HIGHLIGHTS
-
•
We used stakeholder-engaged concept mapping to identify social health research opportunities.
-
•
We generated 59 unique social health empirical questions rated on impact and priority.
-
•
The ranked and topic-driven list can help to guide other researchers in this space.
-
•
The broad range of questions revealed the nascency of the evidence base.
-
•
Strategic and rigorous research is needed to maximize social health benefits.
Keywords: Concept mapping, social determinants of health, social risk, social needs, research agenda
Graphical abstract
Abstract
Introduction
Healthcare systems such as Kaiser Permanente are increasingly focusing on patients’ social health. However, there is limited evidence to guide social health integration strategy. The purpose of this study was to identify social health research opportunities using a stakeholder-driven process.
Methods
A modified Concept Mapping approach was implemented from June 2021 to February 2022. Stakeholders (n=746) received the prompt, “One thing I wish we knew more about to advance my work addressing social health...” An inductive content analysis approach was used to assign topics and synthesize and refine research-focused statements into research questions. Questions were then rated on impact and priority by researcher stakeholders (n=16). Mean impact and priority scores and an overall combined score were calculated. Question rankings were generated using the combined score.
Results
Brainstorming produced 148 research-focused statements. A final list of 59 research questions was generated for rating. Question topics were (1) Data, Measures, and Metrics; (2) Intervention Approach and Impact; (3) Technology; (4) Role of Healthcare Systems; (5) Community-Based Organizations; (6) Equity; (7) Funding; and (8) Social Health Integration. On a scale from 1 (low) to 10 (high), the mean impact score was 6.12 (range=4.14–7.79), and the mean priority score was 5.61 (range=3.07–8.64). Twenty-four statements were rated as both high impact (>6.12) and high priority (>5.61).
Conclusions
The broad range of topics with high impact and priority scores reveals how nascent the evidence base is, with fundamental research on the nature of social risk and health system involvement still needed.
INTRODUCTION
Social factors (e.g., housing, food, finances) account for an estimated 40%–70% of a person's total health, reflecting a much higher impact than health care or genetics.1, 2, 3, 4 To address the strong influence of social determinants on health outcomes, health systems in the U.S., such as Kaiser Permanente (KP), are increasingly prioritizing social health integration. As per the National Academies of Sciences, Engineering, and Medicine, social health integration consists of 5 complementary activities: awareness, adjustment, assistance, alignment, and advocacy.5 Social health integration research is a broad-reaching and rapidly proliferating field. The lack of coordination across an expansive range of settings, topics, and populations presents a challenge for healthcare systems that are interested in strategic and systematic approaches to these complex, sensitive, and sometimes costly activities.6
In 2017, KP established the Social Needs Network for Evaluation and Translation (SONNET) to bring evidence to KP's social health strategy and rigorously evaluate member- and community-centered interventions.7 SONNET convenes an Evaluation and Research Committee (ERC) of social health researchers in each of KP's 8 regional markets: California (Northern and Southern), Colorado, Georgia, Hawaii, Oregon, Washington, and the Mid-Atlantic—the District of Columbia, Virginia, and Maryland. To focus SONNET's research activities, the ERC used a modified Concept Mapping process. Concept mapping provides a structured, stakeholder-driven approach to identifying the most relevant and important empirical questions to pursue.7 This paper reports our findings and a call to action for future directions.
METHODS
Procedures and Participants
Our modified Concept Mapping process occurred from June 2021 to February 2022 and was a subactivity of a larger KP social health agenda Concept Mapping initiative that is currently ongoing. The goal for our subactivity was to identify high-priority and high-impact empirical research questions for SONNET ERC members to pursue from the larger initiative. The first step was brainstorming, which sought responses to the following statement using the groupwisdom web-based platform8: “One thing I wish we knew more about to advance my work addressing social health...” Because the ERC members are social health experts as well as the primary end users and beneficiaries of this concept mapping substudy, we sought to engage them throughout the process to ensure that their perspectives were represented in the findings. The statement was generated by the study team; refined by the ERC (n=16); and sent on November 8–26, 2021 to 746 social health stakeholders, including the ERC members from across KP's regional markets and job roles. These stakeholders spanned the delivery system, health plan, and research institutes and needed empirical guidance to make strategic and operational decisions.
