Abstract
Objective:
To determine the mismatch of desired support versus support received and to evaluate the impact of these mismatches on health outcomes of people with diabetes.
Methods:
This cross-sectional study is a secondary data analysis of medical record and survey data of participants with Type 1 and Type 2 diabetes from a diabetes care and education program. Biophysical metrics included HbA1c, body mass index, systolic blood pressure, diastolic blood pressure, triglycerides, and high- and low-density lipoproteins. Psychosocial and self-care survey outcomes included diabetes distress, diabetes self-care, and diabetes self-efficacy. Support mismatch was a difference score (support desired-support received). Descriptive statistics were computed for demographics, clinical characteristics, and primary outcomes. Multiple linear regressions were computed.
Results:
The percentage of participants experiencing support mismatch (surplus/deficits) across six domains was: 15%/27% (foot care), 22%/24% (take medicine), 24%/23% (test blood sugar), 21%/29% (physical activity), and 18%/34% (follow meal plan). Greater support deficits were associated with higher triglyceride levels, increased diabetes distress, and lower diabetes self-efficacy.
Conclusions:
Findings indicate that greater support deficits can be a risk factor for some poorer physical and psychosocial health outcomes.
Practice Implications:
Interventions to facilitate functional supportive behaviors are an avenue for future research and clinical practice.
Keywords: diabetes mellitus, social support, self-care, self-management, and coping behavior
1. Introduction
Research has demonstrated the buffering effect of social support on morbidity and mortality and patients’ management of a chronic illness, such as diabetes.[1–3] Self-management support, in particular, is a crucial component within the chronic care model, which helps empower and engage individuals in managing their chronic illness to promote better health.[4] Researchers have found that partner or spousal support is associated with effective diabetes management behaviors, such as more physical activity[5], and improved psychosocial health (e.g., reduced diabetes distress).[6] However, support and diabetes management research has largely overlooked that preferences for and actual social support may differ, resulting in a support mismatch for people with diabetes. Identification of two possible social support mismatches: those who receive more support than desired, thus experiencing a support surplus, and those receiving less support than desired, categorized as having unmet needs and experiencing support deficits. Research on both types of support mismatch indicate that social support may be most effective when received support matches one’s desired support.[7] Notably, a person’s desire for support has implications on support effectiveness and their physical (e.g., self-care activities) and psychological (e.g., anxiety and depression) wellbeing.[8–11]
Dyadic coping theories suggest that partner involvement may improve illness management by using collaborative and supportive strategies.[12] Some research has found that patients’ diabetes management and functioning can be impacted by the patients’ perceived appraisals of the degree to which diabetes management is a shared effort with their partner and the unity of the patient/partner alignment of this appraisal.[11,13] However, support mismatch has been underexplored in relation to illness management. This suggests that it is of both clinical and practical importance to examine the role support mismatch plays in the effectiveness of diabetes management.
Despite research on support mismatch in various health contexts, research that specifically examines the implications of support mismatch experienced by individuals with diabetes is limited. Additional research is needed to assess whether the mismatch between received and desired support is a risk factor for poor biophysical and psychological health and self-care of people diagnosed with diabetes. This study aims to 1) determine the level of support match and mismatch that people with diabetes experience and 2) examine the association between support mismatch, particularly support deficits, and biophysical and psychosocial health as well as self-care behaviors. Based on previous research and theoretical frameworks,[4,9,10,12] we hypothesize that individuals with diabetes experiencing greater support deficits will have poorer biophysical, psychosocial, and self-care health outcomes than those experiencing support match.
2. Methods
This cross-sectional study assessed the frequency of support match and mismatch that individuals with diabetes report and the associations between support mismatch and biophysical, psychosocial, and self-care outcomes for individuals diagnosed with Type 1 and Type 2 diabetes. The study is a secondary analysis of data that was collected as part of a larger quality improvement study of a one-day diabetes care and education intervention program that was approved by the Institutional Review Board [#00105292].
Eligible participants were adults diagnosed with Type 1 or Type 2 diabetes who enrolled in the one-day diabetes care and education care program, which encouraged attendance of their support partners. Self-reported survey data were collected prior to participants’ clinic visit for the intervention and biophysical metrics were collected on the day of the clinic visit for the intervention. Analysis inclusion required participants to complete a baseline survey and have available biophysical metric (e.g., HbA1c) data. Study questionnaires were administered online via RedCap, during a phone call, or on a printed copy (based on participant preference) before the one-day diabetes care and education intervention. Consent was obtained electronically via RedCap or by the study coordinator. The study took place from December 2017 to August 2019. Participation was voluntary, and participants were not compensated for completing the study.
2.1. Measures
2.1.1. Demographic and diabetes information.
Participants completed a self-report survey to record their demographic information including age, gender identity, marital status, education level, race and ethnicity, and gross household income. Participants were also asked to self-report their diabetes type and the duration of time, in years, they have been diagnosed with diabetes.
2.1.2. Biophysical outcomes.
Hemoglobin A1c (HbA1c), body mass index (BMI), systolic and diastolic blood pressure, triglycerides, high-density lipoprotein (HDL) and low-density lipoprotein (LDL) data were extracted from the electronic medical record for each participant from the date of their clinic visit for the intervention.
2.1.3. Diabetes distress.
The Problem Areas in Diabetes Questionnaire (PAID) [14] assessed participants’ level of distress related to their diabetes, particularly related to emotion concerns, diet and diabetes complications. The PAID is widely-used in diabetes literature, has had consistent reliability and validity over the past two decades, and is more psychometrically robust relative to other measures of diabetes distress15. Participants rated from 0 (not a problem) to 4 (serious problem) on 20 items (e.g., feeling discouraged with diabetes treatment plan). Scores were added and multiplied by 1.25 to generate a total score between 0–100. Higher scores indicate greater distress, with 40 or greater indicating emotional burnout.
2.1.4. Diabetes self-efficacy.
The Self-Efficacy for Diabetes Scale[16] determined participants’ confidence in various behaviors important for diabetes management. Participants rated their confidence from 1 (not at all confident) to 100 (totally confident) on 6 items (e.g., feel that you can control your diabetes so that it does not interfere with the things you want to do). Mean scores were computed with higher scores indicating greater diabetes self-efficacy.
