction
Antimicrobials continue to be used significantly more per capita than in previous decades,1,2 with an associated increase in antimicrobial resistance (AMR).3 AMR infections are among the greatest threats to human health. In 2019, 4.95 million deaths were associated with AMR (i.e. where AMR played some role) and 1.27 million deaths were attributable to AMR alone. Lower respiratory tract infections accounted for the largest proportion of these deaths.4 To help to tackle AMR, antimicrobial stewardship (AMS) programmes have been developed internationally to ensure that current antimicrobial options remain viable.5
An ageing population, an increase in chronic disease, and the shift of health services from secondary to primary care, combined with the difficulties in many countries to attract and retain GPs (also called primary care physicians), has meant that new models of primary care delivery have been developed worldwide.6,7 In many countries, an increasingly established approach to overcome this increasing shortage of human resources is task shifting, a process of delegation whereby tasks are moved to other specialized healthcare workers. Physician–nurse task shifting is carried out by transferring specific functions or tasks traditionally from the domain of physicians to nurses.8–16 A clinical task or function that many of these nurses now undertake is the prescription of medicines.
Within the UK, district nurses and public health nurses (previously known as health visitors) were the first groups of nurses enabled to prescribe independently from a restricted list of products. Later legislative changes in 2001 enabled any appropriately qualified registered nurse to prescribe any medicine independently for any condition within their area of competence, i.e. nurse independent prescribers (NIPs).17
In the UK, over 70% of antibiotic prescribing takes place in primary care and general practice.18,19 The UK government 5 year national action plan aims to reduce the use of antimicrobials in humans by 15% by 2024.20 In 2015, more than 6% of all dispensed antibiotics prescribed in England primary care were prescribed by NIPs, representing 13% of all nurse prescriptions.21 This demonstrates that nurses play a key role in AMS but their contributions and potential to have an impact on AMR is absent from the UK’s national action plan.22
The aim of our study was to analyse routinely collected data on NIP and GP numbers in England, and NIP and GP antibiotic prescriptions dispensed in the community in England, to identify: (i) the number of NIPs and GPs; (ii) the proportions of dispensed prescriptions for antibiotics written by NIPs and GPs; (iii) the types of antibiotics most frequently prescribed by these groups; and (iv) the impact of COVID-19 on the volume, rate and types of antibiotic prescriptions dispensed.
Methods
Design
This was a descriptive population-based retrospective cohort study using routinely collected data on NIP and GP antibiotic prescriptions dispensed in the community in England between January 2014 and October 2021.
Data sources
Dispensing data between January 2014 and October 2021 were obtained from the NHS Business Service Authority (NHSBSA) under a Freedom of Information (FOI) request. The NHSBSA Prescription Service provides prescribing information to prescribers and managing organizations within the NHS in England. The original request was for all prescriber types, with an indicator variable for prescriber type, and for monthly dispensing data of all antibiotics broken down into the BNF categories and a separate row covering ‘all other medicines’.
Data on the number of nurse prescribers working in England whose prescriptions were dispensed in the community were obtained from NHS Organisation Data Service ‘enurse’ file (https://digital.nhs.uk/services/organisation-data-service/file-downloads/gp-and-gp-practice-related-data). This dataset provided the cumulative month-on-month increase in the number of nurse prescribers writing prescriptions that were dispensed in the community, between 2014 and 2021. Annual data for years 2014–21 on nurses working in all settings in England and recorded as an NIP on the Nursing and Midwifery Council (NMC) register, were obtained from the NMC. The NMC is the regulator for the nursing profession in the UK.
Data on the number of GPs were obtained from General Practice Workforce Minimum Data Set (https://digital.nhs.uk/data-and-information/publications/statistical/general-and-personal-medical-services). We extracted GP headcount for the period January 2014 up to October 2021. Headcount provided us with the figure for the total number of GPs employed, regardless of whether they were part-time or full-time. These data were originally provided on a quarterly basis and then monthly from July 2021.
Statistical methods
Within the dispensing data from the NHSBSA, NIPs were identified by the roles of ‘community practitioner nurse’ or ‘nurse independent’; GPs working in primary care were identified by the roles ‘prescribing only doctor’ or ‘dispensing only doctor’. A ‘prescribing only doctor’ is able to write a prescription for a medicine dispensed in the community. Dispensing doctors are GPs who provide primary healthcare to patients living in a rural geographical area. At the patient’s request, dispensing doctors are allowed to dispense the medicines they prescribe to these patients. As our objective was to identify the number of GP antibiotic prescriptions dispensed in the community, the prescription data from both of these groups were included. Medical prescribing in hospitals was excluded. Antibiotics were summarized in aggregated form on a monthly basis, i.e. for 94 months from January 2014 until October 2021 inclusive, and also disaggregated by type, with a specific focus on penicillins, antibiotics commonly used to treat urinary tract infections (UTIs), BNF categories ‘sulphonamides/trimethoprim’ and ‘nitrofurantoin’, and other antibiotics commonly used to treat respiratory infections (BNF categories ‘macrolides’ and ‘tetracyclines’).
To investigate changes in the number of NIPs whose prescriptions were dispensed in the community for the years 2014 to 2021, we reported the total number of these nurses for each year using data from the enurse file, and expressed this as a percentage of the total number of NIPs across all settings, using data obtained from the NMC.
