Abstract
Purpose of Review
Persistent stigma remains a crucial barrier to HIV prevention and treatment services among people who use drugs (PWUD), particularly for those living with or at-risk for HIV. This scoping review examines the current state of science with regard to approaches for measuring and addressing stigma within HIV interventions among PWUD.
Recent Findings
Sixteen studies fit the inclusion criteria for this review. Half the studies originated within the USA, and the remaining represented four different regions. Within these studies, stigma was measured using various quantitative, qualitative, and mixed methods. The studies primarily focused on HIV stigma, including value-based judgments, anticipated stigma, and perceived stigma domains. Information-based and skills building approaches at the individual level were the most common for the stigma reduction interventions.
Summary
Adoption of systematic evaluations is needed for measuring stigma, including intersectional stigma, within HIV interventions among PWUD. Future studies should focus on developing multilevel intersectional stigma reduction interventions for PWUD with and at-risk for HIV globally.
Keywords: HIV, People Who Use Drugs, Substance Use, Stigma, Intersectionality, Scoping Review
Introduction
As we are near 40 years into the HIV epidemic with tremendous biomedical and behavioral advancements, people who use drugs (PWUD) remain disproportionately affected by HIV [1, 2]. The relationship between HIV transmission and drug use has shifted throughout the epidemic, with decreases in the proportion of people acquiring HIV via injection drug use, yet more recent HIV clusters and outbreaks identified both nationally and internationally among people who inject drugs (PWID) [3, 4]. In 2017, an estimated 18% of PWID globally were living with HIV [1]. While sharing needles and injection equipment continues to significantly increase the risk for HIV acquisitions compared to sexual intercourse, non-injection drug use can also increase the risk for HIV and prevent engagement in HIV care. The HIV prevalence among PWUD more broadly is rising not only due to injection drug use but also sub-optimal engagement in prevention (e.g., PrEP and inconsistent condom use) and engagement in risk behaviors such as multiple sex partners, overlapping of sexual networks between PWID and non-PWID, and polysubstance use coupled with the potential to start injecting drugs [5–9]. PWUD are often discriminated against and stigmatized which can lead to limited access and engagement in HIV prevention and treatment services further exacerbating their HIV burden.
A significant barrier to HIV prevention and treatment services for PWUD is stigma. Stigma is a complex social process conceptualized as an “attribute that is deeply discrediting” imposed by society that diminishes someone “from a whole and usual person to a tainted, discounted one” [10]. Broadly, stigma has four primary components, including distinguishing and labeling differences among individuals, associating negative attributes to identified differences, and separation and distancing that results in status loss and discrimination [11]. Stigma has been conceptually differentiated into several manifestations—experienced, perceived, anticipated, and internalized. Experienced stigma includes actual experiences of the interpersonal act of discrimination. Perceived stigma is one’s perception that individuals or societies treat people differently due to a stigmatized attribute. Anticipated stigma is the expectation of stigma or discrimination within a particular context. Finally, internalized stigma refers to accepting experienced and perceived stigma leading to a belief of one’s lesser status within a society.
Both external and internal stigma can negatively affect engagement in HIV prevention and treatment [12–14]. External stigma refers to experiential acts of discrimination, including perceived and anticipated stigma that can occur within one’s community [15]. Internal stigma is the shame or internal oppression that can result in self-loathing, isolation, and low levels of self-worth [15, 16]. External and internalized stigma related to HIV can undermine ongoing efforts for enhancing HIV prevention, testing, linkage to care, and treatment adherence. Substantial evidence exists demonstrating HIV stigma can hinder one’s utilization of HIV prevention and delay HIV testing and knowledge of status [17–19]. Furthermore, HIV stigma is a well-documented barrier to linkage to care and treatment [18, 20], thus severely hindering ambitious goals for ending the HIV epidemic by 2030 [21].
PWUD often endure overlapping or intersectional stigma, further obstructing HIV prevention and treatment provision and utilization. Intersecting stigma is the convergence of multiple stigmas from social identities, health conditions, or behaviors, such as drug use and HIV [22–24]. PWUD experience various types of intersecting stigma related to drug use and HIV and potentially other intersecting identities (e.g., related to a mental health condition, gender, or sexual orientation). Evidence indicates that PWUD often have elevated levels of internalized and anticipated stigma related to their drug use [25]. As a result, PWUD may avoid seeking healthcare, including HIV care [26–29]. HIV stigma has similarly been associated with sub-optimal engagement in HIV prevention and treatment among PWUD [30, 31]. PWUD may avoid HIV testing, pre-exposure prophylaxis (PrEP) use, HIV treatment due to shame, fear of disclosure, or possible isolation or ostracization from social networks [32–36]. Both drug use and HIV stigma likely are not occurring in isolation from one another but rather are interrelated.
PWUD uniquely experience intersecting drug use stigma in conjunction with HIV and potentially other forms of stigma. Intersectional stigma is the juncture of multiple stigmas from social identities, health conditions, or behaviors, such as drug use and HIV [22–24, 37, 38]. While recent studies are beginning to assess intersecting HIV and drug stigma quantitively [23, 39], challenges remain given the complexity in estimations and interpretations [40, 41]. Additionally, internalized substance use stigma may be under-reported because it is a stigma that ascribes blame to the stigmatized individual, further complicating the assessment of intersectional stigma among PWUD [42].
Several reviews have documented a rich history of HIV stigma reduction within HIV prevention and treatment interventions [43–47]. Broadly, most reviews have identified substantial progress in the HIV stigma reduction field, with a growing body of evidence on multilevel strategies for reducing HIV stigma. However, few examine stigma-reduction strategies and studies specifically for PWUD, which are needed to optimize HIV biomedical and behavioral advancements. For example, one meta-analysis quantified HIV and drug-related stigma associations on injection equipment sharing across studies, specifically among PWID [47]. The majority of these reviews broadly include all HIV stigma regardless of the target population, limiting our understanding of interventions tailored for PWUD and other stigmatized conditions, such as drug use or addiction.
