Abstract
Background
Recent advances in the management of inflammatory bowel disease (IBD) striving for new treatment targets may have decreased rates of hospitalization for flares. We compared all-cause, IBD-related, and non-IBD-related hospitalizations while accounting for the rising prevalence of IBD.
Methods
Population-based, administrative health care databases identified all individuals living with IBD in Alberta between fiscal year 2002 and 2018. Hospitalization rates (all-cause, IBD-related, and non-IBD-related) were calculated using the prevalent Alberta IBD population. Hospitalizations were stratified by disease type, age, sex, and metropolitan status. Data were age and sex standardized to the 2019 Canadian population. Log-linear models calculated Average Annual Percentage Change (AAPC) in hospitalization rates with associated 95% confidence intervals (CIs).
Results
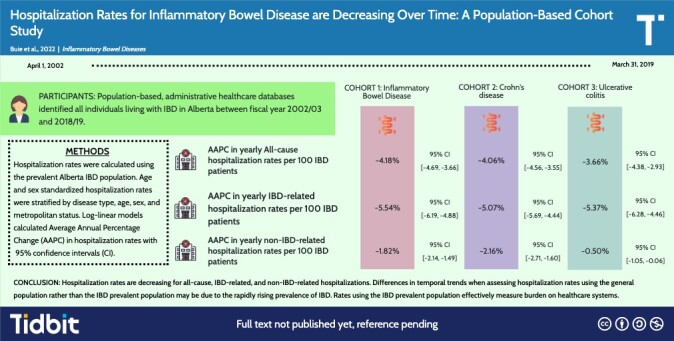
From 2002-2003 to 2018-2019, all-cause hospitalization rates decreased from 36.57 to 16.72 per 100 IBD patients (AAPC, −4.18%; 95% CI, −4.69 to −3.66). Inflammatory bowel disease–related hospitalization rate decreased from 26.44 to 9.24 per 100 IBD patients (AAPC, −5.54%; 95% CI, −6.19 to −4.88). Non-IBD-related hospitalization rate decreased from 10.13 to 7.48 per 100 IBD patients (AAPC, −1.82%; 95% CI, −2.14 to −1.49). Those over 80 years old had the greatest all-cause and non-IBD-related hospitalization rates. Temporal trends showing decreasing hospitalization rates were observed across age, sex, IBD type, and metropolitan status.
Conclusions
Hospitalization rates are decreasing for all-cause, IBD-related, and non-IBD-related hospitalizations. Over the past 20 years, the care of IBD has transitioned from hospital-based care to ambulatory-centric IBD management.
Keywords: inflammatory bowel disease, Crohn’s disease, ulcerative colitis, hospitalization rates, epidemiology
Graphical Abstract
Key Messages.
What is already known?
Advances in clinical management of inflammatory bowel disease over the past decade have transitioned care from the inpatient to outpatient setting.
What is new here?
We contrast methodological differences in assessing temporal trends in hospitalization rates.
How can this study help patient care?
Understanding temporal trends in hospitalization rates is necessary for understanding the future needs and rising costs of IBD on health care systems.
Introduction
Inflammatory bowel disease (IBD) and its subtypes Crohn’s disease (CD) and ulcerative colitis (UC) are incurable chronic diseases with low mortality, and the majority of new diagnoses are made in adolescence and early adulthood.1 The number of people living with IBD is increasing over time. The prevalence of IBD in Canada increased from 0.51% in 2008 to 0.7% in 2018 and is expected to increase to 1% by 2030.2 Moreover, those 65 years or older with IBD are the fastest growing prevalent group due to long-standing disease, as well as new IBD diagnoses.3
Admissions to hospital due to an IBD flare may be decreasing due to the advent of new therapeutic options.4,5 However, a systematic review and meta-analysis of hospitalizations rates among those with IBD from 2000 to 2018 indicated that hospitalization rates were stable for persons hospitalized for IBD-related causes and increasing for non-IBD-related admissions.4 Comorbid conditions that occur more frequently in the aging IBD population may ultimately increase the occurrence of all-cause hospitalizations.3
In a systematic review,4 the vast majority of population-based studies assessed IBD hospitalization rates using the general population as the denominator, which may have influenced the interpretation of temporal trends because the number of people living with IBD has risen faster than the overall population. Accurately assessing historical temporal trends of hospitalization rates and investigating non-IBD-related admissions are essential for predicting the care needs associated with IBD and provide valuable information to shape health care policy and clinical practice to meet future demands.
Therefore, the aim of this study was to define temporal trends of IBD hospitalization rates among the prevalent IBD population of Alberta, Canada, between fiscal year [FY] 2002 and 2018. Moreover, we describe hospitalization rates among individuals living with IBD per number of people in the prevalent population and per number of people in the general population to assess the potential for misinterpretation of temporal trends.
Methods
Data Sources
Population-based administrative health care databases covering 99% of the Alberta population (4.3 million people in fiscal year [FY] 2018-2019) was used to identify the prevalent population of people with IBD from fiscal year 2002-2003 to 2018-2019 (April 1 to March 31).6,7 The databases used include the Discharge Abstract Database (DAD), National Ambulatory Care Reporting System (NACRS)/Alberta ambulatory care reporting system (AACRS), practitioner claims, and the Provincial Registry. Discharge Abstract Database includes data from acute care facilities (ie, hospitals) on acute inpatient admissions such as patient demographics, date of admission, procedures performed, diagnoses, and discharge or transfer to another institution. The AACRS/NACRS includes day procedures (colonoscopy), same-day surgery, and emergency department visits. practitioner claims include patient interactions with physicians including specialists such as gastroenterologists. The provincial registry provides the location of the individual in 1 of the 5 health zones and other patient demographics (eg, age and sex). Statistics Canada provides age and sex population estimates of Canada and Alberta.8 Alberta Health Services Analytics has data available from April 1, 2002, onwards. The data included in the analysis spans from April 1, 2002, to March 31, 2019.
