Abstract
Background
The American Heart Association's Life's Essential 8 (LE8) are 8 risk factors for cardiovascular disease, with poor attainment across all racial, ethnic, and socioeconomic groups. Attainment is lowest among Americans of low socioeconomic status (SES). Evidence suggests the association of SES with LE8 may vary by race and ethnicity.
Methods and Results
The association of 4 SES categories (education, income‐to‐poverty line ratio, employment, insurance) with LE8 was computed in age‐adjusted linear regression models, with an interaction term for race and ethnicity, using National Health and Nutrition Examination Survey data, years 2011 to 2018. The sample (n=13 529) had a median age of 48 years (51% female) with weighting to be representative of the US population. The magnitude of positive association of college education (relative to ≤high school) with LE8 was greater among non‐Hispanic White Americans (NHWA) compared with non‐Hispanic Black Americans, Hispanic Americans, and non‐Hispanic Asian Americans (all interactions P<0.001). NHWA had a greater magnitude of positive association of income‐to‐poverty line ratio with LE8, compared with non‐Hispanic Black Americans, Hispanic Americans, and non‐Hispanic Asian Americans (all interactions P<0.001). NHWA with Medicaid compared with private insurance had a greater magnitude of negative association with LE8 compared with non‐Hispanic Black Americans, non‐Hispanic Asian Americans, or Hispanic Americans (all interactions P<0.01). NHWA unemployed due to disability or health condition (compared with employed) had a greater magnitude of negative association with LE8 than non‐Hispanic Black Americans, non‐Hispanic Asian Americans, or Hispanic Americans (all interactions P<0.05).
Conclusions
The magnitude of association of SES with LE8 is greatest among NHWA. More research is needed on SES's role in LE8 attainment in minority group populations.
Keywords: cardiovascular disease, ethnicity, primordial prevention, race, risk factors, socioeconomic status
Subject Categories: Epidemiology, Lifestyle, Race and Ethnicity, Primary Prevention, Risk Factors
Nonstandard Abbreviations and Acronyms
- CVH
cardiovascular health
- HA
Hispanic Americans
- LE8
Life's Essential 8
- NHAA
non‐Hispanic Asian Americans
- NHANES
National Health and Nutrition Examination Survey
- NHBA
non‐Hispanic Black Americans
- NHWA
non‐Hispanic White Americans
- PIR
income‐to‐poverty‐line ratio
- SDoH
social determinants of health
Clinical Perspective.
What Is New?
The association of socioeconomic status with cardiovascular health is of greatest magnitude among non‐Hispanic White Americans compared with non‐Hispanic Black Americans, non‐Hispanic Asian Americans, and Hispanic Americans.
What Are the Clinical Implications?
Improving socioeconomic status is beneficial in all populations but may have differential magnitudes of effect in different races and ethnicities; thus, multi‐pronged approaches may be necessary to advance cardiovascular health equity.
Cardiovascular disease (CVD) is the leading cause of death in the United States. 1 Significant disparities in CVD mortality exist based on the social constructs of race and ethnicity. Non‐Hispanic Black Americans (NHBA) have lower life expectancy than non‐Hispanic White Americans (NHWA), and 32% to 43% of this disparity is due to differences in CVD mortality rates. 2 The diverse group of non‐Hispanic Asian Americans (NHAA) have a higher burden of hypertension and hemorrhagic stroke than NHWA. 3 Conversely, for the diverse group of Hispanic Americans (HA), rates of coronary heart disease and stroke are lower than rates among NHWA 4 ; however, prevalence of diabetes is twice as high among HA than NHWA. 5
Whether racial and ethnic minority groups have higher or lower rates of CVD than the majority group, all CVD rates are unacceptably high, as 80% to 90% of CVD is preventable. 6 In an effort to lower CVD rates, the American Heart Association identified 8 factors pivotal for the prevention of CVD, called Life's Essential 8 (LE8). 7 Racial and ethnic disparities in attainment of ideal levels of these 8 factors (blood pressure, total cholesterol, blood glucose, body mass index, diet, physical activity, sleep, and smoking) exist in the United States, with NHBA having the lowest LE8 scores. 8 , 9 Attainment of Life's Simple 7, which preceded LE8 and has the same factors (except sleep), is independently associated with socioeconomic status (SES), which is an aggregate construct that includes education, income, and occupation. 8 Participants with higher SES have better attainment of Life's Simple 7 across racial and ethnic groups. 8 It has been posited that the racial and ethnic disparities in ideal cardiovascular health (CVH) attainment are related to racial and ethnic disparities in higher SES attainment and that improving SES attainment in racial and ethnic minority groups will close the CVH gap. However, a recent paper suggests a low magnitude of association of SES with CVH among NHBA men. 10 Here, we examine the association of SES with LE8 across racial and ethnic groups in the United States using nationally representative National Health and Nutrition Examination Survey (NHANES) data. NHANES is the preferred method of population‐based assessment of LE8 indicated in the American Heart Association presidential statement. 7 We hypothesized that racial and ethnic minority groups would have a lower magnitude of association of SES with LE8 compared with NHWA.
METHODS
Sample Characteristics
NHANES is a cross‐sectional, multistage, stratified, clustered probability sample of the US civilian noninstitutionalized population conducted by the National Center for Health Statistics of the Centers for Disease Control and Prevention. All data and guidance on analytical approaches are publicly and freely available from the Centers for Disease Control and Prevention's National Center for Health Statistics and can be accessed at https://www.cdc.gov/nchs/nhanes/index.htm. The NHANES data analyzed were collected in 4 waves from 2011 to 2018 (2011–2012, 2013–2014, 2015–2016, and 2017–2018). These waves included oversampling of NHAA. These waves were combined and sample weights were adjusted following National Center for Health Statistics guidelines. 11 Participants were interviewed and physical examination included blood collection. For this analysis, we included adults aged ≥20 years who were not missing any components of the LE8 score, SES variables, or covariates (n=13 529; Figure S1). Table S1 shows characteristics of included participants and participants excluded due to missing data. All participants gave written informed consent, and the NHANES study protocol was approved by the National Center for Health Statistics Institutional Review Board. This analysis of secondary data was exempted from approval by The Ohio State University Institutional Review Board, as the use of deidentified secondary data does not constitute human subjects research.
Socioeconomic Status Variables (Exposures)
Education
NHANES provided data on education status, with the following levels: less than 9th grade, 9 to 11th grade (includes 12th grade with no diploma), high school graduate/General Educational Development or equivalent, some college or associate's degree, and college graduate or above. Because of the small sample size, and consistent with our prior analyses, 10 the lower levels of education were condensed. The 3 categories used in this analysis were high school graduate/General Educational Development or less, some college or associate's degree, and college graduate or above.
Income
Annual family income was divided by the applicable poverty line, based on family size, to calculate the income‐to‐poverty line ratio (PIR). In NHANES, PIR is reported continuously in values ranging from 0 (no income) to 5 (≥5 times the poverty line). In the particpant characteristics table, PIR was reported categorically, but in regression models it was used continuously.