2.1.5. Diabetes self-care.
The Self-Care Inventory-Revised version[17] assessed participants’ self-reported engagement in behaviors to support adherence to diabetes self-care recommendations using ratings from 1 (never) to 5 (always). One item (“take diabetes pills/insulin at the right time) was missing due to an error so the total number of items in the measure were 14 for this study. Since not all individuals are treated with oral medication or insulin or recommended to check ketones and not all individuals experience low blood glucose, “not applicable or N/A” are allowed for the questions that ask about ketones, insulin, pills or treatment of carbohydrate for low blood glucose. The formula used for scoring is: . Higher mean scores indicated more frequent self-care behaviors. One item about insulin use (“If on insulin: adjust insulin dosage values, food, and exercise”) was used to dictotomised those who were using insulin (i.e., responses 1–5 were classified as “yes”) and those who were not (i.e., response of 6-“not on insulin” was categorized as “no”).
2.1.6. Support Mismatch (i.e., support deficits and surpluses).
Participants’ perception of support desired and received were measured using Diabetes Care Profile.[18] Participants rated 1 (strongly disagree) to 5 (strongly agree) on six domains (e.g., following a meal plan, take medicine). For each domain, participants indicated the extent to which they wanted help from their family and friends (i.e., support desired) and the extent to which they perceived that their family and friends supported them (i.e., support received). A mean score was computed across all items. Similar to an approach utilized by previous research10, we assessed support mismatch by computing a difference score resulted from subtracting perceptions of support received mean scores from perceptions of support desired mean scores. Support mismatch scores were dichotomized for the main analyses into perceptions of support deficits (M = 0.68, SD = 0.85, actual range = 0 – 4) and support surpluses (M = 0.48, SD = 0.66, actual range = 0 – 3). Additional details on the support survey items and scoring are located in Appendices Table A.1.
2.2. Data analysis
Analyses were conducted using SPSS (version 26 for Windows). Descriptive statistics were conducted for participant demographic and clinical characteristics, and main outcomes. The frequencies for perceived support match and mismatch (i.e., support deficits and support surpluses) based on percentage were also analyzed. Associations between support deficits, support surpluses, biophysical, psychosocial, and self-care outcomes were examined using bivariate correlations. A series of multiple linear regression analyses were then conducted to test significant associations while accounting for demographic and clinical characteristics. Model 1 included demographic and clinical characteristics. Model 2 added perceived support. In consideration of the differential impact of diabetes burden, type of diabetes was entered into the main regression analyses and supplemental analyses included self-reported insulin treatment in Model 1. The results section will summarize the results of the supplemental analyses in text only. Statistical significance was determined by a p –value < .05.
3. Results
3.1. Sample characteristics
Most participants reported that they had a diagnosis of Type 2 diabetes (n = 162; 81%). The mean age of the sample was approximately 57 years old (range = 18–87), 59% reported being female, and 83% reported that they were White. Additional sociodemographic information for the overall sample and by type of diabetes is reported in Table 1. Participants’ mean HbA1c was 8.2 % ± 2.1 % and mean diabetes duration was approximately 12 years. Descriptive statistics for biophysical outcomes and psychosocial and self-care outcomes are further described in Table 2. Some significant differences by type of diabetes were found where participants with Type 2 diabetes reported older age, shorter diabetes duration, higher BMI, higher systolic blood pressure, higher triglycerides, lower HDL, and poorer self-care compared to participants with Type 1 diabetes.
Table 1.
Demographic Characteristics of Participants
| Type 1 Diabetes n = 38 |
Type 2 Diabetes n = 162 |
Total N = 200 |
p-value | |
|---|---|---|---|---|
| Age, mean (standard deviation) | 41.0 (17.43) | 60.54 (12.76) | 56.8 (15.7) | < .001 |
| Gender, no. (%)* | 1.00 | |||
| Male | 15 (39.5) | 66 (41.3) | 81 (41) | |
| Female | 23 (60.5) | 94 (58.8) | 1127 (59) | |
| Marital status, no. (%)* | .07 | |||
| Married or domestic partnership | 16 (42.1) | 94 (59.5) | 110 (56) | |
| Single/divorced/widowed/other | 22 (57.9) | 64 (40.5) | 88 (44) | |
| Education level, no. (%)* | .03 | |||
| ≤ High school degree or technical, trade, or vocational diploma | 12 (31.6) | 37 (23.0) | 19 (25) | |
| Some college | 15 (39.5) | 39 (24.2) | 54 (27) | |
| Associate’s or Bachelor’s degree | 7 (18.4) | 58 (36.0) | 65 (33) | |
| Master’s degree | 4 (10.5) | 20 (12.4) | 24 (12) | |
| Professional degree or Doctorate | 0 (0.0) | 7 (4.3) | 7 (4) | |
| Race & Ethnicity, no. (%) | ||||
| White | 34 (85.0) | 137 (83.0) | 171 (83.4) | .61 |
| Black or African American | 0 (0.0) | 7 (4.2) | 7 (3.4) | .35 |
| Asian or Asian American | 2 (5.0) | 3 (1.8) | 5 (2.4) | .36 |
| American Indian or Alaskan Native | 0 (0.0) | 8 (4.8) | 8 (3.9) | .24 |
| Native Hawaiian or Pacific Islander | 0 (0.0) | 1 (0.6) | 1 (0.5) | 1.00 |
| Other | 1 (2.5) | 2 (1.2) | 3 (1.5) | .47 |
| Prefer not to answer | 3 (7.5) | 7 (4.2) | 10 (4.9) | .40 |
| Hispanic or Latin/o/a/x of any race | 1 (7.9) | 24 (15.0) | 25 (12.5) | .05 |
| Gross Household Income, no. (%) | .77 | |||
| ≤ $39,999 | 15 (39.5) | 57 (35.2) | 72 (36) | |
| $40,000-$79,999 | 9 (23.7) | 36 (22.2) | 45 (23) | |
| ≥ $80,000 | 6 (15.8) | 41 (25.3) | 47 (24) | |
| Prefer to not answer | 8 (21.1) | 28 (17.3) | 36 (18) |
Note. For continuous outcomes, independent samples t-tests were used and for dichotomous outcomes, Fisher’s exact tests were used to assess significant differences between participants with Type 1 and Type 2 diabetes.
Data were missing for participants with Type 2 diabetes as follows: age (n=1), gender (n=3), marital status (n=3), and education (n=2).
Table 2.
