Abstract
Transgender and nonbinary people with female birth sex may utilize testosterone therapy for masculinization. Individuals interested in reproduction using their own gametes should be offered fertility preservation prior to starting testosterone. However, logistical and practical barriers prevent many from accessing fertility preservation options prior to starting testosterone. Some of these transmasculine and nonbinary individuals may later become interested in carrying a pregnancy or using their oocytes for reproduction after being on testosterone. Many questions remain about the reproductive impact of long-term masculinizing testosterone therapy. Emerging literature has documented pregnancies and successful assisted reproduction for some people after taking testosterone, but it is not known whether individuals can expect these successful outcomes. Testosterone appears to impact the reproductive tract, including the ovaries, uterus, and fallopian tubes, but the reversibility and functional impact of these changes also remain unclear. A greater understanding of the impact of masculinizing testosterone on reproductive capacity remains a priority area for future research.
Keywords: gender-affirming hormones, transgender, transmasculine, nonbinary, testosterone, fertility, reproduction
Graphical abstract
Graphical Abstract.
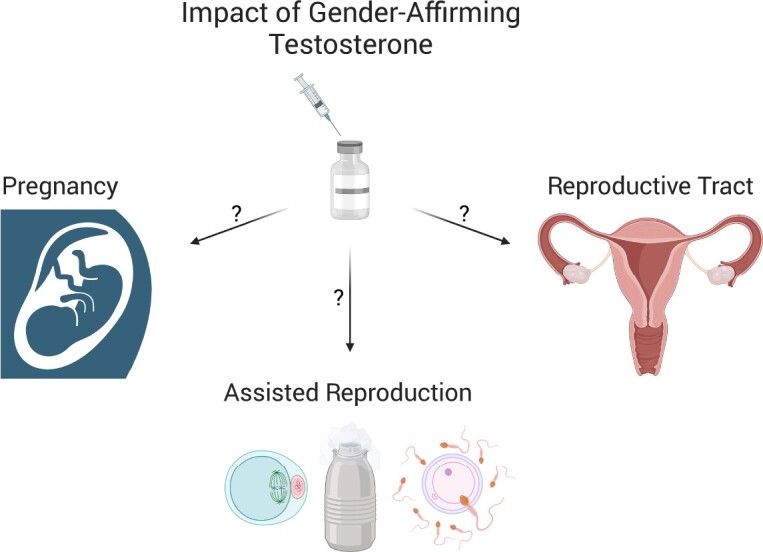
Pregnancies and successful assisted reproduction have been documented after gender-affirming testosterone, but much uncertainty remains regarding expectations for successful outcomes and the functional impact and reversibility of testosterone on the reproductive tract. (Created with BioRender.)
Introduction
Gender-affirming testosterone therapy is typically used by transgender and nonbinary individuals seeking masculinization. Testosterone can be administered as an injection intramuscularly or subcutaneously or as a transdermal gel or patch. Clinicians generally follow testosterone levels to ensure that testosterone is in the range for cisgender (non-transgender) men, although some transmasculine and nonbinary individuals have chosen to be on a lower dose of testosterone (Coleman et al., 2022). Individuals on testosterone typically notice deepening of the voice, clitoral enlargement, menstrual suppression, changes in muscle and body fat distribution, and growth of body and facial hair (Coleman et al., 2022). Masculinization with testosterone does not allow for individuals to only select certain desired characteristics while avoiding others that occur on a similar timeframe. Testosterone may be continued indefinitely depending on individual goals and needs.
The impact of testosterone on reproductive potential has not been fully elucidated. Counseling about fertility preservation options before starting testosterone is currently recommended by national and international medical organizations (Ethics Committee of the American Society for Reproductive Medicine, 2015; Hembree et al., 2017; Coleman et al., 2022), as there remain insufficient data to guarantee reproductive potential after testosterone therapy. Unfortunately, the fertility preservation options of oocyte or embryo cryopreservation are time-consuming, invasive, and costly. These hurdles are sometimes prohibitive and many do not choose fertility preservation before beginning testosterone, but later may have interest in carrying a pregnancy or using their oocytes for reproduction (Auer et al., 2018; Baram et al., 2019). There has been a recent expansion in research focused on reproductive capacity following testosterone therapy, with data suggesting that at least some individuals retain reproductive potential after T therapy (Light et al., 2014, 2018; Adeleye et al., 2019; Leung et al., 2019; Yaish et al., 2021). Of note, a nuanced discussion of family-building options in the context of sterilizing gender-affirming surgeries is beyond the scope of this review. Additional research is needed to assist with clinical guidance and reproductive decision-making for individuals on long-term masculinizing testosterone.
In this review, we discuss recent developments in research around pregnancy and assisted reproduction after masculinizing testosterone therapy. We contextualize these findings with data regarding the impact of testosterone on the reproductive tract, including the ovaries, uterus, and fallopian tubes and incorporate findings from transgender and nonbinary individuals as well as relevant animal models. We conclude by highlighting important remaining questions.
Pregnancies after testosterone
Multiple reports in the literature point to the possibility of pregnancy after testosterone therapy. These are typically smaller studies or case reports where an individual served as a gestational parent using their own oocytes or served as an oocyte donor after a period of being on testosterone therapy (Table 1). These reports do not typically include individuals who were attempting to conceive and may not have been successful. Even in reports that describe pregnancies after testosterone, there is often little reported about births or outcomes for offspring. Notably, testosterone is considered by the United States Food and Drug Administration as contraindicated during pregnancy due to concerns about teratogenicity based on animal studies of in utero testosterone exposure (United States Food and Drug Administration, 2022). Although masculinizing testosterone is not considered sufficient contraception, it often suppresses ovulation (Taub et al., 2020) and so pausing testosterone would be recommended for those attempting to conceive. While this emerging literature suggests that we cannot assume that prior testosterone leads to infertility, larger studies on conception rates, pregnancy, birth, and offspring outcomes are critically needed to determine the impact of prior testosterone therapy on reproductive potential.
Table 1.
