Abstract
Genes for two group 1 β-lactamases, SRT-1 and SST-1, were sequenced. These β-lactamases were produced by clinical isolates of Serratia marcescens, isolates GN16694 and GN19450, respectively. The resulting enzymes were 96% identical. SRT-1 hydrolyzed oxyimino cephalosporins, but SST-1 hardly hydrolyzed them. At residue 213 in the third motif, which is conserved among group 1 β-lactamases, SRT-1 and SST-1 had Lys and Glu, respectively. By site-directed mutagenesis, the substitution of Glu by Lys at residue 213 in SST-1 resulted in an enzyme that hydrolyzed oxyimino cephalosporins.
With the extended use of β-lactams in clinical practice, organisms resistant to these antibiotics have increasingly been isolated. Resistance can be mediated by the production of β-lactamases, such as in derepressed mutants (18, 19), the acquisition of plasmids with a β-lactamase gene from other strains (2, 5, 8, 17, 25), and the expansion of the substrate specificity of the organism’s own enzyme (16, 22, 23).
To protect the β-lactam ring from hydrolysis by β-lactamases, cephalosporins with a 7-oxyimino moiety on the side chain of the cephem nucleus have been synthesized, and these have been shown to be stable. Recently, it was reported that the group 1 β-lactamase hydrolyzed oxyimino cephalosporins in Enterobacter cloacae (16) and Citrobacter freundii (23). The β-lactamase from E. cloacae P99 hardly hydrolyzes oxyimino cephalosporins, but this enzyme with an insertion of three residues just behind Arg 210 did hydrolyze them. Likewise, the β-lactamase from E. cloacae GC1, which was isolated clinically and which had a duplication of Ala-Val-Arg at the same position, showed the same hydrolytic activity as the P99 β-lactamase with the three-residue insertion. The group 1 β-lactamase from C. freundii GN346 hardly hydrolyzed oxyimino cephalosporins, but the artificial substitution of Glu for Lys at position 219 allowed the enzyme to hydrolyze oxyimino cephalosporins.
In a previous study, we reported that Serratia marcescens GN16694 is resistant to oxyimino cephalosporins. The organism was isolated clinically and produced SRT-1, a group 1 β-lactamase (1) that hydrolyzed these cephems and that had a molecular weight of 42,000 and a pI of 8.6 (14).
In the report described in this paper, we determined the nucleotide sequences of genes encoding SRT-1 and SST-1 (SST-1 was produced by the β-lactam-susceptible strain S. marcescens GN19450 and hardly hydrolyzed oxyimino cephalosporins) and describe the relationship between the extended substrate specificity and the differences in the amino acid residues in their sequences.
S. marcescens GN16694, which has a high level of resistance to oxyimino cephalosporins, is a clinical isolate (14). S. marcescens GN19450 is a clinical isolate and is susceptible to various β-lactams (6). Escherichia coli JM83 (24) was used for DNA techniques. Plasmids pHSG398 (21) and pHSG399 (21) were used as the cloning vector and the vector for DNA sequencing, respectively. The following antimicrobial agents were used: streptomycin sulfate, cephaloridine, cefotaxime, ceftazidime, cefmenoxime, and cefuroxime.
Susceptibility testing, the purification of β-lactamases from S. marcescens GN16694 and GN19450 and from E. coli JM83/pGFS11, JM83/pGFR5, and JM83/pGFSK, and studies of their kinetics were based on a previously described method (14). β-Lactamase activities were assayed spectrophotometrically. The kinetic parameters were determined with a Lineweaver-Burk plot.
