HIGHLIGHTS
-
•
We examined ICD-10-CM social determinants of health (SDOH)–related Z codes among adults with hypertension.
-
•
Documentation of SDOH-related Z codes was <4% for all the 3 insurance groups.
-
•
Documentation was higher among inpatient claims for all the 3 insurance groups.
-
•
Those with SDOH-related Z codes had more chronic conditions.
-
•
Medical expenditures were more than 1.5 times higher for those with SDOH-related Z codes.
Keywords: Z codes, social determinants of health, hypertension, ICD-10-CM, delivery of health care
Abstract
Introduction
Tracking social needs can provide information on barriers to controlling hypertension and the need for wraparound services. No recent studies have examined ICD-10-CM social determinants of health–related Z codes (Z55–Z65) to indicate social needs with a focus on patients with hypertension.
Methods
Three cohorts were identified with a diagnosis of hypertension during 2016–2017 and continuously enrolled in fee-for-service insurance through June 2021: (1) commercial, age 18–64 years (n=1,024,012); (2) private insurance to supplement Medicare (Medicare Supplement), age ≥65 years (n=296,340); and (3) Medicaid, age ≥18 years (n=146,484). Both the proportion of patients and healthcare encounters or visits with social determinants of health–related Z code were summarized annually. Patient and visit characteristics were summarized for 2019.
Results
In 2020, the highest annual documentation of social determinants of health–related Z codes was among Medicaid beneficiaries (3.02%, 0.46% commercial, 0.42% Medicare Supplement); documentation was higher among inpatient than among outpatient visits for all insurance types. Z63 (related to primary support group) was more common among commercial and Medicare Supplement beneficiaries, and Z59 (housing and economic circumstances) was more common among Medicaid beneficiaries. The 2019 total unadjusted medical expenditures were 1.85, 1.78, and 1.61 times higher for those with social determinants of health–related Z code than for those without commercial, Medicare Supplement, and Medicaid, respectively. Patients with social determinants of health–related Z code also had higher proportions of diagnosed chronic conditions. Among Medicaid beneficiaries, differences in the presence of social determinants of health–related Z code by race or ethnicity were observed.
Conclusions
Although currently underreported, social determinants of health–related Z codes provide an opportunity to integrate social and medical data and may help decision makers understand the need for additional services among individuals with hypertension.
INTRODUCTION
Social determinants of health (SDOH) refer to the social and economic conditions of daily life that can result in more social needs and therefore affect a range of health and life outcomes. Many health systems are screening and addressing patients’ social needs as part of broader strategies to improve health.1, 2, 3, 4, 5, 6 The lack of standardized, national data on social needs linked to healthcare encounters is a barrier to understanding the patterns and impacts of health system efforts.7 In late 2015, SDOH-related V codes in the ICD-9-CM system were converted to SDOH-related Z codes in the ICD-10-CM code system to indicate social and economic circumstances that are tied to social needs. Z55 (problems related to education and literacy) through Z65 (problems related to other psychosocial circumstances) are standardized for documenting considerations related to SDOH.8, 9, 10, 11
In 2019, the American Hospital Association (AHA) Coding Clinic recommended also using notes from nonphysician providers (e.g., community health workers) for documenting SDOH-related Z codes at hospitals and health systems.12 Nonphysician providers can document using SDOH-related Z codes during any type of encounter.9 SDOH-related Z codes can be an efficient and lower-cost way to share information through medical records and insurance claims among clinicians, hospitals, and health plans. The AHA and multiple professional healthcare organizations promote screening and documenting using SDOH-related Z codes in medical records.13
There are few studies examining the patterns of SDOH-related Z codes or the associations of SDOH-related Z codes with outcomes using large hospital discharge, Medicaid, or Medicare fee-for-service (FFS) data.5,7,14, 15, 16, 17 Several studies including 2 or more years of data reported increasing trends of SDOH-related Z codes over time. Nevertheless, the presence of SDOH-related Z codes (∼2% or lower) was limited in all of these studies.7,17 In addition, few studies have focused on specific electronic health record systems.18, 19, 20
Hypertension is a significant public health problem; approximately 50% of adults in the U.S. have hypertension.21 Attributable to high blood pressure, the death rate increased by 34.2%, and the number of deaths increased by 65.3% from 2009 to 2019.22 Timely diagnosis and adequate blood pressure treatment are essential for preventing adverse outcomes of hypertension, including stroke and associated disability and death.22,23
In a Centers for Medicare & Medicaid Services (CMS) study of Medicare FFS beneficiaries in 2017, hypertension was the most common condition (72%) reported among 467,136 beneficiaries with an SDOH-related Z code.16 The results of the CMS study indicate a need to consider social needs and health and that hypertension may be a particularly relevant chronic condition. No recent SDOH-related Z code studies have focused solely on patients with hypertension to better understand patterns. This study updates the literature by year and beneficiary type and by focusing on a specific chronic condition. We examined the presence of SDOH-related Z codes among patients with hypertension enrolled in commercial, Medicare Supplement, or Medicaid insurance plans and their healthcare encounters from January 1, 2018 to June 30, 2021. This research may inform larger efforts to track social need barriers to hypertension control and for providing wraparound services to improve patient care and well-being.24,25 To expand the literature on this topic we did the following:
-
1.
explored whether documentation of SDOH-related Z codes increased over time by encounter setting7,17;
-
2.
described what SDOH-related Z codes were documented; and
-
3.
described the patterns of healthcare use and patient characteristics associated with the presence of an SDOH-related Z code.5,14,15
To avoid associations with coronavirus disease 2019 (COVID-19), this analysis was conducted for 2019 because it was the most recent year before the pandemic.
METHODS
Study Population
We used the MarketScan research databases—commercial claims and encounters (CCAE), Medicare Supplement, and Medicaid—from January 1, 2016 to June 30, 2021. The CCAE contains inpatient, emergency department (ED), and outpatient claims among enrollees and their dependents from employer-sponsored commercial health insurance plans. The CCAE is collected from >300 employers, >30 health plans, and over 500 hospitals in the U.S. The Medicare Claims Database contains claims information for retirees with employer-sponsored supplemental health plans. The Medicaid data represents beneficiaries from 5 to 8 deidentified states (states vary by year). We accessed all data through Treatment Pathways, a tool to extract data through a cloud-based online query.26 All data were deidentified, and this study was exempt from review by the IRB of the Centers for Diseases Control and Prevention (Bethesda, MD).
