Abstract
Multidrug resistance (MDR) seriously limits the clinical application of chemotherapy. A mechanism underlying MDR is the overexpression of efflux transporters associated with chemotherapeutic drugs. P-glycoprotein (P-gp) is an ATP-binding cassette (ABC) transporter, which promotes MDR by pumping out chemotherapeutic drugs and reducing their intracellular concentration. To date, overexpression of P-gp has been detected in various types of chemoresistant cancer and inhibiting P-gp-related MDR has been suggested. The present review summarizes the mechanisms underlying MDR mediated by P-gp in different tumors and evaluated the related signaling pathways, with the aim of improving understanding of the current status of P-gp-mediated chemotherapeutic resistance. This review focuses on the main mechanisms of inhibiting P-gp-mediated MDR, with the aim of providing a reference for the study of reversing P-gp-mediated MDR. The first mechanism involves decreasing the efflux activity of P-gp by altering its conformation or hindering P-gp-chemotherapeutic drug binding. The second inhibitory mechanism involves inhibiting P-gp expression to reduce efflux. The third inhibitory mechanism involves knocking out the ABCB1 gene. Potential strategies that can inhibit P-gp include certain natural products, synthetic compounds and biological techniques. It is important to screen lead compounds or candidate techniques for P-gp inhibition, and to identify inhibitors by targeting the relevant signaling pathways to overcome P-gp-mediated MDR.
Keywords: multidrug resistance, P-glycoprotein, tumor, chemotherapy, mechanisms
1. Introduction
With the development of medical science and technology, the diagnostic efficiency and treatment of cancer has markedly improved. There are three main types of systemic cancer treatments: Chemotherapy, targeted therapy and immunotherapy (1,2). There are notable individual differences in the therapeutic effects of targeted therapy and immunotherapy. Chemotherapy, which kills tumor cells indiscriminately, is considered an irreplaceable cancer treatment. Unfortunately, tumor multidrug resistance (MDR), resulting in the lack of tumor sensitivity to a number of chemotherapy drugs, is an obstacle limiting chemotherapy application (3). The mechanisms underlying MDR include ATP-binding cassette (ABC) transporter overexpression, autophagy, DNA damage repair, cancer stem cells, genetic mutations and DNA methylation (4-8). Overexpressed ABC transporters, which are the main cause of chemotherapy MDR, use the energy generated by ATP hydrolysis to pump chemotherapy drugs out of the cell (9). MDR-related ABC transporters include P-glycoprotein (P-gp), breast cancer resistance protein (BCRP), multidrug resistance-associated protein (MRP) and lung resistance-associated protein (LRP). P-gp is the main cause of MDR in tumors according to numerous studies (10,11).
P-gp was the first drug resistance-related protein to be discovered. In 1976, P-gp was identified in drug-resistant Chinese hamster ovary cells as a membrane glycoprotein with a molecular weight of ~170 kDa (12). P-gp, encoded by the ABCB1 gene, is the most studied transmembrane transporter in the ABC transporter family. The structure of P-gp consists of two nucleotide-binding domains (NBDs) and two transmembrane domains (TMDs) (13). NBDs are located in the cytoplasm and transfer energy through membranes to transport substrates. TMDs consist of six transmembrane α-helical structures that provide specificity for substrates. Chemotherapy drugs that act as P-gp substrates are pumped out of tumor cells (14,15).
P-gp has been reported to be overexpressed in various tumors, such as osteosarcoma, hepatocellular carcinoma (HCC) (16), breast cancer (17), gastric cancer (18), lung cancer (19,20) and bowel cancer (21), resulting in chemotherapy resistance. P-gp overexpression reduces intracellular drug concentrations and cytotoxicity by using its efflux pump function to expel cisplatin (20), paclitaxel (22), 5-fluorouracil (5-Fu) (23), doxorubicin (DOX) (24) and other chemotherapeutic drugs out of cells, which results in inadequate proliferation-inhibiting effects of chemotherapy drugs on tumor cells. In view of the common phenomenon of clinical chemotherapy resistance, a large number of studies have been carried out on the mechanism of P-gp-mediated chemotherapy resistance and P-gp inhibitors (25,26).
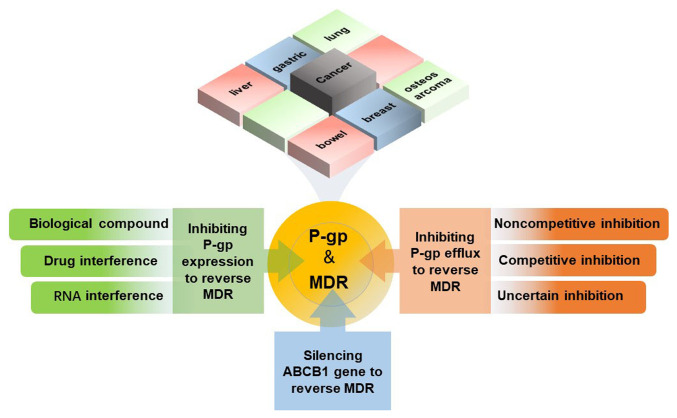
The present review aims to provide an overview of the overexpression of P-gp in different types of cancer leading to chemotherapy resistance (Fig. 1). This review summarizes and elaborates on three current strategies for overcoming P-gp-mediated chemotherapy resistance (Fig. 2). The first strategy involves competitive or noncompetitive suppression of the P-gp efflux pump function. The second strategy involves inhibition of the expression of P-gp and efflux transporters on the cell membrane that bind to chemotherapy drugs. The third approach involves knockout of the ABCB1 gene. The active substances that reverse P-gp-mediated chemotherapy resistance through these three pathways can also be classified into groups. They are roughly divided into natural products, synthetic compounds, endogenous RNAs and biological compounds. The present review aims to alert researchers to the important contribution of P-gp overexpression in chemotherapy resistance and to provide a reference for P-gp-related chemotherapy resistance research.
Figure 1.
Overexpression of P-gp in liver cancer, lung cancer, breast cancer, gastric cancer, bowel cancer and osteosarcoma results in resistance to multiple chemotherapies. There are three ways to reverse P-gp-mediated resistance to chemotherapies: i) Inhibiting the efflux function of P-gp; ii) inhibiting P-gp expression; iii) silencing MDR genes. MDR, multidrug resistance; P-gp, P-glycoprotein.
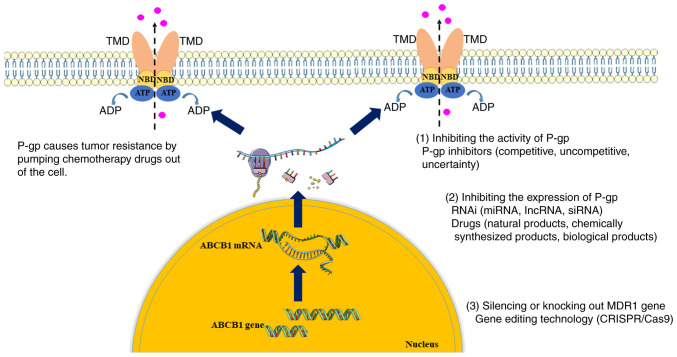
Figure 2.
Upregulation of P-gp pumps chemotherapeutic drugs out of cells, reducing the intracellular concentration of chemotherapeutic drugs and leading to chemotherapeutic drug resistance. There are three ways to reverse P-gp mediated chemotherapy resistance: (1) Inhibiting the activity of P-gp; (2) inhibiting the expression of P-gp; (3) silencing or knocking out the ABCB1 gene. These ways increase the concentration of intracellular chemotherapy drugs and reverses resistance to chemotherapy drugs. MDR, multidrug resistance; P-gp, P-glycoprotein; NBD, nucleotide-binding domains; TMD, transmembrane domain; RNAi, RNA interference; miRNA, microRNA; lncRNA, long non-coding RNA; siRNA, small interfering RNA.
2. MDR caused by P-gp in various tumor tissues
Before the advent of targeted therapy and immunotherapy, chemotherapy was the most common clinical treatment for a variety of malignant tumors; therefore, P-gp is a common mechanism underlying MDR in multiple malignant tumors. In general, ABC transporters, including P-gp, are expressed more highly in resistant tumors, which increases the chance of drug efflux. The high expression of P-gp in liver cancer, lung cancer, breast cancer, bowel cancer, gastric cancer and osteosarcoma leads to chemoresistance.
MDR caused by P-gp in liver cancer
Liver cancer is a type of malignant tumor that can be caused by alcoholism, drug injury and viral infection (27). Before sorafenib, a small-molecule targeted drug, was approved by the United States Food and Drug Administration for the treatment of advanced HCC, chemotherapy was the preferred treatment for unresectable liver cancer (28).
P-gp overexpression-mediated MDR is sometimes induced by external factors and not the spontaneous behavior of cancer cells following prolonged exposure to chemotherapy drugs. HepG2 cells are resistant to DOX in an acute or chronic hypoxic environment, and have high expression levels of nuclear factor erythroid-2 related factor 2 (Nrf2) and P-gp. It has been hypothesized that hypoxia can induce the expression of P-gp by inducing the expression of Nrf2 (29).
The regulatory mechanism of P-gp is a multimolecular process. In DOX-resistant liver cancer cells, the levels of NF-κB and P-gp are relatively high, thus indicating that the expression of NF-κB in HCC may be closely related to the ABCB1 gene (16). It has also been reported that the resistance of HCC to epirubicin is associated with the high expression of tripartite motif protein 25 (TRIM25). Epirubicin-resistant HCC cells in which TRIM25 was knocked down have been shown to exhibit increased sensitivity to epirubicin, an increased apoptosis rate and downregulation of P-gp (30). Furthermore, Bcl-2-associated transcription factor 1 can promote 5-Fu resistance, and the expression of P-gp and MRP1 in HCC cells by directly binding to the promoter region of long non-coding RNA (lncRNA) NEAT1 (31).
MDR caused by P-gp in lung cancer
Lung cancer is one of the most life-threatening types of cancer (27). P-gp-mediated cisplatin resistance is prominent in lung cancer. Metastasis-associated lung adenocarcinoma transcript 1 (MALAT1) was first found in non-small cell lung cancer (NSCLC). It has been reported that upregulated MALAT1 in A549 NSCLC cells promotes P-gp expression and P-gp-mediated cisplatin resistance by increasing signal transducer and activator of transcription 3 (STAT3) phosphorylation levels (32). In addition, it has been confirmed that the mRNA stability of ABCB1 and STAT3 phosphorylation in lung cancer cells can be enhanced by sodium butyrate (SB); therefore, it can be inferred that P-gp expression may be positively mediated by SB-induced expression or phosphorylation of STAT3 (33). Chloride channel-3 (ClC-3) promotes ABCB1 and P-gp expression by activating the NF-κB signaling pathway, and the key point of this process is the nuclear translocation of NF-κB P65 (19). Furthermore, upregulation of hypoxia-inducible factor (HIF) in NSCLC may lead to P-gp overexpression and promote cisplatin resistance (20); this result is similar to the mechanism of hypoxia-induced P-gp overexpression in liver cancer. Therefore, it may be suggested that modulating oxygen supply to tumors could overcome P-gp-mediated MDR.
MDR caused by P-gp in osteosarcoma
Osteosarcoma is a highly malignant tumor with a poor prognosis; however, chemotherapy before and after surgery can greatly improve this prognosis (34). Previous studies have confirmed that P-gp expression is positively associated with MDR in osteosarcoma (11,35). The expression levels of P-gp in cisplatin-resistant osteosarcoma cells have been shown to be much higher than those in nondrug-resistant cells. Furthermore, following knockdown of P-gp expression, the sensitivity of osteosarcoma cells to cisplatin was restored (11). Pleiotrophin (PTN), a neurotrophic growth factor, is linked to DOX resistance caused by P-gp overexpression. PTN can upregulate ABCB1/P-gp by mediating ALK/GSK3β/β-catenin signaling (35). LIM domain kinase 1 (LIMK1), a member of the serine/threonine protein kinase family, can also contribute to MDR by upregulating the levels of P-gp. This finding was demonstrated by transfecting MG63/VCR osteosarcoma cells with LIMK1-small interfering RNA (siRNA), wild-type-LIMK1 or empty vector; the apoptosis rate of cells transfected with LIMK1-siRNA was higher (36).
MDR caused by P-gp in breast cancer
P-gp is associated with drug resistance to a variety of anticancer drugs used in the treatment of breast cancer. At present, there are two types of breast cancer resistance mechanisms related to P-gp: Activation of the P-gp efflux pump and enhancement of P-gp expression.
The interaction of programmed cell death ligand 1 (PD-L1) and programmed cell death-1 (PD-1) on T cells can enhance chemotherapeutic resistance in breast cancer cells by inhibiting immune responses (37). Therefore, the regulation of MDR by the tumor immune microenvironment was investigated. From the perspective of tumor autoimmune regulation, P-gp-mediated MDR may be an immune response to exogenous chemotherapy drugs. Activation of multiple signaling pathways promotes P-gp expression and MDR in breast cancer. Notably, activating PI3K/AKT and MAPK/ERK pathways can increase the expression of ABCB1/P-gp and enhance DOX resistance (37). ABCB1 transcription can also be directly promoted by WW domain-binding protein 2 through binding to ERα, which is a potential mechanism of P-gp-related MDR (38). Nkx-2.5, a transcription factor, can bind to the +4 to +10 binding site of the upstream promoter of ABCB1 in breast cancer cells, thereby transactivating ABCB1 for transcription. Eventually, P-gp is upregulated, thus leading to breast cancer resistance (39). In addition to studies regarding the increased expression of P-gp, β1-integrin binding to collagen type 1 has been reported to induce chemoresistance of breast cancer cells by activating ABC efflux transporters (40).
Furthermore, resistance to trastuzumab emtansine, which is an antibody-conjugated drug used to treat metastatic breast cancer, is related to the upregulation of P-gp (41).
MDR caused by P-gp in gastric cancer
A number of studies on gastric cancer resistance have been conducted because of its high incidence (42,43). Notably, lncRNAs are closely related to the occurrence of P-gp-mediated gastric cancer resistance. The high expression of lncRNAs differentiation antagonizing non-protein coding RNA (DANCR) and gastric carcinoma proliferation enhancing transcript 1 (GHET1) in gastric cancer cells can increase the occurrence of drug resistance by upregulating the expression of ABCB1, which has been confirmed by silencing DANCR and GHET1 (44,45).
Zinc finger protein 139 inhibits the transcriptional activity of the microRNA (miRNA/miR)-185 promoter to downregulate miR-185, which also reduces the expression of ABCB1 (46). lncRNAs and miRNAs are non-coding RNAs transcribed from the genome that regulate epigenetics and signal transduction in vivo. Therefore, the involvement of lncRNAs and miRNAs in P-gp-mediated MDR is not surprising.
