Abstract
Objective
Our study aimed to explore the diagnostic value of triglyceride–glucose (TyG) and its related parameters in metabolism-associated fatty liver disease (MAFLD).
Design
A cross-sectional study of residents who attended medical checkups at the First Hospital of Nanping City, Fujian Medical University, between 2015 and 2017.
Setting
One participation centre.
Participants
2605 subjects met the inclusion–exclusion criteria and were grouped according to whether they had MAFLD.
Results
The TyG index and its associated parameters are positively associated with the risk of developing MAFLD (p<0.001). Restriction cube spline analysis showed a significant dose–response relationship between the TyG index and MAFLD. The risk of developing MAFLD increases significantly with a higher TyG index. After adjusting for confounders, this relationship remains (OR: 4.89, 95% CI 3.98 to 6.00). The areas under the receiver operating characteristic curves of the TyG index for MAFLD detection were 0.793 (0.774 to 0.812). The areas under the curve (AUC) of TyG-related parameters were improved, among which TyG-waist circumference (TyG-WC) showed the largest AUC for MAFLD detection (0.873, 95% CI 0.860 to 0.887). In addition, the best cut-off value of the TyG-WC was 716.743, with a sensitivity and specificity of 88.7% and 71.4%, respectively.
Conclusion
The TyG index effectively identifies MAFLD, and the TyG-related parameters improved the identification and diagnosis of MAFLD, suggesting that TyG-related parameters, especially TyG-WC, may be a useful marker for diagnosing MAFLD.
Keywords: epidemiology, hepatology, lipid disorders
STRENGTHS AND LIMITATIONS OF THIS STUDY.
We combined metabolic-related indices with the triglyceride–glucose (TyG) index to diagnose metabolism-associated fatty liver disease (MAFLD) with a comprehensive index.
This study used the latest diagnostic criteria to define MAFLD.
The strengths of this study are the large sample size and the rigorous screening of subjects.
A more comprehensive range of confounding variables was considered compared with previous studies.
Measurement error in self-reported dietary habits and other data in this study is unavoidable.
Introduction
Non-alcoholic fatty liver disease (NAFLD), with hepatic steatosis as the main pathological manifestation, can progress to cirrhosis and hepatocellular carcinoma,1 2 affecting approximately one-quarter of the adult population worldwide.3 In recent years, there has been increasing recognition of the inherent flaws in the term ‘non-alcoholic’. It overemphasises the presence or absence of alcohol use disorders and ignores the importance of metabolic risk for NAFLD progression. As such, an international panel of experts renamed NAFLD to metabolism-associated fatty liver disease (MAFLD) in 2020.4 MAFLD is a more appropriate disease designation for liver diseases associated with metabolic dysfunction.5 Due to its high global prevalence, it poses a serious threat to human health and a huge economic burden to society.6 Steatosis is a reversible condition in its early stages and can be addressed through behavioural changes.7 8 For example, increasing physical activity and controlling energy intake are particularly effective interventions in the early stages of the disease.9 10 However, the aggressive form of steatohepatitis can progress to fibrosis and eventually cirrhosis, which is irreversible damage.11 Due to the high prevalence of MAFLD and its progressive nature, the early detection of MAFLD is of great significance to enable the provision of early intervention, thus avoiding the progression of MAFLD.12
Although the gold standard for identifying fatty liver disease (FLD) is still liver biopsy, it is unsuitable for large-scale epidemiological surveys because of its invasiveness, poor acceptability, cost and sampling variability.12 Thus, it is necessary to develop a simple tool to identify MAFLD. Significant progress has been made in the non-invasive assessment of FLD in recent years, including fatty liver index (FLI) and hepatic steatosis index (HSI).13 The FLI is a prevalent biomarker panel consisting of body mass index (BMI), waist circumference (WC), triglycerides (TGs) and gamma-glutamyl transferase.14 The HSI is a biomarker panel consisting of BMI, diabetes and the alanine transaminase (ALT)/aspartate transaminase (AST) ratio.15 However, the calculation process of both indices is more complicated and involves more traits and indicators. An ideal non-invasive test should be simple, easily accessible, cost-effective, and efficient and allow easy visualisation to detect and identify people at high risk of MAFLD.16 With such a test, large-scale population-wide screening and preventive programmes in large populations would be possible. Prior studies have confirmed that insulin resistance (IR) is an important pathogenic mechanism in MAFLD.17 Homeostasis model assessment of insulin resistance (HOMA-IR) is the gold standard diagnostic method of IR and has an excellent diagnostic effect on MAFLD.18 However, HOMA-IR is costly, time-consuming and complex, which limits its widespread implementation in large epidemiological investigations.19 Triglyceride–glucose (TyG), a non-invasive index calculated from fasting glucose and TGs, has been proposed as a reliable marker for IR in clinical practice.20 Since MAFLD is associated with IR and dyslipidaemia, the TyG index is also considered a useful predictive marker for MAFLD.21 However, the results from epidemiological studies remain controversial.22 The longitudinal association between baseline TyG index and the risk of MAFLD was assessed in a cohort study conducted in Jiangsu, China, which included 2056 subjects.21 The results showed that the TyG index was independently associated with the risk of developing MAFLD (HR: 1.784, 95% CI 1.383 to 2.302, p<0.001).21 A cross-sectional study in US adults also showed a positive association between the TyG index and the risk of MAFLD/NAFLD; as for MAFLD, TyG-WC presented the highest OR (OR 28.435, 95% CI 12.121 to 66.705).23 However, the sample sizes of these studies were small, and more large prospective studies are needed to validate the association between the two further. Nanping City is located in the north of Fujian Province. Our previous study reported the prevalence of NAFLD (32.8%) in the population with physical examination in Nanping,24 which is higher than in other cities in Fujian province.25 The present study aimed to investigate the association of the TyG index and its related parameters with MAFLD in Nanping and to assess their diagnostic efficacy for MAFLD.
