Abstract
Background
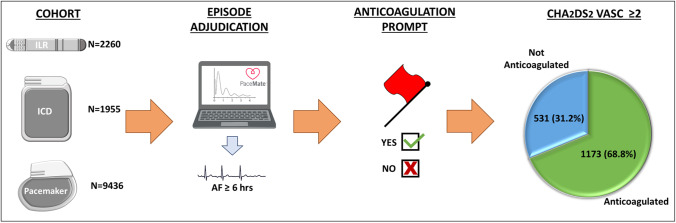
Remote monitoring (RM) can facilitate early detection of subclinical and symptomatic atrial fibrillation (AF), providing an opportunity to evaluate the need for stroke prevention therapies. We aimed to characterize the burden of RM AF alerts and its impact on anticoagulation of patients with device-detected AF.
Methods
Consecutive patients with a cardiac implantable electronic device, at least one AF episode, undergoing RM were included and assigned an estimated minimum CHA2DS2-VASc score based on age and device type. RM was provided via automated software system, providing rapid alert processing by device specialists and systematic, recurrent prompts for anticoagulation.
Results
From 7651 individual, 389,188 AF episodes were identified, 3120 (40.8%) permanent pacemakers, 2260 (29.5%) implantable loop recorders (ILRs), 987 (12.9%) implantable cardioverter defibrillators, 968 (12.7%) cardiac resynchronization therapy (CRT) defibrillators, and 316 (4.1%) CRT pacemakers. ILRs transmitted 48.8% of all AF episodes. At twelve-months, 3404 (44.5%) AF < 6 min, 1367 (17.9%) 6 min–6 h, 1206 (15.8%) 6–24 h, and 1674 (21.9%) ≥ 24 h. A minimum CHA2DS2-VASc score of 2 was assigned to 1704 (63.1%) of the patients with an AF episode of ≥ 6 h, 531 (31.2%) who were not anticoagulated at 12-months, and 1031 (61.6%) patients with an AF episode duration of ≥ 24 h, 290 (28.1%) were not anticoagulated.
Conclusions
Despite being intensively managed via RM software system incorporating cues for anticoagulation, a substantial proportion of patients with increased stroke risk remained unanticoagulated after a device-detected AF episode of significant duration. These data highlight the need for improved clinical response pathways and an integrated care approach to RM.
Trial registration
Australian New Zealand Clinical Trial Registry: ACTRN12620001232921.
Graphical Abstract
Keywords: Atrial fibrillation, Remote monitoring, Anticoagulation, Cardiac implantable electronic device
Introduction
Atrial fibrillation (AF) is associated with a significant risk of ischemic stroke [1]. Device-detected AF has now been correlated with elevated stroke risk [2] independent of the presence or absence of clinical AF symptoms [3]. Anticoagulation reduces both stroke risk and mortality in AF patients. The CHA2DS2-VASc scoring system correlates risk factors to predict the annual stroke risk in patients with non-valvular AF, and guidelines recommend initiation of anticoagulation in patients with a score of ≥ 2 for men and ≥ 3 for women, and consideration of anticoagulation for patients with a score of 1 for men and 2 for women [4].
Over the past decade, remote monitoring (RM) of cardiac implantable electronic devices (CIEDs) has evolved as a management tool and is now a standard component of device follow-up [5, 6]. RM provides physician access to patient/device information in between clinic visits, in the form of both routine transmissions, which act as a surrogate for an in-person device check, and alerts, which may indicate a patient event, programming concern, or device malfunction. RM alerts facilitate early detection of device-detected arrhythmias, including AF, compared with in-clinic follow-up alone [7, 8]. In the absence of RM, AF would be detected only in the event of a routine follow-up, or an unscheduled encounter pertaining to AF symptoms, heart failure, and embolic event or other untoward clinical events [7]. Early recognition of device-detected AF via RM presents an opportunity to implement anticoagulation and initiate rhythm or rate control strategies in both the asymptomatic patient and the symptomatic patient, who has not yet sought medical attention. Institution of such therapies likely has implications for the associated risks of stroke [4] and heart failure [9] in AF patients.
Using a large clinical cohort of patients undergoing RM via an automated system (PaceMate), we characterize the burden of AF episodes in a remote-monitored CIED population. Specifically, we aimed to determine the impact of AF episodes on rates of anticoagulation, in accordance with CHA2DS2-VASc scoring.
Methods
Data source
For this study, the PaceMate™ RM system was utilized. This system is a partially automated, vendor-neutral RM software system. The system presents RM data acquired from all vendors in a standardized format. The database includes all RM alerts transmitted by CIED patients undergoing RM via PaceMate Live™.
For the study protocol, consecutive AF episodes transmitted via RM from March 2019 until February 2020 were assessed. The study was reviewed and approved by the Human Research Ethics Committees of the Central Adelaide Local Health Network and the University of Adelaide. The study was registered with the Australian New Zealand Clinical Trials Registry (ACTRN12620001232921).
Study population
Patients were derived from 26 centers in the United States of America and Australia, with devices from multiple manufacturers including Medtronic, Abbott Medical, Boston Scientific, and Biotronik. All patients, who transmitted at least one AF episode with specified episode duration during the twelve-month window, were included and classified according to age, CIED-type, estimated minimum CHA2DS2-VASc score (details below), and anticoagulation status.
Protocol for analysis of AF alerts
All AF alerts are received and assessed by device specialists certified by the International Board of Heart Rhythm Examiners (IBHRE). PaceMate device specialists are on-call 24 h a day, 7 days a week for immediate analysis (where possible, depending on the burden of RM transmissions queued for analysis) of RM alerts. After alert analysis, a concise written alert summary is transmitted to patient’s relevant clinic, via an integrated web-based interface, which is streamlined to display alerts from all device manufacturers. The management of incoming alerts/episodes on the PaceMate interface is dictated by each clinic, with allocation of their chosen staff member/s (e.g., cardiac technician, nurse, and physician) to routinely check the interface, and escalation to more senior staff (e.g., physician and electrophysiologist) as per the individualized clinic protocol.
