Abstract
Invariant natural killer T (iNKT) cells are a subset of T cells that are characterized by a restricted T-cell receptor (TCR) repertoire and a unique ability to recognize glycolipid antigens. These cells are found in all tissues, and evidence to date suggests that they play many immunological roles in both homeostasis and inflammatory conditions. The latter include lung inflammatory diseases such as asthma and infections: the roles of lung-resident iNKT cells in these diseases have been extensively researched. Here, we provide insights into the biology of iNKT cells in health and disease, with a particular focus on the role of pulmonary iNKT cells in airway inflammation and other lung diseases.
Subject terms: NKT cells, Mucosal immunology
Immunology: cellular gatekeepers of pulmonary inflammation
A small subset of immune cells residing in the lung plays a pivotal part in governing the inflammatory response in a range of pulmonary disorders. Invariant natural killer T (iNKT) cells monitor the blood vessels in the lung for infection or other sources of tissue damage, which cause the cells to release chemical signals that rally a broader immune response. Doo Hyun Chung of Seoul National University, South Korea, and colleagues review the complex role of iNKT cells in determining the severity and outcome of respiratory disorders ranging from flu to pulmonary fibrosis. Sometimes iNKT cells are protective, for example by helping to quell the damaging inflammatory response associated with pulmonary fibrosis. However, some studies suggest that iNKT cells can exacerbate certain forms of asthma, highlighting the complexity of their physiological function.
Introduction
NKT cells are a unique subset of T cells that share features of both conventional T cells and natural killer cells. Unlike conventional T cells, NKT cells express TCRs that recognize glycolipid antigens loaded on CD1d, which is a nonpolymorphic major histocompatibility complex (MHC) class I-like protein1. NKT cells are classified into two distinct subsets (types I and II) on the basis of their TCR repertoire. Type I NKT cells express semi-invariant TCRβ chains combined with an invariant TCRα chain (Vα14 chain in mice and Vα24 chain in humans); these cells are, therefore, also called iNKT cells. They respond particularly strongly to α-galactosyl ceramide (α-GalCer), a marine sponge-derived glycolipid. In contrast, type II NKT cells have diverse polyclonal TCR repertoires that recognize lipid antigens such as sulfatide2. Studies on type II NKT cells are very limited due to the rarity of these cells and their lack of clear surface markers3. In contrast, iNKT cells have been extensively studied in many contexts because they are relatively abundant and can be readily identified with α-GalCer-loaded CD1d tetramers. The remainder of this review will focus on iNKT cells.
iNKT cells are largely sessile cells that reside in most tissues, including nonlymphoid tissues such as the liver, lungs, intestine, urogenital tract, adipose tissue, and skin4. However, their frequency relative to other lymphocytes varies depending on the tissue5,6. Thus, in mice, the lymphocytes in the liver are dominated by iNKT cells (10–30% of all lymphocytes). iNKT-cell dominance is also observed in murine adipose tissue (2–8% of all lymphocytes, 8–12% of adipose T cells), lungs (5–10% of all lymphocytes), and spleen (1–3% of all lymphocytes)6,7. In humans, iNKT cells are much less frequent in the liver (0.05–1% of all lymphocytes)8 and spleen (0.5–2% of all lymphocytes). However, they represent 10–25% of the T cells in adipose tissue, similar to their frequency in murine fat9. In contrast, the blood and thymus of both mice and humans contain low frequencies of iNKT cells (0.5–2%)10.
Although iNKT cells account for only ~1% percent of circulating T cells overall10, they often have a powerful immunological effect because of their abundant secretion of cytokines a few hours after activation of their TCR. Their cytokines include T-helper type-1 (Th1) cytokines, namely, interferon-gamma (IFN-γ) and tumor-necrosis factor-α (TNF-α); T-helper type-2 (Th2) cytokines, namely, interleukin (IL)-4 and IL-13; T-helper type-17 (Th17) cytokines, namely, IL-17A and IL-22; and the regulatory cytokine IL-1011. These cytokines impact various immune cells, ranging from innate immune cells such as macrophages, dendritic cells (DCs), and natural killer cells to adaptive immune cells such as T and B cells. Thus, iNKT cells can regulate both innate and adaptive immune responses. These regulatory activities have been found to play a role in many diseases, including rheumatoid arthritis12, asthma13, tumors14, and infectious diseases15.
Thymic development of iNKT cells
Similar to conventional T cells, iNKT cells develop in the thymus via four double-negative stages16 that eventually lead to TCRα chain-expressing CD4+CD8+ double-positive (DP) thymocytes. These cells then undergo positive selection with CD1d-presented glycolipids on DP thymocytes17. This differs from the development of conventional T cells, which are instead positively selected by MHC-presented peptides on thymic epithelial cells. iNKT-cell positive selection is driven by not only TCR activation but also costimulation signals from the signaling lymphocytic-activation molecule (SLAM) receptor on nascent iNKT cells; these signals induce the expression of the transcription factor early growth response protein 2 (Egr2), which is dispensable for conventional T-cell development18. Positively selected iNKT cells then enter unique development stages. The earliest is stage 0, which is characterized by CD24 expression. Stage 0 cells transition into the next stages, which can be defined differently depending on the proposed model. The linear maturation model, which is based on the expression of surface molecules such as CD24, CD44, and NK1.1, proposes that stages 1, 2, and 3 are characterized by CD24loCD44hiNK1.1−, CD24loCD44loNK1.1−, and CD24loCD44hiNK1.1+ phenotypes, respectively. In contrast, the lineage differentiation model, which is defined by transcription factor expression and cytokine production, proposes that stage 0 cells (NKT0s) develop into NKT1, NKT2, NKT17, and NKT10 subsets19–22. Thus, T-bet+ iNKT1s secrete Th1 cytokines (IFN-γ and TNF-α), Gata3+ iNKT2s produce Th2 cytokines (IL-4 and IL-13), and RORγt+ iNKT17s generate Th17 cytokines (IL-17A and IL-22)23–25. With regard to iNKT10s, their signature transcription factor remains unknown, but they secrete the anti-inflammatory cytokine IL-1021,26,27.
Recently, several groups employing single-cell RNA sequencing and unbiased computational analysis have proposed a third model that is based on transcriptional profiles and integrates both of the previous models. Thus, iNKT0 cells express Sox4, Lef1, and Id3, and their surface molecule phenotype is similar to that of stage 0 and 1 iNKT cells, namely, CD24+CD44–/loNK1.1−. iNKT1 cells express Ifng, Tbx21, Xcl1 and Il2rb and bear the stage 3 surface phenotype (CD24loCD44hiNK1.1+). iNKT2 cells express Il4, Gata3, Icos, and Zbtb16, and their surface molecule phenotype is that of stage 2 cells (CD24loCD44loNK1.1−). iNKT17 cells express Il17a, Rorc, Ccr6, and Itgb7 and bear the stage 2 surface phenotype23,24,28–30. Several studies have also shown that the thymic development of iNKT cells, but not conventional T cells, is regulated by specific cytokines (IL-15 and GM-CSF), SAP-Fyn signaling, other transcription factors (PLZF, Nur77, and SOX4), the epigenetic regulator and histone demethylase UTX, autophagy-related gene 7 (Atg7), and the microRNA miR-18131–38. Thus, a precise and unique machinery that differs from that used by conventional T cells is required for iNKT-cell development.
After thymic development, iNKT cells acquire some memory characteristics and exit the thymus39. They then travel to the peripheral tissues, where the iNKT pool is maintained unless cued otherwise26,40. Notably, the thymic iNKT-cell subsets (i.e., iNKT1, iNKT2, and iNKT17 cells) display different patterns of peripheral localization. For example, iNKT1 cells account for most of the iNKT cells in the liver, with the other subsets being infrequent. This may be due to their expression of different chemokine receptors and integrins41.
General characteristics of pulmonary iNKT cells
In the mouse lung, iNKT cells account for ~5% of the resident lymphocytes and localize in the interstitial space as well as the vasculature of the lungs42. All three iNKT-cell subsets are present in the lung. Interestingly, RNA sequencing analysis of iNKT cells in various tissues showed that pulmonary iNKT subsets share common characteristics in terms of their transcriptome profiles that distinguish them from iNKT cells in other tissues6,43. Specifically, all pulmonary iNKT cells, but not other iNKT cells, display high expression of AP-1, other bZIP family members, some NF-κB family members, CTLA-4, CD69, and Nur7743. It is likely that this unique transcriptome profile is driven by the homeostatic lung microenvironment since Lee et al. showed that the profile was unchanged by local infection or inflammation6,43. This notion is further supported by the fact that lung-resident mucosa-associated invariant T (MAIT) cells, γδ T cells, and alveolar macrophages also bear lung-specific signatures that are different from those of the corresponding cells in other tissues44–46.
Localization of pulmonary iNKT cells
After moving from the thymus into the circulation, iNKT cells accumulate in the lung microvasculature. When the lung tissue is stimulated by airborne antigens or infections that bear the glycolipid or microbial membrane component targets of iNKT cells, the iNKT cells extravasate into the interstitium and bronchiolo-alveolar spaces42. This is not observed in other organs; for example, the large numbers of iNKT cells in the liver remain within the microvasculature40. The trafficking of iNKT cells to the lung and their extravasation into the lung appears to be driven by (i) the chemokines that are generated by the lung tissue when it encounters airborne iNKT-cell ligands42 and (ii) iNKT-cell expression of a specific chemokine-receptor profile47. The chemokines include thymus-and-activation-regulated chemokine (TARC, also known as CCL17), MIG/CXCL9, and BCA-1/CXCL1341,48,49, while the iNKT-cell chemokine receptors include CCR4, CCR9, and CXCR647 (Fig. 1a). CCR4, in particular, appears to play a crucial role in iNKT-cell migration to the lungs and airways and the subsequent redistribution of iNKT cells within the lung. For example, aerosol administration of exogenous CCR4 ligand (TARC/CCL17) causes iNKT cells to promptly extravasate into the lung tissue42. Moreover, antibody-mediated neutralization of CCR4 or CCR4 deletion blocks iNKT cell migration to the lungs, thereby attenuating the airway hyperresponsiveness (AHR) induced in mice by pulmonary administration of antigen or αGalCer47–49. In addition, asthma patients have elevated levels of both CCR4 ligands (TARC/CCL17 and CCL22, which is also known as macrophage-derived chemokine) in their bronchoalveolar lavage fluid (BALF)50–53. Similarly, mice that are deficient in one component of another key pulmonary iNKT-cell chemokine/chemokine-receptor combination, namely, CXCR6 and its ligand CXCL16, bear significantly fewer iNKT cells within the intravascular compartment of the lungs40,42. Similar observations have been made for CCR9, the third pulmonary iNKT-cell chemokine receptor54–56.