Participant Clinical Characteristics and Diabetes Outcomes
| Type 1 Diabetes | Type 2 Diabetes | Total* | p-value* | |
|---|---|---|---|---|
| Diabetes duration | n = 38 | n = 155 | n = 193 | |
| Mean (SD) | 17.18 (15.81) | 10.41 (8.19) | 11.7 years (11.0) | .02 |
| Insulin, no. (%) | n = 38 | n = 150 | n = 188 | < .001 |
| Yes | 38 (100) | 82 (54.7) | 120 (63.8) | |
| No | 0 (0) | 68 (45.3) | 68 (36.2) | |
| Biophysical Outcomes | ||||
| Hemoglobin A1C | n = 36 | n = 150 | n = 186 | .92 |
| Mean (SD) | 8.23 (2.03) | 8.19 (2.10) | 8.2 (2.1) | |
| Body mass index | n = 36 | n = 155 | n = 191 | <.001 |
| Mean (SD) | 28.21 (7.24) | 35.05 (8.39) | 33.7 (8.6) | |
| Systolic blood pressure | n = 36 | n = 155 | n = 191 | <.001 |
| Mean (SD) | 117.67 (14.29) | 125.62 (12.04) | 124.1 (12.8) | |
| Diastolic blood pressure | n = 36 | n = 155 | n = 191 | .18 |
| Mean (SD) | 73.83 (10.02) | 76.15 (9.23) | 75.7 (9.4) | |
| Triglycerides | n = 29 | n = 121 | n = 150 | <.001 |
| Mean (SD) | 113.41 (66.25) | 197.15 (145.72) | 181.0 (137.9) | |
| High-density lipoprotein | n = 29 | n = 121 | n = 150 | .02 |
| Mean (SD) | 57.41 (25.73) | 45.08 (15.22) | 47.5 (18.3) | |
| Low-density lipoprotein | n = 30 | n = 121 | n = 151 | .31 |
| Mean (SD) | 99.83 (51.69) | 91.15 (39.27) | 92.9 (42.0) | |
| Psychosocial and Self-Care Outcomes | ||||
| Diabetes distress | n = 35 | n = 150 | n = 190 | .74 |
| Mean (SD) | 35.29 (23.2) | 36.61 (21.1) | 36.20 (21.3) | |
| α | .95 | .95 | .95 | |
| Diabetes self-care | n = 36 | n = 146 | n = 186 | <.001 |
| Mean (SD) | 59.50 (16.27) | 50.34 (14.32) | 52.2 (15.3) | |
| α | .83 | .72 | - | |
| Diabetes self-efficacy | n = 35 | n = 153 | n = 188 | .23 |
| Mean (SD) | 69.66 (14.99) | 65.93 (21.17) | 66.6 (20.2) | |
| α | .79 | .86 | .85 | |
Note. For diabetes duration, a continuous score was entered such that participants who had diabetes for < 6 months were coded as 0, participants with duration between 6 months and 1 year were coded as 1, and so on. Independent samples t-tests or chi-square tests (for dichotomous variables) were used to evaluate significant differences between participants with Type 1 and Type 2 diabetes.
3.2. Frequency of Support Match and Mismatch
The percentages of participants experiencing support match and mismatch (support surpluses and deficits) across the six domains of diabetes support are displayed in Figure 1. Roughly half of the participants experienced at least one type of support mismatch. Particularly, for each domain, the percentage of participant perceptions of support mismatch in each domain as follows: 52% in following a meal plan, 46% in taking medicine, 42% in care of feet, 50% in physical activity, 46% in testing blood sugar, and 49% in handling feelings about diabetes. Of these, 23% to 34% of participants had support deficits in which they perceived that they received less support than they reported they desired (see Figure 1 for details). In particular, participants reported the highest support deficits, relative to support surpluses, for domains related to following a meal plan, help with handling their feelings about diabetes, and help with getting enough physical activity.
Figure 1.
