HIGHLIGHTS
-
•
Hepatitis C virus–related liver disease is a leading cause of death among Latinos.
-
•
Community health centers serve a high proportion of Latinos and are an important setting.
-
•
Latino English-preferred patients had lower hepatitis C virus screening rates than other groups.
-
•
Understanding how language preference impacts screening disparities is needed.
Keywords: Hepatitis C virus, risk screening, disparities, minority health, electronic health record, community health centers
Abstract
Introduction
Hepatitis C virus is associated with high morbidity and mortality—chronic liver disease is a leading cause of death among Latinos in the U.S. Screening for hepatitis C virus in community health center settings, which serve a disproportionate percentage of Latinos, is essential to eradicating hepatitis C virus infection. We assessed hepatitis C virus screening disparities in adults served by community health centers by ethnicity and language preference.
Methods
This was an observational cohort study (spanning 2013–2017) of adults born in 1945–1965 in the Accelerating Data Value Across a National Community Health Center Network electronic health record data set. Our exposure of interest was race/ethnicity and language preference (non-Hispanic White, Latino English preferred, Latino Spanish preferred). Our primary outcome was the relative hazard of hepatitis C virus screening, estimated using multivariate Cox proportional hazards regression.
Results
A total of 182,002 patients met the study criteria and included 60% non-Hispanic Whites, 29% Latino Spanish preferred, and 11% Latino English preferred. In total, 9% received hepatitis C virus screening, and 2.4% were diagnosed with hepatitis C virus. Latino English-preferred patients had lower rates of screening than both non-Hispanic Whites and Latino Spanish preferred (5.5% vs 9.4% vs 9.6%, respectively). Latino English preferred had lower hazards of hepatitis C virus screening than non-Hispanic Whites (adjusted hazard ratio=0.56, 95% CI=0.44, 0.72), and Latino Spanish preferred had similar hazards of hepatitis C virus screening (adjusted hazard ratio=1.11, 95% CI=0.88, 1.41).
Conclusions
We found that in a large community health center network, adult Latinos who preferred English had lower hazards of hepatitis C virus screening than non-Hispanic Whites, whereas Latinos who preferred Spanish had hazards of screening similar to those of non-Hispanic Whites. The overall prevalence of hepatitis C virus screening was low. Further work on the role of language preference in hepatitis C virus screening is needed to better equip primary care providers to provide this recommended preventive service in culturally relevant ways.
INTRODUCTION
Hepatitis C virus (HCV) affects 2.4 million people in the U.S., and new HCV infections have tripled in recent years,1 conjointly with the opioid crisis and rise of injection drug–related infections. HCV is associated with high morbidity and mortality,2,3 impacting Latino populations disproportionately.4, 5, 6 Chronic liver disease is a leading cause of death among Latinos in the U.S., and Latinos experience a higher rate of HCV-related deaths than non-Hispanic Whites (6.8 vs 4.5 per 100,000).7 Published studies report that screening in Latino populations remains low, and multiple barriers exist for HCV screening.6,8,9 The role of Spanish-language preference on healthcare utilization and outcomes compared with that of English preference varies by setting and service.10, 11, 12, 13 Community health center (CHC) settings are key to HCV screening efforts because many older, low-income Latino patients receive care in CHCs.14
Previous studies have identified disparities in HCV screening rates through surveys15,16 or registry data, which may be subject to underreporting. Electronic health records (EHRs) may provide additional details of screening disparities and opportunities to target interventions along the HCV treatment cascade; however, most studies using EHR data are limited to local settings, and few examine language preference.8,9,17 Using a multistate EHR data set of CHCs, we evaluated whether there were differences in HCV screening rates between non-Hispanic White, Latino English language–preferring adults, and Latino Spanish language–preferring adults.
METHODS
Study Population
We performed a retrospective cohort study of Latino and non-Hispanic White adults who were seen at CHCs between 2013 and 2017 in the ADVANCE (Accelerating Data Value Across a National Community Health Center Network) clinical data research network in 21 states.18 Queries and data tables for analyses were standardized in the PCORnet common data model, Version 3.1, from the ADVANCE data warehouse, which includes specific deduplication protocols. We defined the eligible population as patients born between 1945 and 1965 (thus meeting the U.S. Preventive Services Task Force 2013 guideline) whose first encounter in the CHC network occurred during the observation period beginning in 2013 when the HCV screening policy was updated. Observation spanned from the first visit until screening or censoring (death or end of study period). We excluded patients with an existing HCV diagnosis (diagnosis codes: International Classification of Diseases 070.41, 070.44, 070.51, 070.54, 070.70, 070.71, B17.10, B17.11, B18.2, B19.20, B19.21) at the start of observation.