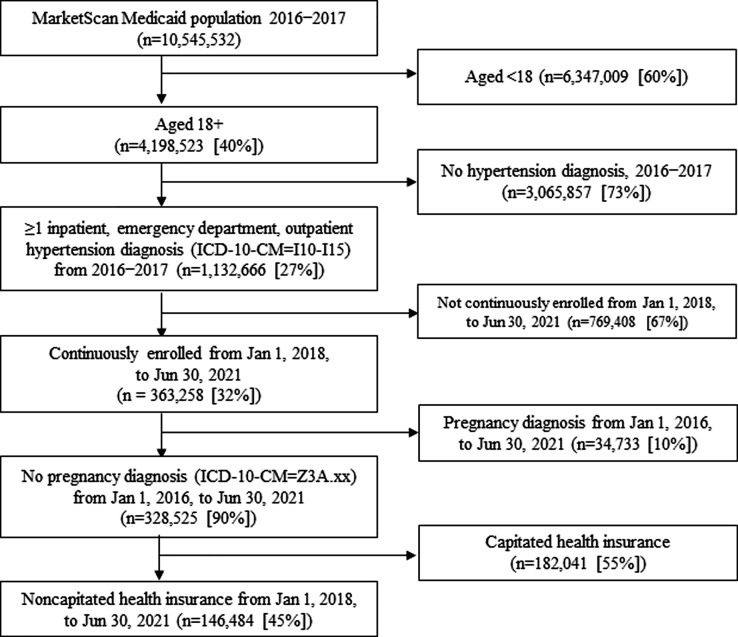
We derived 3 study cohorts that were based on beneficiaries in different insurance plans: commercial insurance, Medicare Supplemental, and Medicaid. As shown in Figures 1 and 2, we used data from January 1, 2016 through December 31, 2017 to identify our study cohorts using age and hypertension diagnoses. We used data from January 1, 2018 through June 30, 2021 for additional inclusion and exclusion criteria and for our analyses. We restricted the patients to ages 18–64 years for the commercial cohort, age ≥65 years for the Medicare cohort, and age ≥18 years for the Medicaid cohort. In addition, we included patients with at least 1 diagnosis of hypertension (ICD-10-CM) diagnosis code of I10—I1527 (Appendix Table 1, available online) and with inpatient, ED, or outpatient claims from January 1, 2016 through December 31, 2017 and continuously enrolled from January 1, 2018 through June 30, 2021 in noncapitated or FFS health insurance. The requirement for continuous enrollment in FFS health insurance was implemented for comparable healthcare use and cost patterns. Finally, to exclude patients with gestational hypertension and pregnancy-related health care, we excluded patients with a pregnancy diagnosis at any point from January 2016 through June 2021 (Appendix Table 2, available online). Our final study cohorts were commercial (n=1,024,012), Medicare Supplement (n=296,340), and Medicaid (n=146,484) (Figures 1 and 2).
Figure 1.
Study sample selection of patients diagnosed with hypertension, MarketScan Commercial Claims and Encounters Database and Medicare Supplement, January 2016–June 2021.
Note: The MarketScan Commercial Claims and Encounters Database from January 1, 2016 to June 30, 2021 are used. Inpatient, outpatient, and emergency department visits were identified using the ICD-10-CM. ICD-10-CM codes of I10–I15 were used to define the diagnosis of hypertension. ICD-10-CM codes of Z3A were used to exclude patients with pregnancy diagnoses. Patients with established hypertension were defined if there were at least 1 inpatient, emergency department, or outpatient hypertension diagnosis (ICD-10-CM=I10–I15) from January 1, 2016 to December 31, 2017. Among the patients with established hypertension with capitated and noncapitated health insurance, the trend analysis was performed from January 1, 2018 to June 30, 2021. Patients were restricted with noncapitated health insurance for the cost analysis because of inaccurate payment information in capitated health insurance. The inclusion would be as follows if the continuous enrollment at step 3 changed: continuously enrolled from January 1, 2018 to December 31, 2020: n=1,895,746 (27%) and continuously enrolled from January 1, 2018 to December 31, 2019: n=2,483,062 (35%).
Figure 2.
Study sample selection of patients diagnosed with hypertension, MarketScan Medicaid database, January 2016–June 2021.
Note: The MarketScan Medicaid Database from January 1, 2016 to December 31, 2020 are used. Inpatient, outpatient, and emergency department visits were identified using the ICD-10-CM. ICD-10-CM codes of I10–I15 were used to define the diagnosis of hypertension. ICD-10-CM codes of Z3A were used to exclude patients with pregnancy diagnoses. Patients with established hypertension were defined if there were at least 1 inpatient, emergency department, or outpatient hypertension diagnosis (ICD-10-CM=I10–I15) from January 1, 2016 to December 31, 2017. Among the patients with established hypertension with capitated and noncapitated health insurance, the trend analysis was performed from January 1, 2018 to June 30, 2021. Patients were restricted with noncapitated health insurance for the cost analysis because of inaccurate payment information in capitated health insurance. The inclusion would be as follows if the continuous enrollment at Step 3 changed: continuously enrolled from January 1, 2018 to December 31, 2020: n=377,328 (33%) and continuously enrolled from January 1, 2018 to December 31, 2019: n=428,349 (38%).
Essentially, the analysis populations were identified with hypertension from January 1, 2016 through December 31, 2017, and their subsequent healthcare encounters were examined for analysis. Thus, we required continuous enrollment for the entire time period to examine the trends in SDOH-related Z codes. We explored whether documentation increased over time for more recent years.7,17 To avoid associations with the COVID-19 pandemic or COVID-19–related disruptions, some results are presented for 2019, the most recent year before the COVID-19 pandemic.
Time points for inclusion of patients and analysis are represented as follows:
| January 1, 2016–December 31, 2017 | January 1, 2018–June 30, 2021 | |
|---|---|---|
| Inclusion criteria: | Hypertension identified and enrolled | Continued to be enrolled |
| Analysis: | Excluded | Included |
Measures
The following SDOH-related Z codes were included: Z55 (problems related to education and literacy), Z56 (problems related to employment and unemployment), Z57 (occupational exposure to risk factors), Z58 (problems related to physical environment), Z59 (problems related to housing and economic circumstances), Z60 (problems related to social environment), Z62 (problems related to upbringing), Z63 (other problems related to primary support group), Z64 (problems related to certain psychosocial circumstances), and Z65 (problems related to other psychosocial circumstances) (Appendix Table 1, available online).9
Statistical Analysis
First, to explore whether documentation of SDOH-related Z codes increased over time by encounter setting,7,17 we summarized data over time per patient and per encounter and calculated changes: (1) the proportion of unique patients with any claim with an SDOH-related Z code by insurance type was summarized by quarter from January 2018 to June 2021 (Figure 3) and (2) the proportion of encounters with SDOH-related Z codes by insurance type was stratified by settings and summarized by quarter from January 2018 to June 2021 (Figure 4, Figure 5, Figure 6). Overall differences between groups within insurance type and between insurance types were evaluated using a 2-proportion Z-test. To quantify the change over time, the percentage change was calculated for each group and presented with the trends as follows:
where a higher percentage indicates that there was a larger increase over time in the proportion of healthcare encounters where SDOH-related Z codes were documented. Second, to describe what SDOH-related Z codes were documented, the proportion of SDOH-related Z codes by SDOH domain and insurance type was summarized by year from 2018 to 2020 (Table 2).
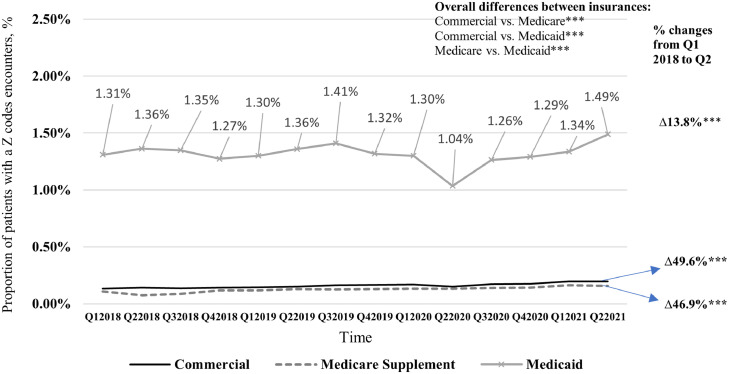
Figure 3.