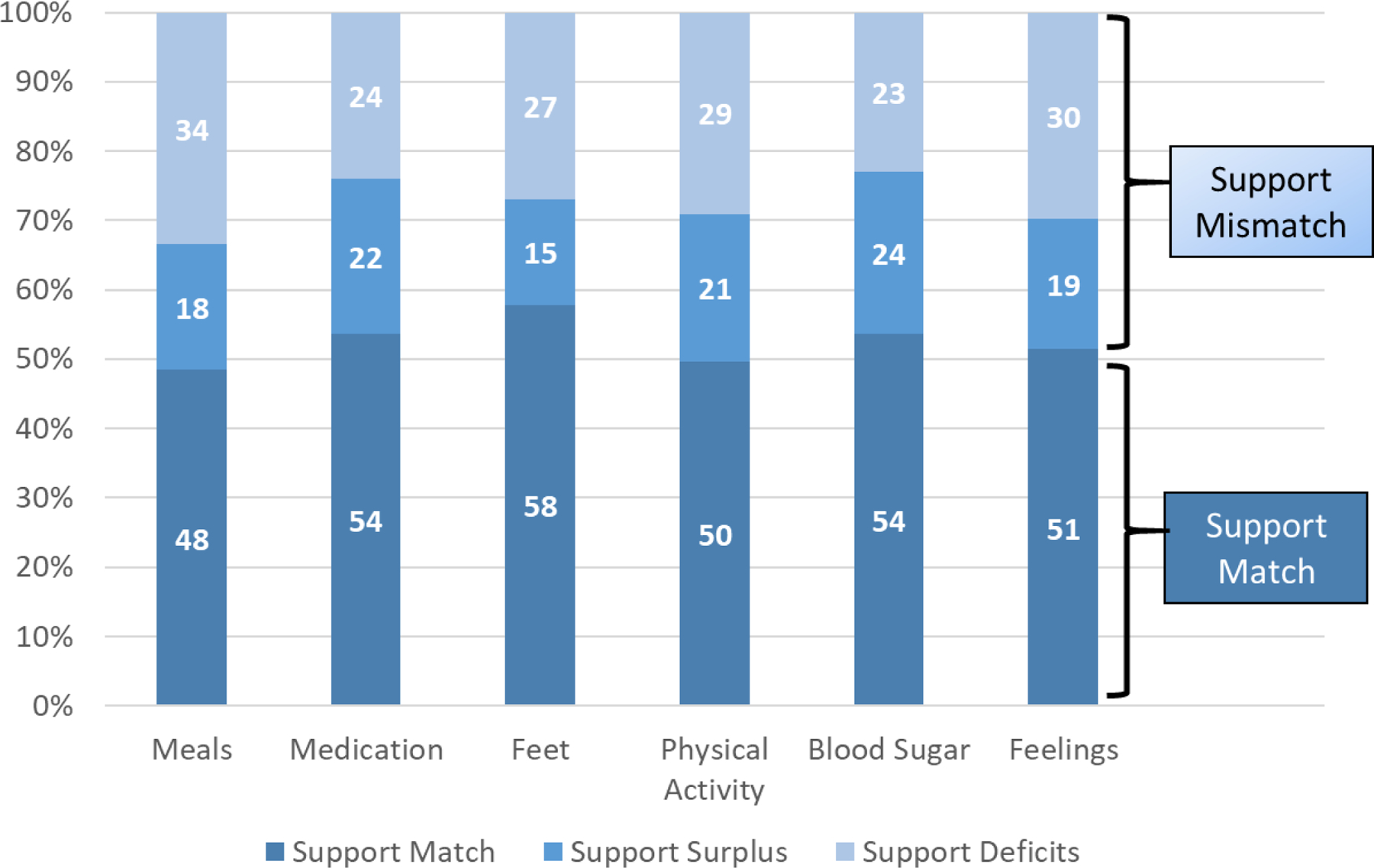
Frequency of Support Match and Mismatch by Self-Care Domain
3.3. Bivariate correlations among key study variables
Table 3 shows the correlations between perceived support deficits, support surpluses, biophysical, and psychosocial outcomes. Participants who reported higher levels of perceived support deficits were significantly more likely to have a higher HbA1C (r = .24, p = .011), higher BMI (r = .23, p = .01), higher triglycerides (r = .24, p = .02), higher LDL levels (r = .25, p = .02), higher diabetes distress (r = .37, p < .001) and lower diabetes self-efficacy (r = −.27, p = .004). No significant associations were found with perceived support deficits and blood pressure, HDL, or diabetes self-care. Support surpluses were not significantly associated with any key study outcomes. Table A.2 also includes bivariate correlations with perceived support deficits and support surpluses and demographic and clinical characteristics. Women (r = .20, p = .03) and participants who reported using insulin (r =.21, p = .02) reported greater support deficits. No significant associations were found with perceived support surpluses.
Table 3.
Correlations between Support Deficits, Support Surplus, Biophysical and Psychosocial Outcomes
| Support deficits | Support surplus | HbA1c | BMI | Systolic blood pressure | Diastolic blood pressure | Triglycerides | High-density lipoprotein | Low-density lipoprotein | Diabetes distress | Diabetes self-care | Diabetes self-efficacy | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Support deficits | -- | -- | ||||||||||
| Support surplus | -- | -- | ||||||||||
| Hemoglobin A1c | 0.24** | 0.05 | -- | |||||||||
| Body mass index | 0.23** | 0.10 | 0.01 | -- | ||||||||
| Systolic blood pressure | 0.03 | 0.03 | −0.05 | 0.17* | -- | |||||||
| Diastolic blood pressure | 0.04 | 0.05 | 0.06 | 0.15v | 0.48*** | -- | ||||||
| Triglycerides | 0.24* | −0.12 | 0.19* | 0.32*** | 0.11 | 0.14 | -- | |||||
| High-density lipoprotein | −0.13 | −0.04 | −0.10 | −0.25** | 0.00 | −0.04 | −0.24** | -- | ||||
| Low-density lipoprotein | 0.25* | −0.03 | 0.21* | 0.06 | 0.07 | 0.30*** | 0.17* | 0.05 | -- | |||
| Diabetes distress | 0.37*** | 0.15 | 0.17* | 0.18* | −0.01 | 0.14 | 0.30*** | −0.02 | 0.09 | -- | ||
| Diabetes self-care | −0.14 | 0.04 | −0.15 | −0.29*** | −0.06 | −0.16* | −0.19* | 0.09 | −0.11 | −.19** | -- | |
| Diabetes self-efficacy | −0.27** | −0.07 | −0.18* | −0.29*** | 0.04 | −0.10 | −0.14 | −0.04 | −.198* | −.037*** | 0.36*** | -- |
Note. Correlation is significant at the 0.001 level;
Correlation is significant at the 0.01 level (2-tailed);
Correlation is significant at the 0.05 level (2-tailed). Hemoglobin A1c= HbA1c, Body mass index = BMI.
3.4. Linear regressions among key outcomes
Based on the significant bivariate correlations, six hierarchical regression models were conducted to assess whether support deficits were significantly associated with HbA1c, BMI, triglycerides, LDL, diabetes distress, and diabetes self-efficacy, after controlling for participant characteristics (e.g., age, gender, race, diabetes type, and diabetes duration). Table 4 presents each regression model.
Table 4.