MDR caused by P-gp in bowel cancer
Chemotherapeutic resistance is also a vital obstacle in the clinical treatment of bowel cancer. Activation of the ABCB1 promoter region promotes P-gp expression and MDR. Visfatin regulates ABCB1 transcription by regulating ABCB1 promoter activity to mediate the DOX resistance of colorectal cancer cells. When transfected with visfatin-specific siRNA, the expression of ABCB1 in colorectal cancer cells was significantly reduced and the sensitivity to DOX was restored (47). ABCB1 mRNA and protein expression can be stimulated by forkhead box O3 through binding to the promoter region of ABCB1, and the proliferation of colon cancer cells and MDR can be induced by the overexpression of forkhead box O3 (48). In addition, IL-8 is significantly upregulated in DOX-resistant colorectal cancer cells. Notably, NF-κB (P65) may be activated by IL-8 via upregulation of IKKβ phosphorylation, thus resulting in overexpression of P-gp (49). P-gp expression can also be promoted by SET and MYND domain-containing protein 2 through the MEK/ERK/AP-1 signaling pathway, leading to the resistance of colon cancer to oxaliplatin (21). A relationship also exists between ABCB1 and adhesion G protein-coupled receptor G1 (GPR56), a type of adhesion G-protein coupled receptor. GPR56 can enhance drug resistance through upregulation of ABCB1 levels via a RhoA-mediated signaling mechanism in primary colon tumors (50).
3. Signaling pathways involved in P-gp mediated MDR
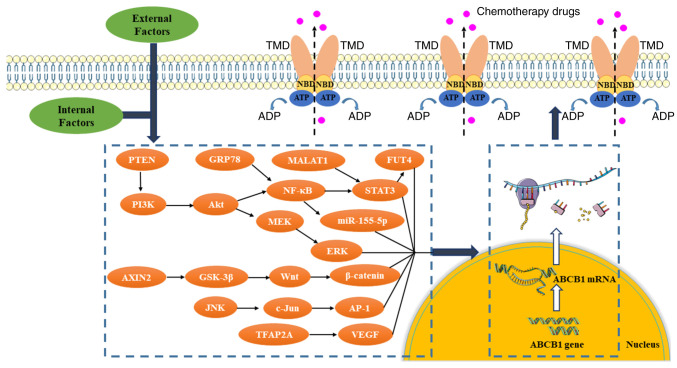
P-gp exerting its efflux pump function is the final step leading to chemotherapy MDR. Considering the large number of molecules in the body, P-gp-mediated MDR is likely to be regulated by a variety of signaling pathways (Fig. 3) P-gp overexpression mediates MDR in various types of cancer and the signaling pathways involved are similar. These pathways may seem intricate, but they all contain the same key molecule, NF-κB, which acts as a hub. Simultaneous overexpression of NF-κB and P-gp in drug-resistant tumors has prompted studies on the regulation of P-gp by NF-κB (51,52). The positive regulatory effect of NF-κB on P-gp has been verified by comprehensive analysis of the signaling pathway of P-gp inhibitors (16). It has been reported that NF-κB regulates P-gp through the downstream STAT3 signaling pathway and the regulation of NF-κB on P-gp is influenced by a number of upstream molecules in the body. N-acetyl-glucosaminyl transferase III can inhibit DOX resistance by negatively regulating P-gp expression through the TNFR2-NF/κB signaling pathway (53). Furthermore, melatonin inactivates the NF-κB pathway and downregulates P-gp, thus increasing sensitivity to epirubicin chemotherapy (54). By contrast, IL-8 positively regulates P-gp expression in DOX-resistant cells by activating the IKKβ/NF-κB signaling pathway (49). ClC-3 also increases ABCB1 mRNA and P-gp levels by activating the NF-κB signaling pathway (19).
Figure 3.
External and internal factors activate or inhibit some signaling pathways, thus upregulating P-gp expression and promoting chemotherapy drug resistance. MDR, multidrug resistance; P-gp, P-glycoprotein; NBD, nucleotide-binding domains; TMD, transmembrane domain.
Dysregulation of the PI3K/Akt signaling pathway, which is commonly seen in cancer, and regulates metabolism, proliferation, cell survival, growth and angiogenesis, has also been reported to serve an important role in regulating P-gp expression and MDR (55,56). Notably, activation of the PI3K/Akt pathway can upregulate P-gp in leukemia (56), ovarian cancer (51), liver cancer (57) and lung cancer (55). Compared with PI3K alone, the CDK6-PI3K signal axis synergistically regulates ABCB1 expression more strongly (25). Therefore, the idea of multipathway and multitarget synergistic inhibition of P-gp expression and efficient reversal of MDR was investigated. MEK/ERK is an important downstream signaling pathway of PI3K/Akt. Notably, the MEK/ERK signaling pathway positively regulates P-gp expression, and mediates resistance to DOX, paclitaxel, oxaliplatin, colchicine and vincristine (21,55). Wnt/β-catenin, which regulates the high expression of P-gp in colon cancer, HCC and leukaemia, is another major signaling pathway associated with P-gp-mediated MDR. Moreover, the MALAT1/STAT3/fucosyltransferase 4 (FUT4) (58), JNK/c-Jun/AP-1 (59) and PTN/β-catenin axes (60) are involved in regulating P-gp expression and mediating MDR.
In conclusion, the expression of P-gp is the result of the combined action of several signaling pathways. The discovery of these signaling pathways and regulatory molecules could clarify the role of P-gp and aid in identification of its inhibitors. These signaling pathways and regulatory molecules that promote P-gp expression and MDR can be used as potential targets to reverse chemotherapy resistance; however, no related inhibitors are currently used in clinical chemotherapy. In basic research, direct or indirect inhibition of a target can appropriately alleviate numerous drug resistance phenomena. The future application of these targeted inhibitors in clinical treatment may alleviate chemotherapy resistance and restore the therapeutic effect of chemotherapy drugs.
4. Reversing MDR by inhibiting P-gp
Inhibition of the efflux pump, which can be divided into noncompetitive inhibition and competitive inhibition according to the mechanism, is a direct way to solve MDR induced by P-gp.
Noncompetitive inhibition
Noncompetitive inhibition means that the inhibitor does not compete with the chemotherapeutic agent as a substrate for binding P-gp. There are a number of natural products (61-63) that have been reported as noncompetitive inhibitors of P-gp. Acetylshikonin and acetoxyisovalerylshikonin, which are shikonin derivatives, may be noncompetitive inhibitors of MDR-related transport proteins. They can inhibit ABCB1, BCRP and MRP2 independent of concentration to increase the accumulation of daunorubicin in carcinoma cells and chemotherapy sensitivity (62). Phytic acid, a natural phosphorylated inositol, can also noncompetitively suppress P-gp; this may be related to reduced P-gp ATPase activity and altered conformations of the P-gp molecule (61). A previous study reported that (±)-30-O, 40-O-dicynnamoyl-cis-kellactone, a derivative of (±)-praeruptorin A, noncompetitively inhibits P-gp-mediated DOX efflux by changing the conformation of P-gp and inhibiting ATPase activity (63).
Some synthetic substances can also be used as noncompetitive inhibitors to inhibit P-gp. Quaternized thiourea main-chain polymer, which is not a substrate for P-gp, has been shown to induce DNA damage and overcome P-gp-associated tumor MDR (64). The novel microtubule inhibitor 5-(4-ethoxyphenyl)-1-(3,4,5-trimethoxyphenyl)-1H-1,2,4-triazol-3-amine (YAN), which is not a substrate of P-gp, enhances the cytotoxicity of paclitaxel in NSCLC by decreasing the expression and efflux activity of P-gp (65).
It can be concluded from the aforementioned reports that noncompetitive inhibitors do not bind to the efflux substrate binding pockets of P-gp. However, they may combine with other domains of P-gp to affect its conformation. This principle is similar to the application of allosteric regulators that do not bind to the active site of target proteins to induce protein conformational changes.
Competitive inhibition
Competitive inhibitors binding to P-gp hinder P-gp-drug binding and P-gp-mediated efflux pathways. This method of replacing the drug with another substance as the target of efflux significantly increases the intracellular concentration of the drug.
Small molecule targeted drugs branebrutinib (66), pyrazolo[3,4-d]pyrimidines (67), almonertinib (68) and ribociclib (69) may be potential inhibitors of P-gp. They can compete with P-gp while exerting their own tumor-killing effects, thereby improving chemotherapy sensitivity. This means that there is a dual antitumor effect of chemotherapy combined with targeted therapy. Almonertinib can bind to the TMD of P-gp, whereas ribociclib and branebrutinib interact with the substrate-binding site of P-gp.
As well as existing drugs, a number of natural products have also been shown to inhibit P-gp. Wilforine (14), betulin (70), betulinic acid (71) and lathyrane diterpenes (72), which are terpenoids, all competitively inhibit P-gp efflux activity and overcome MDR. Wilforine may bind to residues of P-gp, such as Leu884, Lys887, Thr176 and Asm172 (14). Betulin tightly binds to the TMD region of P-gp (70). Glabridin (73) and 5-hydroxy-7,8-dimethoxyflavanone (74), which are flavonoid compounds, have also been proven to competitively inhibit P-gp and to increase the accumulation of chemotherapy drugs. Notably, 5-hydroxy-7,8-dimethoxyflavanone may slightly change the conformation of P-gp. Min et al (75) proposed that emodin, which is an anthraquinone derivative, can competitively bind to the R site of P-gp to inhibit the efflux function of P-gp and reduce the resistance to DOX. Voacamine, an alkaloid, has been validated as a substrate of P-gp, which was revealed to competitively inhibit the P-gp-mediated export of paclitaxel in ovarian cancer (76). Due to the development of computer simulation techniques and protein structure prediction, precise binding sites of these substances to P-gp have been reported. For the exploration of competitive inhibitors of P-gp, there is a large library of active compounds in natural products. Compared with curcumin, the synthesized dimethyl curcumin pyrazole derivatives with N-p-phenylcarboxyamide substitution have higher binding affinity for P-gp and can effectively reverse MDR of chronic myeloid leukaemia to DOX (77). Further modification of natural products enhances the inhibition of P-gp while reducing side effects. This is a future direction for the study of natural products as lead compounds for P-gp inhibition.
The sensitivity of adrenocortical carcinoma to mitotane, DOX, etoposide, cisplatin and streptozotocin can be significantly enhanced by verapamil and tariquidar, which are known as competitive P-gp inhibitors and nontransporter P-gp inhibitors (78). DHW-221, a dual PI3K/mTOR inhibitor, has also been found to bind P-gp to competitively inhibit efflux function and downregulate P-gp (15). The triazolo[1,5-a]pyrimidine derivative WS-716 (79), some 1,4-substituted arylalkyl piperazine derivatives (80), pyrimidine aminobenzene derivatives (81), 5-phenylfuran derivatives characterized by alkyl-substituted phenols and 6,7-dimethoxy1,2,3,4-tetrahydroisoquinoline (82), and the 4-indolyl quinazoline derivative YS-370 (83) have been reported to be potential P-gp competitive inhibitors. They block substrate efflux only by binding to P-gp, but do not affect P-gp expression. The inhibitory activity of most synthetic compounds is an accidental discovery distinct from their initial pharmacological action. However, the initial pharmacological action on patients cannot be ignored as a potential side effect; this may hinder the use of existing drugs to inhibit P-gp.
At present, most recognized P-gp inhibitors are competitive inhibitors. High-affinity compounds that can be pumped out of the cell as P-gp substrates have the potential to reverse P-gp-associated MDR as competitive inhibitors. However, it is necessary to consider the physiological activity of these compounds on the body, which makes it difficult to use competitive inhibitors in clinical MDR. The application of computer aided simulation technology has significantly improved the screening efficiency of P-gp competitive inhibitors and provided the basis for protein conformation binding in biological experiments.
Uncertain inhibition
Aside from definite competitive and noncompetitive inhibitors, a number of substances that have not been demonstrated to inhibit the efflux activity of P-gp in a clear way can also increase the sensitivity to chemotherapy drugs in certain experiments. According to the source, inhibitors with uncertain mechanisms can be divided into chemically synthesized substances and natural products.
Although it has been reported that decitabine upregulates P-gp expression in resistant cells, it has been found that the drug sensitivity of hematomas and solid tumors with high P-gp expression could be restored by decitabine through activation of the MAPK signaling pathway and inhibition of the efflux pump activity of P-gp (84). Methoxypolyethylene glycol (MPEG)-glycine-quinidine conjugates, which couple MPEG to quinidine via a glycine linker, can also inhibit P-gp in resistant cancer cells (85), and enequidar, a gut-specific P-gp inhibitor, reduces DOX efflux by inhibiting P-gp activity (86).
There are more studies on natural P-gp inhibitors than synthetic P-gp inhibitors. Celastrol has two possible antitumor drug resistance targets, the sarcoplasmic/endoplasmic reticulum Ca2+ATPase (SERCA) pump and P-gp. The sensitivity to chemotherapy drugs can be increased by celastrol, which simultaneously inhibits SERCA to induce autophagy in resistant tumor cells and inhibits the efflux pump function of P-gp (87). Naringenin and dihydrokaempferol extracted from Pistacia integerrima can bind to the hydrophobic pocket of P-gp; therefore, naringenin and dihydrokaempferol may be used to reverse MDR by inhibiting the activity of P-gp (88). Moreover, it has been reported that Camellia sinensis non-fermentative extract Noviphenone can overcome Adriamycin resistance by inhibiting the activity of P-gp. instead of its expression levels (89). The sensitivity to DOX can be restored in paclitaxel-resistant HepG2 and DOX-resistant colon-26 cells without influencing P-gp expression when the cells were treated with the 50% ethanol extract of Azadirachta indica, thus it has been inferred that the 50% ethanol extract of A. indica can inhibit the activity of P-gp based on the accumulation of the substrate rhodamine 123 (Rh-123) (90).
Antibodies against ABCB1 seem to be the most direct and targeted way to inhibit the activity of ABCB1. Monoclonal antibody (mAb) ABCB1-modified chitosan nanoparticles loaded with gefitinib and the autophagy inhibitor chloroquine have been prepared to overcome acquired EGFR-TKI resistance. The binding of mAb-ABCB1 to receptor (P-gp) suppresses the efflux pump activity of ABCB1, leading to the accumulation of chemotherapeutics (91).
Compared with competitive and noncompetitive inhibitors, uncertain inhibitors can suppress the efflux activity of P-gp without clear mechanisms and are therefore not considered safe candidates. Studies have shown that these inhibitors do not affect the expression of P-gp. Understanding the mechanism of action of uncertain inhibitors is the key to promote their clinical application.
5. Reversing MDR by inhibiting P-gp expression
RNA interference
lncRNAs
lncRNAs are a class of noncoding RNAs that are involved in intracellular regulation, including the function of overcoming MDR caused by P-gp (Table I).
Table I.