Study Population
The Alberta IBD Surveillance Cohort is a previously validated population-based cohort of prevalent IBD patients living in Alberta between fiscal year 2002-2003 to 2018-2019.9 Individuals with IBD were identified using admissions/claims from DAD, AACRS/NACRS, and practitioner claims. These databases use diagnostic codes from the International Classification of Diseases, ninth (ICD-9) or tenth (ICD-10) editions. Coding algorithms to identify patients with CD (ICD-9 555.x, ICD-10 K50.x) or UC (ICD-9 556.x, ICD-10 K51.x) were used and have previously been validated in Alberta to maximize specificity and the positive predictive value.10 Individuals with IBD were identified if they had 2 hospitalizations from DAD, four claims from practitioner claims, or 2 medical contacts from AACRS/NACRS within 2 years. The algorithm has a sensitivity of 78.0%, a specificity of 99.8%, a PPV of 97.2%, and a negative predictive value of 98.0%.10 The provincial registry identifies when an individual is registered or removed from the Alberta Health Care Insurance Plan (AHCIP). It was used to ensure that individuals were only included in the annual prevalent cohort as long as they were registered in the AHCIP and therefore assumed to be a resident of AB. Furthermore, CD, UC, and IBD-unclassified (IBD-U) diagnoses are differentiated by the validated algorithm using the following scoring system: −1 for any CD diagnostic code, and +1 for a UC diagnostic code.10 Those with the assigned number of points equal to or between −2 and +2 were defined as IBD-U.10 Those defined as IBD-U have an accurate diagnosis of IBD but the scoring algorithm is unable to differentiate between CD and UC. This scoring system has a specificity >99% for both CD and UC, and a sensitivity of 93.5% for CD and 86.3% for UC.10 The cohort created by the validated algorithm was used to analyze the prevalence of IBD.
Data Collection
The electronic patient records for all individuals with IBD in the Alberta IBD Surveillance Cohort was queried for IBD subtype, clinic attendance, hospital admission(s), and demographic data. Data were analyzed annually with patient age calculated as (year of analysis) − (year of birth).
Outcomes
IBD hospitalizations were identified using admission records in the DAD. All admissions for all individuals with a confirmed diagnosis of IBD from April 1, 2002 to March 31, 2019 were obtained. An individual with IBD admitted to hospital for at least 24 hours for any reason were captured as a hospitalization. Individuals sent to and returned from another facility in a single day for testing or a procedure, transferred from one hospital to another, and/or discharged home and re-admitted within 24 hours were counted as a single episode of hospitalization; this way, patients with multiple hospitalizations to treat the same health issue are not counted as independent events, which would inflate the hospitalization rate. Hospitalizations spanning less than 24 hours were excluded from our analysis to remove elective day-case attendance (eg, biologic infusion, endoscopy).
All-cause hospitalizations were defined as all admissions to hospital, regardless of the indication. All cause hospitalizations were then stratified into 2 mutually exclusive groups: (1) IBD-related hospitalizations that include all admissions in which an IBD diagnostic code (CD: ICD-9 555.x, ICD-10 K50.x; UC: ICD-9 556.x, ICD-10 K51.x) or an IBD-related symptom, complication, or extraintestinal manifestation was the most responsible, comorbid, or transfer diagnosis (Supplementary Table 1, page 1); and (2) non-IBD-related hospitalizations that were admissions not due directly to IBD or a complication or comorbidity of IBD. Coding algorithm for IBD-related hospitalizations were conducted via consensus by the Canadian Gastro-Intestinal Epidemiology Consortium (CanGIEC).11–14 The frequency of diagnostic codes not captured by our IBD-related definition labelled as a most responsible diagnosis were tabulated across 5 age groups (≤17, 18-39, 40-59, 60-79, and ≥ 80 years) to confirm that these admissions were not IBD-related.
Stratification Variables
Inflammatory bowel disease hospitalization rates were further stratified by disease subtype, age group, sex, and metropolitan status. Disease subtype (CD, UC, and IBD-U) annual hospitalization rates were calculated using the appropriate prevalent IBD subtype population as the denominator. Age was based on the age at hospitalization and stratified by the following age groups: younger than 18 years, 18 to 39 years, 40 to 59, 60 to 79, and older than 80 years. Sex was stratified by classification of either male or female. Metropolitan vs nonmetropolitan was defined based on the provincial registry; which reports based on the health zones of Alberta (Calgary, Edmonton, Central, North, and South).15 Those in the Calgary or Edmonton health zones were defined as living in a metropolitan city, whereas those in the Central, North, and South health zones were defined as living in a nonmetropolitan region.
Data Analysis
We used 2 denominators to calculate hospitalization rates: (1) yearly number of prevalent IBD, CD, and UC cases in Alberta during the matching fiscal year (April 1 to March 31); and (2) the general population reported by Statistics Canada used to calculate annual hospitalization rates.6 The latter was chosen because a majority of prior hospitalization rate studies in IBD were published using the general population as the denominator, and thus reporting our data likewise allows comparison of our results to other regions. Crude hospitalization rates using the prevalent IBD population were reported as number of cases per 100 persons with IBD, and rates using the general population denominator were reported as number of hospitalizations per 100,000 persons. The former provides a more accurate representation of burden because only those with IBD at risk of hospitalization are included in the denominator. Crude rates were age- and sex-standardized to the 2018 general Canadian population using the 5 age groups previously described to maximize comparability to other Canadian studies.
Data and methods were reported according to the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) statement.16 In our primary analysis, we analyzed the annual all-cause, IBD-related, and non-IBD-related hospitalization rates per 100 persons using the prevalence of the Alberta IBD population as the denominator and stratified by disease subtype, age, sex, and metropolitan status. Secondarily, we described the yearly all-cause, IBD-related, and non-IBD-related hospitalization rates per 100,000 person-years using the general population of Alberta as the denominator and stratified by disease type, age, sex, and metropolitan status.
Temporal analysis was performed in Stata v16 (College Station, TX) using log linear models; Poisson regression, or negative binomial regression if the data displayed overdispersion. Our regression model was used to calculate Average Annual Percentage Change (AAPC) and associated 95% confidence intervals (CIs) of all-cause, IBD-related, and non-IBD-related hospitalization rates for each disease subtype, age group, sex, and metropolitan status—with both denominators. The AAPCs were calculated as 100% × [1 - 100eβ] with 95% CI, whereby both CIs are <0 are significantly decreasing, cross zero stable, and >0 significantly increasing. The AAPCs for a given stratification variable were assessed for effect measure modification by independently treating a covariate (ie, disease type, age group, sex, metropolitan status) as an interaction term in the generalized linear model. A 1- and 3-year washout period was performed to see if trends differed; this is reported in Supplementary Table 2 and 3. Data visualization was done using Rstudio version 4.0.3, with the ggplot217 package.
Ethics approval was obtained from the Conjoint Research Ethics Board at the University of Calgary (REB21-0398).
Results
The 37,413 identified patients with IBD accounted for 75,388 all-cause IBD hospitalizations from FY 2002-2003 to 2018-2019 (44,284 among those with CD; 22,860, UC; and 8,244, IBD-U). Of all the all-cause IBD hospitalizations, 43,954 were categorized as being IBD-related (27,791 among those with CD; 12,825, UC; and 3,338, IBD-U), and 31,434 were categorized as being non-IBD-related (16,493 among those with CD; 10,035, UC; and 4,906, IBD-unclassified).