Six Multivariable Linear Regression Models to Assess with Association between Support Deficits and Key Outcomes
|
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HbA1c | BMI | Triglycerides | LDL | Diabetes Distress | Diabetes Self-Efficacy | |||||||||||||
|
|
||||||||||||||||||
| B | SE | p | B | SE | p | B | SE | p | B | SE | p | B | SE | p | B | SE | p | |
| Model 1 | F (9, 97) = 1.30, p = .25, R2 = .10 | F (8, 101) = 3.86, p < .001, R2 = .23 | F (8, 76) = 1.87, p = .08, R2 = .08 | F (8, 76) = 1.22, p = .30, R2 = .11 | F (8, 06) = 3.08, p < .001, R2 = .27 | F (8, 104) = 3.02, p = .004, R2 = .19 | ||||||||||||
|
| ||||||||||||||||||
| Age | −0.04 | 0.02 | 0.02 | −0.15 | 0.07 | 0.02 | −2.54 | 1.33 | 0.06 | −0.54 | 0.33 | 0.11 | −0.03 | 0.01 | <.001 | 0.40 | 0.16 | 0.01 |
| Female | 0.21 | 0.47 | 0.65 | 2.81 | 1.66 | 0.09 | 41.50 | 34.70 | 0.24 | 13.68 | 8.56 | 0.11 | 0.40 | 0.16 | 0.01 | −8.13 | 3.94 | 0.04 |
| White | 0.11 | 0.78 | 0.89 | 6.95 | 2.71 | 0.01 | 114.18 | 65.06 | 0.08 | 6.44 | 16.05 | 0.69 | −0.22 | 0.25 | 0.37 | 3.36 | 6.21 | 0.59 |
| Married | −0.10 | 0.53 | 0.84 | 0.85 | 1.88 | 0.65 | −3.32 | 39.11 | 0.93 | 0.13 | 9.65 | 0.99 | 0.04 | 0.17 | 0.82 | 6.94 | 4.43 | 0.12 |
| Education | 0.04 | 0.22 | 0.86 | 0.13 | 0.79 | 0.87 | 2.95 | 16.58 | 0.86 | 4.03 | 4.09 | 0.33 | 0.00 | 0.07 | 0.98 | −0.08 | 1.83 | 0.97 |
| Income | −0.20 | 0.26 | 0.44 | −1.34 | 0.94 | 0.16 | 4.44 | 19.23 | 0.82 | −4.79 | 4.74 | 0.32 | −0.10 | 0.09 | 0.27 | 1.22 | 2.18 | 0.58 |
| Type 2 diabetes | 0.78 | 0.69 | 0.26 | 10.66 | 2.52 | <.001 | 119.46 | 49.56 | 0.02 | 5.43 | 12.23 | 0.66 | 0.20 | 0.24 | 0.40 | −9.45 | 5.94 | 0.12 |
| Diabetes duration | 0.03 | 0.02 | 0.18 | 0.04 | 0.08 | 0.66 | −0.88 | 1.75 | 0.62 | −0.22 | 0.43 | 0.60 | −0.01 | 0.01 | 0.56 | 0.17 | 0.20 | 0.41 |
|
| ||||||||||||||||||
| Model 2 | F (9, 96)=21.59, p=.13; R2Δ =.03, p=.06 | F (9, 100) = 3.85, p<.001; R2Δ = .02, p=.08 | F (9, 75)= 2.25, p=.03; R2Δ = .05, p=.04 | F (9, 84) = 1.48, p =.04; R2Δ = .05, p = .08 | F (9, 05) =6.89, p < .001; R2Δ = .10, p < .001 | F (9, 103) = 3.52, p < .001; R2Δ=.05, p=.004 | ||||||||||||
|
| ||||||||||||||||||
| Age | −0.04 | 0.02 | 0.05 | −0.13 | 0.07 | 0.05 | −2.13 | 1.31 | 0.11 | −0.45 | 0.33 | 0.17 | −0.02 | 0.01 | <.001 | 0.33 | 0.16 | 0.04 |
| Female | −0.01 | 0.47 | 0.99 | 2.16 | 1.68 | 0.20 | 24.26 | 34.85 | 0.49 | 10.06 | 8.67 | 0.25 | 0.27 | 0.15 | 0.08 | −5.77 | 3.95 | 0.15 |
| White | 0.09 | 0.77 | 0.91 | 6.86 | 2.68 | 0.01 | 109.61 | 63.61 | 0.09 | 5.48 | 15.82 | 0.73 | −0.20 | 0.23 | 0.39 | 3.02 | 6.06 | 0.62 |
| Married | 0.03 | 0.52 | 0.96 | 1.19 | 1.87 | 0.53 | 2.45 | 38.31 | 0.95 | 1.34 | 9.53 | 0.89 | 0.13 | 0.16 | 0.44 | 5.24 | 4.38 | 0.23 |
| Education | 0.05 | 0.22 | 0.83 | 0.15 | 0.78 | 0.85 | 4.10 | 16.21 | 0.80 | 4.27 | 4.03 | 0.29 | 0.01 | 0.07 | 0.84 | −0.28 | 1.79 | 0.87 |
| Income | −0.27 | 0.26 | 0.31 | −1.52 | 0.93 | 0.11 | 1.01 | 18.86 | 0.96 | −5.51 | 4.69 | 0.24 | −0.14 | 0.08 | 0.08 | 2.15 | 2.16 | 0.32 |
| Type 2 diabetes | 0.52 | 0.70 | 0.46 | 9.82 | 2.54 | <.001 | 99.22 | 49.34 | 0.05 | 1.19 | 12.27 | 0.92 | 0.05 | 0.23 | 0.82 | −7.09 | 5.87 | 0.23 |
| Diabetes duration | 0.02 | 0.02 | 0.39 | 0.01 | 0.09 | 0.95 | −1.71 | 1.75 | 0.33 | −0.40 | 0.44 | 0.36 | −0.01 | 0.01 | 0.12 | 0.28 | 0.20 | 0.18 |
| Support deficits | 0.52 | 0.27 | 0.06 | 1.72 | 0.97 | 0.08 | 40.09 | 18.70 | 0.04 | 8.40 | 4.65 | 0.08 | 0.36 | 0.09 | <.001 | −5.67 | 2.26 | 0.01 |
Note: Bold text indicates significant associations. Categories were coded as follows: Female (0 = male, 1 = female), White (0 = underrepresented minority, 1 = White), Married (0 = single, divorced, separated, widowed, 1 = married or living with partner); Type 2 diabetes (0 = Type 1 diabetes, 1 = Type 2 diabetes). Unstandardized coefficients are presented.
3.4.1. Models with diabetes type.
In Model 1, older age was associated with lower A1c, lower BMI, lower diabetes distress, and higher diabetes self-efficacy. Women reported higher diabetes distress and lower diabetes self-efficacy. Participants who were White had higher BMI. Participants with Type 2 diabetes had higher BMI and triglycerides levels.
After accounting for demographic and clinical characteristics, greater perceived support deficits were significant associated with higher triglyceride levels (R2 Δ = .05, p = .04), diabetes distress (R2 Δ = .10, p < .001), and diabetes self-efficacy (R2 Δ = .05, p = .004). Support deficits were not significantly associated with A1c (R2 Δ = .03, p = .06), BMI (R2 Δ = .02, p = .08), or LDL (R2 Δ = .05, p = .08).
3.4.2. Supplemental analyses with insulin (Appendix, Table A.3).
In Model 1, older age was associated with lower diabetes distress, and higher diabetes self-efficacy. Women reported lower diabetes self-efficacy.
After accounting for demographic and clinical characteristics, greater perceived support deficits were significant associated with higher BMI (R2 Δ = .04, p =.03), higher triglyceride levels (R2 Δ = .07, p =.02), diabetes distress (R2 Δ = .11, p < .001), and diabetes self-efficacy (R2 Δ = .06, p = .007). Support deficits were not significantly associated with A1c (R2 Δ = .03, p =.08) or LDL (R2 Δ = .04, p =.07).
