Abstract
The application and provision of prehospital care in disasters and mass-casualty incident response in Europe is currently being explored for opportunities to improve practice. The objective of this translational science study was to align common principles of approach and action and to identify how technology can assist and enhance response. To achieve this objective, the application of a modified Delphi methodology study based on statements derived from key findings of a scoping review was undertaken. This resulted in 18 triage, eight life support and damage control interventions, and 23 process consensus statements. These findings will be utilized in the development of evidence-based prehospital mass-casualty incident response tools and guidelines.
Keywords: disaster, mass casualty, prehospital, trauma
Introduction
Increasing frequency and magnitude of disasters bring to light the constantly emerging risks and the planetary health-related consequences of their impact. 1,2 Consequently, a more integrated approach to prevent and quickly respond to the threat of hazards becoming sudden-onset disasters and mass-casualty incidents is urgently needed. 3,4 Within this goal, the Horizon 2020 Novel Integrated Toolkit for Enhanced Prehospital Life Support and Triage in Challenging and Large Emergencies (NIGHTINGALE) project has been established to support preparedness of first responders during sudden-onset disasters and mass-casualty incidents through the description of evidence-based guidelines for mass-casualty incident triage, prehospital life support and damage control interventions, and prehospital processes together with the creation of a series technological tools that will enhance the first responders capabilities. 5 The need to improve the preparedness and capability of first responders to plan for and respond to these events is consistent with published findings identifying that triage and organization in mass-casualty incidents is a prehospital research priority. 6 This goal is consistent with the Sendai Framework for Disaster Risk Reduction, which identifies the need to improve health system resilience and develop local capacity at all health levels in reducing and addressing disaster risk. 7 The nature of sudden-onset disasters that produce mass-casualty incidents creates challenges in conducting research, such as randomized control trials and conventional prospective studies, due to the unpredictable and uncontrolled nature of the events that lead to more exploratory research methodologies being applied in many cases. 8,9 To overcome this, a modified Delphi study has been conducted to answer the research question: What are the common denominators in the provision of mass-casualty incident triage, prehospital life support and damage control, and prehospital processes to enhance operational capacities during the prehospital management of mass-casualty incidents? 10
A Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) scoping review was performed 11 that extracted and synthesized the evidence base of mass-casualty incident triage, prehospital life support and damage control, and prehospital processes. The findings of this scoping review informed the development of statements utilized in this modified Delphi method study. This expert-based method is widely used to reach consensus and explore assumptions and alternatives. 12–14 This study aimed to produce mass-casualty incident triage, prehospital life support and damage control, and prehospital process consensus statements that will be incorporated in the third stage development of evidence-based prehospital mass-casualty incident response tools and guidelines.
Methods
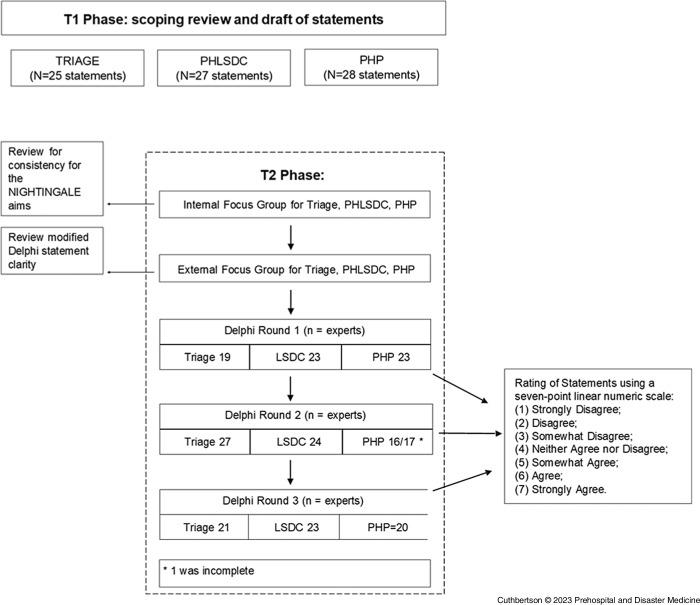
The modified Delphi technique used in this study differs from the standard Delphi approach of using an open questionnaire to retrieve expert data from which these experts offer to create statements (Figure 1). Once statements are created, these experts provide their opinions to achieve group consensus in subsequent Delphi stages. 15 The modification of this study applied the outcomes of a previously conducted PRISMA-ScR scoping review to capture data related to the research topic in a robust, valid manner. 16
Figure 1.