Examples of RNA molecules reversing P-gp-related chemotherapy resistance.
| A, lncRNAs
| |||||
|---|---|---|---|---|---|
| First author, year | Substance | Tumor type | Corresponding drug | Anti-MDR mechanism | (Refs.) |
| Chen, 2020 | lncRNA-GAS5 | Breast cancer | Adriamycin | Regulating miR-221-3p/DKK2 axis and Wnt/β-catenin/ABCB1 pathway | (92) |
| Han, 2018 | lncRNA LUCAT1 | Osteosarcoma | Methotrexate | Regulating miR-200c/ABCB1 pathway | (93) |
| Kang, 2020 | lncCRNDE | Acute myeloid leukemia | Adriamycin | Inhibiting Wnt/β-catenin pathway and P-gp expression | (94) |
| Zou, 2019 | lncRNA LINC00152 | Ovarian cancer | Cisplatin | Inhibiting P-gp expression | (95) |
|
| |||||
| B, miRNAs | |||||
|
| |||||
| First author, year | Substance | Tumor type | Corresponding drug | Anti-MDR mechanism | (Refs.) |
|
| |||||
| Zou, 2017 | miR-495 | Ovarian cancer, gastric cancer | DOX, taxol | Inhibiting P-gp expression by binding to the 3′-UTR of ABCB1 | (96) |
| Zhao, 2017 | miR-491-3p | Hepatocellular Carcinoma | DOX, vinblastin | Inhibiting P-gp expression by binding to the 3′-UTR of ABCB1 | (97) |
| Deng, 2021 | hsa-miR-34a-5p | Gastric cancer | 5-Fu | Inhibiting expression of SIRT1 and P-gp by binding to the 3′-UTR of SIRT1 | (43) |
| Yi, 2019 | miR-381 | Breast cancer | Cisplatin | Directly inhibiting ABCB1 expression | (98) |
| Zheng, 2019 | miR-34a | Hepatocellular carcinoma | DOX | Possibly inhibiting P-gp expression by regulating p53 expression | (99) |
| Wei, 2020 | miR-451 | Bladder cancer | Adriamycin | Inhibiting P-gp expression | (100) |
| Kenworthy, 2018 | miR-149 | Mesothelioma | Taxane | Inhibiting P-gp expression | (101) |
| Cao, 2019 | miR-122 | Hepatocellular carcinoma | Oxaliplatin | inhibiting Wnt/β-catenin pathway and P-gp expression | (103) |
| Wang, 2022 | miR-200c | Gastric cancer | Vincristine | Inhibiting P-gp expression | (102) |
| Sousa, 2020 | miR-204-5p | Lung cancer | DOX | Unreported | (104) |
| Sousa, 2020 | miR-139-5p | Lung cancer | DOX | Unreported | (104) |
| Sousa, 2020 | miR-29c-5p | Lung cancer | DOX | Unreported | (104) |
| Sousa, 2020 | miR-551b-3p | Lung cancer | DOX | Unreported | (104) |
| Sousa, 2020 | miR-29b-2-5p | Lung cancer | DOX | Unreported | (104) |
| Sousa, 2020 | miR-204-3p | Lung cancer | DOX | Unreported | (104) |
| Xie, 2021 | miR-1246 | Leukemia | Adriamycin | Inhibiting AXIN2/GSK-3β/Wnt/β-catenin pathway and P-gp expression | (106) |
| Li, 2022 | miR-205 | Liver cancer | DOX | Regulating PTEN/PI3K/Akt pathway and P-gp expression | (24) |
| Shi, 2020 | miR-29a | Colon cancer | DOX | Regulating PTEN/PI3K/Akt pathway and P-gp expression | (105) |
|
| |||||
| C, siRNAs | |||||
|
| |||||
| First author, year | Substance | Tumor type | Corresponding drug | Anti-MDR mechanism | (Refs.) |
|
| |||||
| Peng, 2022 | si ABCB1 | Breast cancer | DOX | Silencing ABCB1 gene | (154) |
| Liu, 2022 | si ABCB1, siBcl-2 | Breast cancer | DOX | Silencing ABCB1 gene | (112) |
| Wu, 2021 | si ABCB1 | Ovarian cancer | Paclitaxel | Silencing ABCB1 gene | (113) |
P-gp, P-glycoprotein; lncRNA, long non-coding RNA; miRNA, microRNA; siRNA, small interfering RNA; MDR, multidrug resistance.
The overexpression of some lncRNAs can directly or indirectly inhibit P-gp-mediated MDR. lncRNA-GAS5 can directly bind to miR-221-3p and inhibit its expression, the downregulation of which inhibits Dickkopf-related protein (DKK)2 and then activates the Wnt/β-catenin signaling pathway; ultimately, P-gp expression is reduced in DOX-resistant breast cancer cells (92). In methotrexate-resistant osteosarcoma cells, miR-200c inhibition can upregulate the expression of lncRNA LUCAT1 and P-gp. Upregulation of lncRNA LUCAT1 promotes P-gp expression and P-gp-mediated MDR (93). Knockout of some lncRNAs can also reverse MDR. The expression of colorectal neoplasia differentially expressed (CRNDE) in drug-resistant acute myeloid leukemia cells is directly proportional to the expression of ABCB1 and the sensitivity to Adriamycin has been reported to be enhanced after lncRNA CRNDE knockout. These results may be related to the inhibition of Wnt/β-catenin pathway by lncRNA CRNDE knockout (94). Furthermore, the expression of ABCB1is reduced when lncRNA LINC00152 is knocked down, which can increase the chemosensitivity of epithelial ovarian cancer cells to cisplatin (95).
miRNAs
miRNAs are another type of non-coding RNA associated with tumors. These single-stranded RNA molecules can bind to mRNA to regulate gene expression. In recent years, the regulatory role of miRNAs in tumor resistance has gradually attracted attention (Table I).
miRNAs alleviate chemoresistance mainly by directly (96,97) or indirectly (43,60) downregulating P-gp in various types of cancer. It has been reported that miR-495 (96) and miR-491-3p (97) can bind to two sites on the 3′-untranslated region (UTR) of ABCB1 mRNA, thereby inhibiting the expression of ABCB1 and sensitizing cancer cells to chemotherapeutic drugs. The high expression of hsa-miR-34a-5p in gastric cancer cells can inhibit uracil resistance by directly binding to the 3′-UTR of sirtuin 1 (SIRT1), and downregulating SIRT1, P-gp and MRP1 (43).
Numerous studies have shown that the expression of miRNAs in cancer tissues is associated with the levels of P-gp. It has been reported that upregulation of miR-381 (98), miR-34a (99), miR-451 (100), miR-149 (101) and miR-495 (96) can significantly reduce P-gp expression, thereby enhancing the sensitivity of cancer tissues to chemotherapeutic drugs. A retrospective clinical study reported the negative association between miR-200c and the expression of P-gp in gastric cancer tissue. miR-200c overexpression and P-gp downregulation were shown to reverse MDR by increasing drug sensitivity and predicted a better prognosis in patients with gastric cancer (102). The overexpression of miR-122, which has been reported as a negative regulator, can also inhibit the Wnt/β-catenin signaling pathway and further suppress ABCB1 expression (103). A previous study revealed that there are a number of miRNAs (miR-204-5p, miR-139-5p, miR-29c-5p, miR-551b-3p, miR-29b-2-5p and miR-204-3p) that are specific to lung cancer cells with P-gp-mediated resistance and extracellular vesicles. These miRNAs are likely markers of MDR or key molecules that could be used to overcome P-gp-mediated MDR (104). It has also been reported that miR-205 (24) and miR-29a (105) significantly inhibit P-gp expression by upregulating protein tyrosine phosphatase, thereby enhancing the sensitivity of cancer tissues to DOX.
In addition to the association between the overexpression of miRNAs and the downregulation of P-gp, downregulation of certain miRNAs can also inhibit P-gp expression and MDR through complex signaling pathways. The chemoresistance of MDR leukaemia cells can be attenuated by the loss of miR-1246 via negatively regulating axis inhibition protein 2 and glycogen synthase kinase-3β to inactivate the Wnt/β-catenin pathway and suppress P-gp expression (106).
Several miRNAs that inhibit P-gp expression have been identified; however, the expression of P-gp is not the result of a single miRNA. Although miRNAs do not translate proteins, they are involved in regulating P-gp through a variety of signaling pathways.
siRNAs
siRNAs are short non-coding RNAs that can regulate gene expression in the body (107). siRNA-ABCB1 (si ABCB1) targets ABCB1 mRNA to form a double-stranded RNA and hinder the translation of ABCB1 mRNA, decreasing P-gp expression and enhancing chemotherapy sensitivity. Studies on si ABCB1 in tumor resistance have mainly focused on the effect of si ABCB1 delivered by different delivery systems in reversing MDR (108) and the therapeutic effect of siABCB1 in combination with different drugs (109-111).
There have been numerous research achievements regarding the delivery of siRNAs and other materials via nanoparticles or nanocarriers (109,112,113). Liu et al (112) prepared a targeted nanoplatform based on biodegradable boronic acid modified ε-polylysine to codeliver P-gp siRNA, Bcl-2 siRNA and DOX. In breast cancer, compared with P-gp siRNA, Bcl-2 siRNA and/or DOX alone, the combined application of P-gp siRNA, Bcl-2 siRNA and DOX supported by nanocarriers has a stronger antitumor effect and ABCB1 gene-silencing effect (112). Wang et al (109) designed a biomimetic lipid/dextran hybrid nanocarrier with a diameter of ~100 nm. In this nanocarrier, the anionic si ABCB1 and the hydrophobic drug paclitaxel were loaded into the cationic lipid shell and the hydrophobic internal core of the hybrid nanocarriers, respectively, in order to improve the effect of paclitaxel. In another previous study, a multifunctional polymeric nanoparticle called Py-TPE/siRNA@PMP was loaded with paclitaxel and si ABCB1; this nanoparticle drug delivery system has been shown to enhance chemotherapy sensitivity in ovarian cancer (113).
As well as nanoparticles, there are other types of drug delivery systems. An EphA10-mediated pH-sensitive lipoplex has been developed to codeliver ABCB1-targeting siABCB1 and DOX (114). In another study, a carrier-free system with MDR as the backbone, loaded with cisplatin and divalent copper was constructed to treat drug-resistant tumors (110).
Developments in the field of materials have improved the delivery of siRNAs in cells. The use of materials to deliver chemotherapeutic drugs and siRNA at the same time allows both agents to be of maximum benefit. If the modified material can be delivered to the target tumor, it will greatly attenuate the downregulation of P-gp in normal tissue and the side effects of chemotherapy.
Drugs that inhibit P-gp expression
Chemically synthesized products
In the process of exploring tumor MDR, a number of chemically synthesized products have been detected to inhibit tumor MDR. Studies conducted in recent years have shown that some anticancer and non-anticancer drugs can downregulate P-gp, enhance chemosensitivity and rescue tumor MDR.
According to a previous study, hypoxia increases HIF1α expression resulting in P-gp overexpression and NSCLC MDR. By contrast, the HIF1α inhibitor LW6 can attenuate cisplatin MDR by downregulating P-gp (20). A novel platinum complex can also effectively alleviate cisplatin resistance by inhibiting the expression of P-gp (115). Ribociclib, a CDK4/6 inhibitor, inhibits P-gp-mediated DOX resistance by downregulating the expression and efflux activity of P-gp (69). The small molecule targeted inhibitors sorafenib and apatinib also inhibit P-gp expression and MDR while inducing anticancer effects (116). The killing effect of these drugs may cause tumors to lose the self-protection mechanism of chemotherapy-induced P-gp overexpression.
LSS-11, a novel naphthalimide derivative-based topoisomerase inhibitor, may reduce paclitaxel resistance in A549 lung cancer cells through two different underlying pathways. One of the mechanisms is that it could hinder the binding of STAT3 to the ABCB1 promoters downregulating P-gp (117). A novel microtubule inhibitor, YAN, can inhibit the resistance of NSCLC to paclitaxel by inhibiting the expression of P-gp (65). BAY-1082439, a chemical molecule undergoing phase I clinical trials in patients with advanced cancer, can efficiently inhibit the expression of P-gp and BCRP by selectively inhibiting PI3K 110α and 110β, and slightly suppress the efflux effect of P-gp and BCRP (118). A tumor-targeted anticancer agent, FFCLB, covalently linked by the delocalized lipophilic cation FF and CLB, inhibits P-gp expression, thereby increasing the intracellular concentration and cytotoxicity of DOX (119).
According to the aforementioned results, a number of drugs or their derivatives used to treat other diseases can inhibit P-gp expression and reverse chemotherapy resistance. It may be hypothesized that there is an intersection between the signaling pathway these drugs originally interact with to treat disease and the signaling pathway that regulates P-gp expression. Although these drugs can overcome P-gp-mediated chemotherapy resistance, their originally discovered effects are not negligible. However, the combination of small molecule targeted drugs with inhibitory activity and chemotherapy drugs may play a dual role in cancer suppression.
Natural products
In the search for antitumor molecules to combat tumor resistance, screening of natural products may yield safer options than screening chemical compounds. To date, a variety of natural product-derived compounds (120) and plant extracts (121) have been shown to inhibit ABCB1 and reverse tumor MDR in vitro and in vivo. These research objects can be roughly divided into flavonoids, alkaloids, coumarins, saponins, lignans, phenolic acids and terpenes. The present review summarized these natural products that reverse tumor drug resistance by inhibiting ABCB1 expression (Table II).
Table II.
Examples of natural products reversing P-gp-related chemotherapy resistance.
