HIGHLIGHTS
-
•
We used lifetable modeling for the Australian population.
-
•
Adherence to physical activity guidelines reduces anxiety and depression by 4%–7%.
-
•
This reduces lifetime burden by gains >0.5 million health-adjusted life years for each outcome.
-
•
This reduces lifetime healthcare costs by >AU$5 billion for each outcome (anxiety and depression).
Keywords: Physical activity, anxiety, depression, mental health, Australia
Abstract
Introduction
Mental disorders, in particular, depressive and anxiety disorders, are a leading cause of disability in Australia and globally. Physical activity may reduce the incidence of anxiety and depression, and this supports the inclusion of physical activity in strategies for the prevention of mental ill health. Policy makers need to know the potential impact and cost savings of such strategies. We aimed to quantify the impact of changes in physical activity on the burden of anxiety and depression and healthcare costs in Australia.
Methods
We used a proportional multistate lifetable model to estimate the impact of changes in physical activity levels on anxiety and depression burdens for the 2019 Australian population (numbering 24.6 million) over their remaining lifetime. The changes in physical activity were modeled through 3 counterfactual scenarios informed by policy targets: attainment of the Australian Physical Activity Guidelines and achievement of the WHO Global Action Plan on Physical Activity targets of a 10% relative reduction in the prevalence of insufficient physical activity by 2025 and a 15% relative reduction by 2030.
Results
If all Australians adhered to the recommended minimum physical activity levels, in 25 years’ time, the burden of anxiety could be reduced by up to 6.4% (95% uncertainty intervals=2.5, 10.6), and that of depression could be reduced by 4.4% (95% uncertainty intervals=2.3, 6.5). Over the lifetime of the 2019 Australian population, the gains could add up to 640,592 health-adjusted life years for anxiety (26 health-adjusted life years per 1,000 persons), 523,717 health-adjusted life years for depression (21 health-adjusted life years per 1,000 persons), and healthcare cost savings of 5.4 billion Australian dollars for anxiety (220 Australian dollars per capita) and 5.8 billion for depression (237 Australian dollars per capita).
Conclusions
Adherence to the Australian physical activity guidelines and achievement of the 2025 and 2030 global physical activity targets could lead to a substantial reduction of the burden of anxiety and depression. This study provides empirical support for the inclusion of physical activity in strategies for the prevention of mental ill health. Future studies should also assess the size and distribution of the benefits for different socioeconomic and ethnic groups.
Graphical Abstract
INTRODUCTION
Mental disorders, in particular, depressive and anxiety disorders, are a leading cause of disability worldwide.1 In Australia, mental disorders were the fourth leading cause of disability in 2019, with 4.3 million prevalent cases.1 Depressive and anxiety disorders constituted 57% of this burden, which further increased owing to the coronavirus disease 2019 (COVID-19) pandemic‒induced impairment in work and social functioning.2,3 People experiencing severe mental health conditions also die as many as 2 decades prematurely because of preventable physical conditions.4,5
Staying active regularly has been identified as essential for good mental health.6, 7, 8 Prospective studies suggest that physical activity (PA) may reduce the incidence of depression and anxiety.9,10 More than half (55%) of adults in Australia do not meet the recommended PA guidelines,11,12 and people living in socioeconomically disadvantaged communities tend to be less active.13
The Australian national mental health policy and the mental health plan emphasize the need for efforts that prevent the onset of mental ill health.14,15 In a companion paper,16 we systematically reviewed the available epidemiologic evidence to establish the relationship between PA and incident cases of anxiety and depression. We found that PA may reduce the incidence of anxiety and depression by up to 17% and 26%, respectively, and judged the relationship to be probably causal. In this paper, we use these findings in a proportional multistate lifetable (pMSLT) modeling study to quantify the impacts of an increase in PA levels on the burden of anxiety and depression and healthcare costs in Australia. The pMSLT modeling is an established approach that has been used previously in Australia to estimate the health and economic impacts of various preventive health strategies.17, 18, 19, 20 Specifically, several studies have applied this method to investigate the health and economic impact of strategies that increase PA such as PA intervention programs in various settings and strategies that increase the use of active transport.21, 22, 23, 24, 25 In New Zealand, Mizdrak and colleagues26 used the pMSLT to estimate the health and economic gains that would occur if the 2018 Global Action Plan for Physical Activity target was met. Our study expands research in this area and introduces a novel aspect wherein we estimate the health and economic impact of PA on anxiety and depression, outcomes not included in the previous studies.
Our study was part of a broader project commissioned by the New South Wales (NSW) Ministry of Health to value the health benefits of active transport. We developed the NSW Active Transport Health model and sought to include all relevant health outcomes that have sufficiently strong epidemiologic evidence of an association with active transport. On the basis of the findings in our companion paper,16 anxiety and depression were included as health outcomes within the NSW Active Transport Health model.27
METHODS
Study Population
We applied epidemiologic modeling to estimate the impact of changes in the Australian population's PA levels on anxiety and depression burdens. We used a pMSLT model28 to simulate the 2019 Australian population in 5-year age groups over their remaining lifetime (Appendix Figure 1, available online). The pMSLT method copes with multiple diseases and allows for comorbidity. The 2 conditions were modeled independently as 2 separate mental-health outcomes.28, 29, 30 We used the Guidelines for Accurate and Transparent Health estimates Reporting checklist to guide the documenting of our modeling data and methods.31
Measures
We used PA data from the Australia National Health Survey 2017–2018 (Appendix Table 1, available online).11 We calculated weekly PA levels by multiplying the minutes of total weekly PA by the average MET of task.32 To convert the weekly PA levels to METs, we used the activity categories of walking, moderate PA, and vigorous PA that were reported in the Australia National Health Survey microdata (walking=3.5METs, moderate PA=5METs, and vigorous PA=7.5METs). PA was modeled as a categorical approximation of a Dirichlet distribution, a generalization of the Beta distribution to multiple categories.33 For the model, PA was categorized into 4 levels: inactive (0 MET), low active (>0 and <600 MET minutes per week), moderately active (≥600 and <1,600 MET minutes per week), and highly active (≥1,600 MET minutes per week). The average MET minutes for each PA category except inactive were assigned a lognormal distribution.