Classification of device type
CIED-type was classified as either dual-chamber permanent pacemaker (PPM), dual chamber implantable cardioverter-defibrillator (ICD), cardiac resynchronization therapy defibrillator (CRT-D), cardiac resynchronization therapy pacemaker (CRT-P), or implantable loop recorder (ILR). Single-chamber PPMs, leadless PPMs, and single-chamber ICDs were not included in the analysis.
AF episode duration
AF episodes without an attached episode duration available in the remote transmission were excluded. All remaining AF episodes were classified according to duration. Episodes occurring within a 24-h period were pooled to create a total duration of AF within 24 h. Pooled episodes were then re-classified into one of four pre-specified AF duration windows: (1) less than 6 min during a 24-h period (AF < 6 min), (2) at least 6 min, but less than 6 h during a 24-h period (AF 6 min–6 h), (3) at least 6 h but less than 24 h during a 24-h period (AF 6–24 h), and (4) 24 h or above (AF ≥ 24 h). Patients were then allocated to one of the four AF duration categories, according to their longest pooled episode duration.
Classification of stroke risk
Patient parameters available to estimate CHA2DS2-VASc scores included patient age and the presence of a cardiac resynchronization device consistent with heart failure or left ventricular (LV) dysfunction. The RM database did not contain information regarding patient history of hypertension, diabetes mellitus, stroke, vascular disease, or sex.
For the purposes of the study, given the available parameters, we classified the following patients with an AF burden of at least 6 h over 24 h as having an indication for anticoagulation:
Patients aged ≥ 75 years; minimum CHA2DS2-VASc score of 2, due to their age
Patients aged ≥ 75 years with a CRT-D or CRT-P in situ; minimum CHA2DS2-VASc score of 3, due to accrual of 2 points for age, and a third point for the likely presence of underlying LV dysfunction or heart failure, implied by their CIED-type
Patients aged 65 to 74 years with a CRT-D, or CRT-P in situ; minimum CHA2DS2-VASc score of 2, due to accrual of one point for age, and a second point for the likely presence of LV dysfunction or heart failure, implied by their CIED-type
Patients aged 65 to 74 years; minimum CHA2DS2-VASc score of 1, due to their age
System prompts for anticoagulation and classification of anticoagulation status
Anticoagulation status for each patient was updated following each transmission of an AF episode via bidirectional software system-based communication between PaceMate staff and clinic staff, or by interrogation of the patient’s integrated electronic medical record, which was accessible via the database in some sites. In patients who transmitted an AF episode, whose record did not indicate the current presence of anticoagulation, PaceMate technicians communicated to staff in the relevant clinic the need for consideration of anticoagulation, via the PaceMate web-based interface. Following this communication, clinic staff would respond and the patient’s anticoagulation status would accordingly be updated on the PaceMate user interface. In the absence of a response from clinic staff, PaceMate technicians would continue to re-communicate the anticoagulation query to clinic staff until a response was received, with anticoagulation status clarification. For the purposes of our analysis, anticoagulation status of each patient was as per the PaceMate interface at the close of the 12-month monitoring period.
Statistical analysis
Continuous data are expressed as the mean ± standard deviation or median (1st and 3rd quartiles). Categorical data are presented as absolute values and percentages. Tests for significance were conducted using the chi-squared test or Fisher’s exact test for categorical variables. A p value of ≤ 0.05 was considered significant. All analyses were performed using commercial software (SPSS version 26.0®, SPSS, Inc., Chicago 5 IL, USA).
Results
In total, 416,360 consecutive AF episodes from 7988 patients were transmitted via remote monitoring during the twelve-month window from March 2019 until February 2020. After exclusion of AF episodes of unspecified duration, 389,188 (93.5%) episodes from 7651 (95.8%) individual patients were included in the analysis.
AF alert cohort
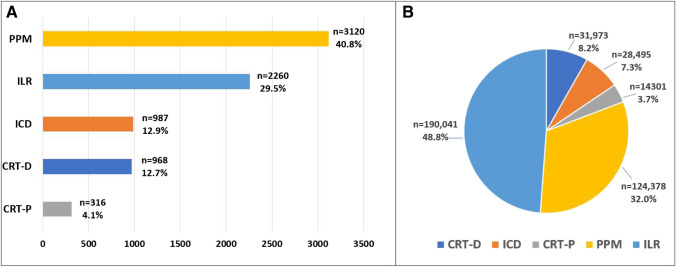
The final AF alert cohort of 7651 patients included 3120 (40.8%) dual-chamber PPMs, 2260 (29.5%) ILRs, 987 (12.9%) dual-chamber ICDs, 968 (12.7%) CRT-Ds, and 316 (4.1%) CRT-Ps (central figure, Fig. 1, Table 1). Of the 389,188 AF episodes transmitted, 190,041 alerts (48.8%) were transmitted by ILRs, 124,378 alerts (32.0%) by PPMs, 31,973 alerts (8.2%) by CRT-Ds, 28,495 alerts (7.3%) by ICDs, and 14,301 alerts (3.7%) by CRT-Ps (Fig. 1).
Fig. 1.
Panel A demonstrates the device types in the cohort. Panel B demonstrates the proportion of AF episodes per device type. PPM, permanent pacemaker; CRT-P, cardiac resynchronization therapy pacemaker; ICD, standard implantable cardioverter defibrillator; CRT-D, cardiac resynchronization therapy defibrillator; ILR, implantable loop recorder
Table 1.