Material and methods
Study subjects and design
This cross-sectional study included 2605 subjects who underwent a physical examination and completed an abdominal ultrasound examination at Nanping First Hospital, Fujian Medical University (Nanping, China) between April 2015 and August 2017. All the participants provided their informed consent before the study started.
The inclusion criteria for participants in the current study were permanent residency in Nanping, aged between 18 and 75 years, and completed ultrasonography examination. The diagnosis of FLD in this study was primarily based on ultrasonographic findings rather than a liver biopsy26 because recent standardised criteria have significantly improved the diagnostic accuracy of ultrasonography so that even minor degrees of steatosis can be detected. Subjects with malignant tumours, incomplete data or pregnant or lactating women were excluded.
Data collection and measure
Data on MAFLD risk factors were obtained through direct interviews with the help of a structured medical questionnaire. The risk factors included were age, gender, marital status, income, educational level, smoking, drinking, lifestyle, dietary habits, medical history and family history of MAFLD. After an overnight fast, all subjects underwent a physical examination in the morning. The clinical variables collected were height (m2), weight (kg), WC (cm), hip circumference (cm), waist-to-hip ratio (WHR), diastolic blood pressure (DBP, mm Hg), and systolic blood pressure (SBP, mm Hg), serum TG (mg/dL), total cholesterol (TC, mmol/L), low-density lipoprotein (mmol/L), and high-density lipoprotein (HDL, mmol/L), fasting plasma glucose (FPG, mg/dL), gamma-glutamyltransferase (GGT, U/L) ALT (U/L) and AST (U/L). All these variables were assessed using standard procedures (TG: 1 mmol/L=88.5 mg/dL; FPG: 1 mmol/L=18 mg/dL). BMI was calculated as body weight/(height)2. Food consumption was assessed with the help of a food frequency questionnaire, and total consumption was calculated by multiplying the frequency of food consumption by the amount of food consumed each time. Hypertension was defined as SBP ≥140 mm Hg and/or DBP ≥90 mm Hg or the current use of antihypertensive medication.27 Diabetes was defined as FPG ≥7.0 mmol/L or the current use of hypoglycaemic agents.28
Triglyceride–glucose index and related parameters
The TyG index and its related parameters were calculated according to the previous studies.20 26 The specific calculation formulas were as follows:
TyG=ln [fasting triglyceride (mg/dL) × fasting plasma glucose (mg/dL)/2].
TyG-WC=TyG× WC.
TyG-BMI=TyG× BMI.
TyG-WHR=TyG× WHR.
Diagnostic of FLD
Liver ultrasonography is used to diagnose fatty liver. The presence of criteria (1) and any of criteria (2) through (4) indicates the presence of fatty liver: (1) diffuse enhancement of the near-field echoes of the liver and gradual attenuation of the far-field echoes of the liver; (2) mild-to-moderate hepatomegaly with rounded obtuse borders; (3) unclear structure of intrahepatic ducts; (4) reduced hepatic blood flow signal.
Diagnosis of MAFLD
MAFLD is diagnosed by ultrasound showing hepatic steatosis and having one of the following three criteria (3) : (1) overweight or obesity (BMI≥23.0 kg/m2 for Asians); (2) type 2 diabetes mellitus; and (3) metabolic dysregulation among non-overweight individuals (BMI<23.0 kg/m2). The metabolic disorder was defined as the presence of at least two of the following metabolic risk abnormalities: (1) WC≥90 cm for Asian men and 80 cm for Asian women; (2) BP≥130/85 mm Hg or specific drug treatment; (3) TG≥1.70 mmol/L or specific drug treatment; (4) HDL-c<1.0 mmol/L for men and <1.3 mmol/L for women; (5) pre-diabetes; (6) HOMA-IR≥2.5; and (7) C-reactive protein>2 mg/L. Non-overweight individuals meeting any two or more metabolic disorders are diagnosed as MAFLD.
Statistical analyses
The baseline characteristics of subjects were analysed using the non-parametric Kruskal-Wallis test for non-normal continuous variables and the χ2 test for nominal variables. Continuous variables were expressed as median (IQR). Univariate and multivariate logistic regression methods were used to analyse the association of TyG and related parameters with MAFLD risk. The restricted cubic spline (RCS) was used to explore the dose–response relationship between TyG and its related parameters and the risk of MAFLD. The predictive value of TyG and related parameters were compared using the area under receiver operating characteristic (AUROC). The Net Reclassification Index (NRI) and the Integrated Discrimination Improvement Index (IDI) were used to reflect the overall improvement of the diagnostic model. All analyses were performed in R (V.4.2.1, R Foundation) software or SPSS V.26.0 software. All p values were based on the two-sided test, and p<0.05 was considered statistically significant.