All-cause Hospitalizations
When the prevalent IBD population was used as the denominator, age- and sex-standardized all-cause hospitalization rates decreased from 36.57 (95% CI, 35.37-37.77) to 16.72 (95% CI, 16.28-17.17) hospitalizations per 100 IBD patients (AAPC, −4.18%; 95% CI, −4.69 to −3.66; Table 1; Supplementary Table 4, page 7). In contrast, the age- and sex-standardized all-cause IBD hospitalization rate increased from 110.65 (95% CI, 106.96-114.33) to 142.18 (95% CI, 138.61-145.74) hospitalizations per 100,000 total Alberta population from 2002 to 2018 (AAPC, 1.56%; 95% CI, 1.32-1.80; Table 1, Supplementary Table 4, Page 7). The disease-specific age- and sex-standardized all-cause IBD hospitalization rates decreased from 40.44 (95% CI, 38.80-42.08) to 18.41 (95% CI, 17.74-19.08) CD hospitalizations per 100 CD patients (AAPC = −4.06%; 95% CI, −4.56 to −3.66) and from 30.83 (95% CI, 28.91-32.76) to 15.56 (95% CI, 14.87-16.26) UC hospitalizations per 100 UC patients (AAPC = −3.66%; 95% CI, −4.38 to −2.93; Supplementary Table 5, page 8; Table 1).
Table 1.
Average Annual Percentage Change (AAPC) in IBD Hospitalization rates (all-cause, IBD-related, and non-IBD-related hospitalizations) from FY 2002 to 2018 with 95% confidence intervals (CI) stratified by disease type, age group, sex, and metropolitan status.a
| Stratification variable |
Diagnosis Type | |||||
|---|---|---|---|---|---|---|
| All-Cause | IBD-related | Non-IBD-related | ||||
| AAPC (95% CI) Relative to IBD Prevalent Population | AAPC (95% CI) Relative to General Population | AAPC (95% CI) Relative to IBD Prevalent Population | AAPC (95% CI) Relative to General Population | AAPC (95% CI) Relative to IBD Prevalent Population | AAPC (95% CI) Relative to General Population | |
| IBD | −4.18 (−4.69, −3.66) | 1.56 (1.32, 1.80) | −5.54 (−6.19, −4.88) | −0.27 (−0.53, −0.01) | −1.82 (−2.14, −1.49) | 4.15 (3.48, 4.81) |
| CD | −4.06 (−4.56, −3.55) | 0.42 (0.11, 0.72)b | −5.07 (−5.69, −4.44) | −1.08 (−1.43, −0.73)b | −2.16 (−2.71, −1.60)b | 2.87 (2.30, 3.44)b |
| UC | −3.66 (−4.38, −2.93) | 3.29 (2.94, 3.63)b | −5.37 (−6.28, −4.46) | 1.24 (0.75, 1.73)b | −0.50 (−1.05, −0.06)b | 5.98 (5.11, 6.86)b |
| <18 | −5.46 (−6.67, −4.23) | −3.21 (−4.40, −2.01) | −6.02 (−7.19, −4.85) | −3.77 (−4.97, −2.57) | −2.79 (−4.75, −0.80) | −0.53 (−2.51, 1.48) |
| 18-39 | −4.97 (−5.60, −4.33) | −2.12 (−2.48, −1.76) | −6.24 (−6.98, −5.50) | −3.36 (−3.80, −2.92) | −2.11 (−2.59, −1.63) | 0.47 (−0.09, 1.03) |
| 40-59 | −3.41 (−3.84, −2.97)c | 1.17 (0.76, 1.59)c | −4.89 (−5.41, −4.37) | −0.35 (−0.76, 0.06)c | −0.70 (−1.13, −0.27) | 3.86 (3.14, 4.59)c |
| 60-79 | −3.33 (−3.82, −2.84)c | 3.44 (2.97, 3.91)c | −4.53 (−5.36, −3.69)d | 2.28 (1.69, 2.89)c | −2.18 (−2.59, −1.77) | 4.50 (3.81, 5.20)c |
| 80+ | −2.77 (−3.61, −1.92)c | 6.60 (5.59, 7.63)c | −4.99 (−6.33, −3.63) | 4.44 (3.40, 5.48)c | −1.33 (−2.18, −0.47) | 8.22 (6.70, 9.75)c |
| Female | −4.07 (−4.63, −3.50) | 1.66 (1.33, 1.99) | −5.70 (−6.45, −4.95) | −0.39 (−0.66, −0.12) | −1.58 (−1.99, −1.16) | 4.34 (3.57, 5.12) |
| Male | −4.28 (−4.84, −3.72) | 1.43 (1.13, 1.73) | −5.36 (−6.06, −4.65) | −0.13 (−0.50, −0.24) | −2.12 (−2.57, −1.67) | 3.82 (3.13, 4.51) |
| Metropolitan | −3.36 (−3.82, −2.90)e | 2.35 (2.09, 2.61)e | −4.67 (−5.19, −4.14)e | −0.56 (−0.25, −0.86)e | −1.04 (−1.51, −0.57)e | 4.92 (4.37, 5.47)e |
| Nonmetropolitan | −5.47 (−6.20, −4.75)e | 0.27 (−0.05, 0.59)e | −6.96 (−8.00, −5.92)e | −1.66 (−2.02, −1.29)e | −3.04 (−3.49, −2.59)e | 2.86 (1.92, 3.81)e |
aAAPCs are calculated using both the IBD-specific prevalent population (all IBD, CD, or UC) and the total Alberta population denominators, respectively. (Green, significantly decreasing; red, significantly increasing; yellow, stable).
bAAPC trends comparing UC to CD show a significant effect measure modifier (P < .001).
cAAPC trends comparing age group to the referent age group (<18) show a significant effect measure modifier (P < .001).
dAAPC trends comparing age group to the referent age group (<18) show a significant effect measure modifier (p=0.04).
eAAPC trends comparing Metropolitan to Non-metropolitan show a significant effect measure modifier (P < .001).
IBD-related Hospitalizations
The age- and sex-standardized IBD-related hospitalization rate decreased from 26.44 (95% CI, 25.42-27.46) to 9.24 (95% CI, 8.91-9.57) hospitalizations per 100 IBD patients (AAPC = −5.54%; 95% CI, −6.19 to −4.88) and decreased from 77.08 (95% CI, 74.01-80.16) to 69.15 (95% CI, 66.67-71.64) hospitalizations per 100,000 persons (AAPC = −0.27%; 95% CI, −0.53 to −0.01; Supplementary Table 6, page 9; Table 1). The disease-specific age- and sex-standardized IBD-related hospitalization rates decreased from 29.32 (95% CI, 27.93-30.72) to 10.59 (95% CI, 10.09-11.10) CD hospitalizations per 100 CD patients (AAPC = −5.07%; 95% CI, −5.69 to −4.44) and from 23.45 (95% CI, 21.77-25.13) to 8.86 (95% CI, 8.33-9.38) UC hospitalizations per 100 UC patients (AAPC = −5.37%; 95% CI, −6.28 to −4.46; Supplementary Table 7, page 10; Table 1).
