Highlights
-
•
There are widening racial disparities in opioid mortality.
-
•
Black males were 1.5 times more likely to die of opioid overdose than White males.
-
•
Untreated mental health disorders are a risk factor for opioid mortality.
-
•
Early treatment of mental health disorders and opioid use disorder is critical to prevent deaths.
-
•
Comprehensive socioecologic data can identify the precursors to fatal overdoses.
Keywords: Health equity, opioid mortality, opioid use disorder, racial disparities, mental health, population Health
Abstract
Introduction
There were more than 100,000 fatal drug overdoses in the U.S. in 2021 alone. In recent years, there has been a shift in opioid mortality from predominantly White rural communities to Black urban communities. This study aimed to identify the Virginia communities disproportionately affected by the overdose crisis and to better understand the systemic factors contributing to disparities in opioid mortality.
Methods
Using the state all-payer claims database, state mortality records, and census data, we created a multivariate model to examine the community-level factors contributing to racial disparities in opioid mortality. We used generalized linear mixed models to examine the associations between socioecologic factors and fatal opioid overdoses, opioid use disorder diagnoses, opioid-related emergency department visits, and mental health diagnoses.
Results
Between 2015 and 2020, racial disparities in mortality widened. In 2020, Black males were 1.5 times more likely to die of an opioid overdose than White males (47.3 vs 31.6 per 100,000; p<0.001). The rate of mental health disorders strongly correlated with mortality (β=0.53, p<0.001). Black individuals are not more likely to be diagnosed with opioid use disorder (β=0.01, p=0.002) or with mental health disorders (β= −0.12, p<0.001), despite higher fatal opioid overdoses.
Conclusions
There are widening racial disparities in opioid mortality. Untreated mental health disorders are a major risk factor for opioid mortality. Findings show pathways to address inequities, including early linkage to care for mental health and opioid use disorders. This analysis shows the use of comprehensive socioecologic data to identify the precursors to fatal overdoses, which could allow earlier intervention and reallocation of resources in high-risk communities.
INTRODUCTION
More than 100,000 fatal drug overdoses occurred in the U.S. in 2021 alone, largely related to opioid overdoses.1 This represents over a 30% increase in mortality from 2019 to 2020.2 In 2010, the opioid death rate was highest among White people, with a disproportionate impact in rural communities.2,3 In recent years, there has been a shift in mortality, with the sharpest rise among Black people in urban communities.3,4 In 2019, the fatal opioid overdose rate among Black people was disproportionately higher than that of other groups. Among non-Hispanic Black men aged ≥55 years, the mortality rate was 40 per 100,000, 4 times higher than the overall opioid mortality rate of 10 per 100,000 among persons of the same age.4
There is evidence of racial differences in the diagnosis and treatment of opioid use disorder (OUD).5, 6, 7 Black people are less likely to receive a prescription for buprenorphine, a key treatment for OUD, than White people.6 There are significant racial disparities in retention in Office Based Addiction Treatment, with young Black people half as likely to remain in a program for 1 year than White people.7
The National Academies of Sciences, Engineering, and Medicine have called for research addressing the social factors that contribute to health disparities, including race and racism.8 The U.S. Preventive Services Task Force identified racism as a leading cause of inequities in outcomes for preventable conditions and has called for more evidence to understand the structural factors leading to these disparities and the potential interventions that could address the problem.9
Virginia can serve as an important case example for the overdose crisis given the spiking rates of opioid mortality, diversity across race/ethnicity and rurality, and the successful implementation of an Addiction and Recovery Treatment Services (ARTS) benefit through Virginia's Medicaid program. The ARTS benefit aims to improve the identification of substance use disorders and access to addiction treatment services for Medicaid members, with a focus on expanding care in primary care settings.
This study, funded by a Department of Medical Assistance Services Support Act Grant, sought to identify Virginia communities disproportionately suffering from opioid mortality and understand the systemic factors contributing to variation in mortality. We aimed to create a multivariate model to examine the community-level factors contributing to racial disparities in opioid mortality.