Employment
Employment status levels were student, retired, employed, unemployed, and unable to work for health reasons/disability.
Health Insurance Status
Health insurance levels were private, uninsured, Medicare, Medicaid, military, combination, and other. Combination insurance is any combination of insurances.
Life's Essential 8 Scoring (Outcome)
LE8 score (0–100 scale) was the average of the scores for the 8 individual components detailed next. An average score of 0 to 49 is defined as low CVH, 50 to 79 is moderate CVH, and 80 to 100 is high CVH in the participant characteristics table, although in regression analyses, LE8 score was modeled continuously.
Body Mass Index
Body mass index (kg/m2) was measured in the Mobile Examination Center by trained health technicians. Scoring for Asian and non‐Asian participants is described in Table 1. Non‐Asian participants with a body mass index <25 kg/m2 received 100 points, and Asian participants with a body mass index <23 kg/m2 received 100 points.
Table 1.
Measurement and Scoring of Life's Essential 8
| Cardiovascular health metric | Method of measurement | Scoring | |
|---|---|---|---|
| Diet | 2‐ to 24‐h recalls, intakes averaged. DASH score calculated as described. 12 | Points | Quantile of DASH score |
| 100 | ≥95th percentile | ||
| 80 | 75th–94th | ||
| 50 | 50th–74th | ||
| 25 | 25th–49th | ||
| 0 | 1st–24th | ||
| Physical activity | NHANES physical activity questionnaire, leisure min/wk | Points | Minutes/week |
| 100 | ≥150 | ||
| 90 | 120–149 | ||
| 80 | 90–119 | ||
| 60 | 60–89 | ||
| 40 | 30–59 | ||
| 20 | 1–29 | ||
| 0 | 0 | ||
| Smoking | NHANES smoking questionnaire | Points | Status |
| 100 | Never smoker | ||
| 75 | Quit ≥5 y | ||
| 50 | Quit 1 to <5 y | ||
| 25 | Quit <1 y, or current nicotine delivery system use | ||
| 0 | Current smoker | ||
| Subtract 20 (if score ≥25) for living with active indoor smoker | |||
| Sleep |
2011 and 2013 cycles: average sleep per night 2015 and 2017 cycles: average weekday sleep per night |
Points | Hours of sleep |
| 100 | 7 to <9 | ||
| 90 | 9 to <10 | ||
| 70 | 6 to <7 | ||
| 40 | 5 to <6 or ≥10 | ||
| 20 | 4 to <5 | ||
| 0 | <4 | ||
| Body mass index | Weight in kg/height in m squared | Points | kg/m2 |
| Non‐Asian Americans | |||
| 100 | <25 | ||
| 70 | 25.0–29.9 | ||
| 30 | 30.0–34.9 | ||
| 15 | 35.0–39.9 | ||
| 0 | ≥40.0 | ||
| Asian Americans | |||
| 100 | <23.0 | ||
| 70 | 23.0–24.9 | ||
| 50 | 25.0–29.9 | ||
| 25 | 30.0–34.9 | ||
| 0 | ≥35.0 | ||
| Non‐HDL‐c | Enzymatically measured total cholesterol minus HDL‐c | Points | Non‐HDL‐c, mg/dL |
| 100 | <130 | ||
| 60 | 130–159 | ||
| 40 | 160–189 | ||
| 20 | 190–219 | ||
| 0 | ≥220 | ||
| If drug‐treated level, subtract 20 (if score ≥20) | |||
| Blood glucose | Glycated hemoglobin | Points | % |
| 100 | <5.7, no diabetes | ||
| 60 | 5.7–6.4, no diabetes | ||
| 40 | <7.0, with diabetes | ||
| 30 | 7.0–7.9, with diabetes | ||
| 20 | 8.0–8.9, with diabetes | ||
| 10 | 9.0–9.9, with diabetes | ||
| 0 | ≥10.0, with diabetes | ||
| Blood pressure | Appropriately measured systolic and diastolic blood pressure, mm Hg | Points | mm Hg |
| 100 | <120/<80 | ||
| 75 | 120–129/<80 | ||
| 50 | 130–139 or 80–89 | ||
| 25 | 140–159 or 90–99 | ||
| 0 | ≥160 or ≥100 | ||
| If drug‐treated level, subtract 20 (if score ≥20) | |||
The table is adapted from Lloyd‐Jones et al 7 with permission. Copyright © 2022 the American Heart Association, Inc.
DASH indicates Dietary Approaches to Stop Hypertension; HDL‐c, high‐density lipoprotein cholesterol; and NHANES, National Health and Nutrition Examination Survey.
Blood Pressure
Blood pressure was measured a minimum of 3 times, with a fourth measure taken if necessary, after 5 minutes' seated rest by physician examiners, per NHANES protocol. The average of all measurements was used in this analysis, after removing 0 values for diastolic blood pressure. Blood pressure scores ranged from 0 to 100, as described in Table 1.
Smoking
Smoking status was self‐reported through the NHANES smoking (SMQ) questionnaire, which probed for use of cigarettes, pipes, hookah, chewing tobacco, snuff, and other smokeless tobacco. All current users of tobacco received 0 points. If participants reported quitting, they received between 25 and 75 points, depending on how long it had been since they quit, as described in Table 1. Participants who never smoked received 100 points. For the 2013 to 2017 cycles, e‐cigarette use resulted in a subtraction of 20 points (if the scores were 20 or more). The 2011 cycle does not include e‐cigarette data, but e‐cigarette use was rare at that time.
Physical Activity
Weekly leisure moderate physical activity bouts were multiplied by bout duration in minutes. Weekly leisure vigorous physical activity bouts were multiplied by vigorous bout duration in minutes. These values were added together with the sum equaling weekly physical activity minutes. Greater than or equal to 150 physical activity minutes received 100 points, and 0 physical activity minutes was scored as 0 points. Values in between 0 and 150 minutes received scores between 0 and 100, as described in Table 1.
Diet
Diet was scored based on the Dietary Approaches to Stop Hypertension score, as developed by Fung et al. 12 The diet criteria were scored from 2 days' dietary recall data (averaged). The first recall was collected in person at the Mobile Examination Center. The second was collected over the phone 3 to 10 days later. Cup and ounce equivalents for the requisite food groups were obtained from the US Department of Agriculture Agricultural Research Service. 13 Intake levels were then adjusted for caloric targets for each age/sex group (Table S2). The US Department of Agriculture did not report low‐fat dairy, so total dairy was used. The US Department of Agriculture did not report sugar‐sweetened beverage consumption, so kilocalories from sugar‐sweetened beverages were averaged from the 2 days' recall. Once the Dietary Approaches to Stop Hypertension score was calculated, it was converted to LE8 points based on quantiles, as described in Table 1.
