ABSTRACT
Studies on traditional and social media have found that misinformation about vaccines has been widely spread over the last decade, negatively impacting public opinion and people’s willingness to get vaccinated. We reviewed the sentiments of Italian users to define the characteristic of anti-vax and pro-vax contents and defined the strategies to deal with the misinformation. Scopus, MEDLINE/PubMed, Google Scholar (up to page 10), and ISI Web of Knowledge databases were systematically searched. Research articles, brief reports, commentaries, and letters published between January 1, 2010 and March 30, 2022 were included in the search. No-vax or ambiguous contents in Italian mass media are not prevalent compared to neutral and pro-vax content; the communication of no-vax groups is significantly simplified, favoring the understanding of the topics by users. Events related to vaccinations are associated with news coverage by media, search engine consultations, and user reactions on social networks. In this context, the activity of no-vax groups is triggered, and misinformation and fake news spread even further. A multifactorial approach is necessary to manage online user sentiment and use mass and social media as health promotion tools.
KEYWORDS: Vaccine compliance, COVID-19, social network, web 2.0, newspaper, no-vax, VaccinarSì Network, Vaxveria, Fluad, communication, social media, Italy, vaccine hesitancy
Introduction
In 2019, the World Health Organization (WHO) listed vaccine hesitancy (VH) as a major public health threat that year.1 Today, VH is still a challenging health threat as it can compromise the effectiveness of vaccination campaigns in the general population and subgroups.2–6 Web 2.0 has allowed everyone to express themselves on everything; 4.66 billion people worldwide used the Internet in 2021, up by 316 million (7.3%) from the previous year, and 4.20 billion social media users worldwide were reported in the same year.7 In recent years, social media have become more widely accessible on various platforms, including smartphones and mobile devices, with the potential to accelerate the spread of information (true or false) and offer a means to rapidly select what is relevant to public discourse. Furthermore, it must be considered that the influence of anti-vax groups on social media, although representing a small minority of subjects, has begun to instill doubts about the benefit/risk profile of vaccination through a well-organized communication strategy, capable of spreading misinformation and fake news (reported by traditional media or new content) in a very short time.8
Moreover, the social isolation imposed on citizens due to the COVID-19 pandemic has further contributed to the increased use of digital platforms. Indeed, according to the “We are Social – Digital in 2021 Report,” Internet users in Italy exceed 50 million, and 41 million are active on social media daily.7
In this context, our study aims to systematically review Italian experiences over the past 12 years related to the approach of traditional media, social networks, and digital tools on vaccination issues. We analyzed the attitudes of Italian users to define the characteristics of anti-vax and pro-vax content and defined the strategies suggested by the scientific literature to deal with the misinformation spread in the mass media. To the best of our knowledge, this is the first study to conduct a systematic review of the literature on the Italian context, analyzing the available data from a public health perspective.
Material and methods
Scopus, MEDLINE/PubMed, Google Scholar (up to page 10), and ISI Web of Knowledge databases were systematically searched. Research articles, brief reports, commentaries, and letters published between January 1, 2010 and March 30, 2022, were included in the search. The following terms were used for the search strategy: (vaccin*) AND (social media OR newspaper OR mass media) AND (Ital*). Studies in English with full text were included. Abstracts without full text, systematic reviews, meta-analyses, studies by Italian authors not focusing on Italian topics, and all studies focusing on issues unrelated to the purpose of this review (vaccine knowledge, adverse vaccine reactions, etc.) were excluded (Figure 1). When necessary, the authors of the studies were contacted to obtain additional information. The references of all articles were reviewed to identify additional studies. The list of articles was independently screened by title and/or abstract by two reviewers who applied the predefined inclusion/exclusion criteria. Discrepancies were recorded and resolved by consensus.
Figure 1.
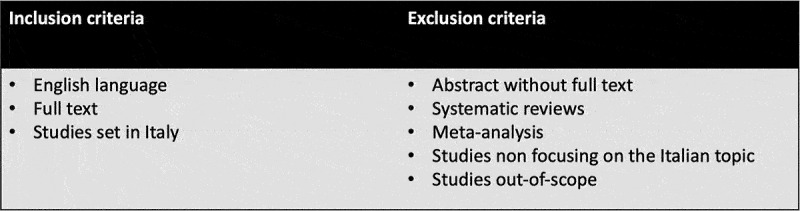
Summary of inclusion and exclusion criteria.
Identification of relevant studies
The flow-chart, constructed following the PRISMA guide9 (Figure 2), shows the article selection process. According to the aforementioned inclusion criteria, 3 articles were identified in Google Scholar, 9 in Scopus, 49 in ISI Web of Knowledge, and 37 in MEDLINE/PubMed; 16 studies were identified through references and/or web search. After the exclusion of duplicate articles in the two databases, there were 56 eligible studies. Of these, four were excluded because they evaluated the same phenomenon in more recent, comprehensive articles already included in the review, two because they did not fulfill the chosen theme, and two because the full text was unavailable. Thus, a total of 48 studies were eligible10–57 (Table 1). The remaining 208 studies did not meet the inclusion criteria.
Figure 2.
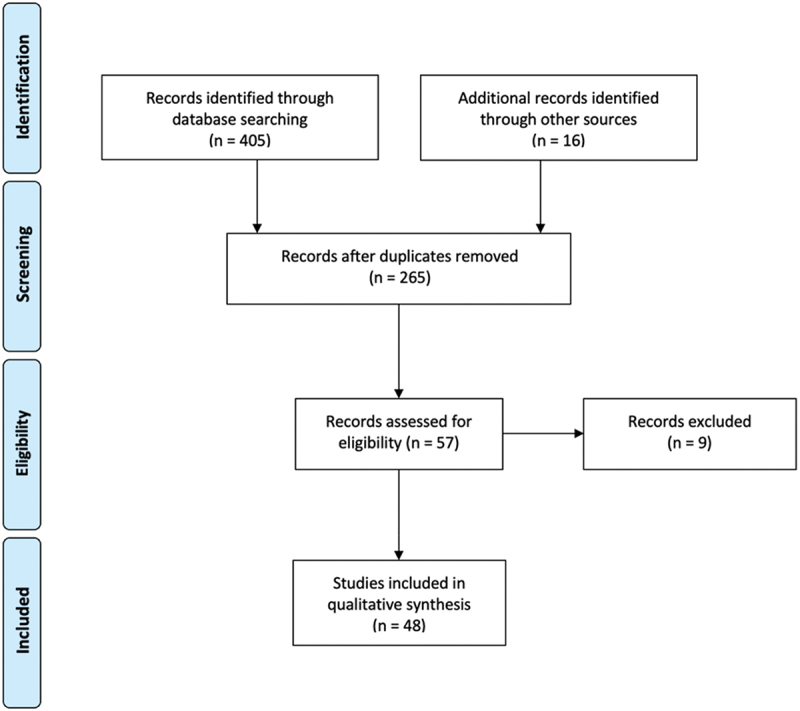
Flow-chart of the bibliographic research.
Table 1.
Characteristics of the selected studies included in systematic review.