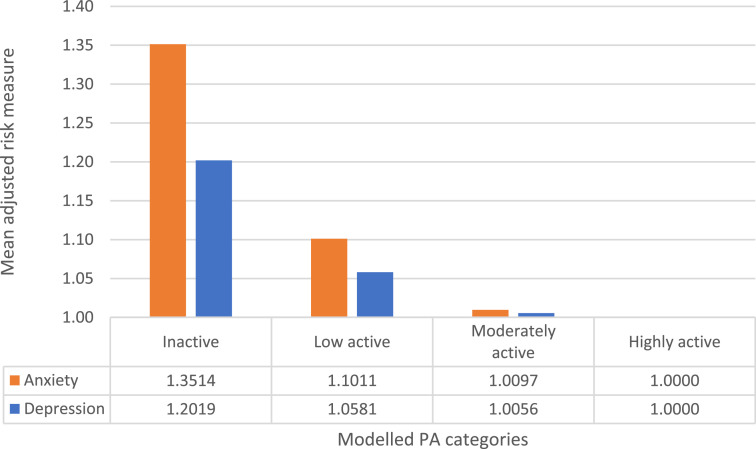
In this study, we used the measures of association from our systematic review of reviews study whose findings are reported in a companion paper.16 In summary, we found sufficient evidence to support an association between PA and incident cases of anxiety and depression. The association was graded as a probable causal relationship on the basis of the Bradford Hill criteria34,35 and the World Cancer Research Fund grading system.36 To model the association between PA and depression, we used the adjusted RR=0.83 (95% CI=0.76, 0.90),37 and for the association between PA and anxiety, we used the adjusted OR=0.74 (95% CI=0.62, 0.88).38 The resulting risk chart is shown in Figure 1.37,38 We assumed that the lowest and highest PA categories reported for the measures of association37,38 refer to the inactive and highly active categories in our model, respectively. To derive the measures of association for all the 4 modeled PA categories, scaling was done to interpolate values between the lowest and highest PA level categories using the findings from the meta-analysis by Ekelund et al.39 because PA is measured relatively precisely using accelerometry. In their review, studies with good-quality PA exposure measures showed diminishing returns with increasing PA levels. We assume that this also applies to the outcomes of our study. This means that the greatest reduction in risk per unit of PA is seen in the lowest PA category, and the health gains diminish at higher levels of PA (Figure 137,38). We modeled the risk measures as lognormally distributed.40
Figure 1.
RR of incident anxiety and depression by the level of PA. PA categories: inactive (0 MET), low active (>0 and <600 MET-minutes per week), moderately active (≥600 and <1,600 MET-minutes per week), and highly active (≥1,600 MET-minutes per week). Source of risk measures: Adjusted ORs (anxiety)38 and adjusted RRs (depression).37
PA, physical activity.
We used age- and sex-specific incidence and prevalence data, prevalent years of life lived with disability rates, and population data from the Global Burden of Disease (GBD) 2019 study.1,41 GBD was the preferred source because it provides the latest disease estimates for Australia. We used DisMod II42 to enforce internal consistency in the epidemiologic estimates obtained from the GBD 2019 study while deriving remission parameters that are not provided in the GBD data (Appendix Figure 2, available online, and Appendix Tables 2 and 3, available online). To determine the loss of quality of life, we used disability weights, which were calculated on the basis of disease-specific prevalence and years of life lived with disability estimates (Appendix Tables 4 and 5, available online).1
Healthcare costs were calculated using data from the Disease Expenditure in Australia 2018–19 report prepared by the Australian Institute of Health and Welfare (Appendix Table 6, available online).43 Costs per prevalent case of anxiety and depression were calculated on the basis of GBD 2019 disease prevalence and population numbers.1 Overall healthcare costs for all other health conditions were also included in our model (Appendix Table 7, available online). This is necessary because as interventions prolong life, additional healthcare costs will be incurred during added years of life.44 A summary of the model input parameters is presented in Table 1.1,11,32,37, 38, 39, 40, 41, 42, 43,45,46
Table 1.
Model Input Parameters
| Input data | Uncertainty | Source |
|---|---|---|
| Disease incidence | N/A | GBD 2019 study.1,41 (Appendix Tables 2–6, available online) |
| Disease prevalence | ||
| Disease remissiona | ||
| All-cause mortality rates | ||
| Disability weightsb | ||
| YLD (all causes and disease-specific YLDs) | ||
| Population numbers | ||
| RRsc | Normal (Ln RR)d | Schuch et al.37,38 (Figure 1) |
| Scaling the lowest and highest PA categories reported in RRs to the 4 modeled PA categories | N/A | Ekelund and colleagues39 |
| MET-minutes (walking=3.5, moderate PA=5, vigorous PA= 7.5) | N/A | Ainsworth et al.32 |
| PA categories defining PA levels in the population | Dirichlet | NHS 2017–2018.11 (Appendix Table 1, available online). |
| Modeled PA categories derived from MET minutes | Lognormal | |
| Healthcare costs | N/A | Disease Expenditure in Australia 2018–2019 report prepared by the AIHW43 (Appendix Tables 7 and 8, available online) |
| Discount rates applied in the sensitivity analysis | N/A | Australian Government Best Practice Regulation Guidance.45,46 |
We used DisMod II42 to enforce internal consistency in the epidemiologic estimates obtained from the GBD 2019 study while deriving remission parameters that are not provided in the GBD data (Appendix Figure 2, available online, and Appendix Tables 2 and 3, available online).
Disability weights were calculated on the basis of disease-specific prevalence and YLD estimates (Appendix Table 4, available online).
Adjusted RR measures for the outcome depression and adjusted OR for the outcome anxiety.
We used a modified version of the log of the RR function, which was used to avoid a skewed lognormal distribution.40
AIHW, Australian Institute of Health and Welfare; GBD, Global Burden of Disease; N/A, not applied; NHS, Australia National Health Survey; PA, physical activity; YLD, years lived with disability.
First, we simulated a business-as-usual scenario in which the current PA levels (by age and sex) continue in the reference population and, in parallel, comparator counterfactual scenarios in which the entire population achieves changes in PA levels. The changes in PA were modeled through 3 counterfactual scenarios: attainment of the Australian PA guidelines7 and achievement of the 20256 and 2030 global PA targets.8 We used the proportions shift method47 to model changes in PA levels by changing the proportion of the population in each PA category.