The brainstorming phase typically yields more statements than can move forward to the rating phase; the goal is to synthesize them into 100 or fewer.7 To achieve this for our empirical research–focused subactivity, we used an inductive content analysis approach with 3 primary coders. First, the primary coder (MCB) identified all empirical research-focused statements within the full list of statements and coded each on the basis of statement topic (e.g., social health integration, funded). Then, CCL synthesized these empirically focused statements into research questions that captured the overarching themes across these statements. Finally, the remaining coders (MCB, ARP, CK) reviewed these questions to ensure that key ideas were maintained and to make edits for clarity.
In the rating phase, we invited SONNET ERC members to rate each question on impact (How critical do you think this is in improving the social health of our members and the communities we serve?) and priority (How urgent do you think this is and recommend KP addresses it now?) using a scale from 1 (least impactful/lowest priority) to 10 (most impactful/highest priority).9 ERC members had 10 days to respond, and the response rate was 88% (n=14).
Data Interpretation
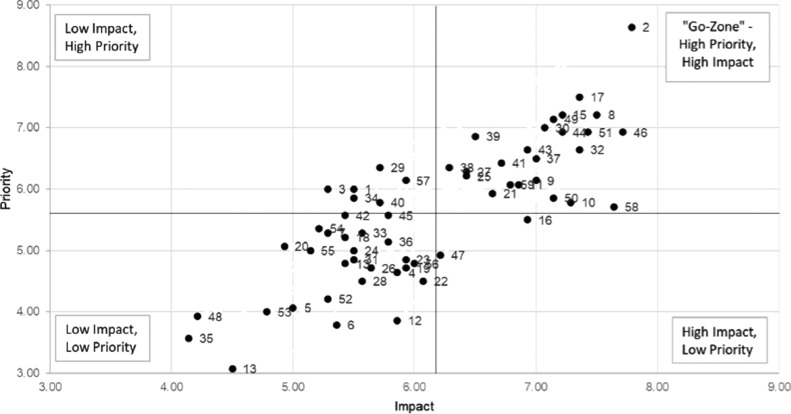
We calculated mean impact and priority scores from the rating phase and a combined overall score as the sum of these 2 scores. The combined score was used to provide an overall ranking of each question. The mean impact and priority scores were placed onto a scatterplot with 4 quadrants, consistent with Concept Mapping go-zone graphs.10 Questions rated high impact and high priority reflected the go-zone or upper right quadrant (Figure 1). For the final concept mapping phase, interpretation, we presented the rankings and go-zone graph back to the ERC in February 2022 to gather additional feedback and identify future SONNET research activities.
Figure 1.
Go-zone map.
The solid black lines indicate the mean priority and impact scores overall. Each point and number represent the impact and priority score for a given statement (Appendix 1, available online, for statements).
RESULTS
For brainstorming, by design, most stakeholders (742 of 746) were employed by KP; 66 email addresses were undeliverable, and 680 were successfully delivered. A total of 329 respondents (Table 1) completed the brainstorming phase. Of the 515 statements submitted, 148 were empirical research−focused statements. After inductive content analysis, 59 research questions moved forward to the rating phase. The 59 questions covered 8 nonmutually exclusive topics (statements could belong to more than 1 category but are presented in: (1) Data, Measures, and Metrics; (2) Intervention Approach and Impact; (3) Technology; (4) Role of Healthcare Systems; (5) Community-Based Organizations; (6) Equity; (7) Funding; and (8) Social Health Integration (Appendix File A, available online).
Table 1.