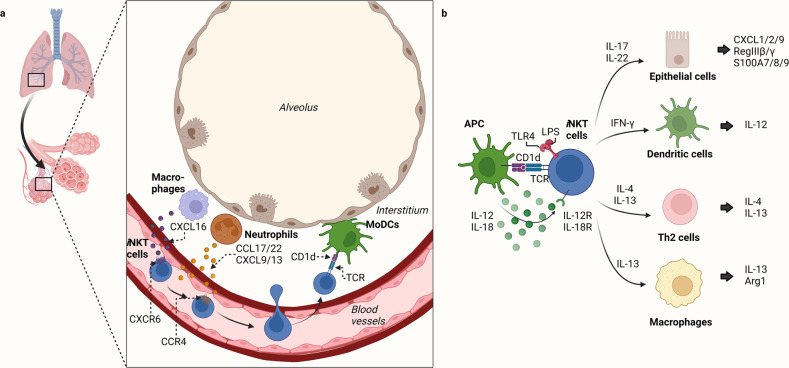
Fig. 1. Distribution of pulmonary iNKT cells and their interactions with other cells in the lung.
a Migration of iNKT cells to the lungs. After developing in the thymus, iNKT cells express CXCR6, a tissue localization molecule, and migrate to the CXCL16-expressing periphery. iNKT cells accumulate in the lumen of the lung microvasculature and then enter the lung tissue when neutrophils in the lung interstitium secrete the CCR4 ligands CCL17/22 and CXCL9/13. The neutrophils, therefore, guide the iNKT cells to the source of lung injury in the interstitium. The monocyte-derived DCs (moDCs) in this area present glycolipid antigens from the lung injury source to the iNKT cells, which become activated and then remain in the interstitium. b Crosstalk between iNKT cells and other cells in the lung. iNKT cells are activated by antigens expressed by lung antigen-presenting cells (APCs), such as MoDCs, by cytokines from other cells (such as IL-12/18), and by TLR ligands (e.g., LPS). The activated iNKT cells then secrete a variety of cytokines that regulate the function of many types of neighboring cells.
Notably, intravital imaging of the lung tissue showed that neutrophils play a key role in the α-GalCer- or Streptococcus pneumoniae infection-induced migration of pulmonary iNKT cells from the vasculature into the interstitium; specifically, neutrophils produce CCL17, which guides the migration of iNKT cells through the lung tissue. Antigen-presenting cells (APCs), including monocyte-derived DCs, also play an important role in iNKT-cell migration: they promote neutrophil extravasation into the lung and present antigen to iNKT cells, thereby halting further migration of these cells57 (Fig. 1a).
Activation of pulmonary iNKT cells
iNKT cells are most often activated by recognizing glycolipid antigens presented on CD1d58 (Fig. 1b). While many immune cells express CD1d on their surface, DCs are the most potent APCs in terms of glycolipid:CD1d-induced iNKT-cell activation59,60. While the most potent glycolipid identified to date is α-GalCer61, several studies have shown that iNKT cells can also recognize glycolipids from various microorganisms62. For example, the transfer of Sphingomonas-pulsed DCs into mice successfully activated lung-resident iNKT cells; the stimulatory ligands were found to be α-galacturonosylceramide and α-glucuronosylceramide63. Moreover, mycobacterium-derived phosphatidylinositol mannoside can activate iNKT cells64. Thus, despite the restricted TCR repertoire of iNKT cells, they may recognize a wider range of glycolipid antigens than initially thought.
Another common mechanism by which iNKT cells are activated is the signaling induced by cytokines65 from surrounding immune cells, particularly DCs66 (Fig. 1b). For example, when DCs are activated by the engagement of Toll-like receptors (TLRs) on their surface, they produce IL-12, which successfully activates pulmonary iNKT cells even when CD1d is absent67. The importance of this mechanism is supported by the constitutive expression of the IL-12 receptor of iNKT cells and the fact that they rapidly upregulate their STAT4 expression when they encounter IL-12. Similarly, IL-18 and type-1 interferon produced by DCs can also induce pulmonary iNKT cells to secrete their own cytokines68–70.
Finally, iNKT cells can be activated by their own innate immune sensors, including TLR4. Flow cytometry and confocal microscopy analyses show that iNKT cells express TLR4 on their surface and in their endosomes and that simultaneously stimulating TCR and TLR4 on iNKT cells increases their expression of IFN-γ. Notably, this dual stimulation also decreases iNKT-cell expression of IL-4, which suggests that the TLR4 signaling pathway skews iNKT cells toward type-1 immune responses. Notably, this regulatory skewing appears to be particularly important for several lung diseases. For example, we showed that while the adoptive transfer of LPS-treated iNKT cells (LPS stimulates TLR4) suppresses pulmonary fibrosis, it worsens hypersensitivity pneumonitis71.
Taken together, these studies suggest that pulmonary iNKT cells can be activated via multiple mechanisms, although the mechanism that plays the most prominent role in lung health and disease remains to be determined. These observations also suggest that pulmonary iNKT cells may be readily activated in pathological environments that bear iNKT-cell antigens, cytokines from other immune cells, and/or TLR-activating molecules. Indeed, it is likely that such environments activate pulmonary iNKT cells via several or all of these mechanisms. Further improving our understanding of these mechanisms is important for enhancing our understanding of pulmonary iNKT cells.
Functions of pulmonary iNKT cells
iNKT cells exert their immune effects in vivo via several mechanisms. The most prominent involves iNKT-cell secretion of cytokines and other soluble factors65. Consequently, most studies on iNKT-cell functions have focused on this mechanism. Given that multiple iNKT-cell subsets exist (i.e., iNKT1, iNKT2, iNKT17, and iNKT10), iNKT cells are considered multipotent cytokine-secreting cells. This ability to secrete powerful cytokines with opposing properties also suggests that these cells can regulate the cytokine production of neighboring immune cells in various ways, thus controlling the entire cytokine milieu (Fig. 1b). Indeed, there are many cases of this in the literature. For example, iNKT cells secrete granulocyte-macrophage colony-stimulating factor (GM-CSF), which promotes macrophage production of IL-1β. Conversely, they also express IL-4, which promotes M2-macrophage differentiation; this inhibits macrophage secretion of IL-1β in vitro11. Another example is that the IL-4 secreted by iNKT cells can suppress the IFN-γ production of neutrophils in the respiratory tract72. Conversely, iNKT cells can themselves secrete IFN-γ, which in turn regulates neutrophil production of IL-10 and C5a in a sepsis model73. Thus, iNKT cells have the clear potential to balance immune responses via their versatile secretion of powerful cytokines.
Indeed, the cytokine production of iNKT cells has been shown to facilitate or even play a critical role in immune diseases such as autoimmunity, allergy, infection, and cancer6,65,74–76. More specifically, the cytokine production of iNKT cells has been implicated in numerous lung conditions, including allergic asthma77, mycobacterium infection78, viral infection79, chronic obstructive pulmonary disease (COPD)80, pulmonary fibrosis81, hypersensitivity pneumonitis72, and immune complex-induced lung injury82. Of the many soluble factors that pulmonary iNKT cells can secrete, IL-4 and IFN-γ appear to play particularly important roles in respiratory tract diseases83,84. Other important soluble factors include IL-17, IL-22, and IL-13, which regulate the activities of neighboring cells such as helper T cells85, lung epithelial cells86, DCs13,87, and macrophages88. The roles of these factors in lung disease are detailed further below (Fig. 1b).
Other mechanisms by which iNKT cells exert immune effects include cytotoxicity and cell-to-cell contact-mediated immune regulation89. However, research on the roles of these mechanisms in lung diseases is lacking.
It should be noted here that iNKT cells can play both beneficial roles, such as protecting the lungs from tuberculosis (TB)90, and detrimental roles, such as driving COPD by producing IL-1791. Further research on the roles of pulmonary iNKT cells in respiratory tract diseases is likely to be particularly valuable because it may promote the development of novel therapeutic targets.
Metabolism of pulmonary iNKT cells
Although little is known about the metabolism of pulmonary iNKT cells, it can be inferred by examining the metabolic properties of peripheral iNKT cells and the metabolic environment of the lung. Before we discuss these points, we will first describe what is known about the metabolism of conventional T cells. These cells first engage in glycolytic metabolism, which is induced by PI3K-Akt signals from the pre-TCR and Notch1 during β-selection in the thymus92. Thereafter, mature naïve quiescent T cells in the periphery primarily utilize oxidative phosphorylation (OXPHOS) or fatty acid oxidation (FAO) to generate ATP; thus, fatty acids are their main energy source. However, once T cells are activated, they switch to aerobic glycolysis93 for ATP production and primarily use glucose as their fuel source. While this is less efficient than glycolysis, this switch provides the rapid energy needed for effector T-cell long-term survival, proliferation, cytokine secretion, and migration to sites of inflammation92,94.
Although the proliferation of developing iNKT cells appears to rely on glucose utilization, glycolysis has been suggested to exert a negative effect on the function of iNKT cells since glucose uptake and Glut1 expression are higher in immature iNKT cells present in the thymus than in mature iNKT cells34,95. Glucose uptake and Glut1 expression are attenuated in mature iNKT cells and upregulated when there are defects in developmental factors of iNKT cells, including Keap1 or PLZF34,96,97. Furthermore, iNKT cells are more susceptible to modifications in the function of the mitochondrial electron transport chain than conventional T cells. The crucial role of mitochondrial metabolism in the development and function of iNKT cells is exerted through the regulation of TCR/IL-15 signaling and NFAT activity98.