METHODS
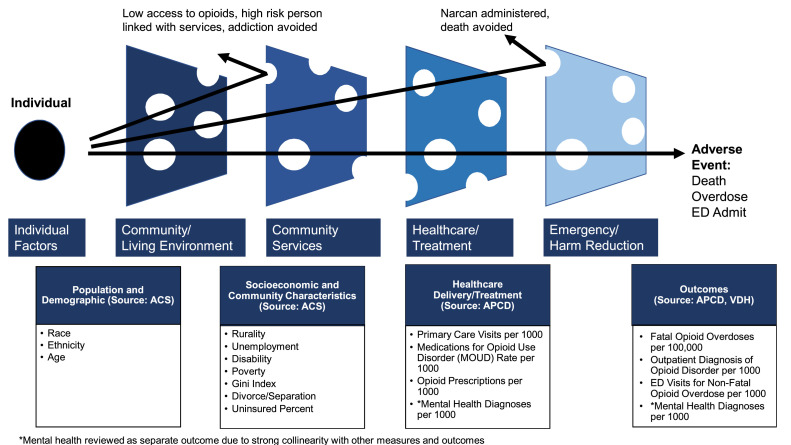
This is a retrospective observational analysis of 2015–2020 data on fatal opioid overdoses and community-level characteristics. We trended fatal opioid overdoses for each census tract and compared the characteristics of communities with at least 1 fatal overdose with the characteristics of those with none. We created a multivariate model to understand the associations between fatal opioid overdoses and community-level characteristics, which was informed by the socioecologic model.10 Figure 1 shows the theoretical model we created to identify key measures and relevant data sources needed to inform our multivariate model. Although many factors contribute to opioid outcomes, we focused on 14 socioecologic factors for which data were available. Strong collinearity between fatal opioid overdoses and mental health diagnoses led us to remove this variable from the model. Instead, we conducted 4 multivariate analyses to understand the associations between various community characteristics with 3 opioid-related outcomes (OUD diagnoses, nonfatal opioid overdoses, and fatal opioid overdoses) and with the rate of mental health diagnoses. We then compared the findings from each multivariate analysis for similarities and differences in factors predicting outcomes. The unit of analysis in the models was the census tract level. The Virginia Commonwealth University IRB deemed this not human subject research.
Figure 1.
Fatal opioid overdose logic model: socioecologic measures and data sources.
Study population
Our sample for analysis included residents and all census tracts throughout Virginia.
Measures
Data sources
Fatal opioid overdose data from 2015 to 2020 were provided by the Virginia Department of Health (VDH) Office of the Chief Medical Examiner. VDH monitors all overdose-related mortality for Virginia residents. Data elements included type of fatal overdose as reported on death records (including prescription opioids, heroin, fentanyl, methamphetamine, and cocaine), contributory/multiple causes of death codes, and residential ZIP code. Death rate was tabulated using ZIP code and then converted to counts per census tract using associated weights between ZIP code and census tracts for Virginia, provided by the U.S. Department of Housing and Urban Development.11
Demographic data and community characteristics were sourced at the census tract level through American Community Survey (ACS) data courtesy of the U.S. Census.12 The 2016–2019 data were used, as detailed below.
Health and prescription outcomes from 2016 to 2019 were queried from the Virginia All-Payer Claims Database (APCD), which includes medical, dental, and pharmacy claims collected from private and public payers.13 Most payers in Virginia are required to report claims, including Medicare, Medicaid managed care, Medicare fee-for-service, Medicare Advantage Care, commercial, and self-insured plans. Each claim and enrollment record includes patient demographics, location of care, providers, diagnoses, and allowed amount of service. Each person in the APCD has a unique identification that allows us to track care across settings and time and to capture the ZIP code of residence. The Virginia APCD has nearly 5 million covered lives of Virginia's 8 million residents.13
Of note, our time trend analysis included VDH mortality data from 2015 to 2020. The multivariate analysis utilized APCD and ACS data from 2016 to 2019 only because this was the data range available from the APCD at the time of analysis.
Summary of Measures
We used different dependent variables for each multivariate model: fatal opioid overdoses per 100,000, OUD diagnoses per 1,000, emergency department (ED) visits for opioid overdose per 1,000, and diagnoses with mental health disorders per 1,000. After reviewing the literature for meaningful gaps, we identified 14 socioecologic factors associated with opioid-related outcomes for inclusion as independent variables in our model. Of note, mental health diagnoses were intended to be included as an independent variable, but given the collinearity with fatal overdoses, we created a separate model using mental health as the dependent variable. The independent variables included the following:
-
•
Population characteristics: percentage of residents who are Black, are Hispanic, and aged >65 years.
-
•
Socioeconomic characteristics: percentage of residents who are unemployed, disabled, impoverished, divorced, and with bachelor's degree education or higher. Gini coefficient, multiplied by 100, was used to measure income inequality.14
-
•
Community characteristics: rurality of census tract, calculated using Rural-Urban Commuting Area codes.15
-
•
Healthcare delivery measures: percentage of residents who are uninsured, rate of primary care provider visits per 1,000 in the past year,16 and rate of medication for OUD (MOUD) prescriptions (e.g., buprenorphine and methadone). Our team created a measure to calculate the ratio of MOUD to opioid prescriptions in a community and calculated a rate per 1,000.
Population characteristics and socioeconomic characteristics were collected from the ACS. Using the total population at each census tract, ACS data were converted to percentages at each tract.
The APCD was used for the healthcare delivery measures, including ICD-10 codes (Appendix Table 1, available online), visit types (e.g., visits with primary care providers, ED visits), visit dates, prescriptions (e.g., prescriptions for opioids, buprenorphine, methadone), and prescription dates. APCD-based measures were converted to rates per 1,000.
Statistical Analysis
Time trend analysis. Fatal opioid overdose rates were calculated annually in 2015–2020. Total and fentanyl-related overdoses were stratified by race and sex, as reported on death records. Fatal overdose rates were calculated by census tract. ACS data were utilized to adjust rates for age and population size. We compared the characteristics of census tracts with at least 1 death with those of census tracts with no deaths.