Baseline cohort characteristics
| Device type | Number (%) | Average age (years) |
|---|---|---|
| PPM | 3436 (44.9) | 77 ± 11 |
| Dual-chamber PPM | 3120 (40.8) | 77 ± 11 |
| CRT-P | 316 (4.1) | 78 ± 12 |
| ICD | 1955 (25.6) | 71 ± 12 |
| Dual-chamber ICD | 987 (12.9) | 70 ± 12 |
| CRT-D | 968 (12.7) | 73 ± 12 |
| ILR | 2260 (29.5) | 70 ± 12 |
| All devices | 7651 (100) | 74 ± 12 |
Values in bold represent total number and overall average age of cohort
AF, atrial fibrillation; PPM, permanent pacemaker; CRT-P, cardiac resynchronization therapy pacemaker; ICD, implantable cardioverter defibrillator; CRT-D, cardiac resynchronization therapy defibrillator; S-ICD, subcutaneous implantable cardioverter defibrillator; ILR, implantable loop recorder
Device manufacturers
The cohort included patients with devices from Medtronic, Abbott Medical, Boston-Scientific, and Biotronik. Medtronic devices accounted for 56.1% (n = 4293) of the cohort, Boston Scientific devices for 26.2% (n = 2001), Abbott Medical devices for 11.4% (n = 875), and Biotronik devices for 4.0% (241) (Table 2).
Table 2.
Device types according to manufacturer
| Device type | Device manufacturer | n (%) |
|---|---|---|
| PPM | Medtronic | 1807 |
| Boston Scientific | 1168 | |
| St. Jude Medical (Abbott) | 150 | |
| Biotronik | 311 | |
| ICD | Medtronic | 826 |
| Boston Scientific | 833 | |
| St. Jude Medical (Abbott) | 140 | |
| Biotronik | 156 | |
| ILR | Medtronic | 1660 |
| St. Jude Medical (Abbott) | 585 | |
| Biotronik | 15 | |
| All CIEDs | Medtronic | 4293 (56.1) |
| Boston Scientific | 2001 (26.2) | |
| St. Jude Medical (Abbott) | 875 (11.4) | |
| Biotronik | 482 (6.3) |
PPM, permanent pacemaker; ICD, implantable cardioverter defibrillator; ILR, implantable loop recorder; CIED, cardiac implantable electronic device
AF episode duration
After calculation of the longest aggregate AF burden within 24 h per patient, 3404 (44.5%) patients had AF < 6 min, 1367 (17.9%) patients had AF 6 min–6 h, 1206 (15.8%) patients had AF 6–24 h, and 1674 (21.9%) patients had AF ≥ 24 h. This equated to 2880 (37.6%) patients having at least 6 h of AF within a 24-h period.
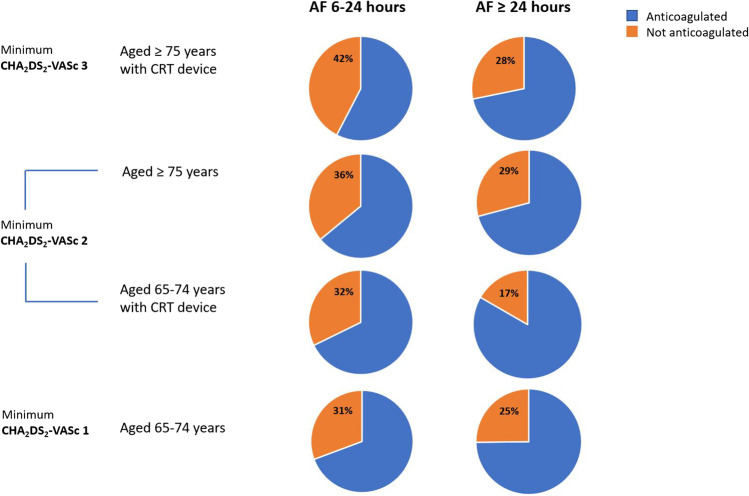
Anticoagulation rates in patients aged ≥ 75 years (minimum CHA2DS2-VASc score of 2) with AF episode at least 6 h in duration
Of the 7651 total patients who transmitted AF episodes, 3841 (50.2%) were aged 75 years or above, with a minimum CHA2DS2-VASc score of 2. Of these patients, 642 (16.7%) had AF durations between 6–24 h and 231 (36.0%) of these patients were not anticoagulated. A further 947 (24.7%) patients aged at least 75 years had AF ≥ 24 h and 276 (29.1%) of these patients were not anticoagulated (Fig. 2).
Fig. 2.
Demonstrates anticoagulation rates in patients with an AF episode of at least 6 h in duration, according to minimum CHA2DS2-VASc score
In patients aged at least 75 years with an AF episode of at least 6 h, 1082 (68.1%) of a total 1589 patients were receiving anticoagulation at the end of the 12-month monitoring period, while 507 (31.9%) were not.
Of the 3841 patients aged ≥ 75 years, 682 had a CRT-D or CRT-P in situ, elevating their minimum CHA2DS2-VASc score to 3. Of these patients, 92 had AF 6–24 h with 39 (42.4%) not anticoagulated. A further 234 patients had AF ≥ 24 h with 66 (28.2%) not anticoagulated (Fig. 2).
Of the total 326 patients designated a minimum CHA2DS2-VASc score of 3, due to a combination of their age and device type, who transmitted an AF episode of at least 6 h in duration, there were 221 (67.8%), who were receiving anticoagulation and 105 (32.2%) who were not.
Anticoagulation rates in patients aged 65–74 years with AF episodes at least 6 h in duration
A total of 2051 patients in the cohort were aged 65–74 years, with a minimum CHA2DS2-VASc score of 1. Of these patients, 339 had AF 6–24 h and 104 (30.7%) were not anticoagulated. A further 449 patients had AF ≥ 24 h and 113 (25.2%) were not anticoagulated (Fig. 2). When all patients aged 65–74 years with an AF episode of at least 6 h were pooled, 517 (72.5%) of a total 788 patients were receiving anticoagulation, while 217 (27.5%) were not.