We calculated the total volume of dispensed NIP and GP prescriptions for antibiotics and antibiotic subtypes defined above, for each observed month. These data were based on courses of antibiotics, rather than individual antibiotic items. From this, we calculated the ‘rate of community-dispensed antibiotics prescribed by NIPs per NIP headcount’ by dividing dispensed prescription data from NHSBSA by community NIP headcount data from enurse. Similarly, we used the total number of GPs (headcount) to standardize the total number of dispensed antibiotics prescribed by GPs as a rate of dispensed antibiotics prescribed by GPs per GP headcount.
Data are reported in the text, tables and figures. Where data are reported in figures, we indicate the onset of control measures aiming to limit transmission of SARS-CoV-2, the respiratory virus that causes COVID-19. We classified everything from April 2020 to October 2021 as ‘following the onset of the COVID-19 pandemic’. In the UK, pandemic-related restrictions started to be introduced in mid-March 2020. This is indicated with a vertical dashed line at April 2020. Data were managed using SPSS V26.0 and analysed using Stata V16.0.
Results
Numbers of NIPs and GPs in England
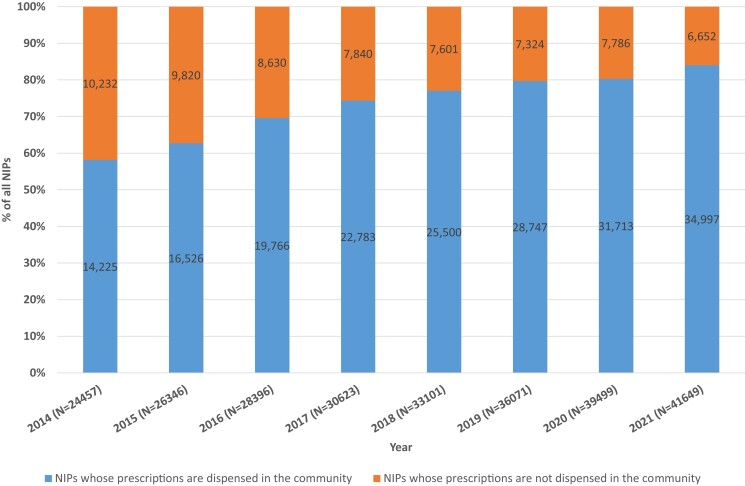
Between 2014 and 2021, the number of NIPs (headcount) in England almost doubled from 24 457 to 41 649. Of the 41 649 NIPs in 2021, the prescriptions of 34 997 (84%) were dispensed in the community (see Figure 1). The remaining 16% worked in settings in which prescriptions are not dispensed in the community, e.g. the hospital setting where in-patient prescriptions, commonly known as drug charts, are used. Between 2014 and January 2021, the number of these NIPs in England whose prescriptions were dispensed in the community rose from 14 225 to 34 997, i.e. a rise of 146% . Over the same time period, the number of GPs in England (headcount) rose from 40 584 in 2014 to 44 681 in 2021, i.e. a rise of 10% (see Table 1).
Figure 1.
Year-on-year change in the total number of NIPs and NIPs whose prescriptions are dispensed in the community. This figure appears in colour in the online version of JAC and in black and white in the print version of JAC.
Table 1.
Trends in NIP and GP antibiotic prescriptions dispensed in the community
| Year start | Number of NIPs (headcount) | Number of dispensed antibiotics prescribed by NIPs | Rate of dispensed antibiotics prescribed by NIPs (per NIP headcount) | Number of GPs (headcount) | Number of dispensed antibiotics prescribed by GPs | Rate of dispensed antibiotics prescribed by GPs (per GP headcount) | Total number of dispensed antibiotics | % prescribed by NIPs |
|---|---|---|---|---|---|---|---|---|
| 2014 | 14 225 | 265 417 | 18.66 | 40 584 | 3 250 250 | 80.09 | 3 515 667 | 7.5 |
| 2015 | 16 526 | 295 095 | 17.86 | 40 584 | 3 348 233 | 82.50 | 3 643 328 | 8.1 |
| 2016 | 19 766 | 279 364 | 14.13 | 41 193 | 2 854 373 | 69.29 | 3 133 737 | 8.9 |
| 2017 | 22 783 | 274 763 | 12.06 | 41 642 | 3 055 781 | 73.38 | 3 330 544 | 8.2 |
| 2018 | 25 500 | 299 539 | 11.74 | 41 999 | 3 146 170 | 74.91 | 3 445 709 | 8.7 |
| 2019 | 28 747 | 289 594 | 10.07 | 42 325 | 2 849 566 | 67.33 | 3 139 160 | 9.2 |
| 2020 | 31 713 | 294 676 | 9.29 | 43 368 | 2 761 229 | 63.67 | 3 055 905 | 9.6 |
| a 2021 | 34 997 | 187 802 | 5.37 | 44 681 | 1 921 321 | 43.00 | 2 109 123 | 8.9 |
| Total | 2 186 250 | 23 186 923 | 25 373 173 | 8.6 |
2021 data only run from January to October.