Peripheral iNKT cells bear memory T-cell features such as high cell surface expression of CD44 and retention of antigen specificity after maturation and antigen exposure99. Moreover, these cells are in a ready-to-respond state that allows them to produce cytokines within hours, even when they are only stimulated by interleukins such as IL-12 and IL-18100. Thus, peripheral iNKT cells are similar to memory T cells in that their metabolism allows rapid responsiveness. However, while conventional effector/memory, CD4+ T cells use glucose for glycolysis, which leads to lactate production, iNKT cells metabolize glucose via the pentose phosphate pathway and OXPHOS, and these pathways are essential for their survival, proliferation, and cytokine production96. This is supported by the fact that iNKT cells have higher ATP levels than CD4+ T cells both before and after activation96. Moreover, peripheral iNKT cells display lower glucose uptake than conventional CD4+ T cells due to the inhibitory effect of PLZF on glycolysis96. Finally, although both CD4+ T and iNKT cells require glutamine to proliferate, CD4+ T cells need glucose to expand optimally, whereas iNKT cells depend on fatty acid metabolism96.
The metabolism of iNKT cells in the lungs may be shaped by the metabolic environment in the lung. This environment is determined by several dynamic and complex factors, including mucus and microbacterial components. The mucus is produced by the airway epithelium. Since it is a rich source of nutrients for bacteria, it can affect the metabolic activity of these microorganisms101. Moreover, microbacterial components such as LPS and other bacterial byproducts can create a complex metabolic environment that alters the local pH, oxygen levels, and nutrient availability. This can affect the metabolism and consequent energy production and cellular behavior of not only the microorganisms but also the host cells102, including local iNKT cells. It seems likely that pulmonary iNKT cells are characterized by a specific metabolomic profile that promotes their use of metabolic pathways such as fatty acid metabolism.
iNKT-cell responses are now known to be highly dependent on their synthesis of lipids. For example, compared to conventional T cells, iNKT cells express higher levels of PPAR-γ, a master regulator of lipid metabolism. They also increase their cholesterol synthesis after activation, which is needed for their TCR signaling, proliferation, and production of IFN-γ. Interestingly, however, blocking cholesterol synthesis only slightly diminished the production of IL-4 by activated iNKT cells; rather, glucose appeared to be more critical for IL-4 production by iNKT cells103. The influence of lipid biosynthesis on iNKT-cell function is highlighted by the fact that iNKT cells skew toward an iNKT1 phenotype.
iNKT cells in pulmonary diseases
Despite their relatively low numbers in the lungs, pulmonary iNKT cells appear to play vital roles in host defense against microorganisms. This role involves them patrolling the lumen of the pulmonary vessels and the interstitial tissue until the lung tissue is injured by infection and emits danger signals. Such signals cause iNKT cells to migrate to the injured site, which contains glycolipid antigens, and induce iNKT cells to elicit early host defense mechanisms. However, pulmonary iNKT cells can also participate in the pathogenesis of various lung diseases104, either via direct pathogenic effects of their cytokines or more indirectly via regulation of neighboring immune-cell subset functions105. The triggers that generate pathogenic iNKT-cell activity are generally the same as those that initiate protective iNKT-cell responses, namely, glycolipid antigens and/or the surrounding cytokine milieu. Below, we will summarize what is known about the role of iNKT cells in the four most common lung diseases (asthma, mycobacterium infection, viral infection, and COPD) as well as several more minor pulmonary diseases.
Asthma
Asthma is a common respiratory disease that affects millions of people worldwide104. Its cardinal feature is AHR, but there are several distinct forms of asthma that are underpinned by disparate pathogenic pathways106,107. The most common form is allergic asthma, which is triggered by allergens and is characterized by Th2-immune responses, eosinophil infiltration, high IgE levels, and AHR108. Another important endotype is nonallergic asthma, which is Th2-independent and characterized by lung/airway neutrophil infiltration, Th17-immune responses, and AHR109.
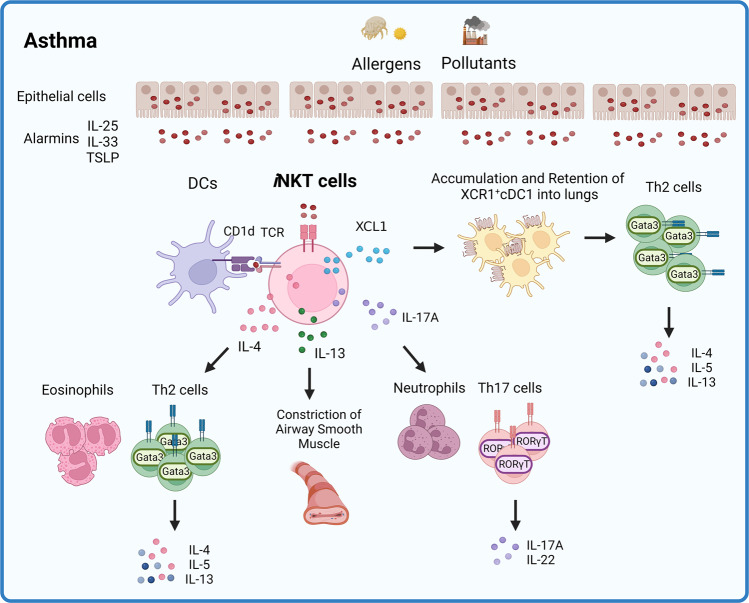
Studies in mice110–112 and nonhuman primates113 show that iNKT cells can directly trigger the development of asthma. For example, intranasal administration of α-GalCer114 or Sphingomonas-derived glycolipids in mice induces AHR54. Moreover, IL-4 and particularly IL-13 from iNKT cells are key drivers of allergic asthma83: IL-4 facilitates the overall Th2 response in allergic lungs, while IL-13 acts as a direct pathogenic factor83 by inducing lung epithelial cell contraction115. The triggers for IL-4/IL-10 secretion by iNKT cells are IL-25, thymic stromal lymphopoietin (TSLP), and IL-33: these so-called ‘alarmin’ cytokines are released by injured lung cells, can directly activate iNKT cells and are abundant in early asthmatic lungs116. Similarly, iNKT cells help drive the development of Th17-mediated asthma. While less is known about the role of iNKT cells117,118, it has been shown that intranasal administration of α-GalCer causes pulmonary CD4−NK1.1− iNKT cells to secrete IL-17119, which promotes airway neutrophilia and AHR. This was also observed when a more physiological model of IL-25-dependent AHR was employed120 (Fig. 2).
Fig. 2. Roles of pulmonary iNKT cells in asthma pathogenesis.
Inhaled allergens or pollutants cause lung epithelial cells to release alarmins and dendritic cells (DCs) to present the antigens contained in these environmental insults. Both the alarmins and the DCs then activate iNKT cells. Activated iNKT cells subsequently secrete cytokines that modulate the function of various immune cells or cause airway smooth muscle constriction. In particular, iNKT cells promote the recruitment and lung retention of XCR1-expressing cDC1s by secreting the chemokine XCL1. The XCR1+ cDC1s subsequently amplify the type-2 immune responses during asthma.
Our recent study13 on the role of iNKT cells in murine allergic asthma models induced by ovalbumin (OVA) and house-dust mite (HDM) suggests that iNKT cells also promote the development of allergic asthma by enhancing the migration of XCR1-expressing type-1 conventional DCs (cDC1s) into asthmatic lungs. This migration appears to be driven by iNKT-cell production of X-C-motif chemokine ligand 1 (XCL1). This ligand may be specific for cDC1s since they are the only immune-cell subset that appears to express the receptor for XCL1 (XCR1). The importance of this iNKT cell-cDC1 relationship was demonstrated by the fact that XCL1-knockout (KO), XCR1-KO, and Jα18-KO (which lack iNKT cells) mice failed to develop AHR and Th2-immune responses, which was associated with diminished cDC1 infiltration into the lungs. This iNKT cell-cDC1 relationship was confirmed by adoptively transferring wild-type (WT) or XCL1-deficient iNKT cells into Jα18-KO mice: the WT cells, but not the XCL1-deficient cells, induced AHR and cDC1 migration into the lungs. Similarly, adoptive transfer of WT cDC1s into XCL1-KO, XCR1-KO, or Jα18-KO mice induced AHR. Notably, we also showed that once cDC1s entered the lungs, they activated the Th2 responses of CD4+ T cells13. This is interesting because cDC1s are generally thought to regulate CD8+ T-cell responses121. Our finding is supported by Nakano et al., who also showed that cDC1s can regulate the Th2 responses of CD4+ T cells in allergic asthma122. Thus, iNKT cells play critical roles in the murine asthma model by not only generating directly pathogenic cytokines but also recruiting key cells that then evoke the pathogenic activities of Th2 T cells (Fig. 2).
It should be noted that there is some controversy about the importance of iNKT cells in murine asthma models123 because several studies have shown that KO of Jα18 or CD1d (and therefore iNKT cells) has no effect on the development of asthma in commonly used murine models (the OVA and HDM models)124,125. This may reflect differences in microbiota between animal facilities since germ-free mice show increased pulmonary iNKT-cell numbers126. However, the role of iNKT cells in asthma is even more controversial in humans. While Akbari et al. showed that the BALF of patients with moderate to severe asthma had very high frequencies of iNKT cells (60% of CD3+ cells)83, other groups observed frequencies of only ~2%. These disparities may reflect improper flow cytometric analysis, nonspecific binding of the CD1d tetramers used, or differences in patient cohorts. As an aside, the BALF of childhood asthma patients bears increased iNKT-cell numbers127, which suggests that iNKT cells may participate in juvenile asthma. Overall, it seems possible that iNKT cells promote asthma, although this role may only emerge in specific conditions.
Mycobacterium infection
TB remains a serious public health concern worldwide: approximately 2 million people die per year from this disease128. This reflects the high contagiousness of the pathogenic Mycobacterium species (M. tuberculosis, M. bovis, M. microti, and M. africanum129) and the poor protection generated by the Bacillus Calmette–Guerin vaccine in adults130.