For the first counterfactual scenario in which the entire population meets the Australian PA targets, we used the updated PA guidelines for Australians.7 For those aged 18–64 years, the recommendation is to be active on most (preferably all) days to a weekly total of 2.5–5 hours of moderate activity (150–300 minutes) or 1.25–2.5 hours (75–150 minutes) of vigorous activity or an equivalent combination of both. For those aged ≥65 years, at least 30 minutes of moderate activity on most (preferably all) days is recommended. In the model, we implemented this scenario by moving the proportions of people in the inactive (METs=0) and low active (>0 and <600 MET-minutes per week) PA categories to the moderately active level (≥600 and <1,600 MET-min/week). For the second and third counterfactual scenarios in which the entire population achieves the set global targets, we modeled 2 targets:
-
1.
a 10% relative reduction in the prevalence of insufficient PA by 2025, one of the 9 voluntary global targets set in the WHO Global Action Plan for the Prevention and Control of Noncommunicable diseases 2013–2020.6 In the model, 10% of people in the inactive and low active PA categories were moved to the moderately active level; and
-
2.
a 15% relative reduction in the global prevalence of physical inactivity in adults and in adolescents by 2030 as set in the WHO Global Action Plan on PA 2018–2030,8 modeled as 15% of people in the inactive and low active PA categories moved to the moderately active level.
The resulting proportions of people in the 4 PA categories for each modeled scenario are presented in Appendix Table 8 (available online). This analysis was restricted to adults aged ≥15 years. To reflect the attainment of the target by 2025 and 2030, we phased in the intervention effect with linear increases from 2019 to 2025 and from 2019 to 2030 toward achieving the respective targets.
Statistical Analysis
We used the pMSLT model28 to simulate changes in the PA levels on anxiety and depression for the 2019 population (numbering 24.6 million [Appendix Table 9, available online]) over their remaining lifetime. The lifetables were populated with a closed cohort disaggregated by sex and 5-year age groups.
The pMSLT is divided into sections: a standard cause elimination life table (main lifetable) and a section for each disease with an independent illness death process (which we refer to as disease-specific sections in this manuscript) (Appendix Figure 1, available online).28
Two disease-specific sections were generated in our model. We created a switch that allowed each disease to be switched on or off and hence model one outcome at a time. The proportion of the Australian population assigned to each disease section was determined by the disease incidence (inflow) and case-fatality (outflow) rates. We assumed no mortality (case fatality) from anxiety and depression. The 2 included diseases were modeled by applying a set of differential equations to describe the transition between 4 states: healthy, diseased, dead from the disease, and dead from all other causes (Appendix Figure 2, available online).37 Transition probabilities among the 4 states reflected the rates of incidence, remission, case fatality, and mortality from all other causes (Appendix Tables 2 and 3, available online). For each age‒sex group, a change in exposure to the risk factor, insufficient PA, modified the postintervention incidence through potential impact fraction (PIF) calculations.47 For every modeled disease, the PIF calculates the proportional change in incidence after a change in exposure to PA (Appendix Table 10, available online).47 We used the disease-specific sections to report changes in incidence and prevalence. Over time, reduced incidence of disease in the intervention population results in reductions in prevalence compared with that in the reference population. Changes in disease-related quality of life at every age were calculated using disease-specific disability weights (Appendix Table 4, available online). These disease-specific changes feed into a lifetable. The lifetables were populated with a closed cohort of the entire 2019 Australia population disaggregated by sex and 5-year age group (Appendix Table 9, available online). The lifetables integrated all-cause mortality rates and years of life lived in poor health owing to disease (Appendix Tables 3 and 5, available online) and changes in disease-specific quality of life to calculate the number of health-adjusted life-years (HALYs) for the Australian population. These calculations for the stratified cohorts are simulated with 1-year cycle lengths until everyone dies or reaches the age of 100 years for both the reference and intervention populations. Where exposure to risk-factor-insufficient PA is reduced in the intervention population, there is an increase in the number of HALYs when compared with that of the reference population (business-as-usual scenario).
Because the national survey only provides PA information for persons aged ≥15 years, we restricted our analysis to these age groups. However, we ran the model from age 0 so the avoidable burden in younger cohorts is included in the outputs once they reach age 15 years. For the main analyses, we applied no discounting of health outcomes and healthcare costs.
We quantified the simultaneous and combined effect of the uncertainty in model inputs on our outcomes. We implemented this using a Monte Carlo simulation with bootstrapping (2,000 iterations) while incorporating probabilistic uncertainty from risk measures and PA input parameters. The 95% uncertainty intervals (UIs) were calculated, reflecting parameter uncertainty in the model (2.5 and 97.5 percentiles capturing sampling error with input data).
Sensitivity analyses were carried out to quantify the impact of change in discount rates applied on costs and health effects (HALYs). In line with the Australian Government Best Practice Regulation Guidance, we applied a discount rate of 3% for the health outcomes and 7% for the healthcare costs to all modeled scenarios.45,46
We used Microsoft Excel 365 and two software add-ins. The EpiGearXL 5.0 add-in was used for the calculation of the PIF, and Ersatz (Version 1.35) was used for the uncertainty analysis.48 Ethics approval was not required for the lifetable analysis.
RESULTS
For the HALYs and healthcare costs outcomes, we report outputs estimated for the remaining lifetime of the 2019 population of Australia. For the changes in incidence, we report outputs estimated for the next 25 years (between the years 2019 and 2044) and changes in prevalence for the year 2044. In the Appendix Tables 10 to 20 (available online) results table, we give additional results for all outcomes for different time periods such as the global and national noncommunicable diseases policy cycles, years 2025 and 2030, respectively. In addition, in this manuscript, we present results only for the modeled scenario in which all people adhered to the PA guidelines in Australia. Over the lifetime of the 2019 population of Australia, gains from a 10% relative reduction in the prevalence of insufficient PA by 2025 could add up to 60,016 HALYs for anxiety (95% UIs=24,103–98,457) and 50,333 for depression (95% UIs=25,954–75,379) (Appendix Table 13, available online) and healthcare cost savings of 508 million Australian dollars (AUDs) for anxiety and 561 million AUD for depression (Appendix Table 15, available online). A 15% relative reduction in the prevalence of insufficient PA by 2030 could yield a gain of 85,983 HALYs for anxiety (95% UIs=34,852–140,789) and 72,399 for depression (95% UIs=38,099–106,895) (Appendix Table 13, available online) and healthcare cost savings mean estimates of 732 million AUD for anxiety and 810 million AUD for depression (Appendix Table 15, available online) over the lifetime of the 2019 population of Australia.