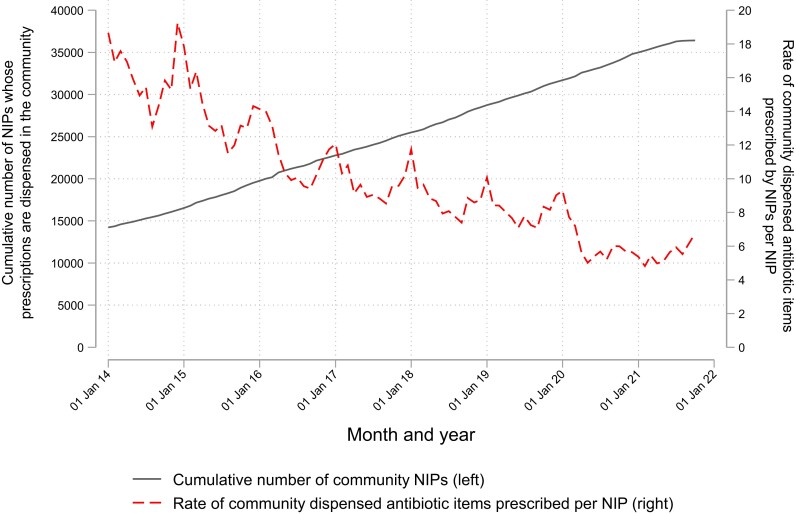
Volume and rate of dispensed antibiotic prescription items prescribed by NIPs and GPs
The total number of NIP prescription items dispensed in the community between January 2014 and October 2021 was 196 951 071. The number of these prescription items steadily increased year upon year. The total number of dispensed antibiotic prescription items issued by NIPs over the same time period was 2 186 250, representing 1.1% of the total number of NIP prescription items dispensed in the community (see Table 1). The proportion of all NIP prescribing that was antibiotics was lower at the end of the period, at less than 1%, than in 2014. On average, the annual rate of antibiotic prescriptions written by NIPs per NIP fell year on year from 18.66 at the end of 2014 to 9.29 at the end of 2020. This is a 50% relative reduction. The rate by the end of October 2021 was 5.37 (see Table 1). However, we only had access to data for 2021 from January to October and so this figure cannot be compared with annual rates.
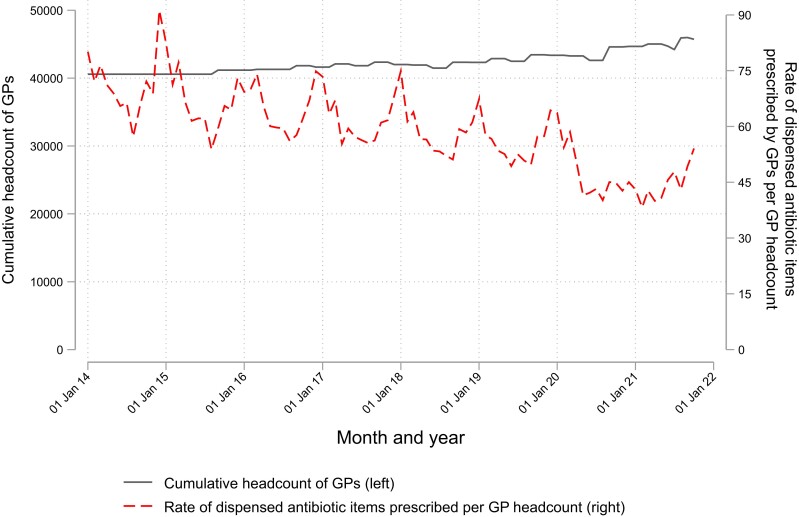
The total number of GP prescription items dispensed in the community between January 2014 and October 2021 was 8 246 357 234. The numbers of these prescription items remained steady year upon year (see Table 1). The total number of dispensed antibiotic prescription items issued by GPs over the same time period was 23 186 923, representing 0.3% of the total number of GP prescription items dispensed in the community. Over the whole period, GP antibiotic prescribing fell as a proportion of total prescribing. Individual GPs generally prescribe a higher volume of antibiotics than NIPs: over 80 items per annum by the end of 2014 and 64 (per GP headcount) by the end of 2020, representing a relative decrease of 21%. By the end of October 2021, the rate of dispensed antibiotics prescribed by GPs per GP headcount was 43 items. Of the 25.373 million antibiotic prescriptions dispensed between 2014 and 2021, NIPs were responsible for 8.6%. At the start of the observation period, 7.5% of all dispensed antibiotic prescriptions were prescribed by NIPs. This increased to 8.9% at the end of the observation period.