Measures
We defined our primary outcome as the relative hazard of HCV screening test during the study period. We also determined the prevalence of a new HCV diagnosis during the study period by noting whether the individual had a new HCV diagnosis code after the start of observation.
Our primary independent variable was a composite of 3 mutually exclusive ethnicity and language preference groups: non-Hispanic White, Latino Spanish language preferred, and Latino English language preferred. Ethnicity and language were based on patient self-reported clinic registration data.
We adjusted for the following potential confounders: age, sex, insurance status at visits during the study period (all public, all private, public and private, no insurance); substance use disorder from encounters and diagnosis ICD-9/ICD-10 codes excluding tobacco and nicotine; Type I or II diabetes diagnosis (to indicate obtaining periodic bloodwork); and the number of primary care visits during the study period (a proxy for general healthcare utilization).
Statistical Analysis
We conducted descriptive analyses of patient characteristics overall and by ethnicity/language groups, including the prevalence of HCV screening and HCV diagnosis. For our outcome, we used Cox proportional hazards models to estimate covariate-adjusted hazard ratios (AHR) of receipt of HCV screening by ethnic–language groups. We used a proportional hazards approach because we were interested in whether there were differences in time to screening in addition to hazards of screening. Of the 180,053 observations used in the final model, 165,540 were censored at recorded death, end of the study period, or date of disenrollment; 1,662 had a recorded death date before receipt of screening. Non-Hispanic White patients were considered the ref group, and robust SEs were estimated to account for the clustering of patients within clinics. Analyses were conducted using Stata, Version 15, and R, Version 4.1.3, with 2-sided testing and Type I error set at 5%. This study was approved by the IRB of Oregon Health & Science University.
RESULTS
There were 182,002 eligible patients across 21 states. The average age was 61.9 years (SD=3.89), with 54% female sex. Patients were predominantly non-Hispanic White (60.2%), with 28.8% Latino Spanish preferred and 11.0% Latino English preferred (Table 1).
Table 1.
Description of the ADVANCE Sample by Race and Language Preference
| Characteristics | ||||
|---|---|---|---|---|
| Ethnicity/language groups |
||||
| Overall, n (%) | Non-Hispanic White, n (%) | Latino: prefers English, n (%) | Latino: prefers Spanish, n (%) | |
| (N=182,002) | (n=109,368) | (n=19,982) | (n=52,382) | |
| Age at first encounter, years (mean [SD]) | 61.90 [3.89] | 61.86 [3.92] | 61.53 [3.84] | 62.12 [3.85] |