Between 2019 and 2044 (25 years), our model projects that if all people adhered to the PA guidelines in Australia, there would be a reduction in the cumulative number of new cases of anxiety by 187,266 (95% UIs=73,802–309,167) and of depression by more than 1.1 million (95% UIs=582,556–1,681,544) (Table 2). The reduction in new cases was greater for females than for males. A reduction in total incident cases of anxiety and depression over different time periods is shown in Appendix Tables 10 and 11 (available online).
Table 2.
Reduction in Disease Incidence and Prevalence
| Outcome | Incident and prevalence count |
Proportional reduction in year 25 |
||||
|---|---|---|---|---|---|---|
| Male, mean (95% UI) |
Female, mean (95% UI) |
Total, mean (95% UI) |
Male, % (95% UI) |
Female, % (95% UI) |
Total, % (95% UI) |
|
| Incidence count in years 0–25 (2019–2044) | ||||||
| Anxiety | 81,078 | 106,188 | 187,266 | 5.96 | 6.86 | 6.42 |
| (31,817–134,310) | (41,985–174,857) | (73,802–309,167) | (2.35–9.86) | (2.72–11.27) | (2.54–10.59) | |
| Depression | 418,718 | 704,103 | 1,122,821 | 3.91 | 4.69 | 4.36 |
| (216,508–628,825) | (366,048–1,052,719) | (582,556–1,681,544) | (2.02–5.86) | (2.45–6.99) | (2.27–6.52) | |
| Prevalence count in year 25 (2044) | ||||||
| Anxiety | 21,297 | 38,756 | 60,053 | 4.89 | 5.21 | 5.09 |
| (8,356–35,308) | (15,318–63,875) | (23,673–99,183) | (1.92–8.10) | (2.06–8.58) | (2.01–8.40) | |
| Depression | 16,109 | 26,850 | 42,959 | 3.82 | 4.55 | 4.24 |
| (8,345–24,164) | (13,996–40,086) | (22,342–64,250) | (1.98–5.73) | (2.37–6.79) | (2.21–6.35) | |
Note: Results for the modeled scenario: all people adhered to the physical activity guidelines in Australia.
UI, uncertainty interval.
If all people adhered to the PA guidelines in Australia, our model projected a reduction in prevalent cases of anxiety by 60,053 (95% UIs=23,673–99,183) and of depression by 42,959 (95% UIs=22,342–64,250) in 2044, an estimated 5.1% proportional reduction in prevalent cases of anxiety and 4.2% of depression (Table 2). The estimated reduction in number and proportions over different time periods are shown in Appendix Table 12 (available online).
Table 3 shows that if all people adhered to the PA guidelines in Australia, over the lifetime of the 2019 population, almost twice as many HALYs would be gained in females (∼400,000) compared with those in males (∼200,000) for each health outcome. Additional results for the total HALYs gained in the lifetime for the additional 2 modeled scenarios and over different time periods are shown in Appendix Tables 13 and 14 (available online).
Table 3.
Total HALYs Gained and Reductions in Healthcare Expenditure
| Outcomes by sex | Total HALYs gained over the lifetime, | Reduction in healthcare expenditure over the lifetime (in AUD), |
|---|---|---|
| mean (95% UIs) | mean (95% UIs) | |
| Anxiety | ||
| Female | 416,256 | 3,498,614,451 |
| (165,494–683,306) | (1,395,653,298–5,728,440,670) | |
| Male | 224,336 | 1,907,269,567 |
| (88,530–370,372) | (754,908,697–3,141,478,744) | |
| Both | 640,592 | 5,405,884,018 |
| (254,024–1,053,678) | (2,150,561,995–8,869,919,414) | |
| Depression | ||
| Female | 330,758 | 3,875,838,612 |
| (173,193–491,919) | (2,029,465,286–5,764,237,082) | |
| Male | 192,958 | 1,955,792,166 |
| (100,242–288,740) | (1,016,788,020–2,924,800,592) | |
| Both | 523,717 | 5,831,630,778 |
| (273,435–780,658) | (3,046,253,306–8,689,037,674) |
Note: Results for the modeled scenario: all people adhered to the physical activity guidelines in Australia.
AUD, Australian dollar; HALY, health-adjusted life-year; UI, uncertainty interval.
Over the lifetime of the 2019 Australian population, if all people adhered to the PA guidelines, the estimated savings are 5.41 billion AUDs for anxiety and 5.83 billion AUDs for depression (Table 3). (Additional results are in Appendix Tables 15 and 16, available online). Compared with the base case (no discounting applied), for all the 3 modeled scenarios, applying 3% discounting for the health outcomes reduced the total number of HALYs gained over the lifetime of the 2019 Australian population for both anxiety and depression by about 60% (Table 4 and Appendix Table 17, available online). The total HALYs gained increased with time (Appendix Table 18, available online).
Table 4.
Total HALYs Gained and Reductions in Healthcare Expenditure With Discounting
| Outcome by sex | Total HALYs gained in the lifetime with discounting,a | Reduction in healthcare expenditure over the lifetime (in AUD) with discounting,b |
|---|---|---|
| mean (95% UIs) | mean (95% UIs) | |
| Anxiety | ||
| Female | 170,588 | 567,991,909 |
| (66,175–279,175) | (220,647,903–929,106,644) | |
| Male | 95,675 | 341,693,061 |
| (36,828–157,478) | (131,663,556–562,377,354) | |
| Both | 266,262 | 909,684,970 |
| (103,003–436,653) | (352,311,459–1,491,483,998) | |
| Depression | ||
| Female | 142,633 | 812,131,892 |
| (72,327–215,802) | (411,002,153–1,230,863,543) | |
| Male | 83,433 | 403,147,404 |
| (42,031–126,868) | (202,928,419–613,472,778) | |
| Both | 226,065 | 1,215,279,296 |
| (114,357–342,670) | (613,930,572–1,844,336,322) |
Note: Results for the modeled scenario: all people adhered to the physical activity guidelines in Australia.
A 3% discount rate on health effects applied.
A 7% discount rate on healthcare costs applied.
AUD, Australian dollar; HALY, health-adjusted life-year; UI, uncertainty interval.