| First Author | Year | Study design | Study period | Main topic | Vaccine investigated |
|---|---|---|---|---|---|
| Bianchi FP | 2022 | commentary | 2020 | Traditional and social media | COVID-19 |
| Bianchi FP | 2022 | descriptive study | 2018–2019 | Social media | Influenza |
| Bucchi M | 2022 | descriptive study | 2020–2021 | Traditional and social media | COVID-19 |
| Di Mauro A | 2022 | descriptive study | 2021–2022 | Social media | COVID-19 |
| Marchetti F | 2022 | descriptive study | 2020 | Social networks | Rotavirus |
| Spitale G | 2022 | descriptive study | 2021 | Telegram | COVID-19 |
| Ajovalasit S | 2021 | descriptive study | 2018 | General vaccination | |
| Arghittu A | 2021 | descriptive study | 2013–2021 | VaccinarSì Network | General vaccination |
| Arghittu A | 2021 | descriptive study | 2017–2021 | VaccinarSì Network | General vaccination |
| Bordin P | 2021 | descriptive study | 2013–2019 | VaccinarSì Network | General vaccination |
| Brandmayr F | 2021 | commentary | n.r. | Traditional and social media | General vaccination |
| Di Mauro A | 2021 | descriptive study | 2016–2017 | Pediatric vaccines | |
| Gori D | 2021 | descriptive study | 2020–2021 | General vaccination | |
| Melot B | 2021 | descriptive study | 2019 | Traditional and social media, VaccinarSì Network | General vaccination |
| Rovetta A | 2021 | descriptive study | 2016–2021 | Search engines | General vaccination |
| Vai B | 2021 | descriptive study | 2020 | Traditional and social media | COVID-19 |
| Boccalini S | 2020 | descriptive study | 2017–2020 | VaccinarSi website | General vaccination |
| Brilli Y | 2020 | descriptive study | 2014 | Traditional media | Influenza |
| Costantino C | 2020 | descriptive study | 2017 | Social media, VaccinarSì Network | General vaccination |
| Gesualdo F | 2020 | descriptive study | 2016 | General vaccination | |
| Ghezzi P | 2020 | descriptive study | n.r. | Search engines | General vaccination |
| Lovari A | 2020 | descriptive study | 2018 | Traditional and social media | General vaccination |
| Porreca A | 2020 | descriptive study | 2017–2018 | YouTube | General vaccination |
| Tavoschi L | 2020 | descriptive study | 2016–2017 | General vaccination | |
| Angioli R | 2019 | descriptive study | 2015–2016 | Social networks | HPV |
| Bianchi FP | 2019 | descriptive study | 2016–2017 | Social media | Influenza |
| Carrieri V | 2019 | letter | 2006–2016 | Social media | General vaccination |
| Costantino C | 2019 | descriptive study | 2007–2019 | Social networks | General vaccination |
| Salvador Casara BG | 2019 | descriptive study | 2018 | Search engines and social networks | General vaccination |
| Arif N | 2018 | descriptive study | 2017 | Search engines | General vaccination |
| Bonanni P | 2018 | editorial | n.r. | Traditional and social media | General vaccination |
| Costantino C | 2018 | descriptive study | 2016 | Social networks | meningococcus |
| Donzelli G | 2018 | descriptive study | 2007–2017 | YouTube | General vaccination |
| Gilardi F | 2018 | descriptive study | 2017–2018 | Social media | Influenza |
| Odone A | 2018 | descriptive study | 2007–2017 | Traditional media | General vaccination |
| Panatto D | 2018 | descriptive study | 2017 | search engines | Influenza |
| Aquino F | 2017 | descriptive study | 2010–2015 | Search engines and social networks | General vaccination |
| Covolo L | 2017 | descriptive study | 2015–2016 | YouTube | General vaccination |
| Tabacchi G | 2017 | descriptive study | 2015 | Traditional and social media, VaccinarSì Network | General vaccination |
| Biasio LR | 2016 | letter | 2016 | Traditional and social media | General vaccination |
| Fadda M | 2015 | descriptive study | 2008–2014 | Online forum | Pediatric vaccines |
| Ferro A | 2015 | descriptive study | 2013–2014 | VaccinarSì Network | General vaccination |
| Signorelli C | 2015 | letter | 2014 | Traditional and social media | Influenza |
| Tafuri S | 2015 | descriptive study | 2014 | Search engines | General vaccination |
| La Torre G | 2014 | descriptive study | 2012–2013 | General vaccination | |
| Covolo L | 2013 | descriptive study | 2010 | Search engines | Influenza |
| Trivellin V | 2011 | descriptive study | 2009 | Traditional and social media | Influenza |
| Tozzi AE | 2010 | descriptive study | 2008 | Search engines | HPV |
n.r.= not reported.
The authors reviewed all relevant studies and independently extracted data, which were put in a chart with their characteristics, to qualitatively compile the results (Table 1). Any discrepancies were resolved by consensus between the authors. The influence of mass and social media on vaccine attitudes was extracted from the entirety of available studies, and their respective outcomes were juxtaposed, with particular emphasis placed on the evidence presented across multiple included papers. Five overarching domains were delineated (traditional media, social networks, and digital platforms, Web 2.0 and social media as health promotion tools, characteristics of pro-vaccine and anti-vaccine content, and recommendations and strategies for misinformation management). These categories were elaborated based on information gleaned from the included studies.
Results
Traditional media
Odone A et al.44 retrospectively reviewed all articles published on vaccine-related topics by the most widely read Italian newspaper “Il Corriere della Sera”, considering an 11-year study period (2007–2017). A total of 635 articles were published, of which 31% were broadcast in 2016–2017. In August 2017, the Italian Government increased the number of mandatory vaccinations from 4 to 10 through Decree-Law 73; the highest number of articles was recorded in that period, followed by 2009, the year of the A H1N1 influenza pandemic. Overall, 86% of the articles retrieved had a favorable or neutral approach to immunization; there was an increase in articles having a hesitant approach in the second semester of 2017 (21%, compared to 14% over the entire study period) was reported. Lovari A et al.31 investigated politicians’ reactions to the 2017 vaccine mandatory decree; vaccines represented a subject matter with 680 media news stories that totaled 644,069 Facebook interactions, 356,101 reactions, 213,616 comments, and 74,352 shares. The effects of communication during the 2009 A H1N1 pandemic showed that the reiterated presentation of severe and fatal cases by the media generated the idea that the influenza A H1N1 virus was responsible for severe pathologies that required medical attention in the nosocomial setting; in fact, there was a 100% increase in the number of pediatric emergency room visits for influenza-like illness, but it was not associated with hospitalizations and mortality rates. Moreover, mass media communications created a disproportionate fear of immunization in the population and HCWs, who are essential to promote the vaccination campaign; therefore, another negative consequence was the low adherence to the 2009 and 2010 influenza vaccination campaigns.56
Aquino F et al.46 reported that the March 2012 Rimini Court of Justice decision (which recognized a causal link between the MMR vaccine and autism and awarded compensation for vaccine injury) received extensive coverage in the Italian mainstream media, triggering anti-vaccination activity on the Internet. Nevertheless, the verdict was overturned on appeal by the Court of Bologna in 2015, but the news did not spread more extensively in the media.
In 2014, three deaths that occurred following the administration of an adjuvanted influenza vaccine were widely reported in the media, which likely influenced the decision of the Italian Drug Agency (AIFA) to briefly suspend vaccination52 and increase VH among the population. After confirmation that the deaths were not causally related to the vaccine, the suspension was revoked, and the vaccination campaign resumed. However, vaccination coverage was much lower than in previous years, and the number of flu cases and flu-related deaths was much higher. The news about the alleged fatal adverse effects of flu vaccination has resulted in a decrease of about 2.5% in the daily vaccination count, corresponding to approximately 78 fewer vaccinations per day compared with the average daily vaccination count of the previous campaign.27
Gesualdo F et al.29 analyzed the sentiment of vaccine-related tweets posted before, during, and 8 days after the airing of two broadcasts dedicated to vaccines on Italian TV in 2016, which explored the topic from different perspectives. A high peak of tweets about vaccines was observed for both broadcasts during airing, confirming that TV shows can trigger intense social media discourse. Nevertheless, generally positive sentiment was recorded in most tweets, and a high positive-to-negative ratio was recorded for both broadcasts, just as anti-vax messages in TV broadcasts did not necessarily seem to elicit negative opinions on Twitter.
Bianchi FP et al.10 commented on the role of mass media after the suspension of two batches of the Vaxveria vaccine in Italy, subsequent to five deaths after vaccine administration (March 2020). The reaction of the already vaccinated and vaccine candidates had long-lasting consequences, as 10–20% of vaccine candidates declined vaccination with the Vaxveria vaccine. In addition to the delay in vaccination, ~200,000 doses were not administered. The authors pointed out the role of the mass media in publicizing the alleged fatal reactions (mainly without a scientific point of view on the issue), as their reports were quickly picked up, manipulated, and spread even further by social media.
Social network and digital tools
Several studies have evaluated the sentiment on vaccines among Italian Twitter users; the proportion of anti-vax content has fluctuated from 23% in 2016–201733 to 30% in 201816 to 24% in 2020.22 Regarding the temporal trend of tweets, relevant interactions showed clear peaks in correspondence with vaccine-related news and political speeches.16,22,33,36,46 The spikes were associated with a marked decrease in the neutrality rate of tweets, which continued for the next 10 days, with significant changes in pro-vax or anti-vax content, depending on the news.
Marchetti F et al.14 analyzed Italian social media users’ conversations about the rotavirus vaccine (2019–2020); a total of 2250 mentions on rotavirus were recorded, of which 60.7% were negative, 29.8% positive, and 9.4 unclassified, with Facebook representing the primary source of influence (63%). Angioli R et al., in a similar study,34 analyzed 5,347 conversations on the general topic of HPV vaccine (2015–2016), showing that conversations with negative perceptions were characterized by some peaks that could be related to particular events; most of the negative conversations (77%) came from social networks. Fadda M et al.50 evaluated the pediatric vaccination topic on three Italian online forums for 2008–2014, showing that the posted topics were slightly more negative (52.1%) than positive.
Three studies32,42,47 focused on the YouTube platform. The percentage of anti-vax content ranged from 23% to 70% during 2007–2017;42,47 two channels (Radio Autismo and Autismo Vaccini) uploaded 27% of no-vax videos. This platform also saw an increase in no-vax or pro-vax videos corresponding to vaccination-related events reported in the media.42,47 Porreca A et al.32 investigated users’ sentiment during and after the implementation of the 2017 mandatory law; vaccine-related topics in 2017 on YouTube were highly critical of their mandatory nature, but the intense vaccination campaign also promoted by HCWs and scientists in the mass media and on the web prompted the feeling to change polarity from a predominant negative opinion in 2017 (52% negative) to a positive one in 2018 (54% positive).