Non-IBD-related Hospitalizations
The age- and sex-standardized non-IBD-related hospitalization rate decreased from 10.13 (95% CI, 9.49, 10.76) to 7.48 (95% CI, 7.18-7.78) hospitalizations per 100 IBD patients (AAPC = −1.82%; 95% CI, −2.14 to −1.49) and increased from 33.56 (95% CI, 31.53-35.59) to 73.02 (95% CI, 70.47-75.58) hospitalizations per 100,000 Albertans (AAPC = 4.15%; 95% CI, 3.48-4.81; Supplementary Table 8, page 11; Table 1). The disease-specific age- and sex-standardized non-IBD-related hospitalization rates decreased from 11.12 (95% CI, 10.26-11.98) to 7.82 (95% CI, 7.38-8.25) CD hospitalizations per 100 CD patients (AAPC = −2.16%; 95% CI, −2.71 to −1.60) and from 7.38 (95% CI, 6.44-8.32) to 6.70 (95% CI, 6.25-7.16) UC hospitalizations per 100 UC patients (AAPC = −0.50%; 95% CI, −1.05 to −0.06; Supplementary Table 9, page 12; Table 1). Trends in non-IBD-related UC and CD hospitalization rates were significantly different (P < .001).
Age-stratified Hospitalization Rates
Age-stratified hospitalization rates using the prevalent IBD population as the denominator are displayed for all-cause, IBD-related, and non-IBD-related diagnoses in Figures 1, 2, and 3, respectively. Those aged 80+ had the greatest all-cause and non-IBD-related hospitalization rates among all age groups and years (Figures 1 and 3), while those aged <18 and 80+ had the greatest IBD-related hospitalization rates (Figure 2). The AAPC in all-cause hospitalization rate per 100 IBD patients in those aged <18 (AAPC = −5.46%; 95% CI, −6.67 to −4.23) were decreasing at a greater rate than those aged 40–59 (AAPC = −3.41%; 95% CI, −3.84 to −2.97), 60–79 (AAPC = −3.33%; 95% CI, −3.82 to −2.84) and those aged 80+ (AAPC = −2.77%; 95% CI, −3.61 to −1.92) [Table 1, Figure 1]. Similarly, the AAPC in IBD-related hospitalizations per 100 IBD patients in those aged <18 (AAPC = −6.02%; 95% CI, −7.19 to −4.85) was decreasing at a greater rate than those aged 60–79 (AAPC = −4.53%; 95% CI, −5.36 to −3.69) [Table 1, Figure 2]. Trends in non-IBD-related hospitalization rates were not statistically different among age groups.
Figure 1.
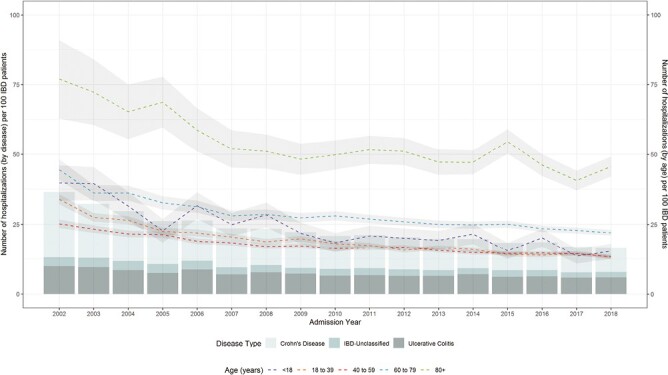
Age- and sex-standardized all-cause IBD hospitalization rates per 100 IBD patients stratified by age groups and disease type. The scale on the left refers to the summative bar graphs representing the distribution of disease type; the scale on the right refers to the line graphs representing the hospitalization rates by age group.
Figure 2.
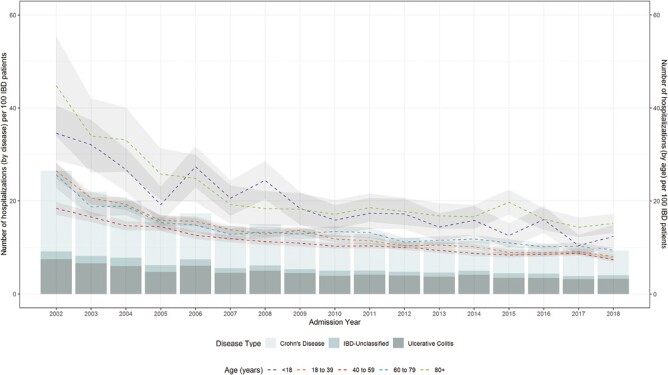
Age- and sex-standardized IBD-related diagnosis IBD hospitalization rates per 100 IBD patients stratified by age groups and disease type. The scale on the left refers to the summative bar graphs representing the distribution of disease type; the scale on the right refers to the line graphs representing the hospitalization rates by age group.
Figure 3.
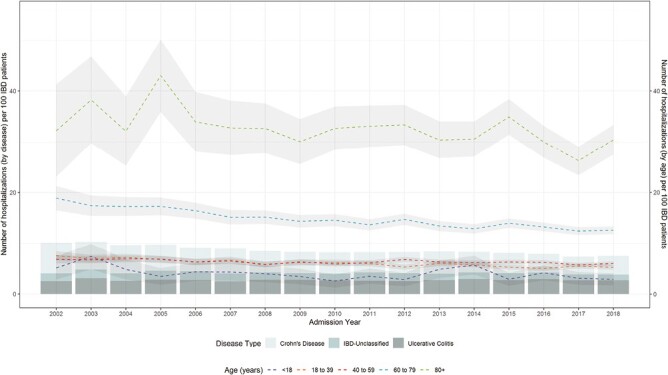
Age- and sex-standardized non-IBD-related diagnosis IBD hospitalization rates per 100 IBD patients stratified by age groups and disease type. The scale on the left refers to the summative bar graphs representing the distribution of disease type; the scale on the right refers to the line graphs representing the hospitalization rates by age group.