Cholesterol
Total cholesterol (measured enzymatically by hydrolyzing cholesterol esters and producing H2O2, which was then quantified chromatically with paraquinone), high‐density lipoprotein cholesterol concentration, and self‐reported use of hypercholesterolemia medications were used to calculate the cholesterol score. Non‐high‐density lipoprotein cholesterol cholesterol (total cholesterol minus high‐density lipoprotein cholesterol) <130 mg/dL without the use of medication was considered optimal (100 points). Non‐high‐density lipoprotein cholesterol of 220 mg/dL or more received 0 points. Values between 130 and 220 mg/dL received scores between 0 and 100, as described in Table 1.
Blood Glucose
The blood glucose score was based on diabetes status (self‐reported diagnosis, hemoglobin A1c [HbA1c] ≥6.5, or use of diabetes medication) and HbA1c. HbA1c was measured using high‐performance liquid chromatography. An HbA1c of <5.7% in the absence of diabetes received 100 points. For people with diagnosed diabetes, the highest score achievable was 40 points (HbA1c of <7.0%). Participants with an HbA1c ≥10.0% received 0 points. Values of HbA1c between 7.0% and 10.0% received scores between 0 and 40, as described in Table 1.
Sleep
Hours of average weekday sleep was used for cycles 2015 and 2017, and average sleep per night was used for cycles 2011 and 2013. Both were measured with the NHANES Sleep Disorders questionnaire. Optimal sleep was 7 to <9 hours per night (100 points), and 0 points were awarded for sleep <4 hours per night. Other sleep durations received points between 0 and 100, as described in Table 1.
Demographic Variables (Covariates)
Race and Ethnicity
Race and ethnicity were self‐reported from the options non‐Hispanic White, non‐Hispanic Black, non‐Hispanic Asian, non‐Hispanic Other, Mexican American, and Other Hispanic. For this analysis, participants who identified as non‐Hispanic Other were excluded, and participants who identified as Mexican American or Other Hispanic were combined into the group Hispanic.
Age
Age at time of survey was calculated in years from the participant's self‐reported or imputed date of birth. Participants >80 years of age were coded as 80 to minimize disclosure risk.
Sex
Sex was self‐reported at the time of interview, with male or female being the only options.
Statistical Analysis
Our conceptual model is shown in Figure S2. Sample characteristics are reported in Table 2 and Table S3 as counts of observations and the number and percentage of US adults those observations represent, based on the provided sample weights. Linear regression was used to quantify the association of SES components with LE8 score. An interaction term was placed in the model to test the interaction of race and ethnicity with SES in the association with LE8 score. Models were fit with an interaction term of racial and ethnic group with each SES component in turn. Univariate models contained only the race×SES variable interaction term describing LE8 score. Age‐adjusted models contained the interaction term and age. Multivariable models were adjusted for age, sex, and all SES variables not included in the interaction term (Table S4). To determine if the interaction term improved model fit, likelihood ratio tests were performed on models with and without the interaction term. Predicted values were calculated from the age‐adjusted models that included the interaction term, with age held constant at the median. These values are presented in Figure 1. Sensitivity analyses were performed on data imputed with the mice() function in R using the cart method (Table S5). Additional sensitivity analyses were performed on data excluding participants with a history of CVD (heart failure, heart attack, stroke, or coronary heart disease; Table S6). All analyses were performed accounting for NHANES sample weights, primary sampling units, and strata in R using the survey package. 14 , 15 , 16 , 17 , 18 Statistical analyses were performed in R version 4.0.3 (R Foundation for Statistical Computing, Vienna, Austria). Statistical significance for all analyses was defined as 2‐sided alpha <0.05 for main effects of the models and alpha <0.1 for interaction terms. 19
Table 2.
NHANES Observations, Weighted n, and Weighted Percentage of Sociodemographic Variables and Cardiovascular Health Scores by Racial and Ethnic Group
| NH White | NH Black | NH Asian | Hispanic | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Obs | No. | % | Obs | No. | % | Obs | No. | % | Obs | No. | % | |
| Age | ||||||||||||
| 20–30 y | 893 | 23 M | 59 | 565 | 5.1 M | 13 | 328 | 2.6 M | 7 | 592 | 8 M | 21 |
| 31–50 y | 1794 | 42 M | 64 | 958 | 7.3 M | 11 | 590 | 4 M | 6 | 1095 | 12 M | 18 |
| 51–65 y | 1404 | 39 M | 74 | 982 | 5.4 M | 10 | 378 | 2.4 M | 5 | 955 | 5.7 M | 11 |
| 66+ y | 1736 | 28 M | 83 | 564 | 2.3 M | 7 | 174 | 1 M | 3 | 521 | 2.3 M | 7 |