Various studies have evaluated search engine output; these studies showed a lack of institutional websites on the first page of Google.it and other search engines39 in 2017, with the percentage of no-vax or ambiguous websites ranging from 16% in 2008 to 48% in 201739,45,53,55,57 (based on selected keywords). Tafuri S et al.53 reported that the number of posts from non-governmental entities was higher than from institutions. However, the proportion of websites providing information on the benefits of vaccination was 66%. A 2020 study30 reported that less-used search engines had a higher percentage of negative web pages regarding vaccines than Google.it, with Virgilio.it and Arianna.it returning the highest number of negative pages. Comparing Italian search engines with those of other countries, it found that Italy shows the most anti-vax content.30,39,56 Arif N et al.39 reported that Andrew Wakefield (the progenitor of the vaccine-autism hoax) was still highly cited in Google.it in 2017; a word count found that his name recurred 361 times, more than most European countries. Google’s trend analysis confirmed that searches for vaccination-related topics showed peaks in correspondence with positive or negative news about vaccines.24,45,46
Rovetta A et al.24 focused on the COVID-19 vaccination campaign and fake news, revealing that the pandemic significantly increased the phenomenon of conspiracies and interest in them; moreover, web interest in fake news sources increased more than interest in anti-hoax services.
Web 2.0 and social media as tools for promoting health
One of the first Italian experiences of health dissemination on social networks was reported by La Torre G et al.,54 who described the Italian Alliance of vaccination strategies project; this project aimed to inform HCWs and the general population about vaccinations through Facebook. The Italian “Alleanza Vaccini” account was created in May 2012, showing a good response from users and, likewise, that links posted on Wednesdays and Fridays had the most followers.
Subsequently, in 2013, the Italian Society of Hygiene and Preventive Medicine (SItI) launched the national VaccinarSì project (www.vaccinarsi.it). This national vaccine communication website quickly involved the Ministry of Health, the National Institute of Health, and all major pediatricians’ and general practitioners’ societies in the venture, rapidly receiving the HonCode and WHO approval.40 In the site’s first six years of operation (2013–2019), there were 3,363,329 accesses to the site. There was a significant increase in visits in 2017, probably related to a large measles outbreak in Italy in January of that year. In August 2019, the portal ranked first in Google.it for the keyword “vaccinarsi” and 5th for “vaccinations”.19 However, three surveys showed that the proportion of respondents who knew about the “VaccinarSì” website ranged from 6% to 19%,23,28,48 although Costantino C et al.28 highlighted that tailored vaccination counseling interventions on the general population could increase accesses to the website. Official Twitter and Facebook accounts were launched in 2013 and 2014, respectively.51 Moreover, since 2014, the Ministry of Health has funded a multicenter project that provided for the creation of a VaccinarSì website for each of the participating Italian regions (VaccinarSì Network); Veneto was the first region to develop a portal, followed by Tuscany, Apulia, Liguria, Sicily, Lazio, Campania, Marche, Trentino Alto Adige and Sardinia; in January 2020, Sardinia also published an English-language version of the portal. These websites are dedicated to region-specific topics, including the immunization schedule, information on immunization programs, and services offered in the region.51 Two studies18,26 investigated the performance of two regional portals (Sardinia and Tuscany), showing positive web user satisfaction regarding the usefulness of published content and hundreds of questions answered by the communications task force. A 2021 study17 reported on the performance of the VaccinarSì Network during the COVID-19 pandemic; in terms of site visits, the number of sessions decreased by 6%, while the number of users remained almost unchanged. Compared with the pre-COVID-19 period, there was an 18% increase in mobile phone use/day and a 37% reduction in personal computer use. Concerning the VaccinarSì Network, all regional sites recorded an increase in metrics, with the highest values for the number of users (from +51.6% to + 498.1%). The authors explained the decrease in page views of the VaccinarSì website and the increase in access to the VaccinarSì Network by the management autonomy of the Italian regions.
Brandmayr F20 reported on the experience of Professor Roberto Burioni, who in late 2015 became actively engaged on social networks (especially Facebook) in debates about vaccine safety and mandatory vaccination; he quickly became known to the general public, started appearing on talk shows and radio programs, addressed concerns about the risks associated with vaccines on his Facebook page, and published books on the subject.
Several studies11,13,21,35,37,41,43 have reported the use of social media and/or institutional websites to promote immunization campaigns in different population subgroups (in combination with more classical strategies); even though these papers have concluded that the use of digital tools may be useful in increasing childhood, meningococcal, and influenza vaccination coverage in infants, adolescents, and HCWs, respectively, the design of the studies did not allow for causality analysis, and thus it is at least challenging to demonstrate the role of health promotion through social media in improving vaccination coverage.
Characteristic of pro-vax and anti-vax content
Positive and neutral web pages had on average longer words and sentences that reduced their readability and focused relatively more on the vaccination itself and health aspects;45,53,55 as reported by Covolo L et al.,47 positive YouTube videos were usually shorter than negative ones. Pro-vax content distinguished itself by revealing increased transparency, credibility, and privacy protection.45,47,53,55 Otherwise, non-institutional websites showed an 8.6-fold increase in belonging to the category of negative or ambiguous pages;45,53 these pages used a relatively high number of images that could improve the intelligibility of the text, as the denotative meaning of technical terms, names of major vaccine manufacturers and other registered trademarks (Big Pharma conspiracy theory), accentuated fatal risks (high usage of the word death) and words related to politics (conspiracy theories).24,29,34,45 These findings were confirmed by analyzing keywords relevant to tweets with positive sentiments (responsibility, disease, thanks, ignorance, science, medicine and save) and negative sentiments (damage, pharmaceutical, doctor, mercury, baby, drug, law, and oblige).29 Interestingly, Arif N et al.39 showed that nearly 71% of commercial websites had a negative bias toward vaccines, after searching for vaccination-related topics on search engines YouTube videos with a negative tone were more viewed, shared, and had more likes than those with a positive or neutral tone.42,47 Gori D et al.22 reported that few unique users shared the majority of tweets on vaccination and that tweets at the extremes of opinion polarization were shared much more actively, with a prevalence of attention for those with no-vax content vs. pro-vax content. Tafuri S et al.53 reported that institutions and anti-vaccine movements focused on a few specific topics and used one-dimensional communication on their websites. They chose to talk about only some specific topics, neglecting all others, producing a dichotomy of available information. In particular, anti-vaccine websites never discussed the benefits and safety of vaccines, while government websites omitted to explain possible adverse reactions after vaccine administration.
The arguments of the anti-vaxers and ambiguous content were adverse events associated with vaccines (regardless of severity), lack of trust in institutions and pharmaceutical companies, inadequate perception of a clear and present danger regarding infections, fear that vaccinations may overload the immune system, negativity around vaccines in general, logistical obstacles to obtaining vaccination, and negativity around the issue of mandatory vaccination.14,34,47,50 The reason why the side effects of vaccines play a central role in persuading against their use, while the efficacy and advantages of immunizations take a back seat, may be because reason is limited when we have to make a decision, and we tend to choose the most satisfactory solution over the optimal one.34 Furthermore, risk perception exaggerates severe but rare consequences and gives less importance to more probable but less dangerous events. Spitale G et al.15 collected data from two chat groups on Telegram in 2021 investigating the issue of the Italian green-pass, which was introduced to deal with the COVID-19 pandemic in Italy; the authors showed that the green-pass had become a proxy and catalyst for vaccine skepticism; indeed, no-vax supporters shifted their focus to the green-pass, which allowed them to advance new arguments to indirectly bring in less socially problematic arguments against vaccine use. In these groups, moderate positions coexisted with conspiracy, so opposition to the green-pass glued together these opinions and attitudes.
The most frequent sources for anti-vax content were the personal experiences of users, the media, rumors, and the experiences of relatives or friends, while pro-vax and neutral contents source were institutional references;50 nevertheless, both positions cited medical professionals, who were used mostly in pro-vax contents. Many studies have shown that women, especially younger ones, are more active in discussions about the vaccine than men and are more sensitive to conversations about adverse effects.14,17–19,26,34,50,51
Suggestions and strategies to manage misinformation
Eight studies have focused on the role of traditional media, suggesting that, especially during the COVID-19 pandemic, reporting by established news outlets must be accompanied by a strong sense of responsibility and awareness of the potential consequences of distorted or unconfirmed information. These studies have suggested that it may become routine to compare the information in the article with official scientific sources or to seek scientific advice for particularly complex topics, choosing less sensationalistic communication targeted at “clicks” and “likes.”10,24,25,27,31,49,52,56 Indeed, TV and/or radio news seems to be the primary source for collecting information on vaccination.12,25,28,48
The role of digital tools has also been questioned. Two authors suggested that search engine algorithms that index purely on “relevance” should also be designed to index on quality.30,57 Digital platforms should be motivated to stop spreading misleading information about health and science that can have strong economic and social impacts.31 During the COVID-19 pandemic, under every piece of content related to the pandemic, YouTube, Facebook, and Instagram had affixed a warning bar that offered users the opportunity to read the latest news about COVID-19 on the official website of the Ministry of Health, complete with a button to access it. Moreover, these companies banned accounts and channels that were protagonists in the spread of fake news in Italy.24 Indeed, the internet and social media are one of the most important sources of information on vaccines, even though trust in these tools is reported to be very low;12,23,25,28,48 not surprisingly, at the beginning of the pandemic, a quarter of Italian users perceived COVID-19 to be less threatening than influenza and, if a vaccine had been available, would not have vaccinated.25 In addition, many authors reported that accessibility to non-traditional media reduced children’s immunization rates, especially MMR vaccination.36,38,46 Salvador Casara BG et al.38 evidenced how users actively selected digital outputs that were in line with their opinion, as well as how exposure to online comments questioning vaccination influenced attitudes toward vaccines; this association was disrupted by exposure to pro-vax messages, but only if antivaccine alternatives were absent.