Compared with the base case (no discounting applied), applying 7% discounting to the healthcare costs reduced the total cost offsets in the lifetime of the 2019 Australian population for all 3 modeled scenarios for both anxiety and depression by more than 80% (Table 4 and Appendix Table 19, available online). For the scenario where all people adhered to the PA guidelines in Australia, 7% discounting reduced the total cost offsets by ∼4.5 billion AUDs for each health outcome (anxiety and depression). Additional results for the additional 2 modeled scenarios and over different time periods are shown in Appendix Tables 19 and 20 (available online).
DISCUSSION
We found that if all Australians adhered to the recommended minimum PA levels, in 25 years’ time, the burden of these 2 conditions could be reduced substantially—by 6.4% (95% UIs=2.5–10.6) for anxiety and by 4.4% (95% UIs=2.3–6.5) for depression. Over the lifetime of the 2019 Australian population, the gains could add up to 640,592 years in perfect health (HALYs) for anxiety and 523,717 HALYs for depression and healthcare cost savings of 5.4 billion AUD for anxiety and 5.8 billion AUD for depression. The health and economic impacts are larger for females than for males. This is largely because a greater percentage of females than males across all ages were in the inactive and low active PA categories at baseline (Appendix Table 1, available online).11 In addition, women had a higher starting prevalence of anxiety and depression (Appendix Table 2, available online).1
To our knowledge, this is the first study to quantify the impact of PA on the burden of anxiety and depression over the life course in Australia or any other country. Specifically, we assessed the impact of achieving 3 policy targets: attainment of the Australian PA guidelines, a 10% relative reduction in the prevalence of insufficient PA is achieved by 2025, and a 15% relative reduction in the prevalence of physical inactivity by 2030.6, 7, 8 We report estimates on changes in incidence, prevalence, HALYs, and healthcare costs. Given that we model across the lifetime of the population, our study provides a comprehensive picture of the potential health gains because of increased PA levels, as opposed to other study types with shorter time horizons. This is valuable information for health planning and prevention policy.
Our work complements earlier studies that have applied the proportional multistate life table method to investigate the health impact of strategies that increase PA.21, 22, 23, 24, 25, 26 Findings from these previous studies confirm the health and economic benefits of increasing PA at the population level. Our study expands this research by investigating the health and economic impact of PA on the outcomes of anxiety and depression. These outcomes have not previously been included in health and economic assessments of PA. Our study complements the GBD 2019 study and the Australian Burden of Disease 2015 study,49,50 which have estimated the disease burden attributable to physical inactivity in Australia. Neither of the 2 studies included mental health outcomes. Our findings show that the inclusion of mental health benefits of PA into burden of disease estimates could have substantial policy implications. The findings from our review add to the recently published criticism of the estimation of the latest version of the GBD study using outdated and incomplete evidence on the health risks attributable to PA.51
Limitations
One of our study limitations is that for the strength of the associations between PA and depression and anxiety, we rely on the evidence from previous studies—primary cohort studies summarized in systematic reviews37,38 with pooled estimates. In their main analysis, the primary studies included by the review authors had varying definitions of high and low PA. Efforts to get additional information included contacting the corresponding author of the systematic reviews37,38 and our review of their included primary cohort studies. Owing to the variations presented, we could not establish homogenous PA categories. We applied the assumption that the lowest and highest PA categories reported in the review studies37,38 refer to the inactive and highly active categories in our model, respectively. Additional limitations of this evidence are discussed in our companion review study.16 Another limitation is that the pMSLT model has an assumption that modeled diseases are independent.28, 29, 30 This might lead to a slight overestimation of impact because with the disability-weight formula used to combine the impact of the 2 conditions, the impact is smaller if both are in the same individual. However, this would have a limited impact on overall estimates.29 In addition, our model did not incorporate migration, but the lifetable approach does include the effects of population aging. The UIs reflect only uncertainty in RRs and PA input parameters and not all uncertainty in the analysis, particularly, disease rates. The proportions shift method that we used to model changes in PA has been found to introduce nonlinearities where there should be none.47 However, for our case, the proportions shift method was the most intuitive for our model scenarios where we simplify and redistribute people to different PA categories.
The use of self-reported data in the estimate of the Australian PA levels was limiting, but this is appropriate, given that the risk measures were also based on studies that used self-report.
The reduction of prevalent cases owing to increased PA levels might happen faster than reported in this study because in our model, an increase in PA levels modifies only incidence and does not include established beneficial effects in people living with anxiety or depression.52, 53, 54, 55 As such, our estimates are conservative, and the true benefits of measures that increase PA are likely to be even greater.
Our findings are relevant to policy makers, clinicians, epidemiologists, and public health researchers. Our study provides empirical support for the adoption of PA in strategies for the prevention of mental ill health. Efforts to increase PA levels can make significant contributions to improving mental health.
At an individual level, our findings show that even a modest increase of PA for individuals with less-than-optimal PA levels (i.e., inactive or insufficient PA) could result in a significant benefit to mental health. The potential impact of PA on the burden of anxiety and depression may also encourage clinicians to emphasize PA as a key aspect of the prevention of mental ill health for their clients, in particular, clients who currently have low levels of PA.
At a population level, tackling broader social and environmental determinants that support active lives such as secure walkable neighborhoods; access to green and blue spaces; and safe roads for pedestrians, cyclists, and other active transport users can improve the uptake of PA at the population level.8,56,57 Evidence shows that strategies that seek to create healthier environments that encourage PA are more effective than those that only target individuals.8 Furthermore, our research supports prioritizing PA interventions for populations who experience relatively higher levels of physical inactivity such as people living in socioeconomically disadvantaged communities.13 These findings are particularly important for informing policy making in light of evidence that suggests that without targeted approaches, place-based infrastructure investments tend to benefit those already socioeconomically advantaged, therefore missing opportunities to both address health equity and allocate limited resources where they will achieve the best outcomes.58, 59, 60
Our findings make a strong case for the inclusion of PA in potential strategies for the prevention of mental ill health. For example, they could be used in economic appraisals for business cases of such prevention strategies. The true benefits of measures that increase PA levels are likely to be even much greater because the mental health benefits would be additional to those accrued from the reduction of other diseases associated with PA such as cardiovascular disease, diabetes, several types of cancer, and other chronic health conditions.61,62
For the strength of the associations between PA and depression and anxiety, further research could strengthen the evidence base for sex- and age-specific measures of association. This is important because with the low prevalence of optimal PA levels in Australia and globally,11,12 even a modest effect of PA on anxiety and depression could result in a significant benefit to mental health from interventions that improve the levels of PA.