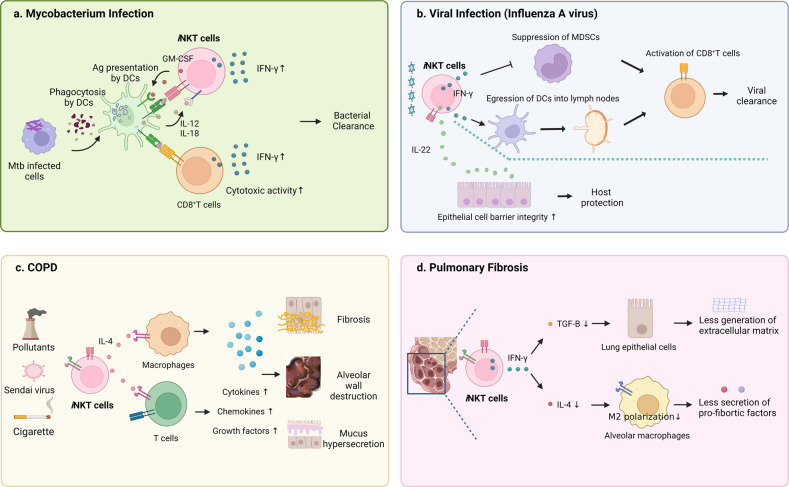
The role of iNKT cells in TB has been studied in murine models. iNKT cells in infected mice are activated by not only CD1d-presented mycobacterial antigen131 but also cytokines in the environment such as IL-12 and IL-18132: the resulting activated iNKT cells help protect the mice from the infection78. This role is partly mediated by the GM-CSF secretion of iNKT cells: this activates cDC1s, which in turn promote the antimicrobial activities of CD8+ T cells133. Another mechanism is that iNKT cells facilitate the priming of T cells against TB infection: treatment of TB-infected mice with α-GalCer increases the numbers of TB antigen-specific IFN-γ-producing T cells in the lung134. Finally, it is possible that iNKT cells exert their protective abilities in TB by releasing IFN-γ and engaging in cytotoxicity: when iNKT cells from M. tuberculosis or M. bovis-infected mice were cocultured in vitro with infected macrophages, the iNKT cells secreted IFN-γ and killed the macrophages132 (Fig. 3a). However, this function remains to be validated in vivo.
Fig. 3. Role of pulmonary iNKT cells in various lung diseases.
a In mycobacterium infection, cDC1s activate pulmonary iNKT cells by secreting IL-12 and IL-18 and by presenting antigen on CD1d. The iNKT cells then reciprocally stimulate the cDC1s via GM-CSF, which activates the cytotoxic CD8+ T cells that eliminate the infected cells and clear the bacteria. This activity is further supported by the IFN-γ produced by the iNKT cells. b During lung viral infections, pulmonary iNKT cells produce IFN-γ, which downregulates myeloid-derived suppressor cells (MDSCs), which would otherwise suppress CD8+ T cells. Moreover, iNKT cells promote the maturation of DCs and their migration to draining lymph nodes by IFN-γ, which enhances CD8+ T-cell responses. Finally, iNKT cells protect the host by increasing epithelial cell integrity by producing IL-22. c COPD pathogenesis is promoted by IL-4-secreting iNKT cells. IL-4 generates IL-13-secreting macrophages and activates T cells, which in turn secrete many cytokines, chemokines, and growth factors that directly induce fibrosis, alveolar wall destruction, and mucus hypersecretion. d Pulmonary fibrosis is inhibited by iNKT cells. The mechanism involves iNKT-cell expression of IFN-γ, which suppresses the production of the master profibrotic regulator TGF-β in the lung. This blocks the extracellular matrix (ECM) production that is responsible for pulmonary fibrosis. Another mechanism involves downregulating lung expression of IL-4, which inhibits the polarization of lung macrophages to the M2 phenotype. This phenotype plays an important role in fibrosis by producing type-2 cytokines and large amounts of TGF-β.
With regard to humans, the iNKT cells in the sputum of TB patients bear activated phenotypes and secrete high IFN-γ levels135. However, their numbers are significantly decreased. Interestingly, these cells express high levels of PD-1 on their surface and have a tendency to undergo apoptosis. Indeed, when these cells were treated in vitro with a PD-1 blocker, the iNKT-cell frequency rose136. Moreover, the decreased iNKT-cell numbers in the blood of humans normalize after TB is eliminated by treatment137. Notably, cocultured human iNKT cells can also kill M. tuberculosis-infected macrophages in vitro138. This supports the murine in vitro study above that suggests iNKT cells can protect the host from TB infection via cytotoxicity132.
These preclinical and clinical studies suggest that iNKT cells can protect against TB infection. Thus, cell-based therapies with iNKT cells may be useful for TB patients139. This is supported by a study showing that when iNKT cells were activated exogenously with α-GalCer and then transferred into mice, the mice were protected from lethal TB infection140. Another possibility is to incorporate α-GalCer into the Bacillus Calmette–Guerin vaccine: this strategy has been shown to enhance the overall immune response of TB-infected mice134.
Viral infections
Influenza A virus
Influenza A virus (IAV) is another common cause of respiratory tract disease. It is especially prominent during winter and can cause severe and sometimes fatal lung damage. It can also increase host susceptibility to secondary bacterial infections141.
Pulmonary iNKT cells protect mice from the H1N1 and H3N2 IAV strains since iNKT cell deficiency (Jα18-KO and CD1d-KO) resulted in more severe bronchopneumonia, greater weight loss, and shorter time to death142,143. Moreover, treatment with exogenous α-GalCer before IAV infection reduces infection-induced weight loss and increases CD8+ T- and NK-cell responses to IAV infection; the latter effects are due to IFN-γ secreted by iNKT cells144 (Fig. 3b). There are also several other mechanisms by which iNKT cells protect the host from IAV. First, they downregulate myeloid-derived suppressor cells, which inhibit the CD8+ T-cell responses that limit IAV replication during moderate H1N1 infection143. Second, they promote the maturation of DCs and their migration to draining lymph nodes, which enhances CD8+ T-cell responses during severe H3N2 infection142. Third, iNKT cells protect the host from excessive lung damage by producing IL-22, which may strengthen the epithelial barrier integrity of host lungs86. Fourth, iNKT cells reduce the local levels of MCP-1. This decrease downregulates the accumulation of inflammatory monocytes in the lungs, which diminishes the overall damage to the lung tissue. This, in turn, promotes the survival of mice infected with a highly pathogenic strain of IAV88. Thus, iNKT cells help block the deleterious effects of IAV infection by both promoting anti-viral responses and protecting the lung tissue of the host (Fig. 3b).
COVID-19
Only a few studies have assessed the role of iNKT cells in the recent pandemic caused by SARS-CoV-2 infection. One recent study reported that patients with severe COVID-19, but not patients with mild COVID-19, demonstrate a tenfold reduction in pulmonary iNKT-cell frequencies145. However, another group found that COVID-19 patients and healthy individuals did not differ markedly in iNKT-cell frequencies146. Another study showed that COVID-19-mediated pneumonia was associated with elevated eosinophil and neutrophil numbers in the sputum and BALF and that these numbers correlated positively with the numbers of iNKT cells in peripheral blood and BALF. This suggests that iNKT cells could play a pathogenic role in COVID-19147. Finally, hematopoietic stem cell (HSC)-engineered iNKT cells, which were differentiated from TCR-engineered HSCs, efficiently killed SARS-CoV-2-infected cells in vitro148. Thus, iNKT cells may help protect the host from SARS-CoV-2 infection by killing infected cells. These observations together suggest that iNKT cells are involved in COVID-19-related immune responses. However, whether their role is primarily protective or pathogenic remains to be determined.
Chronic obstructive pulmonary disorder (COPD)
The frequency and severity of COPD has steadily increased over the last few decades, and COPD now affects more than 200 million people worldwide and is the fourth leading cause of death149. COPD is characterized by lung tissue emphysema, respiratory bronchiolitis, and eventual chronic bronchitis150.
Key risk factors for COPD are cigarette smoke and industrial pollutants150. Several studies suggest that iNKT cells play pathogenic roles in COPD. First, the murine cigarette smoke model of COPD features increased pulmonary iNKT-cell numbers. Second, both Jα18-KO and CD1d-KO mice are resistant to forming COPD based on exposure to cigarette smoke80. Third, repeated intranasal administration of α-GalCer can induce COPD, and this is ameliorated when an anti-IL-4 antibody is coadministered80. Fourth, consistent with the mouse COPD model, COPD patients have greater iNKT-cell numbers in their peripheral blood and sputum than healthy individuals151. Fifth, iNKT cells from COPD patients produce high levels of IFN-γ and IL-17A that can activate cigarette smoke extract-exposed lung DCs or airway epithelial cells in vitro91. Sixth, iNKT-cell deficiency ameliorates symptoms in the Sendai virus infection model of COPD. This is mediated by iNKT-cell downregulation of the numbers of IL-13+ macrophages, which are critical COPD regulators because IL-13 derived from these cells directly induces goblet cell metaplasia, AHR, and mucus production. This mechanism may also participate in human COPD since the lungs of COPD patients demonstrate elevated numbers of not only iNKT cells but also IL-13+ CD68+ macrophages152 (Fig. 3c). Thus, it is likely that iNKT cells promote COPD pathogenesis, possibly by direct and/or indirect interactions with IL-13+ macrophages.
Pulmonary fibrosis, hypersensitivity pneumonia, and immune complex-induced lung injury
Our studies suggest that pulmonary iNKT cells also play critical protective or pathogenic roles in pulmonary fibrosis, hypersensitivity pneumonitis, and immune complex-induced lung injury, as detailed below.
Pulmonary fibrosis
Pulmonary fibrosis is characterized by progressive scarring of the lungs and the eventual development of lung interstitial fibrosis. This results in progressive shortness of breath153. Since this disease is caused by excessive extracellular matrix (ECM) production by fibroblasts in the lungs154, the recruitment, proliferation, and ECM production of fibroblasts have been extensively studied. At present, it is thought that these fibroblast activities are largely driven by transforming growth factor beta (TGF-β), which is a potent profibrotic mediator155.
Two studies suggest that iNKT cells can play protective roles in pulmonary fibrosis by downregulating TGF-β expression81,156. First, we found that CD1d-KO mice developed more severe bleomycin-induced pulmonary fibrosis than WT mice, as shown by their worse lung histology, higher hydroxyproline levels, and greater mortality64. These severe effects were associated with higher TGF-β levels and lower IFN-γ levels in the lungs. Moreover, the adoptive transfer of WT iNKT cells into CD1d-KO mice not only ameliorated the severity of the disease in these mice but also restored the IFN-γ levels in the lung while concomitantly reducing the TGF-β levels. Interestingly, when bleomycin-treated BALF cells were treated in vitro with recombinant IFN-γ, their production of TGF-β dropped markedly. These findings suggest that IFN-γ-secreting iNKT cells help protect against pulmonary fibrosis by downregulating TGF-β1 expression in the fibrotic lung81. Our findings are supported by Grabarz et al., who observed that when WT mice were injected intratracheally with bleomycin and intraperitoneally with α-GalCer on the same day, pulmonary fibrosis was less severe. This was associated with lower IL-4 levels in the lung and lower expression of arginase-1 by neighboring alveolar macrophages. These findings suggest that iNKT cells may protect mice from pulmonary fibrosis by suppressing lung production of IL-4, which inhibits M2-macrophage polarization156. This is significant because the recruitment of monocytes to the lung and their conversion into type-2 cytokine- and TGF-β-secreting M2 macrophages drive the overall progression of pulmonary fibrosis157. Thus, iNKT cells protect mice from pulmonary fibrosis by (i) producing IFN-γ, thereby downregulating lung TGF-β levels and (ii) decreasing lung IL-4 levels, thereby inhibiting M2-macrophage activity (Fig. 3d).