Research Agenda Participant Demographics (n=329)
| Category | % (n) or mean (SD) |
|---|---|
| Delivery system role | |
| Care delivery | 14% (45) |
| Health plan operations | 15% (50) |
| Community health | 14% (47) |
| Research | 19% (61) |
| Other | 16% (51) |
| Missing | 23% (75) |
| Region | |
| California | 16% (52) |
| Colorado | 14% (46) |
| Georgia | 3% (9) |
| Hawaii | 1% (3) |
| Mid-Atlantic | 2% (8) |
| Oregon | 8% (26) |
| Washington | 6% (20) |
| Program office | 27% (89) |
| Missing | 23% (76) |
| Race and ethnicity | |
| Asian or Pacific Islander | 13% (43) |
| Black or African American | 4% (15) |
| Hispanic or Latino | 4% (14) |
| Native American or Alaskan native | <1% (1) |
| White | 50% (170) |
| Multiracial or biracial | 2% (8) |
| Other | 2% (6) |
| Missing | 24% (81) |
| Years of social health experience | 8 (7) |
| How central is social health to your present role? | |
| Social health is the central focus of my work | 18% (58) |
| Social health is a part of my work, but not the main focus | 41% (135) |
| Social health is only a small part of my work | 17% (57) |
| Missing | 24% (79) |
Most (n=14, 88%) ERC members participated in the rating phase. Impact scores ranged from 4.14 to 7.79 (mean=6.12). Priority scores ranged from 3.07 to 8.64 (mean=5.61). A total of 24 questions fell into the go-zone (high impact—above the mean of 6.12; high-priority—above the mean of 5.61). A list of the top 10 questions based on combined impact and priority score is offered in Table 2. The question, “Which social risks are critical (for health systems) to address first given their common comorbid presentation and why or must all or an underlying issue be addressed for improvement?” had both the highest impact (7.79) and priority (8.64) scores, for a combined score of 16.43. The top 10 statements covered several themes, including Intervention Approach and Impact (“What are the most cost-effective social health interventions/priorities?”), Technology (“Which patients benefit from digital/technology informed interventions versus which need higher touch care team interventions?”), and Equity (“How do we reach the hard-to-reach individuals and ensure they receive services they need to address social needs?”).
Table 2.
Top 10 Empirical Research Questions
| Combined score ranking | Question number | Question | Impact (average) | Priority (average) | Combined score |
|---|---|---|---|---|---|
| 1 | 2 | Which social risks are critical (for health systems) to address first given their common comorbid presentation and why, or must all or an underlying issue be addressed for improvement? | 7.79 | 8.64 | 16.43 |
| 2 | 17 | To what extent does health system supported connection to community-based resources resolve social needs and lead to improvements in health and reductions in healthcare costs? | 7.36 | 7.50 | 14.86 |
| 3 | 8 | What are the best measures of social health that are sensitive to change and can reveal (predict) intervention impact? | 7.50 | 7.21 | 14.71 |
| 4 | 46 | How do we reach the hard-to-reach individuals and ensure they receive services they need to address social needs? | 7.71 | 6.93 | 14.64 |
| 5 | 15 | What is the most effective approach to identifying people's social needs, connecting to resources, and tracking resolution? | 7.21 | 7.21 | 14.43 |
| 6 | 51 | How can we address social risks/needs that result in avoidable hospitalization? | 7.43 | 6.93 | 14.36 |
| 7 | 49 | What are the most cost-effective social health interventions/priorities? | 7.14 | 7.14 | 14.29 |
| 8 | 44 | Which patients benefit from digital/technology informed interventions versus which need higher touch care team interventions? | 7.21 | 6.93 | 14.14 |
| 9 | 30 | What is the most appropriate, effective, efficient, and patient centered way for health systems to address/acknowledge social health? | 7.07 | 7.00 | 14.07 |
| 10 |
32 |
With whom and when are patients most receptive to conversations about their social health? | 7.36 | 6.64 | 14.00 |
DISCUSSION
Our multistakeholder-engaged, asynchronous web-based modified Concept Mapping activity resulted in 59 unique empirical social health−focused research questions across numerous topics. This broad range of questions reveals the nascency of the evidence base, with fundamental questions arising concerning the nature of social risk (who is most vulnerable, how it manifests) and how and to what extent it is even appropriate for health systems to take on this work.
Most existing social health research tends to be smaller studies with limited generalizability or studies that otherwise lack the capacity for hypothesis testing of cost, utilization, and health outcomes.10, 11, 12 With the new HEDIS (Healthcare Effectiveness Data and Information Set) metric for social determinants of health screening,13 we expect to see healthcare systems’ investment in social health integration continue to outpace the existing evidence base. Therefore, strategically pursuing research questions with rigor is critical to ensuring that social health integration investments provide maximum benefit to patients, providers, and systems. We offer our ranked and topic-driven lists as a guide for other researchers in this space.
Our process can also serve as an example for other systems interested in undertaking their own agenda-setting and social health initiatives. Following our process, SONNET supported a small grants program for ERC members to take on studies in go-zone areas such as patient screening preferences and links between screening, resource connection, and healthcare utilization. We encourage other healthcare systems to form similar networks or partnerships with health services researchers and to use similar measures in tackling high-priority and impactful research questions.
In addition to directly addressing the evidence gaps, this relatively new field needs concerted efforts to grow infrastructure and capacity. For instance, we need to address issues that undermine knowledge accumulation across studies (e.g., multiple screening tools)14 and researcher capacity (e.g., limited training institutes, conference series, journals) to grow and support this new field.