Of the 2051 patients aged 65–74 years, 313 had a CRT-D or CRT-P in situ, elevating their minimum CHA2DS2-VASc score to 2. Of these patients, 31 had AF 6–24 h, 10 (32.3%) of whom were not anticoagulated. A further 84 patients had AF ≥ 24 h and 14 (16.7%) were not anticoagulated (Fig. 2).
Of the total, 115 patients aged 65–74 years with a CRT-D or CRT-P in situ, and an AF episode of at least 6 h, 91 (79.1%) were receiving anticoagulation, while 24 (20.9%) were not.
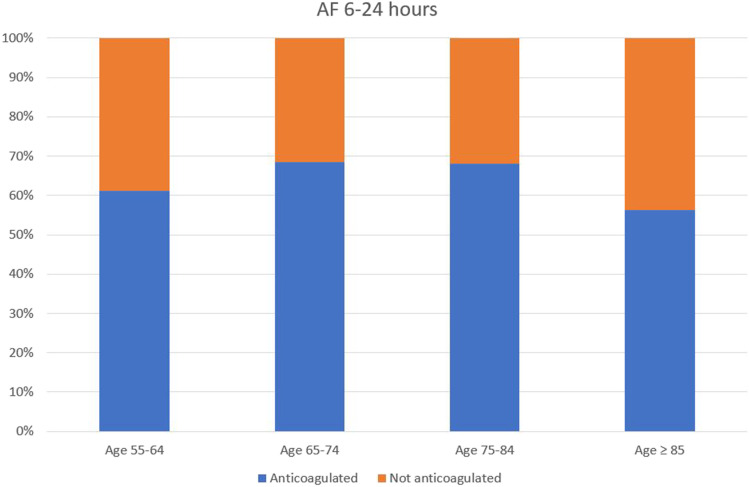
Comparison of anticoagulation rates across patient age groups
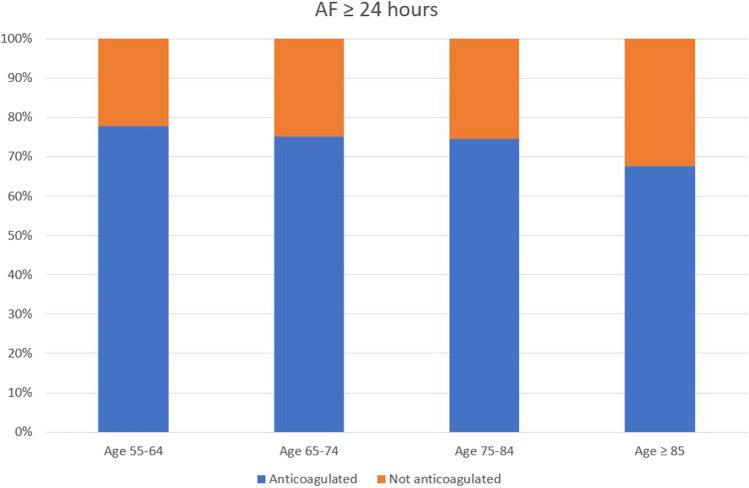
Use of anticoagulation was compared across age categories in all patients aged at least 55 and above, with an AF episode duration of at least 6 h. In patients with AF 6–24 h, anticoagulation was present in 61.2% of those aged 55–64 years, 68.5% of those aged 65–74 years, 68.0% of those aged 75–84 years, and 56.4% of those aged ≥ 85 years (Fig. 3). In patients with AF ≥ 24 h, anticoagulation was present in 77.8% of those aged 55–64 years, 75.2% of those aged 65–74 years, 74.5% of those aged 75–84 years, and 67.6% of those aged ≥ 85 years (Fig. 4).
Fig. 3.
Demonstrates anticoagulation status across different age brackets, in patients with maximum AF episode duration of 6 to 24 h
Fig. 4.
Demonstrates anticoagulation status across different age brackets, in patients with maximum AF episode duration of more than 24 h
Discussion
Major findings
Early detection of AF and the potential opportunity to intervene to reduce stroke risk is a key benefit of RM. Using a large clinical RM database across multiple centers, we identified the following with regards to AF episodes:
• AF episode burden was significant across all device types; however, there was an over-representation of AF episodes detected by ILRs
• A substantial proportion of patients with a significant risk of ischemic stroke as indicated by their AF episode duration combined with their CHA2DS2-VASc score remain not anticoagulated
• Anticoagulation rates among older patients were comparatively lower than rates among younger patients
Burden of AF alerts
A large proportion (48.8%) of AF episodes were transmitted by ILRs, despite ILRs accounting for only 29.5% of the cohort. This may be partially attributable to the nature of ILR indications, including syncope [10, 11], cryptogenic stroke [12–14], and palpitations [15, 16], all of which may be caused by AF or its termination. Alternatively, this may represent transmission of false-positive episodes, which are a common occurrence in ILRs, largely due to atrial ectopy or noise [17].
By comparison, despite accounting for the bulk of CIEDs (44.9%) in the cohort, PPMs were responsible for only 35.7% of AF episodes, while defibrillator patients represented 25.6% of the cohort but transmitted only 15.5% of AF episodes. Device programming in PPMs and ICDs may further explain this between-device group disparity; patients with known AF, on appropriate therapy, may be programmed with a longer AF duration threshold for triggering of an RM alert.