Patient and public involvement
Patients or the public were not involved in our research’s design, conduct, reporting or dissemination plans.
Results
Baseline characteristics
Demographic and lifestyle habits and clinical characteristics are detailed in table 1 and table 2. Of the 2605 participants, 747 had FLD, with an FLD prevalence of 28.68%; 726 were patients with MAFLD, and the prevalence of MAFLD was 27.9%. The mean age of the participants was 45 years, and 56.5% of the subjects were male. Compared with those without MAFLD, subjects with MAFLD were more likely to be male, older, married, smokers, drinkers, tea drinkers and have a history of diabetes or hypertension (all p<0.05). In addition, the subjects in both groups were different in terms of clinical detection indicators (SBP, DBP, TG, FPG, TC, GGT, HDL, BMI, WC, WHR, FLI and HSI) (all p<0.001).
Table 1.
Comparison of general characteristics
| Variables | Overall (n=2605) | With MAFLD (n=726) | Without MAFLD (n=1879) | P value* |
| Age (years), M (IQR) | 45 (33, 52) | 43 (31, 51) | 48 (38, 54) | <0.001 |
| Gender, n (%) | <0.001 | |||
| Males | 1471 (56.5) | 584 (80.4) | 887 (47.2) | |
| Females | 1134 (43.5) | 142 (19.6) | 992 (52.8) | |
| Marital status, n (%) | <0.001 | |||
| Single | 378 (14.5) | 68 (9.4) | 310 (16.5) | |
| Married | 2209 (84.8) | 652 (89.8) | 1557 (82.9) | |
| Divorced | 9 (0.4) | 2 (0.3) | 7 (0.4) | |
| Widowed | 9 (0.4) | 4 (0.6) | 5 (0.3) | |
| Educational level, n (%) | 0.032 | |||
| Bachelor’s degree or above | 913 (35.1) | 228 (31.4) | 685 (36.5) | |
| Junior college | 603 (23.2) | 172 (23.7) | 431 (22.9) | |
| Senior high school | 593 (22.8) | 189 (26.0) | 404 (21.5) | |
| Junior high school | 319 (12.3) | 87 (12.0) | 232 (12.3) | |
| Primary school | 140 (5.4) | 35 (4.8) | 105 (5.6) | |
| Illiteracy | 37 (1.4) | 15 (2.1) | 22 (1.2) | |
| Income (yuan/month), n (%) | 0.066 | |||
| <2000 | 147 (5.6) | 35 (4.8) | 112 (6.0) | |
| 2000–3000 | 794 (30.5) | 202 (27.8) | 592 (31.5) | |
| ≥3000 | 1664 (63.9) | 489 (67.4) | 1175 (62.5) | |
| Smoking status, n (%) | <0.001 | |||
| Never | 1916 (73.6) | 448 (61.7) | 1468 (78.1) | |
| Former | 113 (4.3) | 45 (6.2) | 68 (3.6) | |
| Current | 576 (22.1) | 233 (32.1) | 343 (18.3) | |
| Drinking status, n (%) | <0.001 | |||
| Never | 1624 (62.3) | 389 (53.6) | 1235 (65.7) | |
| Former | 42 (1.6) | 15 (2.1) | 27 (1.4) | |
| Current | 939 (36.1) | 322 (44.4) | 617 (32.8) | |
| Tea drinking status, n (%) | <0.001 | |||
| Never | 1052 (40.4) | 205 (28.2) | 847 (45.1) | |
| Former | 8 (0.3) | 3 (0.4) | 5 (0.3) | |
| Current | 1545 (59.3) | 518 (71.3) | 1027 (54.7) | |
| History of diabetes, n (%) | <0.001 | |||
| No | 2459 (94.4) | 650 (89.5) | 1809 (96.3) | |
| Yes | 146 (5.6) | 76 (10.5) | 70 (3.7) | |
| History of hypertension, n (%) | <0.001 | |||
| No | 1666 (64.0) | 294 (40.5) | 1372 (73.0) | |
| Yes | 939 (36.1) | 432 (59.5) | 507 (27.0) |
Data are presented as median with the IQR (M (P25, P75)).
*Comparison of the differences between the groups calculated by Mann-Whitney U or χ2 tests.
Table 2.
