HIGHLIGHTS
-
•
Human sex trafficking is widespread and a nationally recognized public health crisis.
-
•
A lack of training and awareness is a barrier to identifying trafficked individuals.
-
•
Increased knowledge and confidence illustrate the utility of this educational intervention.
-
•
Specialties can adapt this educational program by adding local statistics.
Keywords: Resident education, sex trafficking, human tracking, continuing medical education, research methods
Abstract
Introduction
Human sex trafficking is widespread and a nationally recognized public health crisis. Trafficked individuals and survivors often utilize the healthcare system, yet healthcare professionals cite a lack of formal training to identify and provide appropriate care. This study aims to increase obstetrics/gynecology, emergency medicine, and family medicine residents’ knowledge and confidence when caring for individuals involved in sex trafficking.
Methods
Obstetrics/gynecology, emergency medicine, and family medicine residents voluntarily attended an evidence-based education session and received an electronic pre-, immediate post-, and 5-month post-session survey measuring knowledge, attitudes, beliefs, and confidence. Validated survey items were adapted from previous studies. Paired t-tests (p<0.05) and descriptive analyses were used to determine differences. A concluding focus group was facilitated to further understand trainee experiences and awareness when caring for suspected sex-trafficked individuals and survivors. Thematic analysis determined reoccurring themes.
Results
Between 2019 and 2021, 48 pre-session, 28 immediate post-session, and 13 5-month post-session surveys were collected. Resident knowledge and confidence increased from the pre-session to the immediate post-session period. Session pre- and post-surveys were linked (n=14) and showed a statistically significant increase in knowledge (p<0.05) and an increase in confidence. The mean number of correct knowledge questions remained higher 5 months after the session than in the pre-session period. Focus group themes included increased resident knowledge and confidence.
Conclusions
Improvement and retention in resident knowledge and confidence in caring for sex-trafficked individuals illustrate the utility of this education intervention and expand on current literature. This study provides an example of an education session that can be adapted for other medical trainees.
INTRODUCTION
Human trafficking has increased in prevalence throughout the U.S., with cases spanning all the 50 states.1 Defined as obtaining labor or commercial sexual acts from an individual against their will, 11,500 cases of human trafficking were identified by the National Human Trafficking Hotline in 2020.2,3 This is a 5% increase compared with that in 2018.2 Of these human trafficking cases reported, 7,648 specifically identified sex trafficking or the “harboring, transportation, provision, or obtaining or a person for the purpose of commercial sex.”2,4 Sex trafficking is an important public health concern to healthcare providers owing to the prevalence but also because sex-trafficked individuals and survivors experience adverse physical, mental, and reproductive health outcomes.5,6 Furthermore, a qualitative study by Lederer et al. showed that 87.8% of survivors had direct contact with a healthcare provider while trafficked.5 Therefore, healthcare professionals are in an optimal position to screen for sex trafficking and care for trafficked individuals and survivors. More specifically, obstetrics/gynecology (OBGYN), emergency medicine (EM), and family medicine (FM) residents are in a unique and prominent position to screen for sex trafficking because residents often interact with patients presenting to labor and delivery, clinics, and the emergency department.
The greatest barriers for these healthcare professionals in identifying trafficked individuals are a lack of training and awareness.7 Efforts across the country have been attempted to advance healthcare professionals' knowledge and clinical skills.8 Most commonly, studies evaluating these education interventions focus on emergency department and pediatric healthcare professionals as a targeted sample and leave out other specialties, such as obstetricians/gynecologists, who may more commonly interact with trafficked individuals.8, 9, 10, 11, 12, 13 In addition, residents in any specialty should be able to confidently recognize the signs of sex trafficking and provide the necessary support to trafficked individuals and survivors. This study provides an example of a sex-trafficking education program for OBGYN, EM, and FM residents with an aim to increase residents’ knowledge and confidence when caring for trafficked individuals and survivors.
METHODS
Study Design and Setting
A prospective, mixed-methods education intervention was conducted at a single academic medical center in the Midwestern U.S. The study was approved by the Medical College of Wisconsin IRB.