Reports in the literature of pregnancies after testosterone (T) therapy.
| Author, year | # Pregnancies after T (self-carried) | # Pregnancies after T (partner/surrogate carried) | # Live births reported after T (self or partner/surrogate carried) | Relevant details |
|---|---|---|---|---|
| Light et al., 2014 | 25 | – | 25 | Cross-sectional survey of transgender men who were pregnant and delivered. Prior T use in 25 individuals, of whom 21/25 used their own oocyte to conceive. No statistical difference seen for pregnancy, delivery, or birth outcomes based on prior T use. |
| Ellis et al., 2015 | 6 | – | 6 | Qualitative study of conception, pregnancy, and birth. Screened for pregnancies not resulting in loss. Prior T in six of eight male-identified or gender-variant gestational parents. |
| Broughton and Omurtag, 2017 | – | 1 | – | Case reports, including one transgender man with IVF and ongoing pregnancy (partner-carried) after prior T. |
| Light et al., 2018 | 11 | – | 6 | Survey study with a focus on family planning and contraception. Of the 11 pregnancies reported with prior T, 5 ended in abortion. |
| Adeleye et al., 2019 | 1 | 2 | 1 | Chart review of ovarian stimulation in transgender men, including seven with prior T. Of three pregnancies after prior T, one spontaneous abortion in transgender man, one pregnancy with uncomplicated delivery (partner-carried), and one ongoing pregnancy (partner-carried). |
| Hahn et al., 2019 | 1 | – | 1 | Case report about providing perinatal care to one transgender man who had a few months of prior T before conception. |
| Leung et al., 2019 | 3 | 7 | 7 | A retrospective cohort study of transmasculine assisted reproductive outcomes. Includes embryo transfers leading to pregnancy and birth for seven transmasculine individuals (six with prior T, all included in this table as individual without T not identified). Two transmasculine individuals self-carried (one carried two pregnancies with one ongoing). Partner carried seven pregnancies for five transmasculine individuals (includes one pregnancy loss and one ongoing pregnancy). |
| Stroumsa et al., 2019 | 1 | – | – | A case report of a transgender man with prior T use who came to the emergency department lacking awareness of his pregnancy. He was not urgently triaged, but then found to be in labor with cord prolapse and ultimately delivered a stillborn baby. |
| Amir et al., 2020 | – | 1 | – | Retrospective cohort study of ovarian stimulation outcomes including six transgender men with prior T. One pregnancy using oocytes from a transgender man with 11 years of prior T carried by surrogate (ongoing). |
| de Sousa Resende et al., 2020 | – | 1 | – | A case report of one transgender man with 2 years of prior T and IVF leading to an ongoing pregnancy (partner-carrying). |
| Falck et al., 2020 | 8 | – | 8 | Qualitative study of 12 transmasculine individuals who had given birth, including eight with prior T. |
| Fischer, 2021 | 2 | – | 2 | Qualitative interviews about non-binary reproduction, including one transmasculine/non-binary person on T for about 6 months prior who had two children while off T. |
| Greenwald et al., 2021 | – | 1 | 1 | A case report of IVF from a transgender man with a 10-year history of T use who remained on T during ovarian stimulation. Pregnancy carried by partner. |
| Moseson et al., 2021 | 15 | – | – | Transgender, nonbinary, and gender-expansive people surveyed regarding pregnancy intentions and outcomes. Prior T in 12 individuals who reported 15 self-carried pregnancies. Of these 15 pregnancies, 4 occurred while on T with outcomes of 2 miscarriages, 1 abortion, and 1 unknown. Birth outcomes for other pregnancies with prior T not specifically reported. |
| Yaish et al., 2021 | 6 | 1 | 7 | Study including both a prospective pilot and a cross-sectional study looking at functional ovarian reserve with T. Includes reports of seven children born after prior T, including one carried by a surrogate and six carried by three transgender men (one carried four pregnancies). |
| Yoshida et al., 2022 | 1 | – | 1 | Case report, one transgender man with prior T, unplanned conception due to delay in accessing T, resumed T until aware of pregnancy, was too late for abortion and gave birth. |
| Israeli et al., 2022 | – | 4 | 3 | Retrospective comparison of in vitro fertilization outcomes including seven transgender men with prior T, four pregnancies carried by surrogates, two births (singleton and twins), and two ongoing pregnancies. |
| Moravek et al., 2023 | – | 1 | 1 | Two case reports, includes one transmasculine person who remained on T during ovarian stimulation and partner-carried pregnancy resulted in uncomplicated live birth. |
Assisted reproductive outcomes after testosterone
Multiple recent studies have reported on outcomes with assisted reproductive technology (ART) for individuals who have utilized testosterone. For fertility preservation, ART typically involves ovarian stimulation with oocyte collection. Oocytes are either cryopreserved as oocytes or fertilized and then cryopreserved as embryos. Family-building ART often involves ovarian stimulation with oocyte collection, fertilization, and blastocyst transfer to oneself or to someone else. For transgender and nonbinary people interested in carrying a pregnancy themselves, simpler assisted reproductive options can also include intrauterine insemination or medications to promote ovulation.
Although there has been limited study of any of these ART options, three recent studies (Table 2) have compared transgender men with prior testosterone to cisgender women or to transgender men without prior testosterone and found similar oocyte retrieval and oocyte maturity outcomes (Adeleye et al., 2019; Leung et al., 2019; Amir et al., 2020). Although their fertilization data was not comparative, these three studies also demonstrated examples of successful fertilization and pregnancy (Adeleye et al., 2019; Leung et al., 2019; Amir et al., 2020), as well as live birth for two of the studies (Adeleye et al., 2019; Leung et al., 2019). A recent retrospective study reported comparative fertilization data and found no detectable differences between the fertilization rates from transgender men with prior testosterone and cisgender controls groups (social fertility preservation or infertility), with comparable numbers of cryopreserved embryos as well as mean morphokinetic and morphological scores (Israeli et al., 2022). Several case reports have also demonstrated successful retrieval of mature oocytes after pausing testosterone (Broughton and Omurtag, 2017; de Sousa Resende et al., 2020; Insogna et al., 2020), with two cases of successful fertilization and ongoing pregnancies (Broughton and Omurtag, 2017; de Sousa Resende et al., 2020). Another study demonstrated successful cryopreservation of mature oocytes in two young adults with prior testosterone use (paused for 2–3 months), with the added complication of mild to moderate ovarian hyperstimulation syndrome in both of these individuals (Barrett et al., 2022). A recent retrospective cohort study did not find an association using linear regression between timing of testosterone cessation and number of total or mature oocytes for 18 individuals undergoing fertility preservation with prior testosterone treatment, although they noted that sample size may have limited their detection power (mean time on testosterone 44 months with SD 29.6 months, median time off testosterone 7.7 weeks with interquartile range 4.3–20.7 weeks) (Albar et al., 2023). Notably, these studies are relatively small and involve individuals pausing testosterone for varied durations.
Table 2.