| Age group, years | ||||
| 50–54 | 1,583 (0.9) | 1,095 (1.0) | 189 (0.9) | 299 (0.6) |
| 55–59 | 63,412 (34.8) | 38,546 (35.2) | 7,645 (38.3) | 17,221 (32.9) |
| 60–64 | 76,389 (42.0) | 45,219 (41.2) | 8,376 (41.9) | 22,794 (43.5) |
| 65–69 | 35,729 (19.6) | 21,998 (20.1) | 3,289 (16.5) | 10,442 (19.9) |
| 70–73 | 4,889 (2.7) | 2,780 (2.5) | 483 (2.4) | 1,626 (3.1) |
| Female sex | 98,353 (54.0) | 56,546 (51.6) | 10,681 (53.5) | 31,126 (59.4) |
| Insurance | ||||
| Never insured | 35,414 (19.5) | 19,087 (17.4) | 3,957 (19.8) | 12,370 (23.6) |
| Some private | 35,764 (19.7) | 24,273 (22.1) | 3,737 (18.7) | 7,754 (14.8) |
| Some public | 101,057 (55.5) | 59,733 (54.5) | 11,196 (56.0) | 30,128 (57.5) |
| Some public and private | 9,767 (5.4) | 6,545 (6.0) | 1,092 (5.5) | 2,130 (4.1) |
| Screened for HCV | 16,462 (9.0) | 10,342 (9.4) | 1,092 (5.5) | 5,028 (9.6) |
| HCV diagnosis | 4,305 (2.4) | 3,328 (3.0) | 655 (3.3) | 322 (0.6) |
| SUD | 17,260 (9.5) | 13,949 (12.7) | 1,966 (9.8) | 1,345 (2.6) |
| FPL | ||||
| <138% | 99,381 (54.6) | 49,546 (45.2) | 12,447 (62.3) | 37,388 (71.4) |
| ≥138% | 29,388 (16.1) | 21,710 (19.8) | 2,961 (14.8) | 4,717 (9.0) |
| Missing | 53,233 (29.2) | 38,382 (35.0) | 4,574 (22.9) | 10,277 (19.6) |
| Visits per year | ||||
| <1 | 50,566 (27.8) | 33,391 (30.5) | 5,614 (28.1) | 11,561 (22.1) |
| 1–3 | 59,350 (32.6) | 35,696 (32.6) | 6,369 (31.9) | 17,285 (33.0) |
| 3–5 | 31,110 (17.1) | 16,825 (15.3) | 3,370 (16.9) | 10,915 (20.8) |
| 5–10 | 27,276 (15.0) | 14,645 (13.4) | 3,045 (15.2) | 9,586 (18.3) |
| ≥10 | 13,700 (7.5) | 9,081 (8.3) | 1,584 (7.9) | 3,035 (5.8) |
| Age at HCV diagnosis | ||||
| 50–54 | 9 (0.0) | 8 (0.0) | 1 (0.0) | 0 (0.0) |
| 55–59 | 1,284 (0.7) | 939 (0.9) | 281 (1.4) | 64 (0.1) |
| 60–64 | 2,135 (1.2) | 1,724 (1.6) | 215 (1.1) | 196 (0.4) |
| 65–69 | 761 (0.4) | 563 (0.5) | 149 (0.7) | 49 (0.1) |
| 70–73 | 116 (0.1) | 94 (0.1) | 9 (0.0) | 13 (0.0) |
| Not diagnosed | 177,697 (97.6) | 106,310 (97.0) | 19,327 (96.7) | 52,060 (99.4) |
FPL, federal poverty level; HCV, hepatitis C virus; SUD, substance use disorder.
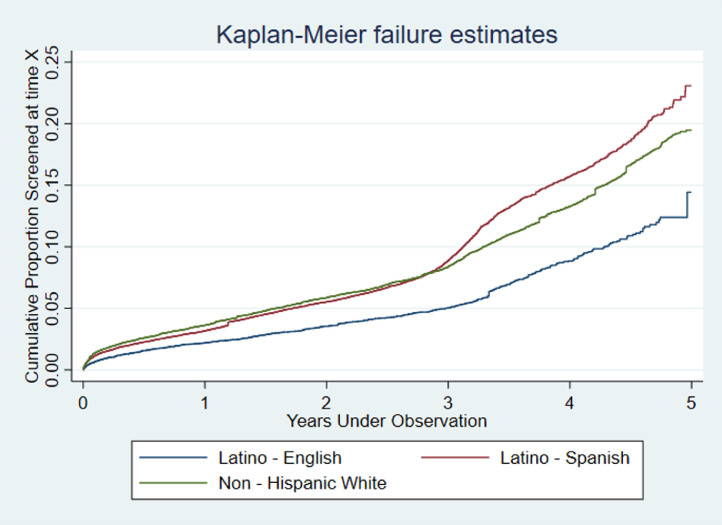
In total, 9% had an HCV screening test, and 2.4% were diagnosed with HCV during the study period. In the unadjusted analysis, Latino English-preferred patients had lower rates of HCV screening than non-Hispanic Whites and Latino Spanish preferred (5.5% vs 9.4% vs 9.6%, respectively, p<0.001). After adjustment, Latino English language–preferred patients had lower hazards of HCV screening than non-Hispanic Whites (AHR=0.56, 95% CI=0.44, 0.72), whereas Latino Spanish language–preferred patients had similar hazards of HCV screening (AHR=1.11, 95% CI=0.88, 1.40) (Table 2 and Figure 1).
Table 2.