The influence of healthcare professionals is crucial to maintaining confidence in vaccination. Several studies have shown a lack of participation in online discussions by HCWs; greater online participation by these professionals would help reduce online misinformation.12,14,23,28,53 Nevertheless, during the COVID-19 pandemic, scientific experts’ public communication performance on mass media and social media was perceived as predominantly confusing by Italian consumers;12 for this reason, too, the General Practitioner probably seems to be one of the most reliable from whom to obtain information.12,23,28,48
Seven studies focused on the role of Public Health institutions, pointing out that policymakers should implement more effective infosurveillance systems and real-time tools to explore key public concerns about vaccination and intervene quickly when misinformation spreads on social media;24,29,31,42,46,50,54 indeed, analysis of web search trends and social network data could represent a proxy for VH at the population level, and thus specific communication campaigns might be implemented.46 For example, in the case of the spread of fake news on adverse events following vaccination (as happened during the Fluad and Vaxveria cases), health authorities should aim to reestablish trust in the vaccine as soon as possible with an appropriate communication campaign in traditional and mass media.10,27,52 It should also be considered that the reaction of users on social media after the dissemination of true/false news about vaccination, characterized by a negative/positive polarization of content, seemed to return to normal after 10 days;33 this trend was also confirmed by vaccination behavior during the Fluad case in 2014, which reverted to normal 10 days after the news spread.27 So, in this time span, institutional communication should provide maximum effort to disclose scientifically valid information.
Otherwise, Government institutions are asked to invest in health education and digital communication to deliver health information and raise awareness among users, especially younger ones; it seems necessary to better orient vaccine communication to mitigate the impact of VH and refusal.10,15–17,23,32,34,47,49 Marchetti F et al.14 proposed an institutional web listening service to promptly provide scientifically-validated information to hesitant individuals.
Finally, Italian politicians have a significant role in spreading information or misinformation about vaccines, either directly or by opening the door to pseudoscientific and conspiratorial content. This amplifies misinformation or partisan information on the web.16,31 Effectively, through politicians’ statements aimed at courting the no-vax vote, conspiracy and pseudomedical theories have reached the mainstream media and, arguably, a more comprehensive range of people and voters.
Discussion
From the evidence of our systematic scoping review, no-vax or ambiguous content related to the Italian mass media is not prevalent compared to neutral and pro-vax content. Despite this, it seems clear that no-vax groups are one of the leading causes of VH; a 2020 network analysis reported that although anti-vaccination clusters are numerically smaller and hold ideologically fringe opinions, they have become central in positioning within the network.58 The communication of the no-vax groups is extremely simplified, with heavy use of images and arguments that avoid scientific terms; this non-technical mode of communication promotes users’ understanding of the topics, especially those with a low level of education, and hence seems to have a greater hold on users. The anti-vax movement creates user-friendly messages, posting emotional personal stories and using direct language; health professionals do not create their content in most cases, and they use a limited number of arguments in their messages.2,59 Moreover, this content offers a wide range of potentially appealing narratives that blend topics such as safety concerns, conspiracy theories, alternative health and medicine, and even the cause and/or cure of vaccine-preventable infectious diseases.58 Further, no-vax movements can shift attention to other topics (e.g., the green-pass) to indirectly bring socially less problematic arguments against vaccine use.15 All these features allow for better understanding (of fake content) by users and greater sharing of this content. On the other hand, pro-vax content is mainly reported from institutional sources, websites are more reliable from the point of view of user security and privacy and mainly use technical and scientific terminology.
One of the most interesting pieces of evidence from our systematic scoping review is that events (true or false) related to vaccination are associated with increased mainstream media reporting, search engine consultations, and user reactions on social networks. In this context, the activity of no-vax groups is triggered, and misinformation and fake news become even more widespread. As a possible effect of this phenomenon, previous literature has observed that the struggle between pro- and anti-vaccinists, particularly on social media, leads to an increase in the number of undecided people who are more likely to cluster around anti-vaccination movements rather than science-based information.58,60 This dynamic has damaged immunization campaigns in Italy on at least three distinct occasions, as described above.10,46,52
A multifactorial approach seems necessary in order to manage the phenomenon described above. Traditional media editors need to understand that their news can impact consumers’ health choices, even considering the speed of news circulation on digital platforms. A 2019 review61 highlighted how journalistic goals include entertainment, profitability, and favorability and may clash with institutional public health objectives. Another dynamic of most Italian traditional media, especially television talk shows, is to pair the comments of scientists with the nonscientific evidence-based opinions of exponents of no-vax groups; this is a wrong interpretation of the concept of balanced information, which contributes to increased levels of hesitation in the population. Most of Italy’s mainstream media have little knowledge of the scientific method, and people with no scientific background edit news. Therefore, publishers should entrust this category of news to qualified journalists or seek advice from scientists who are experts in the field. Also, it is necessary to understand, and to make the population understand, that data based on scientific evidence are not opinions that can be debated from pseudo- scientific or a- scientific positions. The rush to click, like, and share, vital as it is for the mass media, must necessarily take a back seat when discussing public health issues.
Social network and digital platform feed algorithms mediate and influence content promotion by considering users’ preferences and attitudes. This affects the construction of social perceptions and the framing of narratives, influencing policy making, political communication, and the evolution of public debate, especially on polarizing topics, including health and vaccination.62 Another characteristic feature of online communication networks is their marked degree of homophily. Indeed, online users tend to prefer information that adheres to their worldviews, ignore dissenting information, and form polarized groups around shared narratives. The presence of these clusters formed by users homogeneously producing and broadcasting content has been called echo chambers.63 This mechanism creates a high polarization of content and users, and misinformation proliferates rapidly in this environment. To cope with the dynamics described above, some digital companies have changed their policies and guidelines to counter the spread of controversial content on vaccination and misinformation.64–67 Nonetheless, social media still represents the main battleground of Italian no-vax groups,8 probably because social companies’ algorithms select and make visible specific content, increasing polarization and partisanship, thus encouraging the spread of fake news. Therefore, further efforts need to be made by these companies to block the spread of misinformation to improve health literacy and foster public trust in vaccination.68
Scientific dissemination on social networks seems effective in counteracting misinformation and fake news; starting with Professor Burioni,20 several scientists have opened public channels to promote health education, just as various anti-hoax services are active on social media. These channels, followed by hundreds of thousands of Italian users, can be an important reference for undecided or confused users. Otherwise, the COVID-19 pandemic has highlighted how the overexposure of scientists, especially in the conventional media, has led to consumer confusion.12 We believe that the figure of the superstar scientist is not useful for health promotion; as it happened, an inaccurate declaration of these figures may be enough to fuel the attacks of no-vax groups with the consequent spread of misinformation. Besides, participation in talk shows where these personalities are opposed by individuals who promote anti-scientific theses (giving the impression that public health issues are based on opinions) is counterproductive. The presence of senior scientific figures in the mass media and social media is fundamental to disseminate the most up-to-date scientific evidence and to inform and educate the public.69 However, it would be preferable to avoid media overexposure to prevent the problems outlined above. The scientific community must address this issue with a higher willingness to also communicate clinical studies to those people who are unable to independently understand medical information; yet, reliable science must also limit the diffusion of studies that do not meet the essential criteria of methodological rigor and certainty of results, in order to reduce misinformation.70
Government and public health institutions are pivotal in dealing with misinformation and VH. There is a need to use the digital tools of the web and implement real-time infovigilance systems to continuously monitor sentiments about vaccination among Italian users;71 as reported by the European Center for Disease Control and Prevention, social media monitoring is a plausible way to capture the nature and direction of online discourse about vaccination. It could help understand how social media can influence public perceptions, to restore public trust in vaccines.72 Communication strategies must be calibrated on disclosure usable even by less educated individuals, and effective networking on digital platforms that can disseminate evidence-based information extensively. There may be a need, modeled after the Centers for Disease Control and Prevention (CDC) website, for communication aimed at the general population, with specific insights for health professionals, in order to ensure the comprehensibility of what is reported to a wide audience; in some contexts, it might be an idea to “mimic” the simplistic modes of communication of no-vax content, for example by using images and memes to popularize easily usable content73 and/or build a community of engaged influencers who support the dissemination of scientific insights.60 Moreover, a strong presence of institutional channels, especially on social media, is needed at vaccination-related events involving user reactions and the diffusion of fake news and misinformation to orient consumers on scientific positions. On the other hand, the implementation of an efficient communication network is useless unless institutional communication is improved;74 in the Fluad and Vaxveria cases,10,52 the Italian Drug Agency (AIFA) did not conduct a causality assessment in compliance with WHO recommendations75 before withdrawing vaccine batches, and the communication of these events by government institutions was inadequate; in fact, the lack of coordinated decision-making process had an impact on citizens’ trust in health authorities and their willingness to vaccinate.76 Another recent example is the introduction of the green-pass in Italy, which evidently has not been well communicated and poorly understood by Italians.77 Furthermore, massive investments in education are needed; Italy has the highest rate of functionally illiterate adults in Europe,78 as well as being ranked among the European countries with the highest levels of skepticism toward vaccinations;79 although it is not yet clear, a low level of health literacy may be associated with a higher probability of VH.80 There are no quick solutions to increase the health literacy levels of a population. However, government institutions must invest in the schooling and education of younger people to increase their knowledge of the scientific method and aspects of preventive health care.81
Particularly, targeted educational programs should be developed to address the characteristics of the Italian no-vax movement. Recent studies conducted in Italy have identified specific traits associated with the no-vax population, including limited engagement in political and cultural activities, a predominantly male and older demographic, a tendency to hold skeptical views toward science, and a political inclination toward the right-wing.82,83 Additionally, extreme behaviors within this movement have been documented in existing literature.84 Given these distinct attributes, educational initiatives should tailor their approaches to engage these specific groups effectively. Nevertheless, it is important to underscore that the Italian anti-vax movement displays notable resistance even in response to coercive measures, such as the suspension of salaries for healthcare workers who decline COVID vaccination during the initial stages of the vaccination campaign. The decision to forego vaccination despite the salary suspension has been extensively studied among a sample of nurses, revealing that the anti-vax behavior can be categorized into seven key themes: (1) job satisfaction, (2) primary sources of information about COVID-19, (3) reasons for refusing the COVID-19 vaccine, (4) attitudes of family members toward the COVID-19 vaccine, (5) prior experiences with other vaccines, (6) firm opposition to vaccination (nurses who have never been vaccinated), and (7) hesitant acceptance (nurses vaccinated with other vaccines).85 Addressing and diminishing anti-vaccination attitudes will require substantial time and concerted efforts.