Comparative case series for assisted reproductive outcomes with prior testosterone (T) exposure.
| Author, year | # patients with previous T | Duration on T | Duration off T | Comparison groups | Differences in transgender men with prior T | Fertilization, pregnancy, birth with prior T |
|---|---|---|---|---|---|---|
| Adeleye et al., 2019 | 7 | Median 46 months | 1–13 months (median 6 months) | Transgender men without prior T and cisgender controls. | Peak estradiol and total oocytes retrieved lower. Oocyte maturity rate comparable. | One live birth and one ongoing pregnancy carried by partners, spontaneous abortion transgender man. |
| Leung et al., 2019 | 16 | 3 months to 17 years (mean 44 months) | 1–12 months (mean 4 months) | Matched cisgender controls. | Required higher gonadotropin doses. No detectable differences in number of oocytes retrieved, mature oocyte percentage, or peak estradiol. | Fresh and frozen transfers in seven couples (two self-carried, five partner-carried) with live birth reported for all seven (some required multiple transfers). |
| Amir et al., 2020 | 6 | 14–144 months (mean 77 months) | 5–21 months (mean 9.3 months) | Transgender men without prior T and fertile cisgender controls. | No detectable differences in number of oocytes retrieved, oocyte maturity rates, or peak estradiol. | One ongoing surrogate-carried pregnancy. Five individuals preserved embryos and all had good quality embryos. |
| Israeli et al., 2022 | 7 | 14–156 months (mean 99.7 months) | 4–10 months (mean 6.5 months) | Cisgender women who completed in vitro fertilization for social fertility preservation (n = 10) or for infertility (n = 24, 4/24 mechanical factor infertility, 20/24 unexplained infertility) | No detectable differences in mean FSH stimulation days or peak estradiol. Amount of FSH used and oocytes retrieved higher for transgender men when compared to cisgender controls undergoing IVF for infertility but comparable for social fertility preservation. | No detectable differences in fertilization rate or mean morphokinetic and morphological scores between transgender men and both groups of cisgender controls. No detectable differences in number of cryopreserved embryos or distribution of embryo age at cryopreservation between transgender men and social fertility preservation cisgender controls. Four pregnancies carried by surrogates, two births (singleton and twins) and two ongoing pregnancies. |
Stopping testosterone for ovarian stimulation may be a hurdle to using assisted reproduction. Two recent case reports have demonstrated successful oocyte retrieval, fertilization, embryo transfer to a partner, and live birth without stopping testosterone, as well as the creation of euploid embryos (Greenwald et al., 2021; Moravek et al., 2023). Additional case reports have described successful cryopreservation of oocytes while on testosterone (Gale et al., 2021; Stark and Mok-Lin, 2022) or after 1 week off testosterone (Cho et al., 2020). Individuals could also potentially cryopreserve ovarian tissue from a gender-affirming oophorectomy without needing to undergo ovarian stimulation.
The experimental technique of ovarian tissue oocyte in vitro maturation has also been proposed as a possible method for fertility preservation that might not require ovarian stimulation or pausing testosterone. Oocytes collected during gender-affirming oophorectomies have been matured in vitro and have developed normal metaphase II spindles (De Roo et al., 2017) with intact spindle morphology after vitrification and thawing (Lierman et al., 2017). However, a recent study from this same group looked at the fertilization of in vitro matured oocytes collected from ovarian tissue for 83 individuals on testosterone and reported a low developmental capacity with high aberrant cleavage patterns and early embryo arrest (Lierman et al., 2021). They recommend further optimization before recommending ovarian tissue oocyte in vitro maturation as a method for transmasculine fertility preservation (Lierman et al., 2021). Another recent study (including some of the same authors) of oocytes matured in vitro from testosterone-treated transgender men also demonstrated low fertilization rates and very low rates of Day-5 blastocysts. Notably, spindle transfer from the oocytes of transgender men to enucleated mature control oocytes improved Day-5 blastocyst rates, suggesting that the poor embryo development in the testosterone-exposed oocytes matured in vitro may relate to poor oocyte cytoplasmic quality (which was also indicated by poor calcium release) (Christodoulaki et al., 2023). Additional strategies to support individuals undergoing ART may include transabdominal rather than transvaginal ultrasounds whenever possible and aromatase inhibitors to reduce estradiol elevation during gonadotropin stimulation (Moravek et al., 2020).
Ultimately, further comparative studies are needed to address varied options for assisted reproduction in individuals with prior testosterone use. For approaches focused on ovarian stimulation with oocyte collection, the need to stop testosterone should be further assessed.
Reproductive tract after testosterone
A systematic scoping review of studies reporting histological findings after masculinizing hormone therapy and including the reproductive tract was recently published in 2022 (Andrews et al., 2022). As such, we will focus here on key relevant findings, particularly for the ovaries, uterus, and fallopian tubes, as well as data from relevant animal models.
Ovarian impact of testosterone
Characteristics seen in ovaries with testosterone exposure are often similar to characteristics observed in ovaries from patients with polycystic ovary syndrome (PCOS). Notably, PCOS is multifactorial, and morphological ovarian similarities should not imply broader association between exogenous testosterone therapy and the complex syndrome that is PCOS. Commonly noted characteristics in ovaries with testosterone therapy include thickened tunica albuginea or increased collagenization of the outer cortex (Amirikia et al., 1986; Futterweit and Deligdisch, 1986; Spinder et al., 1989; Pache et al., 1991; Chadha et al., 1994; Ikeda et al., 2013) and changes to the ovarian stroma including stromal luteinization or stromal hyperplasia (Futterweit and Deligdisch, 1986; Spinder et al., 1989; Pache et al., 1991; Chadha et al., 1994; Grynberg et al., 2010; Ikeda et al., 2013; Borrás et al., 2021), which are also commonly seen with PCOS (Hughesdon, 1982). Varied terminology has been used to describe the follicular phenotype with testosterone therapy, but studies have reported increased or multiple cystic follicles (Futterweit and Deligdisch, 1986; Miller et al., 1986; Spinder et al., 1989; Pache et al., 1991; Chadha et al., 1994; Khalifa et al., 2019; Lin et al., 2022), multifollicular ovaries (Loverro et al., 2016), antral follicle counts of more than 12 follicles per ovary (Grynberg et al., 2010), or increased numbers of atretic follicles with similar overall follicle counts (Ikeda et al., 2013). Multiple studies have concluded that testosterone leads to polycystic ovary-like morphology (Futterweit and Deligdisch, 1986; Spinder et al., 1989; Pache et al., 1991; Grynberg et al., 2010) while others disagree (Ikeda et al., 2013; Caanen et al., 2017), which may stem from variations in terms and classification. Flattening this nuance into a debate of polycystic ovary-like morphology or not may serve as a barrier to alternative inquiry. Collectively, these studies generally suggest that testosterone therapy leads to some ovarian histological differences. However, it is challenging to determine if there are functional consequences to these changes, in addition to serving as potential biomarkers of prior testosterone exposure. Limitations to these studies include varied testosterone durations (which are often short), serum levels, and administration regimens. High rates of PCOS diagnoses prior to testosterone therapy in transmasculine people may also serve as an additional confounder (Baba et al., 2007; Mueller et al., 2008; Becerra-Fernández et al., 2014). Furthermore, although rarely documented, some surgeons may have required brief pauses in testosterone before surgery and histological comparisons might include ovaries from people after a recent pause in testosterone (Chadha et al., 1994).