Study Sample
OBGYN, EM, and FM residents from the Medical College of Wisconsin Affiliated Hospitals’ Residency Programs voluntarily attended the evidence-based education session and completed anonymous electronic surveys. The EM residency is composed of 9−12 residents per postgraduate year, across 3 years for a total of 31 residents. The FM residency is composed of 8−9 residents per postgraduate year for a total of 26 residents, and the OBGYN residency is composed of 8 residents across 4 postgraduate years for a total of 32 residents (Table 1).
Table 1.
Gender and Residency Year of Residents Who Completed the Pre-session Survey
| Demographics | OBGYN | Emergency medicine | Family medicine |
|---|---|---|---|
| Gender | |||
| Male | 6 | 8 | 2 |
| Female | 26 | 3 | 2 |
| Other | 0 | 0 | 1 |
| Year in residency | |||
| First | 12 | 6 | 1 |
| Second | 7 | 1 | 3 |
| Third | 6 | 4 | 1 |
| Fourth | 5 | 0 | 0 |
| Prefer not to respond | 2 | 0 | 0 |
OBGYN, obstetrics/gynecology.
Measures
The 45-minute education session was created on the basis of an extensive literature review of 202 articles that produced 7 studies that evaluated sex/human trafficking education programs in 2019.9,10,13, 14, 15, 16 These education sessions varied from facilitator-led lectures to self-directed online learning modules. Both virtual and in-person education programs included a didactic component through a PowerPoint or video and an interactive component through case discussions or quizzes. Content included definitions and statistics regarding sex trafficking in addition to the identification and treatment of potential trafficked individuals.7, 8, 9, 10, 11,14,15 The American College of Obstetrics and Gynecology's Committee Opinion on Human Trafficking and best practice resources from the National Human Trafficking Hotline and Health Education Advocacy Linkage Trafficking were also utilized.17, 18, 19
Using data from previous research, a PowerPoint was created with learning objectives that presented standardized definitions for human and sex trafficking. National and local statistics were also provided, highlighting human trafficking rates, strategies to identify sex-trafficked individuals, and principles of trauma-informed care and presenting an algorithm to care for suspected or established sex-trafficked individuals with local and national resources (Appendix A, available online). The algorithm was adapted from the algorithm created by Rabbit et al. to include patients aged >18 years (Appendix B, available online).6 After completing the education session, participants were provided with the algorithm and a list of local resources. Questions were embedded throughout the education session to engage active learning and for participants to make connections with the content. The research team decided to focus on sex trafficking rather than on the larger topic of human trafficking owing to the concern that the full topic of human trafficking may not be adequately covered in one 45-minute session. The Health Education Advocacy Linkage Assessment Tool for healthcare provider Human Trafficking Training was used to confirm that important content was included in the presentation. The educational presentation was reviewed by a locally recognized institutional leader in the field of sex trafficking education.
The 45-minute education session was facilitated by one of the authors (MRB) during the residents’ scheduled didactic time. Owing to the sudden onset of the coronavirus disease 2019 (COVID-19) global pandemic, the educational session for all OBGYN residents was converted from an in-person learning experience to a virtual format through Webex, a video conferencing and online meeting application (n=21) owing to mandatory restrictions on in-person gatherings. A second in-person education session was held for the incoming OBGYN first-year residents during their residency orientation (n=8). EM residents completed an in-person session during their scheduled didactic session (n=18). FM residents completed a virtual session during their scheduled didactic time (n=17). A recorded version of the OBGYN virtual session was provided to the OBGYN and EM residents through e-mail for those that could not attend the session. All sessions were completed between May 2020 and May 2021.
An anonymous 27-item electronic survey was developed to assess residents’ baseline knowledge, confidence, experience, and perceived barriers regarding suspected or confirmed sex-trafficked individuals and survivors (Appendix C, available online). The 9 knowledge questions were acquired with permission from the studies performed by Hansen et al. and Beck et al. with the intent to increase the validity of the knowledge questions.7,9 Previous studies informed the development of 5 Likert scale questions (1=not at all confident, 2=somewhat confident, 3=confident, 4=moderately confident, 5=extremely confident) to evaluate residents’ confidence to identify and screen trafficked individuals, identifying indicated medical evaluation and treatment, providing resources, and discussing the topic with patients.10,14,16 Questions asking participants to reflect on experiences and barriers were also included.7,11 In addition, the pre-education-session survey requested demographic questions of postgraduate year in the residency program and identified gender. Participants were asked to create an identification code used to link surveys across the 3 instances of pre-, immediate post, and 5-month post-survey.