Future studies should also assess the size and distribution of the benefits for different socioeconomic and ethnic groups and could be expanded to include children and adolescents (aged <15 years).
When people are being physically inactive, they often spend a lot of their time in sedentary behavior such as sitting. Emerging evidence suggests that high levels of sedentary behavior may also be unfavorably associated with depression and anxiety.63, 64, 65 Further research is needed to quantify the impact that sedentary behavior has on mental health among both children and adults.
CONCLUSIONS
Adherence to the Australian PA guidelines7 and achievement of the 20256 and 2030 global PA targets6,8 could lead to a substantial reduction of the burden of anxiety and depression. Over the lifetime of the 2019 Australian population, if all adhered to the recommended minimum PA levels, the gains could add up to 640,592 years in perfect health (HALYs) for anxiety and 523,717 HALYs for depression and healthcare cost savings of 5.4 billion AUD for anxiety and 5.8 billion AUD for depression.
This study provides empirical support for the inclusion of PA in strategies for the prevention of mental ill health.
Acknowledgments
ACKNOWLEDGMENTS
The authors are grateful to the late Jan Barendregt for developing previous model versions and frameworks adapted and expanded in this analysis. The authors acknowledge the New South Wales Ministry of Health for funding this study. The authors thank the AJPM Focus editorial team and external reviewers for their great input.
The funder had no say in the design/interpretation of the study.
This project was inspired by a larger project under the New South Wales Ministry of Health aimed at identifying a best practice method to cost the health benefits of active transport. This work was funded by the New South Wales Ministry of Health
Declarations of interest: none.
CREDIT AUTHOR STATEMENT
Mary Njeri Wanjau: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft. Holger Möller: Investigation, Writing – review & editing. Fiona Haigh: Investigation, Writing – review & editing. Andrew Milat: Writing – review & editing. Rema Hayek: Writing – review & editing. Peta Lucas: Writing – review & editing. J. Lennert Veerman: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Supervision, Validation, Writing – review & editing.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.focus.2022.100030.
Appendix. Supplementary materials
REFERENCES
- 1.Global Burden of Disease Collaborative . Institute for Health Metrics and Evaluation (IHME); Seattle, WA: 2020. Network. Global Burden of Disease Study 2019 (GBD 2019) Results.https://vizhub.healthdata.org/gbd-results/ Accessed March 2020. [Google Scholar]
- 2.Dawel A, Shou Y, Smithson M, et al. The effect of COVID-19 on mental health and wellbeing in a representative sample of Australian adults. Front Psychiatry. 2020;11(1026) doi: 10.3389/fpsyt.2020.579985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.COVID-19 Mental Disorders Collaborators Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–1712. doi: 10.1016/S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oude Voshaar RC, Aprahamian I, Borges MK, et al. Excess mortality in depressive and anxiety disorders: the Lifelines Cohort Study. Eur Psychiatry. 2021;64(1):e54. doi: 10.1192/j.eurpsy.2021.2229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wahlbeck K, Westman J, Nordentoft M, Gissler M, Laursen TM. Outcomes of Nordic mental health systems: life expectancy of patients with mental disorders. Br J Psychiatry. 2011;199(6):453–458. doi: 10.1192/bjp.bp.110.085100. [DOI] [PubMed] [Google Scholar]
- 6.WHO . WHO; Geneva, Switzerland: Published November 14, 2013. Global action plan for the prevention and control of NCDs 2013–2020.https://www.who.int/nmh/events/ncd_action_plan/en/ Accessed September 2020. [Google Scholar]
- 7.Physical activity and exercise guidelines for all Australians. Australian Government. https://www.health.gov.au/health-topics/physical-activity-and-exercise/physical-activity-and-exercise-guidelines-for-all-australians/for-adults-18-to-64-years. Updated 10 May 2021. Accessed June 2021.
- 8.WHO . WHO; Geneva, Switzerland: Published 2018. Global action plan on physical activity 2018–2030: more active people for a healthier world.https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwj3-OTahpD6AhUwB7cAHXbID90QFnoECBMQAQ&url=https%3A%2F%2Fapps.who.int%2Firis%2Fbitstream%2Fhandle%2F10665%2F272722%2F9789241514187-eng.pdf&usg=AOvVaw0rghKRuqgGKVTFb3SGvic3 Accessed September 2020. [Google Scholar]
- 9.McDowell CP, Dishman RK, Vancampfort D, et al. Physical activity and generalized anxiety disorder: results from the Irish Longitudinal Study on Ageing (TILDA) Int J Epidemiol. 2018;47(5):1443–1453. doi: 10.1093/ije/dyy141. [DOI] [PubMed] [Google Scholar]
- 10.Ku PW, Fox KR, Chen LJ. Physical activity and depressive symptoms in Taiwanese older adults: a seven-year follow-up study. Prev Med. 2009;48(3):250–255. doi: 10.1016/j.ypmed.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 11.Microdata: national health survey, 2017–18. Australian Bureau of Statistics. https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwjU0J6Kh5D6AhXxXWwGHbpdCSQQFnoECBEQAQ&url=https%3A%2F%2Fwww.abs.gov.au%2FAusstats%2Fabs%40.nsf%2Fc1061106e0c3442fca2568b5007b861d%2Fafe17893065f4400ca2568a900143b61!OpenDocument&usg=AOvVaw3u8YKuEIlsrf2NITGCwWzk. Updated 2019. Accessed April 2020.
- 12.Insufficient physical activity. Australian Institute of Health and Welfare. https://www.aihw.gov.au/reports/risk-factors/insufficient-physical-activity. Updated October 20, 2020. Accessed March 22, 2021.