Multivariate analysis. Data from 2016 to 2019 were used for the multivariate analysis. The year 2019 data were the most recent data available for the APCD at the time of analysis. Four adjusted generalized linear mixed models were used to examine the associations between the 14 total socioecologic factors and our main outcomes (dependent variables): fatal opioid overdoses per 100,000, OUD diagnosis per 1,000, ED visits for opioid overdose per 1,000, and diagnosis with mental health disorder per 1,000. For each year 2016–2019, population estimates for every census tract in Virginia were pulled from the ACS. APCD measures were calculated annually in 2016–2019, tabulated by ZIP code using residential ZIP code, and then converted to counts per census tract. From each model, parameter estimates and p-values are reported. This manuscript reports on 2019 data from the multivariate analysis because there were only minor year-to-year differences that do not impact the interpretation of findings. We qualitatively compared the findings from each of the 4 multivariate analyses to review similarities and differences.
All data cleaning, structuring, and arranging were performed using R software. All statistical analyses were performed at a 5% statistical significance level using SAS Statistical Software, Version 9.4 (SAS Institute, Cary, NC). We considered coefficients <0.2 as not clinically meaningful, consistent with previous literature.17,18 Coefficients <0.2 would not lead to substantial differences in any rate on the basis of the 1,000; 10,000; or 100,000 scales, even if the values were statistically significant (likely owing to large sample size).17,18
RESULTS
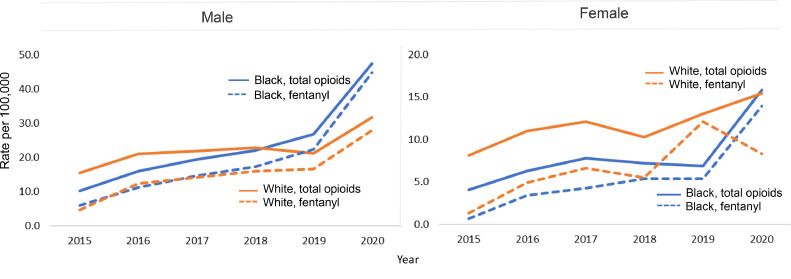
Between 2015 and 2020, the rate of fatal opioid overdoses in Virginia increased from 10.8 to 25.1 deaths per 100,000 residents, with a 48.5% increase in 2020 alone (Appendix Table 2, available online). Although the rate of fatal opioid overdoses increased for both Black males and White males between 2015 and 2020, the rate of increase was significantly greater for Black males (Figure 2). In 2020, Black males were 1.5 times more likely to die of an opioid overdose than White males (47.3 vs 31.6 per 100,000; p<0.001). In 2015, fatal opioid overdose rates were similar for Black and White females, but by 2020, the proportion of Black female deaths was higher (p<0.001). Rates for Black females increased by 129% between 2019 and 2020, nearly 7 times the percentage increase for White females (Figure 2).
Figure 2.
Race-specific sex differences in total opioid and fentanyl-related mortality (rate per 100,000).
Most fatal opioid overdoses for both Black and White males and females were due to fentanyl. Notably, there was a sharp decrease in fentanyl deaths from 2019 to 2020 for White females.
Community factors associated with fatal opioid overdoses. Among the 1,907 census tracts in Virginia, 1,322 had at least 1 resident with an opioid death in 2019. Communities with 1 or more deaths had a higher proportion of Black and Hispanic residents and more uninsured people than communities with no deaths (Table 1). Communities at all levels of education, affluence, (dis)ability, and primary care visit rate were at risk for having a fatal opioid overdose. Communities with at least 1 death were largely urban (92.6%). Most urban communities (75.1%) had at least 1 death, compared with 45.1% of suburban and only 17.4% of rural communities.
Table 1.