Proportion of patients with an SDOH-related Z code encounter, among patients with established hypertension by insurance type, MarketScan Commercial Claims and Encounters, Medicare Supplement, and Medicaid Database, Quarter 1, 2018 through Quarter 2, 2021.
Note: On the Y-axis, we report the proportion of patients with an SDOH-related Z code encounter among patients with established hypertension. There are 1,024,012; 296,340; and 146,484 patients with established hypertension for commercial insurance, Medicare Supplement, and multistates Medicaid, respectively, used for the analysis. SDOH-related Z codes were identified using ICD-10-CM=Z55–Z65. Z code–related encounters include Z code–related inpatient, ED, and outpatient encounters. Patients with established hypertension were defined if there was at least 1 inpatient, ED, or outpatient hypertension diagnosis (ICD-10-CM=I10–I15) from January 1, 2016 to December 31, 2017. Q denotes calendar quarter. The difference in the average proportion of patients with an SDOH-related Z code encounter by commercial versus Medicare supplement, commercial versus Medicaid, and Medicare supplement versus. Medicaid were tested using the 2-proportion Z-test. The ∆% is the percentage change from Q1 2018 to Q2 2021. The differences in the changes were tested using the 2-proportion Z-test. *p<0.05, **p<0.01, and ***p<0.001.
ED, emergency department; Q, quarter; SDOH, social determinant of health.
Figure 4.
Proportion of SDOH-related Z code inpatient, ED, and outpatient encounters by quarter among patients with established hypertension, MarketScan commercial claims and encounters, Medicare Supplement, and Medicaid database, January 1, 2018–June 30, 2021, by encounter settings—MarketScan commercial.
Note: On the Y-axis, we report the percentage of SDOH-related Z-codes encounters among patients with established hypertension (i.e., the ratio of the total number of Z-codes–related respective encounters to the total number of respective encounters, then multiplied by 100 among patients with established hypertension). There are 1,024,012 patients with established hypertension in commercial insurance used for the analysis. SDOH-related Z-codes were identified using ICD-10-CM=Z55–Z65. All encounters included inpatient, ED, and outpatient encounters. Patients with established hypertension were defined if there were at least 1 inpatient, ED, or outpatient hypertension diagnosis (ICD-10-CM=I10–I15) from January 1, 2016 to December 31, 2017. The difference in the proportions of SDOH-related Z code−related encounters by inpatient versus outpatient, inpatient versus ED, and outpatient versus ED were tested using the 2-proportion Z-test. The ∆% is the percentage change from Q1 2018 to Q2 2021. The differences in the changes were tested using the 2-proportion Z-test. *p<0.05, **p<0.01, and ***p<0.001.
ED, emergency department; Q, quarter; SDOH, social determinant of health.
Figure 5.
Proportion of SDOH-related Z code inpatient, ED, and outpatient encounters by quarter among patients with established hypertension, MarketScan commercial claims and encounters, Medicare Supplement, and Medicaid database, January 1, 2018–June 30, 2021, by encounter settings—MarketScan Medicare Supplement.
Note: On the Y-axis, we report the percentage of SDOH-related Z-code encounters among patients with established hypertension (i.e., the ratio of the respective encounters with a Z code to the total number of respective encounters, then multiplied by 100 among patients with established hypertension). There are 296,340 patients with established hypertension in Medicare Supplement insurance used for the analysis. SDOH-related Z-codes were identified using ICD-10-CM=Z55–Z65. All encounters included inpatient, ED, and outpatient encounters. Patients with established hypertension were defined if there were at least 1 inpatient, ED, or outpatient hypertension diagnosis (ICD-10-CM=I10–I15) from January 1, 2016 to December 31, 2017. The difference in the proportions of SDOH-related Z code–related encounters by inpatient versus outpatient, inpatient versus ED, and outpatient versus ED were tested using the 2-proportion Z-test. The Δ% is the percentage change from Q1 2018 to Q2 2021. The differences in the changes were tested using the 2-proportion Z-test. *p<0.05, **p<0.01, and ***p<0.001.
ED, emergency department; Q, quarter; SDOH, social determinant of health.
Figure 6.
Proportion of SDOH-related Z code inpatient, ED, and outpatient encounters by quarter among patients with established hypertension, MarketScan commercial claims and encounters, Medicare Supplement, and Medicaid database, January 1, 2018–June 30, 2021, by encounter settings—MarketScan Medicaid.
Note: On the Y-axis, we report the percentage of SDOH-related Z-code encounters among patients with established hypertension (i.e., the ratio of respective encounters with a Z code to the total number of respective encounters, then multiplied by 100 among patients with established hypertension). There are 146,484 patients with established hypertension in Medicaid insurance used for the analysis. SDOH-related Z-codes were identified using ICD-10-CM=Z55–Z65. All encounters included inpatient, ED, and outpatient encounters. Patients with established hypertension were defined if there were at least 1 inpatient, ED, or outpatient hypertension diagnosis (ICD-10-CM=I10–I15) from January 1, 2016 to December 31, 2017. The difference in the proportions of SDOH-related Z code–related encounters by inpatient versus outpatient, inpatient versus ED, and outpatient versus ED were tested using the 2-proportion Z-test. The Δ% is the percentage change from Q1 2018 to Q2 2021. The differences in the changes were tested using the 2-proportion Z-test. *p<0.05, **p<0.01, and ***p<0.001.
ED, emergency department; Q, quarter; SDOH, social determinant of health.
Table 2.
Proportion of Patients With An SDOH-Related Z Code and Proportion by SDOH Domain Among Patients With Established Hypertension and by Insurance Type and Year Documented
| SDOH-related Z code status | Commercial n=1,024,012 |
Medicare supplement n=296,340 |
Medicaid for select states n=146,484 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| 2018 | 2019 | 2020 | 2018 | 2019 | 2020 | 2018 | 2019 | 2020 | |
| % of patients with 1+ SDOH-related Z code | 0.389 | 0.438 | 0.461 | 0.306 | 0.382 | 0.417 | 3.132 | 3.117 | 3.019 |
| Number of unique patients who had 1+ SDOH-related Z code | 14,680 | 16,230 | 19,514 | 2,498 | 3,409 | 3,616 | 34,764 | 40,565 | 32,627 |
| Z codes by SDOH domain | % | % | % | % | % | % | % | % | % |
| Z55: problems related to education and literacy | 0.28 | 0.51 | 0.67 | 0.28 | 0.09 | 0.47 | 0.45 | 0.96 | 1.60 |
| Z56: problems related to employment and unemployment | 9.46 | 8.88 | 8.29 | 0.60 | 0.65 | 1.11 | 1.46 | 1.92 | 3.17 |
| Z57: occupational exposure to risk factors | 1.22 | 1.19 | 1.04 | 1.64 | 1.41 | 1.24 | 0.23 | 0.08 | 0.06 |
| Z58: problems related to physical environment | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Z59: problems related to housing and economic circumstances | 2.33 | 2.11 | 2.31 | 2.56 | 4.08 | 4.48 | 80.83 | 81.12 | 71.46 |
| Z60: problems related to social environment | 5.39 | 4.49 | 4.63 | 27.06 | 29.10 | 24.23 | 4.19 | 4.85 | 8.87 |
| Z62: problems related to upbringing | 12.87 | 13.71 | 12.47 | 6.16 | 5.72 | 5.17 | 2.39 | 2.48 | 4.61 |
| Z63: other problems related to primary support group | 62.75 | 63.91 | 64.96 | 53.28 | 50.78 | 55.09 | 6.90 | 5.80 | 8.05 |
| Z64: problems related to certain psychosocial circumstances | 0.19 | 0.35 | 0.13 | 0.04 | 0.06 | 0.00 | 0.03 | 0.05 | 0.03 |
| Z65: problems related to other psychosocial circumstances | 5.52 | 4.87 | 5.51 | 8.37 | 8.13 | 8.21 | 3.52 | 2.75 | 2.15 |
Note: The proportion of SDOH-related Z codes is calculated by dividing the total number of encounters observed with each SDOH-related Z code by the total number of SDOH-related Z codes in all encounters (identified with ICD-10-CM of Z55–Z65). The proportions were calculated by SDOH-related Z code domain, year documented, and insurance. Proportions sum to 100%. Patients with established hypertension were defined if at least 1 inpatient, emergency department, or outpatient hypertension diagnosis (ICD-10-CM=I10–I15) from January 1, 2016 to December 31, 2017.