Evaluation of biochemical indices
| Variables | Overall (n=2605) | With MAFLD (n=726) | Without MAFLD (n=1879) | P value* |
| BMI (kg/m²), M (IQR) | 22.9 (20.8, 25.1) | 25.4 (23.9, 27.0) | 22.0 (20.3, 23.8) | <0.001 |
| SBP (mm Hg), M (IQR) | 118 (110, 128) | 125 (118, 136) | 115 (107, 123) | <0.001 |
| DBP (mm Hg), M (IQR) | 80 (72, 86) | 85 (80, 90) | 78 (70, 82) | <0.001 |
| TG (mg/dL), M (IQR) | 109.7 (79.7, 163.8) | 169.0 (118.6, 243.4) | 94.7 (73.5, 131.9) | <0.001 |
| FPG (mg/dL), M (IQR) | 93.1 (88.4, 99.7) | 96.7 (91.1, 106.4) | 92.2 (87.7, 97.2) | <0.001 |
| TC (mmol/L), M (IQR) | 5.0 (4.5, 5.6) | 5.2 (4.7, 5.9) | 5.0 (4.4, 5.5) | 0.007 |
| GGT (U/L), M (IQR) | 23 (16, 36) | 34 (24, 52) | 20 (15, 29) | <0.001 |
| HDL (mmol/L), M (IQR) | 1.3 (1.1, 1.5) | 1.2 (1.0, 1.3) | 1.4 (1.2, 1.5) | <0.001 |
| WC (cm), M (IQR) | 82 (75, 89) | 90 (85, 95) | 78 (70, 85) | <0.001 |
| WHR, M (IQR) | 0.9 (0.8, 0.9) | 0.9 (0.9, 0.9) | 0.84 (0.8, 0.9) | <0.001 |
| FLI, M (IQR) | 0.3 (0.1, 1.1) | 1.4 (0.6, 3.4) | 0.2 (0.1, 0.5) | <0.001 |
| HSI, M (IQR) | 31.6 (28.5, 34.8) | 35.5 (32.9, 38.6) | 30.2 (27.7, 32.9) | <0.001 |
| TyG, M (IQR) | 8.6 (8.2, 9.0) | 9.0 (8.7, 9.4) | 8.4 (8.1, 8.7) | <0.001 |
| TyG-WC, M (IQR) | 703.1 (623.9, 790.6) | 814.6 (759.2, 875.4) | 660.9 (600.3, 730.5) | <0.001 |
| TyG-BMI, M (IQR) | 197.0 (174.2, 222.6) | 228.8 (211.0, 248.9) | 184.3 (167.4, 205.1) | <0.001 |
| TyG-WHR, M (IQR) | 7.4 (6.7, 8.1) | 8.2 (7.7, 8.7) | 7.1 (6.5, 7.7) | <0.001 |
Data are presented as median with the IQR (M (P25, P75)).
*Comparison of the differences between the groups calculated by the Mann-Whitney U test.
BMI, body mass index; DBP, diastolic blood pressure; FLI, fatty liver index; FPG, fasting plasma glucose; GGT, gamma-glutamyltransferase; HDL, high-density lipoprotein; HIS, hepatic steatosis index; SBP, systolic blood pressure; TC, total cholesterol; TG, serum triglyceride; TyG, triglyceride–glucose; TyG-BMI, triglyceride–glucose body mass index; TyG-WC, triglyceride–glucose waist circumference; TyG-WHR, triglyceride–glucose waist-to-hip ratio; WC, waist circumference; WHR, waist-to-hip ratio.
Association of MAFLD with TyG and its related parameters
The associations between MAFLD and TyG and its related parameters were mainly analysed using the logistic regression model. In the crude model, TyG and its related parameters were positively correlated with MAFLD risk (table 3). The positive correlations of TyG and its related parameters with MAFLD remained unchanged after adjusting for gender, age, marital status and educational level in model 1 (each p<0.001). Model 2 further adjusted for variables such as smoking, drinking and tea drinking based on model 1. The results remained unchanged (each p<0.001). The results remained similar after adjusting some disease history indicators in model 3.
Table 3.
Univariate and multivariate logistic analysis of triglyceride–glucose (TyG) and related parameters and metabolism-associated fatty liver disease (MAFLD)
| Variables | Crude model | Model 1* | Model 2† | Model 3‡ | ||||
| OR (95% CI) | P value | OR (95%CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | |
| TyG | 6.33 (5.27 to 7.60) | <0.001 | 4.96 (4.09 to 6.01) | <0.001 | 5.15 (4.23 to 6.27) | <0.001 | 4.89 (3.98 to 6.00) | <0.001 |
| TyG-WC | 1.02 (1.01 to 1.02) | <0.001 | 1.01 (1.01 to 1.02) | <0.001 | 1.02 (1.01 to 1.02) | <0.001 | 1.01 (1.01 to 1.02) | <0.001 |
| TyG-BMI | 1.05 (1.05 to 1.05) | <0.001 | 1.05 (1.04 to 1.05) | <0.001 | 1.05 (1.04 to 1.05) | <0.001 | 1.05 (1.04 to 1.05) | <0.001 |
| TyG-WHR | 4.44 (3.89 to 5.08) | <0.001 | 4.18 (3.60 to 4.87) | <0.001 | 4.32 (3.70 to 5.04) | <0.001 | 4.08 (3.48 to 4.78) | <0.001 |
*Adjusted for gender, age, marital status and educational level.
†Adjusted for gender, age, marital status, educational level, smoking, drinking and tea drinking.
‡Adjusted for gender, age, marital status, educational level, smoking, drinking, tea drinking, history of diabetes and history of hypertension.
TyG, triglyceride–glucose; TyG-BMI, triglyceride–glucose body mass index; TyG-WC, triglyceride–glucose waist circumference; TyG-WHR, triglyceride–glucose waist-to-hip ratio.