Plasmid DNA was prepared by the rapid alkaline extraction method (11). Restriction endonucleases were obtained from Nippon Gene Co. Ltd., Toyama, Japan, and the DNA-Ligation Kit was obtained from Takara Shuzo Co. Ltd., Kyoto, Japan. DNA techniques were done according to the manufacturer’s recommendation. For the cloning of the genes for SRT-1 and SST-1, BamHI-digested fragments of DNAs from S. marcescens GN16694 and GN19450, respectively, were ligated into the BamHI site of pHSG398. These recombinants were introduced into E. coli JM83, and transformants with the gene for SRT-1 or SST-1 were selected on Luria-Bertani agar plates containing chloramphenicol (30 μg/ml) and ceftazidime (6.25 μg/ml) or cephaloridine (12.5 μg/ml), respectively. These resultant transformants maintained a plasmid with a 4.0-kbp fragment carrying the gene for SRT-1 or SST-1. These recombinant plasmids with the gene for SRT-1 and SST-1 were termed pGFR5 and pGFS11, respectively. These fragments were subcloned into pHSG399 to sequence both strands.
Double-stranded plasmid DNA templates for the sequences were constructed by using the Kilo-sequence Deletion Kit (Takara Shuzo). The nucleotide sequences were determined by the dideoxy chain termination method (20) by using the TAKARA Taq Cycle Sequencing kit for the Shimadzu DNA Sequencer, version 2, M13 forward and reverse fluorescence primers (Takara Shuzo), and a DSQ-1000 DNA Sequencer (Shimadzu, Kyoto, Japan). The nucleotide sequence data were organized and analyzed by using DNASIS (Hitachi Software Engineering Co. Ltd., Yokohama, Japan).
The oligonucleotide primer composed of a 21-mer (CTGGACGCCAAATCTTACGGC) was used for site-directed mutagenesis. This primer corresponded to the DNA sequence encoding amino acid residues of 210 to 216 in SRT-1, and an attempt was made to anneal the primer to the corresponding region of the SST-1 gene. Site-directed mutagenesis was carried out by using a modification of the manufacturer’s information for Mutan-Express Km (Takara Shuzo) by using pGFS11 with the gene for SST-1 as a template.
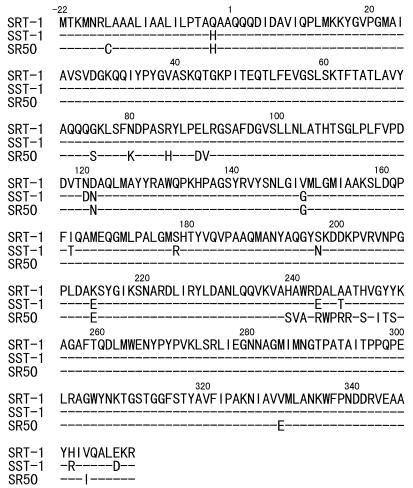
Within the 4.0-kbp DNA fragments, a 1,290-bp segment containing the gene for SRT-1 and a 1,288-bp segment containing the gene for SST-1 were sequenced. These sequenced regions each embraced an open reading frame, and it was deduced that they were composed of 379 amino acids (Fig. 1). The amino acid sequence of the group 1 β-lactamase (cephalosporinase) from S. marcescens SR50 that hardly hydrolyzes oxyimino cephalosporins has been presented previously (1, 15). The amino-terminal region from positions −22 to −1 was assumed to be the signal peptide because a typical sequence (A-X-A) was found, and this sequence was recognized by the signal peptidase. Consequently, it was supposed that in SRT-1 and SST-1 the mature proteins are composed of 357 amino acids. The amino acid sequence of SST-1 showed an identity of 96% to that of SRT-1. There was a high degree of similarity of the amino acid sequence of SST-1 to those of the group 1 β-lactamases from S. marcescens SR50 (92% identity) (15), C. freundii (42% identity) (9, 22), and Pseudomonas aeruginosa (49% identity) (10).
FIG. 1.
Alignment of amino acids of SRT-1, SST-1, and the group 1 β-lactamase, indicated SR50, from S. marcescens SR50 (15). Dashes indicate residues identical to those of SRT-1. The position of the N-terminal amino acid of the mature enzymes is designated position 1. The amino acid sequence from positions −22 to −1 is assumed to be the signal peptide.