Although researchers have attempted to use antimüllerian hormone (AMH) levels to evaluate the functional ovarian reserve after testosterone therapy, studies to date have generally been limited by confounders. After 12 months of testosterone, one prospective study noted a significant decrease in AMH of 0.71 ng/ml (median 4.99 ng/ml) from baseline, but this difference was mainly driven by a decrease in AMH in the 27 patients with prior PCOS and not seen in the 27 who did not have prior PCOS (Yaish et al., 2021). Other studies of AMH with testosterone therapy have included confounding medications that may also alter AMH and have found no difference from baseline (when also using a progestin (Tack et al., 2016)) or a decrease from baseline (when also using a gonadotropin-releasing hormone agonist and an aromatase inhibitor (Caanen et al., 2015)). Other approaches considering the ovarian reserve include histological studies during T therapy, which have demonstrated relatively normal cortical follicular distributions (De Roo et al., 2017; Marschalek et al., 2020) or a greater proportion of primordial follicles with a reduction in the proportion of morphologically healthy primordial follicles and increased markers of oocyte DNA damage for the primordial and transitory follicular pool (Bailie et al., 2023).
Menstrual suppression occurs for many but not all people on masculinizing levels of testosterone. Reports of small numbers of corpora lutea or corpora albicantia suggest that ovulation may be occasionally occurring during testosterone therapy (Futterweit and Deligdisch, 1986; Miller et al., 1986; Spinder et al., 1989; Ikeda et al., 2013; Loverro et al., 2016; Khalifa et al., 2019; Lin et al., 2022). One study followed 22 individuals on testosterone (a mix of new and continuing T users) over 12 weeks and used the urinary indicator of elevated pregnanediol-3-glucoronide for 3 days as a proxy measurement for ovulation. They observed seven people with transient elevations potentially indicative of dysfunctional ovulation and one person with well-defined ovulation. The majority of these elevations were in the month after starting testosterone, although two transient elevations were seen months later (Taub et al., 2020). This pattern of suppressed menses with periodic breakthroughs reinforces the recommendation that testosterone should not be considered sufficient for contraception, which is also supported by multiple reports of pregnancies conceived despite the individuals using T and being amenorrheic (Light et al., 2014).
Uterine impact of testosterone
Studies suggest individuals on testosterone therapy may have two predominant uterine presentations. A mix of proliferative endometria (54/112) and atrophic endometria (50/112) has been reported (Grynberg et al., 2010). Similar findings include a balance of atrophic/inactive endometria (41/81) and active endometria (proliferative 33/81, secretory 3/81) (Hawkins et al., 2021). In addition to these reports with fairly even splits, some studies have reported a predominance of active endometria (Loverro et al., 2016; Grimstad et al., 2019), while others have reported a majority of inactive endometria (Perrone et al., 2009; Lin et al., 2022). Assessment by transvaginal ultrasound demonstrated reduced endometrial thickness for 51 transmasculine people after at least 1 year of testosterone therapy (median 3.9 mm, interquartile range 2.8–5.1 mm) as compared to 77 cisgender controls during the early follicular phase on cycle days 2–5 (median 4.9 mm, interquartile range 4.0–6.3 mm), with the caveat that the data for the transmasculine individuals were collected immediately before gender-affirming surgery and the participants had been advised to pause testosterone for 2–6 weeks prior to surgery (Asseler et al., 2022). Additional uterine findings have included endometrial polyps (Perrone et al., 2009; Lin et al., 2022), endometrial stromal fibrosis (Lin et al., 2022), endometrial tubal metaplasia (Lin et al., 2022), and cervical atrophy (Miller et al., 1986). Notably, persistent bleeding on testosterone (for 12/52) and intermittent pelvic pain or cramping on testosterone (for 30/52) have also been reported (Grimstad et al., 2019). With pauses in testosterone for reproductive purposes, studies generally report the return of menses, although the time course for resumption may vary (Light et al., 2014; Armuand et al., 2017; Adeleye et al., 2019; Leung et al., 2019). While the uterine impact and reversibility of testosterone is particularly relevant for transmasculine and nonbinary individuals interested in gestational parenthood, this understanding may also be relevant for the emerging practice of uterine transplantation, as some transgender men undergoing gender-affirming hysterectomies have reported their willingness to serve as uterine donors (Carbonnel et al., 2022). Broadly, the uterine studies share similar limitations to the ovarian comparisons, including multiple testosterone regimens and durations, and potential poorly documented brief pauses in testosterone before surgery.
Fallopian tube impact of testosterone
Although there are limited reports on the impact and reversibility of fallopian tube changes with testosterone therapy (Patek et al., 1973; Dulohery et al., 2020), androgen receptor expression suggests that testosterone can directly act on the human tubal epithelium (Dulohery et al., 2020). A comparative study noted viscous luminal secretions in the tubal ampulla and luminal narrowing in the isthmus, in contrast to controls with a generally open isthmus and ampulla secretions that ranged from open to watery to viscous during menstrual cycles (Dulohery et al., 2020). While changes in the fallopian tubes are less relevant in the setting of oocyte retrieval, potential changes may be important for attempts at conception with minimal intervention.