The 27-item pre-education session survey was adapted to inform the 21-item posteducation survey and the 22-item, 5-month posteducation survey (Appendix C, available online). Each of these surveys included the same questions evaluating participants’ perceptions, knowledge, confidence, and perceived barriers. The immediate post-session and 5-month post-session surveys included additional questions on screening for sex-trafficked individuals and the usefulness of the education session (Appendix C, available online). The surveys were pilot tested by faculty, residents of non-OBGYN and EM specialties, and nonresident/physicians for clarity.
Before the education session, an e-mail was provided to all residents with a description of the study and a link to the anonymous pre-session survey (n=39 OBGYN, 35 EM, 26 FM residents). The immediate post-session and 5-month post-session surveys were distributed in a similar fashion.
The OBGYN and EM residents were encouraged/reminded to complete the surveys by the research team with 1 additional e-mail. The FM residents received a due date in the e-mail with the embedded link.
Statistical Analysis
Survey data were stored in an electronic database. Ten surveys were removed owing to noncompletion or error in the identification code. Paired sample t-tests with a p-value of 0.05 were used to investigate changes in knowledge and confidence among residents using survey responses with matched codes. Descriptive statistics were used to compare the total number of correct knowledge questions, reported confidence levels, reported barriers to care, and encounters with sex-trafficked individuals and survivors, from the preintervention period to postintervention and 5-month postintervention periods.
A concluding focus group was facilitated to further understand trainee experiences and awareness when caring for suspected sex-trafficked individuals and survivors. The semistructured session occurred over Zoom, an online meeting platform. One of the study team members (MRB) led 4 OB/GYN residents through 8 open-ended interview questions (Appendix D, available online). The session was recorded and transcribed verbatim. Two study team members (MRB and KK) independently coded the transcription to structure reoccurring codes and subsequent themes.
RESULTS
Demographics
The pre-, immediate post-, and 5-month posteducation session surveys were emailed to 39 OBGYN, 35 EM, and 26 FM residents. The pre-session surveys were completed by 32 OBGYN (82%), 11 EM (31%), and 5 FM (19%) residents at the Medical College of Wisconsin Affiliated Hospitals (n=48). Most residents who completed the pre-session survey were female (n=31, 64.5%) and in their first year of residency (n=19, 39.5%). The education session was attended by 29 OBGYN (21 virtual, 8 in person), 18 EM (in person), and 17 FM (virtual) residents. Twenty-eight residents (16 OBGYN, 7 EM, and 5 FM) completed the posteducation session survey. Of the residents who completed the immediate posteducation session survey, 16 residents attended the virtual session, 10 attended an in-person session, and 2 residents watched a recorded virtual session. Thirteen residents (9 OBGYN, 3 EM, and 1 FM) completed the 5-month post-session survey.
Clinical Knowledge
Knowledge was assessed by the number of questions answered correctly of 9. Globally, the mean number of correct knowledge questions answered by participants increased from before session to immediately after session and then decreased from immediately after session to 5 months after session. The mean number of correct knowledge questions remained higher 5 months after the session than before session (Figure 1).
Figure 1.
Change in the mean number of correct knowledge questions answered by residents from pre-session period to immediate post-session period to 5-month post-session period.
Paired sample t-tests of the 14 sets of linked pre-session and immediate post-session surveys showed a statistically significant increase in knowledge from pre-session (mean=5.92, SD=1.63) to post-session (mean=7.71, SD=0.91; t[13]=3.88, p<0.01) (Table 2). Paired sample t-tests of the 4 sets of surveys that included linked pre-session, immediate post-session, and 5-month post-session surveys showed a persistent statistically significant improvement in knowledge from pre-session (mean=5.75, SD=1.25) to 5-months post-session (mean=7.25, SD=0.95, t[3]=3, p<0.05) period (Table 3). Overall knowledge decreased from immediate post-session to 5-months post-session period.
Table 2.