Sex-stratified Hospitalization Rates
Females (AAPC = −4.07%; 95% CI, −4.63 to −3.50) and males (AAPC = −4.28%; 95% CI, −4.84 to −3.72) had comparable (p=0.60) and significantly decreasing trends in all-cause hospitalization rates using the prevalent IBD population as the denominator. [Table 1, Supplementary Figure 1, page 15]. Trends in IBD-related hospitalization rates per 100 IBD patients were decreasing for both males (AAPC = −5.36; 95% CI, −6.06 to −4.65) and females (AAPC = −5.70; 95% CI, −6.45 to −4.95) and were not significantly different. [Table 1; Supplementary Figure 2, page 16]. Trends in non-IBD-related hospitalization rates per 100 IBD patients were decreasing as well for both males (AAPC = −2.12; 95% CI, −2.57 to −1.67) and females (AAPC = −1.58; 95% CI, −1.99 to −1.16) and were not significantly different (Supplementary Figure 3, page 17). Notably, non-IBD-related hospitalization rates among females were greater than males across all years (Supplementary Figure 3, page 17). When comparing metropolitan hospitalization rates to nonmetropolitan hospitalization rates, nonmetropolitan hospitalization rates were decreasing at a greater rate across all hospitalization types (P < .001), but metropolitan hospitalization rates were greater across all years (Table 1; Supplementary Figures 4, 5, and 6, pages 18, 19, and 20).
Discussion
Trends in hospitalization rates for people living with IBD vary based on the methodology used. When using the IBD prevalent population as the denominator, hospitalization rates in Alberta decreased over time for all-cause hospitalizations, as well as for admission related and unrelated to IBD. However, when using the Alberta general population as the denominator, trends in hospitalization rates were decreasing at a slower rate, stable, or even increasing. These hospitalization rates differ because the IBD prevalent population in Alberta increased over 3-fold from 2002 to 2018, whereas the general population only increased 1.4-fold during the same period. Consequently, these differing denominators alter the interpretations of IBD hospitalization trends. This finding is important, as a previous systematic review identified that the vast majority of prior publications reported IBD hospitalization rates relative to the general population.4 Future studies on hospitalization trends should use the prevalent IBD population and the general population as the denominator to accurately represent the burden and trends in hospitalization for IBD because both methodologies offer different insights into trends.
At the beginning of the 21st century, the implementation of biologics and other advances in medical therapy had decreased the risk of hospitalization and surgery for patients living with IBD.5 For example, anti-TNF therapies were introduced in the early 2000s in Canada, which has been associated with decreasing surgical rates for IBD in Alberta.18,19 Our systematic review reported that hospitalization rates are primarily stable or decreasing in the Western world.4 In 2022, Lyons et al published a study investigating annual IBD hospitalization rates from 2010 to 2019 in Scotland.20 They found that IBD-related admissions decreased from 39.4 to 25.5 per 100,000 population (AAPC = −3%; 95% CI, −4.5 to −2.1).20 These results are comparable; primary-cause IBD hospitalization rates in Alberta decreased from 38.18 to 21.81 per 100,000 from 2002 to 2018 (AAPC = −3.01%; 95% CI, −3.38 to −2.64). Even with the inclusion of data before 2010, trends in hospitalization rates in Alberta are comparable.
Lyons et al also reported IBD-related admissions per 100 IBD patients. They found that IBD-related admissions decreased from 6.22 to 3.26 hospitalizations per 100 IBD patients from 2010 to 2018.20 These rates are similar to rates in Alberta; primary-cause IBD hospitalization rates decreased from 5.19 to 4.02 per 100 IBD patients from 2010 to 2018. Similarly, a study from Portugal showed hospitalization rates increased by 2% per year from 2000 to 2015 when using the general population as the denominator; however, rates were decreasing when corrected for the rising prevalence of IBD.21 Our data, in conjunction with the studies from Scotland and Portugal, highlight the importance of correcting for the rising prevalence of IBD when calculating hospitalization rates and trends. Therefore, studies that report both primary- and all-cause hospitalization rates using the IBD prevalent population as the denominator will provide a more accurate representation of burden on the patient and health care system.
The decreasing rates of hospitalization for IBD may be explained by several factors. The last 2 decades have seen the introduction of several advanced therapies with novel mechanisms of action.22 The introduction of these therapies has been accompanied by changes in management strategies that include earlier introduction of advanced therapies based on risk stratification, treat-to-target, and monitoring strategies.5,23–26 These advancements include risk stratification, allowing for earlier introduction of advanced therapies; proactive clinical management algorithms to monitor disease activity; and therapeutic drug monitoring allowing for continued concentration-based dosing.23–26 The net effect of these medical advances shifted IBD management from the hospital to the outpatient setting.27
The definition of hospitalization is important to differentiate the type of hospitalization being studied. All-cause hospitalizations include flaring patients and those with IBD but hospitalized for alternate reasons (eg, acute pancreatitis). In contrast, IBD-related hospitalizations focus on hospitalizations directly attributed to a flare of IBD or a symptom (eg, high ostomy output), complication (eg, intra-abdominal abscess), or comorbidity (eg, extraintestinal manifestation) associated with IBD. IBD-related hospitalization rates reflect disease burden due to disease activity or complication of IBD, whereas all-cause hospitalizations report the overall burden of IBD to the health care system. Prior studies on hospitalization rates for IBD have used mixed definitions such as only including hospitalizations where IBD is the most responsible diagnosis or where IBD is in any diagnostic coding position regardless of whether the admission was attributable to IBD. Future hospitalization studies should use strict and comparable definitions (eg IBD-related and/or all-cause) based on the research questions posed.
Those aged 80 years or older had the highest all-cause and non-IBD-related hospitalization rate from 2002 to 2018, whereas those younger than 18 years had the highest or second highest IBD-related hospitalization rate. Inflammatory bowel disease is commonly first diagnosed in younger individuals, and disease severity is often the greatest in the years following the diagnosis, as medical management is modified to induce and maintain remission.28 In contrast, all-cause hospitalization rates are greater among older adults because age-related comorbidities (eg, cardiovascular disease, cancer) driving admissions directly or contributing to the complexity of an IBD flare. Hospitalizations for seniors with IBD may increase the burden of IBD management, as those 65 years or older with IBD are the fastest growing prevalent group in Canada due to aging from long-standing disease and new IBD diagnoses in seniors.3 Therefore, health care systems must be prepared to shape health care policies to meet future demands, which are different between age cohorts.
Sex-based differences also exist in IBD. For example, female sex is more commonly associated with hospitalization for fractures among individuals living with IBD.29 In contrast, 1-year hospital readmission is significantly associated with being male, and being male is significantly associated with risk of colectomy.30,31 However, sex-based differences in trends were not observed in Alberta IBD hospitalization rates.