| Income/poverty line | ||||||||||||
| 0.00–1.00 | 915 | 13 M | 49 | 771 | 5.2 M | 20 | 169 | 1.3 M | 5 | 899 | 7 M | 27 |
| 1.01–2.00 | 1582 | 24 M | 60 | 820 | 5.5 M | 14 | 209 | 1.4 M | 4 | 977 | 8.6 M | 22 |
| 2.01–3.00 | 860 | 20 M | 69 | 500 | 3.1 M | 11 | 204 | 1.4 M | 5 | 502 | 4.3 M | 15 |
| 3.01–4.00 | 654 | 17 M | 71 | 345 | 2.3 M | 9 | 222 | 1.6 M | 6 | 310 | 3.4 M | 14 |
| 4.01–5.00 | 1816 | 59 M | 82 | 633 | 4.1 M | 6 | 666 | 4.4 M | 6 | 475 | 4.6 M | 6 |
| Employment status | ||||||||||||
| Disabled/health | 547 | 8.7 M | 67 | 344 | 2.1 M | 16 | 27 | 0.18 M | 1 | 270 | 2 M | 15 |
| Employed | 3048 | 81 M | 68 | 1738 | 12 M | 10 | 1014 | 7 M | 6 | 1864 | 19 M | 16 |
| Homemaker | 273 | 6.3 M | 63 | 95 | 0.61 M | 6 | 124 | 0.85 M | 9 | 314 | 2.3 M | 23 |
| Retired | 1555 | 27 M | 84 | 538 | 2.4 M | 7 | 160 | 0.98 M | 3 | 418 | 2 M | 6 |
| Student | 70 | 1.6 M | 50 | 64 | 0.5 M | 16 | 64 | 0.49 M | 16 | 45 | 0.59 M | 19 |
| Unemployed | 334 | 6.6 M | 56 | 290 | 2.2 M | 19 | 81 | 0.57 M | 5 | 252 | 2.3 M | 20 |
| Education | ||||||||||||
| High school or less | 2086 | 40 M | 61 | 1337 | 8.6 M | 13 | 264 | 2 M | 3 | 1905 | 15 M | 23 |
| Some college | 2053 | 44 M | 71 | 1113 | 7.5 M | 12 | 301 | 2.2 M | 4 | 833 | 8.2 M | 13 |
| College+ | 1688 | 48 M | 77 | 619 | 4.1 M | 7 | 905 | 6 M | 10 | 425 | 4.2 M | 7 |
| Health insurance | ||||||||||||
| Combination | 1292 | 22 M | 84 | 426 | 2 M | 7 | 83 | 0.53 M | 2 | 307 | 1.7 M | 6 |
| Medicaid | 345 | 5.4 M | 48 | 378 | 2.9 M | 25 | 81 | 0.57 M | 5 | 294 | 2.5 M | 22 |
| Medicare | 586 | 9.8 M | 77 | 276 | 1.2 M | 10 | 81 | 0.49 M | 4 | 265 | 1.2 M | 9 |
| Military | 119 | 2.3 M | 70 | 86 | 0.58 M | 17 | 14 | 0.14 M | 4 | 28 | 0.26 M | 8 |
| Other | 267 | 5.8 M | 59 | 203 | 1.4 M | 15 | 89 | 0.73 M | 7 | 214 | 1.8 M | 19 |
| Private | 2477 | 72 M | 74 | 1140 | 7.8 M | 8 | 926 | 6.2 M | 6 | 1085 | 11 M | 11 |
| Uninsured | 741 | 14 M | 49 | 560 | 4.4 M | 15 | 196 | 1.4 M | 5 | 970 | 9.3 M | 32 |
| Sex | ||||||||||||
| Female | 2954 | 67 M | 69 | 1626 | 11 M | 11 | 728 | 5.1 M | 5 | 1682 | 14 M | 14 |
| Male | 2873 | 65 M | 70 | 1443 | 9.1 M | 10 | 742 | 4.9 M | 5 | 1481 | 14 M | 15 |
| Life's Essential 8 score | ||||||||||||
| Low (0–49) | 1204 | 22 M | 68 | 822 | 4.9 M | 16 | 111 | 0.73 M | 2 | 615 | 4.5 M | 14 |
| Moderate (50–79) | 3630 | 82 M | 68 | 1964 | 13 M | 11 | 908 | 6.3 M | 5 | 2118 | 18 M | 15 |
| High (80–100) | 993 | 29 M | 74 | 283 | 2.1 M | 5 | 451 | 3.1 M | 8 | 430 | 5 M | 13 |
% indicates weighted percentage; disabled/health, people out of work because of disability or health reasons; M, millions; No., weighted number of US adults represented by observations; NH, non‐Hispanic; NHANES, National Health and Nutrition Examination Survey; and Obs, observations.
Figure 1. Predicted Life's Essential 8 values for each level of socioeconomic status with age held constant at the median (48 years).
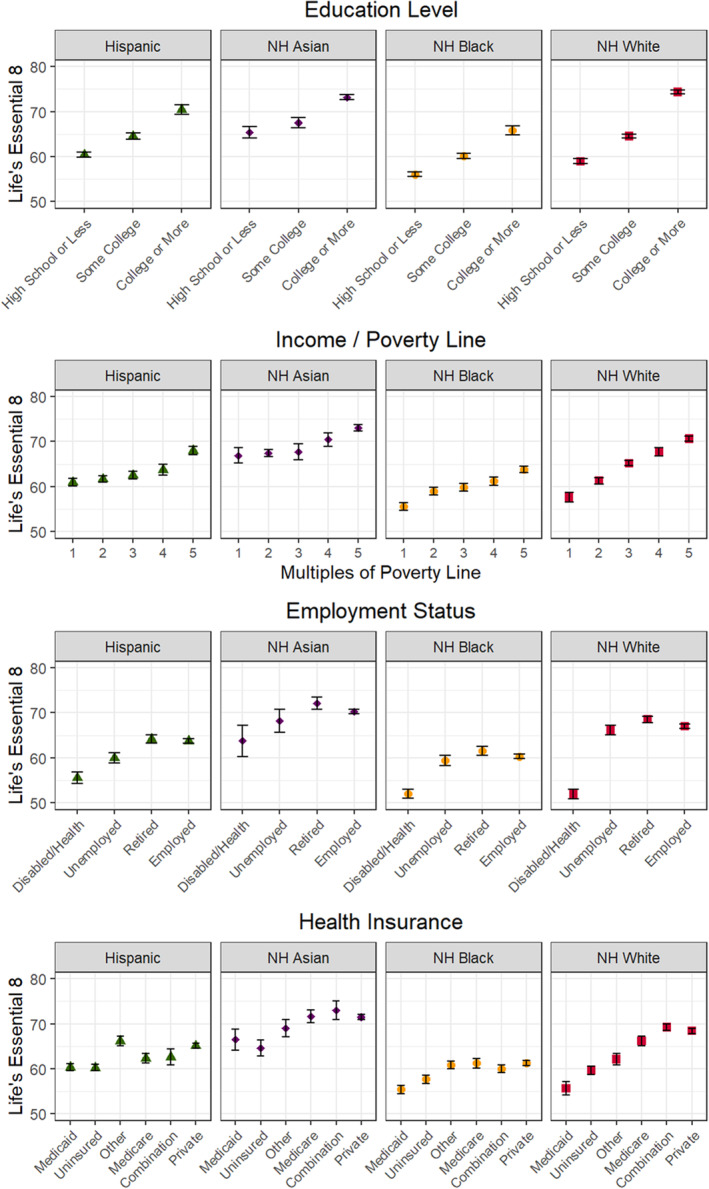
Predicted Life's Essential 8 scores are from models adjusted for age. Age was held constant at the median (48 years) in predicting the Life's Essential 8 scores from the models. Error bars represent the estimate±SE. Disabled/health indicates people out of work because of disability or health reasons. Interpretation: non‐Hispanic White Americans have the greatest variability in predicted Life's Essential 8 scores across levels of socioeconomic status variables. NH indicates non‐Hispanic.
RESULTS
Sample Characteristics
The overall weighted sample (n=13 529) was 15% HA, 11% NHBA, 5% NHAA, 69% NHWA, 49% male, and representative of the United States' adult population. Median age was 48 years. Table 2 shows weighted sample characteristics by racial and ethnic group. The least common type of insurance was military insurance, and the least common occupation was student (student option presented only to those who did not work). NHWA were underrepresented in the low CVH category (LE8 scores from 0–49), whereas NHBA were overrepresented in the low CVH category. In addition, NHAA were overrepresented in the high CVH category (LE8 scores from 80–100).
Table S3 lists the weighted sample characteristics by racial and ethnic group and LE8 category (low, moderate, or high CVH). The unadjusted numbers show the decreasing prevalence of participants in the low CVH category as income and education increase, and this decreasing prevalence had the greatest magnitude among NHWA.
Age‐Adjusted Predicted Life's Essential 8 Scores
Figure 1 shows the age‐adjusted variation in LE8 scores with each of the 4 SES metrics by race and ethnicity. For each SES metric, the greatest variation in LE8 scores was seen among NHWA. For example, the spread between LE8 scores seen between levels of employment status among NHWA is 17 points. Among NHBA, the employment‐level‐based variation in LE8 scores is only 10 points.