Paired Sample t-Tests Comparing the Correct Number of Knowledge Questions and Confidence Levels from Pre-Session to Immediate Post-Session Periods for the 14 Individuals Whose Surveys Could Be Linked
| Question type | Pre-education session |
Immediately after education session |
DF |
||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | t observed | |
| Number of correct knowledge questions | 5.92 | 1.63 | 7.71 | 0.91 | 1.78 | 1.71 | 3.88 |
| Identification | 1.42 | 0.51 | 3.07 | 0.82 | 1.64 | 0.63 | 9.7 |
| Screening | 1.71 | 0.82 | 3.78 | 0.89 | 2.07 | 0.82 | 9.35 |
| Management | 1.85 | 1.16 | 3.5 | 0.85 | 1.64 | 1.21 | 5.05 |
| Community resources | 1.42 | 0.85 | 3.38 | 1.06 | 1.85 | 1.23 | 5.64 |
| Patient discussion | 1.42 | 0.75 | 3.28 | 1.06 | 1.85 | 1.16 | 5.95 |
Note: Critical t=2.65 for 1-tailed p=0.01 or 1.77. DF=13.
DF, difference.
Table 3.
Paired Sample t-Tests Comparing the Correct Number of Knowledge Questions and Confidence Levels from Pre- to 5-Months Post-Session Periods for the 4 Participants Whose Pre-Survey and 5-Month Surveys Could Be Linked
| Question type | Pre-education session |
5-months-post education session |
DF |
||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | t observed | |
| Number of correct knowledge questions | 5.75 | 1.25 | 7.25 | 0.95 | 1.5 | 1 | 3 |
| Identification | 1.25 | 0.5 | 2.25 | 0.5 | 1 | 0 | Could not be calculated |
| Screening | 1.75 | 0.5 | 2.25 | 0.5 | 0.5 | 0.57 | 1.73 |
| Management | 2.25 | 1.5 | 3.25 | 0.95 | 1 | 1.63 | 1.22 |
| Community resources | 1.25 | 0.5 | 1.75 | 0.5 | 0.5 | 0.57 | 1.73 |
| Patient discussion | 1.25 | 0.5 | 2 | 0 | 0.75 | 0.5 | 3 |
Note: Critical t right single 0.05=2.353. Critical 2-tailed 0.05=3.182. DF=13.
DF, difference.
Two sample t-tests comparing the correct number of knowledge questions immediately after session between participants who attended a virtual session (mean=7.5, SD=1.4) and those who attended an in-person session (mean=7, SD=1.15) showed no statistically significant difference (t[24]=0.91, p=0.36). Similarly, the number of correct knowledge questions 5 months after the session was not significantly different between participants who attended the virtual session (mean=6.71, SD=1.49) and those that attended an in-person session (mean=6.8, SD 1.3) (t[10]= −0.10, p=0.92). Correct number of knowledge questions immediately after education session was similar between OBGYN (mean=7.5, SD=1.20) and EM (mean=6.71, SD=1.38) (t[21]=1.48, p=0.15) residents, between OBGYN and FM (mean=7, SD=1.58) (t[19]=0.84, p=0.40) resident, and between EM and FM (t[10]= −0.33, p=0.74) resident.
Confidence in Providing Care
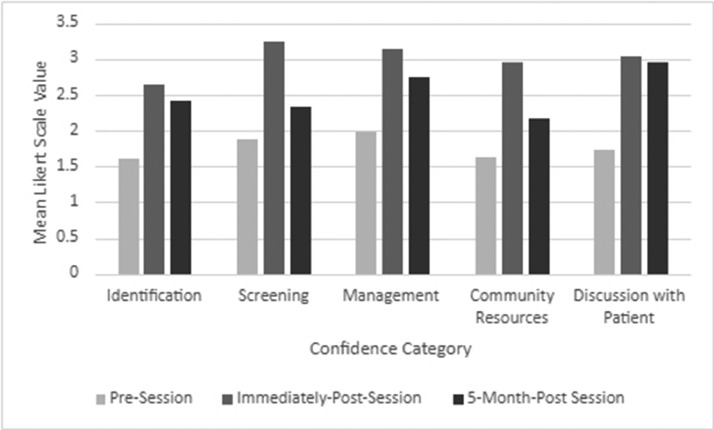
Before the education session, most residents were not at all confident or somewhat confident in identifying (n=41, 85%) and screening (n=38, 79%) sex-trafficked individuals, identifying indicated medical evaluation and treatment (n=35, 72%), providing resources (n=42, 87%), and discussing the topic of sex trafficking with patients (n=41, 85%). The mean confidence level reported by residents increased from pre-session to immediate post-session period and then decreased from immediate post-session to 5-month post-session period across all confidence categories. The mean confidence level of all confidence categories remained higher during 5-month post-session period than during the pre-session period (Figure 2).