The precision of our estimates are high, and the risk of selection bias is mitigated because administrative data encompasses >99% of the Alberta population. Therefore, if other populations (ie, other Canadian provinces) share similar environmental exposures, determinants (ie, access to health care), or population distributions, our results may be generalizable.32 However, important limitations must be addressed. As with all studies using routinely collected administrative health data, there are several limitations. First, administrative data are at risk of misclassification of the diagnosis of IBD.33 To mitigate this risk, we implemented a previously validated coding algorithm that minimizes false positives contained in the prevalent cohort.10 Furthermore, the definition of IBD-U has no clinical relevance but is a methodological artefact relating to the scoring algorithm used to distinguish CD from UC and, thus, is an overestimation of and clinically different than a clinical diagnosis of IBD-U.10 Additionally, outpatient management may differ for individuals with easy access to health care (eg, living in a metropolitan city with greater availability of gastroenterologists). However, hospitalization trends were not significantly different for those in metropolitan and nonmetropolitan zones, suggesting equitable care across the geographic regions of Alberta. Furthermore, all-cause hospitalization rates in the IBD population were not compared with all-cause hospitalizations in the general Alberta population. Decreasing trends of all-cause hospitalizations in the IBD population may reflect a general shift away from hospital care in the Alberta population. For example, outpatient management of venous thromboembolism has increased in the last decade.34 If a similar shift in IBD care practice were to be observed, trends in IBD hospitalization rates may reflect general trends in the health care setting.
This population-based administrative data cohort study provides annual IBD hospitalization rates in Alberta, Canada. All-cause, IBD-related, and non-IBD-related hospitalization rates are decreasing regardless of age, sex, or metropolitan status. However, when assessing the same IBD hospitalization rates but using the general population as the denominator, the interpretation of temporal trends changes because the prevalence of IBD has risen faster than the general population rates. Future studies should assess outcome-defined hospitalization rates using the IBD prevalent population and the general population as the denominator to better represent the burden and trends in hospitalization rates for those with IBD.
Supplementary Material
Acknowledgments
Ethics approval was obtained from the Conjoint Research Ethics Board at the University of Calgary (REB21-0398). All research data were stored in a secure central electronic database and de-identified. All analysis was done on a remote server that maintains compliance with ISO 17799/27001 information security management system standards.
Contributor Information
Michael J Buie, Department of Medicine, University of Calgary, Calgary, Alberta, Canada; Department of Community Health Sciences, University of Calgary, Calgary, Alberta, Canada.
Stephanie Coward, Department of Medicine, University of Calgary, Calgary, Alberta, Canada; Department of Community Health Sciences, University of Calgary, Calgary, Alberta, Canada.
Abdel-Aziz Shaheen, Department of Medicine, University of Calgary, Calgary, Alberta, Canada; Department of Community Health Sciences, University of Calgary, Calgary, Alberta, Canada.
Jayna Holroyd-Leduc, Department of Medicine, University of Calgary, Calgary, Alberta, Canada; Department of Community Health Sciences, University of Calgary, Calgary, Alberta, Canada.
Lindsay Hracs, Department of Medicine, University of Calgary, Calgary, Alberta, Canada; Department of Community Health Sciences, University of Calgary, Calgary, Alberta, Canada.
Christopher Ma, Department of Medicine, University of Calgary, Calgary, Alberta, Canada; Division of Gastroenterology and Hepatology, Department of Medicine, University of Calgary, Calgary, Alberta, Canada.
Remo Panaccione, Department of Community Health Sciences, University of Calgary, Calgary, Alberta, Canada; Division of Gastroenterology and Hepatology, Department of Medicine, University of Calgary, Calgary, Alberta, Canada.
Eric I Benchimol, SickKids Inflammatory Bowel Disease Centre, Division of Gastroenterology, Hepatology and Nutrition, The Hospital for Sick Children, Toronto, Ontario, Canada; Child Health Evaluative Sciences, SickKids Research Institute, Toronto, Ontario, Canada; Institute of Health Policy, Management and Evaluation, University of Toronto, Toronto, Ontario, Canada; Institute for Clinical Evaluative Sciences, Toronto, Ontario, Canada; Department of Paediatrics, University of Toronto, Toronto, Ontario, Canada.
Charles N Bernstein, Department of Medicine, and the University of Manitoba IBD Clinical and Research Centre, Max Rady College of Medicine, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, Manitoba, Canada.
Alain Bitton, Division of Gastroenterology and Hepatology, McGill University and McGill University Health Centre, Montreal, Quebec, Canada.
Anthony R Otley, Department of Pediatrics, Faculty of Medicine, Dalhousie University, Halifax, Nova Scotia, Canada.
Jennifer L Jones, Division of Digestive Care & Endoscopy, Department of Medicine, Dalhousie University, Halifax, NS, Canada.
Sanjay K Murthy, Department of Medicine, University of Ottawa, Ottawa, Ontario, Canada; Division of Gastroenterology, The Ottawa Hospital IBD Centre, Ottawa, Ontario, Canada; Clinical Epidemiology Program, Ottawa Hospital Research Institute, Ottawa, Ontario, Canada; School of Epidemiology and Public Health, University of Ottawa, Ottawa, Ontario, Canada.
M Ellen Kuenzig, SickKids Inflammatory Bowel Disease Centre, Division of Gastroenterology, Hepatology and Nutrition, The Hospital for Sick Children, Toronto, Ontario, Canada; Child Health Evaluative Sciences, SickKids Research Institute, Toronto, Ontario, Canada.
Juan-Nicolás Peña-Sánchez, Department of Community Health and Epidemiology, College of Medicine, University of Saskatchewan, Saskatoon, Saskatchewan, Canada.
Laura E Targownik, Zane Cohen Centre for Digestive Diseases, Mount Sinai Health, Toronto, Ontario, Canada.
Harminder Singh, Departments of Medicine and Community Health Sciences, University of Manitoba, Max Rady College of Medicine, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, Manitoba, Canada; Research Institute, CancerCare, Winnipeg, Manitoba, Canada.
Antonio Avina-Zubieta, Division of Rheumatology, Department of Medicine, University of British Columbia, Vancouver, British Columbia, Canada.
Gilaad G Kaplan, Department of Medicine, University of Calgary, Calgary, Alberta, Canada; Department of Community Health Sciences, University of Calgary, Calgary, Alberta, Canada.
Author Contributions
M.J.B., S.C., and G.G.K. have full access to all data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. M.J.B., S.C., and G.G.K. conceived and designed the study. M.J.B., S.C., L.H., and G.G.K. analyzed the data. M.J.B., S.C., and G.G.K. drafted the manuscript. All authors interpreted the data and provided critical revisions of the manuscript for important intellectual content. All authors have approved the final draft of the manuscript.
Funding
Canadian Institutes of Health Research, Project Scheme Operating Grant (Reference number PJT-162393).
Conflicts of Interest
G.K. has received honoraria for speaking or consultancy from AbbVie, Janssen, Pfizer, Amgen, and Takeda. He has received research support from Ferring, Janssen, AbbVie, GlaxoSmith Kline, Merck, and Shire. He has been a consultant for Gilead. He shares ownership of a patent: TREATMENT OF INFLAMMATORY DISORDERS, AUTOIMMUNE DISEASE, AND PBC. UTI Limited Partnership, assignee. Patent WO2019046959A1. PCT/CA2018/051098. September 7, 2018.