Likelihood Ratio Tests
All likelihood ratio tests for the interaction term of race×SES factor (education, income, employment and health insurance) in unadjusted, age‐adjusted, and multivariable models yielded P values less than 0.001. To illustrate how the association of SES factor with LE8 score varies by race and ethnicity, we describe the individual interaction terms for each nonmajority group compared with the majority group in the text that follows.
Education
In Table S4 and Figure 2, when comparing participants with a college degree or more to high school or less, all racial and ethnic groups had a higher LE8 score with college education compared with high school or less in age‐adjusted models (all P<0.001). NHWA had a greater magnitude of association of college education versus high school or less with LE8 compared with NHBA, HA, and NHAA (all P for interactions <0.001). As shown in Figure 2 and Table S4, the change in LE8 scores associated with college or more versus high school or less was highest in NHWA (+15.4 [95% CI, 13.9–16.8]), followed by HA (+10.0 [95% CI, 7.5–12.5]), NHBA (+9.7 [95% CI, 7.8–11.7]), and NHAA (+7.7 [95% CI, 5.0–10.5]).
Figure 2. The association of education level with Life's Essential 8 cardiovascular health scores by race and ethnicity, with race and ethnicity interaction P values listed.
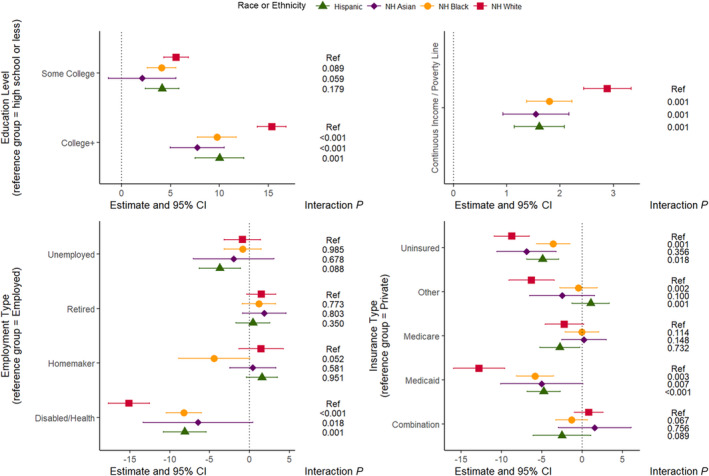
Plotted estimates and CI are from age‐adjusted linear models (Table S4). Interaction P values (interaction P) are from race×socioeconomic status factor interaction terms in the age‐adjusted linear models. Interpretation: there is a significantly greater magnitude of positive association of education level with Life's Essential 8 among non‐Hispanic White Americans than other groups (likelihood ratio test P<0.001). There is a significantly greater magnitude of positive association of income level with Life's Essential 8 among non‐Hispanic White Americans than other groups (likelihood ratio test P<0.001). There is a significantly greater magnitude of negative association of having a disability or health issue that prevents work with Life's Essential 8 among non‐Hispanic White Americans than other groups (likelihood ratio test P<0.001). There is a significantly greater magnitude of negative association of having Medicaid insurance with Life's Essential 8 among non‐Hispanic White Americans than other groups (likelihood ratio test P<0.001). NH indicates non‐Hispanic.
Income
As PIR increases, all racial and ethnic groups have higher LE8 scores (P<0.001) in age‐adjusted models. Compared with NHBA, HA, and NHAA, NHWA had a greater magnitude of association of PIR with LE8. As shown in Figure 2 and Table S4, the increase in LE8 associated with 1‐point increase in PIR was highest in NHWA (+2.9 [95% CI, 2.4–3.3]), followed by NHBA (+1.8 [95% CI, 1.4–2.2], interaction P=0.001), NHAA (+1.5 [95% CI, 0.9–2.2], interaction P=0.001), and HA (+1.6 [95% CI, 1.1–2.1], interaction P=0.001).
Employment
Compared with NHBA, HA, and NHAA, NHWA have a greater magnitude of association of disability status with LE8, as shown in Figure 2 and Table S4. Compared with employed people, NHWA with a disability or health condition that prevents them from working have a more negative associated change in LE8 scores (−15.1 [95% CI, −17.7 to −12.5]) than NHBA (−8.2 [95% CI, −10.5 to −6.0]), HA (−8.1 [95% CI, −10.8 to −5.4]), or NHAA (−6.4 [95% CI, −13.3 to 0.4]) (all interactions P<0.05).
Health Insurance
Compared with racial and ethnic minority groups, NHWA had a greater magnitude of association between some insurance statuses and LE8 score, as shown in Figure 2 and Table S4. NHWA with Medicaid insurance compared with private insurance had a greater magnitude of negative association with LE8 scores (−12.8 [95% CI, −16.0 to −9.6]) compared with NHAA (−5.0 [95% CI, −10.1 to 0.1]; interaction P=0.007), HA (−4.8 [95% CI, −6.9 to −2.7]; interaction P<0.001), or NHBA (−5.9 [95% CI, −8.1 to −3.6], interaction P=0.003).
The other findings were not consistent across racial and ethnic minority groups. For NHBA and HA, there was a lower magnitude of association of uninsured versus private insurance with LE8 scores than NHWA (interaction P<0.05).
Sensitivity Analyses
Sensitivity analyses performed with imputed data for missing variables (n=18 417) and excluding individuals with a history of CVD (n=12 157), yielded similar findings as the main analysis (Tables S5 and S6, respectively).
DISCUSSION
Summary
In this novel study comparing 4 SES measures with CVH in a diverse, nationally representative sample, the association of SES with LE8 was significant across racial and ethnic groups but had the greatest magnitude of association among NHWA. NHWA had greater positive associations of higher income and education with CVH scores than racial and ethnic minority groups but also had greater negative associations of disability (compared with employed) and of Medicaid (compared with private insurance) with CVH scores. The findings suggest that although eliminating inequities in SES is a critical component for CVD primordial and primary prevention, in order to advance CVH equity, addressing additional social determinants of health (SDoH) may be necessary.
These results are concordant with the only study with similar methodology known to the authors. Johnson et al 20 observed a lower magnitude of association between education and Life's Simple 7 CVH score among racial and ethnic minority groups in NHANES data, but this study did not assess other measures of SES. There are studies that have evaluated the interaction of race and SES with other health‐related outcomes. An NHANES analysis of hypertension, diabetes, and obesity rates between NHWA and NHBA among SES strata found that racial disparities in the prevalence of obesity were worst in higher income and education strata. 21 An analysis of the interaction of race and socioeconomic position describing a count of doctor‐diagnosed diseases among NHBA and NHWA in Tennessee found some socioeconomic position factors were differentially associated with disease among NHWA and NHBA, with significant associations among NHWA and nonsignificant associations among NHBA. 22
Mechanisms
The lower magnitude of positive association of education and income with LE8 scores observed in racial and ethnic minority groups could be described as diminishing returns 23 and may be due to a number of factors including racism, the wealth gap, stress, medical mistrust, and the opportunity gap.