Relative rates of hydrolysis by SRT-1 and SST-1 prepared from S. marcescens GN16694 and GN19450, respectively, showed the enzymes have very different hydrolytic profiles. SRT-1 also hydrolyzed cephaloridine and oxyimino cephalosporins such as ceftazidime and cefotaxime, showing a higher degree of hydrolysis of these drugs than of cephaloridine. On the other hand, SST-1 hardly hydrolyzed oxyimino cephalosporins (data not shown).
To study the relationship between the expansion of the substrate specificity of SRT-1 in comparison with that of SST-1 and the differences in the amino acid residues in their sequences, the amino acid sequences in the region of the mature enzymes were compared. There were differences at 11 amino acid residues (Fig. 1). At positions 120, 164, 178, 197, 348, and 354, the amino acid residues in SRT-1 were different from those in SST-1, whereas those in SRT-1 were the same as those in the group 1 β-lactamase of S. marcescens SR50. At positions 121, 149, 243, and 246, these residues in SRT-1 differed from those in SST-1 and the enzyme of S. marcescens SR50. In a comparison of the amino acid sequences of β-lactamases with the same substrate specificity produced by the same genus of bacilli, it was found that there is not necessarily complete identity among them (3, 9, 16, 22). Although SST-1 is the same as the enzyme from S. marcescens SR50 with regard to its low level of hydrolysis of oxyimino cephalosporins, there is disagreement between their amino acid sequences (92% identity). These findings suggest that the differences between these residues in SRT-1 and those in SST-1 and the enzyme of S. marcescens SR50 has little effect on the expansion of the substrate specificity toward oxyimino cephalosporins. However, at position 213, the amino acid residue was Lys in SRT-1, whereas it was Glu in SST-1 and the enzyme of S. marcescens SR50. Since Lys is a basic amino acid and Glu is acidic, resulting in a potentially different character, we anticipated that the Lys at position 213 contributed to the expansion of the substrate specificity in SRT-1, and the substitution of Glu in SST-1 into Lys was carried out by site-directed mutagenesis.
By site-directed mutagenesis of the gene encoding SST-1, a variant termed SST-K was obtained. This variant hydrolyzed oxyimino cephalosporins. DNA sequencing certified that the sequence of the region encoding residues 210 to 216 in SST-K was the same as that of the gene for SRT-1, and the amino acid at residue 213 was Lys.
Table 1 presents the susceptibilities of E. coli JM83 producing SST-K, SRT-1, and SST-1. The oxyimino cephalosporins MICs for E. coli JM83/pGFSK (the strain producing SST-K) were higher than those for parent strain (JM83/pHSG398) and the same as those for JM83/pGFR5 (the strain producing SRT-1). The MICs of cefotaxime, cefuroxime, and cefmenoxime for E. coli JM83/pGFS11 (the strain producing SST-1) were also elevated. The cause of resistance would be high affinities of SST-1 for these antibiotics (Table 2).
TABLE 1.
Susceptibility of E. coli harboring the recombinant plasmids to β-lactams
| E. coli strain (β-lactamase) | MIC (μg/ml)
|
|||
|---|---|---|---|---|
| Cefotaxime | Cefuroxime | Cefmenoxime | Ceftazidime | |
| JM83/pGFSKa (SST-K) | 3.13 | 200 | 0.78 | 50 |
| JM83/pGFR5 (SRT-1) | 3.13 | 200 | 0.78 | 50 |
| JM83/pGFS11 (SST-1) | 3.13 | 100 | 0.39 | 0.39 |
| JM83/pHSG398 | <0.05 | 3.13 | <0.05 | 0.2 |
The recombinant carrying the gene for SST-K.
TABLE 2.