Adjusted Relative Hazard of Receipt of Hepatitis C Virus Screening Test
| Model | Patient group | HR estimate (95% CI) |
|---|---|---|
| Adjusted HRa | Latino English speaking | 0.56 (0.43, 0.72) |
| Latino Spanishspeaking | 1.11 (0.88, 1.40) | |
| Non-Hispanic White | ref | |
| Unadjusted HR | Latino Englishspeaking | 0.61 (0.47, 0.79) |
| Latino Spanish speaking | 1.08 (0.81, 1.45) | |
| Non-HispanicWhite | ref |
Note: Patients included in the time-to-event analysis were required to have entered the study population during the study period and not have a screening at their first visit.
Adjusted for age category, female sex, insurance, visits per year, diabetes diagnosis, and substance use disorder.
HR, hazard ratio.
Figure 1.
Kaplan–Meier.plots for HCV screening completion by race/ethnicity and language (non-Hispanic White, Latino English language preferred, and Latino Spanish language preferred)
Note: The proportion screened at each time point is among patients who have not yet been screened or censored.
HCV, hepatitis C virus.
DISCUSSION
In a large multistate cohort of established CHC patients, we found low HCV screening prevalence (9%) but slightly higher than the national average HCV diagnosis rates (2.4% vs 1%).16 We also found significant HCV screening disparities by ethnicity and language preference. Our population's HCV screening prevalence is lower than national estimates on the basis of the National Health Interview Survey (17.3% in 2017)9 and consistent with previous estimates of CHC screening prevalence among a smaller network (8.3% of 61,000 eligible).19 Other studies reveal variability in HCV screening rates in CHCs,8,9,20 which warrants further investigation.
We also found that Latinos who preferred Spanish had rates and hazards of screening similar to those of non-Hispanic White, but Latinos who preferred English had lower rates and hazards of HCV screening. This was surprising because we hypothesized that Spanish-preferring Latino patients would have lower screening rates than English-preferring patients, as previous studies have shown with regard to access to health services and utilization,2,10 HIV prophylaxis awareness,21 and use of physician services.22 However, we now have increasing evidence that in our practice-based research network, Spanish-preferring patients often utilize preventive services more than non-Hispanic Whites and English-preferring Latinos.11,12,23 One explanation may be that heightened attention to Spanish-preferred patients in CHCs, which have additional community, cultural, and language engagement resources, facilitates trust between CHC providers and Spanish-speaking patients, leading to increased adherence to screening recommendations, as other screening evaluations in our network suggest.24,25 Organizational differences in care settings (e.g., variability in support staff such as bilingual navigators) have been shown to explain differences in receipt and understanding screening mammography results across ethnic groups.26 It is also important to note that these were patients seeking care at CHCs, as opposed to general populations, which might also explain our findings. Further exploration into why English-preferring Latinos had lower rates of screening is required.
Limitations
There are several limitations to the analyses. Screening as opposed to diagnostic testing for HCV is difficult to ascertain in our data set. Our definition of screening is subject to misclassification bias if patients received the test outside the EHR network or received the test before cohort inception, which we mitigated by limiting the sample to patients whose first visit to the network occurred during the observation period. We also have evidence that most patients seen in our network tend to receive all their care within the network.27,28 Second, this is an observational study that may be subject to unmeasured confounding. This analysis did not adjust for social determinants of health such as education level or provider-level factors that might explain the differences we observed. We also recognize that the U.S. Preventive Services Task Force guidelines have since been updated to include universal screening for all adults29—our findings remind us that expanding screening initiatives without addressing underlying inequities in access to screening and subsequent treatment may worsen disparities in care.8
CONCLUSIONS
In a nationally representative cohort of CHC patients, we found low rates of HCV screening overall and significant disparities in the hazards of HCV screening by language preference among Latinos. Further work examining language preference is needed to better equip primary care providers to implement HCV screening in culturally relevant ways.
CRediT authorship contribution statement
Brian L. Chan: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Writing – original draft. David Ezekiel-Herrera: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Visualization, Writing – review & editing. Steffani R. Bailey: Conceptualization, Investigation, Methodology, Writing – review & editing. Miguel Marino: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Writing – review & editing. Jennifer A. Lucas: Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Writing – review & editing. Sophia Giebultowicz: Data curation, Methodology, Software, Validation, Writing – review & editing. Erika Cottrell: Conceptualization, Project administration, Resources, Supervision, Writing – review & editing. Joe Carroll: Conceptualization, Investigation, Methodology, Writing – review & editing. John Heintzman: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing.
ACKNOWLEDGMENTS
This work was conducted with the ADVANCE (Accelerating Data Value Across a National Community Health Center Network) Clinical Research Network. OCHIN leads the ADVANCE network in partnership with Health Choice Network, Fenway Health, and Oregon Health & Science University.