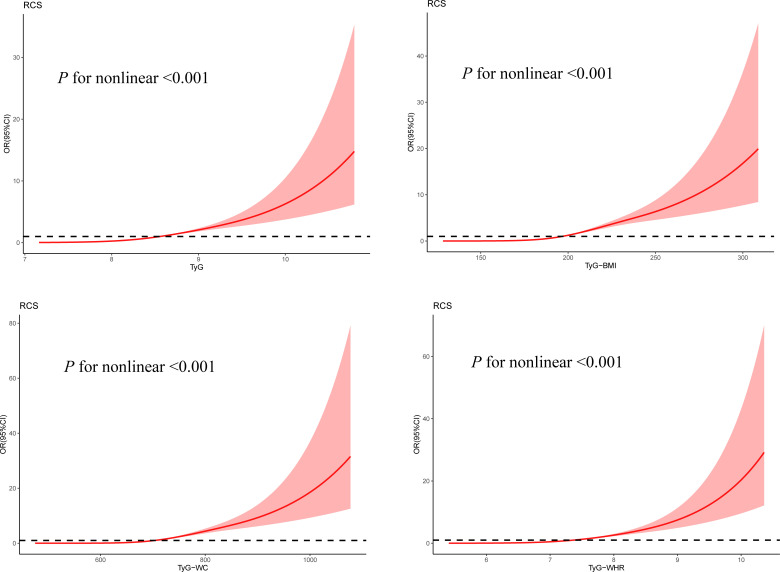
The RCS analyses were applied to interpret the dose–response relationships of TyG and its related parameters with MAFLD risk (figure 1). The ORs of MAFLD increased with increasing TyG levels. The ORs of MAFLD also rose with the increasing TyG-BMI, TyG-WC and TyG-WHR.
Figure 1.
Restrictive cubic spline modelling of the association between NAFLD and TyG and its related parameters. Red area, 95% CI. Each model was adjusted for gender, age, marital status, educational level, smoking, drinking, tea drinking, history of diabetes and history of hypertension.
Assessment of the accuracy of TyG and its related parameters for the diagnosis of MAFLD
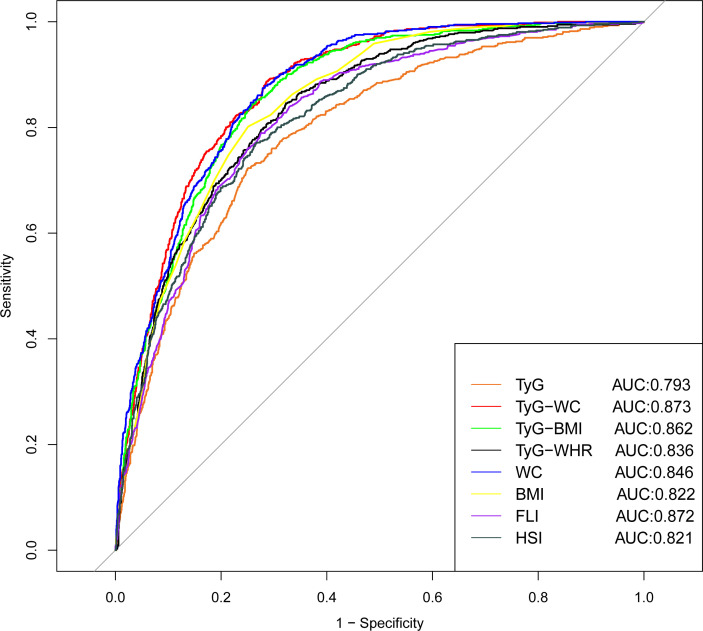
The ROC curve for the ability of TyG and its related parameters and traditional indicators to predict the risk of MAFLD is shown in figure 2. The performance of these models is detailed in online supplemental table 1. The AUROCs of TyG and related parameters were greater than traditional indicators, including the HSI. The TyG-WC performed the highest AUROC (0.873, 95% CI 0.860 to 0.887, p<0.001), compared with TyG-BMI (0.862, 95% CI 0.847 to 0.876, p<0.001), TyG-WHR (0.836, 95% CI 0.820 to 0.852, p<0.001). Based on the results of NRI, it can be seen that the accuracy of TyG-WC, TyG-BMI and TyG-WHR were improved by 26.4%, 18.7% and 12.5%, respectively, compared with TyG (all p<0.001). Moreover, the IDI values of TyG-WC, TyG-BMI and TyG-WHR were 0.148, 0.125 and 0.071, respectively, which were all greater than 0, indicating that the diagnostic ability of the TyG-related parameters improved compared with the TyG index alone. The related results are shown in online supplemental table 2.
Figure 2.
Receiver operating characteristic curves of triglyceride–glucose (TyG) and its related parameters and biochemical indexes. AUC, areas under the curve; BMI, body mass index; FLI, fatty liver index; HSI, hepatic steatosis index; WC, waist circumference; WHR, waist-to-hip ratio.
bmjopen-2023-075413supp001.pdf (104.5KB, pdf)
Discussion
In this cross-sectional study, different parameters were tested to predict the presence of MAFLD. The results showed that the TyG index and its associated parameters were independent predictors of MAFLD. Advanced results of ROC curve analysis showed that TyG-BMI, TyG-WC and TyG-WHR, especially TyG-WC, had better diagnostic values than the TyG index alone in diagnosing MAFLD.