In this scoping review, we assess the recent state of science with regard to approaches for measuring and addressing stigma within HIV interventions among PWUD. We will describe the country and origin of research studies, detail the measurements utilized to understand HIV and drug use stigma, and depict the design and participants of the HIV interventions. We conclude by highlighting opportunities for new research. We chose a scoping review of the literature to allow for rapid mapping of all types of available evidence underpinning this research topic [48].
Methods
For this scoping review, we followed the Arksey and O’Malley’s framework for a scoping study, including (a) identifying the research question (if and how has stigma been measured and/or addressed in HIV prevention and treatment interventions among PWUD?); (b) identifying relevant studies; (c) selecting studies; (d) charting the data; and (e) summarizing and reporting results [48]. Our review considered the following types of stigma, including HIV stigma and stigma surrounding marginalized populations such as PWUD.
Identifying Relevant Studies
The search was conducted in five bibliographic databases, including PubMed, Web of Science, CINAHL, PsycINFO, and Academic Search Complete, to identify relevant publications. Keywords were used in combination according to the proper syntax of each database and included the following expressions: “HIV/AIDS”; “HIV”; “Human Immunodeficiency Virus”; “AIDS”; “Acquired immune deficiency syndrome”; “PrEP”; “Pre-exposure prophylaxis”; “Preexposure prophylaxis”; “ART”; “Antiretroviral therapy”; “Antiretrovirals”; “drug-use”; “drug use”; “PWID”; “PWUD”; “people who use drugs”; “people who inject drugs”; “substance use”; “substance use disorder”; “Stigma”; “Prejudice”; “Attitude”; and “Discrimination” (see supplementary document for the detailed search strategy).
To increase the relevance of the findings of this review for current practice, only papers published from September 1, 2011, through October 15, 2021, were included. Papers not published in English were excluded along with commentaries, letters, editorials, review articles not including primary data collection, articles with no reported drug use or measure of stigma, and articles without an intervention. Additionally, papers that detailed cross-sectional studies and protocol papers that did not contain an endpoint were excluded from our search. Only interventions that contained prospective follow-up or a measure of feasibility and effectiveness outcomes were included.
Study Selection
The selection process consisted of two phases. First, two of five reviewers screened all titles and abstracts independently. Studies were selected for second phase review if reviewers had consensus, where discrepancies could not be resolved, and if eligibility could not be determined based on the titles and abstracts. Two of five reviewers independently screened full texts of the studies selected in phase 1 to determine eligibility conclusively in the second phase. A hand review was then conducted of final articles, in which references of included papers were scanned for any additional articles that fit the defined search criteria. Any discrepancies in study eligibility after this phase were subject to a third-party reviewer who decided whether to include the article in our scoping review and resolve any remaining disputes.
Charting Data
Peer-reviewed titles and abstracts identified during the literature search were uploaded, assigned an article ID number, and reviewed in an excel spreadsheet. (1) abstracts without full text available, (2) non-peer-reviewed, (3) review or not original research, (4) non-human subjects research, (5) no illicit drug use reported among participants or intervention goal was not focused on PWUD, (6) no measures of stigma reported, or (7) not an HIV or stigma reduction intervention. After this was completed, the third reviewer checked over their work to ensure accuracy.
All articles passing the first phase of study selection were added to a second excel spreadsheet. Reviewers then exported the title, author, year of publication, and article ID number for all the studies into the excel spreadsheet for data abstraction and charting. Two of the five reviewers then abstracted data on the following topics from each article: study population, study origin, stigma instrument, assessment format, stigma reduction approach, and intervention level. Stigma reduction approaches included information-based, skills building, counseling, contact and partnership, structural, or biomedical approaches [12]. Intervention level was informed by the social-ecological environment involving individual, interpersonal, organizational, and structural levels [49]. Abstracted data were reviewed for consistency, and the first author and reviewers discussed any discrepancies and settled any disputes.
Results
Our initial search produced 2441 results (PubMed = 730; CINAHL = 292; PsycInfo = 483; Academic Search Complete = 384; Web of Science = 552). After removing duplicates, 1,151 peer-reviewed studies remained. Review of the titles and abstracts identified 134 studies for full-text examination, after which 16 studies were identified as meeting the inclusion criteria (Fig. 1).
Fig. 1.
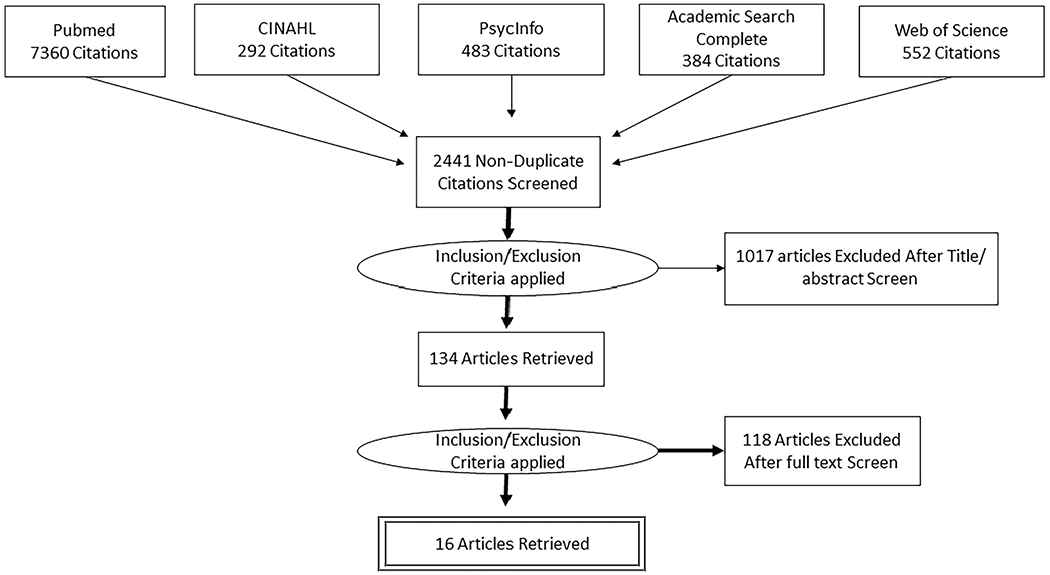
Overview of study selection
Study Characteristics
The studies represented five WHO regions (Table 1). Eight studies originated from the Americas, three from the Western Pacific region, two from the African region, one European region, and one from Southeast Asia. In addition, one study included multiple regions, including the Southeast Asia, Western Pacific, and European regions. Of all the studies, a total of six originated from World Bank defined low to middle-income countries.