Racism
The different forms of racism (structural, institutional, interpersonal, and internalized) all contribute to the racial and ethnic health disparities pervasive in the United States. 24 Structural and institutional racism in the past and present created and perpetuate the wealth and opportunity gaps between some racial and ethnic minority groups and NHWA. All forms of racism contribute to the perceived racism and resultant chronic stress that racial and ethnic minority groups experience on a daily basis. The following paragraphs provide more detail about the effects of racism on the health of racial and ethnic minority groups.
The Wealth Gap
Net worth, liabilities subtracted from assets, is a frequently used definition of personal wealth. This metric is used to track the widening disparity between wealth trends among NHWA and some racial and ethnic minority groups. 25 , 26 Many attempts to explain this disparity have been made. The best supported theories include the racial income gap that persists even after accounting for education and occupation, 27 lower return on investments, especially housing investments, 28 lower rates and amounts of intergenerational transfers of wealth among racial and ethnic minority groups, 29 , 30 and historical forms of legal discrimination, like redlining. 31 Whatever the cause, there persists a wealth gap between some racial and ethnic minority groups and NHWA even when the SES factors analyzed in this article are considered. The wealth gap may partially explain the lower achievement of ideal LE8 metrics at higher incomes and education levels of racial and ethnic minority groups compared with NHWA, as wealth is associated with greater CVH. 32
Psychosocial Stress
Stress, defined by Cohen et al as the process in which the environmental demands tax or exceed the adaptive capacity of an organism… 33 can have positive effects on the body, if experienced in moderation. 34 Prolonged stress, as in low SES, 35 perceived racial discrimination, 36 or sleep deprivation, 37 leads to negative physiological changes collectively referred to as weathering by some 38 and allostatic load by others. 34 By either name, racial and ethnic minority groups have higher stress‐induced physiological damage than NHWA. 35 The accumulation of the stresses of being a member of a racial and ethnic minority group may explain why NHBA have greater biological age (derived from a number of biomarkers) than chronological age (years since birth), whereas NHWA have lower biological age than chronological age. 39 Another reputed consequence of this stress is the accelerated shortening of telomeres observed in NHBA compared with NHWA even when controlling for initial telomere length at birth. 40 Weathering, or allostatic load, may partially explain why the difference in LE8 scores between higher and lower SES groups was greater among NHWA than racial and ethnic minority groups.
Medical Mistrust
NHBA and HA are more likely to mistrust the health care system than NHWA, 41 especially if health care providers are not racially concordant. 42 People with medical mistrust are less likely to follow medical advice and fill prescriptions and more likely to miss follow‐up appointments and postpone needed care. 43 More research is needed on the association of medical mistrust with health outcomes and risk factors like LE8.
Opportunity Gap
Racial and ethnic minority groups are more likely than NHWA to have reading levels lower than their level of completed education. 44 This achievement gap, or more justly, opportunity gap, has been posited to be associated with the racism‐related segregation and selective underfunding of schools (resource inequity) throughout history and today. 45 The opportunity gap may be yet another explanation for the observed diminishing returns of higher education and other aspects of SES on racial and ethnic minority groups in this study.
Access to Care
All of the data analyzed in this report was collected after the passage of the Affordable Care Act in 2010. The Affordable Care Act reduced, but did not eliminate, health care access disparities by race and ethnicity. 46 NHBA and HA are still more likely to be uninsured or underinsured than NHWA, even after adjustment for sociodemographic factors, including education. 46 Similarly, the Affordable Care Act narrowed access disparities by SES, even when adjusting for race and ethnicity. 47 More research is needed to determine the interaction between race and ethnicity and SES describing health care access. Such an interaction may partially explain the present results.
Other Potential Mechanisms: Rural–Urban Disparities, Medication Adherence, Other SDoH
Rural residents have poorer health and access to health care than urban residents, 48 and rural residents are more likely to be NHWA, older, living with a disability, unemployed, and of low SES than urban residents. 49 This may partially explain why NHWA with Medicaid (compared with private insurance) have relatively poorer LE8 scores than racial and ethnic minority groups with Medicaid (compared to private insurance). A separate potential reason for this phenomenon is that Medicaid covers medications completely, which may increase medication adherence in racial and ethnic minority groups more than NHWA, who have the highest rates of medication adherence. 50 More research is needed to describe the effect of Medicaid participation on medication adherence by race. Finally, although SES factors are SDoH, there are many other SDoH that were not analyzed. 51 These unmeasured factors may be correlated with the exposures and outcomes in this analysis. 8 Although outside the context of the current study, further research is needed to examine the effect of other SDoH on LE8 achievement.
Strengths and Limitations
The strengths of this study include the use of a nationally representative sample, standardized, census‐based definitions of race and ethnicity, a validated physical activity questionnaire, gold standard ascertainment of diet (24‐hour recall), and reliably measured laboratory values. Results should be considered in light of a few limitations. The study is cross‐sectional in design, so causation can neither be ascertained nor inferred. NHANES lacks a question that assesses wealth consistently across years, so the mediation of wealth in SES relationships with LE8 by race could not be assessed. Similarly, racism (perceived or insidious) was not measured, thus the nature of its effects is only theorized. People who identify as Indigenous or mixed race are not covered in this analysis. The possibility of systematic measurement error across racial and ethnic groups in self‐reported variables exists. Finally, individuals of different national origin and immigration status are considered together within the 4 racial and ethnic groups described. Due to power considerations, these groups could not be further subdivided.
CONCLUSIONS
The magnitude of association of SES with LE8 is greatest in NHWA. NHWA have greater increases in LE8 with higher education and income and greater decreases in LE8 under Medicaid and disability than racial and ethnic minority groups. The former may be an effect of the wealth gap, psychosocial stress experienced by racial and ethnic minority groups due to racism, the opportunity gap, medical mistrust, and differential access to care. The latter may be due to the psychosocial resilience of racial and ethnic minority groups, rural–urban disparities, and differences in medication adherence in Medicaid. The findings suggest cardiovascular disease primordial and primary prevention efforts should not rely solely on the closing of SES disparities by racial and ethnic group but must additionally address other SDoH that drive CVH inequities.
Sources of Funding
The Robert Wood Johnson Foundation (Harold Amos Medical Faculty Development Program ID# 76236 [J.J.J.]) and the American Heart Association Strategically Focused Research Network on Biologic Pathways of Chronic Psychosocial Stressors on Cardiovascular Health (J.J.J.). This publication was supported, in part, by the National Center for Advancing Translational Sciences of the National Institutes of Health under grant number UL1TR002733. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosures
None.
Supporting information
Tables S1–S6
Figures S1–S2
This article was sent to Mahasin S. Mujahid, PhD, MS, FAHA, Associate Editor, for review by expert referees, editorial decision, and final disposition.