SDOH, social determinant of health.
Finally, to describe the patterns of healthcare use and patient characteristics associated with the presence of an SDOH-related Z code,5,14,15 we summarized patient and encounter characteristics, stratified by patients with an SDOH-related Z code versus those without an SDOH-related Z code, in 2019, the most recent year before the COVID-19 pandemic (Table 3). These included total annual medical net payments made by health plan by encounter type, the number of annual medical services by encounter type, and patient characteristics (age, sex, and clinical diagnoses for all patients; race/ethnicity; Census region; and urbanicity of residence, if available). Health was characterized using the Quan modification of the Charlson Comorbidity Index (CCI) for ICD-10-CM codes (Appendix Table 3, available online),28 including both continuous and categorized (0, 1, 2, 3+) measures for 2019. To assess differences between patients with and without an SDOH-related Z code, the Wilcoxon rank-sum test, for nonparametric data, was used for continuous variables, and Pearson's chi-square test was used for categorical variables.
Table 3.
Healthcare Use and Patient Characteristics Among Patients With Established Hypertension in MarketScan Commercial Claims and Encounters, Medicare Supplement, and Medicaid Database, 2019
| Patient health care use and characteristics | Commercial |
Medicare supplement |
Medicaid |
|||
|---|---|---|---|---|---|---|
| SDOH-related Z code in 2019 = no | SDOH-related Z code in 2019 = yes | SDOH-related Z code in 2019 = no | SDOH-related Z code in 2019 = yes | SDOH-related Z code in 2019 = no | SDOH-related Z code in 2019 = yes | |
| n=1,019,531 | n=4,481 | n=295,207 | n=1,133 | n=141,918 | n=4,566 | |
| Medical costs and utilization of services, mean (SD) | ||||||
| Total medical net payments | $11,240.9 (34,260.7) | $20,834.0***(50,122.1) | $6,126.0 (18,679.0) | $10,883.5***(23,473.2) | $22,993.0 (36,416.0) | $37,014.7***(40,038.9) |
| Total inpatient net payments | $2,373.6 (19,425.3) | $6,012.6***(31,223.9) | $1,259.6 (9,826.2) | $3,015.1***(13,181.7) | $,3,118.1 (13,453.0) | $10,265.0***(22,963.2) |
| Total ED net payments | $511.3 (2,531.5) | $1,267.4***(3,964.5) | $163.8 (795.1) | $497.8***(1,894.3) | $977.9 (2,474.6) | $3,586.1***(7,900.1) |
| Total outpatient net payments | $4,783.6 (18,699.6) | $8,834.6***(26,422.2) | $2,788.9 (9,465.3) | $4,834.8***(9,567.6) | $11,260.7 (23,907.0) | $13,734.8***(21,657.0) |
| Total pharmacy net payments | $3,284.1 (13,211.3) | $4,155.4***(12,467.3) | $1,799.4 (8,793.5) | $2,377.6* (9,823.0) | $7,028.6 (17,914.8) | $8,434.3***(15,193.5) |
| Number of inpatient encounters | 0.1 (0.4) | 0.3***(0.8) | 0.2 (0.5) | 0.3***(0.7) | 0.3 (1.0) | 1.4***(2.7) |
| Number of ED encounters | 0.3 (0.9) | 0.8***(2.1) | 0.4 (1.1) | 1.1***(2.3) | 1.5 (3.4) | 5.7***(12.4) |
| Number of outpatient encounters | 13.2 (15.7) | 24.5***(21.6) | 23.3 (21.4) | 34.8***(26.7) | 58.8 (99.6) | 83.2***(103.9) |
| Number of pharmacy encounters | 25.3 (23.2) | 33.8***(28.1) | 32.5 (24.4) | 38.5***(28.4) | 67.6 (71.3) | 74.1***(66.7) |
| Dummy indicators of having any of the ICD-10-CM diagnosis of 17 conditions from the CCI in any setting, n (%) | ||||||
| Myocardial infarction | 15,841 (1.55%) | 110***(2.45%) | 12,009 (4.07%) | 65**(5.74%) | 7,387 (5.21%) | 406***(8.89%) |
| Congestive heart failure | 29,771 (2.92%) | 165**(3.68%) | 34,558 (11.71%) | 165**(14.56%) | 17,124 (12.07%) | 728***(15.94%) |
| Peripheral vascular disease | 38,320 (3.76%) | 201* (4.49%) | 58,813 (19.92%) | 242 (21.36%) | 14,800 (10.43%) | 558***(12.22%) |
| Cerebrovascular disease | 10,734 (1.05%) | 80***(1.79%) | 13,352 (4.52%) | 87***(7.68%) | 7,134 (5.03%) | 327***(7.16%) |
| Dementia | 856 (0.08%) | 16***(0.36%) | 11,504 (3.90%) | 121***(10.68%) | 3,275 (2.31%) | 116 (2.54%) |
| Chronic pulmonary disease | 113,871 (11.17%) | 752***(16.78%) | 57,375 (19.44%) | 279***(24.62%) | 44,971 (31.69%) | 2,055***(45.01%) |
| Rheumatic disease | 22,967 (2.25%) | 125* (2.79%) | 12,057 (4.08%) | 48 (4.24%) | 4,935 (3.48%) | 186* (4.07%) |
| Peptic ulcer disease | 6,376 (0.63%) | 48***(1.07%) | 3,331 (1.13%) | 17 (1.50%) | 2,103 (1.48%) | 99***(2.17%) |
| Mild liver disease | 51,892 (5.09%) | 341***(7.61%) | 14,247 (4.83%) | 74**(6.53%) | 12,226 (8.61%) | 704***(15.42%) |
| Diabetes without chronic complication | 249,189 (24.44%) | 1,138 (25.40%) | 88,833 (30.09%) | 332 (29.30%) | 48,686 (34.31%) | 1,869***(40.93%) |
| Diabetes with chronic complication | 68,861 (6.75%) | 363***(8.10%) | 44,336 (15.02%) | 185 (16.33%) | 23,622 (16.64%) | 971***(21.27%) |
| Hemiplegia or paraplegia | 3,187 (0.31%) | 34***(0.76%) | 2,621 (0.89%) | 17* (1.50%) | 4,746 (3.34%) | 198***(4.34%) |
| Renal disease | 42,342 (4.15%) | 186 (4.15%) | 43,749 (14.82%) | 182 (16.06%) | 13,928 (9.81%) | 538***(11.78%) |
| Any malignancy, including lymphoma and leukemia, except malignant neoplasm of skin | 49,323 (4.84%) | 247* (5.51%) | 46,310 (15.69%) | 183 (16.15%) | 6,637 (4.68%) | 257**(5.63%) |
| Moderate or severe liver disease | 2,084 (0.20%) | 22***(0.49%) | 786 (0.27%) | 3 (0.26%) | 1,200 (0.85%) | 78***(1.71%) |
| Metastatic solid tumor | 5,539 (0.54%) | 47***(1.05%) | 4,428 (1.50%) | 31***(2.74%) | 1,075 (0.76%) | 47* (1.03%) |
| AIDS/HIV | 3,739 (0.37%) | 25* (0.56%) | 280 (0.09%) | 1 (0.09%) | 2,790 (1.97%) | 184***(4.03%) |
| CCI score=0, n (%) | 566,646 (55.58%) | 2,218***(49.50%) | 88,841 (30.09%) | 291**(25.68%) | 48,914 (34.47%) | 914***(20.02%) |