| A, Flavonoids
| |||||
|---|---|---|---|---|---|
| First author, year | Substance | Tumor type | Corresponding drug | Anti-MDR mechanism | (Refs.) |
| Kong, 2020 | Hesperetin | Lung cancer | Cisplatin | Inhibiting NF-κB pathway and P-gp expression | (124) |
| Sui, 2021 | Cajanol | Ovarian cancer | Paclitaxel | Inhibiting PI3K/Akt/NF-κB pathway and P-gp expression | (51) |
| Qin, 2022 | Luteolin | Osteosarcoma | Cisplatin and DOX | Upregulate miR-384, inhibiting PTN/β-catenin axis and P-gp expression | (60) |
| Wang, 2018 | Icaritin | Osteosarcoma | DOX | Inhibiting P-gp expression | (127) |
| Satonaka, 2017 | (-)-Epigallocatechin-3-gallate | Liver cancer | DOX | Inhibiting PI3K/Akt and MEK/ERK pathway, P-gp expression | (57) |
| La, 2019 | (-)-Epigallocatechin gallate | Colorectal cancer | 5-Fu | Inhibiting GRP78/NF-κB/miR-155-5p/ABCB1 pathway and P-gp expression | (125) |
| Tang, 2017 | Epigallocatechin gallate | Gastric cancer | 5-Fu | Inhibiting TFAP2A/VEGF pathway and P-gp expression | (42) |
| Qian, 2019 | Glabridin | Breast cancer | Paclitaxel, DOX | Inhibiting P-gp expression and P-gp ATPase activity, competitively inhibiting the efflux activity of P-gp | (73) |
| Teng, 2021 | 5-Hydroxy-7,8-dimethoxyflavanone | Oral cavity carcinomas | Vincristine | Competitively inhibiting the efflux activity of P-gp | (74) |
|
| |||||
| B, Alkaloids | |||||
|
| |||||
| First author, year | Substance | Tumor type | Corresponding drug | Anti-MDR mechanism | (Refs.) |
|
| |||||
| Huang, 2017 | Cepharanthine | Ovarian cancer | Paclitaxel | Inhibiting PI3K/Akt pathway and P-gp expression | (132) |
| Zhou, 2017 | Cepharanthine | Esophageal squamous cell carcinoma | Cisplatin | Activating JNK/p53 pathway and inhibiting P-gp expression | (129) |
| Zhou, 2022 | Tetrandrine | Leukemia | Daunorubicin | Inhibiting the efflux activity and expression of P-gp | (130) |
| Qian, 2021 | Berberine | Breast cancer | DOX | Inhibiting the efflux activity and expression of P-gp | (131) |
| Liu, 2020 | Nuciferine | Lung cancer, bowel cancer | Paclitaxel, DOX, docetaxel, daunorubicin | Inhibiting PI3K/AKT/ERK pathway and activation of Nrf2 and HIF-1α, P-gp expression | (55) |
| Quarti, 2021 | Piperine | Leukemia | Vincristine | Inhibiting P-gp expression | (134) |
|
| |||||
| C, Coumarins | |||||
|
| |||||
| First author, year | Substance | Tumor type | Corresponding drug | Anti-MDR mechanism | (Refs.) |
|
| |||||
| Wang, 2011 | Archangelicin | Leukemia | DOX | Inhibiting the function and expression of P-gp | (135) |
| Wang, 2016 | Osthole | Leukemia | DOX | Inhibiting PI3K/Akt pathway and expression of P-gp | (56) |
| Shen, 2006 | (±)-30-O, 40-O-dicynnamoyl-cis-kellactone | Hepatocellular carcinoma, leukemia | DOX | Noncompetitively inhibiting the efflux activity of P-gp | (63) |
|
| |||||
| D, Saponins | |||||
|
| |||||
| First author, year | Substance | Tumor type | Corresponding drug | Anti-MDR mechanism | (Refs.) |
| Huang, 2012 | Astragaloside II | Hepatic cancer | 5-Fu | Inhibiting the efflux activity and expression of P-gp via phosphorylation of ERK1/2, p38 and JNK | (140) |
| Wang, 2017 | Astragaloside IV | Hepatic cancer | 5-Fu | Inhibiting JNK/c-Jun/AP-1 pathway and P-gp expression | (59) |
| Liu, 2018 | Ginsenoside Rh2 | Colorectal carcinoma | 5-Fu | Inhibiting P-gp expression | (142) |
| Liu, 2018 | 20(S)-ginsenoside Rg3 | Lung cancer | Cisplatin | Inhibiting P-gp expression | (143) |
|
| |||||
| E, Lignans | |||||
|
| |||||
| First author, year | Substance | Tumor type | Corresponding drug | Anti-MDR mechanism | (Refs.) |
|
| |||||
| Sadava, 2013 | Silibinin | Small cell lung carcinoma | Etoposide, DOX | Possibly inhibiting P-gp expression | (144) |
| Dobiasová, 2020 | Silibinin stereoisomer В | Ovarian cancer | DOX | Inhibiting P-gp expression and P-gp ATPase activity | (145) |
| Dobiasová, 2020 | 2,3-Dehydrosilibinin A | Ovarian cancer | DOX | Unreported | (145) |
| Zhang, 2018 | Schisandrin A | Breast cancer | DOX | Inhibiting the P-gp, NF-кВ and Stat3 pathway, and inhibiting P-gp expression | (146) |
|
| |||||
| E, Phenolic acids | |||||
|
| |||||
| First author, year | Substance | Tumor type | Corresponding drug | Anti-MDR mechanism | (Refs.) |
| Liao, 2020 | Rosmarinic acid | Non-small cell lung cancer | Cisplatin | Possibly activating JNK phosphorylation and inhibiting P-gp expression | (147) |
| Muthusamy, 2019 | Ferulic acid | Oral cavity carcinomas | DOX, vincristine | Inhibiting PI3K/Akt/NF-κB pathway and P-gp expression | (148) |
| Gao, 2021 | Curcumol | Colon cancer | 5-Fu | Inhibiting Wnt/β-catenin pathway and P-gp expression | (23) |
| Teng, 2020 | Caffeic acid | Oral cavity carcinomas | DOX | Competitively inhibiting efflux activity of P-gp | (155) |
|
| |||||
| F, Terpenes | |||||
|
| |||||
| First author, year | Substance | Tumor type | Corresponding drug | Anti-MDR mechanism | (Refs.) |
|
| |||||
| Oh, 2020 | Cordycepin | Bladder cancer | Cisplatin | Inhibiting PI3K pathway, ETS-1 phosphorylation and P-gp expression | (149) |
| Ma, 2020 | Asiaticoside | Hepatocellular carcinoma | DOX, paclitaxel, colchicine, vincristine | Inhibiting PI3K/Akt and MAPK/ERK pathway | (156) |
| Ding, 2022 | Alantolactone | Lung cancer | Paclitaxel | Inhibiting MALAT1/STAT3/FUT4 axis and P-gp expression | (58) |
| Ding, 2022 | Brevilin A | Lung cancer | Paclitaxel | Inhibiting MALAT1/STAT3/FUT4 axis and P-gp expression | (58) |
| Chang, 2020 | Wilforine | Cervical cancer | DOX | Competitively inhibiting the efflux activity of P-gp | (14) |
| Laiolo, 2021 | Betulin | Leukemia | DOX | Competitively inhibiting the efflux activity of P-gp | (70) |
| Liu, 2021 | Betulinic acid | Breast cancer | Adriamaycin, vincristine | Competitively inhibiting the efflux activity of P-gp | (71) |
| Yang, 2020 | Lathyrane diterpenes | Hepatocellular carcinoma | DOX | Competitively inhibiting the efflux activity of P-gp | (72) |
|
| |||||
| G, Quinones | |||||
|
| |||||
| First author, year | Substance | Tumor type | Corresponding drug | Anti-MDR mechanism | (Refs.) |
| Mirzaei, 2018 | Acetylshikonin | Breast cancer | Daunorubicin | Noncompetitively inhibiting the efflux activity of P-gp | (62) |
| Mirzaei, 2018 | Acetoxyisovalerylshikonin | Breast cancer | Daunorubicin | Noncompetitively inhibiting the efflux activity of P-gp | (62) |
P-gp, P-glycoprotein; MDR, multidrug resistance.
Flavonoids
Flavonoids are a class of plant metabolites with a 2-phenylchromone structure that exist widely in nature. A variety of flavonoids have been shown to have antitumor and anti-resistance activities (122). Different structures of flavonoids have different mechanisms of action and inhibitory activities (123).
The NF-κB signaling pathway is involved in the mechanism by which a variety of natural compound monomers inhibit P-gp expression. Hesperetin, a derivative of hesperidin that is extracted from tangerine peel, has been reported to inhibit tumor growth in vivo and to restore the sensitivity of A549 lung cancer cells to cisplatin by inhibiting the NF-κB signaling pathway and expression of P-gp (124). Cajanol, an isoflavone from pigeon pea, can inhibit the transcription and translation of P-gp through the PI3K/Akt/NF-κB pathway, and reverse the resistance of ovarian cancer cell lines to paclitaxel in vitro and in vivo (51). It has also been reported that P-gp expression and P-gp ATPase activity are suppressed by glabridin (73).
The regulation of P-gp expression by various natural products is related to miRNAs (60,125). Luteolin can enhance the sensitivity of osteosarcoma to cisplatin and DOX; it has been reported that luteolin can upregulate miR-384, which indirectly inhibits P-gp expression by negatively regulating the PTN/β-catenin axis (60).
Additionally, natural products that have been shown to inhibit P-gp expression also include epigallocatechin gallate (42), theaflavin, quercetin, rutin, epicatechin 3 gallate, tamarixetin (126) and icaritin (127).
Alkaloids
Salvia miltiorrhiza (128), cepharanthine hydrochloride (129), tetrandrine (130) and berberine (131) can inhibit the expression of P-gp to reverse tumor MDR. Cepharanthine hydrochloride can serve a role in reversing drug resistance in ovarian cancer via inhibiting the expression of ABCB1, and reducing the mRNA and protein expression levels of P-gp, which may be caused by inhibiting the PI3K/Akt signaling pathway (132). Tetrandrine (133), nuciferine (55) and berberine (131) have been reported to increase the intracellular aggregation of chemotherapeutic drugs via their dual inhibitory effects of inhibiting the efflux activity of P-gp and inhibiting the expression of P-gp. Tetrandrine and berberine are isoquinoline alkaloids. Notably, inhibition of P-gp expression by tetrandrine does not occur through the inhibition of ABCB1 transcription (133). Furthermore, inhibition of P-gp expression by nuciferine is regulated by a series of signaling pathways. Nuciferine can effectively inhibit the PI3K/AKT/ERK signaling pathway, and the activation of Nrf2 and HIF-1α, which can reduce P-gp expression and enhance MDR sensitivity in tumor cells (55). Additionally, the ability of piperine to overcome MDR in leukaemia cells may be related to downregulation of P-gp (134).
Coumarins
Coumarins are a class of aromatic compounds ubiquitous in nature with a benzopyrone structure. Some coumarins have been reported to overcome MDR by inhibiting the activity and expression of P-gp. A previous study revealed that archangelicin can inhibit the function and expression of P-gp, and ultimately reduce the resistance of the leukaemia cell line K562/A02 to DOX (135). Osthole has also been shown to inhibit the expression of P-gp by inhibiting the PI3K/Akt signaling pathway, which can be induced by the uptake and efflux of Rh-123 and the accumulation of DOX (56).
Saponins
Saponins, consisting of sapogenins and sugars, are mainly found in plants. There are a number of types and complex structures of saponins (136). Numerous saponins, including Paris saponin VII (137), ginsenoside Rb1 (138) and sodium aescinate (139), have been reported to inhibit the expression of P-gp and reverse tumor resistance. Astragaloside II has been found to increase the intracellular accumulation of P-gp substrates by inhibiting the efflux pump activity of P-gp. On the other hand, it can also inhibit the expression of ABCB1 and suppress the phosphorylation of ERK1/2, p38 and JNK; these functions facilitate its role in reversing tumor MDR (140). Wang et al (141) investigated astragaloside IV and verified that astragaloside IV can inhibit the expression of ABCB1, increase the intracellular accumulation of 5-Fu, and ultimately achieve the goal of inhibiting tumor resistance. In subsequent experiments, it was further confirmed that the specific mechanism by which astragaloside IV inhibits the expression of ABCB1 is by inhibiting the JNK/c-Jun/AP-1 signaling pathway (59). In addition, the activity of ginsenoside Rh2 in reversing tumor resistance may be related to its inhibition of P-gp expression. In a previous study, it was revealed that the expression levels of MRP1, ABCB1, LRP and glutathione S-transferase are negatively correlated with ginsenoside Rh2 (142). In addition to ginsenoside Rh2, 20(S)-ginsenoside Rg3 can also enhance the cytotoxicity of chemotherapy drugs by inhibiting the expression of drug resistance genes (143).
Lignans
Silibinin is considered to be the main bioactive component of silymarin. In a previous report, it was speculated that silibinin increased the chemosensitivity of small cell lung cancer by downregulating P-gp rather than inhibiting the efflux function of P-gp (144). However, in recent years, silibinin stereoisomer B and its derivative 2,3-dehydrosilibinin A have also been found to sensitize ovarian cancer cells to DOX, and silibinin stereoisomer B exhibits dual inhibition of P-gp ATPase activity and P-gp expression (145). Schisandrin A can also inhibit the expression of P-gp by reducing the levels of phosphorylated (p)-IκB-α (Ser32) and p-Stat3 (Tyr705). Combined with its blocking of P-gp efflux activity, it enhances the sensitivity of MDR breast cancer cells to DOX (146).
Phenolic acids
Rosmarinic acid reverses cisplatin resistance in NSCLC by activating MAPK and thereby inhibiting P-gp expression (147). Ferulic acid has also been reported to enhance the cytotoxicity of DOX and vincristine on MDR cells with high P-gp expression, which is dependent on the PI3K/Akt/NF-κB signaling pathway to inhibit P-gp expression (148). Curcumin has also been reported to downregulate the expression of P-gp (23).
Terpenes
Terpenoids are widely found in animals and plants, such as essential oils, resins, pigments, hormones and vitamins. Terpenoids have isoprene basic units in their structure. Cordycepin inhibits the expression of ABCB1, thereby enhancing the sensitivity of cisplatin-resistant bladder cancer cells to cisplatin. Cordycepin may inhibit the PI3K signaling pathway and thereby attenuate the phosphorylation of ETS-1 (Thr38), a transcription factor that can activate the ABCB1 promoter after phosphorylation. The reduction in ETS-1 (Thr38) phosphorylation hinders the transcription and expression of ABCB1, downregulates the expression of P-gp and reduces the resistance of bladder cancer cells (149). Alantolactone and brevilin A, which are sesquiterpene lactones, can inhibit the resistance of lung cancer cells to paclitaxel (58). The mechanism involves the inhibition of MALAT1 expression by alantolactone and brevilin A, the subsequent activation of STAT3 and the upregulation of FUT4, and ultimately the positive reduction of P-gp expression.
These natural products inhibit P-gp expression and reverse chemotherapy resistance by regulating the NF-κB/STAT3, PI3K/AKT, MEK/ERK and Wnt/β-catenin signaling pathways. These involved signaling pathways are consistent with those that promote P-gp-related chemotherapy resistance in different tumors. Furthermore, these results confirm that these signaling pathways are important and inhibitors targeting these signaling pathways should be studied.
Biological compounds
In addition to some of their own biological activities, a number of biological compounds in the human body, including proteins, enzymes, nucleic acids, hormones, antibodies and cytokines, have been proven to be effective in antitumor MDR.
Tumor necrosis factor α-induced protein 8-like 2 (TIPE2) is a tumor suppressor that is related to P-gp. P-gp can be inhibited by TIPE2 via inhibiting the TAK1-NF-κB-AP-1 signaling pathway, thus sensitizing osteosarcoma cells to cisplatin (52). It may be hypothesized that the overall inhibition of tumors by other targets may affect the expression of P-gp in tumors. This seems to confirm the win-win effect of chemotherapy in combination with other treatments. The NF-κB signaling pathway has an important role in regulating P-gp expression. Melatonin downregulates NF-κB/P65 expression in the nucleus and disrupts the binding of P65 to the ABCB1 promoter. Melatonin-mediated downregulation of P-gp expression increases the chemosensitivity of diffuse large B-cell lymphoma cells to epirubicin (54). Estrogen 2-methoxyestradiol can interact with cadmium in ovarian cancer to reduce P-gp expression as a potential MDR regulator (150). γ-Tocotrienol inhibits P-gp expression in breast cancer via the NF-κB signaling pathway (151). The impact of tumors on the body is systemic rather than local and the malignant progression of tumors is accompanied by changes in hormone levels. To overcome P-gp mediated MDR, systemic treatment, such as targeted therapy combined with chemotherapy and targeted therapy combined with immunotherapy, should be considered (1,2).
In addition to these endogenous substances, biologics used to inhibit P-gp in the body are also effective. It has been found that an adenovirus vector carrying DKK3 can augment the antitumor effect of temozolomide in glioblastoma cells by reducing the expression of P-gp, which is associated with inhibition of Akt/NF- (152).
Active substances in humans have better biosafety profiles than those derived from natural products or synthetic compounds. These biological compounds can regulate the expression of P-gp by inhibiting or activating certain signaling pathways and molecules. Therefore, regulation of P-gp expression and chemotherapy resistance can be affected by altering the expression levels or activities of these biological compounds in vivo and in vitro.