Lastly, vaccinations have become a subject used by politicians to divide public opinion and gain an advantage at the polls.16,31 A study conducted in 202386 examined the potential link between far-right politics and vaccine hesitancy among 3,800 individuals in Spain. The authors suggested that far-right politicians could contribute to vaccine hesitancy. They emphasized that individuals who align with far-right parties appear receptive to their leaders’ discourse regarding vaccines. The voting pool of the no-vax and anti-scientific community should not seduce politicians. However, they should rely on scientific evidence and educate the population to make data-driven decisions.
What has been described above appears to have been amplified during the COVID-19 pandemic. Indeed, a continuous and constant flow of increased and even uncontrolled data characterized that period, defined by WHO as an overabundance of information, including false or misleading information, both online and offline, referred to as “infodemia.”87 This phenomenon could further endanger public health efforts to curb the spread and effects of the pandemic, fostering distrust in health authorities and undermining the public health response. Within this context, 132 nations worldwide have signed an official document to ensure their commitment to combat misinformation and misinformation.88 As recommended by WHO, infodemics management aims to enable good health practices through listening to community concerns, promoting understanding of risk and advice from health experts, building resilience to misinformation, and engaging and empowering communities to take positive action.87 In order to prevent future infodemics, special attention will need to be paid to increase the visibility of evidence-based knowledge generated by health organizations and academia and identify possible sources of mis/disinformation,89 as we described earlier.
To our knowledge, our study is the first to systematically review the Italian experiences on mass media and social media communication and the sentiment of Italian users toward vaccination; one of the main strengths is the long period of observation (about 12 years), which allows a very extended excursus of the communication skills and problems of the Italian media related to vaccination, as well as the dynamics of anti-vaccination groups on social media. The main limitation is that much of the knowledge reported is now dated; future studies will need to investigate the issues reported in greater depth to propose an update on what has been observed in previous years. Besides, it should be considered that the COVID-19 pandemic has caused a change in communication methods, particularly by government and public health institutions, and thus it would be interesting to evaluate this phenomenon scientifically. In addition, to our knowledge, there are no studies on next-generation social networks, such as Instagram and TikTok.
Recommendations and future perspective
Anti-vaccination movements have always existed, ever since the smallpox immunization campaign;90 this phenomenon is opposed to the actions of public health institutions, and it is difficult to imagine that it can be eliminated quickly. It is estimated that anti-vax content on digital platforms will dominate within a decade,58 considering that strong business interests often seem to be behind the leaders of anti-vax groups.39,91 Hence, addressing VH in anticipation of the desegregation of these movements is harsh. The literature highlights various approaches for addressing no-vax movements on social media. Key strategies involve transparent communication grounded in evidence, the creation of safe spaces to foster audience discussions, the cultivation of community partnerships, and the careful debunking of misinformation. Communicators should confront misinformation directly, considering its potential impact on the passive audience – those who observe content without openly engaging through comments, likes, or shares. Counterarguments should be concise and clear and avoid inadvertently amplifying the misinformation. Communicators might also find it practical to complement scientific evidence with narratives that resonate with the beliefs and values of the audience. Furthermore, organizations can bolster vaccine promotion and credibility on social media by establishing strong affiliations with groups with similar values and objectives.92
The battle against misinformation largely rests within the purview of government bodies and public health institutions. Naturally, this phenomenon extends beyond the borders of Italy, as evidenced by similar cases documented in other countries.93–97 Improved institutional communication, using social media as a thermometer of user sentiment and a tool to disseminate usable and evidence-based content, and strong education campaigns are indispensable to stem the VH phenomenon.98 We also observed, especially during the COVID-19 pandemic, how the difficulty in communicating the fundamental importance of vaccination to the population can have adverse outcomes on the immunization campaign, as observed during the Vaxveria case or the insufficient COVID-19 vaccination coverage in children aged 5–11 years. Indeed, it should be considered that the COVID-19 pandemic has been observed to increase VH toward all vaccinations.99
Our study sheds light on the intricate dynamics between misinformation and vaccine attitudes, providing a foundation for further investigations. By elucidating the mechanisms through which fake news influences public perceptions, our research contributes to developing targeted interventions and strategies to mitigate vaccine hesitancy and promote accurate health information. This advances our understanding of the issue and paves the way for more effective approaches in public health communication and policy-making. In conclusion, the issue of VH and the role of social and traditional media is extremely complex; consequently, a multifactorial approach is needed so that institutions can regain the trust of the population and thus better manage the feelings of online users and use mass media and social media as health promotion tools.
Acknowledgments
We acknowledge Mr. Nazario Brescia for the copy-editing of this paper.
Funding Statement
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors
Abbreviations
- VH:
vaccine hesitancy
- HCW:
Healthcare worker
- CDC:
Centers for Disease Control and Prevention
- WHO:
Word Health Organization
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.World Health Organization . Ten threats to global health in 2019; accessed 2022 Apr 5. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.
- 2.Wang Y, McKee M, Torbica A, Stuckler D.. Systematic literature review on the spread of health-related misinformation on social media. Social Sci Med. 2019. Nov;240:112552. doi: 10.1016/j.socscimed.2019.112552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Di Giuseppe G, Pelullo CP, Della Polla G, Montemurro MV, Napolitano F, Pavia M, Angelillo IF. Surveying willingness toward SARS-CoV-2 vaccination of healthcare workers in Italy. Expert Rev Vaccines. 2021. Jul;20(7):881–12. doi: 10.1080/14760584.2021.1922081. [DOI] [PubMed] [Google Scholar]
- 4.Bianchi FP, Vimercati L, Mansi F, De Nitto S, Stefanizzi P, Rizzo LA, Fragnelli GR, Cannone ESS, De Maria L, Larocca AMV, et al. Compliance with immunization and a biological risk assessment of health care workers as part of an occupational health surveillance program: the experience of a university hospital in southern Italy. Am J Infect Control. 2020. Apr;48(4):368–74. doi: 10.1016/j.ajic.2019.09.024. [DOI] [PubMed] [Google Scholar]
- 5.Gencer H, Özkan S, Vardar O, Serçekuş P. The effects of the COVID-19 pandemic on vaccine decisions in pregnant women. Women Birth. 2021 May 19;35(3):S1871-5192(21)00082–2. doi: 10.1016/j.wombi.2021.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aldossari KK, Alharbi MB, Alkahtani SM, Alrowaily TZ, Alshaikhi AM, Twair AA. COVID-19 vaccine hesitancy among patients with diabetes in Saudi Arabia. Diabetes Metab Syndr. 2021. Sep-Oct;15(5):102271. doi: 10.1016/j.dsx.2021.102271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.We are social . SPECIAL REPORT DIGITAL 2021; accessed 2022 Apr 8. https://wearesocial.com/uk/blog/2021/01/digital-2021-uk/.