| CCI score=1, n (%) | 243,129 (23.85%) | 1,127* (25.15%) | 62,321 (21.11%) | 233 (20.56%) | 30,136 (21.23%) | 1,024 (22.43%) |
| CCI score=2, n (%) | 89,916 (8.82%) | 458***(10.22%) | 46,571 (15.78%) | 182 (16.06%) | 18,356 (12.93%) | 710***(15.55%) |
| CCI score≥3, n (%) | 119,840 (11.75%) | 678***(15.13%) | 97,474 (33.02%) | 427***(37.69%) | 44,512 (31.36%) | 1,918***(42.01%) |
| CCI score, mean (SD) | 0.9 (1.5) | 1.1***(1.8) | 2.1 (2.3) | 2.4***(2.6) | 2.0 (2.4) | 2.8***(2.8) |
| Characteristics | ||||||
| Age at first dx, mean (SD) | 50.1 (8.0) | 48.5***(8.6) | 72.5 (7.2) | 73.8***(7.8) | 47.8 (11.4) | 47.4* (10.3) |
| Female, n (%) | 471,918 (46.29%) | 2,578***(57.53%) | 162,073 (54.90%) | 730***(64.43%) | 84,942 (59.85%) | 2,525***(55.30%) |
| Urban, n (%) | 856,167 (83.98%) | 3,840**(85.70%) | 253,257 (85.79%) | 959 (84.64%) | — | — |
| Northeast, n (%) | 227,865 (22.35%) | 956 (21.33%) | 141,507 (47.93%) | 453a (39.98%) | — | — |
| South, n (%) | 517,241 (50.73%) | 2,089***(46.62%) | 61,663 (20.89%) | 200**(17.65%) | — | — |
| Midwest, n (%) | 184,356 (18.08%) | 908***(20.26%) | 83,883 (28.41%) | 441***(38.92%) | — | — |
| West, n (%) | 88,056 (8.64%) | 520***(11.60%) | 8,007 (2.71%) | 39 (3.44%) | — | — |
| Non-Hispanic White, n (%) | — | — | — | — | 60,783 (42.83%) | 1,790***(39.20%) |
| Non-Hispanic Black, n (%) | — | — | — | — | 59,930 (42.23%) | 2,234***(48.93%) |
| Hispanic, n (%) | — | — | — | — | 2,603 (1.83%) | 58**(1.27%) |
| Other race, n (%) | — | — | — | — | 3,972 (2.80%) | 83***(1.82%) |
Note: p values were obtained from the Wilcoxon rank-sum test for continuous variables and Pearson's chi-square test for dummy indicators for comparisons between the presence of SDOH-related Z code versus not. Total medical net payments are the average of payments made by insurance plans in 2019. Total inpatient, ED, outpatient, and pharmacy payments are the average of the total inpatient, ED, outpatient, and pharmacy payments made by insurance plans in 2019. The number of inpatients, ED, outpatient, and pharmacy visits are the average numbers of inpatient, ED, outpatient, and pharmacy visits in 2019. The ICD-10-CM codes to identify the CCI dummy variables are in Appendix Table 3 (available online). All the dummy variables for the diseases were identified as equal one if at least 1 ICD-10-CM code of the respective ICD-10-CM was identified in any setting. Patients with established hypertension were defined if there were at least 1 inpatient, ED, or outpatient hypertension diagnosis (ICD-10-CM=I10–I15) from January 1, 2016 to December 31, 2017. Dash (–) indicates that data are not available in the respective databases. Boldface indicates statistical significance (*p<0.05; **p<0.01; ***p<0.001).
CCI, Charlson Comorbidity Index; ED, emergency department; SDOH, social determinant of health.
To indicate statistical significance, p-values <0.05 were used. All analyses were conducted using Stata MP, Version 14.2 (StataCorp, College Station, TX), in 2022.
RESULTS
Table 1 shows the summaries of the available patient characteristics at first hypertension diagnosis, which was identified for the analysis cohorts in 2016–2017. Of 1,024,012 (commercial insurance aged 18–64 years), 296,340 (Medicare Supplement aged ≥65 years), and 146,484 (Medicaid aged ≥18 years) patients with established hypertension (Figures 1 and 2), the average age was 50 years for commercial beneficiaries, 73 years for Medicare Supplement beneficiaries, and 48 years for Medicaid beneficiaries. The proportion of patients who were female ranged from 46% among commercial beneficiaries to nearly 60% among Medicaid.
Table 1.
Patient Characteristics at First Diagnosis, Patients With Established Hypertension in 2016–2017 in MarketScan Commercial Claims and Encounters, Medicare Supplement, and Medicaid Database
| Patient characteristics | Commercial | Medicare supplement | Medicaid |
|---|---|---|---|
| n=1,024,012 | n=296,340 | n=146,484 | |
| Age at first dx, mean (SD) | 50.1 (8.0) | 72.5 (7.2) | 47.8 (11.3) |
| Female, n (%) | 474,496 (46.34%) | 162,803 (54.94%) | 87,467 (59.71%) |
| Urban, n (%) | 860,007 (83.98%) | 254,216 (85.79%) | — |
| Northeast, n (%) | 228,821 (22.35%) | 141,960 (47.90%) | — |
| South, n (%) | 519,330 (50.72%) | 61,863 (20.88%) | — |
| Midwest, n (%) | 185,264 (18.09%) | 84,324 (28.46%) | — |
| West, n (%) | 88,576 (8.65%) | 8,046 (2.72%) | — |
| Non-Hispanic White, n (%) | — | — | 62,573 (42.72%) |
| Non-Hispanic Black, n (%) | — | — | 62,164 (42.44%) |
| Hispanic, n (%) | — | — | 2,661 (1.82%) |
| Other race, n (%) | — | — | 4,055 (2.77%) |
dx, diagnosis.
Proportion of unique patients with any claim with SDOH–related Z code over time. All differences over time and between insurance groups were statistically significant (p<0.001). Although the absolute increases in the proportion of SDOH-related Z code documented from 2018 to 2021 were small, the relative increases were 46.9% (from 0.11% to 0.16%) among patients with Medicare supplemental insurance and 13.8% (from 1.31% to 1.49%) among patients with Medicaid, from the first quarter of 2018 through the second quarter of 2021 (Figure 3). In addition, there appeared to be a dip in SDOH-related Z codes among patients with Medicaid during the beginning of the COVID-19 pandemic. The annual proportions of patients with Z codes were 0.39%, 0.44%, and 0.46% in 2018, 2019, and 2020, respectively, for commercial insurance; 0.31%, 0.38%, and 0.42% in 2018, 2019, and 2020, respectively, for Medicare Supplement; and 3.13%, 3.12%, 3.02% in 2018, 2019, and 2020, respectively, for Medicaid insurance (Table 2).