6. Reversing MDR by silencing ABCB1 DNA
The reversal of P-gp-mediated tumor MDR by inhibiting the activity and expression of P-gp has been introduced in the present review. If these two methods block the intermediate steps of P-gp-mediated tumor resistance, then directly knocking out or silencing the ABCB1 gene can completely inhibit P-gp expression and curb resistance.
CRISPR/Cas9 is an efficient and convenient gene editing technology. It can use single guide RNA (sgRNA) to identify target gene DNA and guide Cas9 endonuclease to cut DNA to achieve gene knockout. Three sgRNAs targeting the fourth and fifth exons of the human ABCB1 gene were designed by Norouzi-Barough et al (153). When all three Cas9-sgRNA plasmids were transfected into Adriamycin-resistant cells, the three sgRNAs bound to the target exons of ABCB1 inducing the Cas9 endonuclease to cut the target gene ABCB1. Finally, ABCB1 was knocked out. Low-level expression of P-gp was detected in the experiment, which verified that CRISPR/Cas9 technology successfully knocked down the ABCB1 gene. In addition, the increased sensitivity of ABCB1-knockdown cells to Adriamycin suggested that knocking out drug resistance genes through gene editing may be a new way to solve drug resistance (153). However, how to safely and effectively apply this to the clinical treatment of cancer is a difficult problem to be solved. The urgency of the problem is alleviated by the continual discovery of new drugs.
7. Conclusions and perspective
Chemotherapy drugs inhibit tumor cells by killing them indiscriminately and thus have cytotoxic effects on normal cells, leading to strong side effects. Targeted therapy and immunotherapy have fewer side effects and are emerging therapies for cancer. However, due to the difference in individual immune status, the therapeutic effect of immunotherapy differs significantly among individuals. Differences in the phenotype of targeted genes also limit the use of targeted therapy. Therefore, chemotherapy remains an irreplaceable therapy in cancer treatment.
P-gp upregulation in cancer leads to chemoresistance since P-gp pumps chemotherapeutic agents out of the cell. Multiple signaling pathways, including PI3K/AKT (25), MEK/ERK (21), Wnt/β-catenin and NF-κB/STAT3, promote the chemotherapy resistance of various tumor cells. The mechanism of P-gp upregulation is consistent in different tumors (16,20,37,49). Multiple signaling pathways, including PI3K/AKT (37), MEK/ERK (21), Wnt/β-catenin and NF-κB/STAT3, promote the chemotherapy resistance of various tumor cells. Notably, the consistent mechanisms in different tumors reduces the burden of exploring ways to overcome P-gp-mediated chemotherapeutic resistance in different tumors.
Currently, the pathways found to reverse P-gp mediated chemotherapeutic resistance can be divided into three categories: Inhibition of the efflux function of P-gp, inhibition of the expression of P-gp and knockdown of the ABCB1 gene. Competitive or noncompetitive inhibition of P-gp efflux function represents the most direct method. This class of inhibitors, which mainly includes natural products and synthetic compounds, impedes the binding of P-gp to chemotherapy drugs by binding to P-gp or changing the conformation of P-gp. Computer-aided simulation technology can be used to screen P-gp inhibitors. Downregulation of P-gp is the way in which most inhibitors act. The regulation of P-gp expression by natural products, synthetic compounds, RNA and biological compounds in humans involves a variety of mechanisms and molecular targets, such as the PI3K/AKT (51), MEK/ERK, Wnt/β-catenin and NF-κB/STAT3 (58) signaling pathways. Numerous small molecule targeted inhibitors not only exert antitumor effects, but also inhibit P-gp expression and MDR, reflecting the increased efficacy of the combination of targeted therapy and chemotherapy. However, compared with inhibition of signaling pathways, direct inhibition of the substrate-binding site and efflux activity of P-gp is more effective in theory. To some extent, some P-gp competitive and noncompetitive inhibitors act in a manner similar to allosteric regulation, regulating protein activity by changing the structure of the protein. At present, there is a complete and feasible development process for allosteric regulators of target proteins. Perhaps the research of P-gp efflux inhibitors can refer to the exploration of allosteric regulators.
In conclusion, the present review describes P-gp-mediated chemotherapeutic resistance and related mechanisms in various types of cancer to alert researchers to the importance of P-gp in chemotherapeutic resistance. It may be possible to explore the related mechanisms to overcome P-gp-mediated chemoresistance. In addition, the present review summarized the active substances that reverse P-gp-mediated chemotherapeutic resistance to provide candidate compounds for screening clinical P-gp inhibitors and lead compounds for the development of new P-gp inhibitors.
Acknowledgments
Not applicable.
Funding Statement
This work was supported by the National Major Scientific Research Instrument Development Project of NSFC (grant no. 21827812) and the Foundation and Advanced Research Project of CQ CSTC (grant nos. cstc2018jscx-mszd0280 and cstc2017shms-xdny0033).
Availability of data and materials
Not applicable.
Authors' contributions
YT and FX designed the article. YT, YL, YW and JL participated in the literature search. YT was the major contributor in writing the manuscript. FX and JW participated in manuscript revision. Data authentication is not applicable. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Xu T, Wang X, Xin Y, Wang Z, Gong J, Zhang X, Li Y, Ji C, Sun Y, Zhao F, et al. Trastuzumab combined with irinotecan in patients with HER2-positive metastatic colorectal cancer: A phase II single-arm study and exploratory biomarker analysis. Cancer Res Treat. 2023;55:626–635. doi: 10.4143/crt.2022.1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Torka P, Groman A, Wong J, Nichols J, Kader A, Mavis C, Anampa-Guzmán A, Sait SJ, Block A, Przespolewski E, et al. Carfilzomib combined with rituximab, ifosfamide, carboplatin, and etoposide for relapsed or refractory DLBCL. Blood Adv. 2023;7:1146–1155. doi: 10.1182/bloodadvances.2022008543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yin Q, Shen J, Zhang Z, Yu H, Li Y. Reversal of multidrug resistance by stimuli-responsive drug delivery systems for therapy of tumor. Adv Drug Deliv Rev. 2013;65:1699–1715. doi: 10.1016/j.addr.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 4.Ruan T, Liu W, Tao K, Wu C. A review of research progress in multidrug-resistance mechanisms in gastric cancer. Onco Targets Ther. 2020;13:1797–1807. doi: 10.2147/OTT.S239336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lu C, Wei Y, Wang X, Zhang Z, Yin J, Li W, Chen L, Lyu X, Shi Z, Yan W, You Y. DNA-methylation-mediated activating of lncRNA SNHG12 promotes temozolomide resistance in glioblastoma. Mol Cancer. 2020;19:28. doi: 10.1186/s12943-020-1137-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Galle E, Thienpont B, Cappuyns S, Venken T, Busschaert P, Van Haele M, Van Cutsem E, Roskams T, van Pelt J, Verslype C, et al. DNA methylation-driven EMT is a common mechanism of resistance to various therapeutic agents in cancer. Clin Epigenetics. 2020;12:27. doi: 10.1186/s13148-020-0821-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leon G, MacDonagh L, Finn SP, Cuffe S, Barr MP. Cancer stem cells in drug resistant lung cancer: Targeting cell surface markers and signaling pathways. Pharmacol Ther. 2016;158:71–90. doi: 10.1016/j.pharmthera.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 8.Vitale D, Kumar Katakam S, Greve B, Jang B, Oh ES, Alaniz L, Götte M. Proteoglycans and glycosaminoglycans as regulators of cancer stem cell function and therapeutic resistance. FEBS J. 2019;286:2870–2882. doi: 10.1111/febs.14967. [DOI] [PubMed] [Google Scholar]
- 9.Zhang H, Xu H, Ashby CR, Jr, Assaraf YG, Chen ZS, Liu HM. Chemical molecular-based approach to overcome multidrug resistance in cancer by targeting P-glycoprotein (P-gp) Med Res Rev. 2021;41:525–555. doi: 10.1002/med.21739. [DOI] [PubMed] [Google Scholar]
- 10.Briz O, Perez-Silva L, Al-Abdulla R, Abete L, Reviejo M, Romero MR, Marin JJG. What 'the cancer genome atlas' database tells us about the role of ATP-binding cassette (ABC) proteins in chemoresistance to anticancer drugs. Expert Opin Drug Metab Toxicol. 2019;15:577–593. doi: 10.1080/17425255.2019.1631285. [DOI] [PubMed] [Google Scholar]
- 11.He C, Sun Z, Hoffman RM, Yang Z, Jiang Y, Wang L, Hao Y. P-glycoprotein overexpression is associated with cisplatin resistance in human osteosarcoma. Anticancer Res. 2019;39:1711–1718. doi: 10.21873/anticanres.13277. [DOI] [PubMed] [Google Scholar]
- 12.Juliano RL, Ling V. A surface glycoprotein modulating drug permeability in Chinese hamster ovary cell mutants. Biochim Biophys Acta. 1976;455:152–162. doi: 10.1016/0005-2736(76)90160-7. [DOI] [PubMed] [Google Scholar]
- 13.Ibrahim MAA, Abdeljawaad KAA, Jaragh-Alhadad LA, Oraby HF, Atia MAM, Alzahrani OR, Mekhemer GAH, Moustafa MF, Shawky AM, Sidhom PA, Abdelrahman AHM. Potential drug candidates as P-glycoprotein inhibitors to reverse multidrug resistance in cancer: An in silico drug discovery study. J Biomol Struct Dyn. 2023:1–16. doi: 10.1080/07391102.2023.2176360. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 14.Chang YT, Lin YC, Sun L, Liao WC, Wang CCN, Chou CY, Morris-Natschke SL, Lee KH, Hung CC. Wilforine resensitizes multidrug resistant cancer cells via competitive inhibition of P-glycoprotein. Phytomedicine. 2020;71:153239. doi: 10.1016/j.phymed.2020.153239. [DOI] [PubMed] [Google Scholar]
- 15.Liu M, Xu C, Qin X, Liu W, Li D, Jia H, Gao X, Wu Y, Wu Q, Xu X, et al. DHW-221, a dual PI3K/mTOR inhibitor, overcomes multidrug resistance by targeting P-glycoprotein (P-gp/ABCB1) and Akt-mediated FOXO3a nuclear translocation in non-small cell lung cancer. Front Oncol. 2022;12:873649. doi: 10.3389/fonc.2022.873649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu T, Wei R, Zhang Y, Chen W, Liu H. Association between NF-κB expression and drug resistance of liver cancer. Oncol Lett. 2019;17:1030–1034. doi: 10.3892/ol.2018.9640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu Y, Cao F, Xia F, Li J, Dong X, Guo Y, Zhang J, Zhao Q, Liu Y. Shc3 facilitates breast cancer drug resistance by interacting with ErbB2 to initiate ErbB2/COX2/MDR1 axis. Cancer Med. 2023;12:10768–10780. doi: 10.1002/cam4.5768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jeddi F, Soozangar N, Sadeghi MR, Somi MH, Shirmohamadi M, Eftekhar-Sadat AT, Samadi N. Nrf2 overexpression is associated with P-glycoprotein upregulation in gastric cancer. Biomed Pharmacother. 2018;97:286–292. doi: 10.1016/j.biopha.2017.10.129. [DOI] [PubMed] [Google Scholar]
- 19.Chen Q, Liu X, Luo Z, Wang S, Lin J, Xie Z, Li M, Li C, Cao H, Huang Q, et al. Chloride channel-3 mediates multidrug resistance of cancer by upregulating P-glycoprotein expression. J Cell Physiol. 2019;234:6611–6623. doi: 10.1002/jcp.27402. [DOI] [PubMed] [Google Scholar]
- 20.Mai L, Luo M, Wu JJ, Yang JH, Hong LY. The combination therapy of HIF1α inhibitor LW6 and cisplatin plays an effective role on anti-tumor function in A549 cells. Neoplasma. 2019;66:776–784. doi: 10.4149/neo_2018_180921N708. [DOI] [PubMed] [Google Scholar]
- 21.Ren H, Wang Z, Chen Y, Liu Y, Zhang S, Zhang T, Li Y. SMYD2-OE promotes oxaliplatin resistance in colon cancer through MDR1/P-glycoprotein via MEK/ERK/AP1 pathway. Onco Targets Ther. 2019;12:2585–2594. doi: 10.2147/OTT.S186806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yamamoto M, Suzuki S, Togashi K, Sanomachi T, Seino S, Kitanaka C, Okada M. AS602801 sensitizes ovarian cancer stem cells to paclitaxel by down-regulating MDR1. Anticancer Res. 2019;39:609–617. doi: 10.21873/anticanres.13154. [DOI] [PubMed] [Google Scholar]
- 23.Gao J, Hou D, Hu P, Mao G. Curcumol increases the sensitivity of colon cancer to 5-FU by regulating Wnt/β-catenin signaling. Transl Cancer Res. 2021;10:2437–2450. doi: 10.21037/tcr-21-689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li M, Li ZH, Song J, Li X, Zhai P, Mu X, Qiu F, Yao L. miR-205 Reverses MDR-1 mediated doxorubicin resistance via PTEN in human liver cancer HepG2 cells. Cell J. 2022;24:112–119. doi: 10.22074/cellj.2022.7231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang L, Li Y, Hu C, Chen Y, Chen Z, Chen ZS, Zhang JY, Fang S. CDK6-PI3K signaling axis is an efficient target for attenuating ABCB1/P-gp mediated multi-drug resistance (MDR) in cancer cells. Mol Cancer. 2022;21:103. doi: 10.1186/s12943-022-01524-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wan Y, Chen Z, Wang Y, Zhao W, Pei Z, Pu L, Lv Y, Li J, Li J, Pei Y. A hyaluronic acid modified cuprous metal-organic complex for reversing multidrug resistance via redox dyshomeostasis. Carbohydr Polym. 2023;311:120762. doi: 10.1016/j.carbpol.2023.120762. [DOI] [PubMed] [Google Scholar]