Comparison of Census Tracts in 2019 With 1 or More Fatal Opioid Overdose Versus Census Tracts With No Deaths
| Category and measurements | Overall (minimum, maximum), n=1,907 | Census tracts with at least 1 death (minimum, maximum), n=1,322 |
Census tracks with no deaths (minimum, maximum), n=585 |
|---|---|---|---|
| Population characteristics | |||
| Race, White, % | 67.4 (0.5, 100.0) | 63.3 (0.5, 100.0) | 77.0 (2.7, 100.0) |
| Race, Black, % | 20.4 (0.0, 97.2) | 23.1 (0.0, 97.2) | 13.9 (0.0, 95.3) |
| Hispanic, % | 8.7 (0.0, 77.0) | 9.9 (0.0, 77.0) | 5.8 (0.0, 62.9) |
| Age, ≥65 years, % | 15.6 (0.0, 100.0) | 14.7 (0.0, 100.0) | 17.9 (0.0, 40.9) |
| Foreign born, % | 4.7 (0.0, 16.8) | 4.9 (0.0, 77.0) | 4.3 (0, 13.0) |
| Population size | 4,433.4 (0.0, 19,438.0) | 4,486.6 (5.0, 14,761.0) | 4,313.1 (0.0, 19,438.0) |
| Socioeconomic characteristics | |||
| Education, Bachelor's degree+, % | 14.7 (0.0, 50.0) | 15.2 (0.0, 50.0) | 13.7 (0.0, 39.2) |
| Unemployment, not working, % | 30.8 (0.0, 100.0) | 29.7 (0.0, 100.0) | 33.3 (0.0, 100.0) |
| Disability, % | 12.0 (0.0, 37.7) | 11.5 (0.0, 33.8) | 13.3 (0.0, 37.7) |
| Poverty, % | 11.0 (0.0, 80.1) | 10.9 (0.0, 80.1) | 11.2 (0.0, 80.0) |
| Gini coefficienta | 40.7 (5.6, 79.4) | 40.3 (5.6, 79.4) | 41.6 (24.8, 70.2) |
| Separate/divorced, % | 10.6 (0.0, 100.0) | 10.6 (0.0, 100.0) | 10.4 (0.0, 42.4) |
| Uninsured, % | 8.4 (0.0, 40.5) | 8.6 (0.0, 40.5) | 7.9 (0.0, 31.5) |
| Healthcare delivery and treatment measures | |||
| ED overdose rate per 1,000 | 0.3 (0.0, 2.5) | 0.4 (0.0, 2.5) | 0.2 (0.0, 1.7) |
| ED opioid-related disorder rate per 1,000 | 0.6 (0.0, 5.4) | 0.6 (0.0, 5.4) | 0.5 (0.0, 4.7) |
| OP opioid-related disorder rate per 1,000 | 1.3 (0.0, 19.6) | 1.2 (0.0, 16.1) | 1.5 (0.0, 19.6) |
| Opioid prescription rate per 1,000 | 132.9 (0.0, 1,877.7) | 128.9 (0.0, 1,877.7) | 141.9 (0.0, 427.8) |
| MOUD/opioid prescription per 1,000b | 17.2 (0.0, 163.7) | 16.3 (0.0, 163.7) | 19.1 (0.0, 112.8) |
| Rate of visits with primary care provider per 1,000 | 442.8 (0.0, 5,245.8) | 444.2 (0.4, 5,245.8) | 439.6 (0.0, 1,023.2) |
Gini coefficient, multiplied by 100, was used to represent income inequality.
Refers to the measure created that calculated the ratio of MOUD, including methadone and buprenorphine, prescriptions to opioid prescriptions in a community.
ED, emergency department; MOUD, medication for opioid use disorder; OP, outpatient.
Opioid mortality was strongly correlated with the rate of mental health diagnosis per 1,000 (β=0.53, p<0.001). Communities with no deaths had a higher ratio of MOUD prescriptions to opioid prescriptions per 1,000 (19.1 vs 16.3).
Multivariate analysis. The results of the generalized linear mixed models, run for 4 main dependent variables (fatal opioid overdoses per 100,000, OUD diagnosis per 1,000, ED visits for opioid overdose per 1,000, and diagnosis with mental health disorder per 1,000), are notable for the following (Table 2):
Table 2.
Multivariate Analysis for Outcomes of Mortality, Mental Health, Opioid Overdose, and Opioid Use Disorder (2019)
| Covariates | Fatal opioid overdose per 100,000 |
ED visit for opioid overdose per 1,000 |
OUD diagnosis per 1,000 |
Mental health diagnosis per 1,000 |
||||
|---|---|---|---|---|---|---|---|---|
| Estimate (β) | p-value | Estimate (β) | p-value | Estimate (β) | p-value | Estimate (β) | p-value | |
| Population characteristics | ||||||||
| Race, Black % | 0.280 | <0.001 | 0.010 | <0.001 | 0.010 | <0.001 | −0.120 | <0.001 |
| Hispanic % | 0.060 | 0.182 | 0.000 | 0.957 | −0.010 | 0.003 | −1.020 | <0.001 |
| Age, >65 years, % | −0.090 | 0.157 | 0.003 | 0.098 | −0.010 | 0.156 | −0.160 | 0.101 |
| Socioeconomic characteristics | ||||||||
| Bachelor's degree+, % | 0.110 | 0.055 | −0.002 | 0.242 | −0.010 | 0.193 | −0.900 | <0.001 |
| Not working, % | −0.001 | 0.991 | −0.003 | 0.033 | −0.004 | 0.353 | −0.100 | 0.148 |
| Disabled, % | 0.250 | 0.007 | 0.010 | 0.076 | 0.040 | <0.001 | 0.570 | <0.001 |
| Impoverished, % | −0.120 | 0.011 | 0.000 | 0.949 | −0.002 | 0.735 | 0.180 | 0.014 |
| Gini coefficient | −4.610 | 0.395 | −0.150 | 0.308 | 0.500 | 0.352 | 35.870 | <0.001 |
| Divorce/separation, % | 0.310 | <0.001 | 0.010 | <0.001 | 0.010 | 0.193 | 0.760 | <0.001 |
| Community characteristics | ||||||||
| Rurality (ref=rural) Suburban |
4.440 |
0.013 |
0.210 |
<0.001 |
0.200 |
0.263 |
5.170 |
0.051 |
| Urban | 10.180 | <0.001 | 0.390 | <0.001 | 0.230 | 0.158 | 1.610 | 0.506 |
| Healthcare delivery | ||||||||
| Rate of visits with primary care provider per 1,000 | 0.020 | <0.001 | 0.001 | <0.001 | 0.002 | <0.001 | 0.270 | <0.001 |
| MOUD/opioid prescriptions per 1,000a | 0.680 | <0.001 | 0.060 | <0.001 | 0.560 | <0.001 | 2.750 | <0.001 |
| Uninsured % | 0.080 | 0.327 | −0.002 | 0.408 | 0.010 | 0.396 | 0.160 | 0.173 |
Note: Boldface indicates statistical significance (p≤0.05).