A-A.S. has research grants (investigator initiated programs) from Gilead and Intercept Pharmaceuticals.
H.S. has been on advisory boards or consulted to Pendopharm, Amgen Canada, Bristol Myers Squibb Canada, Roche Canada, Sandoz Canada, Takeda Canada, and Guardant Health, Inc.,
C.B. has consulted to or served on advisory boards for Abbvie Canada, Amgen Canada, Bristol Myers Squibb Canada, JAMP Pharmaceuticals, Janssen Canada, Pfizer Canada, Sandoz Canada, Takeda, and has received unrestricted educational grants from Abbvie Canada, Janssen Canada, Pfizer Canada, Bristol Myers Squibb Canada, and Takeda Canada. He has been on the speaker’s bureau of Abbvie Canada, Janssen Canada, Pfizer Canada, and Takeda Canada. He has received research grants from Abbvie Canada, Amgen Canada, Pfizer Canada, and Sandoz Canada and contract grants from Janssen.
R.P. has received consulting fees from Abbott, AbbVie, Alimentiv (formerly Robarts), Amgen, Arena Pharmaceuticals, AstraZeneca, Biogen, Boehringer Ingelheim, Bristol-Myers Squibb, Celgene, Celltrion, Cosmos Pharmaceuticals, Eisai, Elan, Eli Lilly, Ferring, Galapagos, Fresenius Kabi, Genentech, Gilead Sciences, Glaxo-Smith Kline, JAMP Bio, Janssen, Merck, Mylan, Novartis, Oppilan Pharma, Organon, Pandion Pharma, Pendopharm, Pfizer, Progenity, Protagonist Therapeutics, Roche, Sandoz, Satisfai Health, Shire, Sublimity Therapeutics, Takeda.
E.B. has acted as a legal consultant for Hoffman La-Roche Limited and Peabody & Arnold LLP.
A.O. has been on advisory boards of AbbVie Canada, Janssen Canada, and Nestle. He has received unrestricted educational grants from AbbVie Canada and Janssen Canada. His site is involved with clinical trials for AbbVie, Pfizer, Takeda, Eli Lily, and Celgene.
L.T. has received investigator initiated funding from Janssen Canada and served on advisory boards for AbbVie Canada, Sandoz Canada, Takeda Canada, Merck Canada, Pfizer Canada, Janssen Canada, and Roche Canada.
C.M. has received consulting fees from AbbVie, Alimentiv, Amgen, AVIR Pharma Inc, BioJAMP, Bristol Myers Squibb, Celltrion, Ferring, Fresenius Kabi, Janssen, McKesson, Mylan, Takeda, Pendopharm, Pfizer, Roche; speaker’s fees from AbbVie, Amgen, AVIR Pharma Inc, Alimentiv, Bristol Myers Squibb, Ferring, Fresenius Kabi, Janssen, Takeda, Pendopharm, and Pfizer; royalties from Springer Publishing; research support from Ferring, Pfizer.
A.B. has been a member of advisory boards for Abbvie, Pfizer, Takeda, Janssen, Merck and speaker’s bureau for Abbvie, Janssen, Takeda, Pfizer.
J.J. reports advisory board fees from AbbVie, Janssen, Pfizer, Ferring; speaker’s fees from AbbVie, Janssen Takeda; and research support from AbbVie, Janssen and Pfizer.
The following authors have no conflicts to declare: M.B., S.C., S.M., J. P., L.H., E.K., A.A-Z, and J.H-L.
Data Availability
All data reported is provided in an open-access, online interactive map: https://kaplan-gi.shinyapps.io/hospitalization/
References
- 1. Seyedian SS, Nokhostin F, Malamir MD.. A review of the diagnosis, prevention, and treatment methods of inflammatory bowel disease. NLM (Medline) 2019;12(2):113-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kaplan GG, Bernstein CN, Coward S, et al. The Impact of Inflammatory Bowel Disease in Canada 2018: Epidemiology. J Can Assoc Gastroenterol. 2019;2(Supplement_1):S6-S16. doi: 10.1093/jcag/gwy054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nguyen GC, Targownik LE, Singh H, et al. The Impact of Inflammatory Bowel Disease in Canada 2018: IBD in Seniors. J Can Assoc Gastroenterol. 2019;2(Supplement_1):S68-S72. doi: 10.1093/jcag/gwy051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Buie MJ, Quan J, Windsor JW, et al. Global hospitalization trends for crohn’s disease and ulcerative colitis in the 21st century: a systematic review with temporal analyses. Clin Gastroenterol Hepatol. 2022. online ahead of print. doi: 10.1016/j.cgh.2022.06.030 [DOI] [PubMed] [Google Scholar]
- 5. Mao EJ, Hazlewood GS, Kaplan GG, Peyrin-Biroulet L, Ananthakrishnan AN.. Systematic review with meta-analysis: comparative efficacy of immunosuppressants and biologics for reducing hospitalisation and surgery in Crohn’s disease and ulcerative colitis. Aliment Pharmacol Ther. Jan 2017;45(1):3-13. doi: 10.1111/apt.13847 [DOI] [PubMed] [Google Scholar]
- 6. Estimates of population by age group and sex for July 1, Canada, provinces and territories annual. Statistics Canada. Accessed February 18, 2022. http://www5.statcan.gc.ca/cansim/a26?lang=eng&retrLang=eng&id=0510001&tabMode=dataTable&srchLan=-1&p1=-1&p2=9 [Google Scholar]
- 7. Interactive Health Data Applications. Government of Alberta. Accessed February 17, 2022. http://www.ahw.gov.ab.ca/IHDA_Retrieval/selectCategory.do
- 8. Canada S. Estimates of population, by age group and sex for July 1, Canada, provinces and territories annual. Accessed March 15 2022, https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000501
- 9. Coward S, Clement F, Benchimol EI, et al. Past and future burden of inflammatory bowel diseases based on modeling of population-based data. Gastroenterology. 2019;156(5):1345-1353.e4. doi: 10.1053/j.gastro.2019.01.002 [DOI] [PubMed] [Google Scholar]
- 10. Rezaie A, Quan H, Fedorak RN, Panaccione R, Hilsden RJ.. Development and validation of an administrative case definition for inflammatory bowel diseases. Can J Gastroenterol. 2012;26(10):711-717. doi: 10.1155/2012/278495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dheri AK, Kuenzig ME, Mack DR, et al. Shifting health care use from hospitalizations and surgeries to outpatient visits in children with inflammatory bowel disease: a population-based cohort study from Ontario, Canada. J Crohns Colitis. 2021;15(12):1991-2000. doi: 10.1093/ecco-jcc/jjab095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kuenzig ME, Stukel TA, Kaplan GG, et al. Variation in care of patients with elderly-onset inflammatory bowel disease in Ontario, Canada: a population-based cohort study. J Can Assoc Gastroenterol. Apr 2021;4(2):e16-e30. doi: 10.1093/jcag/gwz048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Benchimol EI, Kuenzig ME, Bernstein CN, et al. Rural and urban disparities in the care of Canadian patients with inflammatory bowel disease: a population-based study. Clin Epidemiol. 2018;10:1613-1626. doi: 10.2147/clep.S178056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Benchimol EI, Mac KDR, Nguyen GC, et al. Incidence, outcomes, and health services burden of very early onset inflammatory bowel disease. Gastroenterology. 01 Oct 2014;147(4):803-813.e7. doi: 10.1053/j.gastro.2014.06.023 [DOI] [PubMed] [Google Scholar]