- 8.Tafuri S, Gallone MS, Cappelli MG, Martinelli D, Prato R, Germinario C. Addressing the anti-vaccination movement and the role of HCWs. Vaccine. 2014 Aug 27;32(38):4860–5. doi: 10.1016/j.vaccine.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 9.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Clarke M, Deveraux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bianchi FP, Tafuri S. A public health perspective on the responsibility of mass media for the outcome of the anti-COVID-19 vaccination campaign: the AstraZeneca case. Ann Ig. 2022 Nov-Dec;34(6):650–5. [DOI] [PubMed] [Google Scholar]
- 11.Bianchi FP, Tafuri S, Spinelli G, Carlucci M, Migliore G, Calabrese G, Daleno A, Melpignano L, Vimercati L, Stefanizzi P. Two years of on-site influenza vaccination strategy in an Italian university hospital: main results and lessons learned. Hum Vaccin Immunother. 2022 Dec 31;18(1):1993039. doi: 10.1080/21645515.2021.1993039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bucchi M, Fattorini E, Saracino B. Public perception of COVID-19 vaccination in Italy: the role of trust and experts’ communication. Int J Public Health. 2022 Mar 16;67:1604222. doi: 10.3389/ijph.2022.1604222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Di Mauro A, Di Mauro F, De Nitto S, et al. Social media interventions strengthened COVID-19 immunization campaign. Front Pediatr. 2022 Apr 5. doi: 10.3389/fped.2022.869893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marchetti F, Verazza S, Brambilla M, Restivo V. Rotavirus and the web: analysis of online conversations in Italy during 2020. Hum Vaccin Immunother. 2022 Dec 31;18(1):2002087. doi: 10.1080/21645515.2021.2002087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spitale G, Biller-Andorno N, Germani F. Concerns around opposition to the green pass in Italy: social listening analysis by using a mixed methods approach. J Med Internet Res. 2022 Feb 16;24(2):e34385. doi: 10.2196/34385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ajovalasit S, Dorgali VM, Mazza A, d’Onofrio A, Manfredi P, Bovet A. Evidence of disorientation towards immunization on online social media after contrasting political communication on vaccines. Results from an analysis of Twitter data in Italy. PloS One. 2021 Jul 9;16(7):e0253569. doi: 10.1371/journal.pone.0253569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arghittu A, Dettori M, Dempsey E, Deiana G, Angelini C, Bechini A, Bertoni C, Boccalini S, Bonanni P, Cinquetti S, et al. Health communication in COVID-19 era: experiences from the Italian VaccinarSì Network websites. Int J Environ Res Public Health. 2021 May 25;18(11):5642. doi: 10.3390/ijerph18115642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arghittu A, Deiana G, Dettori M, Dempsey E, Masia MD, Plamieri A, Spano AL, Azara A, Castiglia P. Web-based analysis on the role of digital media in health communication: the experience of VaccinarSinSardegna Website. Acta Biomed. 2021 Oct 1;92(S6):e2021456. doi: 10.23750/abm.v92iS6.12072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bordin P, Melot B, Tralli V, Bertoni C, Moretti F, Siddu A, Baldo V, Bonanni P, Castiglia P, Majori S, et al. Six years of activity of the Italian vaccine portal “VaccinarSì”: a web traffic evaluation using google analytics. Ann Ig. 2021. Mar-Apr;33(2):109–22. doi: 10.7416/ai.2021.2417. [DOI] [PubMed] [Google Scholar]
- 20.Brandmayr F. Public epistemologies and intellectual interventions in contemporary Italy. Int J Polit Cult Soc. 2021;34(1):47–68. doi: 10.1007/s10767-019-09346-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Di Mauro A, Di Mauro F, Greco C, Giannico OV, Grosso FM, Baldassarre ME, Capozza M, Schettini F, Stefanizzi P, Laforgia N. In-hospital and web-based intervention to counteract vaccine hesitancy in very preterm infants’ families: a NICU experience. Ital J Pediatr. 2021 Sep 16;47(1):190. doi: 10.1186/s13052-021-01129-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gori D, Durazzi F, Montalti M, Di Valerio Z, Reno C, Fantini MP, Remondini D. Mis-tweeting communication: a vaccine hesitancy analysis among twitter users in Italy. Acta Biomed. 2021 Oct 5;92(S6):e2021416. doi: 10.23750/abm.v92iS6.12251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Melot B, Bordin P, Bertoni C, Tralli V, Zuccali M, Grignolio A, Majori S, Ferro A. Knowledge, attitudes and practices about vaccination in Trentino, Italy in 2019. Hum Vaccin Immunother. 2021 Jan 2;17(1):259–68. doi: 10.1080/21645515.2020.1763085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rovetta A. The impact of COVID-19 on conspiracy hypotheses and risk perception in Italy: infodemiological survey study using Google trends. JMIR Infodemiol. 2021 Aug 6;1(1):e29929. doi: 10.2196/29929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vai B, Cazzetta S, Ghiglino D, Parenti L, Saibene G, Toti M, Verga C, Wykowska A, Benedetti F. Risk perception and media in shaping protective behaviors: insights from the early phase of COVID-19 Italian outbreak. Front Psychol. 2020 Nov 5;11:563426. doi: 10.3389/fpsyg.2020.563426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boccalini S, Bonanni P, Chiesi F, Pisa GD, Furlan F, Giammarco B, Zanella B, Mandò Tacconi F, Bechini A. The experience of VaccinarSinToscana website and the role of new media in promoting vaccination. Vaccines (Basel). 2020 Nov 3;8(4):644. doi: 10.3390/vaccines8040644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brilli Y, Lucifora C, Russo A, Tonello M. Influenza vaccination behavior and media reporting of adverse events. Health Policy (New York). 2020. Dec;124(12):1403–11. doi: 10.1016/j.healthpol.2020.08.010. [DOI] [PubMed] [Google Scholar]
- 28.Costantino C, Caracci F, Brandi M, Bono SE, Ferro A, Sannasardo CE, Scarpitta F, Siddu A, Vella C, Ventura G, et al. Determinants of vaccine hesitancy and effectiveness of vaccination counseling interventions among a sample of the general population in Palermo, Italy. Hum Vaccin Immunother. 2020 Oct 2;16(10):2415–21. doi: 10.1080/21645515.2020.1728157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gesualdo F, D’Ambrosio A, Agricola E, Russo L, Campagna I, Ferretti B, Pandolfi E, Cristoforetti M, Tozzi AE, Rizzo C. How do Twitter users react to TV broadcasts dedicated to vaccines in Italy? Eur J Public Health. 2020 Jun 1;30(3):510–5. doi: 10.1093/eurpub/ckaa022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ghezzi P, Bannister PG, Casino G, Catalani A, Goldman M, Morley J, Neunez M, Prados-Bo A, Smeesters PR, Taddeo M, et al. Online information of vaccines: information quality, not only privacy, is an ethical responsibility of search engines. Front Med. 2020 Aug 11;7:400. doi: 10.3389/fmed.2020.00400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lovari A, Martino V, Righetti N. Blurred shots: investigating the information crisis around vaccination in Italy. Am Behav Sci. 2020. Jan;65(2):351–70. doi: 10.1177/0002764220910245. [DOI] [Google Scholar]
- 32.Porreca A, Scozzari F, Di Nicola M. Using text mining and sentiment analysis to analyse YouTube Italian videos concerning vaccination. BMC Public Health. 2020 Feb 19;20(1):259. doi: 10.1186/s12889-020-8342-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tavoschi L, Quattrone F, D’Andrea E, Ducange P, Vabanesi M, Marcelloni F, Lopalco PL. Twitter as a sentinel tool to monitor public opinion on vaccination: an opinion mining analysis from September 2016 to August 2017 in Italy. Hum Vaccin Immunother. 2020 May 3;16(5):1062–9. doi: 10.1080/21645515.2020.1714311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Angioli R, Casciello M, Lopez S, Plotti F, Minco LD, Frati P, Fineschi V, Panici PB, Scaletta G, Capriglione S, et al. Assessing HPV vaccination perceptions with online social media in Italy. Int J Gynecol Cancer. 2019. Mar;29(3):453–8. doi: 10.1136/ijgc-2018-000079. [DOI] [PubMed] [Google Scholar]