Types of antibiotics most frequently prescribed by NIPs and GPs and the impact of COVID-19
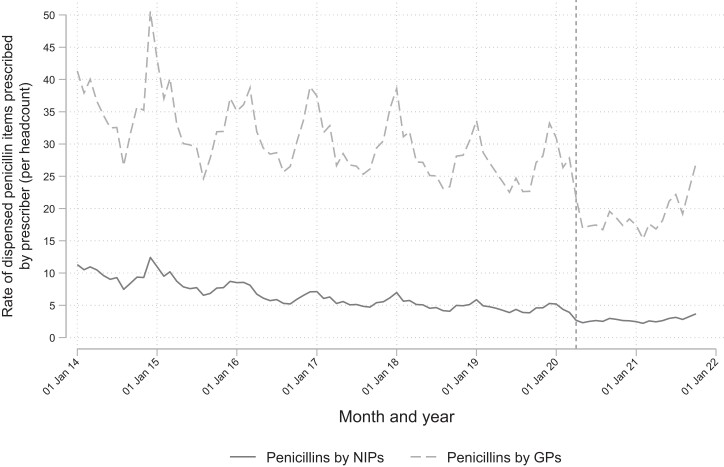
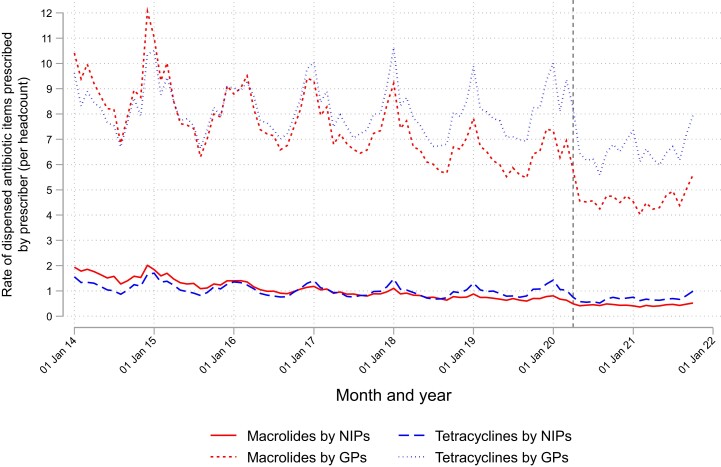
For GPs, the five most commonly dispensed antibiotic classes prescribed, which accounted for 92% of all dispensed antibiotics prescribed over the observation period, were penicillins (1 196 751 items), tetracyclines (331 781 items), macrolides (294 516 items), nitrofurantoin (256 793 items) and sulphonamides/trimethoprim (211 214 items). For NIPs, the five most commonly dispensed antimicrobials prescribed, which accounted for 96% of all dispensed antimicrobials prescribed, were penicillins (132 100 items), nitrofurantoin (27 699 items), tetracyclines (23 742 items), macrolides (21 507 items) and sulphonamides/trimethoprim (17 341 items).
Prior to the COVID-19 pandemic, there was a general decreasing trend in dispensed antibiotics prescriptions written by both NIPs and GPs over time, with regular winter peaks (see Figures 2 and 3). These trends and seasonal fluctuations were dominated by dispensed penicillin prescriptions that are typically used to treat respiratory tract infections. This decreasing trend continued following the onset of the pandemic, with a gradual upwards trend following this initial reduction. The winter peak observed in the years 2014–19 was absent during 2020.
Figure 2.
Change over time in NIP headcount and average number of dispensed antibiotics per NIP per annum. This figure appears in colour in the online version of JAC and in black and white in the print version of JAC.
Figure 3.
Change over time in GP headcount and average number of dispensed antibiotics per GP per annum. This figure appears in colour in the online version of JAC and in black and white in the print version of JAC.
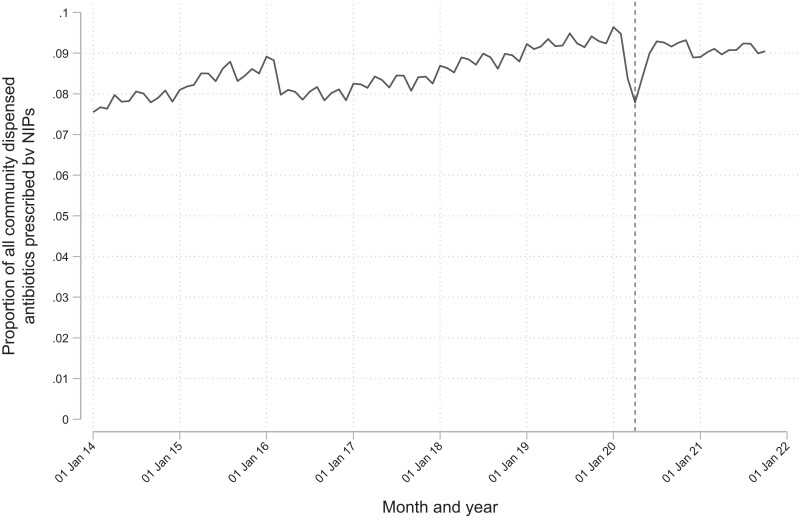
Around the time of the COVID-19 pandemic, the proportion of all dispensed antibiotics prescribed by NIPs decreased from 9.5% in February 2020 to 8.6% in March 2020 to 8.0% in April 2020 (relative decrease between February and April 2020 of 16%) before steadily climbing again (see Figure 4). The March to April 2020 relative decrease in dispensed antibiotic prescriptions was 41.2% for GPs and 20.8% for NIPs.
Figure 4.
Change over time in the proportion of all dispensed antibiotics prescribed by NIPs.