Figure 2.
Change in mean Likert scale confidence level reported by residents from pre-session period to immediate post-session period, and to 5-month post-session period.
Paired sample t-test comparing the change in confidence level from pre-session to immediate post-session period for the 14 residents whose surveys were linked showed a statistically significant increase in confidence to identify and screen victims, identify indicated medical evaluation and treatment, provide resources, and discuss topics (p<0.01) (Table 2).
Paired sample t-tests of the 4 sets of surveys that included linked pre-session, immediate post-session, and 5-month post-session surveys did not show a persistent statistically significant improvement in confidence from pre-session to 5-months post-session periods (Table 3).
Encounters With Sex Trafficking Victims
Before the education session, most participants (n=24, 50%) did not know whether they had encountered a sex-trafficked individual over the course of 12 months. However, 32 (67%) reported encountering a sex-trafficked individual at some point in their training. The percentage of residents who reported having an encounter with a sex-trafficked individual at some point increased from pre-session (n=32, 67%) to immediate post-survey (n=21, 75%) and 5-month post-session (n=11, 85%) period. When asked, do you routinely screen individuals for sex trafficking in your practice?, 5 of 47 (10.6%) residents responded yes pre-session, and 5 of 13 (38.5%) responded yes at 5-month post-session survey. Three residents who reported not routinely screening before session reported routinely screening at 5 months after session.
Barriers to Care
The most common reported barrier when caring for sex-trafficked individuals before session was lack of training (78.3%), lack of awareness (47.8%), and lack of organizational policy/guidelines (32.6%). Immediately after session and 5 months after session, the most commonly reported barriers were lack of training (35.7% and 46.2%, respectively), lack of awareness (46.4% and 38.5%, respectively), and a delicate subject matter (53.6% and 46.2%, respectively). Compared with the pre-session period, a decreased percentage of residents reported a lack of training (n=10, 35.7%) and lack of organization policy/guidelines (n=4, 14.3%) as barriers to care immediately after session.
Participants’ perspectives gathered from the qualitative data from the focus group and open-ended survey questions in addition to categorical survey data provided insight into residents’ perspectives and opinions of the educational session. From the focus group data, themes derived were distilled to (1) residents who experienced an increase in knowledge and awareness after the education session, (2) residents who desired to increase screening, and (3) residents who experienced an overall retrospection of missed opportunities and discomfort when caring for a suspected sex-trafficked individual. An example of a statement supporting residents’ gaining of knowledge includes a participant stating “now when I have a patient with multiple STIs like automatically that's the first thing I think about whereas like before you know your doctor mind is always like just like let's just treat all of these and carry on.” The residents’ desire to increase screening is illustrated by a participant stating, “I feel like the more that we talk about it, I think the easier it is to be aware of and like know what to do when we have a suspicion.”
With respect to residents’ satisfaction with their training regarding sex trafficking, before the education session, 73% of respondents were slightly to extremely dissatisfied with their training to identify and assist sex-trafficked individuals. Immediately after the education session, 63% of respondents reported being moderately to extremely satisfied with their training. In addition, immediately after the education session, 67% (n=19) of the 28 respondents reported that they strongly agree that sex trafficking education should be a standard part of medical education.
Regarding the components of the education session, respondents reported that information about background, prevalence, definitions, community resources, phrasing/troubleshooting questions, and identifying risk factors was useful. Respondents reported that the education session could be improved by adding more interactive components and real-life examples/case scenarios.
DISCUSSION
The research team created this education session focusing on victims and survivors of sex trafficking to help resident physicians feel more prepared to identify and care for these individuals. The findings show that a 45-minute virtual or in-person didactic session improved residents’ knowledge and confidence regarding the sex trafficking of adults and adolescents utilizing both quantitative and qualitative data analysis. The education session was well received by the residents and can be adapted for other residency programs.
The study provides an example of a PowerPoint–based education session that can be adapted by other programs by adding local statistics and resources. The session expands on other studies focusing on trafficked youth to include trafficked adults. The education session also expands the targeted audience of other studies, which have focused on pediatric resident physicians and other healthcare professions. The similar number of correct knowledge questions post-education session between various residency groups shows the utility of the education session for different specialties, specifically OBGYN, EM, and FM.