The research presented in this paper is that of the authors and does not reflect the official policy of the NIH.
ADVANCE is funded through the Patient-Centered Outcomes Research Institute (Contract Number RI-OCHIN-01-MC). This study was supported by National Institute on Aging (Grant Number R01AG056337; recipient: JH) and National Institute on Drug Abuse (Grant Number 1K23DA053390-01A1; recipient: BC)
Preliminary results of this work were presented virtually at the California, Hawaii, Northwest Society of General Internal Medicine regional meeting in January 2022.
Declaration of interest: none.
REFERENCES
- 1.Ryerson AB, Schillie S, Barker LK, Kupronis BA, Wester C. Vital Signs: Newly reported acute and chronic hepatitis C cases - United States, 2009–2018. MMWR Morb Mortal Wkly Rep. 2020;69(14):399–404. doi: 10.15585/mmwr.mm6914a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ly KN, Hughes EM, Jiles RB, Holmberg SD. Rising mortality associated with hepatitis C virus in the United States, 2003–2013. Clin Infect Dis. 2016;62(10):1287–1288. doi: 10.1093/cid/ciw111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chou R, Dana T, Fu R, et al. Screening for hepatitis C virus infection in adolescents and adults: updated evidence report and systematic review for the U.S. Preventive Services Task Force [published correction appears in JAMA. 2020;323(13):1318] JAMA. 2020;323(10):976–991. doi: 10.1001/jama.2019.20788. [DOI] [PubMed] [Google Scholar]
- 4.Rodríguez-Torres M. Latinos and chronic hepatitis C: a singular population. Clin Gastroenterol Hepatol. 2008;6(5):484–490. doi: 10.1016/j.cgh.2008.02.036. [DOI] [PubMed] [Google Scholar]
- 5.Rodriguez-Torres M, Jeffers LJ, Sheikh MY, et al. Peginterferon alfa-2a and ribavirin in Latino and non-Latino whites with hepatitis C [published correction appears in NEngl J Med. 2010;363(25):2474] N Engl J Med. 2009;360(3):257–267. doi: 10.1056/NEJMoa0805062. [DOI] [PubMed] [Google Scholar]
- 6.Turner BJ, Taylor BS, Hanson J, et al. High priority for hepatitis C screening in safety net hospitals: results from a prospective cohort of 4582 hospitalized baby boomers. Hepatology. 2015;62(5):1388–1395. doi: 10.1002/hep.28018. [DOI] [PubMed] [Google Scholar]
- 7.Scaglione S, Kliethermes S, Cao G, et al. The epidemiology of cirrhosis in the United States: a population-based study. J Clin Gastroenterol. 2015;49(8):690–696. doi: 10.1097/MCG.0000000000000208. [DOI] [PubMed] [Google Scholar]
- 8.Kim NJ, Locke CJ, Park H, Magee C, Bacchetti P, Khalili M. Race and hepatitis C care continuum in an underserved birth cohort. J Gen Intern Med. 2019;34(10):2005–2013. doi: 10.1007/s11606-018-4649-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turner BJ, Rochat A, Lill S, et al. Hepatitis C virus screening and care: complexity of implementation in primary care practices serving disadvantaged populations. Ann Intern Med. 2019;171(12):865–874. doi: 10.7326/M18-3573. [DOI] [PubMed] [Google Scholar]
- 10.DuBard CA, Gizlice Z. Language spoken and differences in health status, access to care, and receipt of preventive services among U.S. Hispanics. Am J Public Health. 2008;98(11):2021–2028. doi: 10.2105/AJPH.2007.119008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heintzman J, Bailey SR, Cowburn S, Dexter E, Carroll J, Marino M. Pneumococcal vaccination in low-income Latinos: an unexpected trend in Oregon community health centers. J Health Care Poor Underserved. 2016;27(4):1733–1744. doi: 10.1353/hpu.2016.0159. [DOI] [PubMed] [Google Scholar]
- 12.Heintzman JD, Bailey SR, Muench J, Killerby M, Cowburn S, Marino M. Lack of lipid screening disparities in obese Latino adults at health centers. Am J Prev Med. 2017;52(6):805–809. doi: 10.1016/j.amepre.2016.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heintzman J, Hwang J, Quiñones AR, et al. Influenza and pneumococcal vaccination delivery in older Hispanic populations in the United States. J Am Geriatr Soc. 2022;70(3):854–861. doi: 10.1111/jgs.17589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Community health center chartbook. National Association of Community Health Centers. https://www.nachc.org/research-and-data/research-fact-sheets-and-infographics/2021-community-health-center-chartbook/. Updated January 2022. Accessed January 25, 2022.