Respiratory tract infections (RTIs) and UTIs
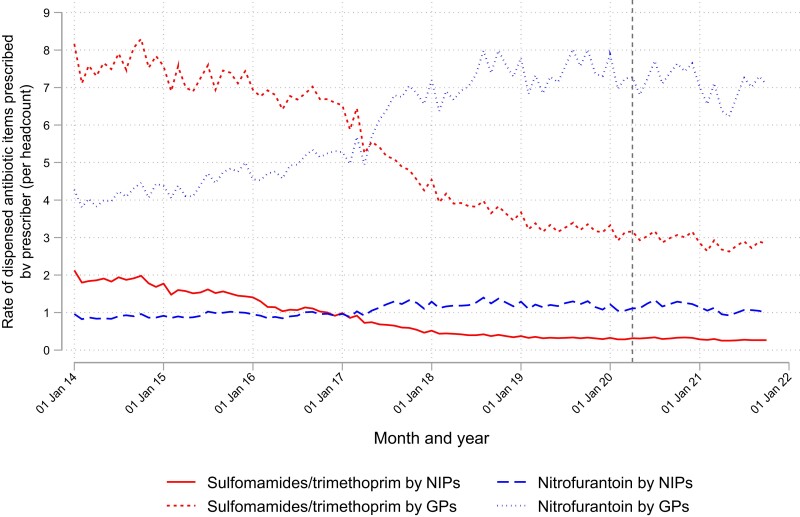
Figures 5, 6 and 7 compare the top five antibiotic classes grouped into those commonly used to treat UTIs (sulphonamides/trimethoprim and nitrofurantoin), penicillins and other antibiotics commonly used to treat RTIs, such as macrolides and tetracyclines. For penicillins, macrolides and tetracyclines there is a seasonal variation and a drop and lack of seasonal variation after the onset of the COVID-19 pandemic. From early 2017, there was a rise in the prescribing pattern of nitrofurantoin, and a fall in the prescribing patterns of sulphonamides/trimethoprim for both GPs and NIP. There were also no seasonal variation observed for these classes of antibiotics. There was, however, a drop in prescribing after the onset of the COVID-19 pandemic.
Figure 5.
Dispensed antibiotics commonly used to treat UTIs over time by antibiotic type and prescriber type. This figure appears in colour in the online version of JAC and in black and white in the print version of JAC.
Figure 6.
Dispensed penicillins over time by prescriber type.
Figure 7.
Dispensed antibiotics commonly used to treat RTIs over time by antibiotic type and prescriber type. This figure appears in colour in the online version of JAC and in black and white in the print version of JAC.
Discussion
Nurses now undertake roles traditionally filled by doctors.8–16 Although many of these nurses prescribe antibiotics,21 nurses are absent from the UK government’s 5 year national action plan,22 and surveillance data of antibiotic use in England23 do not differentiate between medical and non-medical healthcare professionals. To our knowledge, this is the first study that has examined the patterns of dispensed antibiotic prescription items written by GPs and NIPs and dispensed in the community in England.
Over 2 million prescription items, i.e. 1.1% of all dispensed NIP prescriptions, were for antibiotics. In 2014 the proportion of the total number of dispensed antibiotics prescribed by NIPs was 7.5%. This rose to 9.6% in 2020 and confirms that nurses are an increasing contributory influence on total antibiotic prescribing. Given the key role that nurses play in primary and community care services,8,24,25 these numbers will only increase.
The government aims to reduce the use of antimicrobials in humans by 15% in the UK.20 This study demonstrates that GPs and NIPs changed their prescribing behaviour between 2014 and 2020, reducing antibiotic prescriptions by 50% and 21%, respectively. GPs prescribed more antibiotics than NIPs year upon year during this period, even though the numbers of NIPs increased by 146% and GPs by 10%. In 2014, GPs prescribed over four times the amount of antibiotics compared with NIPs. This rose to nearly eight times the amount in 2021. This could be explained by consultation times, i.e. NIPs have been reported to have longer consultations than GPs, and therefore see fewer patients.11–13,15,26,27 It may also be that GPs see more complex patients (such as those who have recurrent chronic infections) and so would be more likely to prescribe an antibiotic to prevent infection. Whilst it has been reported by nurse prescribers that more complex cases should be seen by GPs owing to differences in clinical training (Williams et al., 2018),28 it would be interesting to see whether local triage processes result in nurse prescribers seeing ‘less complex’ cases. This would help to provide insight into the specific kinds of support that nurse prescribers and GPs require in terms of ensuring appropriate antibiotic prescribing.
In early 2020, there was a reduction in the number of antibiotics prescribed by NIPs and GPs. This is in line with surveillance data.23 This reduction was greater for GPs than NIPs. At this time, general practices switched from face-to-face service provision to remote working.29 In April 2020, 90% of GP and 46% of nurse consultations were delivered remotely.30 During this period, the number of face-to-face and remote appointments in the general practice setting fell by 20.80%,31 with the number of antibiotic prescriptions reported to be 6.7% higher than expected, supporting claims of inappropriate antibiotic use in remote consultations.32 The reduction in antibiotic prescriptions seen in our findings may therefore be as a result of reduced appointment numbers.
Diagnostic uncertainty (heightened in remote consultations due to the inability to physically examine patients) has been reported to influence NIP27 and GP33 antibiotic prescribing decisions, with GPs reporting that a prescription for an antibiotic is a safer option than not prescribing.33 During the initial phase of the pandemic, face-to-face consultations were less likely to involve RTIs, given public avoidance of medical services at that time.34 These consultations were more likely to be delivered remotely. NIPs may have been influenced to a greater extent than GPs by the inability to undertake a physical examination during a remote consultation. This may therefore account for the smaller reduction in NIP prescriptions for an antibiotic, compared with GPs, during the early phase of the pandemic.