Table 1.
Characteristics of included studies
| World Health Organization region | |
|---|---|
| Africa | 2 |
| Americas | 8 |
| Europe | 1 |
| Southeast Asia | 1 |
| Western Pacific | 3 |
| Multiple: Southeast Asia, Western Pacific, and Europe | 1 |
Stigma Instruments and Measurement
Studies that met the inclusion criteria reported a variety of quantitative, qualitative, and mixed methods for measuring stigma among PWUD (Table 2). Stigma domains included value-based judgments, anticipated stigma, perceived stigma, with much of the focus on HIV stigma rather than drug use stigma.
Table 2.
Included studies (n = 16) by year of publication
| Authors | Year published | Study origin | Stigma instrument and measurement | Stigma assessment method | Intervention target | Intervention strategy | Level |
|---|---|---|---|---|---|---|---|
| Mateu-Gelabert et al. [50] | 2014 | New York, USA | Keeping It Together 10-item scale | Quantitative | PWID1 | Skills building | Individual |
| Basta, Stambaugh & Fisher [51] | 2015 | Ohio, USA | Nine Likert scale items adapted from a national AIDS and stigma survey | Quantitative | People living in rural Appalachia, unaware of HIV status or HIV negative | Information | Individual |
| Go et al. [57] | 2017 | Vietnam | Experience drug use stigma | Quantitative | HIV-positive men who inject drugs | Information, skills building, and counseling | Individual, interpersonal |
| Burgess et al. [64] | 2018 | Australia | Intervention feedback: lack of stigma | Qualitative | Gay men and other men who have sex with other men who use methamphetamine | Skills building and biomedical | Individual, interpersonal |
| Maskay et al. [52] | 2018 | 6 geographically diverse sites, USA | Six questions on perceived and external HIV stigma adapted from the Behavioral Risk Factor Surveillance System module | Quantitative | HIV positive persons with previous or current substance use disorders or mental illness | Structural | Individual, organizational |
| Sugarman et al. [58] | 2019 | Indonesia, Ukraine, and Vietnam | Reported benefits related to trial participation, including “reduced stigma” | Quantitative | HIV-infected people who use drugs | Biomedical, counseling, and structural | Individual, organizational |
| Duby et al. [61] | 2019 | South Africa | Stigma awareness, understanding of experienced stigma | Mixed methods | Healthcare workers | Information, contact and partnership, and structural | Organizational |
| Tofighi et al. [59] | 2019 | New York, USA | Intervention feedback: open text | Quantitative | Healthcare workers | Information, contact and partnership, structural | Organizational |
| Fix et al. [60] | 2019 | USA | Reported fear/stigma as reason for not HIV testing | Quantitative | Adolescents in juvenile drug court | Information, skills building, and counseling | Individual |
| Lewis et al. [53] | 2020 | New York, USA | HIV Stigma Index 2.0 scale | Quantitative | PWUD2 | Information and biomedical | Individual |
| Gichane et al. [62] | 2020 | South Africa | intervention acceptability and appropriateness | Mixed methods | Women living with HIV and who use alcohol or other drugs |
Information, skills building, and biomedical | Individual |
| Batchelder et al. [54] | 2020 | USA | HIV Shame Inventory (HARSI); intervention participant feedback | Mixed methods | HIV positive individuals with substance use disorders | Counseling, skills building | Individual |
| Silvia [63] | 2020 | USA | Intervention feedback; Change in empathy towards PWUD | Mixed methods | Health care workers | Information | Organizational |
| Lunze et al. [65] | 2021 | St. Petersburg, Russia | Experience and anticipated stigma | Qualitative | HIV positive PWID3 | Skills building and structural | Individual, Organizational |
| Broady et al. [56] | 2021 | Australia | Negative attitudes towards people of their HIV status or IDU with a 5 Likert scale response options ranging from “never” to “always” |
Qualitative | General public | Contact and partnership | Interpersonal |
| Lemons-Lyn et al. [66] | 2021 | Myanmar | Single question on feeling safe and free from stigma in waiting area | Mixed methods | Health care workers | Information, skills building, and structural | Organizational |
People who inject drugs
People who use drugs
People who inject drugs
Five studies reported using or adapting established stigma and stigma-related scales [50–54]. One of these studies among PWUD in New York City measured externalized stigma, which involved a 9-item scale of anticipated HIV shame and blame from the HIV Stigma Index 2.0 [53]. PWUD also participated in qualitative interviews to identify internalized stigma towards accessing post-exposure prophylaxis (PEP). Basta et al. adapted nine Likert scale items from a national AIDS and stigma survey to measure negative attitudes towards or value-based judgments of those with HIV among people living in rural Appalachia and reporting a mental illness and alcohol, tobacco, and drug addiction [55]. The items focused on negative emotions and feelings such as disgust, anger, and fear towards those living with HIV. As part of a non-experimental intervention pilot among PWID in New York, IDU stigma management was examined using a 10-item scale called Keeping It Together [50]. This scale covered three domains: living a normal life, taking care of veins, and distancing oneself socially from other injectors. Lastly, one study originating in Australia measured members of the general public’s negative attitudes towards people living with HIV or who injected drugs with a 5-item Likert scale with options ranging from “never” to “always” [56].
Five studies measured stigma using quantitative evaluations [57–60]. For example, one trial reported drug use stigma quantitatively among PWID in Vietnam using a single question on experiencing stigma by their community due to their drug use [57]. An additional trial conducted in Indonesia, Ukraine, and Vietnam ascertained reported benefits to trial participation that included stigma reduction, without specification on type of stigma or stigmatizing condition [58]. As part of a feasibility study of training and support in managing opioid use disorder among primary care providers (PCPs), pre- and post-training surveys obtained suggestions for improving future trainings [60]. PCPs suggested providing future training on reducing stigma toward PWUD among clinic staff.