Refers to measure created that calculated the ratio of MOUD, including methadone and buprenorphine, prescriptions to opioid prescriptions in a community.
MOUD, medication for opioid use disorder.
Fatal opioid overdoses per 100,000. After adjusting for other factors, there was a positive association between fatal opioid overdose rate and Black race (β=0.28, p<0.001), disability (β=0.25, p=0.007), and divorce/separation (β=0.31, p<0.001). There were higher fatal opioid overdoses in urban areas (β=10.18; p<0.001) and suburban areas (β=4.44; p=0.013) than in rural areas. There was a positive association between fatal overdoses and proportion of MOUD to opioid prescriptions (β=0.68, p<0.001).
Emergency department visits for opioid overdose per 1,000. There was a slight positive association between Black residents and ED visits for opioid overdose, which was statistically significant but not clinically significant (β=0.01, p<0.001). There were higher ED visits for overdoses in urban areas (β=0.39; p<0.001) and suburban areas (β=0.21; p<0.001) than in rural areas. There was a slight positive association between ED visits and the rate of MOUD prescriptions, which was not clinically significant (β=0.06, p<0.001).
Opioid use disorder diagnosis per 1,000. There were no clinically significant associations between OUD and Black race (β=0.01, p=0.002), disability (β=0.04, p<0.001), or divorce/separation (β=0.01, p=0.193). There was a positive association with the proportion of MOUD to opioid prescriptions (β=0.56, p<0.001).
Diagnosis with mental health disorder per 1,000. There was a slight negative association between mental health diagnosis and Black race (β= −0.12, p<0.001). There was a positive association between mental health diagnosis and disability (β=0.57, p<0.001), poverty (β=0.18, p=0.014), and divorce/separation (β=0.76, p<0.001), whereas there was a negative association with bachelor's degrees (β= −0.90, p<0.001) and Hispanic ethnicity (β= −1.02, p<0.001). There was a higher rate of mental health diagnoses in suburban areas (β=5.17; p=0.05) than in rural areas. In addition, there was a positive association between mental health diagnoses and MOUD rate (β=2.75, p<0.001) and primary care visits (β=0.27, p<0.001).
Many of the factors that were strongly correlated with the rate of mental health diagnoses were also strongly correlated with fatal opioid overdoses, yet not with the rate of opioid overdoses or diagnosis with OUD, including percentage disability and percentage divorced/separated.
DISCUSSION
Our results highlight widening racial disparities in opioid-related outcomes in Virginia and identify potential mechanisms. Fatal opioid overdoses are shifting from rural White to urban Black communities. The coronavirus disease 2019 (COVID-19) pandemic has highlighted and amplified racial disparities in opioid mortality, with spiking opioid mortality rates among Black individuals in 2020. This increase in deaths has been hypothesized to be related to reduced access to healthcare and recovery support services during the pandemic as well as to severe socioeconomic stressors such as job loss and housing instability.19,20 Our research indicates that we may be missing opportunities for diagnosing and treating both OUD and mental health comorbidities, which amplifies the risk of fatal overdose.
Our unique analysis, comparing 4 outcomes using the same socioecologic framework of independent variables in 4 multivariate analyses, elucidates the factors leading to changes in fatal opioid overdoses. Black individuals are more likely to have fatal opioid overdoses yet are less likely to have ED visits for opioid overdoses or outpatient diagnoses of OUD. Missing key opportunities for intervention, such as early recognition and linkage to treatment for OUD and mental health disorders, may contribute to racial disparities in opioid mortality. Lack of early linkage to treatment could be explained by a variety of factors. Black persons are less likely to be referred to MOUD programs and have lower 1-year retention than White persons.7,21 Older Black individuals are more likely to have their substance use treatment terminated at a facility than White individuals.22 Previous literature has indicated increased access to buprenorphine among White patients compared with that among other races.6,23 Although Black and Hispanic communities may have more proximity to facilities that provide methadone,24 methadone procedures and practice have been deemed liquid shackles with stigmatizing barriers, including observed daily dosing, regular urine drug screens, transportation, and limits on access to take-home medication.25,26 MOUDs more broadly continue to face stigma, including skepticism from clinicians.27 Furthermore, the lack of quality control for illicit drug supplies likely contributes to the racial disparities in fatal overdoses. Black and Hispanic communities experienced particularly significant increases in overdose deaths involving synthetic opioids, which may be a result of drug supply contamination.3
Leveling out of opioid mortality rates among rural communities may also be explained by resources invested in this population. In 2017, Virginia implemented the ARTS benefit to improve the recognition of substance use disorders and access to addiction treatment services for Medicaid members.28 This program focused largely on rural communities given their heightened risk for opioid overdoses at the time. The program trained clinicians and ultimately led to a surge in addiction treatment services in Virginia, including pharmacotherapy and counseling. The supply of clinicians authorized to prescribe buprenorphine more than doubled,28 and there was a 26% increase in Medicaid members receiving MOUD.29 These programs could contribute to the decrease in fentanyl-related mortality among White women in 2019–2020, although the reason for this is unclear. However, Black residents have not benefited from these interventions equitably. Treatment rates of substance use disorder remain higher in White Medicaid members (56%) than in Black Medicaid members (40%).28 It is essential to reprioritize treatment initiatives and redirect resources to Black urban communities where opioid deaths are spiking.