Trends in antibiotic prescribing during the pandemic are reflected in individual classes of antibiotics prescribed for RTIs. By contrast, antibiotics prescribed for UTIs did not change during the pandemic.
Narrow-spectrum antibiotics were more commonly prescribed than broad-spectrum antibiotics, which are likely to lead to resistance.35,36 In line with guidance for the treatment of minor infections,37 narrow-spectrum antibiotics such as penicillins, macrolides and tetracyclines were the most frequently dispensed NIP and GP prescriptions for antibiotics. Although not differentiating between prescribers, this has also been observed in surveillance reports of antibiotic use in primary care.23
Our data do not enable us to make any judgement on the appropriateness of prescribing by NIPs and GPs, and more information is required to establish whether these prescribers are prescribing appropriately. However, the overall decrease in the rate of dispensed prescriptions for antibiotics by these groups, the most frequently prescribed antibiotics being narrow spectrum such as penicillins, tetracyclines and macrolides recommended when antibiotics are necessary,37 suggests that these prescribers are following government guidance for self-limiting minor infections such as acute cough, sore throat and sinusitis.38–40 The guidance for each condition differs slightly but, in general, antibiotics should not be offered, rather advice on self-care given for patients presenting who are not systemically very unwell or at higher risk of complications. Only those who are at a higher risk of complications and/or systematically very unwell or whose symptoms do not improve after around 7–10 days are offered antibiotics. The rise in dispensed NIP and GP prescriptions for nitrofurantoin can be explained by national infection guidelines,18 recommending its use in the treatment of community UTIs.
Nurses have an important role to play in AMS41 and are involved in a number of AMS activities.42,43 Our work provides evidence that nurse prescribers are an increasing contributory influence on total antibiotic prescribing. Interventions should be tailored to the population and context in which they are delivered.44,45 Although there is some work underway to develop an intervention to support appropriate antibiotic prescribing by NIPs and pharmacist independent prescribers,46,47 current interventions have been designed to target the antibiotic prescribing behaviour of GPs such as the TARGET and Start Smart - then Focus studies.48,49 Although these interventions could potentially target some of the drivers of behaviour among nurses, they are unlikely to target all of these drivers.27
Limitations
The data analysed only included data for NIP and GP prescriptions dispensed. Prescriptions written but not dispensed were not included. Therefore, our findings may not reflect the prescribing patterns of NIPs and GPs. Although our data do tell us the percentage of NIP and GP prescriptions for antibiotics, we were unable to determine whether prescribing was appropriate. Data for 2021 ran from January to October, therefore we were unable to compare annual rates with 2021 data. The total number of nurses whose prescriptions were dispensed in the community was used to standardize the total number of antibiotics prescribed by NIPs. However, although community nurse practitioners are increasingly playing a key role in primary and community care services, with many prescribing antibiotics,50 some do not prescribe antibiotics and so rates may appear low.
The data only included antibiotics prescribed on NHS prescriptions by NIPs and GPs. We have not included data on NIP- and GP-prescribed antibiotics on other types of NHS or private prescriptions. It would be challenging to access privately written prescriptions as there is no central database that contains these data. We do not know whether private prescriptions for antibiotics increased during the study period.
Conclusions
NIPs are an increasing contributory influence on total antibiotic prescribing and an important group to include in AMS efforts. NIPs prescribe fewer antibiotics than GPs but work under different conditions, e.g. longer consultations and less complex patients, so interventions should be tailored to this group and the population and context in which they are delivered.
Acknowledgements
We would like to thank Matt Griffiths and Sally Gilborson for their advice regarding primary and community care services.
Contributor Information
Molly Courtenay, School of Healthcare Sciences, Cardiff University, Cardiff, UK.
David Gillespie, Centre for Trials Research, School of Medicine, Cardiff University, Cardiff, UK.
Rosemary Lim, Reading School of Pharmacy, University of Reading, Reading, UK.
Funding
The study was carried out as part of our routine work through allocated research hours. The Centre for Trials Research receives funding from Health and Care Research Wales and Cancer Research UK.
Transparency declarations
None to declare.
References
- 1. CDDEP . The State of the World’s Antibiotics, 2015. 2015. https://onehealthtrust.org/wp-content/uploads/2015/09/the-state-of-the-worlds-antibiotics-_2015.pdf
- 2. WHO . WHO report on Surveillance of Antibiotic Consumption: 2016-2018 early implementation.2019. https://www.who.int/publications/i/item/who-report-on-surveillance-of-antibiotic-consumption.