Several studies used mixed-methods of qualitative and quantitative measures that also included established quantitative scales [54, 61–63]. In mixed-methods evaluation within South Africa for example, Duby et al. examined the effects of a sensitization training intervention, the “Integrated Key Populations Sensitivity Training Programme for Healthcare Workers in South Africa,” on changes in stigma and discrimination towards key populations, including PWUD [61]. Both quantitative and qualitative methods were conducted. Pre- and post-training assessments documented staff’s awareness on “how stigma affecting key populations limits access to effective healthcare.” Qualitative interviews also revealed how the intervention addressed their previous judgmental attitudes or enhanced their understanding of the discrimination key populations may experience.
Three studies used only qualitative methodology to assess stigma [56, 64, 65]. For example, Lunze et al. conducted an implementation study of an intervention linking PWID to HIV care in Russia [65]. Qualitative interviews were conducted among PWID participants to identify implementation barriers and levers of implementation guided by the Consolidated Framework for Implementation Research (CFIR) and Normalization Process Theory as analytical frameworks. Experience and anticipated stigma and discrimination emerged as inhibiting health-seeking behavior. Within a study among men who have sex with men (MSM) who use methamphetamine, qualitative interviews were conducted as part of participating within a methamphetamine treatment and support program for MSM, in which lack of perceived stigma when engaging with peers emerged in intervention feedback [64]. An implementation study of the Women’s Health CoOp (WHC) is a gender-focused, risk-reduction EBI originally developed for women who use alcohol, and other drugs (AOD) used focus group discussions, joint interviews, and in-depth interviews to explore the intervention acceptability and appropriateness [62]. Participants reported experiencing community-level stigma due to their gender, substance use, and HIV status.
Intervention Characteristics
The most common stigma reduction strategies involved information-based and skills building approaches, including education to enhance knowledge on HIV or drug use or the effect of stigma manifestations on health and well-being (Table 2) [50, 51, 53, 56, 57, 59, 60, 62–66]. For example, in Vietnam, a randomized control trial of a multilevel PWID and HIV stigma reduction intervention was conducted to optimize HIV outcomes, including survival, among PWID [57]. The multilevel intervention addressed structural level stigma with a community educational campaign of door-to-door communications, community video screenings, and individual-level counseling and group support. Community educational campaigns focused on correcting misconceptions related to HIV transmission and promoting positive HIV and drug use messages. At the individual-level counseling and group support were provided to facilitate discussion and skills building to cope with stigma. At baseline, approximately three-fourths reported being stigmatized due to drug use by their community. PWID who were members of the community-wide intervention and the individual-level intervention had increased 2-year survival and improvements in HIV treatment.
Six studies included on stigma reduction towards PWUD with community members or clinic providers [52, 56, 59, 61, 63, 66]. Drawing from Allport’s intergroup contact theory, an online contact intervention was conducted with the goal of reducing stigma and discrimination of members within the Australian general public towards people living with HIV or who inject drugs [56]. Participants were presented a short three-to-five-minute video depicting people living with HIV or who inject drugs describing real-life experiences with discriminatory attitudes or anticipated stigma within community and healthcare settings. Reductions were identified in reports of negative attitudes towards both people living with HIV or who inject drugs. The Integrated Key Populations Sensitivity Training Programme for Healthcare Workers in South Africa involved a one-day sensitization training program for healthcare workers that addressed socio-structural marginalization and prejudice and interventions to foster an enabling healthcare environment for key populations, including PWUD [61]. Post-intervention evaluations identified increases in knowledge of discrimination and marginalization of key populations among healthcare workers.
The individual level was the most frequent target of the interventions [50, 51, 53, 54, 57, 60, 62, 64, 65]. For example, PWUD in NYC received a 10-min vignette-based PEP education video and direct pharmacy access to PEP following HIV exposure [53]. The video content was guided by the social cognitive theory, which focused on enhancing PEP knowledge and did not report an explicit stigma component. Instead, low anticipated stigma was identified as a factor associated with PEP willingness. Another study conducted in the USA developed a brief text-enhanced transdiagnostic emotion regulation intervention for HIV-positive persons with substance use disorders to mitigate the negative consequences of internalized stigma, shame, and other self-conscious emotions on engagement in HIV self-care behaviors [54]. The intervention involved five individual sessions that addressed metacognitive awareness of emotions and cognitions, cognitive reframing (e.g., compassionate self-statements), and identifying and refining self-care goals (e.g., goal setting and problem-solving skill development). Participants also received daily and weekly texts, which included emotion queries and compassionate self-statements.
Discussion
The studies identified in this scoping review were few, highlighting the need for systematic stigma evaluations and multilevel stigma reduction interventions for PWUD with and at-risk for HIV globally. Most of the studies originated from the USA, which may not be directly translatable to other global settings where HIV and drug use may be more prevalent and discriminated against. Further, studies primarily assessed HIV-related stigma. Only a few examined drug use stigma, despite a focus on PWUD, and none of these studies specifically measured intersecting stigmas. Gender-related stigma was also largely unmeasured or unaddressed across the studies. Common approaches for stigma reduction interventions consisted of information-based and skills building approaches mainly situated at the individual level. While a range of interventions have been designed to mitigate the negative consequences of stigma related to drug use [67], our results indicate that few have been implemented among PWUD with and at-risk for HIV. To date, therapeutic interventions to reduce drug-related internalized or self-stigma, motivational interviewing, or sharing humanizing stories of stigmatized others have been used to reduce drug-related social stigma, and contact-based strategies and educational interventions have been used to reduce structural stigma. More work is needed to incorporate these strategies into intersectional stigma reduction interventions for PWUD with and at-risk for HIV.