The session was developed to fit well into an established 45-minute didactic session. Although limited by a small sample size, the lack of difference in the correct number of knowledge questions after session between individuals who attended the virtual and those who attended the in-person session supports that the session can be facilitated either way. The research team also created an algorithm for the identification and care of suspected trafficked individuals and survivors, which can be adapted by other institutions.
Similar to previous studies, our findings suggest that an education program is associated with an improvement in residents’ knowledge and confidence related to caring for sex-trafficked individuals and survivors. Our study findings were parallel to those of Lee et al., showing retention of knowledge months after the education session.20 Furthermore, the focus group supported the positive impact on residents’ perceived knowledge. Our study also showed that residents’ confidence levels remained higher 5 months after the education session than before session. However, the difference between pre- and 5-month post-session confidence levels was not statistically significant.
Our study expanded similar education session evaluations performed by other research teams by including a focus group and categorical questions investigating residents’ perspectives and opinions. The focus group and survey responses suggest that the residents valued the education session. Focus group participants reported that the session was useful. A majority of post-session survey respondents reported being satisfied with their training and strongly agreed that sex trafficking education should be a standard part of medical education. Furthermore, residents provided feedback on how to improve the education session, which is useful for future education session development.
Limitations
The development and facilitation of the education session were limited by a lack of involvement of a sex-trafficking survivor. Similar studies have shown a positive impact of involving survivors, and this education session would likely also benefit from such involvement. Our research team involved a local expert in sex trafficking when developing the education session and evaluation surveys. The focus on sex trafficking rather than on the larger topic of human trafficking also limited the scope of the education session and the ability to compare the education session with those of similar studies.
Furthermore, the pre- and post-survey design utilizing the same knowledge and confidence questions could limit the ability to truly evaluate the participants’ change in knowledge because participants could remember the questions. The evaluation of change in knowledge and confidence could also be limited by incomplete responses or the lack of provision of a code that would allow the surveys to be linked for evaluation.
In addition, the small sample size and high rate of loss to follow-up in paired/matched surveys are important limitations of the study. Our sample size is smaller than the sample sizes of other studies focusing on human trafficking. This small sample size could be explained by the study being performed at 1 location and the onset of the COVID-19 global pandemic. In addition, the education sessions were delivered over only 1 year, which limits the number of residents available to participate. The study had a large decrease in survey completion from pre to posteducation sessions. Possible reasons for this decline could be survey fatigue, lack of interest, or lack of time. Possible strategies to improve the sample size include increasing the study population to additional training programs/locations and increasing the number of years of data. Possible strategies to improve the response rate would be providing time directly after the education session to complete the survey, making the survey shorter, and providing incentives to complete the survey. Finally, differences in participants’ specialties and levels of training may alter the results but also facilitate a broad distribution of the education session.
CONCLUSIONS
Although the small sample size limits the ability of the study to truly evaluate the effectiveness of the education program, the study provides promising preliminary data to support the utility of the education session for resident physicians. The study provides an example of an education program that can be performed in a structured residency curriculum and be well received by the residents. The study also shows the utility of focus groups in evaluating the impact of an education session. Additional data and studies are needed to further evaluate the effectiveness of this program.
Other studies have shown the utility of similar education programs in improving healthcare professionals’ knowledge and confidence when caring for trafficked individuals. A joint effort to provide open access to pooled education resources would likely be beneficial for resident education regarding sex and human trafficking. These education efforts would hopefully lead to improved health outcomes for trafficked individuals and survivors.
CRediT authorship contribution statement
Morgan R. Briggs: Conceptualization, Methodology, Investigation, Formal analysis, Writing – original draft, Writing – review & editing, Visualization. Kristina Kaljo: Conceptualization, Methodology, Formal analysis, Writing – review & editing, Visualization, Supervision.
ACKNOWLEDGMENTS
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of interest: None
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.focus.2023.100088.
Appendix. Supplementary materials
REFERENCES
- 1.Stoklosa H, Grace AM, Littenberg N. Medical education on human trafficking. AMA J Ethics. 2015;17(10):914–921. doi: 10.1001/journalofethics.2015.17.10.medu1-1510. [DOI] [PubMed] [Google Scholar]
- 2.National human trafficking hotline. Hotline statistics. https://humantraffickinghotline.org/states. Accessed February 20, 2022.