Hypersensitivity pneumonitis
Hypersensitivity pneumonitis is caused by repetitive exposure to inhaled environmental antigens that provoke a hyperreactive immune response. This response induces inflammation of the alveoli and bronchioles and often leads to other interstitial lung diseases158. There is little in the literature about the roles of iNKT cells in hypersensitivity pneumonitis. However, we found that CD1d-KO mice were more susceptible to Saccharopolyspora rectivirgula-induced hypersensitivity pneumonitis than WT mice and that this was associated with elevated IFN-γ levels in the lung. IFN-γ was mainly produced by Gr-1+ neutrophils and played an important pathogenic role since blocking IFN-γ or depleting Gr-1+ neutrophils attenuated hypersensitivity pneumonitis-associated inflammation in CD1d-KO mice. Additional experiments then showed that the production of IFN-γ by Gr-1+ neutrophils in hypersensitivity pneumonitis was impaired by IL-4 produced by iNKT cells: adoptive transfer of IFN-γ-deficient, but not IL-4-deficient, iNKT cells downregulated hypersensitivity pneumonitis-related inflammation in CD1d-KO mice72.
Immune complex-induced lung injury
IgM or IgG immune complexes (ICs) are critical regulators of the immune system. However, they can cause acute respiratory distress syndrome (ARDS) or acute lung injury (ALI) due to unwanted inflammation159. We showed that CD1d-KO and Jα18-KO mice are less susceptible to developing ALI in the chicken egg albumin- and anti-chicken egg albumin IgG-induced IC-ALI model than WT mice. Additional experiments showed that the IC-ALI in WT mice was induced by iNKT cells, whose secretion of IFN-γ and macrophage inflammatory protein-1α (MIP-1α) caused neighboring alveolar macrophages and DCs to secrete proinflammatory cytokines. In particular, adoptive transfer of WT iNKT cells into CD1d-KO mice generated the IC-ALI seen in WT mice, but this was not observed when IFN-γ-deficient, MIP-1α-deficient, or FcγR-deficient iNKT cells were transferred82.
Altogether, these studies show that along with their crucial roles in common respiratory tract diseases, pulmonary iNKT cells are also important in many other respiratory tract diseases. These findings demonstrate the importance of these cells in governing overall lung immunity.
Concluding remarks
This review sought to provide a broad perspective on pulmonary iNKT cells and their roles in lung diseases that will hopefully aid further research on these cells. While it is clear that these cells are important for protection from lung infections and play important roles in the pathogenesis of many lung diseases, there are still many missing links. It is increasingly evident that overall immunity is driven by very complex and dynamic interactions between a wide variety of immune cells. Given the cytokine multipotency of iNKT cells and their multiple functions, it is likely that further research on the interrelationships between pulmonary iNKT cells and surrounding immune cells will be fruitful in terms of improving our understanding of the immune mechanisms that protect and harm the lungs.
Acknowledgements
This research was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (grant number: NRF-2020R1A2C2008312). All graphics were created with Biorender.com.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Dongjin Jeong, Yeon Duk Woo.
References
- 1.Godfrey DI, MacDonald HR, Kronenberg M, Smyth MJ, Van Kaer L. NKT cells: what’s in a name? Nat. Rev. Immunol. 2004;4:231–237. doi: 10.1038/nri1309. [DOI] [PubMed] [Google Scholar]
- 2.Burdin N, et al. Selective ability of mouse CD1 to present glycolipids: alpha-galactosylceramide specifically stimulates V alpha 14+ NK T lymphocytes. J. Immunol. 1998;161:3271–3281. doi: 10.4049/jimmunol.161.7.3271. [DOI] [PubMed] [Google Scholar]
- 3.Oh SJ, Kim JH, Min CK, Chung DH. Role of type II NKT cells in the suppression of graft-versus-host disease. Crit. Rev. Immunol. 2008;28:249–267. doi: 10.1615/CritRevImmunol.v28.i3.50. [DOI] [PubMed] [Google Scholar]
- 4.Houston S. iNKT cells circulate. Nat. Immunol. 2022;23:1653. doi: 10.1038/s41590-022-01382-0. [DOI] [PubMed] [Google Scholar]
- 5.Crosby CM, Kronenberg M. Tissue-specific functions of invariant natural killer T cells. Nat. Rev. Immunol. 2018;18:559–574. doi: 10.1038/s41577-018-0034-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee YJ, et al. Tissue-specific distribution of iNKT cells impacts their cytokine response. Immunity. 2015;43:566–578. doi: 10.1016/j.immuni.2015.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lynch L, et al. Adipose tissue invariant NKT cells protect against diet-induced obesity and metabolic disorder through regulatory cytokine production. Immunity. 2012;37:574–587. doi: 10.1016/j.immuni.2012.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang W, et al. The role of CD1d and MR1 restricted T cells in the liver. Front. Immunol. 2018;9:2424. doi: 10.3389/fimmu.2018.02424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lynch L. Adipose invariant natural killer T cells. Immunology. 2014;142:337–346. doi: 10.1111/imm.12269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Montoya CJ, et al. Characterization of human invariant natural killer T subsets in health and disease using a novel invariant natural killer T cell-clonotypic monoclonal antibody, 6B11. Immunology. 2007;122:1–14. doi: 10.1111/j.1365-2567.2007.02647.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ahn S, et al. GM-CSF and IL-4 produced by NKT cells inversely regulate IL-1beta production by macrophages. Immunol. Lett. 2017;182:50–56. doi: 10.1016/j.imlet.2017.01.003. [DOI] [PubMed] [Google Scholar]
- 12.Kim HY, et al. NKT cells promote antibody-induced joint inflammation by suppressing transforming growth factor beta1 production. J. Exp. Med. 2005;201:41–47. doi: 10.1084/jem.20041400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Woo YD, Koh J, Kang HR, Kim HY, Chung DH. The invariant natural killer T cell-mediated chemokine X-C motif chemokine ligand 1-X-C motif chemokine receptor 1 axis promotes allergic airway hyperresponsiveness by recruiting CD103(+) dendritic cells. J. Allergy Clin. Immunol. 2018;142:1781–1792.e1712. doi: 10.1016/j.jaci.2017.12.1005. [DOI] [PubMed] [Google Scholar]
- 14.Terabe M, Berzofsky JA. Tissue-specific roles of NKT cells in tumor immunity. Front. Immunol. 2018;9:1838. doi: 10.3389/fimmu.2018.01838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zingaropoli MA, et al. Major reduction of NKT cells in patients with severe COVID-19 pneumonia. Clin. Immunol. 2021;222:108630. doi: 10.1016/j.clim.2020.108630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dashtsoodol N, Watarai H, Sakata S, Taniguchi M. Identification of CD4(-)CD8(-) double-negative natural killer T cell precursors in the thymus. PLoS ONE. 2008;3:e3688. doi: 10.1371/journal.pone.0003688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bendelac A. Positive selection of mouse NK1+ T cells by CD1-expressing cortical thymocytes. J. Exp. Med. 1995;182:2091–2096. doi: 10.1084/jem.182.6.2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lazarevic V, et al. The gene encoding early growth response 2, a target of the transcription factor NFAT, is required for the development and maturation of natural killer T cells. Nat. Immunol. 2009;10:306–313. doi: 10.1038/ni.1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hogquist K, Georgiev H. Recent advances in iNKT cell development. F1000 Res. 2020;9:F1000. doi: 10.12688/f1000research.21378.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim EY, Lynch L, Brennan PJ, Cohen NR, Brenner MB. The transcriptional programs of iNKT cells. Semin. Immunol. 2015;27:26–32. doi: 10.1016/j.smim.2015.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wingender G, Sag D, Kronenberg M. NKT10 cells: a novel iNKT cell subset. Oncotarget. 2015;6:26552–26553. doi: 10.18632/oncotarget.5270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cohen NR, et al. Shared and distinct transcriptional programs underlie the hybrid nature of iNKT cells. Nat. Immunol. 2013;14:90–99. doi: 10.1038/ni.2490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Georgiev H, Ravens I, Benarafa C, Forster R, Bernhardt G. Distinct gene expression patterns correlate with developmental and functional traits of iNKT subsets. Nat. Commun. 2016;7:13116. doi: 10.1038/ncomms13116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee YJ, et al. Lineage-specific effector signatures of invariant NKT cells are shared amongst gammadelta T, innate lymphoid, and Th cells. J. Immunol. 2016;197:1460–1470. doi: 10.4049/jimmunol.1600643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee YJ, Holzapfel KL, Zhu J, Jameson SC, Hogquist KA. Steady-state production of IL-4 modulates immunity in mouse strains and is determined by lineage diversity of iNKT cells. Nat. Immunol. 2013;14:1146–1154. doi: 10.1038/ni.2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lynch L, et al. Regulatory iNKT cells lack expression of the transcription factor PLZF and control the homeostasis of T(reg) cells and macrophages in adipose tissue. Nat. Immunol. 2015;16:85–95. doi: 10.1038/ni.3047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sag D, Krause P, Hedrick CC, Kronenberg M, Wingender G. IL-10-producing NKT10 cells are a distinct regulatory invariant NKT cell subset. J. Clin. Invest. 2014;124:3725–3740. doi: 10.1172/JCI72308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baranek T, de Amat Herbozo C, Mallevaey T, Paget C. Deconstructing iNKT cell development at single-cell resolution. Trends Immunol. 2022;43:503–512. doi: 10.1016/j.it.2022.04.012. [DOI] [PubMed] [Google Scholar]