Given the broad range of approaches and measures used to assess stigma among PWUD, more rigorous and valid measures of stigma may be warranted. Qualitative research on stigma among PWUD can provide illustrative examples and documentation of the lived experiences and attitudes of stigma among PWUD [68]. While this evidence is critical to enhance our understanding of manifestations of stigma, qualitative work limits our ability to systematically evaluate the impact of stigma reduction interventions or engagement in HIV prevention and treatment. Several validated HIV and drug use stigma scales exist, including the Substance Use Stigma Mechanisms Scale (SU-SMS), Social Distance Scale for Substance Users, and Affect Scale for Substance Users [69, 70]. However, more work is needed to psychometrically establish these scales across populations of people who use drugs with and vulnerable to HIV [71, 72]. Further quantitative research will be critical for developing and culturally adapting well-validated stigma to rigorously measure stigma as part of stigma reduction interventions for specifically for PWUD.
The studies within our review primarily originated within the USA. Yet, HIV incidence is highly concentrated among PWUD in many global settings, including Eastern Europe and parts of Southeast Asia, and the Western Pacific [1, 73, 74]. Notably, an HIV and drug use stigma reduction in Vietnam implemented culturally relevant community-level information-based approaches to delink people living with HIV and using drugs as “social evils” [57, 75]. HIV and drug use stigma can manifest in unique ways across cultural and social norms that vary geographically. Because stigma is culturally bound, culture-based stigma reduction interventions will be critical for mitigating HIV and drug use stigma throughout various contexts.
None of the included studies examined or addressed intersectional stigma explicitly. While this may be attributable to the documented challenges of evaluating intersectional stigma [41], the intersectionality framework indicates that individuals’ identities interlock and interact with social contexts involving privilege and oppression [76–78]. Recent strides have been made in the measurement of intersectional stigma [79, 80]; however, work is needed to integrate substance use stigma into these conceptualizations and measurement strategies. Therefore, according to this framework, identity is not the additive compilations of identities but rather the concurrent experience of the intersection of aspects of one’s identity [81]. From this perspective, the impact of stigmas related to HIV and drug use among PWUD with and at-risk for HIV, as well as potentially other stigmas experienced by this population (e.g., stigmas related to living with mental illness, being a sexual minority, being homeless or marginally housed, and gender), is most meaningfully examined together. Recent work has begun to examine intersecting HIV and drug use stigmas and other intersecting stigmas (e.g., sexual orientation-related stigma) in relation to health outcomes such as engagement in HIV self-care behaviors [25, 26, 38, 39]. However, interventions are needed to address intersecting HIV and drug use stigma.
Relatedly, gender-related stigma was under-investigated across studies. Only one included study focused on women living with HIV and using alcohol or other drugs [62]. While this study had a gender focus, none of the other studies reported gender differences in stigma or examined gender-based stigma or sexism. Evidence indicates that women, both cis- and transgender women, who inject drugs are the most vulnerable to HIV via unprotected sex and unsafe injection practices [74, 82, 83], likely exacerbated by violence, poorer quality of healthcare [84, 85], and stigma and discrimination related to gender (e.g., sexism, transphobia, and femmephobia) [86, 87]. Women-specific, multilevel interventions will be essential to acknowledge and intervene on the unique intersectional stigmas and related barriers women who use drugs face [88, 89].
While this article makes an important contribution to the literature, there are several limitations. Our process of article selection, including studies reported in English only, excluding gray literature, including unpublished and non-peer-reviewed studies, may limit the generalizability of our findings beyond peer-reviewed English studies. To minimize possible selection bias, we did utilize independent secondary article reviewers and data extractors. Our search terms were specific to illicit drug or substance use and therefore did not include articles that evaluated or addressed stigma for people who reported only alcohol or tobacco use. Additionally, we did not include some terms indicative of specific forms of stigma such as minority stress, and homonegativity, potentially limiting the inclusion of studies that focused on specific forms of stigma which used more specific language. Despite these limitations, this synthesis of the current literature indicates critical next steps in the reduction of stigma among PWUD with and at-risk for HIV.
Conclusion
Despite the global progress over the past, there remains the need to strengthen HIV and drug use stigma measurement and interventions for PWUD. Systematic and harmonized stigma measurements, particularly for intersecting stigmas, will enhance comparisons of stigma manifestations and reduction efforts worldwide. Future multilevel stigma reduction interventions should address the intersectional stigma that PWUD with and at-risk for HIV endure.
Supplementary Material
Funding
KEL was supported by the National Institute of Drug Abuse through K01DA048174 (Lancaster, PI) and R21DA053708 (Lancaster, PI). AWB was supported by the National Institute of Drug Abuse through K23DA043418 (Batchelder, PI) and R34DA053686 (Batchelder, PI).
Footnotes
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s11904-022-00619-9.
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest The authors declare no competing interests.
References
- 1.Degenhardt L, Peacock A, Colledge S, Leung J, Grebely J, Vickerman P, et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob Health. 2017;5(12):e1192–207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Csete J, Kamarulzaman A, Kazatchkine M, Altice F, Balicki M, Buxton J, et al. Public health and international drug policy. Lancet (London, England). 2016;387(10026):1427–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Des Jarlais DC, Kerr T, Carrieri P, Feelemyer J, Arasteh K. HIV infection among persons who inject drugs: ending old epidemics and addressing new outbreaks. AIDS (London, England). 2016;30(6):815–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC) Health Alert Network. Recent HIV clusters and outbreaks across the United States among people who inject drugs and considerations during the COVID-19 pandemic. Health Alert Network (HAN), 2020. Retrieved from https://emergency.cdc.gov/han/2020/han00436.asp. Accessed Jan 2022.