- 13.Australian Institute of Health and Welfare . Australian Institute of Health and Welfare; Canberra, Australia: Published 2018. Physical activity across the life stages.https://www.aihw.gov.au/getmedia/c249ef97-e219-44df-a8bd-f5e50d04064c/aihw-phe-225.pdf.aspx?inline=true2020 Accessed March 2020. [Google Scholar]
- 14.Commonwealth of Australia . Commonwealth of Australia; Canberra, Australia: Published August 2017. The fifth national mental health and suicide prevention plan.https://www.mentalhealthcommission.gov.au/getmedia/0209d27b-1873-4245-b6e5-49e770084b81/Fifth-National-Mental-Health-and-Suicide-Prevention-Plan Accessed May 2021. [Google Scholar]
- 15.Commonwealth of Australia . Commonwealth of Australia; Canberra, Australia: Published January 2009. National mental health Policy 2008.https://www.health.gov.au/resources/publications/national-mental-health-policy-2008 Accessed May 2021. [Google Scholar]
- 16.Wanjau MN, Möller H, Haigh F, et al. Physical activity and depression and anxiety disorders: a systematic review of reviews and assessment of causality. AJPM Focus. 2023;2(2) doi: 10.1016/j.focus.2023.100074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carter R, Moodie M, Markwick A, et al. Assessing Cost-Effectiveness in Obesity (ACE-Obesity): an overview of the ACE approach, economic methods and cost results. BMC Public Health. 2009;9(1):419. doi: 10.1186/1471-2458-9-419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Veerman JL, Sacks G, Antonopoulos N, Martin J. The impact of a tax on sugar-sweetened beverages on health and health care costs: a modelling study. PLoS One. 2016;11(4) doi: 10.1371/journal.pone.0151460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Forster M, Veerman JL, Barendregt JJ, Vos T. Cost-effectiveness of diet and exercise interventions to reduce overweight and obesity. Int J Obes (Lond) 2011;35(8):1071–1078. doi: 10.1038/ijo.2010.246. [DOI] [PubMed] [Google Scholar]
- 20.Ananthapavan J, Sacks G, Brown V, et al. Priority-setting for obesity prevention-the Assessing Cost-Effectiveness of obesity prevention policies in Australia (ACE-Obesity Policy) study. PLoS One. 2020;15(6) doi: 10.1371/journal.pone.0234804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brown V, Barr A, Scheurer J, Magnus A, Zapata-Diomedi B, Bentley R. Better transport accessibility, better health: a health economic impact assessment study for Melbourne, Australia. Int J Behav Nutr Phys Act. 2019;16(1):89. doi: 10.1186/s12966-019-0853-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cobiac LJ, Vos T, Barendregt JJ. Cost-effectiveness of interventions to promote physical activity: a modelling study. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zapata-Diomedi B, Gunn L, Giles-Corti B, Shiell A, Lennert Veerman J. A method for the inclusion of physical activity-related health benefits in cost-benefit analysis of built environment initiatives. Prev Med. 2018;106:224–230. doi: 10.1016/j.ypmed.2017.11.009. [DOI] [PubMed] [Google Scholar]
- 24.Zapata-Diomedi B, Knibbs LD, Ware RS, et al. A shift from motorised travel to active transport: what are the potential health gains for an Australian city? PLoS One. 2017;12(10) doi: 10.1371/journal.pone.0184799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Randal E, Shaw C, McLeod M, Keall M, Woodward A, Mizdrak A. The impact of transport on population health and health equity for Māori in Aotearoa New Zealand: a prospective burden of disease study. Int J Environ Res Public Health. 2022;19(4):2032. doi: 10.3390/ijerph19042032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mizdrak A, Ding D, Cleghorn C, Blakely T, Richards J. Hitting the target but missing the point? Modelling health and economic impacts of different approaches to meeting the global action plan for physical activity target. Sports Med. 2021;51(4):815–823. doi: 10.1007/s40279-020-01398-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wanjau MN, Möller H, Haigh F, Zapata-Diomedi B, Veerman L. New South Wales Ministry of Health; St Leonards, Australia: Published 2022. Preliminary report: phase 2 of the economic active transport project to deliver a best practice method to cost the health benefits of active transport in NSW.https://www.health.nsw.gov.au/heal/Pages/publications.aspx Accessed August 2022. [Google Scholar]
- 28.Barendregt JJ, Van Oortmarssen GJ, Van Hout BA, Van Den Bosch JM, Bonneux L. Coping with multiple morbidity in a life table. Math Popul Stud. 1998;7(1):29–49. doi: 10.1080/08898489809525445. 109. [DOI] [PubMed] [Google Scholar]
- 29.Blakely T, Moss R, Collins J, et al. Proportional multistate lifetable modelling of preventive interventions: concepts, code and worked examples. Int J Epidemiol. 2020;49(5):1624–1636. doi: 10.1093/ije/dyaa132. [DOI] [PubMed] [Google Scholar]
- 30.Hoogenveen RT, Boshuizen HC, Engelfriet PM, van Baal PHM. You only die once: accounting for multi-attributable mortality risks in multi-disease models for health-economic analyses. Med Decis Making. 2017;37(4):403–414. doi: 10.1177/0272989X16658661. [DOI] [PubMed] [Google Scholar]
- 31.Stevens GA, Alkema L, Black RE, et al. Guidelines for Accurate and Transparent Health Estimates Reporting: the GATHER statement. Lancet. 2016;388(10062):e19–e23. doi: 10.1016/S0140-6736(16)30388-9. [DOI] [PubMed] [Google Scholar]
- 32.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(9 suppl):S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 33.Gartner CE, Barendregt JJ, Hall WD. Predicting the future prevalence of cigarette smoking in Australia: how low can we go and by when? Tob Control. 2009;18(3):183–189. doi: 10.1136/tc.2008.027615. [DOI] [PubMed] [Google Scholar]
- 34.Rothman KJ, Greenland S, Lash TL. Modern. Epidemiology. 2008 https://vizhub.healthdata.org/gbd-results/ 3e (pb): Lippincott. Accessed March 2020. Available from. [Google Scholar]
- 35.Webb P, Bain C, Page A. 4 ed. Cambridge University Press; Cambridge, United Kingdom: 2019. Essential Epidemiology: An Introduction for Students and Health Professionals.https://ghdx.healthdata.org/record/ihme-data/gbd-2019-population-estimates-1950-2019 Accessed March 2020. Available from. [Google Scholar]
- 36.Judging the evidence. World Cancer Research Fund International. https://www.wcrf.org/wp-content/uploads/2021/02/judging-the-evidence.pdf. Updated 2018. Accessed June 2020.