4. Discussion and conclusion
4.1. Discussion
This study examined the association between support mismatch (i.e., support surpluses and deficits) and biophysical and psychosocial health and self-care of people with diabetes. Support mismatch was found to be a relatively common issue faced by individuals with diabetes. Between 42% to 52% of participants in this study reported experiencing support mismatch across six domains; with 23% to 34% reporting perceptions of support deficits in their diabetes management (i.e., they received less support then they desired). Support deficits, in particular, was correlated with poorer biophysical and psychosocial outcomes. Women and insulin-using participants also reported greater support deficits. Support surpluses were not significantly related to any key study outcomes. After accounting for demographic and clinical characteristics, those who perceived greater support deficits had higher triglyceride levels, greater diabetes distress, and lower diabetes self-efficacy. The regression models that controlled for insulin use (instead of type of diabetes) had similar findings, except that in addition to the aforementioned associations, perceptions of greater support deficits were also associated with higher BMI. Together, these findings highlight the potential that individuals with living with diabetes who perceive support deficits may be at a greater risk for some negative biophysical and psychosocial health outcomes. These findings shed light on the importance of the concordance of desired and received support in diabetes management[11–13] and align with dyadic coping concepts found in theoretical frameworks.[12]
Our study adds to social support literature by moving beyond studying only perceived support available to exploring the mismatch between perceptions of received and desired support. By focusing on the gap between perceptions of received and desired support, we were able to examine the nuances of the associations between support deficits, support surpluses, and health in the context of diabetes. Our findings are consistent with previous research in that the alignment of individuals’ perceptions of desired and received support has implications on individuals’ physical (e.g., self-care activities) and psychosocial health (e.g., anxiety, depressive symptoms) across different health domains (e.g., diabetes, cancer).[7,9,18,19]
4.1.1. Support deficits versus surpluses.
Correlations indicated that perceived support deficits were significantly associated with important diabetes-related outcomes (i.e., A1c, BMI, triglycerides, distress, and self-efficacy), while perceived support surpluses were not correlated with any outcomes. Literature on the implications of support surpluses (i.e., perceptions of receiving more support than wanted) has generated mixed findings. Some research concluded that more support is not always better, as support surpluses have detrimental effects on patients’ psychological adjustment19. Other research8 indicated that support surpluses were not problematic and did not have significant effects on patients’ psychosocial functioning (e.g., anxiety and depression symptoms)9. In the current study, we did not find any significant associations between perceived support surpluses and any of the biophysical and psychosocial outcomes. A few reasons may account for the insignificant findings. First, the sample size of patients who perceived to experience support surpluses is small, potentially limiting the power to detect significant associations. Second, given that diabetes is a chronic illness, receiving support from family and friends may be routine for some patients. Thus, their perceptions of receiving more support than desired may not be problematic in a way that impedes their diabetes management8,23.
4.1.2. Support deficits and individual characteristics.
Findings suggested that women and people using insulin reported greater support deficits. These findings are consistent with previous literature. Women with diabetes often receive less perceived support than men with diabetes24–26. Other studies have also found that people living with Type 2 diabetes who were in insulin-dependent perceived less family social support than those with noninsulin-dependent diabetes25.
4.1.3. Support deficits and biophysical outcomes.
Research that has examined support mismatch among people living with diabetes has mostly been with people who had Type 2 diabetes and focused on diabetes self-care and mental health outcomes8,10. This study adds to the literature by including people with Type 1 and Type 2 diabetes and is one of the first to examine the associations between support deficits and biophysical outcomes, including HbA1c, BMI, and triglycerides levels. Greater perceptions of support deficits were correlated with higher HbA1c, BMI, triglycerides, and LDL levels, but not blood pressure or HDL levels. There may be a few explanations underlying associations between perceived support deficits and biophysical health outcomes. Social networks can provide key information related to diabetes treatment, which in turn can support self-care behaviors that lead to positive health outcomes.[20] Perceptions of receiving less support than desired, where individuals aren’t getting their desired informational or emotional support, may lead to information deficits and/or creating additional stressors related to diabetes management—thereby having a cascading impact on health outcomes.
After controlling for demographic and clinical characteristics, associations only remained between support deficits and triglyceride levels and BMI (only in the insulin-use model). The survey items within the support scale could have influenced different associations with biophysical outcomes. BMI and triglyceride levels are impacted by diet and physical activity27. Therefore, lacking support in relation to those specific domains could have more of an impact on BMI and triglyceride levels. Future studies should continue to explore the association with support deficits and biophysical outcomes by looking at other diabetes management domains.
4.1.4. Support deficits and psychosocial outcomes.
The current study had different findings from other studies8 that examined associations between support deficits and psychosocial outcomes. We found that perceived support deficits were associated with greater diabetes distress and lower diabetes self-efficacy in correlational and regression analyses. Social support may reduce perceived stress and help individuals more efficaciously cope with stressful events related to their chronic disease, manage stress of their treatment regimen, and buffer negative effects of stress on their overall health.[21] People living with diabetes who are experiencing support deficits, where they perceive they are not receiving the support they would like, could likely benefit from support interventions to lower their distress and improve confidence in diabetes management28. These findings differ from a study of people living with Type 2 diabetes in which there was no association between support deficits and depressive symptoms8. Using surveys that specifically address diabetes-related psychosocial outcomes may offer more insight into the stressors that people living with diabetes experience.
4.1.5. Support deficits and diabetes self-care.
Our study did not find significant correlations between support deficits and diabetes self-care. These findings are contrary to two studies that found greater support deficits were associated with poorer self-care management8,10 [8, 10]. Differences in findings with past studies could be related to methodological (e.g., measures of self-care and support deficits) or study sample differences (e.g., other studies only had participants with Type 2 diabetes). Our study sample of people with Type 1 diabetes who reported perceiving support deficits (n =19) was too small to drawn conclusions. Additional research is needed to assess potential differences based on type of diabetes and test replicability of findings using consistent survey measures.