- 3. Llor C, Bjerrum L. Antimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problem. Ther Adv Drug Saf 2014; 5: 229–41. 10.1177/2042098614554919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Antimicrobial resistance collaborators . Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet 2019; 399: 629–55. 10.1016/S0140-6736(21)02724-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Okeah BO, Morrison V, Huws JC. Antimicrobial stewardship and infection prevention interventions targeting healthcare-associated Clostridioides difficile and carbapenem-resistant Klebsiella pneumoniae infections: a scoping review. BMJ Open 2021; 11: e051983. 10.1136/bmjopen-2021-051983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Freund T, Everett C, Griffiths Pet al. Skill mix, roles and remuneration in the primary care workforce: who are the healthcare professionals in the primary care teams across the world? Int J Nurs Stud 2015; 52: 727–43. 10.1016/j.ijnurstu.2014.11.014 [DOI] [PubMed] [Google Scholar]
- 7. Roland M, Nolte E. The future shape of primary care. Br J Gen Pract 2014; 64: 63–4. 10.3399/bjgp14X676960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. NHS England . General Practice Forward View. 2016. https://www.england.nhs.uk/wp-content/uploads/2016/04/gpfv.pdf
- 9. Perloff J, DesRoches CM, Buerhaus P. Comparing the cost of care provided to Medicare 366 beneficiaries assigned to primary care nurse practitioners and physicians. Health Serv Res 2016; 51: 1407–23. 10.1111/1475-6773.12425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bonsall K, Cheater FM. What is the impact of advanced primary care nursing roles on patients, nurses and their colleagues? A literature review. Int J Nurs Stud 2008; 45: 1090–102. 10.1016/j.ijnurstu.2007.07.013 [DOI] [PubMed] [Google Scholar]
- 11. Hollinghurst S, Horrocks S, Anderson Eet al. Comparing the cost of nurse practitioners and GPs in primary care: modelling economic data from randomised trials. Br J Gen Pract 2006; 56: 530–5. [PMC free article] [PubMed] [Google Scholar]
- 12. Horrocks S, Anderson E, Salisbury Cet al. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ 2002; 324: 819–23. 10.1136/bmj.324.7341.819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Martin-Misener R, Harbman P, Donald Fet al. Cost-effectiveness of nurse practitioners in primary and specialised ambulatory care: systematic review. BMJ Open 2015; 5: e007167. 10.1136/bmjopen-2014-007167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Martínez-González NA, Tandjung R, Djalali Set al. The impact of physician–nurse task shifting in primary care on the course of disease: a systematic review. Hum Resour Health 2015; 13: 55. 10.1186/s12960-015-0049-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Martínez-González NA, Rosemann T, Djalali Set al. Task-shifting from physicians to nurses in primary care and its impact on resource utilization: a systematic review and meta-analysis of randomized controlled trials. Med Care Res Rev 2015; 72: 395–418. 10.1177/1077558715586297 [DOI] [PubMed] [Google Scholar]
- 16. Martínez-González NA, Rosemann T, Tandjung Ret al. The effect of physician-nurse substitution in primary care in chronic diseases: a systematic review. Swiss Medical Wkly 2015; 145: w14031. 10.4414/smw.2015.14031 [DOI] [PubMed] [Google Scholar]
- 17. Department of Health . Patients to get quicker access to medicines (press release). 2001.
- 18. PHE . Managing Common Infections: Guidance for Primary Care. 2021. https://www.gov.uk/government/publications/managing-common-infections-guidance-for-primary-care
- 19. UK Health Security Agency . English surveillance programme for antimicrobial utilisation and resistance (ESPAUR) report 2021 to 2022. 2022. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1118310/ESPAUR-report-2021-to-2022.pdf
- 20. Department of Health and Social Care . Tackling Antimicrobial Resistance 2019–2024: The UK’s Five-year National Action Plan. 2019. https://www.gov.uk/government/publications/addendum-to-the-uk-5-year-action-plan-for-antimicrobial-resistance-2019-to-2024/tackling-antimicrobial-resistance-2019-to-2024-addendum-to-the-uks-5-year-national-action-plan
- 21. Courtenay M, Gillespie D, Lim R. Patterns of dispensed non-medical prescriber prescriptions for antibiotics in primary care across England: a retrospective analysis. J Antimicrob Chemother 2017; 72: 2915–20. 10.1093/jac/dkx230 [DOI] [PubMed] [Google Scholar]
- 22. Courtenay M, Castro-Sanchez E, Fitzpatrick Met al. Tackling antimicrobial resistance 2019–2024: the UK’s five-year national action plan. J Hosp Infect 2019; 101: 426–7. 10.1016/j.jhin.2019.02.019 [DOI] [PubMed] [Google Scholar]
- 23. PHE . English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR): Report 2019 to 2020. 2020. https://webarchive.nationalarchives.gov.uk/ukgwa/20211022024510/https://www.gov.uk/government/publications/english-surveillance-programme-antimicrobial-utilisation-and-resistance-espaur-report
- 24. Health Education England . Primary care workforce commission report is a foundation for the short and long term. 2015. https://www.hee.nhs.uk/news-blogs-events/hee-news/primary-care-workforce-commission-report-foundation-short-long-term