Previous studies have shown that factors such as obesity and metabolic disorders contribute to the onset and progression of MAFLD.29 Simple measures such as BMI, WC and FLI have been independently correlated with MAFLD.30–32 These findings were validated in the present study. BMI, WC and FLI were better predictors of MAFLD than TC, TG and FPG. The TyG index is a combination of FPG and TG. Some studies have reported that this index can be used as a surrogate marker for IR and effectively identify MAFLD,21 further confirmed by our findings. The present study’s analysis revealed that the AUC of the TyG index for predicting MAFLD was up to 0.793. It has been well documented that the TyG index is a reliable indicator of IR.33 IR induces an imbalance in glucose metabolism, leading to hyperglycaemia, which triggers inflammation and oxidative stress.34 It has been proven that oxidative stress and chronic inflammation are associated with the development of MAFLD.35 In addition, previous studies have shown that IR leads to high intrahepatic TGs by stimulating hepatic de novo lipogenesis and hepatic gluconeogenesis, among others. Activated hepatic gluconeogenesis also increases blood glucose levels.36 High intrahepatic TGs and fasting blood glucose are the distinguishing features of diagnostic MAFLD pairs. Therefore, using the TyG index as a valid diagnostic indicator of MAFLD is logical.
The TyG index-related parameter combines the TyG index with WC, BMI and WHR. It has been shown that TyG index-related parameters are the best predictors of IR compared with visceral obesity indicators and adipokines,37 consistent with the results of the present study. Previous studies have shown that FLI and HSI have strong diagnostic abilities for MAFLD.38 In the present study, the area under the ROC curve of the TyG-WC index for diagnosing MAFLD was greater than that of FLI and HSI, and it was more effective in diagnosing MAFLD. The ideal non-invasive test should be simple, easy to use, economical, efficient and convenient for detecting and identifying people at risk for MAFLD. Although the TyG index and its associated parameters do not differ significantly from the diagnostic performance of the FLI, the TyG index and its related parameters provide a better balance of the above requirements. Also, among the TyG-related parameters, TyG-WC had a stronger diagnostic performance than TyG-BMI, TyG-WC and TyG-WHR. The most probable explanation for the appearance of this phenomenon is that hepatic steatosis correlates with BMI but correlates more strongly with visceral fat (as measured by WC) because the lipid activity of visceral adipose tissue is higher than that of subcutaneous fat, on a per unit weight basis.39 The findings of Khamseh et al are consistent with ours.40 The AUROC for the TyG index, TyG-BMI and TyG-WC were 0.676, 0.675 and 0.693, respectively, lower than those derived in the present study. This discrepancy may be attributed to the small number of overweight/obese participants in their study. TyG and its related parameters were found to be effective in diagnosing MAFLD in a cross-sectional study using the NHANES (National Health and Nutrition Examination Survey) database to include 1727 adults, and the diagnostic value was superior to other predictors of MAFLD.41
The strengths of this study are the large sample size, rigorous screening criteria and application of the most recent standardised diagnostic criteria for defining MAFLD. However, there are some limitations to this study. First, this was a cross-sectional study, and causality could not be established. Second, self-reported dietary habits and other data are inevitably subject to measurement error. However, because all participants and researchers in this study were blinded to the results of abdominal ultrasonography and blood tests, the absence of differential reporting bias may have weakened our observed associations. Third, unmeasured confounders are also possible in an observational study, even if we consider all potential confounders. In addition, our sample was limited to Chinese adults, and it is unclear whether the findings apply to other populations.
Conclusions
Our study demonstrated that the TyG index effectively identifies MAFLD, and the TyG-related parameters improved the identification and diagnosis of MAFLD. As an inexpensive and convenient index, TyG and its related parameters, especially TyG-WC, maybe a useful marker for identifying MAFLD.
Supplementary Material
Acknowledgments
We want to express our gratitude to all participants for their cooperation and to all staff for recruiting subjects and their technical assistance.
Footnotes
RY, WX and HP contributed equally.
Contributors: X-EP designed the study. RY, WX, HP, LL and SY collected the data. RY analysed the data. RY, WX, HP and LL contributed to interpreting the results. RY, WX and HP drafted the manuscript. X-EP, SX and ZH revised the manuscript. All authors have discussed the results and commented on the manuscript. All authors read and approved the final manuscript. X-EP acts as a guarantor responsible for the overall content.
Funding: This work was supported by the National Natural Science Foundation of China (No. 81473047), the Natural Science Foundation of Fujian Province (No. 2019J01316) and the Natural Science Foundation of Fujian Province (No. 2023J01628).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Data are stored in the Department of Epidemiology and Health Statistics, Fujian Provincial Key Laboratory of Environment Factors and Cancer, School of Public Health, Fujian Medical University, Fujian, China. Data are available upon request from Xian-E Peng; Email address: fmuxe@163.com.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki (6th revision, 2008) and was approved by Ethics Committee of Fujian Medical University (ethics number 2014096). Participants gave informed consent to participate in the study before taking part.