Proportion of claims with SDOH–related Z code by encounter setting. The proportion of claims with an SDOH-related Z code was higher among inpatient than among outpatient or ED settings in all 3 insurance types (Figures 4–6) (p<0.001 for all comparisons). Quarterly, approximately 0.37% (vs 0.12% outpatient or 0.09% ED), 0.12% (0.05% outpatient or 0.05% ED), and 2.09% (0.35% outpatient or 1.38% ED) of inpatient encounters contained SDOH-related Z codes in commercial, Medicare supplement, and Medicaid insurances, respectively. The largest increases over time were observed among ED encounters: 169% for commercial, 73% for Medicare Supplement, and 182% for Medicaid from the first quarter to the last quarter (2018 to mid-2021; p<0.001 for all comparisons).
Proportion of SDOH–related Z code by domain. Z63 (other problems related to primary support group) was the most documented SDOH-related Z code among patients with commercial insurance (62.75%–64.96% of all SDOH-related Z code encounters in 2018–2020) and Medicare Supplement (50.78%–55.09% of all SDOH-related Z code encounters in 2018–2020), whereas Z59 (problems related to housing and economic circumstances) was most common among patients with Medicaid insurance (71.46%–81.12% of all SDOH-related Z code encounters in 2018–2020) (Table 2).
Health care use and patient characteristics associated with a SDOH–related Z code. There were 4,481 (0.44%), 1,133 (0.38%), and 4,566 (3.12%) patients who had 1+ SDOH-related Z codes in the 2019 claims database in commercial, Medicare Supplement, and Medicaid insurance, respectively (Table 3). The unadjusted annual total medical, total inpatient, ED, and outpatient net health plan payments were higher among patients with SDOH-related Z codes than among those without SDOH-related Z codes across all the 3 insurance types (Table 3) (all p<0.001). On average, the 2019 total expenditures for patients with an SDOH-related Z code were 1.85, 1.78, and 1.61 times higher than for patients without an SDOH-related Z code for commercial, Medicare Supplement, and Medicaid insurance, respectively. Patients with 1+ SDOH-related Z codes also tended to have a higher number of encounters and proportions of the 17 CCI conditions than those without an SDOH-related Z code. The mean CCI scores were higher among patients with 1+ SDOH-related Z codes than among those without an SDOH-related Z code for commercial (1.1 vs 0.9; p<0.001), Medicare Supplement (2.4 vs 2.1; p<0.001), and Medicaid insurance (2.8 vs 2.0; p<0.001). The proportion of females was higher among patients with 1+ SDOH-related Z codes than among those without an SDOH-related Z code for commercial (57.5% vs 46.3%; p<0.001) and Medicare Supplement (64.4% vs 54.9%; p<0.001) insurance but lower for those with Medicaid insurance (55.3% vs 59.9%; p<0.001). Additional patient characteristics were available by insurance type. Among Medicaid, the proportion of non-Hispanic Black persons was higher among patients with SDOH-related Z codes than among those without SDOH-related Z codes (48.93% vs 42.23%; p<0.001). Similar patterns were observed for 2018 (data not shown).
DISCUSSION
We examined commercial, Medicare Supplement, and Medicaid beneficiaries with hypertension in 2016–2017 and continuously enrolled through June 30, 2021. We found that the highest documentation of SDOH-related Z codes was among Medicaid beneficiaries (ranging from 3.02% to 3.13% annually). The annual proportion of patients with 1+ SDOH-related Z codes ranged from 0.39% to 0.46% for commercial beneficiaries and from 0.31% to 0.42% for Medicare beneficiaries. Patients with an SDOH-related Z code had more comorbidities and higher annual total unadjusted expenditures than those without an SDOH-related Z code across all insurance types. Among all SDOH-related Z codes, problems related to primary support group (Z63) were most common among commercial (63%–65%) and Medicare Supplement (51%–55%) beneficiaries, whereas problems related to housing and economic circumstances were the most common among Medicaid beneficiaries (71%–81%).
In our study, SDOH-related Z codes were approximately 7 times higher among Medicaid beneficiaries than among commercial and Medicare beneficiaries. This may reflect screening and documenting practices16,29 and patient needs. Despite this pattern, the presence of SDOH-related Z codes was low among adult patients with hypertension across all the 3 cohorts (≤3%), including Medicaid. This seems to be contrary to the findings of national research that suggests that more than half (54%) of U.S. adults with low income had unmet social needs.29,30 Across different periods, analysis populations, and SDOH domains studied, the overall presence of SDOH-related Z codes at the encounter or claims level and patient level has been consistently low (<3%) in other studies.5,7,14, 15, 16, 17,31 Adoption of SDOH-related Z codes has been slow because of a misunderstanding that only physicians can document a patient's social needs, the absence of standard operating procedures for documenting and coding, and unfamiliarity with SDOH-related Z codes among healthcare administrators, providers, and coders.13 It has been suggested that SDOH-related Z codes could be used for payment and that reimbursement policies could lead to better documentation using SDOH-related Z codes.2,11,14
Despite the low documentation, associations between the presence of SDOH-related Z codes and more healthcare use and costs were observed in this study and other studies.5,14,15 For example, a dose–response relationship was found between the number of SDOH domains and hospital readmission (2017 nationwide Healthcare Cost and Utilization Project)14; and the presence of SDOH-related Z codes was associated with 4 times the hospitalizations and ED visits and 9.3 times the annual cost per patient (2017 Florida Healthcare Cost and Utilization Project).5 In this study of patients with hypertension, the 2019 total unadjusted expenditures were 1.85, 1.78, and 1.61 times higher for those with an SDOH-related Z code than those without for commercial, Medicare Supplement, and Medicaid, respectively. Moreover, the Medicaid cohort, which had the highest presence of SDOH-related Z codes and the highest rate of housing and economic issues, had the highest mean total net payments, among all types of encounters. In addition, SDOH-related Z codes tended to be more common for inpatient encounters than for other encounter types. This could represent differences in social needs documentation across settings or that some inpatient primary diagnoses are more obviously related to social and economic circumstances.5,16 Across all of these patterns, differences likely reflect a mixture of factors and are not attributed to social needs alone. However, identifying social needs among patients with hypertension is an opportunity to prevent adverse outcomes and complications.24
The Surgeon General's Call to Action acknowledges that improving hypertension control requires addressing SDOH, and screening for social and economic circumstances and social needs among patients with hypertension has been recommended.23,32 SDOH and social needs can be a barrier to healthy living (e.g., unhealthy built environments) and accessing and paying for recommended diagnostics and referrals to recommended care33 and have been shown to be associated with antihypertensive medication nonadherence at the county level.34 Even among those taking antihypertensive medications by medication class, differences in the proportion of adults with controlled hypertension have been observed by race/ethnicity and SES.35 This suggests that some patients with hypertension need additional support for healthcare and lifestyle management, which has implications for cardiovascular disease risk. For example, among a national, population-based sample (age ≥45 years) without coronary heart disease at baseline, greater SDOH burdens were associated with fatal incident coronary heart disease than among those without SDOH burdens.25