- 25. Laurant M, van der Biezen M, Wijers Net al. Nurses as substitutes for doctors in primary care. Cochrane Database Syst Rev 2018; issue 7: CD001271. 10.1002/14651858.CD001271.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Leong SL, Teoh SL, Fun WHet al. Task shifting in primary care to tackle healthcare worker shortages: an umbrella review. Eur J Gen Pract 2021; 27: 198–210. 10.1080/13814788.2021.1954616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Courtenay M, Rowbotham S, Lim Ret al. Examining influences on antibiotic prescribing by nurse and pharmacist prescribers: a qualitative study using the Theoretical Domains Framework and COM-B. BMJ Open 2019; 9: e029177. 10.1136/bmjopen-2019-029177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Williams SJ, Halls AV, Tonkin-Crine Set al. General practitioner and nurse prescriber experiences of prescribing antibiotics for respiratory tract infections in UK primary care out-of-hours services (the UNITE study). J Antimicrob Chemother 2018; 73: 795–803. 10.1093/jac/dkx429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Majeed A, Maile EJ, Bindman AB. The primary care response to COVID-19 in England’s National Health Service. J R Soc Med 2020; 113: 208–10. 10.1177/0141076820931452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Murphy M, Scott LJ, Salisbury Cet al. Implementation of remote consulting in UK primary care following the COVID-19 pandemic: a mixed-methods longitudinal study. Br J Gen Pract 2021; 71: e166–77. 10.3399/BJGP.2020.0948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Armitage R, Nellums LB. Antibiotic prescribing in general practice during COVID-19. Lancet Infect Dis 2021; 21: e144. 10.1016/S1473-3099(20)30917-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Mehrotra A, Paone S, Martich GDet al. A comparison of care at e-visits and physician office visits for sinusitis and urinary tract infection. JAMA Intern Med 2013; 173: 72–4. 10.1001/2013.jamainternmed.305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Borek AJ, Maitland K, McLeod Met al. Impact of the COVID-19 pandemic on community antibiotic prescribing and stewardship: a qualitative interview study with general practitioners in England. Antibiotics 2021; 10: 1531. 10.3390/antibiotics10121531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Dilworth TJ, Brummitt CF. Reduction in ambulatory visits for acute, uncomplicated bronchitis: an unintended but welcome result of the coronavirus disease 2019 (COVID-19) pandemic. Infect Control Hosp Epidemiol 2021; 42: 1291–2. 10.1017/ice.2020.1233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. NHS England . Quality premium 2017/18 performance. 2018. https://www.england.nhs.uk/publication/quality-premium-2017-18-performance/
- 36. Thomson K, Berry K, Robinson Tet al. An examination of trends in antibiotic prescribing in primary care and the association with area-level deprivation in England. BMC Public Health 2020; 20: 1148. 10.1186/s12889-020-09227-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. NICE . Medicines optimisation: The safe and effective use of medicines to enable the best possible outcomes. 2015. https://www.nice.org.uk/guidance/ng5
- 38. NICE . Cough (Acute): Antimicrobial Prescribing. 2019. https://www.nice.org.uk/guidance/ng120/resources/visual-summary-pdf-6664861405
- 39. NICE . Sore Throat (Acute) in Adults: Antimicrobial Prescribing. 2023. https://www.nice.org.uk/guidance/ng84/resources/sore-throat-acute-in-adults-antimicrobial-prescribing-visual-summary-pdf-11315864557
- 40. NICE . Sinusitis (Acute): Antimicrobial Prescribing. 2017. https://www.nice.org.uk/guidance/ng79/resources/visual-summary-pdf-4656316717
- 41. Gotterson F, Buising K, Manias E. Nurse role and contribution to antimicrobial stewardship: an integrative review. Int J Nurs Stud 2021; 117: 103787. 10.1016/j.ijnurstu.2020.103787 [DOI] [PubMed] [Google Scholar]
- 42. Chater A, Family H, Abraao LMet al. Influences on nurses’ engagement in antimicrobial stewardship behaviours: a multi-country survey using the Theoretical Domains Framework. J Hosp Infect 2022; 129: 171–80. 10.1016/j.jhin.2022.07.010 [DOI] [PubMed] [Google Scholar]
- 43. Courtenay M, Castro-Sanchez E, Gallagher Ret al. Development of consensus based international antimicrobial stewardship competencies for undergraduate nurse education. J Hosp Infect 2019; 103: 244–50. 10.1016/j.jhin.2019.08.001 [DOI] [PubMed] [Google Scholar]
- 44. Germeni E, Frost J, Garside Ret al. Antibiotic prescribing for acute respiratory tract infections in primary care: an updated and expanded meta-ethnography. Br J Gen Pract 2018; 68: e633–45. 10.3399/bjgp18X697889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011; 6: 42. 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Courtenay M, Lim RH, Deslandes Ret al. A theory-based electronic learning intervention to support appropriate antibiotic prescribing by nurses and pharmacist: intervention development and feasibility protocol. BMJ Open 2019; 9: e028326. 10.1136/bmjopen-2018-028326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lim R, Courtenay M, Deslandes Ret al. Theory-based electronic learning intervention to support appropriate antibiotic prescribing by nurse and pharmacist independent prescribers: an acceptability and feasibility experimental study using mixed methods. BMJ Open 2020; 10: e036181. 10.1136/bmjopen-2019-036181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. RCGP . Target Antibiotic Toolkit Hub. https://elearning.rcgp.org.uk/course/view.php? id=553
- 49. PHE . Antimicrobial Stewardship: Start Smart—Then Focus. https://www.gov.uk/government/publications/antimicrobial-stewardship-start-smart-then-focus
- 50. Chater AM, Williams J, Courtenay M. The prescribing needs of community practitioner nurse prescribers: a qualitative investigation using the theoretical domains framework and COM-B. J Adv Nurs 2019; 75: 2952–68. 10.1111/jan.14170 [DOI] [PubMed] [Google Scholar]