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.122.029254
For Sources of Funding and Disclosures, see page 11.
References
- 1. Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, Boehme AK, Buxton AE, Carson AP, Commodore‐Mensah Y, et al. Heart disease and stroke statistics—2022 update: a report from the American Heart Association. Circulation. 2022;145:e153–e639. doi: 10.1161/CIR.0000000000001052 [DOI] [PubMed] [Google Scholar]
- 2. Carnethon MR, Pu J, Howard G, Albert MA, Anderson CAM, Bertoni AG, Mujahid MS, Palaniappan L, Taylor HA, Willis M, et al. Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136:e393–e423. doi: 10.1161/CIR.0000000000000534 [DOI] [PubMed] [Google Scholar]
- 3. Jose PO, Frank ATH, Kapphahn KI, Goldstein BA, Eggleston K, Hastings KG, Cullen MR, Palaniappan LP. Cardiovascular disease mortality in Asian Americans. J Am Coll Cardiol. 2014;64:2486–2494. doi: 10.1016/j.jacc.2014.08.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Daviglus ML, Talavera GA, Avilés‐Santa ML, Allison M, Cai J, Criqui MH, Gellman M, Giachello AL, Gouskova N, Kaplan RC, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308:1775–1784. doi: 10.1001/jama.2012.14517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rodriguez CJ, Allison M, Daviglus ML, Isasi CR, Keller C, Leira EC, Palaniappan L, Piña IL, Ramirez SM, Rodriguez B, et al. Status of cardiovascular disease and stroke in Hispanics/Latinos in the United States. Circulation. 2014;130:593–625. doi: 10.1161/CIR.0000000000000071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Capewell S, Ford ES, Croft JB, Critchley JA, Greenlund KJ, Labarthe DR. Cardiovascular risk factor trends and potential for reducing coronary heart disease mortality in the United States of America. Bull World Health Organ. 2010;88:120–130. doi: 10.2471/BLT.08.057885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lloyd‐Jones DM, Allen NB, Anderson CAM, Black T, Brewer LC, Foraker RE, Grandner MA, Lavretsky H, Perak AM, Sharma G, et al. Life's Essential 8: updating and enhancing the American Heart Association's construct of cardiovascular health: a presidential advisory from the American Heart Association. Circulation. 2022;146:e18–e43. doi: 10.1161/CIR.0000000000001078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Egan BM, Li J, Sutherland SE, Jones DW, Ferdinand KC, Hong Y, Sanchez E. Sociodemographic determinants of Life's Simple 7: implications for achieving cardiovascular health and health equity goals. Ethn Dis. 2020;30:637–650. doi: 10.18865/ed.30.4.637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lloyd‐Jones DM, Ning H, Labarthe D, Brewer L, Sharma G, Rosamond W, Foraker RE, Black T, Grandner MA, Allen NB, et al. Status of cardiovascular health in US adults and children using the American Heart Association's new “Life's Essential 8” metrics: prevalence estimates from the National Health and Nutrition Examination Survey (NHANES), 2013–2018. Circulation. 2022;146:822–835. doi: 10.1161/CIRCULATIONAHA.122.060911 [DOI] [PubMed] [Google Scholar]
- 10. Azap RA, Nolan TS, Gray DM, Lawson K, Gregory J, Capers Q, Odei JB, Joseph JJ. Association of socioeconomic status with ideal cardiovascular health in Black men. J Am Heart Assoc. 2021;10:e020184. doi: 10.1161/JAHA.120.020184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. NHANES tutorials . Centers for Disease Control and Prevention. 2020. Accessed December 21, 2021. https://wwwn.cdc.gov/nchs/nhanes/tutorials/default.aspx
- 12. Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH‐style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168:713–720. doi: 10.1001/archinte.168.7.713 [DOI] [PubMed] [Google Scholar]
- 13. Food Patterns Equivalents Database . USDA Agricultural Research Service. 2021. Accessed December 8, 2021. https://www.ars.usda.gov/northeast‐area/beltsville‐md‐bhnrc/beltsville‐human‐nutrition‐research‐center/food‐surveys‐research‐group/docs/fped‐databases/
- 14. R Core Team . R: a language and environment for statistical computing. Version 4.2.3. 2023. Accessed March 16, 2023. https://www.R‐project.org/
- 15. Lumley T. Survey: analysis of complex survey samples. Version 4.1.1. 2021. Accessed July 19, 2021. https://cran.r‐project.org/web/packages/survey/index.html
- 16. Lumley T. Analysis of complex survey samples. J Stat Softw. 2004;9:1–19. doi: 10.18637/jss.v009.i08 [DOI] [Google Scholar]
- 17. Lumley T. Complex Surveys: A Guide to Analysis Using R. John Wiley & Sons; 2010. doi: 10.1002/9780470580066 [DOI] [Google Scholar]
- 18. Lumley T. svyVGAM: design‐based inference in vector generalised linear models. Version 1.0. 2021. Accessed March 5, 2021. https://CRAN.R‐project.org/package=svyVGAM
- 19. Joseph JJ, Echouffo Tcheugui JB, Effoe VS, Hsueh WA, Allison MA, Golden SH. Renin‐angiotensin‐aldosterone system, glucose metabolism and incident type 2 diabetes mellitus: MESA. J Am Heart Assoc. 2018;7:e009890. doi: 10.1161/JAHA.118.009890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Johnson AE, Herbert BM, Stokes N, Brooks MM, Needham BL, Magnani JW. Educational attainment, race, and ethnicity as predictors for ideal cardiovascular health: from the National Health and Nutrition Examination Survey. J Am Heart Assoc. 2022;11:e023438. doi: 10.1161/JAHA.121.023438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bell CN, Thorpe RJ, Bowie JV, LaVeist TA. Race disparities in cardiovascular disease risk factors within socioeconomic status strata. Ann Epidemiol. 2018;28:147–152. doi: 10.1016/j.annepidem.2017.12.007 [DOI] [PubMed] [Google Scholar]
- 22. Turner RJ, Brown TN, Hale WB. Race, socioeconomic position, and physical health: a descriptive analysis. J Health Soc Behav. 2017;58:23–36. doi: 10.1177/0022146516687008 [DOI] [PubMed] [Google Scholar]
- 23. Farmer MM, Ferraro KF. Are racial disparities in health conditional on socioeconomic status? Soc Sci Med. 2005;60:191–204. doi: 10.1016/j.socscimed.2004.04.026 [DOI] [PubMed] [Google Scholar]
- 24. Braveman PA, Arkin E, Proctor D, Kauh T, Holm N. Systemic and structural racism: definitions, examples, health damages, and approaches to dismantling. Health Aff (Millwood). 2022;41:171–178. doi: 10.1377/hlthaff.2021.01394 [DOI] [PubMed] [Google Scholar]
- 25. Cobb‐Clark DA, Hildebrand VA. The wealth of Mexican Americans. J Hum Resour. 2006;XLI:841–868. doi: 10.3368/jhr.XLI.4.841 [DOI] [Google Scholar]