- 27.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 28.Abou-Alfa GK. Selection of patients with hepatocellular carcinoma for sorafenib. J Natl Compr Canc Netw. 2009;7:397–403. doi: 10.6004/jnccn.2009.0028. [DOI] [PubMed] [Google Scholar]
- 29.Xia X, Wang Q, Ye T, Liu Y, Liu D, Song S, Zheng C. NRF2/ABCB1-mediated efflux and PARP1-mediated dampening of DNA damage contribute to doxorubicin resistance in chronic hypoxic HepG2 cells. Fundam Clin Pharmacol. 2020;34:41–50. doi: 10.1111/fcp.12505. [DOI] [PubMed] [Google Scholar]
- 30.Yuan P, Zheng A, Tang Q. Tripartite motif protein 25 is associated with epirubicin resistance in hepatocellular carcinoma cells via regulating PTEN/AKT pathway. Cell Biol Int. 2020;44:1503–1513. doi: 10.1002/cbin.11346. [DOI] [PubMed] [Google Scholar]
- 31.Mou SJ, Yang PF, Liu YP, Xu N, Jiang WW, Yue WJ. BCLAF1 promotes cell proliferation, invasion and drug-resistance though targeting lncRNA NEAT1 in hepatocellular carcinoma. Life Sci. 2020;242:117177. doi: 10.1016/j.lfs.2019.117177. [DOI] [PubMed] [Google Scholar]
- 32.Fang Z, Chen W, Yuan Z, Liu X, Jiang H. LncRNA-MALAT1 contributes to the cisplatin-resistance of lung cancer by upregulating MRP1 and MDR1 via STAT3 activation. Biomed Pharmacother. 2018;101:536–542. doi: 10.1016/j.biopha.2018.02.130. [DOI] [PubMed] [Google Scholar]
- 33.Zhao L, Bin S, He HL, Yang JM, Pu YC, Gao CH, Wang H, Wang BL. Sodium butyrate increases P-gp expression in lung cancer by upregulation of STAT3 and mRNA stabilization of ABCB1. Anticancer Drugs. 2018;29:227–233. doi: 10.1097/CAD.0000000000000588. [DOI] [PubMed] [Google Scholar]
- 34.Zhu J, Hu W, Zhang Y, Du P, Xiao W, Li Y. Comparison of survival outcomes of chemotherapy plus surgery vs chemotherapy alone for patients with isolated liver metastases from gallbladder carcinoma. Am Surg. 2023;89:676–684. doi: 10.1177/00031348211038563. [DOI] [PubMed] [Google Scholar]
- 35.Wu D, Liu L, Yan X, Wang C, Wang Y, Han K, Lin S, Gan Z, Min D. Pleiotrophin promotes chemoresistance to doxorubicin in osteosarcoma by upregulating P-glycoprotein. Oncotarget. 2017;8:63857–63870. doi: 10.18632/oncotarget.19148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yang JZ, Huang LH, Chen R, Meng LJ, Gao YY, Ji QY, Wang Y. LIM kinase 1 serves an important role in the multidrug resistance of osteosarcoma cells. Oncol Lett. 2018;15:250–256. doi: 10.3892/ol.2017.7317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu S, Chen S, Yuan W, Wang H, Chen K, Li D, Li D. PD-1/PD-L1 interaction up-regulates MDR1/P-gp expression in breast cancer cells via PI3K/AKT and MAPK/ERK pathways. Oncotarget. 2017;8:99901–99912. doi: 10.18632/oncotarget.21914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen S, Wang H, Li Z, You J, Wu QW, Zhao C, Tzeng CM, Zhang ZM. Interaction of WBP2 with ERα increases doxorubicin resistance of breast cancer cells by modulating MDR1 transcription. Br J Cancer. 2018;119:182–192. doi: 10.1038/s41416-018-0119-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lim JS, Jung GY, Park SY. Nkx-2.5 regulates MDR1 expression via its upstream promoter in breast cancer cells. J Korean Med Sci. 2019;34:e100. doi: 10.3346/jkms.2019.34.e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Baltes F, Pfeifer V, Silbermann K, Caspers J, Wantoch von Rekowski K, Schlesinger M, Bendas G. β1-Integrin binding to collagen type 1 transmits breast cancer cells into chemoresistance by activating ABC efflux transporters. Biochim Biophys Acta Mol Cell Res. 2020;1867:118663. doi: 10.1016/j.bbamcr.2020.118663. [DOI] [PubMed] [Google Scholar]
- 41.Li G, Guo J, Shen BQ, Yadav DB, Sliwkowski MX, Crocker LM, Lacap JA, Phillips GDL. Mechanisms of acquired resistance to trastuzumab emtansine in breast cancer cells. Mol Cancer Ther. 2018;17:1441–1453. doi: 10.1158/1535-7163.MCT-17-0296. [DOI] [PubMed] [Google Scholar]
- 42.Tang H, Zeng L, Wang J, Zhang X, Ruan Q, Wang J, Cui S, Yang D. Reversal of 5-fluorouracil resistance by EGCG is mediate by inactivation of TFAP2A/VEGF signaling pathway and down-regulation of MDR-1 and P-gp expression in gastric cancer. Oncotarget. 2017;8:82842–82853. doi: 10.18632/oncotarget.20666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Deng XJ, Zheng HL, Ke XQ, Deng M, Ma ZZ, Zhu Y, Cui YY. Hsa-miR-34a-5p reverses multidrug resistance in gastric cancer cells by targeting the 3′-UTR of SIRT1 and inhibiting its expression. Cell Signal. 2021;84:110016. doi: 10.1016/j.cellsig.2021.110016. [DOI] [PubMed] [Google Scholar]
- 44.Xu YD, Shang J, Li M, Zhang YY. LncRNA DANCR accelerates the development of multidrug resistance of gastric cancer. Eur Rev Med Pharmacol Sci. 2019;23:2794–2802. doi: 10.26355/eurrev_201904_17554. [DOI] [PubMed] [Google Scholar]
- 45.Zhang X, Bo P, Liu L, Zhang X, Li J. Overexpression of long non-coding RNA GHET1 promotes the development of multidrug resistance in gastric cancer cells. Biomed Pharmacother. 2017;92:580–585. doi: 10.1016/j.biopha.2017.04.111. [DOI] [PubMed] [Google Scholar]
- 46.Tan B, Li Y, Zhao Q, Fan L, Wang D. ZNF139 increases multidrug resistance in gastric cancer cells by inhibiting miR-185. Biosci Rep. 2018;38:BSR20181023. doi: 10.1042/BSR20181023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yan X, Zhao J, Zhang R. Visfatin mediates doxorubicin resistance in human colorectal cancer cells via up regulation of multidrug resistance 1 (MDR1) Cancer Chemother Pharmacol. 2017;80:395–403. doi: 10.1007/s00280-017-3365-y. [DOI] [PubMed] [Google Scholar]
- 48.Gao Z, Li Z, Liu Y, Liu Z. Forkhead box O3 promotes colon cancer proliferation and drug resistance by activating MDR1 expression. Mol Genet Genomic Med. 2019;7:e554. doi: 10.1002/mgg3.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Du J, He Y, Li P, Wu W, Chen Y, Ruan H. IL-8 regulates the doxorubicin resistance of colorectal cancer cells via modulation of multidrug resistance 1 (MDR1) Cancer Chemother Pharmacol. 2018;81:1111–1119. doi: 10.1007/s00280-018-3584-x. [DOI] [PubMed] [Google Scholar]
- 50.Zhang S, Chatterjee T, Godoy C, Wu L, Liu QJ, Carmon KS. GPR56 drives colorectal tumor growth and promotes drug resistance through upregulation of MDR1 expression via a RhoA-mediated mechanism. Mol Cancer Res. 2019;17:2196–2207. doi: 10.1158/1541-7786.MCR-19-0436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sui M, Yang H, Guo M, Li W, Gong Z, Jiang J, Li P. Cajanol sensitizes A2780/Taxol cells to paclitaxel by inhibiting the PI3K/Akt/NF-κB signaling pathway. Front Pharmacol. 2021;12:783317. doi: 10.3389/fphar.2021.783317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhao P, Wang S, Jiang J, Liu H, Zhu X, Zhao N, Li J, Yin Y, Pan X, Yang X, et al. TIPE2 sensitizes osteosarcoma cells to cis-platin by down-regulating MDR1 via the TAK1-NF-κB and-AP-1 pathways. Mol Immunol. 2018;101:471–478. doi: 10.1016/j.molimm.2018.08.010. [DOI] [PubMed] [Google Scholar]
- 53.Song W, Liang C, Sun Y, Morii S, Yomogida S, Isaji T, Fukuda T, Hang Q, Hara A, Nakano M, Gu J. Expression of GnT-III decreases chemoresistance via negatively regulating P-glycoprotein expression: Involvement of the TNFR2-NF-κB signaling pathway. J Biol Chem. 2023;299:103051. doi: 10.1016/j.jbc.2023.103051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liu K, Song J, Yan Y, Zou K, Che Y, Wang B, Li Z, Yu W, Guo W, Zou L, et al. Melatonin increases the chemosensitivity of diffuse large B-cell lymphoma cells to epirubicin by inhibiting P-glycoprotein expression via the NF-κB pathway. Transl Oncol. 2021;14:100876. doi: 10.1016/j.tranon.2020.100876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu RM, Xu P, Chen Q, Feng SL, Xie Y. A multiple-targets alkaloid nuciferine overcomes paclitaxel-induced drug resistance in vitro and in vivo. Phytomedicine. 2020;79:153342. doi: 10.1016/j.phymed.2020.153342. [DOI] [PubMed] [Google Scholar]
- 56.Wang H, Jia XH, Chen JR, Wang JY, Li YJ. Osthole shows the potential to overcome P-glycoprotein-mediated multidrug resistance in human myelogenous leukemia K562/ADM cells by inhibiting the PI3K/Akt signaling pathway. Oncol Rep. 2016;35:3659–3668. doi: 10.3892/or.2016.4730. [DOI] [PubMed] [Google Scholar]
- 57.Satonaka H, Ishida K, Takai M, Koide R, Shigemasa R, Ueyama J, Ishikawa T, Hayashi K, Goto H, Wakusawa S. (-)-Epigallocatechin-3-gallate down-regulates doxorubicin-induced overexpression of P-glycoprotein through the coordinate inhibition of PI3K/Akt and MEK/ERK signaling pathways. Anticancer Res. 2017;37:6071–6077. doi: 10.21873/anticanres.12055. [DOI] [PubMed] [Google Scholar]
- 58.Ding Y, Zhen Z, Nisar MA, Ali F, Din RU, Khan M, Mughal TA, Alam G, Liu L, Saleem MZ. Sesquiterpene lactones attenuate paclitaxel resistance via inhibiting MALAT1/STAT3/FUT4 Axis and P-glycoprotein transporters in lung cancer cells. Front Pharmacol. 2022;13:795613. doi: 10.3389/fphar.2022.795613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang PP, Luan JJ, Xu WK, Wang L, Xu DJ, Yang CY, Zhu YH, Wang YQ. Astragaloside IV downregulates the expression of MDR1 in Bel-7402/FU human hepatic cancer cells by inhibiting the JNK/c-Jun/AP-1 signaling pathway. Mol Med Rep. 2017;16:2761–2766. doi: 10.3892/mmr.2017.6924. [DOI] [PubMed] [Google Scholar]
- 60.Qin T, Zhu W, Kan X, Li L, Wu D. Luteolin attenuates the chemoresistance of osteosarcoma through inhibiting the PTN/β-catenin/MDR1 signaling axis by upregulating miR-384. J Bone Oncol. 2022;34:100429–34. doi: 10.1016/j.jbo.2022.100429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Li L, Fu Q, Xia M, Xin L, Shen H, Li G, Ji G, Meng Q, Xie Y. Inhibition of P-glycoprotein mediated efflux in Caco-2 cells by phytic acid. J Agric Food Chem. 2018;66:988–998. doi: 10.1021/acs.jafc.7b04307. [DOI] [PubMed] [Google Scholar]
- 62.Mirzaei SA, Reiisi S, Ghiasi Tabari P, Shekari A, Aliakbari F, Azadfallah E, Elahian F. Broad blocking of MDR efflux pumps by acetylshikonin and acetoxyisovalerylshikonin to generate hypersensitive phenotype of malignant carcinoma cells. Sci Rep. 2018;8:3446. doi: 10.1038/s41598-018-21710-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Shen X, Chen G, Zhu G, Fong WF. (+/−)-3′-O, 4′-O-dicynnamoyl-cis-khellactone, a derivative of (+/−)-praeruptorin A, reverses P-glycoprotein mediated multidrug resistance in cancer cells. Bioorg Med Chem. 2006;14:7138–7145. doi: 10.1016/j.bmc.2006.06.066. [DOI] [PubMed] [Google Scholar]
- 64.Bai Z, Zhou Q, Zhu H, Ye X, Wu P, Ma L. QTMP, a novel thiourea polymer, causes DNA damage to exert anticancer activity and overcome multidrug resistance in colorectal cancer cells. Front Oncol. 2021;11:667689. doi: 10.3389/fonc.2021.667689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gao M, Liu T, Li J, Guan Q, Wang H, Yan S, Li Z, Zuo D, Zhang W, Wu Y. YAN, a novel microtubule inhibitor, inhibits P-gp and MRP1 function and induces mitotic slippage followed by apoptosis in multidrug-resistant A549/Taxol cells. Toxicol In Vitro. 2020;69:104971. doi: 10.1016/j.tiv.2020.104971. [DOI] [PubMed] [Google Scholar]
- 66.Wu CP, Murakami M, Wu YS, Chi YC, Hsiao SH, Huang YH, Hung TH, Ambudkar SV. Branebrutinib (BMS-986195), a bruton's tyrosine kinase inhibitor, resensitizes P-glycoprotein-overexpressing multidrug-resistant cancer cells to chemotherapeutic agents. Front Cell Dev Biol. 2021;9:699571. doi: 10.3389/fcell.2021.699571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Podolski-Renić A, Dinić J, Stanković T, Tsakovska I, Pajeva I, Tuccinardi T, Botta L, Schenone S, Pešić M. New therapeutic strategy for overcoming multidrug resistance in cancer cells with pyrazolo[3,4-d]pyrimidine tyrosine kinase inhibitors. Cancers (Basel) 2021;13:5308. doi: 10.3390/cancers13215308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wu CP, Hung TH, Lusvarghi S, Chu YH, Hsiao SH, Huang YH, Chang YT, Ambudkar SV. The third-generation EGFR inhibitor almonertinib (HS-10296) resensitizes ABCB1-overexpressing multidrug-resistant cancer cells to chemotherapeutic drugs. Biochem Pharmacol. 2021;188:114516. doi: 10.1016/j.bcp.2021.114516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zhang L, Ye B, Lin Y, Li YD, Wang JQ, Chen Z, Ping FF, Chen ZS. Ribociclib inhibits P-gp-mediated multidrug resistance in human epidermoid carcinoma cells. Front Pharmacol. 2022;13:867128. doi: 10.3389/fphar.2022.867128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Laiolo J, Barbieri CL, Joray MB, Lanza PA, Palacios SM, Vera DMA, Carpinella MC. Plant extracts and betulin from Ligaria cuneifolia inhibit P-glycoprotein function in leukemia cells. Food Chem Toxicol. 2021;147:111922. doi: 10.1016/j.fct.2020.111922. [DOI] [PubMed] [Google Scholar]