- 35.Vimercati L, Bianchi FP, Mansi F, Ranieri B, Stefanizzi P, De Nitto S, Tafuri S. Influenza vaccination in health-care workers: an evaluation of an on-site vaccination strategy to increase vaccination uptake in HCWs of a South Italy hospital. Hum Vaccin Immunother. 2019;15(12):2927–32. doi: 10.1080/21645515.2019.1625645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Carrieri V, Madio L, Principe F. Vaccine hesitancy and (fake) news: quasi-experimental evidence from Italy. Health Econ. 2019. Nov;28(11):1377–82. doi: 10.1002/hec.3937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Costantino C, Casuccio A, Caracci F, Bono S, Calamusa G, Ventura G, Maida CM, Vitale F, Restivo V. Impact of communicative and informative strategies on influenza vaccination adherence and absenteeism from work of health care professionals working at the university hospital of Palermo, Italy: a quasi-experimental field trial on twelve influenza seasons. Vaccines (Basel). 2019 Dec 24;8(1):5. doi: 10.3390/vaccines8010005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Salvador Casara BG, Suitner C, Bettinsoli ML. Viral suspicions: vaccine hesitancy in the web 2.0. J Exp Psychol Appl. 2019. Sep;25(3):354–71. doi: 10.1037/xap0000211. Epub 2019 Feb 28. PMID: 30816729. [DOI] [PubMed] [Google Scholar]
- 39.Arif N, Al-Jefri M, Bizzi IH, Perano GB, Goldman M, Haq I, Chua KL, Mengozzi M, Neunez M, Smith H, et al. Fake news or weak science? Visibility and characterization of antivaccine webpages returned by Google in different languages and countries. Front Immunol. 2018 Jun 5;9:1215. doi: 10.3389/fimmu.2018.01215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bonanni P. Enlarged free childhood vaccination offer in Italy proposed to curb the rise in the growing anti-vaccine message. Expert Rev Vaccines. 2018. Jan;17(2):103–5. doi: 10.1080/14760584.2018.1419069. [DOI] [PubMed] [Google Scholar]
- 41.Costantino C, Restivo V, Ventura G, D’Angelo C, Randazzo MA, Casuccio N, Palermo M, Casuccio A, Vitale F. Increased vaccination coverage among adolescents and young adults in the District of Palermo as a result of a public health strategy to counteract an ‘epidemic panic’. Int J Environ Res Public Health. 2018 May 17;15(5):1014. doi: 10.3390/ijerph15051014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Donzelli G, Palomba G, Federigi I, Aquino F, Cioni L, Verani M, Carducci A, Lopalco P. Misinformation on vaccination: a quantitative analysis of YouTube videos. Hum Vaccin Immunother. 2018 Jul 3;14(7):1654–9. doi: 10.1080/21645515.2018.1454572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gilardi F, Castelli Gattinara G, Vinci MR, Ciofi Degli Atti M, Santilli V, Brugaletta R, Santoro A, Montanaro R, Lavorato L, Raponi M, et al. Seasonal influenza vaccination in health care workers. A pre-post intervention study in an Italian paediatric hospital. Int J Environ Res Public Health. 2018 Apr 24;15(5):841. doi: 10.3390/ijerph15050841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Odone A, Tramutola V, Morgado M, Signorelli C. Immunization and media coverage in Italy: an eleven-year analysis (2007-17). Hum Vaccin Immunother. 2018;14(10):2533–6. doi: 10.1080/21645515.2018.1486156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Panatto D, Amicizia D, Arata L, Lai PL, Gasparini R. A comprehensive analysis of Italian web pages mentioning squalene-based influenza vaccine adjuvants reveals a high prevalence of misinformation. Hum Vaccin Immunother. 2018 Apr 3;14(4):969–77. doi: 10.1080/21645515.2017.1407483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aquino F, Donzelli G, De Franco E, Privitera G, Lopalco PL, Carducci A. The web and public confidence in MMR vaccination in Italy. Vaccine. 2017 Aug 16;35(35 Pt B):4494–8. doi: 10.1016/j.vaccine.2017.07.029. [DOI] [PubMed] [Google Scholar]
- 47.Covolo L, Ceretti E, Passeri C, Boletti M, Gelatti U. What arguments on vaccinations run through YouTube videos in Italy? A content analysis. Hum Vaccin Immunother. 2017 Jul 3;13(7):1693–9. doi: 10.1080/21645515.2017.1306159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tabacchi G, Costantino C, Cracchiolo M, Ferro A, Marchese V, Napoli G, Palmeri S, Raia D, Restivo V, Siddu A, et al. ESCULAPIO working group. Information sources and knowledge on vaccination in a population from southern Italy: the ESCULAPIO project. Hum Vaccin Immunother. 2017. Feb;13(2):339–45. doi: 10.1080/21645515.2017.1264733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Biasio LR, Corsello G, Costantino C, Fara GM, Giammanco G, Signorelli C, Vecchio D, Vitale F. Communication about vaccination: a shared responsibility. Hum Vaccin Immunother. 2016. Nov;12(11):2984–7. doi: 10.1080/21645515.2016.1198456. Epub 2016 Jul 26. PMID: 27458874; PMCID: PMC5137540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fadda M, Allam A, Schulz PJ. Arguments and sources on Italian online forums on childhood vaccinations: results of a content analysis. Vaccine. 2015 Dec 16;33(51):7152–9. doi: 10.1016/j.vaccine.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 51.Ferro A, Odone A, Siddu A, Colucci M, Anello P, Longone M, Marcon E, Castiglia P, Bonanni P, Signorelli C. Monitoring the web to support vaccine coverage: results of two years of the portal VaccinarSì. Epidemiol Prev. 2015. Jul-Aug;39(4 Suppl 1):88–93. [PubMed] [Google Scholar]
- 52.Signorelli C, Odone A, Conversano M, Bonanni P. Deaths after Fluad flu vaccine and the epidemic of panic in Italy. BMJ. 2015 Jan 14;350(jan14 23):h116. doi: 10.1136/bmj.h116. [DOI] [PubMed] [Google Scholar]
- 53.Tafuri S, Gallone MS, Gallone MF, Zorico I, Aiello V, Germinario C. Communication about vaccinations in Italian websites: a quantitative analysis. Hum Vaccin Immunother. 2014;10(5):1416–20. doi: 10.4161/hv.28268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.La Torre G, Miccoli S, Ricciardi W. The Italian alliance for vaccination strategies: Facebook as a learning tool for preventive medicine and public health. Hum Vaccin Immunother. 2014;10(10):2910–4. doi: 10.4161/21645515.2014.970497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Covolo L, Mascaretti S, Caruana A, Orizio G, Caimi L, Gelatti U. How has the flu virus infected the web? 2010 influenza and vaccine information available on the Internet. BMC Public Health. 2013 Jan 29;13(1):83. doi: 10.1186/1471-2458-13-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Trivellin V, Gandini V, Nespoli L. Low adherence to influenza vaccination campaigns: is the H1N1 virus pandemic to be blamed? Ital J Pediatr. 2011 Nov 10;37(1):54. doi: 10.1186/1824-7288-37-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tozzi AE, Buonuomo PS, Ciofi Degli Atti ML, Carloni E, Meloni M, Gamba F. Comparison of quality of internet pages on human papillomavirus immunization in Italian and in English. Journal Of Adolescent Health. 2010. Jan;46(1):83–9. doi: 10.1016/j.jadohealth.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 58.Johnson NF, Velásquez N, Restrepo NJ, Leahy R, Gabriel N, El Oud S, Zheng M, Manrique P, Wuchty S, Lupu Y. The online competition between pro- and anti-vaccination views. Nature. 2020. Jun;582(7811):230–3. doi: 10.1038/s41586-020-2281-1. [DOI] [PubMed] [Google Scholar]
- 59.Wawrzuta D, Jaworski M, Gotlib J, Panczyk M. Characteristics of antivaccine messages on social media: systematic review. J Med Internet Res. 2021 Jun 4;23(6):e24564. doi: 10.2196/24564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Germani F, Biller-Andorno N, Lavorgna L. The anti-vaccination infodemic on social media: a behavioral analysis. PloS One. 2021 Mar 3;16(3):e0247642. doi: 10.1371/journal.pone.0247642. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 61.Catalan-Matamoros D, Peñafiel-Saiz C. How is communication of vaccines in traditional media: a systematic review. Perspect Public Health. 2019. Jan;139(1):34–43. doi: 10.1177/1757913918780142. [DOI] [PubMed] [Google Scholar]
- 62.Cinelli M, De Francisci Morales G, Galeazzi A, Quattrociocchi W, Starnini M. The echo chamber effect on social media. Proc Natl Acad Sci USA. 2021 Mar 2;118(9):e2023301118. doi: 10.1073/pnas.2023301118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cota W, Ferreira SC, Pastor-Satorras R, et al. Quantifying echo chamber effects in information spreading over political communication networks. Epj Data Sci. 2019. 8:35. doi: 10.1140/epjds/s13688-019-0213-9. [DOI] [Google Scholar]
- 64.Google . How Google fights disinformation; accessed 2022 Apr 12. https://kstatic.googleusercontent.com/files/388aa7d18189665e5f5579aef18e181c2d4283fb7b0d4691689dfd1bf92f7ac2ea6816e09c02eb98d5501b8e5705ead65af653cdf94071c47361821e362da55b.
- 65.Facebook . Taking action against misinformation across our apps; accessed 2022 Apr 12. https://www.facebook.com/combating-misinfo.
- 66.Instagram . Combatting misinformation on instagram; accessed 2022 Apr 12. https://about.instagram.com/blog/announcements/combatting-misinformation-on-instagram.
- 67.Twitter . Introducing birdwatch, a community-based approach to misinformation; accessed 2022 Apr 13. https://blog.twitter.com/en_us/topics/product/2021/introducing-birdwatch-a-community-based-approach-to-misinformation.