Values of kinetic parameters for SST-K, SRT-1, and SST-1
| Substrate | SST-K
|
SRT-1
|
SST-1
|
||||
|---|---|---|---|---|---|---|---|
| Km (μM) | Relative Vmaxa | Km (μM) | Relative Vmaxa | Km (μM) | Ki (μM) | Relative Vmaxa | |
| Cephaloridine | 670 | 100 | 660 | 100 | 180 | —b | 100 |
| Cefuroxime | 370 | 340 | 330 | 350 | — | 0.3 | <1 |
| Cefotaxime | 390 | 400 | 410 | 410 | — | 2.8 | <1 |
| Cefmenoxime | 180 | 120 | 170 | 130 | — | 1.7 | <1 |
| Ceftazidime | 180 | 20 | 150 | 20 | — | 120 | <1 |
Values relative to that for cephaloridine, which was set at 100.
—, not tested.
Table 2 presents the values of the kinetic parameters for SST-K, SRT-1, and SST-1. SST-K acquired an extended substrate specificity (to oxyimino cephalosporins), whereas SST-1 had a substrate specificity typical of those of a cephalosporinase (12, 13) and the group 1 β-lactamase (1). The affinities of SST-K for cefuroxime, cefotaxime, and cefmenoxime were greatly reduced in comparison with those of SST-1. These kinetic parameters for SST-K were in good agreement with those for SRT-1. These results indicate that the change of Glu into Lys at residue 213 is a means for the hydrolysis of oxyimino cephalosporins.
The work presented here suggests that SRT-1 is a clinically occurring mutant of a group 1 β-lactamase without the ability to hydrolyze oxyimino cephalosporins, and the expansion of the substrate specificity in SRT-1 toward oxyimino cephalosporins is attributable to the change of Glu into Lys at position 213. Table 3 presents four motifs that are conserved in amino acid sequences of group 1 β-lactamases from various gram-negative bacteria (4, 8). Position 213 in SRT-1 and SST-1 corresponds to the third amino acid residue in the third motif. A change of Glu to Lys at this position allowed the enzyme to extend the substrate specificity in the case of SST-1. It was reported that the change of Glu to Lys at position 219 extended the substrate specificity of the group 1 β-lactamase from C. freundii GN346 (23). Position 219 would also correspond to that in the third motif. As indicated in Table 3, the amino acid sequences of the third motif were highly conserved among the group 1 β-lactamases from E. coli, Enterobacter cloacae, P. aeruginosa, Klebsiella pneumoniae, and C. freundii. Moreover, except for the enzyme from E. cloacae, the third amino acid residue in the third motif in their enzymes is Glu. In the future, it is suggested that the Glu at this position in these β-lactamases could be changed into Lys by some clinical action; consequently, they would acquire the expanded substrate specificities.
TABLE 3.
Alignment of the four motifs conserved in amino acid sequences of group 1 β-lactamasesa
| Source (β-lactamase) | Amino acid sequence at the following motif:
|
Refer- ence(s) | |||
|---|---|---|---|---|---|
| First | Second | Third | Fourth | ||
| E. coli | SVSK | YAN | DAEA | KTG | 7 |
| E. cloacae | SISK | YAN | DAQA | KTG | 3 |
| P. aeruginosa | SVSK | YSN | DAEG | KTG | 10 |
| K. pneumoniae (FOX-1) | SVSK | YSN | AAEA | KTG | 8 |
| C. freundii | SVSK | YAN | DAE(K)bA | KTG | 9, 22 |
| S. marcescens SR50 | 58-SLSK | 144-YSN | 211-DAES | 308-KTG | 15 |
| S. marcescens GN19450 (SST-1) | SLSK | YSN | DAES | KTG | This study |
| S. marcescens GN16694 (SRT-1) | SLSK | YSN | DAKS | KTG | This study |
The four motifs are in alignment from the upper position in their amino acid sequences.
In β-lactamases with the extended substrate specificity for oxyimino cephalosporins, E was substituted for K in the third motif.
Nucleotide sequence accession number.