- 71.Liu Z, Wen X, Wang G, Zhou Y. Involvement of P-gp on reversing multidrug resistance effects of 23-hydroxybetulinic acid on chemotherapeutic agents. Front Pharmacol. 2021;12:796745. doi: 10.3389/fphar.2021.796745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yang T, Wang S, Li H, Zhao Q, Yan S, Dong M, Liu D, Chen X, Li R. Lathyrane diterpenes from Euphorbia lathyris and the potential mechanism to reverse the multi-drug resistance in HepG2/ADR cells. Biomed Pharmacother. 2020;121:109663. doi: 10.1016/j.biopha.2019.109663. [DOI] [PubMed] [Google Scholar]
- 73.Qian J, Xia M, Liu W, Li L, Yang J, Mei Y, Meng Q, Xie Y. Glabridin resensitizes p-glycoprotein-overexpressing multidrug-resistant cancer cells to conventional chemotherapeutic agents. Eur J Pharmacol. 2019;852:231–243. doi: 10.1016/j.ejphar.2019.04.002. [DOI] [PubMed] [Google Scholar]
- 74.Teng YN, Lin KI, Lin YC, Thang TD, Lan YH, Hung CC. A novel flavonoid from Fissistigma cupreonitens, 5-hydroxy-7,8-dimethoxyflavanone, competitively inhibited the efflux function of human P-glycoprotein and reversed cancer multi-drug resistance. Phytomedicine. 2021;85:153528. doi: 10.1016/j.phymed.2021.153528. [DOI] [PubMed] [Google Scholar]
- 75.Min H, Niu M, Zhang W, Yan J, Li J, Tan X, Li B, Su M, Di B, Yan F. Emodin reverses leukemia multidrug resistance by competitive inhibition and downregulation of P-glycoprotein. PLoS One. 2017;12:e0187971. doi: 10.1371/journal.pone.0187971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Pellegrini E, Multari G, Gallo FR, Vecchiotti D, Zazzeroni F, Condello M, Meschini S. A natural product, voacamine, sensitizes paclitaxel-resistant human ovarian cancer cells. Toxicol Appl Pharmacol. 2022;434:115816. doi: 10.1016/j.taap.2021.115816. [DOI] [PubMed] [Google Scholar]
- 77.Sagnou M, Novikov FN, Ivanova ES, Alexiou P, Stroylov VS, Titov IY, Tatarskiy VV, Vagida MS, Pelecanou M, Shtil AA, Chilov GG. Novel curcumin derivatives as P-glycoprotein inhibitors: Molecular modeling, synthesis and sensitization of multidrug resistant cells to doxorubicin. Eur J Med Chem. 2020;198:112331. doi: 10.1016/j.ejmech.2020.112331. [DOI] [PubMed] [Google Scholar]
- 78.Creemers SG, van Koetsveld PM, De Herder WW, Dogan F, Franssen GJH, Feelders RA, Hofland LJ. MDR1 inhibition increases sensitivity to doxorubicin and etoposide in adrenocortical cancer. Endocr Relat Cancer. 2019;26:367–378. doi: 10.1530/ERC-18-0500. [DOI] [PubMed] [Google Scholar]
- 79.Wang SQ, Teng QX, Wang S, Lei ZN, Hu HH, Lv HF, Chen BB, Wang JZ, Shi XJ, Xu WF, et al. Preclinical studies of the triazolo[1,5-a]pyrimidine derivative WS-716 as a highly potent, specific and orally active P-glycoprotein (P-gp) inhibitor. Acta Pharm Sin B. 2022;12:3263–3280. doi: 10.1016/j.apsb.2022.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Dei S, Coronnello M, Bartolucci G, Manetti D, Romanelli MN, Udomtanakunchai C, Salerno M, Teodori E. Design and synthesis of new potent N,N-bis(arylalkyl)piperazine derivatives as multidrug resistance (MDR) reversing agents. Eur J Med Chem. 2018;147:7–20. doi: 10.1016/j.ejmech.2018.01.092. [DOI] [PubMed] [Google Scholar]
- 81.Qiu Q, Zou F, Li H, Shi W, Zhou D, Zhang P, Li T, Yin Z, Cai Z, Jiang Y, et al. Structure-based discovery of pyrimidine aminobenzene derivatives as potent oral reversal agents against P-gp- and BCRP-mediated multidrug resistance. J Med Chem. 2021;64:6179–6197. doi: 10.1021/acs.jmedchem.1c00246. [DOI] [PubMed] [Google Scholar]
- 82.Li YS, Yang X, Zhao DS, Cai Y, Huang Z, Wu R, Wang SJ, Liu GJ, Wang J, Bao XZ, et al. Design, synthesis and bioactivity study on 5-phenylfuran derivatives as potent reversal agents against P-glycoprotein-mediated multidrug resistance in MCF-7/ADR cell. Eur J Med Chem. 2021;216:113336. doi: 10.1016/j.ejmech.2021.113336. [DOI] [PubMed] [Google Scholar]
- 83.Yuan S, Wang B, Dai QQ, Zhang XN, Zhang JY, Zuo JH, Liu H, Chen ZS, Li GB, Wang S, et al. Discovery of new 4-indolyl quinazoline derivatives as highly potent and orally bioavailable P-glycoprotein inhibitors. J Med Chem. 2021;64:14895–14911. doi: 10.1021/acs.jmedchem.1c01452. [DOI] [PubMed] [Google Scholar]
- 84.Wang H, Wang X, Liao A, Liu Z. Hypomethylation agent decitabine restores drug sensitivity by depressing P-glycoprotein activity through MAPK signaling pathway. Mol Cell Biochem. 2017;433:141–148. doi: 10.1007/s11010-017-3022-0. [DOI] [PubMed] [Google Scholar]
- 85.Snyder S, Murundi S, Crawford L, Putnam D. Enabling P-glycoprotein inhibition in multidrug resistant cancer through the reverse targeting of a quinidine-PEG conjugate. J Control Release. 2020;317:291–299. doi: 10.1016/j.jconrel.2019.11.027. [DOI] [PubMed] [Google Scholar]
- 86.Zhang H, Bian S, Xu Z, Gao M, Wang H, Zhang J, Zhang M, Ke Y, Wang W, Chen ZS, Xu H. The effect and mechanistic study of encequidar on reversing the resistance of SW620/AD300 cells to doxorubicin. Biochem Pharmacol. 2022;205:115258. doi: 10.1016/j.bcp.2022.115258. [DOI] [PubMed] [Google Scholar]
- 87.Xu SW, Law BYK, Qu SLQ, Hamdoun S, Chen J, Zhang W, Guo JR, Wu AG, Mok SWF, Zhang DW, et al. SERCA and P-glycoprotein inhibition and ATP depletion are necessary for celastrol-induced autophagic cell death and collateral sensitivity in multidrug-resistant tumor cells. Pharmacol Res. 2020;153:104660. doi: 10.1016/j.phrs.2020.104660. [DOI] [PubMed] [Google Scholar]
- 88.Rauf A, Uddin G, Raza M, Ahmad B, Jehan N, Siddiqui BS, Molnar J, Csonka A, Szabo D. Reversal of multidrug resistance in mouse lymphoma cells by extracts and flavonoids from Pistacia integerrima. Asian Pac J Cancer Prev. 2016;17:51–55. doi: 10.7314/APJCP.2016.17.1.51. [DOI] [PubMed] [Google Scholar]
- 89.Giorgi C, Gasser UE, Lafont ME, Holzgang HE, Thalhammer VF. Inhibition of chemoresistance in primary tumor cells by Camellia sinensis non fermentatum extract noviphenone (NPE®) Anticancer Res. 2019;39:4101–4110. doi: 10.21873/anticanres.13568. [DOI] [PubMed] [Google Scholar]
- 90.Kawami M, Yamada Y, Issarachot O, Junyaprasert VB, Yumoto R, Takano M. P-gp modulating effect of Azadirachta indica extract in multidrug-resistant cancer cell lines. Pharmazie. 2018;73:104–109. doi: 10.1691/ph.2018.7116. [DOI] [PubMed] [Google Scholar]
- 91.Zheng Y, Su C, Zhao L, Shi Y. mAb MDR1-modified chitosan nanoparticles overcome acquired EGFR-TKI resistance through two potential therapeutic targets modulation of MDR1 and autophagy. J Nanobiotechnology. 2017;15:66. doi: 10.1186/s12951-017-0302-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chen Z, Pan T, Jiang D, Jin L, Geng Y, Feng X, Shen A, Zhang L. The lncRNA-GAS5/miR-221-3p/DKK2 axis modulates ABCB1-mediated adriamycin resistance of breast cancer via the Wnt/β-catenin signaling pathway. Mol Ther Nucleic Acids. 2020;19:1434–1448. doi: 10.1016/j.omtn.2020.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Han Z, Shi L. Long non-coding RNA LUCAT1 modulates methotrexate resistance in osteosarcoma via miR-200c/ABCB1 axis. Biochem Biophys Res Commun. 2018;495:947–953. doi: 10.1016/j.bbrc.2017.11.121. [DOI] [PubMed] [Google Scholar]
- 94.Kang Y, Zhang S, Cao W, Wan D, Sun L. Knockdown of LncRNA CRNDE suppresses proliferation and P-glycoprotein-mediated multidrug resistance in acute myelocytic leukemia through the Wnt/β-catenin pathway. Biosci Rep. 2020;40:BSR20193450. doi: 10.1042/BSR20193450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zou H, Li H. Knockdown of long non-coding RNA LINC00152 increases cisplatin sensitivity in ovarian cancer cells. Exp Ther Med. 2019;18:4510–4516. doi: 10.3892/etm.2019.8066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zou Z, Zou R, Zong D, Shi Y, Chen J, Huang J, Zhu J, Chen L, Bao X, Liu Y, et al. miR-495 sensitizes MDR cancer cells to the combination of doxorubicin and taxol by inhibiting MDR1 expression. J Cell Mol Med. 2017;21:1929–1943. doi: 10.1111/jcmm.13114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhao Y, Qi X, Chen J, Wei W, Yu C, Yan H, Pu M, Li Y, Miao L, Li C, Ren J. The miR-491-3p/Sp3/ABCB1 axis attenuates multidrug resistance of hepatocellular carcinoma. Cancer Lett. 2017;408:102–111. doi: 10.1016/j.canlet.2017.08.027. [DOI] [PubMed] [Google Scholar]
- 98.Yi D, Xu L, Wang R, Lu X, Sang J. miR-381 overcomes cisplatin resistance in breast cancer by targeting MDR1. Cell Biol Int. 2019;43:12–21. doi: 10.1002/cbin.11071. [DOI] [PubMed] [Google Scholar]
- 99.Zheng SZ, Sun P, Wang JP, Liu Y, Gong W, Liu J. MiR-34a overexpression enhances the inhibitory effect of doxorubicin on HepG2 cells. World J Gastroenterol. 2019;25:2752–2762. doi: 10.3748/wjg.v25.i22.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wei S, Gao J, Zhang M, Dou Z, Li W, Zhao L. Dual delivery nanoscale device for miR-451 and adriamycin co-delivery to combat multidrug resistant in bladder cancer. Biomed Pharmacother. 2020;122:109473. doi: 10.1016/j.biopha.2019.109473. [DOI] [PubMed] [Google Scholar]
- 101.Kenworthy R, Bosco DB, DeLigio JT, Zorio DAR. Micro-RNA149 confers taxane resistance to malignant mesothelioma cells via regulation of P-glycoprotein expression. Cancer Biol Ther. 2018;19:181–187. doi: 10.1080/15384047.2017.1415677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wang S, Guo J, Mo Z, Shi X, Qu C. Clinical significance and correlation of miR-200c and P-gp expression in gastric cancer and the effects on multidrug resistance. J Gastrointest Oncol. 2022;13:581–592. doi: 10.21037/jgo-22-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Cao F, Yin LX. miR-122 enhances sensitivity of hepatocellular carcinoma to oxaliplatin via inhibiting MDR1 by targeting Wnt/β-catenin pathway. Exp Mol Pathol. 2019;106:34–43. doi: 10.1016/j.yexmp.2018.10.009. [DOI] [PubMed] [Google Scholar]
- 104.Sousa D, Matthiesen R, Lima RT, Vasconcelos MH. Deep sequencing analysis reveals distinctive non-coding RNAs when comparing tumor multidrug-resistant cells and extracellular vesicles with drug-sensitive counterparts. Cancers (Basel) 2020;12:200. doi: 10.3390/cancers12010200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Shi X, Valizadeh A, Mir SM, Asemi Z, Karimian A, Majidina M, Safa A, Yosefi B. miRNA-29a reverses P-glycoprotein-mediated drug resistance and inhibits proliferation via up-regulation of PTEN in colon cancer cells. Eur J Pharmacol. 2020;880:173138. doi: 10.1016/j.ejphar.2020.173138. [DOI] [PubMed] [Google Scholar]
- 106.Xie B, Li L, Zhang Z, Zhao L, Cheng J, Zhou C, Cheng J, Yan J, Chen J, Yi J, et al. MicroRNA-1246 by targeting AXIN2 and GSK-3β overcomes drug resistance and induces apoptosis in chemo-resistant leukemia cells. J Cancer. 2021;12:4196–4208. doi: 10.7150/jca.58522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kara G, Calin GA, Ozpolat B. RNAi-based therapeutics and tumor targeted delivery in cancer. Adv Drug Deliv Rev. 2022;182:114113. doi: 10.1016/j.addr.2022.114113. [DOI] [PubMed] [Google Scholar]
- 108.Yalamarty SSK, Filipczak N, Li X, Pathrikar TV, Cotter C, Torchilin VP. Co-delivery of siRNA and chemotherapeutic drug using 2C5 antibody-targeted dendrimer-based mixed micelles for multidrug resistant cancers. Pharmaceutics. 2022;14:1470. doi: 10.3390/pharmaceutics14071470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Wang C, Guan W, Peng J, Chen Y, Xu G, Dou H. Gene/paclitaxel co-delivering nanocarriers prepared by framework-induced self-assembly for the inhibition of highly drug-resistant tumors. Acta Biomater. 2020;103:247–258. doi: 10.1016/j.actbio.2019.12.015. [DOI] [PubMed] [Google Scholar]
- 110.Jiang Y, Liu Y, Wang M, Li Z, Su L, Xu X, Xing C, Li J, Lin L, Lu C, Yang H. siRNA-based carrier-free system for synergistic chemo/chemodynamic/RNAi therapy of drug-resistant tumors. ACS Appl Mater Interfaces. 2022;14:361–372. doi: 10.1021/acsami.1c20898. [DOI] [PubMed] [Google Scholar]
- 111.Yang X, Wang Y, Chen S, Zhang S, Cui C. Cetuximab-modified human serum albumin nanoparticles co-loaded with doxorubicin and MDR1 siRNA for the treatment of drug-resistant breast tumors. Int J Nanomedicine. 2021;16:7051–7069. doi: 10.2147/IJN.S332830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Liu H, Ma D, Chen J, Ye L, Li Y, Xie Y, Zhao X, Zou H, Chen X, Pu J, Liu P. A targeted nanoplatform co-delivery of pooled siRNA and doxorubicin for reversing of multidrug resistance in breast cancer. Nano Res. 2022;15:6306–6314. doi: 10.1007/s12274-022-4254-1. [DOI] [Google Scholar]