Animal models
Large, controlled studies investigating the impact and reversibility of gender-affirming testosterone therapy on reproductive function and fertility cannot be ethically performed in humans. Animal models are frequently utilized to better understand multiple aspects of reproductive physiology, with the acknowledgment that outcomes may not always fully translate across species. Recent mouse models aimed at studying the reproductive impact of gender-affirming testosterone therapy have also demonstrated cycle suppression and a lack of ovarian corpora lutea or reduced corpora lutea while on testosterone (Kinnear et al., 2019; Bartels et al., 2020). These studies have not demonstrated any detectable reduction in the primordial follicle pool of mice on testosterone, suggesting that testosterone likely does not deplete the ovarian reserve (Kinnear et al., 2019, 2023). Furthermore, testosterone-induced acyclicity resolved with cessation of testosterone, with the return of corpora lutea formation noted in one study (Kinnear et al., 2021) and an ongoing reduction in corpora lutea with an increased stromal inflammatory response noted after a longer testosterone exposure (Kinnear et al., 2023). A recent animal model study focused on masculinizing testosterone therapy treated mice with testosterone cypionate injections weekly for 6 weeks and reported similar numbers of fertilized oocytes progressing to the two-cell stage when comparing controls to mice on testosterone or to mice after a period of testosterone cessation (Bartels et al., 2020), also supporting the potential for oocyte retrieval without pausing testosterone.
Although beyond the scope of this review, quite a few animal model studies have focused on androgens and reproduction in the context of studying PCOS, often using prenatal or peripubertal administration of dihydrotestosterone (DHT) (Padmanabhan and Veiga-Lopez, 2013; Walters, 2015). DHT is a nonaromatizable androgen that is not used clinically for gender-affirming care. Studies on adults have also been limited. Sex steroid research has traditionally relied on an organizational/activational paradigm where organizational (permanent) changes could occur during periods of development (prenatal and prepubertal) and changes in adults would only be activational (transient). Over-reliance on this paradigm may have historically limited sex steroid studies in adults (Arnold and Breedlove, 1985), which is relevant as most transgender and nonbinary people start gender-affirming testosterone postpubertally. Importantly, postpubertal animal studies have helped to elucidate neuroendrocrine mechanisms behind androgen-driven menstrual suppression (Esparza et al., 2020), reported reduced fertility and acyclicity in DHT-treated mice when compared to controls (Ma et al., 2017), found similar PCOS-like reproductive changes when comparing DHT-treated to testosterone-treated mice but more metabolic changes with DHT (Aflatounian et al., 2020), and used androgen-receptor knockout mice to suggest that testosterone-induced reproductive changes are likely mediated by both androgenic and estrogenic pathways (Aflatounian et al., 2020). Fundamentally, although PCOS and transmasculine testosterone therapy differ in meaningful ways, animal models attempting to mimic these states often use related or overlapping methods and are relevant to developing a mechanistic understanding of the impact of testosterone on reproduction.
Conclusions and remaining questions
Recent research provides the proof of concept that there are reproductive options for at least some transmasculine and nonbinary people after a period of testosterone therapy. We were able to identify about 99 reports in the medical literature of pregnancies carried by someone previously on testosterone or carried by another using the oocytes from someone previously on testosterone. Furthermore, about 69 live births have been reported from these pregnancies, with some pregnancies ongoing at the time of publication and others with outcomes not reported. Unfortunately, these studies have often selected for successful pregnancy outcomes and so little is known about challenges experienced during conception attempts or pregnancy. Small case series and reports of assisted reproduction using ovarian stimulation in individuals who have paused testosterone have demonstrated successful oocyte retrieval, maturation, and fertilization, with similar results to comparison groups not on testosterone. Questions remain about the potential for continuing testosterone during ovarian stimulation, and there are case reports of two successful births as well as successful oocyte or embryo cryopreservation for four more using oocytes collected while on testosterone. An ongoing body of research describes the impact of testosterone on different organs of the reproductive tract, although the functional impact and reversibility of these testosterone-induced changes remain to be determined. Larger studies are needed to understand the impact of testosterone at each step of the reproductive process, including conception, pregnancy, and birth, and to look at the outcomes for offspring. Given the ethical limitations of controlled studies on human reproductive function and fertility during and after gender-affirming testosterone, we support the use of controlled animal model studies to complement available observational clinical data. We recommend that ongoing research be informed by the needs and lived experiences of transgender and nonbinary people and we encourage multicenter collaborations to increase sample sizes. Despite recent developments in research looking at reproductive capacity after prior testosterone, the studies are small, much uncertainty remains, and fertility preservation prior to testosterone therapy should continue to be offered to those interested in biologically-related children.
Acknowledgements
The graphical abstract was created with BioRender.com.
Contributor Information
Hadrian M Kinnear, Program in Cellular and Molecular Biology, University of Michigan, Ann Arbor, MI, USA; Medical Scientist Training Program, University of Michigan, Ann Arbor, MI, USA.
Molly B Moravek, Division of Reproductive Endocrinology and Infertility, Department of Obstetrics and Gynecology, University of Michigan, Ann Arbor, MI, USA; Department of Urology, University of Michigan, Ann Arbor, MI, USA.
Data availability
No new data were generated or analyzed in this review.
Authors’ roles
H.M.K. and M.B.M. both contributed to the conception and drafting and/or revising of the manuscript, approved the submitted version, and agreed to be accountable for all aspects of the work.
Funding
National Institutes of Health, Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01-HD098233 to M.B.M., F30-HD100163 to H.M.K.).
Conflict of interest
H.M.K. and M.B.M. have nothing to declare.