Our findings also indicate that mental health conditions co-occurring with OUD are a major risk for fatal overdose. Several factors that strongly correlate with opioid mortality (e.g., disability, divorce/separation, and urbanicity) also correlate with receiving a mental health diagnosis. Communities with missed opportunities for early OUD diagnosis also have missed mental health diagnoses related to overall less interaction with the healthcare system, which can compound the risk for opioid mortality.30
Furthermore, there are known racial disparities in the identification of mental health disorders, access to care, and stigma around seeking or accepting mental health treatment.31, 32, 33 Black individuals are less likely than White individuals to have received mental health services in the past year32 and may have fewer opportunities for diagnosis. When receiving care, it is more likely to be of poorer quality.33 There is a stark lack of diversity among mental health providers, with fewer than 3% of psychologists being Black.34 Improving access to and diversity of our mental health workforce is one piece of the puzzle essential for addressing inequities in mental health treatment. Other key solutions include training a more culturally responsive mental health workforce along with the most salient issue of addressing the upstream roots of systemic racism in the U.S. that has led to bias and racism exhibited in mental health diagnosis and treatment of historically marginalized communities.35
Policies are needed that promote early diagnosis and treatment of OUD, equitable access to mental health services, and early identification of at-risk communities. Previous studies have shown that starting medications for opioid use after a nonfatal overdose reduces the risk of future mortality,36 yet most opioid overdose survivors do not start MOUD.35,37 Establishing programs that expand access to early diagnosis and treatment of OUD is critical for addressing the overdose crisis.
Lack of mental health treatment infrastructure may be a critical gap as we look toward reducing opioid mortality. The U.S. mental health treatment infrastructure has been notoriously underfunded and overburdened, contributing to many individuals with co-occurring substance use and mental health disorders not receiving mental health care.38 It is imperative that we strengthen infrastructure to diagnose and treat mental health and substance use disorders, with particular attention to racial inequities in availability and access to treatment. Finally, this study identified several factors that contribute to fatal overdoses in the community, including racial disparities, disability, and mental health comorbidity. Policies on care delivery and resources should prioritize proactively identifying and allocating sufficient resources for communities that appear to be at greater risk of opioid mortality.
This study shows the value and feasibility of using comprehensive socioecologic data to identify contextual factors for fatal overdoses in a community. Investing in comprehensive collection and monitoring of socioecologic data are critical to addressing the overdose crisis at the state and national levels. This would allow for rapid identification of trends and reallocation of resources before deaths increase in communities and create a more nimble and effective public health response system.
Limitations
Limitations of this analysis include a lack of uninsured patients in claims data. APCD data were available through 2019 at the time of this analysis. We focused on disparities between Black and White persons owing to the stark rate of rise of fatal overdoses among Black individuals seen in our early analysis; however, additional research on disparities based on other racial/ethnic identities is essential. Data show correlation, although caution should be taken when inferring causation.
CONCLUSIONS
This study highlights the widening racial disparities in opioid mortality and identifies specific socioecologic factors contributing to these disparities. Our findings show that concurring mental health disorders and OUDs may be a major predictor of death and highlight inequities in early outpatient OUD and mental health treatment. Furthermore, this analysis shows the utility of comprehensive socioecologic data to identify fatal overdose precursors in a community. Early identification of at-risk communities along with equitable access to critical resources could allow the opportunity to intervene and allocate resources for the prevention of fatal opioid overdoses.
Acknowledgments
ACKNOWLEDGMENTS
This study was funded by a Department of Medical Assistance Services Support Act Grant. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Declaration of interest: none.