AF episode duration and anticoagulation
While device-detected AF has been established as a risk factor for stroke, questions remain regarding the appropriate AF episode duration threshold for commencement of anticoagulation. A sub-analysis of the ASSERT study demonstrated a significantly increased risk of stroke or systemic embolism in patients with a device-detected AF episode of at least 24 h, with shorter episodes (6 min–24 h) not correlating with an increase in risk [18]. Another study of over 9000 CIED patients over a ten-year period showed device-detected AF of at least 5.5 h was associated with heightened stroke risk [19]. With regards to shorter duration episodes, the LOOP study anticoagulated high-risk patients with at least 6 min of AF detected on a loop recorder and found no significant reduction in stroke of systemic embolism compared to a control group [20]. A recent meta-analysis of studies reporting stroke events in patients with device-detected AF demonstrated a low risk of stroke (0.93 per 100 person years) in association with “short” duration AF episodes [21]; however, there was significant between-study heterogeneity in the definition of such episodes, ranging from below 6 min duration [3] to below 5.5 h burden in one day [22]. The same meta-analysis showed that overall, device-detected AF was associated with an increased stroke risk (absolute annual risk 1.89 per 100 person years, increased to 2.76 per 100 person years in case of mean CHADS2 score 2.1) [21].
Al-Gibbawi et al. assessed stroke/transient ischemic stroke (TIA) incidence in a high-risk unanticoagulated CIED patient population with an average CHA2DS2-VASc score of 4.1 and a 19.9% rate of previous TIA/stroke. They found no correlation between longest AF episode duration and risk of stroke, nor between overall AF burden and risk of stroke[23]. Comparatively, Go et al. demonstrated an association between AF burden determined by wearable cardiac monitors and risk of stroke, in a population with a lower average CHA2DS2-VASc score (2.6), and a lower rate of previous TIA/stroke (2.7%) [24]. These contrasting findings raise the possibility that in higher-risk patients (as determined by CHA2DS2-VASc scores) with a CIED in situ, AF burden and episode duration are less predictive of stroke [23]. In our cohort, such high-risk patients with CHA2DS2-VASc scores of at least 3, with AF of at least 6 h, but less than 24 h, were anticoagulated at a rate of only 57.6%.
Rates of anticoagulation in patients with CHA2DS2-VASc score ≥ 2
The European Heart Rhythm Association guidelines recommend oral anticoagulation in patients with a CHA2DS2-VASc score ≥ 2 in the presence of an AF burden of more than 5.5 h in one day [25]. Our analysis demonstrates that among patients with a transmitted AF episode of at least 6 h, and a minimum CHA2DS2-VASc score of 2, the overall anticoagulation rate was 68.8% (central figure). Kaplan et al. looked specifically at device-detected AF in a large real-world remote-monitored CIED patient population and described comparatively low rates of anticoagulation. In patients with daily AF burden of between 6 min and 23.5 h, anticoagulation was prescribed in 14.1%, 29.6%, and 44.7% of those with CHA2DS2-VASc scores of 2, 3–4, and ≥ 5, respectively. These rates may be explained by inclusion of short-duration episodes for which treating clinicians opted against anticoagulation; however, anticoagulant use remained low in patients with longer duration AF (> 23.5 h), being prescribed in 24.3%, 45.3%, and 67.2% of those with CHA2DS2-VASc scores of 2, 3–4, and ≥ 5, respectively. [26]. In contrast, Steinberg et al. compared rates of oral anticoagulation in over 60,000 patients with newly diagnosed clinical AF within two AF registries and found anticoagulation use in 69% (GARFIELD-AF (international)) and 87% (ORBIT-AF II (US-only)) of patients with a CHA2DS2VASc score ≥ 2 [27]. The discrepancy in anticoagulation rates may be reflective of physician reluctance in prescribing anticoagulation for patients with device-detected AF, especially as US guidelines do not specify thresholds for the use of anticoagulation in this patient cohort [28]. Given the uncertain benefits of anticoagulation among patients with device-detected AF, particularly in those with episodes shorter than 24 h in duration, outcomes from pending trials (e.g., ARTESIA (NCT01938248) [29] and NOAH-AFNET 6 (NCT02618577)) [30] will hopefully provide further guidance regarding this issue.
Although the CHA2DS2-VASc scoring system was not derived for risk stratification specifically in device-detected AF [31], subclinical AF is a known strong predictor of clinical AF [21], and stroke risk in modern AF cohorts is similar to risk in device-detected AF [21]. Thus, it is not unreasonable to estimate a 2.9% annual risk of stroke, TIA, or systemic embolism in accordance with a CHA2DS2-VASc score of 2 [32]; our analysis left 31.2% of patients in this category without anticoagulation.
Rates of anticoagulation among younger versus older patients
The lowest anticoagulation rates for AF episodes of significant duration were seen in older patients, aged 75 or above. Of these patients with an AF episode of between 6 and 24 h in duration, 64.0% were anticoagulated. In patients aged ≥ 75 years with a CRT device in situ, the anticoagulation rate for an AF episode between 6 and 24 h was even lower, at 57.6%, despite a minimum CHA2DS2-VASc score of 3, inferring an approximate 3.2% annual risk of ischemic stroke, and 4.6% annual risk of stroke/TIA/systemic embolism [32]. Anticoagulation rates among patients aged 65–74 years were comparatively higher at 72.5% in those with an AF episode of at least 6 h in duration and as high as 74.8% in those with AF ≥ 24 h. When comparing younger patients in the cohort (age 55–64 years) and older patients (aged at least 85 years) with AF of at least 6 h in duration, we unexpectedly demonstrated higher anticoagulation rates in the younger patients, compared with their older counterparts (61.2% vs. 56.4% for AF 6–24 h, and 77.8% vs. 67.6% for AF 24 h).
Lower anticoagulation rates in older patients, with higher CHA2DS2-VASc scores, may be attributable to physician or patient concerns around frailty, falls risk, and bleeding risk, as this demographic tends to also have higher HAS-BLED scores. Studies have shown, however, that the net clinical benefit of anticoagulation in AF patients exceeds the risk of significant bleeding in most patients [33, 34]. In a large cohort study of over 180,000 AF patients, Friberg et al. identified only 0.4% of patients with a CHA2DS2-VASc score of ≥ 1 in whom bleeding risk exceeded ischemic stroke risk, with most patients not exhibiting a true contraindication to anticoagulation [33]. Another factor contributing to lower use of anticoagulation in the elderly demographic may be the use of left atrial appendage occlusion to negate the requirement for anticoagulation.