References
- 1.Eslam M, Valenti L, Romeo S. Genetics and epigenetics of NAFLD and NASH: clinical impact. J Hepatol 2018;68:268–79. 10.1016/j.jhep.2017.09.003 [DOI] [PubMed] [Google Scholar]
- 2.Papatheodoridi M, Cholongitas E. Diagnosis of non-alcoholic fatty liver disease (NAFLD): current concepts. Curr Pharm Des 2018;24:4574–86. 10.2174/1381612825666190117102111 [DOI] [PubMed] [Google Scholar]
- 3.Eslam M, Newsome PN, Sarin SK, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol 2020;73:202–9. 10.1016/j.jhep.2020.03.039 [DOI] [PubMed] [Google Scholar]
- 4.Liao X, Ma Q, Wu T, et al. Lipid-lowering responses to dyslipidemia determine the efficacy on liver enzymes in metabolic dysfunction-associated fatty liver disease with hepatic injuries: a prospective cohort study. Diabetes Metab Syndr Obes 2022;15:1173–84. 10.2147/DMSO.S356371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Su W, Chen M, Xiao L, et al. Association of metabolic dysfunction-associated fatty liver disease, type 2 diabetes mellitus, and metabolic goal achievement with risk of chronic kidney disease. Front Public Health 2022;10:1047794. 10.3389/fpubh.2022.1047794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang X, Liu X, He P, et al. The imbalance of mitochondrial homeostasis of peripheral blood-derived macrophages mediated by MAFLD may impair the walking ability of elderly patients with osteopenia. Oxid Med Cell Longev 2022;2022:5210870. 10.1155/2022/5210870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Foghsgaard S, Andreasen C, Vedtofte L, et al. Non-alcoholic fatty liver disease is prevalent in women with prior gestational diabetes mellitus and independently associated with insulin resistance and waist circumference. Diabetes Care 2017;40:109–16. 10.2337/dc16-1017 [DOI] [PubMed] [Google Scholar]
- 8.Sasso M, Miette V, Sandrin L, et al. The controlled Attenuation parameter (CAP): a novel tool for the noninvasive evaluation of steatosis using fibroscan. Clin Res Hepatol Gastroenterol 2012;36:13–20. 10.1016/j.clinre.2011.08.001 [DOI] [PubMed] [Google Scholar]
- 9.Rinella ME, Sanyal AJ. Management of NAFLD: a stage-based approach. Nat Rev Gastroenterol Hepatol 2016;13:196–205. 10.1038/nrgastro.2016.3 [DOI] [PubMed] [Google Scholar]
- 10.El-Agroudy NN, Kurzbach A, Rodionov RN, et al. Are lifestyle therapies effective for NAFLD treatment? Trends Endocrinol Metab 2019;30:701–9. 10.1016/j.tem.2019.07.013 [DOI] [PubMed] [Google Scholar]
- 11.Yong HY, Larrouy-Maumus G, Zloh M, et al. Early detection of metabolic changes in drug-induced steatosis using metabolomics approaches. RSC Adv 2020;10:41047–57. 10.1039/d0ra06577c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Castera L, Friedrich-Rust M, Loomba R. Noninvasive assessment of liver disease in patients with nonalcoholic fatty liver disease. Gastroenterology 2019;156:1264–81. 10.1053/j.gastro.2018.12.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou JH, Cai JJ, She ZG, et al. Noninvasive evaluation of non-alcoholic fatty liver disease: current evidence and practice. World J Gastroenterol 2019;25:1307–26. 10.3748/wjg.v25.i11.1307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang J, Qi Y, Xin Z, et al. Isotemporal substitution of different behaviour patterns with the presence of MAFLD in Chinese adults. Liver Int 2022;42:2683–95. 10.1111/liv.15439 [DOI] [PubMed] [Google Scholar]
- 15.Li H, Zhang Y, Luo H, et al. The lipid accumulation product is a powerful tool to diagnose metabolic dysfunction-associated fatty liver disease in the United States adults. Front Endocrinol 2022;13:977625. 10.3389/fendo.2022.977625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pan X, Xie X, Peng H, et al. Risk prediction for non-alcoholic fatty liver disease based on biochemical and dietary variables in a Chinese Han population. Front Public Health 2020;8:220. 10.3389/fpubh.2020.00220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ding Y-S, Guo S-X, Ma R-L, et al. Association of metabolic syndrome with the adiponectin to homeostasis model assessment of insulin resistance ratio. Mediators Inflamm 2015;2015:607364. 10.1155/2015/607364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Han M, Wang H, Yang S, et al. Triglyceride glucose index and atherogenic index of plasma for predicting colorectal neoplasms in patients without cardiovascular diseases. Front Oncol 2022;12:1031259. 10.3389/fonc.2022.1031259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Luo E, Wang D, Yan G, et al. High triglyceride-glucose index is associated with poor prognosis in patients with acute ST-elevation myocardial infarction after percutaneous coronary intervention. Cardiovasc Diabetol 2019;18:150. 10.1186/s12933-019-0957-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alizargar J, Bai C-H, Hsieh N-C, et al. Use of the triglyceride-glucose index (Tyg) in cardiovascular disease patients. Cardiovasc Diabetol 2020;19:8. 10.1186/s12933-019-0982-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang R, Guan Q, Zhang M, et al. Association between triglyceride-glucose index and risk of metabolic dysfunction-associated fatty liver disease: a cohort study. Diabetes Metab Syndr Obes 2022;15:3167–79. 10.2147/DMSO.S383907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang J, Yan S, Cui Y, et al. The diagnostic and prognostic value of the Triglyceride-glucose index in metabolic dysfunction-associated fatty liver disease (MAFLD): a systematic review and meta-analysis. Nutrients 2022;14:4969. 