The nucleotide sequences of SRT-1 and SST-1 have been given nucleotide sequence accession nos. AB008454 and AB008455, respectively.
Acknowledgments
We are grateful for financial support from Toyama Chemical Co., Ltd.
We thank S. Iyobe and H. Yamada for technical support and valuable advice.
REFERENCES
- 1.Bush K, Jacoby G A, Medeiros A A. A functional classification scheme for β-lactamases and its correlation with molecular structure. Antimicrob Agents Chemother. 1995;39:1211–1233. doi: 10.1128/aac.39.6.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fosberry A P, Payne D J, Lawlor E J, Hodgson J E. Cloning and sequence analysis of blaBIL-1, a plasmid-mediated class C β-lactamase gene in Escherichia coli BS. Antimicrob Agents Chemother. 1994;38:1182–1185. doi: 10.1128/aac.38.5.1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Galleni M, Lindberg F, Normark S, Cole S, Honore N, Joris B, Frere J-M. Sequence and comparative analysis of three Enterobacter cloacae ampC β-lactamase genes and their products. Biochem J. 1988;250:753–760. doi: 10.1042/bj2500753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ghuysen J-M. Serine β-lactamases and penicillin-binding proteins. Annu Rev Microbiol. 1991;45:37–67. doi: 10.1146/annurev.mi.45.100191.000345. [DOI] [PubMed] [Google Scholar]
- 5.Horii T, Arakawa Y, Ohta M, Ichiyama S, Wacharotayankun R, Kato N. Plasmid-mediated AmpC-type β-lactamase isolated from Klebsiella pneumoniae confers resistance to broad-spectrum β-lactams, including moxalactam. Antimicrob Agents Chemother. 1993;37:984–990. doi: 10.1128/aac.37.5.984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iyobe S, Tsunoda M, Mitsuhashi S. Cloning and expression in Enterobacteriaceae of the extended-spectrum β-lactamase gene from a Pseudomonas aeruginosa plasmid. FEMS Lett. 1994;121:175–180. doi: 10.1111/j.1574-6968.1994.tb07096.x. [DOI] [PubMed] [Google Scholar]
- 7.Jaurin B, Grundstrom T. ampC cephalosporinase of Escherichia coli K-12 has a different evolutionary origin from that of β-lactamases of the penicillinase type. Proc Natl Acad Sci USA. 1981;78:4897–4901. doi: 10.1073/pnas.78.8.4897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leiza M G, Perez-Diaz J C, Ayala J, Casellas J M, Martinez-Beltran J, Bush K, Baquero F. Gene sequence and biochemiccal characterization of FOX-1 from Klebsiella pneumoniae, a new AmpC-type plasmid-mediated β-lactamase with two molecular variants. Antimicrob Agents Chemother. 1994;38:2150–2157. doi: 10.1128/aac.38.9.2150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lindberg F, Normark S. Sequence of the Citrobacter freundii OS60 chromosomal ampC β-lactamase gene. Eur J Biochem. 1986;156:441–445. doi: 10.1111/j.1432-1033.1986.tb09601.x. [DOI] [PubMed] [Google Scholar]
- 10.Lodge J M, Minchin S D, Piddock L J V, Busby S J. Cloning, sequencing and analysis of the structural gene and regulatory region of the Pseudomonas aeruginosa chromosomal ampC β-lactamase. Biochem J. 1990;272:627–631. doi: 10.1042/bj2720627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maniatis T, Fritsch E F, Sambrook J. Molecular cloning: a laboratory manual. Cold Spring Harbor, N.Y: Cold Spring Harbor Laboratory; 1982. [Google Scholar]