- 3.National Human Trafficking Hotline. What Is Human Trafficking?https://humantraffickinghotline.org/ Accessed October 20, 2021.
- 4.National Center for Homeless Education. Victims of trafficking and violence protection act of 2000. https://nche.ed.gov/legislation/trafficking-violence-protection/#:∼:text=The%20Victims%20of%20Trafficking%20and,traffickers%20within%20the%20United%20States. Published 2000. Accessed October 21, 2021.
- 5.Lederer L, Wetzel C. The health consequences of sex trafficking and their implications for identifying victims in healthcare facilities. Ann Health Law. 2014;23:61–91. [Google Scholar]
- 6.Rabbitt A. The medical response to sex trafficking of minors in Wisconsin. WMJ. 2015;114:52–59. [PubMed] [Google Scholar]
- 7.Beck ME, Lineer MM, Melzer-Lange M, Simpson P, Nugent M, Rabbitt A. Medical providers’ understanding of sex trafficking and their experience with at-risk patients. Pediatrics. 2015;135(4):e895–e902. doi: 10.1542/peds.2014-2814. [DOI] [PubMed] [Google Scholar]
- 8.Powell C, Dickins K, Stoklosa H. Training US health care professionals on human trafficking: where do we go from here? Med Educ Online. 2017;22(1) doi: 10.1080/10872981.2017.1267980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hansen S, Melzer-Lange M, Nugent M, Yan K, Rabbitt A. Development and assessment of an online training for the medical response to sex trafficking of minors. Acad Pediatr. 2018;18(8):965–968. doi: 10.1016/j.acap.2018.07.009. [DOI] [PubMed] [Google Scholar]
- 10.Donahue S, Schwien M, LaVallee D. Educating emergency department staff on the identification and treatment of human trafficking victims. J Emerg Nurs. 2019;45(1):16–23. doi: 10.1016/j.jen.2018.03.021. [DOI] [PubMed] [Google Scholar]
- 11.Grace AM, Lippert S, Collins K, et al. Educating health care professionals on human trafficking. Pediatr Emerg Care. 2014;30(12):856–861. doi: 10.1097/PEC.0000000000000287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garg A, Panda P, Malay S, Rose JA. A human trafficking educational program and point-of-care reference tool for pediatric residents. MedEdportal. 2021;17:11179. doi: 10.15766/mep_2374-8265.11179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Egyud A, Stephens K, Swanson-Bierman B, DiCuccio M, Whiteman K. Implementation of human trafficking education and treatment algorithm in the emergency department. J Emerg Nurs. 2017;43(6):526–531. doi: 10.1016/j.jen.2017.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Lutz RM. Human trafficking education for nurse practitioners: integration into standard curriculum. Nurse Educ Today. 2018;61:66–69. doi: 10.1016/j.nedt.2017.11.015. [DOI] [PubMed] [Google Scholar]
- 15.Metcalf E, Selous C. Modern slavery response and recognition training. Clin Teach. 2020;17:47–51. doi: 10.1111/tct.13011. [DOI] [PubMed] [Google Scholar]
- 16.Chisolm-Straker M, Richardson LD, Cossio T. Combating slavery in the 21st century: the role of emergency medicine. J Health Care Poor Underserved. 2012;23(3):980–987. doi: 10.1353/hpu.2012.0091. [DOI] [PubMed] [Google Scholar]
- 17.Human trafficking. ACOG COMMITTEE OPINION, Number 787. Obstet Gynecol. 2019;134(3):e90–e95. doi: 10.1097/AOG.0000000000003427. [DOI] [PubMed] [Google Scholar]
- 18.National Human Trafficking Hotline. National hotline overview.https://humantraffickinghotline.org/national-hotline-overview. Accessed October 20, 2021.
- 19.HEAL Trafficking. Literature. https://healtrafficking.org/medical-literature/. Published 2021. Accessed October 21, 2021.
- 20.Lee H, Geynisman-Tan J, Hofer S, Anderson E, Caravan S, Titchen K. The impact of human trafficking training on healthcare professionals’ knowledge and attitudes. J Med Educ Curric Dev. 2021;8 doi: 10.1177/23821205211016523. 23821205211016523. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.