In this study, we observed larger pharmacy payments and more comorbidity for patients with an SDOH-related Z code than for those without an SDOH-related Z code across all the 3 cohorts, with a notable difference in diabetes comorbidity among Medicaid patients. Patients with hypertension and social needs may need to navigate systems for resources to pay for medications and additional services to support blood pressure monitoring and medication adherence and for lifestyle changes.31,32 Although it is not the purpose of SDOH-related Z codes, monitoring social needs can help clinical and public health decision makers to understand the population-wide need for such services, potentially by specific chronic conditions.1,33
Although there are potential benefits to documenting social needs with SDOH-related Z codes, to date, this has not been mandated2; for example, a small review of records for high-risk patients found that 92% of patients had information that could have been coded but were not documented with SDOH-related Z codes.36 There are efforts to increase the documentation of social needs with SDOH-related Z coding in clinical practice. The AHA recently updated guidance to recommend that administrators raise awareness and educate physicians, other healthcare providers, and medical coders on how to screen, document, and code data on patients’ social needs. The AHA guideline suggests that healthcare providers transfer information provided by patients from self-screening tools into the patient's electronic health records. The tools should be available in numerous languages and forms (e.g., with voice instructions) for different levels of literacy. The healthcare providers could use this information to refer patients to community resources and follow-up.13 In the future, there may be more coding of social needs and incentives to use SDOH-related Z codes. For example, Accountable Care Organizations provide care for the whole person, including social needs, and CMS is testing different Accountable Care Organizations models to advance health equity.37,38
Limitations
Although our study expands the existing literature, there are some limitations. First, we cannot generalize our results to other populations, such as those with discontinuous enrollment, those who are uninsured or insured with other types of plans, and the general population. We focus on continuously enrolled beneficiaries who have received health care and had diagnosed hypertension. It is possible that patients with social needs are less likely to have stable access to commercial health insurance because of job insecurity or that patients may move in and out of Medicaid on the basis of need. It is also possible that patients with social needs have additional barriers to receiving health care and therefore have fewer opportunities to diagnose hypertension.39 Second, our data may not be representative of all Medicare or Medicaid populations because we focus on Medicare patients with employer-sponsored supplemental health plans and Medicaid beneficiaries from selected, unidentified states. In addition, there are several reasons why SDOH-related Z codes are underused; thus, screening and documenting for social needs in clinical practice is underreported. Previous studies reported screening for SDOH in a range of 15%–24%.20,40,41 Z codes are nonbillable codes, and coders do not have the financial incentive to document them.5 Although SDOH-related Z codes match most domains included in screening tools, not all SDOH screening domains have a corresponding ICD-10-CM Z code2; therefore, the usage patterns in our study may underestimate screening in clinical practice. Third, our data included race or ethnicity information only for Medicaid, and we found a higher proportion of SDOH-related Z codes among non-Hispanic Black beneficiaries. This is consistent with the finding of another study using 2019 Medicare FFS data where documentation tended to be higher among Black and American Indian/Native Alaskan beneficiaries.17 Future studies are needed to examine whether these findings persist among beneficiaries with commercial insurance and to confirm whether these results reflect racial or ethnic disparities and not ascertainment bias.
CONCLUSIONS
We found that the presence of SDOH-related Z codes among individuals with hypertension was low but tended to be associated with poorer health and more with higher expenditures. Documentation of social needs through SDOH-related Z codes provides an actionable opportunity to integrate social and medical data.2 Our study of adults suggests that this may be a missed opportunity to addressing nonclinical needs that affect hypertension and other health outcomes and healthcare costs.
Acknowledgments
ACKNOWLEDGMENTS
We would like to acknowledge Feijun Luo, Michael Schooley, Adam Vaughan, and Fátima Coronado, with the Centers for Disease Control and Prevention, for their expertise and manuscript review. JSL and KEM are joint first authors.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. HHS.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of interest: None.
CREDIT AUTHOR STATEMENT
Jun Soo Lee: Writing – original draft, Writing – review & editing, Formal analysis, Methodology, Conceptualization, Software. Kara E. MacLeod: Writing – original draft, Writing – review & editing, Formal analysis, Methodology, Conceptualization. Elena V. Kuklina: Writing – review & editing, Conceptualization. Xin Tong: Writing – review & editing, Conceptualization. Sandra L. Jackson: Writing – review & editing, Conceptualization, Supervision.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.focus.2023.100089.
Appendix. Supplementary materials
REFERENCES
- 1.Arons A, DeSilvey S, Fichtenberg C, Gottlieb L. Documenting social determinants of health-related clinical activities using standardized medical vocabularies. JAMIA Open. 2019;2(1):81–88. doi: 10.1093/jamiaopen/ooy051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gottlieb L, Tobey R, Cantor J, Hessler D, Adler NE. Integrating social and medical data to improve population health: opportunities and barriers. Health Aff (Millwood) 2016;35(11):2116–2123. doi: 10.1377/hlthaff.2016.0723. [DOI] [PubMed] [Google Scholar]
- 3.Gurewich D, Garg A, Kressin NR. Addressing social determinants of health within healthcare delivery systems: a framework to ground and inform health outcomes. J Gen Intern Med. 2020;35(5):1571–1575. doi: 10.1007/s11606-020-05720-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang M, Pantell MS, Gottlieb LM, Adler-Milstein J. Documentation and review of social determinants of health data in the EHR: measures and associated insights. J Am Med Inform Assoc. 2021;28(12):2608–2616. doi: 10.1093/jamia/ocab194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bensken WP, Alberti PM, Stange KC, Sajatovic M, Koroukian SM. ICD-10 Z-code health-related social needs and increased healthcare utilization. Am J Prev Med. 2022;62(4):e232–e241. doi: 10.1016/j.amepre.2021.10.004. [DOI] [PubMed] [Google Scholar]
- 6.Eder M, Henninger M, Durbin S, et al. Screening and interventions for social risk factors: technical brief to support the US Preventive Services Task Force. JAMA. 2021;326(14):1416–1428. doi: 10.1001/jama.2021.12825. [DOI] [PubMed] [Google Scholar]
- 7.Truong HP, Luke AA, Hammond G, Wadhera RK, Reidhead M, Joynt Maddox KE. Utilization of social determinants of health ICD-10 Z-codes among hospitalized patients in the United States, 2016–2017. Med Care. 2020;58(12):1037–1043. doi: 10.1097/MLR.0000000000001418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. 2011. ICD-9-CM Official Guidelines for Coding and Reporting. https://www.cdc.gov/nchs/data/icd/icd9cm_guidelines_2011.pdf. Accessed July 15, 2022.
- 9.Centers for Medicare and Medicaid Services. FY2022 April 1 Update ICD-10-CM Guidelines (cms.gov).
- 10.Kostick KM. From V Codes to Z Codes: transitioning to ICD-10 (updated) J AHIMA. 2011;82(11):60–63. [PubMed] [Google Scholar]
- 11.Torres JM, Lawlor J, Colvin JD, et al. ICD social codes: an underutilized resource for tracking social needs. Med Care. 2017;55(9):810–816. doi: 10.1097/MLR.0000000000000764. [DOI] [PubMed] [Google Scholar]
- 12.American Hospital Association. 2019-Q4-codingclinic_icd10.pdf. https://erm365.org/wp-content/uploads/2020/04/2019-Q4-codingclinic_icd10.pdf. Published 2019. Accessed July 15, 2022.
- 13.American Hospital Association. Value-initiative-icd-10-code-social-determinants-of-health.pdf.https://www.aha.org/system/files/2018-04/value-initiative-icd-10-code-social-determinants-of-health.pdf. Published 2022. Accessed July 15, 2022.