CRediT author statement
Jacqueline B. Britz: Conceptualization, Methodology, Investigation, Writing – original draft. Kristen M. O'Loughlin: Data curation, Writing – original draft. Tracey L. Henry: Data curation, Writing – original draft. Alicia Richards: Methodology, Formal analysis, Data curation, Writing – original draft. Roy T. Sabo: Methodology, Formal analysis, Writing – review & editing. Heather G. Saunders: Conceptualization, Data curation, Visualization, Writing – review & editing. Sebastian T. Tong: Data curation, Writing – review & editing. E. Marshall Brooks: Data curation, Writing – review & editing. Jason Lowe: Conceptualization, Data curation, Writing – review & editing, Funding acquisition. Ashley Harrell: Conceptualization, Data curation, Writing – review & editing, Funding acquisition. Christine Bethune: Conceptualization, Data curation, Writing – review & editing, Funding acquisition. F. Gerard Moeller: Conceptualization, Data curation, Writing – review & editing, Funding acquisition. Alex H. Krist: Conceptualization, Methodology, Writing – original draft, Supervision.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.focus.2023.100102.
Appendix. Supplementary materials
REFERENCES
- 1.U.S. Overdose Deaths In 2021 Increased Half as much as in 2020 - But Are Still Up 15%; Published 2022. https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2022/202205.htm. Accessed September 9, 2022.
- 2.Hedegaard H, Miniño AM, Spencer MR, Warner M. Drug overdose deaths in the United States,1999–2020, NCHS Data Brief, 428, 2021, National Center for Health Statistics; Hyattsville, MD. 10.15620/cdc:112340, Accessed January 18, 2023. [DOI]
- 3.Lippold KM, Jones CM, Olsen EO, Giroir BP. Racial/ethnic and age group differences in opioid and synthetic opioid-involved overdose deaths among adults aged ≥18 years in metropolitan areas - United States, 2015–2017. MMWR Morb Mortal Wkly Rep. 2019;68(43):967–973. doi: 10.15585/mmwr.mm6843a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mason M, Soliman R, Kim HS, Post LA. Disparities by sex and race and ethnicity in death rates due to opioid overdose among adults 55 years or older, 1999 to 2019. JAMA Netw Open. 2022;5(1) doi: 10.1001/jamanetworkopen.2021.42982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mennis J, Stahler GJ. Racial and ethnic disparities in outpatient substance use disorder treatment episode completion for different substances. J Subst Abuse Treat. 2016;63:25–33. doi: 10.1016/j.jsat.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 6.Lagisetty PA, Ross R, Bohnert A, Clay M, Maust DT. Buprenorphine treatment divide by race/ethnicity and payment. JAMA Psychiatry. 2019;76(9):979–981. doi: 10.1001/jamapsychiatry.2019.0876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weinstein ZM, Kim HW, Cheng DM, et al. Long-term retention in Office Based Opioid Treatment with buprenorphine. J Subst Abuse Treat. 2017;74:65–70. doi: 10.1016/j.jsat.2016.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on Integrating Social Needs Care into the Delivery of Health Care to Improve the Nation's Health . National Academies Press(U.S.); 2019. Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation's Health.http://www.ncbi.nlm.nih.gov/books/NBK552597/ Accessed July 4, 2022. [Google Scholar]
- 9.US Preventive Services Task Force. Davidson KW, Mangione CM, et al. Actions to transform US Preventive Services Task Force methods to mitigate systemic racism in clinical preventive services. JAMA. 2021;326(23):2405–2411. doi: 10.1001/jama.2021.17594. [DOI] [PubMed] [Google Scholar]
- 10.Bronfenbrenner U. Sage Publications Ltd.; 2004. Making Human Beings Human: Bioecological Perspectives on Human Development. [Google Scholar]
- 11.The U.S. Department of Housing and Urban Development's (HUD's) Office of Policy Development and Research (PD&R). HUD USPS. ZIP code crosswalk files | HUD user. 2020. https://www.huduser.gov/portal/datasets/usps_crosswalk.html. Accessed August 29, 2022.
- 12.Bureau UC. American Community Survey (ACS). Census.gov. https://www.census.gov/programs-surveys/acs. Accessed July 4, 2022.
- 13.All Payer Claims Database (APCD).Virginia Health Information. http://vhi.org/APCD/. Accessed July 4, 2022.
- 14.Bureau UC. Gini index. Census.gov. 2021. https://www.census.gov/topics/income-poverty/income-inequality/about/metrics/gini-index.html. Accessed July 4, 2022.
- 15.USDA, ERS. Rural-Urban Commuting Area Codes. 2019. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx. Accessed July 4, 2022.
- 16.Huffstetler A, Sabo R, Krist A, et al. Using a State All-Payer Claims Data to Identify the Active Primary Care Workforce: A Novel Study in Virginia. Ann Fam Med. 2022;20(5):446–451. doi: 10.1370/afm.2854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chan YH. Biostatistics 104: correlational analysis. Singapore Med J. 2003;44(12):614–619. [PubMed] [Google Scholar]
- 18.Dancey CP, Reidy J. Eighth edition. Pearson; 2020. Statistics Without Maths for Psychology. [Google Scholar]
- 19.Opioids and the COVID-19 pandemic. Opioids. https://www.ihs.gov/opioids/covid19/. Accessed January 16, 2023.