- 12.Mitsuhashi S, Inoue M. Mechanism of resistance to β-lactam antibiotics. In: Mitsuhashi S, editor. Beta-lactam antibiotics. Tokyo, Japan: Japan Sciences Press; 1981. pp. 41–56. [Google Scholar]
- 13.Mitsuhashi S. Resistance to β-lactam antibiotics in bacteria. In: Ishigami J, editor. Recent advances in chemotherapy. Tokyo, Japan: University of Tokyo Press; 1985. pp. 3–9. [Google Scholar]
- 14.Matsumura N, Mitsuhashi S. A β-lactamase from Serratia marcescens hydrolyzing the 2-carboxypenam T-5575. Antimicrob Agents Chemother. 1995;39:2132–2134. doi: 10.1128/aac.39.9.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nomura K, Yoshida T. Nucleotide sequence of the Serratia marcescens SR50 chromosomal ampC β-lactamase gene. FEMS Microbiol Lett. 1990;70:295–300. doi: 10.1111/j.1574-6968.1990.tb13992.x. [DOI] [PubMed] [Google Scholar]
- 16.Nukaga M, Haruta S, Tanimoto K, Kogure K, Taniguchi K, Tamaki M, Sawai T. Molecular evolution of a class C β-lactamase extending its substrate specificity. J Biol Chem. 1995;270:5729–5735. doi: 10.1074/jbc.270.11.5729. [DOI] [PubMed] [Google Scholar]
- 17.Papanicolaou G A, Medeiros A A, Jacoby G A. Novel plasmid-mediated β-lactamase (MIR-1) conferring resistance to oxyimino- and α-methoxy β-lactams in clinical isolates of Klebsiella pneumoniae. Antimicrob Agents Chemother. 1990;34:2200–2209. doi: 10.1128/aac.34.11.2200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sanders C C. Chromosomal cephalosporinases responsible for multiple resistance to newer β-lactam antibiotics. Annu Rev Microbiol. 1987;41:573–593. doi: 10.1146/annurev.mi.41.100187.003041. [DOI] [PubMed] [Google Scholar]
- 19.Sanders C C. β-Lactamases of gram-negative bacteria: new challenges for new drugs. Clin Infect Dis. 1992;14:1089–1099. doi: 10.1093/clinids/14.5.1089. [DOI] [PubMed] [Google Scholar]
- 20.Sanger T, Nicklen S, Coulson A R. DNA sequencing with chain-terminating inhibitors. Proc Natl Acad Sci USA. 1977;74:5463–5467. doi: 10.1073/pnas.74.12.5463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Takeshita S, Sato M, Toba M, Masahashi W, Hashimoto-Gotoh T. High-copy-number plasmid vectors for lacZ α-complementation and chloramphenicol- or kanamycin-resistance selection. Gene. 1987;61:63–74. doi: 10.1016/0378-1119(87)90365-9. [DOI] [PubMed] [Google Scholar]
- 22.Tsukamoto K, Tchibana K, Yamazaki N, Ishii Y, Ujiie K, Nishida N, Sawai T. Role of lysine-67 in the active site of class C β-lactamase from Citrobacter freundii GN346. Eur J Biochem. 1990;188:15–22. doi: 10.1111/j.1432-1033.1990.tb15365.x. [DOI] [PubMed] [Google Scholar]
- 23.Tsukamoto K, Ohono R, Sawai T. Extension of the substrate spectrum by an amino acid substitution at residue 219 in the Citrobacter freundii cephalosporinase. J Bacteriol. 1990;172:4348–4351. doi: 10.1128/jb.172.8.4348-4351.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vieira J, Messing J. The pUC plasmids, an M13mp7-derived system for insertion mutagenesis and sequencing with synthetic universal primers. Gene. 1982;19:259–268. doi: 10.1016/0378-1119(82)90015-4. [DOI] [PubMed] [Google Scholar]
- 25.Watanabe M, Iyobe S, Inoue M, Mitsuhashi S. Transferable imipenem resistance in Pseudomonas aeruginosa. Antimicrob Agents Chemother. 1991;35:147–151. doi: 10.1128/aac.35.1.147. [DOI] [PMC free article] [PubMed] [Google Scholar]