Anticoagulation rates in patients with long duration AF episodes (≥ 24 h)
Device-detected AF episode duration of ≥ 24 h has been established as an independent risk factor for embolic events [18, 35]; Botto et al. found episodes of ≥ 24 h in duration to infer an annual embolic event risk of up to 4%, even in patients with a CHADS2 score of only 1 [36]. The study utilized CHADS2 scores only; however, some patients may have had a higher CHA2DS2-VASc score if calculated. More recently, Kaplan et al. assessed the occurrence of stroke and systemic embolism in over 20,000 unanticoagulated CIED patients and established both increasing AF episode duration and increasing CHA2DS2-VASc score to be associated with a heightened embolic risk. Importantly, in patients with long AF episode duration (≥ 23.5 h) and a CHA2DS2-VASc score of 1, the annual incidence of stroke/systemic embolism was only 0.56% [37], suggesting that long-duration device-detected AF episodes may not warrant anticoagulation in CHA2DS2-VASc-1 patients. Despite this, our study showed that among patients with AF ≥ 24 h, those aged less than 65 years, and those aged 65–74 years, had relatively high anticoagulation rates of 74.9% and 74.8%, respectively. In some patients, this may be reflective of the presence of factors unknown to us, elevating their CHA2DS2-VASc score. Again, use of anticoagulation was comparatively lower (70.9%) in patients aged ≥ 75 years, perhaps reflecting physician confidence regarding low bleeding risk in the younger cohort.
Clinical implications
The findings of this study highlight the need for strategies to address the ischemic stroke/systemic embolism risk that remains unaddressed in a significant proportion of patients with device-detected AF. Education regarding stroke risk in patients with subclinical AF and the net clinical benefit of anticoagulation in high-risk patients provides one with potential opportunity to manage better this patient cohort. Furthermore, implementation of structured RM clinical response pathways and integrated care, to promote consideration of anticoagulation, is required. Given the burden that AF episodes place on current RM pathways, systems can be re-designed with inclusion of automated features to prompt anticoagulation decisions as an alternative to reliance on human prompts.
Limitations
Our data were derived from a large remote monitoring database with a limited number of baseline characteristics. CHA2DS2-VASc scores could not be definitively obtained due to unknowns regarding the presence of hypertension, diabetes mellitus, heart failure/left ventricular dysfunction, and vascular disease in the cohort. Further, we did not have access to sex in a significant proportion of the cohort. Our analysis was performed based on minimum CHA2DS2-VASc scores according to the available patient characteristics. This likely lead to an underestimate of patients in whom stroke risk crossed the threshold to justify anticoagulation. In the absence of data regarding procedural interventions, we cannot exclude to possibility that some unanticoagulated patients in our study population have undergone left atrial appendage occlusion and are thus appropriately without anticoagulation. Though anticoagulation status was assessed only in those patients with a burden of at least 6 h within a 24 h period, meaning the likelihood of a false-positive AF episode is minimal [38], in the absence of individual electrogram review, we cannot definitively exclude the possibility of inclusion of some non-AF rhythms.
Conclusion
Despite participation in an intensively managed RM system with in-built cues for consideration of anticoagulation, more than 30% of patients with device-detected AF were not anticoagulated in the presence of a risk factor profile inferring a significant risk of ischemic stroke or systemic embolism. Older patients, aged 75 or above, were under-anticoagulated compared with their younger counterparts. These data represent potential missed opportunities to implement pharmacotherapy for stroke prevention. Improved RM clinical response pathways are required to ensure adherence to stroke prevention measures in the device-detected AF population.
Abbreviations
- AF
Atrial fibrillation
- CIED
Cardiac implantable electronic device
- CRT
Cardiac resynchronization therapy
- IBHRE
International Board of Heart Rhythm Examiners
- ICD
Implantable cardioverter defibrillator
- ILR
Implantable loop recorder
- LV
Left ventricle
- PPM
Permanent pacemaker
- RM
Remote monitoring
- TIA
Transient ischemic stroke
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. Dr. O’Shea is supported by a Postgraduate Scholarship from the University of Adelaide. Dr. Middeldorp is supported by a Postdoctoral Fellowship from the University of Adelaide. Dr. Hendriks is supported by a Future Leader Fellowship from the Heart Foundation of Australia. Dr. Freeman is support by the American College of Cardiology National Cardiovascular Data Registry and the US National Heart, Lung and Blood Institute. Dr. Sanders is supported by a Practitioner Fellowship from the National Health and Medical Research Council of Australia and by the National Heart Foundation of Australia.
Declarations
Ethics approval
The study was reviewed and approved by the Human Research Ethics Committees of the Central Adelaide Local Health Network and the University of Adelaide.
Informed consent
Not applicable.