References
- Adeleye AJ, Cedars MI, Smith J, Mok-Lin E.. Ovarian stimulation for fertility preservation or family building in a cohort of transgender men. J Assist Reprod Genet 2019;39:1733–1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aflatounian A, Edwards MC, Rodriguez Paris V, Bertoldo MJ, Desai R, Gilchrist RB, Ledger WL, Handelsman DJ, Walters KA.. Androgen signaling pathways driving reproductive and metabolic phenotypes in a PCOS mouse model. J Endocrinol 2020;245:381–395. [DOI] [PubMed] [Google Scholar]
- Albar M, Koziarz A, McMahon E, Chan C, Liu K.. Timing of testosterone discontinuation and assisted reproductive technology outcomes in transgender patients: a cohort study. F S Rep 2023;4:55–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amir H, Yaish I, Samara N, Hasson J, Groutz A, Azem F.. Ovarian stimulation outcomes among transgender men compared with fertile cisgender women. J Assist Reprod Genet 2020;37:2463–2472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amirikia H, Savoy-Moore RT, Sundareson AS, Moghissi KS.. The effects of long-term androgen treatment on the ovary. Fertil Steril 1986;45:202–208. [DOI] [PubMed] [Google Scholar]
- Andrews AR, Kakadekar A, Greene DN, Khalifa MA, Santiago V, Schmidt RL.. Histologic findings in surgical pathology specimens from individuals taking masculinizing hormone therapy for the purpose of gender transition. Arch Pathol Lab Med 2022;146:766–779. [DOI] [PubMed] [Google Scholar]
- Armuand G, Dhejne C, Olofsson JII, Rodriguez-Wallberg KAA.. Transgender men’s experiences of fertility preservation: a qualitative study. Hum Reprod 2017;32:383–390. [DOI] [PubMed] [Google Scholar]
- Arnold AP, Breedlove SM.. Organizational and activational effects of sex steroids on brain and behavior: a reanalysis. Horm Behav 1985;19:469–498. [DOI] [PubMed] [Google Scholar]
- Asseler JD, Caanen MR, Verhoeven MO, Huirne JAF, Goddijn M, van Dulmen-den Broeder E, Overbeek A, Lambalk CB, van Mello NM.. Endometrial thickness assessed by transvaginal ultrasound in transmasculine people taking testosterone compared with cisgender women. Reprod Biomed Online 2022;45:1033–1038. [DOI] [PubMed] [Google Scholar]
- Auer MK, Fuss J, Nieder TO, Briken P, Biedermann SV, Stalla GK, Beckmann MW, Hildebrandt T.. Desire to have children among transgender people in Germany: a cross-sectional multi-center study. J Sex Med 2018;15:757–767. [DOI] [PubMed] [Google Scholar]
- Baba T, Endo T, Honnma H, Kitajima Y, Hayashi T, Ikeda H, Masumori N, Kamiya H, Moriwaka O, Saito T.. Association between polycystic ovary syndrome and female-to-male transsexuality. Hum Reprod 2007;22:1011–1016. [DOI] [PubMed] [Google Scholar]
- Bailie E, Maidarti M, Hawthorn R, Jack S, Watson N, Telfer EE, Anderson RA.. The ovaries of transgender men indicate effects of high dose testosterone on the primordial and early growing follicle pool. Reprod Fertil 2023;4:e220102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baram S, Myers SA, Yee S, Librach CL.. Fertility preservation for transgender adolescents and young adults: a systematic review. Hum Reprod Update 2019;25:694–716. [DOI] [PubMed] [Google Scholar]
- Barrett F, Shaw J, Blakemore JK, Fino ME.. Fertility preservation for adolescent and young adult transmen: a case series and insights on oocyte cryopreservation. Front Endocrinol (Lausanne) 2022;13:873508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartels CB, Uliasz TF, Lestz L, Mehlmann LM.. Short-term testosterone use in female mice does not impair fertilizability of eggs: implications for the fertility care of transgender males. Hum Reprod 2020;36:189–198. [DOI] [PubMed] [Google Scholar]
- Becerra-Fernández A, Pérez-López G, Román MM, Martín-Lazaro JF, Pérez MJL, Araque NA, Rodríguez-Molina JM, Sertucha MCB, Vilas MVA.. Prevalence of hyperandrogenism and polycystic ovary syndrome in female to male transsexuals. Endocrinol Nutr 2014;61:351–358. [DOI] [PubMed] [Google Scholar]
- Borrás A, Manau MD, Fabregues F, Casals G, Saco A, Halperin I, Mora M, Goday A, Barral Y, Carmona F.. Endocrinological and ovarian histological investigations in assigned female at birth transgender people undergoing testosterone therapy. Reprod Biomed Online 2021;43:289–297. [DOI] [PubMed] [Google Scholar]
- Broughton D, Omurtag K.. Care of the transgender or gender-nonconforming patient undergoing in vitro fertilization. Int J Transgenderism 2017;18:372–375. [Google Scholar]
- Caanen MR, Schouten NE, Kuijper EAM, van Rijswijk J, van den Berg MH, van Dulmen-den Broeder E, Overbeek A, van Leeuwen FE, van Trotsenburg M, Lambalk CB.. Effects of long-term exogenous testosterone administration on ovarian morphology, determined by transvaginal (3D) ultrasound in female-to-male transsexuals. Hum Reprod 2017;32:1457–1464. [DOI] [PubMed] [Google Scholar]
- Caanen MR, Soleman RS, Kuijper EAM, Kreukels BPC, Roo CD, Tilleman K, Sutter PD, Trotsenburg MAA, van Broekmans FJ, Lambalk CB. et al. Antimüllerian hormone levels decrease in female-to-male transsexuals using testosterone as cross-sex therapy. Fertil Steril 2015;103:1340–1345. [DOI] [PubMed] [Google Scholar]
- Carbonnel M, Karpel L, Corruble N, Legendri S, Pencole L, Cordier B, Racowsky C, Ayoubi J-M.. Transgender males as potential donors for uterus transplantation: a survey. J Clin Med 2022;11:6081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chadha S, Pache TD, Huikeshoven FJM, Brinkmann AO, Kwast TH, van der. Androgen receptor expression in human ovarian and uterine tissue of long term androgen-treated transsexual women. Hum Pathol 1994;25:1198–1204. [DOI] [PubMed] [Google Scholar]
- Cho K, Harjee R, Roberts J, Dunne C.. Fertility preservation in a transgender man without prolonged discontinuation of testosterone: a case report and literature review. F S Rep 2020;1:43–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christodoulaki A, He H, Zhou M, Cardona Barberán A, De Roo C, Chuva De Sousa Lopes SM, Baetens M, Menten B, Van Soom A, De Sutter P. et al. Characterization of ovarian tissue oocytes from transgender men reveals poor calcium release and embryo development, which might be overcome by spindle transfer. Hum Reprod 2023;38:1135–1150. [DOI] [PubMed] [Google Scholar]
- Coleman E, Radix AE, Bouman WP, Brown GR, Vries A D, Deutsch MB, Ettner R, Fraser L, Goodman M, Green J. et al. Standards of care for the health of transgender and gender diverse people, version 8. Int J Transgend Health 2022;23:S1–S259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Roo C, Lierman S, Tilleman K, Peynshaert K, Braeckmans K, Caanen M, Lambalk CB, Weyers S, T'Sjoen G, Cornelissen R. et al. Ovarian tissue cryopreservation in female-to-male transgender people: insights into ovarian histology and physiology after prolonged androgen treatment. Reprod Biomed Online 2017;34:557–566. [DOI] [PubMed] [Google Scholar]