- 113.Wu J, Wang Q, Dong X, Xu M, Yang J, Yi X, Chen B, Dong X, Wang Y, Lou X, et al. Biocompatible AIEgen/p-glycoprotein siRNA@reduction-sensitive paclitaxel polymeric prodrug nanoparticles for overcoming chemotherapy resistance in ovarian cancer. Theranostics. 2021;11:3710–3724. doi: 10.7150/thno.53828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zhang J, Du Z, Pan S, Shi M, Li J, Yang C, Hu H, Qiao M, Chen D, Zhao X. Overcoming multidrug resistance by codelivery of MDR1-targeting siRNA and doxorubicin using EphA10-mediated pH-sensitive lipoplexes: In vitro and in vivo evaluation. ACS Appl Mater Interfaces. 2018;10:21590–21600. doi: 10.1021/acsami.8b01806. [DOI] [PubMed] [Google Scholar]
- 115.Cao X, Li R, Xiong H, Su J, Guo C, An T, Zong H, Zhao R. Novel Pt(IV) complexes to overcome multidrug resistance in gastric cancer by targeting P-glycoprotein. Eur J Med Chem. 2021;221:113520. doi: 10.1016/j.ejmech.2021.113520. [DOI] [PubMed] [Google Scholar]
- 116.Liu ZL, Jin BJ, Cheng CG, Zhang FX, Wang SW, Wang Y, Wu B. Apatinib resensitizes cisplatin-resistant non-small cell lung carcinoma A549 cell through reversing multidrug resistance and suppressing ERK signaling pathway. Eur Rev Med Pharmacol Sci. 2017;21:5370–5377. doi: 10.26355/eurrev_201712_13922. [DOI] [PubMed] [Google Scholar]
- 117.Ji L, Liu X, Zhang S, Tang S, Yang S, Li S, Qi X, Yu S, Lu L, Meng X, Liu Z. The novel triazolonaphthalimide derivative LSS-11 synergizes the anti-proliferative effect of paclitaxel via STAT3-dependent MDR1 and MRP1 downregulation in chemoresistant lung cancer cells. Molecules. 2017;22:1822. doi: 10.3390/molecules22111822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Zhang L, Li Y, Wang Q, Chen Z, Li X, Wu Z, Hu C, Liao D, Zhang W, Chen ZS. The PI3K subunits, P110α and P110β are potential targets for overcoming P-gp and BCRP-mediated MDR in cancer. Mol Cancer. 2020;19:10. doi: 10.1186/s12943-019-1112-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Liu T, Peng Y, Li X, Liu L, Liu F, He L. A novel delocalized lipophilic cation-chlorambucil conjugate inhibits P-glycoprotein in HepG2/ADM cells. Bioorg Med Chem. 2017;25:5461–5467. doi: 10.1016/j.bmc.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 120.Ganesan M, Kanimozhi G, Pradhapsingh B, Khan HA, Alhomida AS, Ekhzaimy A, Brindha GR, Prasad NR. Phytochemicals reverse P-glycoprotein mediated multidrug resistance via signal transduction pathways. Biomed Pharmacother. 2021;139:111632. doi: 10.1016/j.biopha.2021.111632. [DOI] [PubMed] [Google Scholar]
- 121.Li Y, Li X, Lu Y, Chaurasiya B, Mi G, Shi D, Chen D, Webster TJ, Tu J, Shen Y. Co-delivery of Poria cocos extract and doxorubicin as an 'all-in-one' nanocarrier to combat breast cancer multidrug resistance during chemotherapy. Nanomedicine. 2020;23:102095. doi: 10.1016/j.nano.2019.102095. [DOI] [PubMed] [Google Scholar]
- 122.Ye Q, Liu K, Shen Q, Li Q, Hao J, Han F, Jiang RW. Reversal of multidrug resistance in cancer by multi-functional flavonoids. Front Oncol. 2019;9:487. doi: 10.3389/fonc.2019.00487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Fang Y, Liang F, Xia M, Cao W, Pan S, Wu T, Xu X. Structure-activity relationship and mechanism of flavonoids on the inhibitory activity of P-glycoprotein (P-gp)-mediated transport of rhodamine123 and daunorubicin in P-gp overexpressed human mouth epidermal carcinoma (KB/MDR) cells. Food Chem Toxicol. 2021;155:112381. doi: 10.1016/j.fct.2021.112381. [DOI] [PubMed] [Google Scholar]
- 124.Kong W, Ling X, Chen Y, Wu X, Zhao Z, Wang W, Wang S, Lai G, Yu Z. Hesperetin reverses P-glycoprotein-mediated cisplatin resistance in DDP-resistant human lung cancer cells via modulation of the nuclear factor-κB signaling pathway. Int J Mol Med. 2020;45:1213–1224. doi: 10.3892/ijmm.2020.4485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.La X, Zhang L, Li Z, Li H, Yang Y. (-)-Epigallocatechin gallate (EGCG) enhances the sensitivity of colorectal cancer cells to 5-FU by inhibiting GRP78/NF-κB/miR-155-5p/MDR1 pathway. J Agric Food Chem. 2019;67:2510–2518. doi: 10.1021/acs.jafc.8b06665. [DOI] [PubMed] [Google Scholar]
- 126.Mohana S, Ganesan M, Rajendra Prasad N, Ananthakrishnan D, Velmurugan D. Flavonoids modulate multidrug resistance through wnt signaling in P-glycoprotein overexpressing cell lines. BMC Cancer. 2018;18:1168. doi: 10.1186/s12885-018-5103-1. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 127.Wang ZD, Wang RZ, Xia YZ, Kong LY, Yang L. Reversal of multidrug resistance by icaritin in doxorubicin-resistant human osteosarcoma cells. Chin J Nat Med. 2018;16:20–28. doi: 10.1016/S1875-5364(18)30026-8. [DOI] [PubMed] [Google Scholar]
- 128.Wang F, Huang N, Yang Q, Liu J, Chen J. Reversal of doxorubicin-resistance by Salvia miltiorrhiza ligustrazine in the SHG44/doxorubicin glioma drug-resistant cell line. Oncol Lett. 2017;14:4708–4714. doi: 10.3892/ol.2017.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Zhou P, Zhang R, Wang Y, Xu D, Zhang L, Qin J, Su G, Feng Y, Chen H, You S, et al. Cepharanthine hydrochloride reverses the mdr1 (P-glycoprotein)-mediated esophageal squamous cell carcinoma cell cisplatin resistance through JNK and p53 signals. Oncotarget. 2017;8:111144–111160. doi: 10.18632/oncotarget.22676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Zhou X, Jin N, Chen B. Tetrandrine overcomes drug resistance mediated by bone marrow microenvironment by regulating the expression of P-glycoprotein in acute leukemia. Hematology. 2022;27:274–279. doi: 10.1080/16078454.2022.2034256. [DOI] [PubMed] [Google Scholar]
- 131.Qian K, Tang CY, Chen LY, Zheng S, Zhao Y, Ma LS, Xu L, Fan LH, Yu JD, Tan HS, et al. Berberine reverses breast cancer multidrug resistance based on fluorescence pharmacokinetics in vitro and in vivo. ACS Omega. 2021;6:10645–10654. doi: 10.1021/acsomega.0c06288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Huang CZ, Wang YF, Zhang Y, Peng YM, Liu YX, Ma F, Jiang JH, Wang QD. Cepharanthine hydrochloride reverses P-glycoprotein-mediated multidrug resistance in human ovarian carcinoma A2780/Taxol cells by inhibiting the PI3K/Akt signaling pathway. Oncol Rep. 2017;38:2558–2564. doi: 10.3892/or.2017.5879. [DOI] [PubMed] [Google Scholar]
- 133.Liao D, Zhang W, Gupta P, Lei ZN, Wang JQ, Cai CY, Vera AA, Zhang L, Chen ZS, Yang DH. Tetrandrine interaction with ABCB1 reverses multidrug resistance in cancer cells through competition with anti-cancer drugs followed by downregulation of ABCB1 expression. Molecules. 2019;24:4383. doi: 10.3390/molecules24234383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Quarti J, Torres DNM, Ferreira E, Vidal RS, Casanova F, Chiarini LB, Fialho E, Rumjanek VM. Selective cytotoxicity of piperine over multidrug resistance leukemic cells. Molecules. 2021;26:934. doi: 10.3390/molecules26040934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Wang SQ, Li X, Wang XN, Lou HX. Reversal of P-glycoprotein-mediated multidrug resistance in human leukemia cell line K562/A02 by archangelicin. Chin J Nat Med. 2011;9:146–150. [Google Scholar]
- 136.Sharma P, Tyagi A, Bhansali P, Pareek S, Singh V, Ilyas A, Mishra R, Poddar NK. Saponins: Extraction, bio-medicinal properties and way forward to anti-viral representatives. Food Chem Toxicol. 2021;150:112075. doi: 10.1016/j.fct.2021.112075. [DOI] [PubMed] [Google Scholar]
- 137.Li Y, Sun Y, Tang T, Niu Y, Li X, Xie M, Jin H, Mei Q. Paris saponin VII reverses chemoresistance in breast MCF-7/ADR cells. J Ethnopharmacol. 2019;232:47–54. doi: 10.1016/j.jep.2018.12.018. [DOI] [PubMed] [Google Scholar]
- 138.Niu X, Shi Y, Li Q, Chen H, Fan X, Yu Y, Lv C, Lu J. Ginsenoside Rb1 for overcoming cisplatin-insensitivity of A549/DDP cells in vitro and vivo through the dual-inhibition on two efflux pumps of ABCB1 and PTCH1. Phytomedicine. 2023;115:154776. doi: 10.1016/j.phymed.2023.154776. [DOI] [PubMed] [Google Scholar]
- 139.Li J, Zheng L, Wang R, Sun D, Liang S, Wu J, Liu Y, Tian X, Li T, Yang Y, Han L. Synergistic combination of sodium aescinate-stabilized, polymer-free, twin-like nanoparticles to reverse paclitaxel resistance. Int J Nanomedicine. 2020;15:5839–5853. doi: 10.2147/IJN.S259432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Huang C, Xu D, Xia Q, Wang P, Rong C, Su Y. Reversal of P-glycoprotein-mediated multidrug resistance of human hepatic cancer cells by astragaloside II. J Pharm Pharmacol. 2012;64:1741–1750. doi: 10.1111/j.2042-7158.2012.01549.x. [DOI] [PubMed] [Google Scholar]
- 141.Wang PP, Xu DJ, Huang C, Wang WP, Xu WK. Astragaloside IV reduces the expression level of P-glycoprotein in multidrug-resistant human hepatic cancer cell lines. Mol Med Rep. 2014;9:2131–2137. doi: 10.3892/mmr.2014.2074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Liu GW, Liu YH, Jiang GS, Ren WD. The reversal effect of ginsenoside Rh2 on drug resistance in human colorectal carcinoma cells and its mechanism. Hum Cell. 2018;31:189–198. doi: 10.1007/s13577-017-0189-3. [DOI] [PubMed] [Google Scholar]
- 143.Liu C, Gong Q, Chen T, Lv J, Feng Z, Liu P, Deng Z. Treatment with 20(S)-ginsenoside Rg3 reverses multidrug resistance in A549/DDP xenograft tumors. Oncol Lett. 2018;15:4376–4382. doi: 10.3892/ol.2018.7849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Sadava D, Kane SE. Silibinin reverses drug resistance in human small-cell lung carcinoma cells. Cancer Lett. 2013;339:102–106. doi: 10.1016/j.canlet.2013.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Dobiasová S, Řehořová K, Kučerová D, Biedermann D, Káňová K, Petrásková L, Koucká K, Václavíková R, Valentová K, Ruml T, et al. Multidrug resistance modulation activity of silybin derivatives and their anti-inflammatory potential. Antioxidants (Basel) 2020;9:455. doi: 10.3390/antiox9050455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Zhang ZL, Jiang QC, Wang SR. Schisandrin A reverses doxorubicin-resistant human breast cancer cell line by the inhibition of P65 and Stat3 phosphorylation. Breast Cancer. 2018;25:233–242. doi: 10.1007/s12282-017-0821-9. [DOI] [PubMed] [Google Scholar]
- 147.Liao XZ, Gao Y, Sun LL, Liu JH, Chen HR, Yu L, Chen ZZ, Chen WH, Lin LZ. Rosmarinic acid reverses non-small cell lung cancer cisplatin resistance by activating the MAPK signaling pathway. Phytother Res. 2020;34:1142–1153. doi: 10.1002/ptr.6584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Muthusamy G, Gunaseelan S, Prasad NR. Ferulic acid reverses P-glycoprotein-mediated multidrug resistance via inhibition of PI3K/Akt/NF-κB signaling pathway. J Nutr Biochem. 2019;63:62–71. doi: 10.1016/j.jnutbio.2018.09.022. [DOI] [PubMed] [Google Scholar]
- 149.Oh SS, Lee KW, Madhi H, Jeong JW, Park S, Kim M, Lee Y, Han HT, Hwangbo C, Yoo J, Kim KD. Cordycepin resensitizes T24R2 cisplatin-resistant human bladder cancer cells to cisplatin by inactivating Ets-1 dependent MDR1 transcription. Int J Mol Sci. 2020;21:1710. doi: 10.3390/ijms21051710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Sawicka E, Saczko J, Kulbacka J, Szydełko M, Szymańska B, Piwowar A. The influence of interaction between cadmium with 17β-estradiol, 2-methoxyestradiol and 16α-hydroxyestrone on viability and P-glycoprotein in ovarian cancer cell line. Int J Mol Sci. 2022;23:2628. doi: 10.3390/ijms23052628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Ding Y, Fan J, Fan Z, Zhang K. γ-Tocotrienol reverses multidrug resistance of breast cancer cells through the regulation of the γ-Tocotrienol-NF-κB-P-gp axis. J Steroid Biochem Mol Biol. 2021;209:105835. doi: 10.1016/j.jsbmb.2021.105835. [DOI] [PubMed] [Google Scholar]
- 152.Fujihara T, Mizobuchi Y, Nakajima K, Kageji T, Matsuzaki K, Kitazato KT, Otsuka R, Hara K, Mure H, Okazaki T, et al. Down-regulation of MDR1 by Ad-DKK3 via Akt/NFκB pathways augments the anti-tumor effect of temozolomide in glioblastoma cells and a murine xenograft model. J Neurooncol. 2018;139:323–332. doi: 10.1007/s11060-018-2894-5. [DOI] [PubMed] [Google Scholar]
- 153.Norouzi-Barough L, Sarookhani M, Salehi R, Sharifi M, Moghbelinejad S. CRISPR/Cas9, a new approach to successful knockdown of ABCB1/P-glycoprotein and reversal of chemosensitivity in human epithelial ovarian cancer cell line. Iran J Basic Med Sci. 2018;21:181–187. doi: 10.22038/IJBMS.2017.25145.6230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Peng H, Qiao L, Shan G, Gao M, Zhang R, Yi X, He X. Stepwise responsive carboxymethyl chitosan-based nanoplatform for effective drug-resistant breast cancer suppression. Carbohydr Polym. 2022;291:119554. doi: 10.1016/j.carbpol.2022.119554. [DOI] [PubMed] [Google Scholar]
- 155.Teng YN, Wang CCN, Liao WC, Lan YH, Hung CC. Caffeic acid attenuates multi-drug resistance in cancer cells by inhibiting efflux function of human P-glycoprotein. Molecules. 2020;25:247. doi: 10.3390/molecules25020247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Ma Y, Wen J, Wang J, Wang C, Zhang Y, Zhao L, Li J, Feng X. Asiaticoside antagonizes proliferation and chemotherapeutic drug resistance in hepatocellular carcinoma (HCC) cells. Med Sci Monit. 2020;26:e924435. doi: 10.12659/MSM.924435. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.