- 68.Puri N, Coomes EA, Haghbayan H, Gunaratne K. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Hum Vaccin Immunother. 2020 Nov 1;16(11):2586–93. doi: 10.1080/21645515.2020.1780846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fontaine G, Maheu-Cadotte MA, Lavallée A, Mailhot T, Rouleau G, Bouix-Picasso J, Bourbonnais A. Communicating science in the digital and social media ecosystem: scoping review and typology of strategies used by health scientists. JMIR Public Health Surveill. 2019 Sep 3;5(3):e14447. doi: 10.2196/14447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Signorini L, Ceruso FM, Aiello E, Zullo MJ, De Vito D. Vaccine efficacy denial: a growing concern affecting modern science, and impacting public health. Endocr Metab Immune Disord Drug Targets. 2022 Mar 18;22(9):935–43. doi: 10.2174/1871530322666220318092909. [DOI] [PubMed] [Google Scholar]
- 71.Karafillakis E, Martin S, Simas C, Olsson K, Takacs J, Dada S, Larson HJ. Methods for social media monitoring related to vaccination: systematic scoping review. JMIR Public Health Surveill. 2021 Feb 8;7(2):e17149. doi: 10.2196/17149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.ECDC . Systematic scoping review on social media monitoring methods and interventions relating to vaccine hesitancy; accessed 2022 Apr 10. https://www.ecdc.europa.eu/sites/default/files/documents/vaccine-hesitancy-systematic-scoping-review-social-media.pdf.
- 73.Headley SA, Jones T, Kanekar A, Vogelzang J. Using memes to increase health literacy in vulnerable populations. Am J Health Educ. 2022;53(1):11–15. doi: 10.1080/19325037.2021.2001777. [DOI] [Google Scholar]
- 74.Attwell K, Harper T, Rizzi M, Taylor J, Casigliani V, Quattrone F, Lopalco P. Inaction, under-reaction action and incapacity: communication breakdown in Italy’s vaccination governance. Policy Sci. 2021. Jun;15(3):1–19. doi: 10.1007/s11077-021-09427-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tafuri S, Gallone MS, Calabrese G, Germinario C. Adverse events following immunization: is this time for the use of WHO causality assessment? Expert Rev Vaccines. 2015. May;14(5):625–7. doi: 10.1586/14760584.2015.1029460. [DOI] [PubMed] [Google Scholar]
- 76.Barello S, Palamenghi L, Graffigna G. Public reaction towards the potential side effects of a COVID-19 vaccine: an Italian cross-sectional study. Vaccines (Basel). 2022 Mar 11;10(3):429. doi: 10.3390/vaccines10030429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Stefanizzi P, Bianchi FP, Brescia N, Ferorelli D, Tafuri S. Vaccination strategies between compulsion and incentives. The Italian green pass experience. Expert Rev Vaccines. 2022. Apr;21(4):423–5. doi: 10.1080/14760584.2022.2023012. [DOI] [PubMed] [Google Scholar]
- 78.Organisation For Economic Co-operation and Development (OECD) . Skills matter: further results from the survey of adult skills. OECD skills studies. Paris: OECD Publishing; 2016. accessed 2022 Apr 2. https://www.oecd-ilibrary.org/docserver/9789264258051-en.pdf?expires=1616323644&id=id&accname=guest&checksum=F8FC011F7EFA1DBCC763319F255BF85B. [Google Scholar]
- 79.Larson HJ, de Figueiredo A, Xiahong Z, Schulz WS, Verger P, Johnston IG, Cook AR, Jones NS. The state of vaccine confidence 2016: global insights through a 67-country survey. EBioMedicine. 2016. Oct;12:295–301. doi: 10.1016/j.ebiom.2016.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lorini C, Santomauro F, Donzellini M, Capecchi L, Bechini A, Boccalini S, Bonanni P, Bonaccorsi G. Health literacy and vaccination: a systematic review. Hum Vaccin Immunother. 2018 Feb 1;14(2):478–88. doi: 10.1080/21645515.2017.1392423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Viola C, Toma P, Manta F, Benvenuto M. The more you know, the better you act? Institutional communication in covid-19 crisis management. Technol Forecast Soc Change. 2021. Sep;170:120929. doi: 10.1016/j.techfore.2021.120929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cadeddu C, Daugbjerg S, Ricciardi W, Rosano A. Beliefs towards vaccination and trust in the scientific community in Italy. Vaccine. 2020 Sep 29;38(42):6609–17. doi: 10.1016/j.vaccine.2020.07.076. [DOI] [PubMed] [Google Scholar]
- 83.Crescenzi-Lanna L, Valente R, Cataldi S, Martire F. Predictors of young people’s anti-vaccine attitudes in the context of the COVID-19 pandemic. Public Underst Sci. 2023 Jun 28;9636625231179830. doi: 10.1177/09636625231179830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sablone S, Spagnolo L, Macorano E, Ciavarella MC, Pascale N, Strisciullo G, Introna F, Di Fazio A. “Freedom and dignity are worth more than life”: the dramatic suicide of an anti-vax man. Healthcare (Basel). 2022 Oct 28;10(11):2141. doi: 10.3390/healthcare10112141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Picelli S, Danielis M, Zanotti R. Better to be unpaid than COVID-19 vaccinated! A qualitative study on Italian nurses suspended from work without salary. Vaccines (Basel). 2023 Jul 14;11(7):1239. doi: 10.3390/vaccines11071239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Serrano-Alarcón M, Wang Y, Kentikelenis A, Mckee M, Stuckler D. The far-right and anti-vaccine attitudes: lessons from Spain’s mass COVID-19 vaccine roll-out. Eur J Public Health. 2023 Apr 1;33(2):215–21. doi: 10.1093/eurpub/ckac173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.WHO . Infodemic; accessed 2022 Apr 10. https://www.who.int/health-topics/infodemic#tab=tab_1.
- 88.ONU . Cross-regional statement on “infodemic” in the context of COVID-19; accessed 2022 Apr 7. https://onu.delegfrance.org/IMG/pdf/cross-regional_statement_on_infodemic_final_with_all_endorsements.pdf.
- 89.Alvarez-Galvez J, Suarez-Lledo V, Rojas-Garcia A. Determinants of infodemics during Disease outbreaks: a systematic review. Front Public Health. 2021 Mar 29;9:603603. doi: 10.3389/fpubh.2021.603603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Salmon DA, Teret SP, MacIntyre CR, Salisbury D, Burgess MA, Halsey NA. Compulsory vaccination and conscientious or philosophical exemptions: past, present, and future. Lancet. 2006 Feb 4;367(9508):436–42. doi: 10.1016/S0140-6736(06)68144-0. [DOI] [PubMed] [Google Scholar]
- 91.Mønsted B, Lehmann S. Characterizing polarization in online vaccine discourse-A large-scale study. PloS One. 2022 Feb 9;17(2):e0263746. doi: 10.1371/journal.pone.0263746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Steffens MS, Dunn AG, Wiley KE, Leask J. How organisations promoting vaccination respond to misinformation on social media: a qualitative investigation. BMC Public Health. 2019 Oct 23;19(1):1348. doi: 10.1186/s12889-019-7659-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Olijo II. Nigerian media and the global race towards developing a COVID-19 vaccine: do media reports promote contributions from African countries? Ianna J Interdiscip Stud. 2020;2(1):Regular issue. [Google Scholar]
- 94.Odii A, Ngwu MO, Aniakor MC, Owelle IC, Aniagboso MC, Uzuanwu OW. Effect of COVID-19 lockdown on poor urban households in Nigeria. Where do we go from here? Ianna J Interdiscip Stud. 2020;2(1):Regular issue. [Google Scholar]
- 95.Ahmed S, Rasul ME, Cho J. Social media news use induces COVID-19 vaccine hesitancy through skepticism regarding its efficacy: a longitudinal study from the United States. Front Psychol. 2022 Jun 10;13:900386. doi: 10.3389/fpsyg.2022.900386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Van Nguyen D, Nguyen PH. Social media and COVID-19 vaccination hesitancy: mediating role of the COVID-19 vaccine perception. Heliyon. 2022 Sep 13;8(9):e10575. doi: 10.1016/j.heliyon.2022.e10575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bar-Lev S, Reichman S, Barnett-Itzhaki Z. Prediction of vaccine hesitancy based on social media traffic among Israeli parents using machine learning strategies. Isr J Health Policy Res. 2021 Aug 23;10(1):49. doi: 10.1186/s13584-021-00486-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Agujiobi-Odoh N, Joseph IV, Blessing CO, Amaechi C, Muoh O, Nwokolo P, Celestine GV. Rethinking the frontiers of vaccine acceptance: impact of visual messages in promoting the actual intake of COVID-19 vaccines among vulnerable populations. Human Vaccines & Immunotherapeutics. 2023 Dec 31;19(1):2163811. doi: 10.1080/21645515.2022.2163811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.He K, Mack WJ, Neely M, Lewis L, Anand V. Parental perspectives on immunizations: impact of the COVID-19 pandemic on childhood vaccine hesitancy. J Community Health. 2022. Feb;47(1):39–52. doi: 10.1007/s10900-021-01017-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