- 29.Engel I, et al. Innate-like functions of natural killer T cell subsets result from highly divergent gene programs. Nat. Immunol. 2016;17:728–739. doi: 10.1038/ni.3437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baranek T, et al. High dimensional single-cell analysis reveals iNKT cell developmental trajectories and effector fate decision. Cell Rep. 2020;32:108116. doi: 10.1016/j.celrep.2020.108116. [DOI] [PubMed] [Google Scholar]
- 31.Godfrey DI, Berzins SP. Control points in NKT-cell development. Nat. Rev. Immunol. 2007;7:505–518. doi: 10.1038/nri2116. [DOI] [PubMed] [Google Scholar]
- 32.Borowski C, Bendelac A. Signaling for NKT cell development: the SAP-FynT connection. J. Exp. Med. 2005;201:833–836. doi: 10.1084/jem.20050339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Northrup D, et al. Histone demethylases UTX and JMJD3 are required for NKT cell development in mice. Cell Biosci. 2017;7:25. doi: 10.1186/s13578-017-0152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Salio M, et al. Essential role for autophagy during invariant NKT cell development. Proc. Natl Acad. Sci. USA. 2014;111:E5678–E5687. doi: 10.1073/pnas.1413935112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Henao-Mejia J, et al. The microRNA miR-181 is a critical cellular metabolic rheostat essential for NKT cell ontogenesis and lymphocyte development and homeostasis. Immunity. 2013;38:984–997. doi: 10.1016/j.immuni.2013.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mao AP, et al. Multiple layers of transcriptional regulation by PLZF in NKT-cell development. Proc. Natl Acad. Sci. USA. 2016;113:7602–7607. doi: 10.1073/pnas.1601504113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moran AE, et al. T cell receptor signal strength in Treg and iNKT cell development demonstrated by a novel fluorescent reporter mouse. J. Exp. Med. 2011;208:1279–1289. doi: 10.1084/jem.20110308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Malhotra N, et al. SOX4 controls invariant NKT cell differentiation by tuning TCR signaling. J. Exp. Med. 2018;215:2887–2900. doi: 10.1084/jem.20172021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cui Y, et al. Mucosal-associated invariant T cell-rich congenic mouse strain allows functional evaluation. J. Clin. Invest. 2015;125:4171–4185. doi: 10.1172/JCI82424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thomas SY, et al. PLZF induces an intravascular surveillance program mediated by long-lived LFA-1-ICAM-1 interactions. J. Exp. Med. 2011;208:1179–1188. doi: 10.1084/jem.20102630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Johnston B, Kim CH, Soler D, Emoto M, Butcher EC. Differential chemokine responses and homing patterns of murine TCR alpha beta NKT cell subsets. J. Immunol. 2003;171:2960–2969. doi: 10.4049/jimmunol.171.6.2960. [DOI] [PubMed] [Google Scholar]
- 42.Scanlon ST, et al. Airborne lipid antigens mobilize resident intravascular NKT cells to induce allergic airway inflammation. J. Exp. Med. 2011;208:2113–2124. doi: 10.1084/jem.20110522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Murray MP, et al. Transcriptome and chromatin landscape of iNKT cells are shaped by subset differentiation and antigen exposure. Nat. Commun. 2021;12:1446. doi: 10.1038/s41467-021-21574-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Salou M, et al. A common transcriptomic program acquired in the thymus defines tissue residency of MAIT and NKT subsets. J. Exp. Med. 2019;216:133–151. doi: 10.1084/jem.20181483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hayward SL, et al. Environmental cues regulate epigenetic reprogramming of airway-resident memory CD8(+) T cells. Nat. Immunol. 2020;21:309–320. doi: 10.1038/s41590-019-0584-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lavin Y, et al. Tissue-resident macrophage enhancer landscapes are shaped by the local microenvironment. Cell. 2014;159:1312–1326. doi: 10.1016/j.cell.2014.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Meyer EH, et al. iNKT cells require CCR4 to localize to the airways and to induce airway hyperreactivity. J. Immunol. 2007;179:4661–4671. doi: 10.4049/jimmunol.179.7.4661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thomas SY, et al. CD1d-restricted NKT cells express a chemokine receptor profile indicative of Th1-type inflammatory homing cells. J. Immunol. 2003;171:2571–2580. doi: 10.4049/jimmunol.171.5.2571. [DOI] [PubMed] [Google Scholar]
- 49.Semmling V, et al. Alternative cross-priming through CCL17-CCR4-mediated attraction of CTLs toward NKT cell-licensed DCs. Nat. Immunol. 2010;11:313–320. doi: 10.1038/ni.1848. [DOI] [PubMed] [Google Scholar]
- 50.Gonzalo JA, et al. Mouse monocyte-derived chemokine is involved in airway hyperreactivity and lung inflammation. J. Immunol. 1999;163:403–411. doi: 10.4049/jimmunol.163.1.403. [DOI] [PubMed] [Google Scholar]
- 51.Kawasaki S, et al. Intervention of thymus and activation-regulated chemokine attenuates the development of allergic airway inflammation and hyperresponsiveness in mice. J. Immunol. 2001;166:2055–2062. doi: 10.4049/jimmunol.166.3.2055. [DOI] [PubMed] [Google Scholar]
- 52.Pilette C, Francis JN, Till SJ, Durham SR. CCR4 ligands are up-regulated in the airways of atopic asthmatics after segmental allergen challenge. Eur. Respir. J. 2004;23:876–884. doi: 10.1183/09031936.04.00102504. [DOI] [PubMed] [Google Scholar]
- 53.Sekiya T, et al. Increased levels of a TH2-type CC chemokine thymus and activation-regulated chemokine (TARC) in serum and induced sputum of asthmatics. Allergy. 2002;57:173–177. doi: 10.1034/j.1398-9995.2002.5720256.x. [DOI] [PubMed] [Google Scholar]
- 54.Meyer EH, et al. Glycolipid activation of invariant T cell receptor+ NK T cells is sufficient to induce airway hyperreactivity independent of conventional CD4+ T cells. Proc. Natl Acad. Sci. USA. 2006;103:2782–2787. doi: 10.1073/pnas.0510282103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sen Y, et al. V alpha 24-invariant NKT cells from patients with allergic asthma express CCR9 at high frequency and induce Th2 bias of CD3+ T cells upon CD226 engagement. J. Immunol. 2005;175:4914–4926. doi: 10.4049/jimmunol.175.8.4914. [DOI] [PubMed] [Google Scholar]
- 56.Umetsu DT, McIntire JJ, Akbari O, Macaubas C, DeKruyff RH. Asthma: an epidemic of dysregulated immunity. Nat. Immunol. 2002;3:715–720. doi: 10.1038/ni0802-715. [DOI] [PubMed] [Google Scholar]
- 57.Thanabalasuriar A, Neupane AS, Wang J, Krummel MF, Kubes P. iNKT cell emigration out of the lung vasculature requires neutrophils and monocyte-derived dendritic cells in inflammation. Cell Rep. 2016;16:3260–3272. doi: 10.1016/j.celrep.2016.07.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Brigl M, Bry L, Kent SC, Gumperz JE, Brenner MB. Mechanism of CD1d-restricted natural killer T cell activation during microbial infection. Nat. Immunol. 2003;4:1230–1237. doi: 10.1038/ni1002. [DOI] [PubMed] [Google Scholar]
- 59.Chun T, et al. CD1d-expressing dendritic cells but not thymic epithelial cells can mediate negative selection of NKT cells. J. Exp. Med. 2003;197:907–918. doi: 10.1084/jem.20021366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Venkataswamy MM, Porcelli SA. Lipid and glycolipid antigens of CD1d-restricted natural killer T cells. Semin. Immunol. 2010;22:68–78. doi: 10.1016/j.smim.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhang Y, et al. alpha-GalCer and iNKT cell-based cancer immunotherapy: realizing the therapeutic potentials. Front. Immunol. 2019;10:1126. doi: 10.3389/fimmu.2019.01126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.O’Keeffe J, Podbielska M, Hogan EL. Invariant natural killer T cells and their ligands: focus on multiple sclerosis. Immunology. 2015;145:468–475. doi: 10.1111/imm.12481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kinjo Y, et al. Invariant natural killer T cells recognize glycolipids from pathogenic Gram-positive bacteria. Nat. Immunol. 2011;12:966–974. doi: 10.1038/ni.2096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fischer K, et al. Mycobacterial phosphatidylinositol mannoside is a natural antigen for CD1d-restricted T cells. Proc. Natl Acad. Sci. USA. 2004;101:10685–10690. doi: 10.1073/pnas.0403787101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Reilly EC, Wands JR, Brossay L. Cytokine dependent and independent iNKT cell activation. Cytokine. 2010;51:227–231. doi: 10.1016/j.cyto.2010.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gottschalk C, Mettke E, Kurts C. The role of invariant natural killer T cells in dendritic cell licensing, cross-priming, and memory CD8(+) T cell generation. Front. Immunol. 2015;6:379. doi: 10.3389/fimmu.2015.00379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Brigl M, et al. Innate and cytokine-driven signals, rather than microbial antigens, dominate in natural killer T cell activation during microbial infection. J. Exp. Med. 2011;208:1163–1177. doi: 10.1084/jem.20102555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Paget C, et al. Activation of invariant NKT cells by toll-like receptor 9-stimulated dendritic cells requires type I interferon and charged glycosphingolipids. Immunity. 2007;27:597–609. doi: 10.1016/j.immuni.2007.08.017. [DOI] [PubMed] [Google Scholar]
- 69.Salio M, et al. Modulation of human natural killer T cell ligands on TLR-mediated antigen-presenting cell activation. Proc. Natl Acad. Sci. USA. 2007;104:20490–20495. doi: 10.1073/pnas.0710145104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Paget C, et al. Role of invariant NK T lymphocytes in immune responses to CpG oligodeoxynucleotides. J. Immunol. 2009;182:1846–1853. doi: 10.4049/jimmunol.0802492. [DOI] [PubMed] [Google Scholar]