- de Sousa Resende S, Kussumoto VH, Arima FHC, Krul PC, Rodovalho NCM, de Jesus Sampaio MR, Alves MM.. A transgender man, a cisgender woman, and assisted reproductive technologies: a Brazilian case report. J Bras Reprod Assist 2020;24:513–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dulohery K, Trottmann M, Bour S, Liedl B, Alba‐Alejandre I, Reese S, Hughes B, Stief CG, Kölle S.. How do elevated levels of testosterone affect the function of the human fallopian tube and fertility?—new insights. Mol Reprod Dev 2020;87:30–44. [DOI] [PubMed] [Google Scholar]
- Ellis SA, Wojnar DM, Pettinato M.. Conception, pregnancy, and birth experiences of male and gender variant gestational parents: it’s how we could have a family. J Midwifery Womens Health 2015;60:62–69. [DOI] [PubMed] [Google Scholar]
- Esparza LA, Terasaka T, Lawson MA, Kauffman AS.. Androgen suppresses in vivo and in vitro LH pulse secretion and neural Kiss1 and Tac2 gene expression in female mice. Endocrinology 2020;161:bqaa191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ethics Committee of the American Society for Reproductive Medicine. Access to fertility services by transgender persons: an Ethics Committee opinion. Fertil Steril 2015;104:1111–1115. [DOI] [PubMed] [Google Scholar]
- Falck F, Frisén L, Dhejne C, Armuand G.. Undergoing pregnancy and childbirth as trans masculine in Sweden: experiencing and dealing with structural discrimination, gender norms and microaggressions in antenatal care, delivery and gender clinics. Int J Transgend Health 2020;22:42–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer OJ. Non-binary reproduction: Stories of conception, pregnancy, and birth. Int J Transgend Health 2021;22:77–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Futterweit W, Deligdisch L.. Histopathological effects of exogenously administered testosterone in 19 female to male transsexuals. J Clin Endocrinol Metab 1986;62:16–21. [DOI] [PubMed] [Google Scholar]
- Gale J, Magee B, Forsyth-Greig A, Visram H, Jackson A.. Oocyte cryopreservation in a transgender man on long-term testosterone therapy: a case report. F S Rep 2021;2:249–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald P, Dubois B, Lekovich J, Pang JH, Safer J.. Successful in vitro fertilization in a cisgender female carrier using oocytes retrieved from a transgender man maintained on testosterone. AACE Clin Case Rep 2021;8:19–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimstad FW, Fowler KG, New EP, Ferrando CA, Pollard RR, Chapman G, Gomez-Lobo V, Gray M.. Uterine pathology in transmasculine persons on testosterone: a retrospective multicenter case series. Am J Obstet Gynecol 2019;220:257.e1–257.e7. [DOI] [PubMed] [Google Scholar]
- Grynberg M, Fanchin R, Dubost G, Colau JC, Brémont-Weil C, Frydman R, Ayoubi J-M.. Histology of genital tract and breast tissue after long-term testosterone administration in a female-to-male transsexual population. Reprod Biomed Online 2010;20:553–558. [DOI] [PubMed] [Google Scholar]
- Hahn M, Sheran N, Weber S, Cohan D, Obedin-Maliver J.. Providing patient-centered perinatal care for transgender men and gender-diverse individuals. Obstet Gynecol 2019;134:959–963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins M, Deutsch MB, Obedin-Maliver J, Stark B, Grubman J, Jacoby A, Jacoby VL.. Endometrial findings among transgender and gender nonbinary people using testosterone at the time of gender-affirming hysterectomy. Fertil Steril 2021;115:1312–1317. [DOI] [PubMed] [Google Scholar]
- Hembree WC, Cohen-Kettenis PT, Gooren L, Hannema SE, Meyer WJ, Murad MH, Rosenthal SM, Safer JD, Tangpricha V, T’Sjoen GG.. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2017;102:1–35. [DOI] [PubMed] [Google Scholar]
- Hughesdon PE. Morphology and morphogenesis of the Stein-Leventhal ovary and of so-called “hyperthecosis”. Obstet Gynecol Surv 1982;37:59–77. [DOI] [PubMed] [Google Scholar]
- Ikeda K, Baba T, Noguchi H, Nagasawa K, Endo T, Kiya T, Saito T.. Excessive androgen exposure in female-to-male transsexual persons of reproductive age induces hyperplasia of the ovarian cortex and stroma but not polycystic ovary morphology. Hum Reprod 2013;28:453–461. [DOI] [PubMed] [Google Scholar]
- Insogna IG, Ginsburg E, Srouji S.. Fertility preservation for adolescent transgender male patients: a case series. J Adolesc Health 2020;66:750–753. [DOI] [PubMed] [Google Scholar]
- Israeli T, Preisler L, Kalma Y, Samara N, Levi S, Groutz A, Azem F, Amir H.. Similar fertilization rates and preimplantation embryo development among testosterone-treated transgender men and cisgender women. Reprod Biomed Online 2022;45:448–456. [DOI] [PubMed] [Google Scholar]
- Khalifa MA, Toyama A, Klein ME, Santiago V.. Histologic features of hysterectomy specimens from female-male transgender individuals. Int J Gynecol Pathol 2019;38:520–527. [DOI] [PubMed] [Google Scholar]
- Kinnear HM, Constance ES, David A, Marsh EE, Padmanabhan V, Shikanov A, Moravek MB.. A mouse model to investigate the impact of testosterone therapy on reproduction in transgender men. Hum Reprod 2019;34:2009–2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinnear HM, Hashim PH, Cruz C, Dela Chang FL, Rubenstein G, Nimmagadda L, Elangovan VR, Jones A, Brunette MA, Hannum DF. et al. Presence of ovarian stromal aberrations after cessation of testosterone therapy in a transgender mouse model. Biol Reprod 2023;108:802–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinnear HM, Hashim PH, Cruz C, Dela Rubenstein G, Chang FL, Nimmagadda L, Brunette MA, Padmanabhan V, Shikanov A, Moravek MB.. Reversibility of testosterone-induced acyclicity after testosterone cessation in a transgender mouse model. F S Sci 2021;2:116–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung A, Sakkas D, Pang S, Thornton K, Resetkova N.. Assisted reproductive technology outcomes in female-to-male transgender patients compared with cisgender patients: a new frontier in reproductive medicine. Fertil Steril 2019;112:858–865. [DOI] [PubMed] [Google Scholar]