- 15. Benchimol EI, Kaplan GG, Otley AR, et al. Rural and urban residence during early life is associated with risk of inflammatory bowel disease: a population-based inception and birth cohort study. Am J Gastroenterol. Sep 2017;112(9):1412-1422. doi: 10.1038/ajg.2017.208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Langan SM, Schmidt SA, Wing K, et al. The reporting of studies conducted using observational routinely collected health data statement for pharmacoepidemiology (RECORD-PE). BMJ. 2018;363:k3532. doi: 10.1136/bmj.k3532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wickham H. ggplot2: Elegant Graphics for Data Analysis. R package version 3.3.4. Springer-Verlag New York; 2016. [Google Scholar]
- 18. Kaplan GG, Seow CH, Ghosh S, et al. Decreasing colectomy rates for ulcerative colitis: a population-based time trend study. Am J Gastroenterol. Dec 2012;107(12):1879-1887. doi: 10.1038/ajg.2012.333 [DOI] [PubMed] [Google Scholar]
- 19. Ma C, Moran GW, Benchimol EI, et al. Surgical rates for Crohn’s disease are decreasing: a population-based time trend analysis and validation study. Am J Gastroenterol. 2017;112(12):1840-1848. doi: 10.1038/ajg.2017.394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lyons M, Derikx L, Fulforth J, et al. Patterns of emergency admission for IBD patients over the last 10 years in Lothian, Scotland: a retrospective prevalent cohort analysis. Aliment Pharmacol Ther. Mar 17 2022. doi: 10.1111/apt.16867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dias CC, Santiago M, Correia L, et al. Hospitalization trends of the inflammatory bowel disease landscape: a nationwide overview of 16 years. Dig Liver Dis. Jul 2019;51(7):952-960. doi: 10.1016/j.dld.2019.01.016 [DOI] [PubMed] [Google Scholar]
- 22. Baumgart DC, Le Berre C.. Newer biologic and small-molecule therapies for inflammatory bowel disease. N Engl J Med. 2021;385(14):1302-1315. doi: 10.1056/NEJMra1907607 [DOI] [PubMed] [Google Scholar]
- 23. Asscher VER, Lee-Kong FVY, Kort ED, van Deudekom FJ, Mooijaart SP, Maljaars PWJ.. Systematic review: components of a comprehensive geriatric assessment in inflammatory bowel disease—a potentially promising but often neglected risk stratification. J Crohn’s Colitis. 2019;13(11):1418-1432. doi: 10.1093/ecco-jcc/jjz082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Colombel JF, Panaccione R, Bossuyt P, et al. Effect of tight control management on Crohn’s disease (CALM): a multicentre, randomised, controlled phase 3 trial. Lancet. Dec 23 2017;390(10114):2779-2789. doi: 10.1016/s0140-6736(17)32641-7 [DOI] [PubMed] [Google Scholar]
- 25. Freeman K, Willis BH, Fraser H, Taylor-Phillips S, Clarke A.. Faecal calprotectin to detect inflammatory bowel disease: a systematic review and exploratory meta-analysis of test accuracy. BMJ Open. Mar 8 2019;9(3):e027428. doi: 10.1136/bmjopen-2018-027428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Vande Casteele N, Ferrante M, Van Assche G, et al. Trough concentrations of infliximab guide dosing for patients with inflammatory bowel disease. Gastroenterology. Jun 2015;148(7):1320-1329.e3. doi: 10.1053/j.gastro.2015.02.031 [DOI] [PubMed] [Google Scholar]
- 27. Rahman AJV, Feagan BG, Khanna R, et al. Declining hospitalisation and surgical intervention rates in patients with Crohn’s disease: a population-based cohort. Aliment Pharmacol Ther. 01 Nov 2019;50(10):1086-1093. doi: 10.1111/apt.15511 [DOI] [PubMed] [Google Scholar]
- 28. Yarur AJ, Strobel SG, Deshpande AR, Abreu MT.. Predictors of aggressive inflammatory bowel disease. Gastroenterol Hepatol. 2011;7(10):652-659. [PMC free article] [PubMed] [Google Scholar]
- 29. Ananthakrishnan AN, McGinley EL, Binion DG, Saeian K.. Fracture-associated hospitalizations in patients with inflammatory bowel disease. Dig Dis Sci. Jan 2011;56(1):176-182. doi: 10.1007/s10620-010-1433-9 [DOI] [PubMed] [Google Scholar]
- 30. Mudireddy P, Scott F, Feathers A, Lichtenstein GR.. Inflammatory bowel disease: predictors and causes of early and late hospital readmissions. Inflamm Bowel Dis. 2017;23(10):1832-1839. doi: 10.1097/mib.0000000000001242 [DOI] [PubMed] [Google Scholar]
- 31. Samuel S, Ingle SB, Dhillon S, et al. Cumulative incidence and risk factors for hospitalization and surgery in a population-based cohort of ulcerative colitis. Inflamm Bowel Dis. Aug 2013;19(9):1858-1866. doi: 10.1097/MIB.0b013e31828c84c5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Molodecky NA, Panaccione R, Ghosh S, Barkema HW, Kaplan GG.. Challenges associated with identifying the environmental determinants of the inflammatory bowel diseases. Inflamm Bowel Dis. Aug 2011;17(8):1792-1799. doi: 10.1002/ibd.21511 [DOI] [PubMed] [Google Scholar]
- 33. Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142(1):46-54.e42. doi: 10.1053/j.gastro.2011.10.001 [DOI] [PubMed] [Google Scholar]
- 34. Lutsey PL, Walker RF, MacLehose RF, et al. Inpatient versus outpatient acute venous thromboembolism management: trends and postacute healthcare utilization from 2011 to 2018. J Am Heart Assoc. 2021;10(20):e020428. doi: 10.1161/JAHA.120.020428 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data reported is provided in an open-access, online interactive map: https://kaplan-gi.shinyapps.io/hospitalization/