- 71.Kim JH, Kim HS, Kim HY, Oh SJ, Chung DH. Direct engagement of TLR4 in invariant NKT cells regulates immune diseases by differential IL-4 and IFN-gamma production in mice. PLoS ONE. 2012;7:e45348. doi: 10.1371/journal.pone.0045348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hwang SJ, Kim S, Park WS, Chung DH. IL-4-secreting NKT cells prevent hypersensitivity pneumonitis by suppressing IFN-gamma-producing neutrophils. J. Immunol. 2006;177:5258–5268. doi: 10.4049/jimmunol.177.8.5258. [DOI] [PubMed] [Google Scholar]
- 73.Kim JH, Oh SJ, Ahn S, Chung DH. IFN-gamma-producing NKT cells exacerbate sepsis by enhancing C5a generation via IL-10-mediated inhibition of CD55 expression on neutrophils. Eur. J. Immunol. 2014;44:2025–2035. doi: 10.1002/eji.201343937. [DOI] [PubMed] [Google Scholar]
- 74.Opasawatchai A, Matangkasombut P. iNKT cells and their potential lipid ligands during viral infection. Front. Immunol. 2015;6:378. doi: 10.3389/fimmu.2015.00378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Victor JR, Lezmi G, Leite-de-Moraes M. New insights into asthma inflammation: focus on iNKT, MAIT, and gammadeltaT cells. Clin. Rev. Allergy Immunol. 2020;59:371–381. doi: 10.1007/s12016-020-08784-8. [DOI] [PubMed] [Google Scholar]
- 76.Wilson SB, Delovitch TL. Janus-like role of regulatory iNKT cells in autoimmune disease and tumour immunity. Nat. Rev. Immunol. 2003;3:211–222. doi: 10.1038/nri1028. [DOI] [PubMed] [Google Scholar]
- 77.Iwamura C, Nakayama T. Role of NKT cells in allergic asthma. Curr. Opin. Immunol. 2010;22:807–813. doi: 10.1016/j.coi.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 78.Chackerian A, Alt J, Perera V, Behar SM. Activation of NKT cells protects mice from tuberculosis. Infect. Immun. 2002;70:6302–6309. doi: 10.1128/IAI.70.11.6302-6309.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Dempsey LA. NKT cells aid antiviral responses. Nat. Immunol. 2018;19:99. doi: 10.1038/s41590-017-0039-1. [DOI] [PubMed] [Google Scholar]
- 80.Tsao CC, Tsao PN, Chen YG, Chuang YH. Repeated activation of lung invariant NKT cells results in chronic obstructive pulmonary disease-like symptoms. PLoS ONE. 2016;11:e0147710. doi: 10.1371/journal.pone.0147710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kim JH, et al. Natural killer T (NKT) cells attenuate bleomycin-induced pulmonary fibrosis by producing interferon-gamma. Am. J. Pathol. 2005;167:1231–1241. doi: 10.1016/S0002-9440(10)61211-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kim JH, Chung DH. CD1d-restricted IFN-gamma-secreting NKT cells promote immune complex-induced acute lung injury by regulating macrophage-inflammatory protein-1alpha production and activation of macrophages and dendritic cells. J. Immunol. 2011;186:1432–1441. doi: 10.4049/jimmunol.1003140. [DOI] [PubMed] [Google Scholar]
- 83.Akbari O, et al. Essential role of NKT cells producing IL-4 and IL-13 in the development of allergen-induced airway hyperreactivity. Nat. Med. 2003;9:582–588. doi: 10.1038/nm851. [DOI] [PubMed] [Google Scholar]
- 84.Wallace KL, et al. NKT cells mediate pulmonary inflammation and dysfunction in murine sickle cell disease through production of IFN-gamma and CXCR3 chemokines. Blood. 2009;114:667–676. doi: 10.1182/blood-2009-02-205492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nembrini C, Marsland BJ, Kopf M. IL-17-producing T cells in lung immunity and inflammation. J. Allergy Clin. Immunol. 2009;123:986–994. doi: 10.1016/j.jaci.2009.03.033. [DOI] [PubMed] [Google Scholar]
- 86.Paget C, et al. Interleukin-22 is produced by invariant natural killer T lymphocytes during influenza A virus infection: potential role in protection against lung epithelial damages. J. Biol. Chem. 2012;287:8816–8829. doi: 10.1074/jbc.M111.304758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Murray MP, et al. Stimulation of a subset of natural killer T cells by CD103(+) DC is required for GM-CSF and protection from pneumococcal infection. Cell Rep. 2022;38:110209. doi: 10.1016/j.celrep.2021.110209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kok WL, et al. Pivotal advance: invariant NKT cells reduce accumulation of inflammatory monocytes in the lungs and decrease immune-pathology during severe influenza A virus infection. J. Leukoc. Biol. 2012;91:357–368. doi: 10.1189/jlb.0411184. [DOI] [PubMed] [Google Scholar]
- 89.Konishi J, et al. The characteristics of human NKT cells in lung cancer–CD1d independent cytotoxicity against lung cancer cells by NKT cells and decreased human NKT cell response in lung cancer patients. Hum. Immunol. 2004;65:1377–1388. doi: 10.1016/j.humimm.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 90.Snyder-Cappione JE, et al. Individuals with pulmonary tuberculosis have lower levels of circulating CD1d-restricted NKT cells. J. Infect. Dis. 2007;195:1361–1364. doi: 10.1086/513567. [DOI] [PubMed] [Google Scholar]
- 91.Pichavant M, et al. Oxidative stress-mediated iNKT-cell activation is involved in COPD pathogenesis. Mucosal Immunol. 2014;7:568–578. doi: 10.1038/mi.2013.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.MacIver NJ, Michalek RD, Rathmell JC. Metabolic regulation of T lymphocytes. Annu. Rev. Immunol. 2013;31:259–283. doi: 10.1146/annurev-immunol-032712-095956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.van der Windt GJ, Pearce EL. Metabolic switching and fuel choice during T-cell differentiation and memory development. Immunol. Rev. 2012;249:27–42. doi: 10.1111/j.1600-065X.2012.01150.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Rangel Rivera GO, et al. Fundamentals of T cell metabolism and strategies to enhance cancer immunotherapy. Front. Immunol. 2021;12:645242. doi: 10.3389/fimmu.2021.645242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Yarosz EL, Chang CH, Kumar A. Metabolism in invariant natural killer T cells: an overview. Immunometabolism. 2021;3:e210010. doi: 10.20900/immunometab20210010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kumar A, et al. Enhanced oxidative phosphorylation in NKT cells is essential for their survival and function. Proc. Natl Acad. Sci. USA. 2019;116:7439–7448. doi: 10.1073/pnas.1901376116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Pyaram K, et al. Keap1-Nrf2 system plays an important role in invariant natural killer T cell development and homeostasis. Cell Rep. 2019;27:699–707.e694. doi: 10.1016/j.celrep.2019.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Weng X, et al. Mitochondrial metabolism is essential for invariant natural killer T cell development and function. Proc. Natl Acad. Sci. USA. 2021;118:e2021385118. doi: 10.1073/pnas.2021385118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Larkin J, et al. CD44 differentially activates mouse NK T cells and conventional T cells. J. Immunol. 2006;177:268–279. doi: 10.4049/jimmunol.177.1.268. [DOI] [PubMed] [Google Scholar]
- 100.Brossay L, et al. CD1d-mediated recognition of an alpha-galactosylceramide by natural killer T cells is highly conserved through mammalian evolution. J. Exp. Med. 1998;188:1521–1528. doi: 10.1084/jem.188.8.1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Meldrum OW, Chotirmall SH. Mucus, microbiomes and pulmonary disease. Biomedicines. 2021;9:675. doi: 10.3390/biomedicines9060675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Huffnagle GB, Dickson RP, Lukacs NW. The respiratory tract microbiome and lung inflammation: a two-way street. Mucosal Immunol. 2017;10:299–306. doi: 10.1038/mi.2016.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Fu S, et al. Impaired lipid biosynthesis hinders anti-tumor efficacy of intratumoral iNKT cells. Nat. Commun. 2020;11:438. doi: 10.1038/s41467-020-14332-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Diseases GBD, Injuries C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Paget C, Trottein F. Role of type 1 natural killer T cells in pulmonary immunity. Mucosal Immunol. 2013;6:1054–1067. doi: 10.1038/mi.2013.59. [DOI] [PubMed] [Google Scholar]
- 106.Olin JT, Wechsler ME. Asthma: pathogenesis and novel drugs for treatment. BMJ. 2014;349:g5517. doi: 10.1136/bmj.g5517. [DOI] [PubMed] [Google Scholar]
- 107.Romanet-Manent S, et al. Allergic vs nonallergic asthma: what makes the difference? Allergy. 2002;57:607–613. doi: 10.1034/j.1398-9995.2002.23504.x. [DOI] [PubMed] [Google Scholar]
- 108.Schatz M, Rosenwasser L. The allergic asthma phenotype. J. Allergy Clin. Immunol. Pr. 2014;2:645–648. doi: 10.1016/j.jaip.2014.09.004. [DOI] [PubMed] [Google Scholar]
- 109.Cosmi L, Liotta F, Maggi E, Romagnani S, Annunziato F. Th17 cells: new players in asthma pathogenesis. Allergy. 2011;66:989–998. doi: 10.1111/j.1398-9995.2011.02576.x. [DOI] [PubMed] [Google Scholar]
- 110.Umetsu DT, Dekruyff RH. Natural killer T cells are important in the pathogenesis of asthma: the many pathways to asthma. J. Allergy Clin. Immunol. 2010;125:975–979. doi: 10.1016/j.jaci.2010.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Hachem P, et al. Alpha-galactosylceramide-induced iNKT cells suppress experimental allergic asthma in sensitized mice: role of IFN-gamma. Eur. J. Immunol. 2005;35:2793–2802. doi: 10.1002/eji.200535268. [DOI] [PubMed] [Google Scholar]
- 112.Lisbonne M, et al. Cutting edge: invariant V alpha 14 NKT cells are required for allergen-induced airway inflammation and hyperreactivity in an experimental asthma model. J. Immunol. 2003;171:1637–1641. doi: 10.4049/jimmunol.171.4.1637. [DOI] [PubMed] [Google Scholar]