Conflict of interest
Dr. Brooks is currently employed by Microport. Mr. Harper is currently employed by PaceMate. Dr. Hendriks reports that the University of Adelaide has received on his behalf lecture and/or consulting fees from Medtronic and Pfizer/BMS. Dr. Russo reports research grants from Boston Scientific and Kestra, consulting from Abbott, Boston Scientific, Medtronic and PaceMate, and honoraria from Biotronik. Dr. Freeman reports consulting/advisory board fees from Boston Scientific, Medtronic, Janssen Pharmaceuticals, Biosense Webster, and PaceMate and equity from PaceMate. Dr. Gopinathannair reports that he has received consulting fees or honoraria from Abbott Medical, Boston Scientific, Zoll Medical. Dr. Gopinathannair reports having served on the advisory board of PaceMate, and Altathera. Dr. Deering reports that Piedmont Healthcare receives on his behalf research grants from Abbott, Biotronik, Biosense Webster, Medtronic, and Milestone. He also reports that he has consulted for CVRx, PaceMate, Preventice, and Sanofi while serving as a member of an Adjudication Committee for Abbott. Dr. Varma reports having consulted for Medtronic, Abbott Medical, Boston-Scientific, Biotronik, Microport, and on the advisory board for PaceMate. Dr. Campbell was previously employed by PaceMate. Dr. Sanders reports having served on the advisory board of Medtronic, Abbott Medical, Boston-Scientific, PaceMate, and CathRx. Dr. Sanders reports that the University of Adelaide receives on his behalf lecture and/or consulting fees from Medtronic, Abbott Medical, and Boston-Scientific. Dr. Sanders reports that the University of Adelaide receives on his behalf research funding from Medtronic, Abbott Medical, Boston-Scientific, Microport, and BD. The remaining authors have nothing to disclose.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
2/24/2023
Missing Open Access funding information has been added in the Funding Note.
References
- 1.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22(8):983–988. doi: 10.1161/01.STR.22.8.983. [DOI] [PubMed] [Google Scholar]
- 2.Healey JS, et al. Subclinical atrial fibrillation and the risk of stroke. N Engl J Med. 2012;366(2):120–129. doi: 10.1056/NEJMoa1105575. [DOI] [PubMed] [Google Scholar]
- 3.Brambatti M, et al. Temporal relationship between subclinical atrial fibrillation and embolic events. Circ. 2014;129(21):2094–2099. doi: 10.1161/CIRCULATIONAHA.113.007825. [DOI] [PubMed] [Google Scholar]
- 4.January CT, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64(21):e1–76. doi: 10.1016/j.jacc.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 5.Yee R, et al. Canadian Cardiovascular Society/Canadian Heart Rhythm Society joint position statement on the use of remote monitoring for cardiovascular implantable electronic device follow-up. Can J Cardiol. 2013;29(6):644–651. doi: 10.1016/j.cjca.2012.11.036. [DOI] [PubMed] [Google Scholar]
- 6.Slotwiner D, et al. HRS Expert Consensus Statement on remote interrogation and monitoring for cardiovascular implantable electronic devices. Heart Rhythm. 2015;12(7):e69–100. doi: 10.1016/j.hrthm.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 7.Crossley GH, et al. The CONNECT (Clinical Evaluation of Remote Notification to Reduce Time to Clinical Decision) trial: the value of wireless remote monitoring with automatic clinician alerts. J Am Coll Cardiol. 2011;57(10):1181–1189. doi: 10.1016/j.jacc.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 8.Varma N, et al. Efficacy and safety of automatic remote monitoring for implantable cardioverter-defibrillator follow-up: the Lumos-T Safely Reduces Routine Office Device Follow-up (TRUST) trial. Circ. 2010;122(4):325–332. doi: 10.1161/CIRCULATIONAHA.110.937409. [DOI] [PubMed] [Google Scholar]
- 9.Cha YM, et al. Atrial fibrillation and ventricular dysfunction: a vicious electromechanical cycle. Circ. 2004;109(23):2839–2843. doi: 10.1161/01.CIR.0000132470.78896.A8. [DOI] [PubMed] [Google Scholar]
- 10.Shen WK, et al. 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2017;70(5):e39–e110. doi: 10.1016/j.jacc.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 11.Brignole M, et al. 2018 ESC guidelines for the diagnosis and management of syncope. Eur Heart J. 2018;39(21):1883–1948. doi: 10.1093/eurheartj/ehy037. [DOI] [PubMed] [Google Scholar]
- 12.Cotter PE, et al. Incidence of atrial fibrillation detected by implantable loop recorders in unexplained stroke. Neurol. 2013;80(17):1546–1550. doi: 10.1212/WNL.0b013e31828f1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gladstone DJ, et al. Atrial fibrillation in patients with cryptogenic stroke. N Engl J Med. 2014;370(26):2467–2477. doi: 10.1056/NEJMoa1311376. [DOI] [PubMed] [Google Scholar]
- 14.Sanna T, et al. Cryptogenic stroke and underlying atrial fibrillation. N Engl J Med. 2014;370(26):2478–2486. doi: 10.1056/NEJMoa1313600. [DOI] [PubMed] [Google Scholar]
- 15.Task Force m et al. Indications for the use of diagnostic implantable and external ECG loop recorders. Europace. 2009;11(5):671–87. doi: 10.1093/europace/eup097. [DOI] [PubMed] [Google Scholar]
- 16.Giada F, et al. Recurrent unexplained palpitations (RUP) study comparison of implantable loop recorder versus conventional diagnostic strategy. J Am Coll Cardiol. 2007;49(19):1951–1956. doi: 10.1016/j.jacc.2007.02.036. [DOI] [PubMed] [Google Scholar]
- 17.O'Shea CJ, et al. Remote monitoring of implantable loop recorders: false-positive alert episode burden. Circ Arrhythm Electrophysiol. 2021;14(11):e009635. doi: 10.1161/CIRCEP.121.009635. [DOI] [PubMed] [Google Scholar]