- 5.Tavitian-Exley I, Vickerman P, Bastos FI, Boily MC. Influence of different drugs on HIV risk in people who inject: systematic review and meta-analysis. Addiction (Abingdon, England). 2015:110(4):572–84. [DOI] [PubMed] [Google Scholar]
- 6.Des Jarlais DC, Arasteh K, McKnight C, Feelemyer J, Campbell AN, Tross S, et al. What happened to the HIV epidemic among non-injecting drug users in New York City? Addiction (Abingdon, England). 2017;112(2):290–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Keefe D, Horyniak D, Dietze P. From initiating injecting drug use to regular injecting: retrospective survival analysis of injecting progression within a sample of people who inject drugs regularly. Drug Alcohol Depend. 2016:158:177–80. [DOI] [PubMed] [Google Scholar]
- 8.Neaigus A, Miller M, Gyarmathy VA, Friedman SR. HIV heterosexual sexual risk from injecting drug users among HIV-seronegative noninjecting heroin users. Subst Use Misuse. 2011;46(2–3):208–17. [DOI] [PubMed] [Google Scholar]
- 9.Larney S, Mathers BM, Poteat T, Kamarulzaman A, Degenhardt L. Global epidemiology of HIV among women and girls who use or inject drugs: current knowledge and limitations of existing data. J Acquir Immune Defic Syndr. 2015;69(Suppl 2):S100–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goffman E Stigma: Notes on the management of spoiled identity. New York, New York: Simon & Schuster Inc., 1986:2009. [Google Scholar]
- 11.Link BG, Phelan JC. Stigma and its public health implications. Lancet (London, England). 2006;367(9509):528–9. [DOI] [PubMed] [Google Scholar]
- 12.Nyblade L, Mingkwan P, Stockton MA. Stigma reduction: an essential ingredient to ending AIDS by 2030. The lancet HIV. 2021;8(2):e106–13. [DOI] [PubMed] [Google Scholar]
- 13.Mbonu NC, van den Borne B, De Vries NK. Stigma of people with HIV/AIDS in sub-Saharan Africa: a literature review. J Trop Med. 2009:2009:145891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rankin WW, Brennan S, Schell E, Laviwa J, Rankin SH. The stigma of being HIV-positive in Africa. PLoS Med. 2005;2(8):e247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boyd JE, Otilingam PG, DeForge BR. Brief version of the Internalized Stigma of Mental Illness (ISMI) scale: psychometric properties and relationship to depression, self esteem, recovery orientation, empowerment, and perceived devaluation and discrimination. Psychiatr Rehabil J. 2014:37(1):17. [DOI] [PubMed] [Google Scholar]
- 16.Batchelder AW, Hagan MJ. The clinical relevance of a socioecological conceptualization of self-worth. Rev Gen Psychol 2022. 10.1177/10892680221109201 [DOI] [Google Scholar]
- 17.Musheke M, Ntalasha H, Gari S, McKenzie O, Bond V, Martin-Hilber A, et al. A systematic review of qualitative findings on factors enabling and deterring uptake of HIV testing in sub-Saharan Africa. BMC Public Health. 2013:13:220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gesesew HA, Tesfay Gebremedhin A, Demissie TD, Kerie MW, Sudhakar M, Mwanri L. Significant association between perceived HIV related stigma and late presentation for HIV/AIDS care in low and middle-income countries: a systematic review and meta-analysis. PLoS ONE. 2017;12(3):e0173928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Calabrese SK. Understanding, contextualizing, and addressing PrEP stigma to enhance PrEP implementation. Curr HIV/AIDS Rep. 2020;17(6):579–88. [DOI] [PubMed] [Google Scholar]
- 20.Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. 2013:16(3 Suppl 2):18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bain LE, Tarkang EE, Ebuenyi ID, Kamadjeu R. The HIV/AIDS pandemic will not end by the year 2030 in low and middle income countries. Pan Afr Med J. 2019;32:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Collins PH, Bilge S. Intersectionality: John Wiley & Sons; 2020.
- 23.Earnshaw VA, Smith LR, Cunningham CO, Copenhaver MM. Intersectionality of internalized HIV stigma and internalized substance use stigma: Implications for depressive symptoms. J Health Psychol. 2015;20(8):1083–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Earnshaw VA, Bogart LM, Dovidio JF, Williams DR. Stigma and racial/ethnic HIV disparities: moving toward resilience. Am Psychol. 2013;68(4):225–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Batchelder AW, Foley JD, Kim J, Thiim A, Kelly J, Mayer K, et al. Intersecting internalized stigmas and HIV self-care among men who have sex with men and who use substances. Soc Sci Med. 1982:2021(275):113824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Batchelder AW, Foley JD, Wirtz MR, Mayer K, O’Cleirigh C. Substance use stigma, avoidance coping, and missed hiv appointments among msm who use substances. AIDS Behav. 2021:25(5):1454–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stringer KL, Marotta P, Baker E, Turan B, Kempf MC, Drentea P, et al. Substance use stigma and antiretroviral therapy adherence among a drug-using population Living with HIV. AIDS Patient Care STDS. 2019;33(6):282–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Richard EL, Schalkoff CA, Piscalko HM, Brook DL, Sibley AL, Lancaster KE, et al. “You are not clean until you’re not on anything“: Perceptions of medication-assisted treatment in rural Appalachia. The International journal on drug policy. 2020:102704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schalkoff CA, Richard EL, Piscalko HM, Sibley AL, Brook DL, Lancaster KE, et al. ”Now we are seeing the tides wash in“: Trauma and the Opioid Epidemic in Rural Appalachian Ohio. Subst Use Misuse. 2021;56(5):650–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Levi-Minzi MA, Surratt HL. HIV stigma among substance abusing people living with HIV/AIDS: implications for HIV treatment. AIDS Patient Care STDS. 2014;28(8):442–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heads AM, Hill MJ, Suchting R, Yammine L, Gilmore-Thomas A. Predictors of anticipated PrEP stigma among women with self-reported problematic substance use: implications for engaging women in the PrEP care continuum. Arch Sex Behav. 2021;50(7):2955–64. [DOI] [PubMed] [Google Scholar]
- 32.Basta T HIV-related stigma and knowledge among individuals living in rural Appalachian Ohio. AIDS 2010-XVIII International AIDS Conference. Vienna, Austria, 2020. [Google Scholar]
- 33.White RH, O’Rourke A, Kilkenny ME, Schneider KE, Weir BW, Grieb SM, et al. Prevalence and correlates of receptive syringe-sharing among people who inject drugs in rural Appalachia. Addiction (Abingdon, England) 2021;116(2):328–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thomas N, van de Ven K, Mulrooney KJ. The impact of rurality on opioid-related harms: A systematic review of qualitative research. International Journal of Drug Policy. 2019:102607. [DOI] [PubMed] [Google Scholar]