Despite the abovementioned contributions, findings from the current research need to be interpreted considering some limitations. First, the nature of the data is cross-sectional and retrospective; therefore, there is insufficient evidence to establish causal links or directional relationships among the studied variables. Second, the data collected does not offer insights into the different types of support (e.g., emotional, instrumental, informational) people with diabetes receive and desire. There is also no standard approach to measure support mismatch. Additional studies have considered other approaches, such as using participant- and family-reported actual and desired support to examine communal coping among those living with diabetes8. The ability to examine the experiences of family members of people with diabetes can provide additional insights into their preferences for providing support and impact on their own health34. Third, data about participants’ identification of their primary source of support (e.g., spouse, friend) and the sources’ perspectives of support provision were not collected. Fourth, there are different measures of diabetes distress, such as the Diabetes Distress Scale35, that focuses more on physician-related distress and self-management behaviors. Future studies should explore support deficits in relation to different measures of diabetes distress. Finally, the sample sizes of participants with Type 1 diabetes and Type 2 diabetes were uneven, limiting our ability to examine if participants’ support deficits and diabetes management differ based on the type of their diabetes In our sample, patients with Type 1 diabetes were significantly younger, had longer diabetes duration, had lower BMI, blood sugar, and Triglycerides, and reported greater diabetes self-care compared with those with Type 2 diabetes. As indicated in previous research1, possibly due to age at diagnosis and diabetes duration, patients with Type 1 diabetes may have more access to support from family and friends for diabetes management and thus experience diabetes distress differently than those with Type 2 diabetes. Future research should consider exploring the different experiences of patients with Type 1 diabetes in particular given a lack of research within this population.
4.2. Conclusion
Our study demonstrates the prevalence of the mismatch between desired and received support perceived by people with diabetes. It also reveals the significant associations between support deficits and biophysical and psychosocial health of those with diabetes. Findings from our study offer empirical evidence for designing intervention programs that can ensure patients receive adequate and high-quality support they need during diabetes management.
4.3. Practice implications
In addition to theoretical contributions to the literature of social support and health outcomes, several practical implications can be gleaned from the current study to inform clinical care. First, given the prevalence of support mismatch perceived by participants with diabetes in our sample, tools in the form of pre-visit questionnaires and visit check-ins can be developed to identify patients experiencing support mismatch.[19] Support deficits can be addressed during clinic visits through provider discussions leading to an understanding of helpful interventions such as referrals to social work or therapy.[22,23] Intervention programs can be designed for support providers to assist care partners with identifying the patient’s thresholds of support needs and thus tailoring their support provision.[34 24,25,26] Clinical interventions could also target women and patients with diabetes that are insulin-dependent to improve support as well, given our findings that they were more likely to perceived deficits in support.
An important avenue for future research practices and clinical care would be identifying patients with support deficits and designing interventions to facilitate functional, supportive behaviors, such as family-based interventions to engage individuals who might offer sources of support based on their abilities and strengths. Future research should also continue to examine how those without family and/or friend support may particularly benefit from diabetes-specific online peer support.[36] Additional exploration of the congruency between people with diabetes and their care partners’ perception of support provided and support received will be beneficial when developing dyadic intervention strategies.
Supplementary Material
Acknowledgements and Funding Sources
We would like to acknowledge funding support from the Driving Out Diabetes Larry H. Miller Family Wellness Initiative and Larry H. and Gail Miller Family Foundation.
References
- 1.Beverly EA, Ritholz MD, Dhanyamraju K. The buffering effect of social support on diabetes distress and depressive symptoms in adults with Type 1 and Type 2 diabetes. Diabet Med Apr 2021;38(4):e14472. doi: 10.1111/dme.14472 [DOI] [PubMed] [Google Scholar]
- 2.Strom JL, Egede LE. The impact of social support on outcomes in adult patients with type 2 diabetes: a systematic review. Curr Diab Rep Dec 2012;12(6):769–81. doi: 10.1007/s11892-012-0317-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reyes J, Tripp-Reimer T, Parker E, Muller B, Laroche H. Factors influencing diabetes self-management among medically underserved patients with type II diabetes. Glob Qual Nurs Res 2017;4:1–13. doi: 10.1177/2333393617713097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wagner EH. Chronic disease management: What will it take to improve care for chronic illness? Eff Clin Pract 1998;1(1):1–4. [PubMed] [Google Scholar]
- 5.Khan CM, Stephens MA, Franks MM, Rook KS, Salem JK. Influences of spousal support and control on diabetes management through physical activity. Health Psychol Jul 2013;32(7):739–47. doi: 10.1037/a0028609 [DOI] [PubMed] [Google Scholar]
- 6.Presley CA, Mondesir FL, Juarez LD, et al. Social support and diabetes distress among adults with type 2 diabetes covered by Alabama Medicaid. Diabet Med Apr 2021;38(4):e14503. doi: 10.1111/dme.14503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vodermaier A, Linden W. Social support buffers against anxiety and depressive symptoms in patients with cancer only if support is wanted: a large sample replication. Supportive Care in Cancer 2019;27(7):2345–2347. doi: 10.1007/s00520-019-04737-w [DOI] [PubMed] [Google Scholar]
- 8.Basinger ED, Caughlin JP, Wang N. Examining discrepancies between actual and desired communal coping with type 2 diabetes. Personal Relationships 2018;25(4):538–564. doi: 10.1111/pere.12259 [DOI] [Google Scholar]
- 9.Linden W, Vodermaier A. Mismatch of desired versus perceived social support and associated levels of anxiety and depression in newly diagnosed cancer patients. Support Care Cancer Jul 2012;20(7):1449–56. doi: 10.1007/s00520-011-1228-3 [DOI] [PubMed] [Google Scholar]