- 18.Van Gelder IC, et al. Duration of device-detected subclinical atrial fibrillation and occurrence of stroke in ASSERT. Eur Heart J. 2017;38(17):1339–1344. doi: 10.1093/eurheartj/ehx042. [DOI] [PubMed] [Google Scholar]
- 19.Turakhia MP, et al. Atrial fibrillation burden and short-term risk of stroke: case-crossover analysis of continuously recorded heart rhythm from cardiac electronic implanted devices. Circ Arrhythm Electrophysiol. 2015;8(5):1040–1047. doi: 10.1161/CIRCEP.114.003057. [DOI] [PubMed] [Google Scholar]
- 20.Svendsen JH, et al. Implantable loop recorder detection of atrial fibrillation to prevent stroke (The LOOP Study): a randomised controlled trial. Lancet. 2021;398(10310):1507–1516. doi: 10.1016/S0140-6736(21)01698-6. [DOI] [PubMed] [Google Scholar]
- 21.Mahajan R, et al. Subclinical device-detected atrial fibrillation and stroke risk: a systematic review and meta-analysis. Eur Heart J. 2018;39(16):1407–1415. doi: 10.1093/eurheartj/ehx731. [DOI] [PubMed] [Google Scholar]
- 22.Glotzer TV, et al. The relationship between daily atrial tachyarrhythmia burden from implantable device diagnostics and stroke risk: the TRENDS study. Circ Arrhythm Electrophysiol. 2009;2(5):474–480. doi: 10.1161/CIRCEP.109.849638. [DOI] [PubMed] [Google Scholar]
- 23.Al-Gibbawi M, et al. Relationship between device-detected burden and duration of atrial fibrillation and risk of ischemic stroke. Heart Rhythm. 2021;18(3):338–346. doi: 10.1016/j.hrthm.2020.10.017. [DOI] [PubMed] [Google Scholar]
- 24.Go AS, et al. Association of burden of atrial fibrillation with risk of ischemic stroke in adults with paroxysmal atrial fibrillation: the KP-RHYTHM study. JAMA Cardiol. 2018;3(7):601–608. doi: 10.1001/jamacardio.2018.1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gorenek BC, et al. Device-detected subclinical atrial tachyarrhythmias: definition, implications and management-an European Heart Rhythm Association (EHRA) consensus document, endorsed by Heart Rhythm Society (HRS), Asia Pacific Heart Rhythm Society (APHRS) and Sociedad Latinoamericana de Estimulacion Cardiaca y Electrofisiologia (SOLEACE) Europace. 2017;19(9):1556–1578. doi: 10.1093/europace/eux163. [DOI] [PubMed] [Google Scholar]
- 26.Kaplan RM, et al. Use of oral anticoagulation in a real-world population with device detected atrial fibrillation. J Am Heart Assoc. 2020;9(24):e018378. doi: 10.1161/JAHA.120.018378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Steinberg BA, et al. International trends in clinical characteristics and oral anticoagulation treatment for patients with atrial fibrillation: results from the GARFIELD-AF, ORBIT-AF I, and ORBIT-AF II registries. Am Heart J. 2017;194:132–140. doi: 10.1016/j.ahj.2017.08.011. [DOI] [PubMed] [Google Scholar]
- 28.January CT, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2019;74(1):104–132. doi: 10.1016/j.jacc.2019.01.011. [DOI] [PubMed] [Google Scholar]
- 29.Lopes RD, et al. Rationale and design of the apixaban for the reduction of thrombo-embolism in patients with device-detected sub-clinical atrial fibrillation (ARTESiA) trial. Am Heart J. 2017;189:137–145. doi: 10.1016/j.ahj.2017.04.008. [DOI] [PubMed] [Google Scholar]
- 30.Kirchhof P, et al. Probing oral anticoagulation in patients with atrial high rate episodes: rationale and design of the non-vitamin K antagonist oral anticoagulants in patients with atrial high rate episodes (NOAH-AFNET 6) trial. Am Heart J. 2017;190:12–18. doi: 10.1016/j.ahj.2017.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lip GYH, et al. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137(2):263–272. doi: 10.1378/chest.09-1584. [DOI] [PubMed] [Google Scholar]
- 32.Friberg L, Rosenqvist M, Lip GY. Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182 678 patients with atrial fibrillation: the Swedish Atrial Fibrillation cohort study. Eur Heart J. 2012;33(12):1500–1510. doi: 10.1093/eurheartj/ehr488. [DOI] [PubMed] [Google Scholar]
- 33.Friberg L, Rosenqvist M, Lip GY. Net clinical benefit of warfarin in patients with atrial fibrillation: a report from the Swedish atrial fibrillation cohort study. Circ. 2012;125(19):2298–2307. doi: 10.1161/CIRCULATIONAHA.111.055079. [DOI] [PubMed] [Google Scholar]
- 34.Olesen JB, et al. Risks of thromboembolism and bleeding with thromboprophylaxis in patients with atrial fibrillation: a net clinical benefit analysis using a 'real world' nationwide cohort study. Thromb Haemost. 2011;106(4):739–749. doi: 10.1160/TH11-05-0364. [DOI] [PubMed] [Google Scholar]
- 35.Capucci A, et al. Monitored atrial fibrillation duration predicts arterial embolic events in patients suffering from bradycardia and atrial fibrillation implanted with antitachycardia pacemakers. J Am Coll Cardiol. 2005;46(10):1913–1920. doi: 10.1016/j.jacc.2005.07.044. [DOI] [PubMed] [Google Scholar]
- 36.Botto GL, et al. Presence and duration of atrial fibrillation detected by continuous monitoring: crucial implications for the risk of thromboembolic events. J Cardiovasc Electrophysiol. 2009;20(3):241–248. doi: 10.1111/j.1540-8167.2008.01320.x. [DOI] [PubMed] [Google Scholar]
- 37.Kaplan RM, et al. Stroke risk as a function of atrial fibrillation duration and CHA2DS2-VASc score. Circ. 2019;140(20):1639–1646. doi: 10.1161/CIRCULATIONAHA.119.041303. [DOI] [PubMed] [Google Scholar]
- 38.Kaufman ES, et al. Positive predictive value of device-detected atrial high-rate episodes at different rates and durations: an analysis from ASSERT. Heart Rhythm. 2012;9(8):1241–1246. doi: 10.1016/j.hrthm.2012.03.017. [DOI] [PubMed] [Google Scholar]