- 35.Allen ST, O’Rourke A, White RH, Smith KC, Weir B, Lucas GM, et al. Barriers and facilitators to PrEP use among people who inject drugs in rural Appalachia: a qualitative study. AIDS Behav. 2020;24(6):1942–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Biello KB, Bazzi AR, Mimiaga MJ, Biancarelli DL, Edeza A, Salhaney P, et al. Perspectives on HIV pre-exposure prophylaxis (PrEP) utilization and related intervention needs among people who inject drugs. Harm reduction journal. 2018;15(1):55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jackson-Best F, Edwards N. Stigma and intersectionality: a systematic review of systematic reviews across HIV/AIDS, mental illness, and physical disability. BMC Public Health. 2018;18(1):919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sereda Y, Kiriazova T, Makarenko O, Carroll JJ, Rybak N, Chybisov A, et al. Stigma and quality of co-located care for HIV-positive people in addiction treatment in Ukraine: a cross-sectional study. Journal of the International AIDS Society. 2020;23(5):e25492–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.English D, Rendina HJ, Parsons JT. The effects of intersecting stigma: a longitudinal examination of minority stress, mental health, and substance use among Black, Latino, and multiracial gay and bisexual men. Psychol Violence. 2018;8(6):669–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bowleg L The problem with the phrase women and minorities: intersectionality-an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bowleg L, Bauer G. Invited reflection:quantifying intersectionality. Psychol Women Q. 2016;40(3):337–41. [Google Scholar]
- 42.Kulesza M, Matsuda M, Ramirez JJ, Werntz AJ, Teachman BA, Lindgren KP. Towards greater understanding of addiction stigma: intersectionality with race/ethnicity and gender. Drug Alcohol Depend. 2016;169:85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sengupta S, Banks B, Jonas D, Miles MS, Smith GC. HIV interventions to reduce HIV/AIDS stigma: a systematic review. AIDS Behav. 2011;15(6):1075–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brown L, Macintyre K, Trujillo L. Interventions to reduce HIV/AIDS stigma: what have we learned? AIDS education and prevention: official publication of the International Society for AIDS Education. 2003;15(1):49–69. [DOI] [PubMed] [Google Scholar]
- 45.Mak WWS, Mo PKH, Ma GYK, Lam MYY. Meta-analysis and systematic review of studies on the effectiveness of HIV stigma reduction programs. Soc Sci Med. 1982;2017(188):30–40. [DOI] [PubMed] [Google Scholar]
- 46.Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? Journal of the International AIDS Society. 2013;16(3 Suppl 2):18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bayat AH, Mohammadi R, Moradi-Joo M, Bayani A, Ahounbar E, Higgs P, et al. HIV and drug related stigma and risk-taking behaviors among people who inject drugs: a systematic review and meta-analysis. J Addict Dis. 2020;38(1):71–83. [DOI] [PubMed] [Google Scholar]
- 48.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 49.Sallis JF, Owen N, Fisher E 2015 Ecological models of health behavior. Health behavior: Theory, research, and practice. 2015;5(43–64). [Google Scholar]
- 50.Mateu-Gelabert P, Gwadz MV, Guarino H, Sandoval M, Cleland CM, Jordan A, et al. The staying safe intervention: training people who inject drugs in strategies to avoid injection-related HCV and HIV infection. AIDS education and prevention: official publication of the International Society for AIDS Education. 2014;26(2):144–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Basta TB, Stambaugh T, Fisher CB. Efficacy of an educational intervention to increase consent for HIV testing in rural Appalachia. Ethics Behav. 2015;25(2):125–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Maskay MH, Cabral HJ, Davila JA, Whitlock Davich JA, Marcus R, Quinn EK, et al. Longitudinal stigma reduction in people living with HIV experiencing homelessness or unstable housing diagnosed with mental health or substance use disorders: an intervention study. Am J Public Health. 2018;108(S7):S546–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lewis CF, Lekas HM, Rivera A, Williams SZ, Crawford ND, Pérez-Figueroa RE, et al. Pharmacy PEP access intervention among persons who use drugs in New York City: iPEPcare study-rethinking biomedical HIV prevention strategies. AIDS Behav. 2020;24(7):2101–11. [DOI] [PubMed] [Google Scholar]
- 54.Batchelder AW, Moskowitz JT, Jain J, Cohn M, Earle MA, Carrico AW. A novel technology-enhanced internalized stigma and shame intervention for HIV-positive persons with substance use disorders. Cogn Behav Pract. 2020;27(1):55–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Herek GM, Capitanio JP, Widaman KF. HIV-related stigma and knowledge in the United States: prevalence and trends, 1991–1999. Am J Public Health. 2002;92(3):371–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Broady TR, Brener L, Vuong T, Cama E, Treloar C. Online interventions to reduce stigma towards population groups affected by blood borne viruses in Australia. Int J Drug Policy. 2021;96:103292. [DOI] [PubMed] [Google Scholar]
- 57.Go VF, Frangakis C, Le Minh N, Ha TV, Latkin CA, Sripaipan T, et al. Increased survival among HIV-infected PWID receiving a multi-level HIV risk and stigma reduction intervention: results from a randomized controlled trial. J Acquir Immune Defic Syndr. 2017;74(2):166–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sugarman J, Trumble I, Hamilton E, Sarasvita R, Dumchev K, Viet H, et al. Reported participation benefits in international HIV prevention research with people who inject drugs. Ethics & human research. 2019;41(5):28–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tofighi B, Isaacs N, Byrnes-Enoch H, Lakew R, Lee JD, Berry C, et al. Expanding treatment for opioid use disorder in publicly funded primary care clinics: exploratory evaluation of the NYC health + hospitals buprenorphine ECHO program. J Subst Abuse Treat. 2019;106:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fix RL, Letourneau EJ, Mauro PM, McCart MR, Sheidow AJ. Factors promoting and impeding HIV testing among adolescents in juvenile drug court. AIDS Care. 2019;31(2):177–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Duby Z, Fong-Jaen F, Nkosi B, Brown B, Scheibe A. ‘We must treat them like all the other people’: evaluating the integrated key populations sensitivity training programme for healthcare workers in South Africa. South Afr J HIV Med. 2019;20(1):909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gichane MW, Wechsberg WM, Ndirangu J, Browne FA, Bonner CP, Grimwood A, et al. Implementation science outcomes of a gender-focused HIV and alcohol risk-reduction intervention in usual-care settings in South Africa. Drug Alcohol Depend. 2020;215:108206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Silvia RJ A music assignment to develop pharmacy students’ empathy toward people with opioid use disorder. Am J Pharm Educ. 2020;84(4):7631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Burgess K, Parkhill G, Wiggins J, Ruth S, Stoové M. Re-Wired: treatment and peer support for men who have sex with men who use methamphetamine. Sexual health. 2018;15(2):157–9. [DOI] [PubMed] [Google Scholar]