- 37.Schuch FB, Vancampfort D, Firth J, et al. Physical activity and incident depression: a meta-analysis of prospective cohort studies. Am J Psychiatry. 2018;175(7):631–648. doi: 10.1176/appi.ajp.2018.17111194. [DOI] [PubMed] [Google Scholar]
- 38.Schuch FB, Stubbs B, Meyer J, et al. Physical activity protects from incident anxiety: A meta-analysis of prospective cohort studies. Depress Anxiety. 2019;36(9):846–858. doi: 10.1002/da.22915. [DOI] [PubMed] [Google Scholar]
- 39.Ekelund U, Tarp J, Steene-Johannessen J, et al. Dose-response associations between accelerometry measured physical activity and sedentary time and all cause mortality: systematic review and harmonised meta-analysis. BMJ. 2019;366:l4570. doi: 10.1136/bmj.l4570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barendregt JJ. The effect size in uncertainty analysis. Value Health. 2010;13(4):388–391. doi: 10.1111/j.1524-4733.2009.00686.x. [DOI] [PubMed] [Google Scholar]
- 41.Global Burden of Disease Collaborative . Institute for Health Metrics and Evaluation (IHME; Seattle, WA: 2020. Network. Global Burden of Disease Study 2019 (GBD 2019) Population Estimates 1950–2019.https://ghdx.healthdata.org/record/ihme-data/gbd-2019-population-estimates-1950-2019 Accessed March 2020. [Google Scholar]
- 42.Barendregt JJ, van Oortmarssen GJ, Vos T, Murray CJL. A generic model for the assessment of disease epidemiology: the computational basis of DisMod II. Popul Health Metr. 2003;1(1):4. doi: 10.1186/1478-7954-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Australian Institute of Health and Welfare . 2021. Disease expenditure in Australia 2018–19.https://www.aihw.gov.au/reports/health-welfare-expenditure/disease-expenditure-australia/contents/about [Google Scholar]
- 44.Van Baal PHM, Feenstra TL, Polder JJ, Hoogenveen RT, Brouwer WBF. Economic evaluation and the postponement of health care costs. Health Econ. 2011;20(4):432–445. doi: 10.1002/hec.1599. Accessed October 2020. Published on 11 March 2011. [DOI] [PubMed] [Google Scholar]
- 45.Australian Government . Office of Best Practice Regulation, Australian Government; Canberra, Australia: Published September 7, 2021. Best practice regulation guidance note. Value of statistical life.https://obpr.pmc.gov.au/resources/guidance-assessing-impacts/value-statistical-life Accessed September 2021. [Google Scholar]
- 46.Attema AE, Brouwer WBF, Claxton K. Discounting in economic evaluations. Pharmacoeconomics. 2018;36(7):745–758. doi: 10.1007/s40273-018-0672-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Barendregt JJ, Veerman JL. Categorical versus continuous risk factors and the calculation of potential impact fractions. J Epidemiol Community Health. 2010;64(3):209–212. doi: 10.1136/jech.2009.090274. [DOI] [PubMed] [Google Scholar]
- 48.EpiGear international Pty Ltd. https://www.epigear.com/index.htm. Updated 2016. Accessed March 2020.
- 49.Australian Institute of Health and Welfare, Australian Burden of Disease Study, 2015, Updated August 6, 2020. Accessed October 3, 2022.https://www.aihw.gov.au/reports/burden-of-disease/abds-2015-interactive-data-disease-burden/contents/overview
- 50.GBD Risk factors Collaborators Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223–1249. doi: 10.1016/S0140-6736(20)30752-2. Accessed March 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stamatakis E, Ding D, Ekelund U, Bauman AE. Sliding down the risk factor rankings: reasons for and consequences of the dramatic downgrading of physical activity in the Global Burden of Disease 2019. Br J Sports Med. 2021;55(21):1222–1223. doi: 10.1136/bjsports-2021-104064. [DOI] [PubMed] [Google Scholar]
- 52.Rebar AL, Stanton R, Geard D, Short C, Duncan MJ, Vandelanotte C. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol Rev. 2015;9(3):366–378. doi: 10.1080/17437199.2015.1022901. [DOI] [PubMed] [Google Scholar]
- 53.Jayakody K, Gunadasa S, Hosker C. Exercise for anxiety disorders: systematic review. Br J Sports Med. 2014;48(3):187–196. doi: 10.1136/bjsports-2012-091287. [DOI] [PubMed] [Google Scholar]
- 54.Cooney GM, Dwan K, Greig CA, et al. Exercise for depression. Cochrane Database Syst Rev. 2013;9(9) doi: 10.1002/14651858.CD004366.pub6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Knapen J, Vancampfort D, Moriën Y, Marchal Y. Exercise therapy improves both mental and physical health in patients with major depression. Disabil Rehabil. 2015;37(16):1490–1495. doi: 10.3109/09638288.2014.972579. [DOI] [PubMed] [Google Scholar]
- 56.Veerman JL, Barendregt JJ. Population interventions for obesity. Epidemiol (Camb Mass) 2010;21(2):274–275. doi: 10.1097/EDE.0b013e3181cc9dee. [DOI] [PubMed] [Google Scholar]
- 57.Bauman AE, Reis RS, Sallis JF, et al. Correlates of physical activity: why are some people physically active and others not? Lancet. 2012;380(9838):258–271. doi: 10.1016/S0140-6736(12)60735-1. [DOI] [PubMed] [Google Scholar]
- 58.Hämäläinen RM, Sandu P, Syed AM, Jakobsen MW. An evaluation of equity and equality in physical activity policies in four European countries. Int J Equity Health. 2016;15(1):191. doi: 10.1186/s12939-016-0481-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Smith M, Hosking J, Woodward A, et al. Systematic literature review of built environment effects on physical activity and active transport – an update and new findings on health equity. Int J Behav Nutr Phys Act. 2017;14(1):158. doi: 10.1186/s12966-017-0613-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Corburn J. Urban place and health equity: critical issues and practices. Int J Environ Res Public Health. 2017;14(2):117. doi: 10.3390/ijerph14020117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol. 2012;2(2):1143–1211. doi: 10.1002/cphy.c110025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lee IM, Shiroma EJ, Lobelo F, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Teychenne M, Costigan SA, Parker K. The association between sedentary behaviour and risk of anxiety: a systematic review. BMC Public Health. 2015;15(1):513. doi: 10.1186/s12889-015-1843-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hallgren M, Nguyen TT, Owen N, et al. Cross-sectional and prospective relationships of passive and mentally active sedentary behaviours and physical activity with depression. Br J Psychiatry. 2020;217(2):413–419. doi: 10.1192/bjp.2019.60. [DOI] [PubMed] [Google Scholar]
- 65.Saunders TJ, McIsaac T, Douillette K, et al. Sedentary behaviour and health in adults: an overview of systematic reviews. Appl Physiol Nutr Metab. 2020;45(10 suppl 2):S197–S217. doi: 10.1139/apnm-2020-0272. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.