- 26. Blau FD, Graham JW. Black‐white differences in wealth and asset composition. Q J Econ. 1990;105:321–339. doi: 10.2307/2937789 [DOI] [Google Scholar]
- 27. Barsky R, Bound J, Charles KK, Lupton JP. Accounting for the Black–white wealth gap. J Am Stat Assoc. 2002;97:663–673. doi: 10.1198/016214502388618401 [DOI] [Google Scholar]
- 28. Krivo LJ, Kaufman RL. Housing and wealth inequality: racial‐ethnic differences in home equity in the United States. Demography. 2004;41:585–605. doi: 10.1353/dem.2004.0023 [DOI] [PubMed] [Google Scholar]
- 29. Avery RB, Rendall MS. Lifetime inheritances of three generations of whites and blacks. Am J Sociol. 2002;107:1300–1346. doi: 10.1086/344840 [DOI] [Google Scholar]
- 30. Conley D. Decomposing the Black‐white wealth gap: the role of parental resources, inheritance, and investment dynamics. Sociol Inq. 2001;71:39–66. doi: 10.1111/j.1475-682X.2001.tb00927.x [DOI] [Google Scholar]
- 31. Traub A, Sullivan L, Meschede T, Shapiro T. The asset value of whiteness: understanding the racial wealth gap. 2017. Accessed September 8, 2022. https://www.demos.org/research/asset‐value‐whiteness‐understanding‐racial‐wealth‐gap
- 32. López‐Cevallos DF, Gonzalez P, Bethel JW, Castañeda SF, Isasi CR, Penedo FJ, Ojeda L, Davis SM, Chirinos DA, Molina KM, et al. Is there a link between wealth and cardiovascular disease risk factors among Hispanic/Latinos? Results from the HCHS/SOL sociocultural ancillary study. Ethn Health. 2018;23:902–913. doi: 10.1080/13557858.2017.1315370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cohen S, Kessler RC, Underwood GL. Measuring Stress: A Guide for Health and Social Scientists. Oxford University Press; 1995. [Google Scholar]
- 34. McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338:171–179. doi: 10.1056/NEJM199801153380307 [DOI] [PubMed] [Google Scholar]
- 35. Bird CE, Seeman T, Escarce JJ, Basurto‐Dávila R, Finch BK, Dubowitz T, Heron M, Hale L, Merkin SS, Weden M, et al. Neighbourhood socioeconomic status and biological ‘wear and tear’ in a nationally representative sample of US adults. J Epidemiol Community Health. 2010;64:860–865. doi: 10.1136/jech.2008.08481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Allen AM, Wang Y, Chae DH, Price MM, Powell W, Steed TC, Rose Black A, Dhabhar FS, Marquez‐Magaña L, Woods‐Giscombe CL. Racial discrimination, the superwoman schema, and allostatic load: exploring an integrative stress‐coping model among African American women. Ann N Y Acad Sci. 2019;1457:104–127. doi: 10.1111/nyas.14188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Nollet M, Wisden W, Franks NP. Sleep deprivation and stress: a reciprocal relationship. Interface Focus. 2020;10:20190092. doi: 10.1098/rsfs.2019.0092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Forde AT, Crookes DM, Suglia SF, Demmer RT. The weathering hypothesis as an explanation for racial disparities in health: a systematic review. Ann Epidemiol. 2019;33:1–18.e3. doi: 10.1016/j.annepidem.2019.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Forrester SN, Zmora R, Schreiner PJ, Jacobs DR, Roger VL, Thorpe RJ, Kiefe CI. Racial differences in the association of accelerated aging with future cardiovascular events and all‐cause mortality: the coronary artery risk development in young adults study, 2007–2018. Ethn Health. 2022;27:997–1009. doi: 10.1080/13557858.2020.1839021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rewak M, Buka S, Prescott J, De Vivo I, Loucks EB, Kawachi I, Non AL, Kubzansky LD. Race‐related health disparities and biological aging: does rate of telomere shortening differ across blacks and whites? Biol Psychol. 2014;99:92–99. doi: 10.1016/j.biopsycho.2014.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bazargan M, Cobb S, Assari S. Discrimination and medical mistrust in a racially and ethnically diverse sample of California adults. Ann Fam Med. 2021;19:4–15. doi: 10.1370/afm.2632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Alsan M, Garrick O, Graziani G. Does diversity matter for health? Experimental evidence from Oakland. Am Econ Rev. 2019;109:4071–4111. doi: 10.1257/aer.20181446 [DOI] [Google Scholar]
- 43. LaVeist TA, Isaac LA, Williams KP. Mistrust of health care organizations is associated with underutilization of health services. Health Serv Res. 2009;44:2093–2105. doi: 10.1111/j.1475-6773.2009.01017.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Manly JJ. Deconstructing race and ethnicity: implications for measurement of health outcomes. Med Care. 2006;44:S10–S16. doi: 10.1097/01.mlr.0000245427.22788.be [DOI] [PubMed] [Google Scholar]
- 45. Noguera PA. Race, education, and the pursuit of equity in the twenty‐first century. In: Noguera P, Pierce J, Ahram R, eds. Race, Equity, and Education: Sixty Years from Brown. Cham: Springer International Publishing; 2016:3–23. doi: 10.1007/978-3-319-23772-5_1 [DOI] [Google Scholar]
- 46. Buchmueller TC, Levy HG. The ACA's impact on racial and ethnic disparities in health insurance coverage and access to care. Health Aff (Millwood). 2020;39:395–402. doi: 10.1377/hlthaff.2019.01394 [DOI] [PubMed] [Google Scholar]
- 47. Griffith K, Evans L, Bor J. The Affordable Care Act reduced socioeconomic disparities In health care access. Health Aff (Millwood). 2017;36:1503–1510. doi: 10.1377/hlthaff.2017.0083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Laditka JN, Laditka SB, Probst JC. Health care access in rural areas: evidence that hospitalization for ambulatory care‐sensitive conditions in the United States may increase with the level of rurality. Health Place. 2009;15:761–770. doi: 10.1016/j.healthplace.2008.12.007 [DOI] [PubMed] [Google Scholar]
- 49. Rural America at a glance: 2019 Edition. US Department of Agriculture. 2019. Accessed July 1, 2022. https://www.ers.usda.gov/webdocs/publications/95341/eib‐212.pdf?v=3310.1
- 50. Rolnick SJ, Pawloski PA, Hedblom BD, Asche SE, Bruzek RJ. Patient characteristics associated with medication adherence. Clin Med Res. 2013;11:54–65. doi: 10.3121/cmr.2013.1113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Social determinants of health. Healthy People 2030. Accessed April 1, 2022. https://health.gov/healthypeople/objectives‐and‐data/social‐determinants‐health
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S6
Figures S1–S2