- 14.Bensken WP, Alberti PM, Koroukian SM. Health-related social needs and increased readmission rates: findings from the nationwide readmissions database. J Gen Intern Med. 2021;36(5):1173–1180. doi: 10.1007/s11606-021-06646-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weeks WB, Cao SY, Lester CM, Weinstein JN, Morden NE. Use of Z-codes to record social determinants of health among fee-for-service Medicare beneficiaries in 2017. J Gen Intern Med. 2020;35(3):952–955. doi: 10.1007/s11606-019-05199-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mathew J, Hodge C, Khau M, Codes Z. Utilization Among Medicare Fee-for-Service (FFS) Beneficiaries in 2017. CMS OMH Data Highlight No. 17, 2020, CMS Office of Minority Health; Baltimore, MD. https://www.cms.gov/files/document/cms-omh-january2020-zcode-data-highlightpdf.pdf. Accessed July 15, 2022.
- 17.Maksut JL, Hodge C, Van CD, Razmi A, Khau MT. Utilization of Z Codes for Social Determinants of Health among Medicare Fee-For-Service Beneficiaries, 2019. Office of Minority Health (OMH) Data Highlight No, 24, 2021. Centers for Medicare and Medicaid Services: Baltimore, MD https://www.cms.gov/files/document/z-codes-data-highlight.pdf. Accessed July 15, 2022.
- 18.Friedman NL, Banegas MP. Toward addressing social determinants of health: a health care system strategy. Perm J. 2018;22(4S):18–095. doi: 10.7812/TPP/18-095. [DOI] [Google Scholar]
- 19.Hatef E, Ma X, Rouhizadeh M, Singh G, Weiner JP, Kharrazi H. Assessing the impact of social needs and social determinants of health on health care utilization: using patient- and community-level data. Popul Health Manag. 2021;24(2):222–230. doi: 10.1089/pop.2020.0043. PMCID: PMC8349715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vest JR, Wu W, Mendonca EA. Sensitivity and specificity of real-world social factor screening approaches. J Med Syst. 2021;45(12):111. doi: 10.1007/s10916-021-01788-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention (CDC), Hypertension Cascade: Hypertension Prevalence, Treatment and Control Estimates Among US Adults Aged 18 Years and Older Applying the Criteria From the American College of Cardiology and American Heart Association’s 2017 Hypertension Guideline—NHANES 2015–2018, 2021, HHS; Atlanta, GA https://millionhearts.hhs.gov/data-reports/hypertension-prevalence.html. Accessed July 15, 2022.
- 22.Tsao CW, Aday AW, Almarzooq ZI, et al. Heart disease and stroke statistics-2022 update: a report from the American Heart Association. Circulation. 2022;145(8):e153–e639. doi: 10.1161/CIR.0000000000001052. [DOI] [PubMed] [Google Scholar]
- 23.Substance Abuse and Mental Health Services Administration (US); Office of the Surgeon General (US). The surgeon general's call to action to control hypertension.https://www.ncbi.nlm.nih.gov/books/NBK567645/#:∼:text=The%20Surgeon%20General's%20Call%20to%20Action%20to%20Control%20Hypertension%20seeks,and%20expanded%20across%20diverse%20settings. Published 2020. Accessed July 15, 2022.
- 24.Inouye CF, Kaminski MA. Improve patient-centered care, decrease provider burnout, maximize Z Codes, minimize hierarchical condition category codes. Popul Health Manag. 2022;25(1):1–3. doi: 10.1089/pop.2021.0163. [DOI] [PubMed] [Google Scholar]
- 25.Safford MM, Reshetnyak E, Sterling MR, et al. Number of social determinants of health and fatal and nonfatal incident coronary heart disease in the REGARDS study. Circulation. 2021;143(3):244–253. doi: 10.1161/CIRCULATIONAHA.120.048026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Truven Health MarketScan® Research Databases. https://marketscan.truvenhealth.com/marketscanportal. Accessed June 13, 2022.
- 27.National Center for Chronic Disease Prevention and Health Promotion. Heart disease and stroke. https://www.cdc.gov/dhdsp/maps/atlas/data-sources.html. Updated 2021. Accessed July 15, 2022.
- 28.Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676–682. doi: 10.1093/aje/kwq433. [DOI] [PubMed] [Google Scholar]
- 29.Cartier Y, Gottlieb L. The prevalence of social care in US health care settings depends on how and whom you ask. BMC Health Serv Res. 2020;20(1):481. doi: 10.1186/s12913-020-05338-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cole MB, Nguyen KH. Unmet social needs among low-income adults in the United States: associations with health care access and quality. Health Serv Res. 2020;55(suppl 2):873–882. doi: 10.1111/1475-6773.13555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McCormack LA, Madlock-Brown C. Social determinant of health documentation trends and their association with emergency department admissions. AMIA Annu Symp Proc. 2020;2020:823–832. [PMC free article] [PubMed] [Google Scholar]
- 32.Hannan JA, Commodore-Mensah Y, Tokieda N, et al. Improving hypertension control and cardiovascular health: an urgent call to action for nursing. Worldviews Evid Based Nurs. 2022;19(1):6–15. doi: 10.1111/wvn.12560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Warner M. Account for social determinants of health when coding office visits - AAPC Knowledge Center.https://www.aapc.com/blog/52108-account-for-social-determinants-of-health-when-coding-office-visits/. Published 2020. Accessed July 15, 2022.
- 34.Donneyong MM, Chang TJ, Jackson JW, et al. Structural and social determinants of health factors associated with county-level variation in non-adherence to antihypertensive medication treatment. Int J Environ Res Public Health. 2020;17(18):6684. doi: 10.3390/ijerph17186684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hayes DK, Jackson SL, Li Y, et al. Blood pressure control among non-Hispanic Black adults is lower than non-Hispanic white adults despite similar treatment with antihypertensive medication: NHANES 2013–2018. Am J Hypertens. 2022;35(6):514–525. doi: 10.1093/ajh/hpac011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Coppa D, Winchester SB, McAlvin E, Roberts MB, Maestri X. Use of social determinants of health codes in home-based primary care. J Am Assoc Nurse Pract. 2021;34(1):42–49. doi: 10.1097/JXX.0000000000000586. [DOI] [PubMed] [Google Scholar]
- 37.Ubri PS, Bailey L, Melendez M, Sawyer J, Stead M. The role of state policy in use of Z Codes to document social need in Medicaid data. Published March 2022. Accessed July 15, 2022.
- 38.Centers for Medicaid and Medicare; 2022. ACO REACH. https://innovation.cms.gov/innovation-models/aco-reach. Accessed December 17, 2022.
- 39.Nguyen T, Barefield A, Nguyen GT. Social determinants of health associated with the use of screenings for hypertension, hypercholesterolemia, and hyperglycemia among American adults. Med Sci (Basel) 2021;9(1):19. doi: 10.3390/medsci9010019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fraze TK, Brewster AL, Lewis VA, Beidler LB, Murray GF, Colla CH. Prevalence of screening for food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence by US physician practices and hospitals. JAMA Netw Open. 2019;2(9) doi: 10.1001/jamanetworkopen.2019.11514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schickedanz A, Hamity C, Rogers A, Sharp AL, Jackson A. Clinician experiences and attitudes regarding screening for social determinants of health in a large integrated health system. Med Care. 2019;57(suppl 6 suppl 2):S197–S201. doi: 10.1097/MLR.0000000000001051. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.