- 20.Manchikanti L, Vanaparthy R, Atluri S, Sachdeva H, Kaye AD, Hirsch JA. COVID-19 and the opioid epidemic: two public health emergencies that intersect with chronic pain. Pain Ther. 2021;10(1):269–286. doi: 10.1007/s40122-021-00243-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Entress RM. The intersection of race and opioid use disorder treatment: A quantitative analysis. J Subst Abuse Treat. 2021;131 doi: 10.1016/j.jsat.2021.108589. [DOI] [PubMed] [Google Scholar]
- 22.Grooms J, Ortega A. Substance use disorders among older populations: what role do race and ethnicity play in treatment and completion? J Subst Abuse Treat. 2022;132 doi: 10.1016/j.jsat.2021.108443. [DOI] [PubMed] [Google Scholar]
- 23.Hansen H, Siegel C, Wanderling J, DiRocco D. Buprenorphine and methadone treatment for opioid dependence by income, ethnicity and race of neighborhoods in New York City. Drug Alcohol Depend. 2016;164:14–21. doi: 10.1016/j.drugalcdep.2016.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goedel WC, Shapiro A, Cerdá M, Tsai JW, Hadland SE, Marshall BDL. Association of racial/ethnic segregation with treatment capacity for opioid use disorder in counties in the United States. JAMA Netw Open. 2020;3(4) doi: 10.1001/jamanetworkopen.2020.3711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Frank D, Mateu-Gelabert P, Perlman DC, Walters SM, Curran L, Guarino H. "It's like ‘liquid handcuffs”: the effects of take-home dosing policies on Methadone Maintenance Treatment (MMT) patients’ lives. Harm Reduct J. 2021;18(1):88. doi: 10.1186/s12954-021-00535-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Peterson JA, Schwartz RP, Mitchell SG, et al. Why don't out-of-treatment individuals enter methadone treatment programmes? Int J Drug Policy. 2010;21(1):36–42. doi: 10.1016/j.drugpo.2008.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Volkow ND, Frieden TR, Hyde PS, Cha SS. Medication-assisted therapies — tackling the opioid-overdose epidemic. N Engl J Med. 2014;370(22):2063–2066. doi: 10.1056/NEJMp1402780. [DOI] [PubMed] [Google Scholar]
- 28.Addiction and Recovery Treatment Services (ARTS) policy briefs: Access, Utilization, and Quality of Care 2016 - 2019. Department of Health Behavior and Policy - VCU School of Medicine; 2021. https://hbp.vcu.edu/media/hbp/policybriefs/pdfs/FinalARTS3yearcomprehensivereportforPublishing_07142021(1).pdf [Google Scholar]
- 29.Barnes A, Cunningham P, Walker L, et al. AcademyHealth. 2018. Changes in utilization of treatment services and emergency department visits among Medicaid members with opioid use disorders following implementation of Virginia's addiction and recovery treatment services program.https://academyhealth.confex.com/academyhealth/2018ig/meetingapp.cgi/Paper/25112 Accessed July 25, 2022. [Google Scholar]
- 30.Kelly TM, Daley DC, Douaihy AB. Treatment of substance abusing patients with comorbid psychiatric disorders. Addict Behav. 2012;37(1):11–24. doi: 10.1016/j.addbeh.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eylem O, de Wit L, van Straten A, et al. Stigma for common mental disorders in racial minorities and majorities a systematic review and meta-analysis. BMC Public Health. 2020;20(1):879. doi: 10.1186/s12889-020-08964-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McGregor B, Li C, Baltrus P, et al. Racial and ethnic disparities in treatment and treatment type for depression in a national sample of Medicaid recipients. Psychiatr Serv. 2020;71(7):663–669. doi: 10.1176/appi.ps.201900407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.National healthcare quality & disparities reports; 2010 National healthcare disparities report. Agency for Healthcare Research and Quality (AHRQ). https://www.ahrq.gov/research/findings/nhqrdr/index.html. Accessed July 4, 2022.
- 34.2015. APA survey of psychology health service providers. American Psychological Association. https://www.apa.org. Accessed July 4, 2022. https://www.apa.org/workforce/publications/15-health-service-providers.
- 35.Frazier W, Cochran G, Lo-Ciganic WH, et al. Medication-assisted treatment and opioid use before and after overdose in Pennsylvania Medicaid. JAMA. 2017;318(8):750–752. doi: 10.1001/jama.2017.7818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Larochelle MR, Bernson D, Land T, et al. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality: A cohort study. Ann Intern Med. 2018;169(3):137–145. doi: 10.7326/M17-3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Naeger S, Mutter R, Ali MM, Mark T, Hughey L. Post-discharge treatment engagement among patients with an opioid-use disorder. J Subst Abuse Treat. 2016;69:64–71. doi: 10.1016/j.jsat.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 38.Novak P, Feder KA, Ali MM, Chen J. Behavioral health treatment utilization among individuals with co-occurring opioid use disorder and mental illness: evidence from a national survey. J Subst Abuse Treat. 2019;98:47–52. doi: 10.1016/j.jsat.2018.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.