- 113.Matangkasombut P, et al. Direct activation of natural killer T cells induces airway hyperreactivity in nonhuman primates. J. Allergy Clin. Immunol. 2008;121:1287–1289. doi: 10.1016/j.jaci.2008.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kim JO, et al. Asthma is induced by intranasal coadministration of allergen and natural killer T-cell ligand in a mouse model. J. Allergy Clin. Immunol. 2004;114:1332–1338. doi: 10.1016/j.jaci.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 115.Gour N, Wills-Karp M. IL-4 and IL-13 signaling in allergic airway disease. Cytokine. 2015;75:68–78. doi: 10.1016/j.cyto.2015.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Hiraishi Y, et al. IL-33, IL-25 and TSLP contribute to development of fungal-associated protease-induced innate-type airway inflammation. Sci. Rep. 2018;8:18052. doi: 10.1038/s41598-018-36440-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Rachitskaya AV, et al. Cutting edge: NKT cells constitutively express IL-23 receptor and RORgammat and rapidly produce IL-17 upon receptor ligation in an IL-6-independent fashion. J. Immunol. 2008;180:5167–5171. doi: 10.4049/jimmunol.180.8.5167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Goto M, et al. Murine NKT cells produce Th17 cytokine interleukin-22. Cell Immunol. 2009;254:81–84. doi: 10.1016/j.cellimm.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 119.Michel ML, et al. Identification of an IL-17-producing NK1.1(neg) iNKT cell population involved in airway neutrophilia. J. Exp. Med. 2007;204:995–1001. doi: 10.1084/jem.20061551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Terashima A, et al. A novel subset of mouse NKT cells bearing the IL-17 receptor B responds to IL-25 and contributes to airway hyperreactivity. J. Exp. Med. 2008;205:2727–2733. doi: 10.1084/jem.20080698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Theisen D, Murphy K. The role of cDC1s in vivo: CD8 T cell priming through cross-presentation. F1000Res. 2017;6:98. doi: 10.12688/f1000research.9997.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Nakano H, et al. Pulmonary CD103(+) dendritic cells prime Th2 responses to inhaled allergens. Mucosal Immunol. 2012;5:53–65. doi: 10.1038/mi.2011.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Thomas SY, Chyung YH, Luster AD. Natural killer T cells are not the predominant T cell in asthma and likely modulate, not cause, asthma. J. Allergy Clin. Immunol. 2010;125:980–984. doi: 10.1016/j.jaci.2010.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Das J, et al. Natural killer T cells and CD8+ T cells are dispensable for T cell-dependent allergic airway inflammation. Nat. Med. 2006;12:1345–1346. doi: 10.1038/nm1206-1345. [DOI] [PubMed] [Google Scholar]
- 125.Hyde EJ, Wakelin KA, Daniels NJ, Ghosh S, Ronchese F. Similar immune mechanisms control experimental airway eosinophilia elicited by different allergens and treatment protocols. BMC Immunol. 2019;20:18. doi: 10.1186/s12865-019-0295-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Constantinides MG. Interactions between the microbiota and innate and innate-like lymphocytes. J. Leukoc. Biol. 2018;103:409–419. doi: 10.1002/JLB.3RI0917-378R. [DOI] [PubMed] [Google Scholar]
- 127.Pham-Thi N, et al. Enhanced frequency of immunoregulatory invariant natural killer T cells in the airways of children with asthma. J. Allergy Clin. Immunol. 2006;117:217–218. doi: 10.1016/j.jaci.2005.09.052. [DOI] [PubMed] [Google Scholar]
- 128.Fernandes GFS, Thompson AM, Castagnolo D, Denny WA, Dos Santos JL. Tuberculosis drug discovery: challenges and new horizons. J. Med. Chem. 2022;65:7489–7531. doi: 10.1021/acs.jmedchem.2c00227. [DOI] [PubMed] [Google Scholar]
- 129.Koch A, Mizrahi V. Mycobacterium tuberculosis . Trends Microbiol. 2018;26:555–556. doi: 10.1016/j.tim.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 130.Al-Humadi HW, Al-Saigh RJ, Al-Humadi AW. Addressing the challenges of tuberculosis: a brief historical account. Front. Pharm. 2017;8:689. doi: 10.3389/fphar.2017.00689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Arora P, Foster EL, Porcelli SA. CD1d and natural killer T cells in immunity to Mycobacterium tuberculosis. Adv. Exp. Med. Biol. 2013;783:199–223. doi: 10.1007/978-1-4614-6111-1_11. [DOI] [PubMed] [Google Scholar]
- 132.Sada-Ovalle I, Chiba A, Gonzales A, Brenner MB, Behar SM. Innate invariant NKT cells recognize Mycobacterium tuberculosis-infected macrophages, produce interferon-gamma, and kill intracellular bacteria. PLoS Pathog. 2008;4:e1000239. doi: 10.1371/journal.ppat.1000239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Rothchild AC, Jayaraman P, Nunes-Alves C, Behar SM. iNKT cell production of GM-CSF controls Mycobacterium tuberculosis. PLoS Pathog. 2014;10:e1003805. doi: 10.1371/journal.ppat.1003805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Zenteno-Cuevas R. Update on the development of TB Vaccines. Curr. Pharm. Biotechnol. 2013;14:940–946. doi: 10.2174/1389201014666131226124940. [DOI] [PubMed] [Google Scholar]
- 135.Montoya CJ, et al. Invariant NKT cells from HIV-1 or Mycobacterium tuberculosis-infected patients express an activated phenotype. Clin. Immunol. 2008;127:1–6. doi: 10.1016/j.clim.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 136.Singh A, Dey AB, Mohan A, Mitra DK. Programmed death-1 receptor suppresses gamma-IFN producing NKT cells in human tuberculosis. Tuberculosis. 2014;94:197–206. doi: 10.1016/j.tube.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 137.Sutherland JS, et al. High granulocyte/lymphocyte ratio and paucity of NKT cells defines TB disease in a TB-endemic setting. Tuberculosis. 2009;89:398–404. doi: 10.1016/j.tube.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 138.Gansert JL, et al. Human NKT cells express granulysin and exhibit antimycobacterial activity. J. Immunol. 2003;170:3154–3161. doi: 10.4049/jimmunol.170.6.3154. [DOI] [PubMed] [Google Scholar]
- 139.Zhao J, et al. Mycolic acid-specific T cells protect against Mycobacterium tuberculosis infection in a humanized transgenic mouse model. Elife. 2015;4:e08525. doi: 10.7554/eLife.08525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Huang S. Targeting innate-like T cells in tuberculosis. Front. Immunol. 2016;7:594. doi: 10.3389/fimmu.2016.00594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Hutchinson EC. Influenza virus. Trends Microbiol. 2018;26:809–810. doi: 10.1016/j.tim.2018.05.013. [DOI] [PubMed] [Google Scholar]
- 142.Paget C, et al. Potential role of invariant NKT cells in the control of pulmonary inflammation and CD8+ T cell response during acute influenza A virus H3N2 pneumonia. J. Immunol. 2011;186:5590–5602. doi: 10.4049/jimmunol.1002348. [DOI] [PubMed] [Google Scholar]
- 143.De Santo C, et al. Invariant NKT cells reduce the immunosuppressive activity of influenza A virus-induced myeloid-derived suppressor cells in mice and humans. J. Clin. Invest. 2008;118:4036–4048. doi: 10.1172/JCI36264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Driver JP, de Carvalho Madrid DM, Gu W, Artiaga BL, Richt JA. Modulation of immune responses to influenza A virus vaccines by natural killer T cells. Front. Immunol. 2020;11:2172. doi: 10.3389/fimmu.2020.02172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Bjorkstrom NK, Ponzetta A. Natural killer cells and unconventional T cells in COVID-19. Curr. Opin. Virol. 2021;49:176–182. doi: 10.1016/j.coviro.2021.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Liu J, et al. Analysis of the long-term impact on cellular immunity in COVID-19-recovered individuals reveals a profound NKT cell impairment. mBio. 2021;12:e00085–21. doi: 10.1128/mBio.00085-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Kim DM, et al. Eosinophil-mediated lung inflammation associated with elevated natural killer T cell response in COVID-19 patients. Korean J. Intern. Med. 2022;37:201–209. doi: 10.3904/kjim.2021.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Li YR, et al. Development of off-the-shelf hematopoietic stem cell-engineered invariant natural killer T cells for COVID-19 therapeutic intervention. Stem Cell Res. Ther. 2022;13:112. doi: 10.1186/s13287-022-02787-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Mannino DM, et al. Economic burden of COPD in the presence of comorbidities. Chest. 2015;148:138–150. doi: 10.1378/chest.14-2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Mirza S, Clay RD, Koslow MA, Scanlon PD. COPD guidelines: a review of the 2018 GOLD report. Mayo Clin. Proc. 2018;93:1488–1502. doi: 10.1016/j.mayocp.2018.05.026. [DOI] [PubMed] [Google Scholar]
- 151.Tang Y, et al. Increased numbers of NK cells, NKT-like cells, and NK inhibitory receptors in peripheral blood of patients with chronic obstructive pulmonary disease. Clin. Dev. Immunol. 2013;2013:721782. doi: 10.1155/2013/721782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Kim EY, et al. Persistent activation of an innate immune response translates respiratory viral infection into chronic lung disease. Nat. Med. 2008;14:633–640. doi: 10.1038/nm1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Noble PW, Barkauskas CE, Jiang D. Pulmonary fibrosis: patterns and perpetrators. J. Clin. Invest. 2012;122:2756–2762. doi: 10.1172/JCI60323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kendall RT, Feghali-Bostwick CA. Fibroblasts in fibrosis: novel roles and mediators. Front. Pharm. 2014;5:123. doi: 10.3389/fphar.2014.00123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Yue, X., Shan, B. & Lasky, J. A. TGF-beta: titan of lung fibrogenesis. Curr. Enzym. Inhib.6, 10.2174/10067 (2010). [DOI] [PMC free article] [PubMed]
- 156.Grabarz F, et al. Protective role of NKT cells and macrophage M2-driven phenotype in bleomycin-induced pulmonary fibrosis. Inflammopharmacology. 2018;26:491–504. doi: 10.1007/s10787-017-0383-7. [DOI] [PubMed] [Google Scholar]
- 157.Ogawa T, Shichino S, Ueha S, Matsushima K. Macrophages in lung fibrosis. Int. Immunol. 2021;33:665–671. doi: 10.1093/intimm/dxab040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Costabel U, et al. Hypersensitivity pneumonitis. Nat. Rev. Dis. Prim. 2020;6:65. doi: 10.1038/s41572-020-0191-z. [DOI] [PubMed] [Google Scholar]
- 159.Ward PA, Fattahi F, Bosmann M. New insights into molecular mechanisms of immune complex-induced injury in lung. Front. Immunol. 2016;7:86. doi: 10.3389/fimmu.2016.00086. [DOI] [PMC free article] [PubMed] [Google Scholar]