- 65.Lunze K, Kiriazova T, Blokhina E, Bushara N, Bridden C, Gnatienko N, et al. Linking HIV-positive people in addiction care to HIV services in St Petersburg, Russia - Mixed-methods implementation study of strengths-based case management. Global public health. 2021;16(11):1711–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lemons-Lyn A, Reidy W, Myint WW, Chan KN, Abrams E, Aung ZZ, et al. Optimizing HIV Services for Key Populations in Public-Sector Clinics in Myanmar. Journal of the International Association of Providers of AIDS Care (JIAPAC). 2021;20:23259582211055933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Livingston JD, Milne T, Fang ML, Amari E. The effectiveness of interventions for reducing stigma related to substance use disorders: a systematic review. Addiction (Abingdon, England). 2012;107(1):39–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chambers LA, Rueda S, Baker DN, Wilson MG, Deutsch R, Raeifar E, et al. Stigma, HIV and health: a qualitative synthesis. BMC Public Health. 2015;15:848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Smith LR, Earnshaw VA, Copenhaver MM, Cunningham CO. Substance use stigma: reliability and validity of a theory-based scale for substance-using populations. Drug Alcohol Depend. 2016;162:34–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Brown SA Standardized measures for substance use stigma. Drug Alcohol Depend. 2011;116(1–3):137–41. [DOI] [PubMed] [Google Scholar]
- 71.Relf MVWLH, Holt L, Nyblade L, Ellis Caiola C. A review of the state of the science of HIV and stigma: context, conceptualization, measurement, interventions, gaps, and future priorities. J Assoc Nurse in AIDS Care : JANAC. 2021;32(3):392–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Stevelink S, Wu IC, Voorend CG, van Brakel WH. The psychometric assessment of internalised stigma instruments: a systematic review. Stigma, Res Action. 2012;2(2):100–18. [Google Scholar]
- 73.Mathers BM, Degenhardt L, Ali H, Wiessing L, Hickman M, Mattick RP, et al. HIV prevention, treatment, and care services for people who inject drugs: a systematic review of global, regional, and national coverage. Lancet (London, England). 2010;375(9719):1014–28. [DOI] [PubMed] [Google Scholar]
- 74.Lancaster KE, Hoffman IF, Hanscom B, Ha TV, Dumchev K, Susami H, et al. Regional differences between people who inject drugs in an HIV prevention trial integrating treatment and prevention (HPTN 074): a baseline analysis. J Int AIDS Soc. 2018;21(10):e25195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Thanh DC, Moland KM, Fylkesnes K. Persisting stigma reduces the utilisation of HIV-related care and support services in VietNam. BMC Health Serv Res. 2012;12:428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bowleg L The problem with the phrase women and minorities: intersectionality-an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Crenshaw K Mapping the margins: intersectionality, identity politics, and violence against women of color. Stanford Law Review. 1991;43(6):1241–99. [Google Scholar]
- 78.Wakefield WD, Hudley C. African American male adolescents’ preferences in responding to racil discrimination: effects of ethnic identity and situational influences. Adolescence. 2005;40(158):237. [PubMed] [Google Scholar]
- 79.Karver TS, Atkins K, Fonner VA, Rodriguez-Diaz CE, Sweat MD, Taggart T, et al. HIV-related intersectional stigma and discrimination measurement: state of the science. Am J Public Health. 2022;112(S4):S420–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Earnshaw VA, Jonathon Rendina H, Bauer GR, Bonett S, Bowleg L, Carter J, et al. Methods in HIV-related intersectional stigma research: core elements and opportunities. Am J Public Health. 2022;112(S4):S413–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hankivsky O, Reid C, Cormier R, Varcoe C, Clark N, Benoit C, et al. Exploring the promises of intersectionality for advancing women’s health research. International journal for equity in health. 2010;9:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Azim T, Bontell I, Strathdee SA. Women, drugs and HIV. The International journal on drug policy. 2015;26(01):S16–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Reback CJ, Fletcher JB. HIV prevalence, substance use, and sexual risk behaviors among transgender women recruited through outreach. AIDS Behav. 2014;18(7):1359–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Carter A, Min JE, Chau W, Lima VD, Kestler M, Pick N, et al. Gender inequities in quality of care among HIV-positive individuals initiating antiretroviral treatment in British Columbia, Canada (2000–2010). PLoS ONE. 2014;9(3):e92334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Malinowska-Sempruch K What interventions are needed for women and girls who use drugs? A global perspective. J Acquir Immune Defic Syndr. 2015;69(Suppl 2):S96–7. [DOI] [PubMed] [Google Scholar]
- 86.Hoskin RA Femmephobia: The role of anti-femininity and gender policing in LGBTQ+ people’s experiences of discrimination. Sex Roles. 2019;81(11):686–703. [Google Scholar]
- 87.Lancaster KE, Cooper HLF, Browning CR, Malvestutto CD, Bridges JFP, Young AM. Syringe service program utilization, barriers, and preferences for design in rural Appalachia: differences between men and women who inject drugs. Substance use & misuse. 2020:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.El-Bassel N Strathdee SA 2015 Women who use or inject drugs: an action agenda for women-specific, multilevel, and combination HIV prevention and research. J Acquired Immune Deficiency Syndromes. 1999;69(Suppl 2):S182–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Iversen J, Page K, Madden A, Maher L. HIV, HCV, and health-related harms among women who inject drugs: implications for prevention and treatment. J Acquir Immune Defic Syndr. 2015;69(01):S176–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