- 15.Rosenberg ES, Rosenthal EM, Hall EW, et al. Prevalence of hepatitis C virus infection in U.S. states and the District of Columbia, 2013 to 2016. JAMA Netw Open. 2018;1(8) doi: 10.1001/jamanetworkopen.2018.6371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hofmeister MG, Rosenthal EM, Barker LK, et al. Estimating prevalence of hepatitis C virus infection in the United States, 2013–2016. Hepatology. 2019;69(3):1020–1031. doi: 10.1002/hep.30297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Geboy AG, Nichols WL, Fernandez SJ, Desale S, Basch P, Fishbein DA. Leveraging the electronic health record to eliminate hepatitis C: screening in a large integrated healthcare system. PLoS One. 2019;14(5) doi: 10.1371/journal.pone.0216459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DeVoe JE, Gold R, Cottrell E, et al. The ADVANCE network: accelerating data value across a national community health center network. J Am Med Inform Assoc. 2014;21(4):591–595. doi: 10.1136/amiajnl-2014-002744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cook N, Turse EP, Garcia AS, Hardigan P, Amofah SA. Hepatitis C virus infection screening within community health centers. J Am Osteopath Assoc. 2016;116(1):6–11. doi: 10.7556/jaoa.2016.001. [DOI] [PubMed] [Google Scholar]
- 20.Bian J, Schreiner AD. Population-based screening of hepatitis C virus in the United States. Curr Opin Gastroenterol. 2019;35(3):177–182. doi: 10.1097/MOG.0000000000000520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mansergh G, Herbst JH, Holman J, Mimiaga MJ. Association of HIV pre-exposure prophylaxis awareness, preferred Spanish (vs. English) language use, and sociodemographic variables among Hispanic/Latino men who have sex with men. Ann Epidemiol. 2019;31:8–10. doi: 10.1016/j.annepidem.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 22.Derose KP, Baker DW. Limited English proficiency and Latinos’ use of physician services. Med Care Res Rev. 2000;57(1):76–91. doi: 10.1177/107755870005700105. [DOI] [PubMed] [Google Scholar]
- 23.Heintzman J, Kaufmann J, Lucas J, et al. Asthma care quality, language, and ethnicity in a multi-state network of low-income children. J Am Board Fam Med. 2020;33(5):707–715. doi: 10.3122/jabfm.2020.05.190468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.White RO, Osborn CY, Gebretsadik T, Kripalani S, Rothman RL. Health literacy, physician trust, and diabetes-related self-care activities in Hispanics with limited resources. J Health Care Poor Underserved. 2013;24(4):1756–1768. doi: 10.1353/hpu.2013.0177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heintzman JD, Ezekiel-Herrera DN, Quiñones AR, et al. Disparities in colorectal cancer screening in Latinos and non-Hispanic whites. Am J Prev Med. 2022;62(2):203–210. doi: 10.1016/j.amepre.2021.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kenny JD, Karliner LS, Kerlikowske K, Kaplan CP, Fernandez-Lamothe A, Burke NJ. Organization communication factors and abnormal mammogram follow-up: a qualitative study among ethnically diverse women across three healthcare systems. J Gen Intern Med. 2020;35(10):3000–3006. doi: 10.1007/s11606-020-05972-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huguet N, Kaufmann J, O'Malley J, et al. Using electronic health records in longitudinal studies: estimating patient attrition. Med Care. 2020;58(suppl 6 suppl 1):S46–S52. doi: 10.1097/MLR.0000000000001298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O'Malley JP, O'Keeffe-Rosetti M, Lowe RA, et al. Health care utilization rates after Oregon's 2008 Medicaid expansion: within-group and between-group differences over time among new, returning, and continuously insured enrollees. Med Care. 2016;54(11):984–991. doi: 10.1097/MLR.0000000000000600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Screening for hepatitis C virus infection in adolescents and adults: recommendation statement. Am Fam Physician. 2020;102(6):363–366. [PubMed] [Google Scholar]