CONCLUSIONS
We present critical research questions ripe for investigation by those invested in integrating social health into healthcare. Although this research agenda is limited by its KP-centric inputs and prioritization, it has the potential for broad-reaching impact because KP is one of the largest nonprofit health plans in the U.S. with more than 12.6 million members. In addition, this work presents a window into a systematic process and empirical possibilities to impact patients’ social health.
CRediT authorship contribution statement
Meagan C. Brown: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. Andrea R. Paolino: Conceptualization, Data curation, Funding acquisition, Investigation, Project administration, Writing – original draft, Writing – review & editing. Caitlin N. Dorsey: Data curation, Investigation, Writing – original draft, Writing – review & editing. Cheryl Kelly: Conceptualization, Investigation, Methodology, Writing – review & editing. Cara C. Lewis: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Writing – original draft, Writing – review & editing.
ACKNOWLEDGMENTS
The sponsor had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Funding was provided by Kaiser Permanente National Community Health.
Declaration of interest: None.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.focus.2023.100101.
Appendix. Supplementary materials
REFERENCES
- 1.Hood CM, Gennuso KP, Swain GR, Catlin BB. County health rankings: relationships between determinant factors and health outcomes. Am J Prev Med. 2016;50(2):129–135. doi: 10.1016/j.amepre.2015.08.024. [DOI] [PubMed] [Google Scholar]
- 2.Park H, Roubal AM, Jovaag A, Gennuso KP, Catlin BB. Relative contributions of a set of health factors to selected health outcomes. Am J Prev Med. 2015;49(6):961–969. doi: 10.1016/j.amepre.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 3.Gennuso KP, Jovaag A, Catlin BB, Rodock M, Park H. Assessment of factors contributing to health outcomes in the eight States of the Mississippi Delta region. Prev Chronic Dis. 2016;13:E33. doi: 10.5888/pcd13.150440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Givens ML, Catlin BB, Johnson SP, et al. What do we know about the drivers of health and equity? A narrative review of graphic representations. Health Equity. 2020;4(1):446–462. doi: 10.1089/heq.2020.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Academies of Sciences Engineering and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on Integrating Social Needs Care into the Delivery of Health Care to Improve the Nation's Health . Integrating Social Care Into the Delivery of Health Care: Moving Upstream to Improve the Nation's Health. National Academies Press (U.S.); Washington, DC: 2019. Five health care sector activities to better integrate social care. [PubMed] [Google Scholar]
- 6.Sandhu S, Wildman JM, Alderwick H, Wildman J, Gottlieb LM. Developing a research agenda for social prescribing in the UK using lessons from the US. Br J Gen Pract. 2022;72(725):589–592. doi: 10.3399/bjgp22X721445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Trochim WMK. An introduction to concept mapping for planning and evaluation. Eval Program Plann. 1989;12(1):1–16. doi: 10.1016/0149-7189(89)90016-5. [DOI] [Google Scholar]
- 8.Concept Systems Incorporated. Concept Systems home page; 2022; https://www.conceptsystems.com/home. Accessed July 20, 2022.
- 9.REDCap [computer program]. Nashville, TN 2022.
- 10.Trochim W, Kane M. Concept mapping: an introduction to structured conceptualization in health care. Int J Qual Health Care. 2005;17(3):187–191. doi: 10.1093/intqhc/mzi038. [DOI] [PubMed] [Google Scholar]
- 11.Gottlieb LM, Wing H, Adler NE. A systematic review of interventions on patients’ social and economic needs. Am J Prev Med. 2017;53(5):719–729. doi: 10.1016/j.amepre.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 12.Yan AF, Chen Z, Wang Y, et al. Effectiveness of social needs screening and interventions in clinical settings on utilization, cost, and clinical outcomes: A systematic review. Health Equity. 2022;6(1):454–475. doi: 10.1089/heq.2022.0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Committee for Quality Assurance; Washington, DC: 2022. Proposed new measure for HEDIS®1 Measurement Year (MY) 2023: Social Need Screening and Intervention (SNS-E) [Google Scholar]
- 14.Henrikson NB, Blasi PR, Dorsey CN, et al. Psychometric and pragmatic properties of social risk screening tools: A systematic review. Am J Prev Med. 2019;57(6)(suppl 1):S13–S24. doi: 10.1016/j.amepre.2019.07.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.