- 10.Song Y, Song HJ, Han HR, Park SY, Nam S, Kim MT. Unmet needs for social support and effects on diabetes self-care activities in Korean Americans with type 2 diabetes. Diabetes Educ Jan-Feb 2012;38(1):77–85. doi: 10.1177/0145721711432456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Helgeson VS, Berg CA, Kelly CS, et al. Patient and partner illness appraisals and health among adults with type 1 diabetes. J Behav Med 2019;42(3):480–492. doi: 10.1007/s10865-018-0001-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Falconier MK, Kuhn R. Dyadic coping in couples: A conceptual integration and a review of the empirical literature. Front Psychol 2019;10:571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berg CA, Helgeson VS, Tracy EL, et al. Daily illness appraisal and collaboration in couples with type 1 diabetes. Health Psychol 2020;39(8):689. [DOI] [PubMed] [Google Scholar]
- 14.Welch GW, Jacobson AM, Polonsky WH. The problem areas in diabetes scale. An evaluation of its clinical utility. Diabetes Care May 1997;20(5):760–766. doi: 10.2337/diacare.20.5.760 [DOI] [PubMed] [Google Scholar]
- 15.Fenwick EK, Rees G, Holmes-Truscott E, Browne JL, Pouwer F, Speight J. What is the best measure for assessing diabetes distress? A comparison of the Problem Areas in Diabetes and Diabetes Distress Scale: results from Diabetes MILES–Australia. Journal of Health Psychology 2018;23(5):667–680. doi: 10.1177/1359105316642006 [DOI] [PubMed] [Google Scholar]
- 16.Lorig K, Ritter PL, Villa FJ, Armas J. Community-based peer-led diabetes self-management: a randomized trial. Diabetes Educ Jul-Aug 2009;35(4):641–51. doi: 10.1177/0145721709335006 [DOI] [PubMed] [Google Scholar]
- 17.Weinger K, Butler HA, Welch GW, La Greca AM. Measuring diabetes self-care: a psychometric analysis of the Self-Care Inventory-Revised with adults. Diabetes Care Jun 2005;28(6):1346–52. doi: 10.2337/diacare.28.6.1346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fitzgerald JT, Davis WK, Connell CM, Hess GE, Funnell MM, Hiss RG. Development and validation of the Diabetes Care Profile. Eval Health Prof Jun 1996;19(2):208–30. doi: 10.1177/016327879601900205 [DOI] [PubMed] [Google Scholar]
- 19.Reynolds JS, Perrin NA. Mismatches in social support and psychosocial adjustment to breast cancer. Health Psychol Jul 2004;23(4):425–30. doi: 10.1037/0278-6133.23.4.425 [DOI] [PubMed] [Google Scholar]
- 20.Sanson-Fisher R, Girgis A, Boyes A, Bonevski B, Burton L, Cook P. The unmet supportive care needs of patients with cancer. Supportive Care Review Group. Cancer Jan 2000;88(1):226–237. doi: [DOI] [PubMed] [Google Scholar]
- 21.Griffith LS, Field BJ, Lustman PJ. Life stress and social support in diabetes: Association with glycemic control. The International Journal of Psychiatry in Medicine 1990;20(4):365–372. doi: 10.2190/APH4-YMBG-NVRL-VLWD [DOI] [PubMed] [Google Scholar]
- 22.Sarason BR, Sarason IG, Gurung RA. Close personal relationships and health outcomes. A key to the role of social support. In: Sarason BR, Duck S, eds. Personal Relationships: Implications for Clinical and Community Psychology Wiley; 2001:15–41. [Google Scholar]
- 23.Wilkinson A, Whitehead L, Ritchie L. Factors influencing the ability to self-manage diabetes for adults living with type 1 or 2 diabetes. International Journal of Nursing Studies 2014/01/01/ 2014;51(1):111–122. doi: 10.1016/j.ijnurstu.2013.01.006 [DOI] [PubMed] [Google Scholar]
- 24.van Dam HA, van der Horst FG, Knoops L, Ryckman RM, Crebolder HFJM, van den Borne BHW. Social support in diabetes: a systematic review of controlled intervention studies. Patient Education and Counseling 2005/10/01/ 2005;59(1):1–12. doi: 10.1016/j.pec.2004.11.001 [DOI] [PubMed] [Google Scholar]
- 25.Kvam SH, Lyons JS. Assessment of coping strategies, social support, and general health status in individuals with diabetes mellitus. Psychological Reports 1991;68(2):623–632. doi: 10.2466/pr0.1991.68.2.623 [DOI] [PubMed] [Google Scholar]
- 26.Rubin RR, Peyrot M. Men and diabetes: Psychosocial and behavioral issues. Diabetes Spectrum 1998 2017–10-29 1998;11(2):81. [Google Scholar]
- 27.Andrews RC, Cooper AR, Montgomery AA, et al. Diet or diet plus physical activity versus usual care in patients with newly diagnosed type 2 diabetes: the Early ACTID randomised controlled trial. The Lancet 2011/07/09/ 2011;378(9786):129–139. doi: 10.1016/S0140-6736(11)60442-X [DOI] [PubMed] [Google Scholar]
- 28.Davidson P, LaManna J, Davis J, et al. The effects of diabetes self-management education on quality of life for persons with Type 1 diabetes: A systematic review of randomized controlled trials. The Science of Diabetes Self-Management and Care 2022;48(2):111–135. doi: 10.1177/26350106211070266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kennedy A, Vassilev I, James E, Rogers A. Implementing a social network intervention designed to enhance and diversify support for people with long-term conditions. A qualitative study. Implement Sci Feb 2016;11:27. doi: 10.1186/s13012-016-0384-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Williams CL, Newman D, Hammar LM. Preliminary study of a communication intervention for family caregivers and spouses with dementia. Int J Geriatr Psychiatry Feb 2018;33(2):e343–e349. doi: 10.1002/gps.4816 [DOI] [PubMed] [Google Scholar]
- 31.Drentea P, Clay OJ, Roth DL, Mittelman MS. Predictors of improvement in social support: Five-year effects of a structured intervention for caregivers of spouses with Alzheimer’s disease. Social Science & Medicine 2006;63(4):957–967. doi: 10.1016/j.socscimed.2006.02.020 [DOI] [PubMed] [Google Scholar]
- 32.Roth DL, Mittelman MS, Clay OJ, Madan A, Haley WE. Changes in social support as mediators of the impact of a psychosocial intervention for spouse caregivers of persons with Alzheimer’s disease. Psychol Aging Dec 2005;20(4):634–44. doi: 10.1037/0882-7974.20.4.634 [DOI] [PubMed] [Google Scholar]
- 33.Mayberry LS, Berg CA, Greevy RA, et al. Mixed-methods randomized evaluation of FAMS: a mobile phone-delivered intervention to improve family/friend involvement in adults’ type 2 diabetes self-care. Ann Behav Med 2021;55(2):165–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nicolucci A, Kovacs Burns K, Holt RI, et al. Diabetes Attitudes, Wishes and Needs second study (DAWN2™): Cross‐national benchmarking of diabetes‐related psychosocial outcomes for people with diabetes. Diabetic medicine 2013;30(7):767–777. [DOI] [PubMed] [Google Scholar]
- 35.Polonsky WH, Fisher L, Earles J, et al. Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Diabetes Care 2005;28(3):626–631. [DOI] [PubMed] [Google Scholar]
- 36.Litchman ML, Walker HR, Ng AH, et al. State of the science: A scoping review and gap analysis of diabetes online communities. J diabetes Sci Technol 2019;13(3):466–492. doi: 10.1177/1932296819831042 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