10.3390/nu14234969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peng H, Pan L, Ran S, et al. Prediction of MAFLD and NAFLD using different screening indexes: a cross-sectional study in U.S. Front Endocrinol (Lausanne) 2023;14:1083032. 10.3389/fendo.2023.1083032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peng H, Xie X, Pan X, et al. Association of meat consumption with NAFLD risk and liver-related biochemical indexes in older Chinese: a cross-sectional study. BMC Gastroenterol 2021;21:221. 10.1186/s12876-021-01688-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xiane Peng ZH, Lin J, Lu Q, et al. Analysis of the prevalence and influencing factors of non-alcoholic fatty liver disease in staff. China Public Health 2009;25:1235–7. [Google Scholar]
- 26.Er L-K, Wu S, Chou H-H, et al. Triglyceride glucose-body mass index is a simple and clinically useful surrogate marker for insulin resistance in nondiabetic individuals. PLoS One 2016;11:e0149731. 10.1371/journal.pone.0149731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Koh SM, Chung SH, Yum YJ, et al. Comparison of the effects of triglyceride variability and exposure estimate on clinical prognosis in diabetic patients. Cardiovasc Diabetol 2022;21:245. 10.1186/s12933-022-01681-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mei Y-X, Zhang Z-X, Wu H, et al. Health-related quality of life and its related factors in survivors of stroke in rural China: a large-scale cross-sectional study. Front Public Health 2022;10:810185. 10.3389/fpubh.2022.810185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ijuin S, Oda K, Mawatari S, et al. Serine palmitoyltransferase long chain subunit 3 is associated with hepatocellular carcinoma in patients with NAFLD. Mol Clin Oncol 2022;16:55. 10.3892/mco.2021.2488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li H, Guo M, An Z, et al. Prevalence and risk factors of metabolic associated fatty liver disease in Xinxiang, China. IJERPH 2020;17:1818. 10.3390/ijerph17061818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang H, Zhang Y, Liu Y, et al. Comparison between traditional and new obesity measurement index for screening metabolic associated fatty liver disease. Front Endocrinol 2023;14:1163682. 10.3389/fendo.2023.1163682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Qu J, Dou J, Wang A, et al. Fatty liver index for hyperuricemia diagnosis: a community-based cohort study. BMC Endocr Disord 2022;22:114. 10.1186/s12902-022-01030-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li T, Yang C, Yang J, et al. Elevated triglyceride-glucose index predicts mortality following endovascular abdominal aortic aneurysm repair. Front Nutr 2023;10:1116425. 10.3389/fnut.2023.1116425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tao LC, Xu JN, Wang TT, et al. Triglyceride-glucose index as a marker in cardiovascular diseases: landscape and limitations. Cardiovasc Diabetol 2022;21:68. 10.1186/s12933-022-01511-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xing Y, Chen J, Liu J, et al. Associations between GGT/HDL and MAFLD: a cross-sectional study. DMSO 2022;Volume 15:383–94. 10.2147/DMSO.S342505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van Son KC, Verschuren L, Hanemaaijer R, et al. Non-parenchymal cells and the extracellular matrix in hepatocellular carcinoma in non-alcoholic fatty liver disease. Cancers (Basel) 2023;15:1308. 10.3390/cancers15041308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sheng G, Lu S, Xie Q, et al. The usefulness of obesity and lipid-related indices to predict the presence of non-alcoholic fatty liver disease. Lipids Health Dis 2021;20:134. 10.1186/s12944-021-01561-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Okada A, Yamada G, Kimura T, et al. Diagnostic ability using fatty liver and metabolic markers for metabolic-associated fatty liver disease stratified by metabolic/glycemic abnormalities. J Diabetes Investig 2023;14:463–78. 10.1111/jdi.13966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gruzdeva O, Borodkina D, Uchasova E, et al. Localization of fat depots and cardiovascular risk. Lipids Health Dis 2018;17:218. 10.1186/s12944-018-0856-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Khamseh ME, Malek M, Abbasi R, et al. Triglyceride glucose index and related parameters (Triglyceride glucose-body mass index and Triglyceride glucose-waist circumference) identify non-alcoholic fatty liver and liver fibrosis in individuals with overweight/obesity. Metab Syndr Relat Disord 2021;19:167–73. 10.1089/met.2020.0109 [DOI] [PubMed] [Google Scholar]
- 41.Xue Y, Xu J, Li M, et al. Potential screening indicators for early diagnosis of NAFLD/MAFLD and liver fibrosis: triglyceride glucose index-related parameters. Front Endocrinol (Lausanne) 2022;13:951689. 10.3389/fendo.2022.951689 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-075413supp001.pdf (104.5KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Data are stored in the Department of Epidemiology and Health Statistics, Fujian Provincial Key Laboratory of Environment Factors and Cancer, School of Public Health, Fujian Medical University, Fujian, China. Data are available upon request from Xian-E Peng; Email address: fmuxe@163.com.