- Lierman S, Tilleman K, Braeckmans K, Peynshaert K, Weyers S, T'Sjoen G, De Sutter P.. Fertility preservation for trans men: frozen-thawed in vitro matured oocytes collected at the time of ovarian tissue processing exhibit normal meiotic spindles. J Assist Reprod Genet 2017;34:1449–1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lierman S, Tolpe A, De Croo I, De Gheselle S, Defreyne J, Baetens M, Dheedene A, Colman R, Menten B, T’Sjoen G. et al. Low feasibility of in vitro matured oocytes originating from cumulus complexes found during ovarian tissue preparation at the moment of gender confirmation surgery and during testosterone treatment for fertility preservation in transgender men. Fertil Steril 2021;116:1068–1076. [DOI] [PubMed] [Google Scholar]
- Light AD, Obedin-Maliver J, Sevelius JM, Kerns JL.. Transgender men who experienced pregnancy after female-to-male gender transitioning. Obstet Gynecol 2014;124:1120–1127. [DOI] [PubMed] [Google Scholar]
- Light A, Wang LF, Zeymo A, Gomez-Lobo V.. Family planning and contraception use in transgender men. Contraception 2018;98:266–269. [DOI] [PubMed] [Google Scholar]
- Lin LH, Hernandez A, Marcus A, Deng F-M, Adler E.. Histologic findings in gynecologic tissue from transmasculine individuals undergoing gender-affirming surgery. Arch Pathol Lab Med 2022;146:742–748. [DOI] [PubMed] [Google Scholar]
- Loverro G, Resta L, Dellino M, Edoardo DN, Cascarano MA, Loverro M, Mastrolia SA.. Uterine and ovarian changes during testosterone administration in young female-to-male transsexuals. Taiwan J Obstet Gynecol 2016;55:686–691. [DOI] [PubMed] [Google Scholar]
- Ma Y, Andrisse S, Chen Y, Childress S, Xue P, Wang Z, Jones D, Ko C, Divall S, Wu S.. Androgen receptor in the ovary theca cells plays a critical role in androgen-induced reproductive dysfunction. Endocrinology 2017;158:98–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marschalek J, Pietrowski D, Dekan S, Marschalek M-L, Brandstetter M, Ott J.. Markers of vitality in ovaries of transmen after long-term androgen treatment: a prospective cohort study. Mol Med 2020;26:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller N, Bédard YC, Cooter NB, Shaul DL.. Histological changes in the genital tract in transsexual women following androgen therapy. Histopathology 1986;10:661–669. [DOI] [PubMed] [Google Scholar]
- Moravek MB, Dixon M, Pena SM, Obedin-Maliver J.. Management of testosterone around ovarian stimulation in transmasculine patients: challenging common practices to meet patient needs-2 case reports. Hum Reprod 2023;38:482–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moravek MB, Kinnear HM, George J, Batchelor J, Shikanov A, Padmanabhan V, Randolph JF.. Impact of exogenous testosterone on reproduction in transgender men. Endocrinology 2020;161:bqaa014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moseson H, Fix L, Hastings J, Stoeffler A, Lunn MR, Flentje A, Lubensky ME, Capriotti MR, Ragosta S, Forsberg H. et al. Pregnancy intentions and outcomes among transgender, nonbinary, and gender-expansive people assigned female or intersex at birth in the United States: results from a national, quantitative survey. Int J Transgend Health 2021;22:30–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller A, Gooren LJ, Naton-Schötz S, Cupisti S, Beckmann MW, Dittrich R.. Prevalence of polycystic ovary syndrome and hyperandrogenemia in female-to-male transsexuals. J Clin Endocrinol Metab 2008;93:1408–1411. [DOI] [PubMed] [Google Scholar]
- Pache TD, Chadha S, Gooren LJG, Hop WCJ, Jaarsma KW, Dommerholt HBR, Fauser BCJM.. Ovarian morphology in long-term androgen-treated female to male transsexuals. A human model for the study of polycystic ovarian syndrome? Histopathology 1991;19:445–452. [DOI] [PubMed] [Google Scholar]
- Padmanabhan V, Veiga-Lopez A.. Animal models of the polycystic ovary syndrome phenotype. Steroids 2013;78:734–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patek E, Nilsson L, Johannisson E, Hellema M, Bout J.. Scanning electron microscopic study of the human fallopian tube. Report III. The effect of midpregnancy and of various steroids. Fertil Steril 1973;24:31–43. [PubMed] [Google Scholar]
- Perrone AM, Cerpolini S, Maria Salfi NC, Ceccarelli C, De Giorgi LB, Formelli G, Casadio P, Ghi T, Pelusi G, Pelusi C. et al. Effect of long‐term testosterone administration on the endometrium of female‐to‐male (FtM) transsexuals. J Sex Med 2009;6:3193–3200. [DOI] [PubMed] [Google Scholar]
- Spinder T, Spijkstra JJ, Tweel JG, van den Burger CW, Kessel H, van Hompes PGA, Gooren LJG.. The effects of long term testosterone administration on pulsatile luteinizing hormone secretion and on ovarian histology in eugonadal female to male transsexual subjects. J Clin Endocrinol Metab 1989;69:151–157. [DOI] [PubMed] [Google Scholar]
- Stark BA, Mok-Lin E.. Fertility preservation in transgender men without discontinuation of testosterone. F S Rep 2022;3:153–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroumsa D, Roberts EF, Kinnear H, Harris LH.. The power and limits of classification—a 32-year-old man with abdominal pain. N Engl J Med 2019;380:1885–1888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tack LJW, Craen M, Dhondt K, Bossche H, Vanden Laridaen J, Cools M.. Consecutive lynestrenol and cross-sex hormone treatment in biological female adolescents with gender dysphoria: a retrospective analysis. Biol Sex Differ 2016;7:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taub RL, Ellis SA, Neal-Perry G, Magaret AS, Prager SW, Micks EA.. The effect of testosterone on ovulatory function in transmasculine individuals. Am J Obstet Gynecol 2020;223:229.e1–229.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Food and Drug Administration. Testosterone Cypionate Injection. 2022. https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/216318s000lbl.pdf (13 June 2023, date last accessed).
- Walters KA. Role of androgens in normal and pathological ovarian function. Reproduction 2015;149:R193–R218. [DOI] [PubMed] [Google Scholar]
- Yaish I, Tordjman K, Amir H, Malinger G, Salemnick Y, Shefer G, Serebro M, Azem F, Golani N, Sofer Y. et al. Functional ovarian reserve in transgender men receiving testosterone therapy: evidence for preserved anti-Müllerian hormone and antral follicle count under prolonged treatment. Hum Reprod 2021;36:2753–2760. [DOI] [PubMed] [Google Scholar]
- Yoshida A, Kaji T, Imaizumi J, Shirakawa A, Suga K, Nakagawa R, Maeda K, Irahara M, Iwasa T.. Transgender man receiving testosterone treatment became pregnant and delivered a girl: a case report. J Obstet Gynaecol Res 2022;48:866–868. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were generated or analyzed in this review.