Modified Delphi Flowchart.
Abbreviations: PHLSDC, prehospital life support and damage control interventions; PHP, prehospital processes; LSDC, life support and damage control interventions; NIGHTINGALE, Novel Integrated Toolkit for Enhanced Prehospital Life Support and Triage in Challenging and Large Emergencies.
Data retrieved has been analyzed and synthesized into three initial sets of statements, brought to the attention of internal focus groups (IFGs) and external focus groups (EFGs) to produce the final Delphi statements (Figure 1).
Three IFGs for mass-casualty incident triage, prehospital life support and damage control, and prehospital processes were conducted in parallel in January and February 2022. Participants comprised expert practitioners and researchers in mass-casualty incident response. Experts were engaged in three parallel one-hour video conferences and then exchanged drafts via email to review the three sets of draft statements produced from the scoping review, to render them clear, concise, and consistent with the objectives of NIGHTINGALE.
To reduce risk of bias from the statement creation process, three EFGs were conducted. Participants included international experts not engaged in the NIGHTINGALE project, comprising practitioners and researchers in the field of mass-casualty incident triage, prehospital life support and damage control, and prehospital processes, who were identified as authors of relevant references discovered during the scoping review, or members of scientific societies, namely the European Society for Trauma and Emergency Surgery (ESTES; Vienna, Austria), the World Association for Disaster and Emergency Medicine (WADEM; Madison, Wisconsin USA), and the National Association of Emergency Medical Services Physicians (NAEMSP; Atlanta, Georgia USA). Experts participated in three parallel one-hour video conferences and then exchanged drafts via email, intending to ensure that the three sets of statements met the specifics of the Delphi format, that statements are preferred over questions, and that one statement discusses one fact.
Delphi Rounds
The three expert round modified Delphi were conducted from March 14 through April 11, 2022 using the Stat59 platform (STAT59 Services Ltd; Edmonton, Alberta, Canada). Recruited experts included operational first responders, academic researchers identified among the authors of included scoping review references, alumni of the European Master of Disaster Medicine (EMDM), and members of the professional scientific societies that were not focus group participants from ESTES, WADEM, and NAEMSP as experts in the field of either mass-casualty incident triage, prehospital life support and damage control, or prehospital processes. Experts that did not meet these criteria were excluded.
In the present research, the rationale underlying the selection of experts was based on their geographic distribution and the heterogeneity of the overall group of experts in terms of domains of expertise to establish geographic coverage and a balanced distribution of expertise related to disaster management practices considered.
Following the methodology of Weinstein, et al, 17 experts who agreed received a formal explanation of the modified Delphi, and the first modified Delphi round questionnaire with 25 triage, 27 prehospital life support and damage control, and 28 prehospital process statements with instruction to rank each statement on a seven-point linear numeric scale with one = “Strongly Disagree” to seven = “Strongly Agree” and four demographic questions. Consensus among experts was defined as a standard deviation (SD) ≤1.0.
Statements that attained consensus after this first expert round were included in the final report, while those that were not in agreement but reached consensus were removed from further consideration. Statements not reaching consensus advanced to the second expert round. For this second expert round (and subsequent rounds if required), the mean response of the experts for the remaining statements and their own response for each of them were displayed. The experts were asked to reconsider their seven-point linear numeric scale. The final report lists all statements reaching consensus.
The McLeod Health Institutional Review Board Office (Florence, South Carolina USA) has determined that this study does meet the exemption criteria found at 45 CFR 46.104(d)(2). 18
Data Analysis
Descriptive statistics of the mean and SD were calculated. The response rate was calculated as the percentage of experts who responded in each round (Table 5).
Table 5.
Delphi Expert Response Rate
| Number of Delphi Experts | Response Rate = # of Delphi Experts in this Round/ Initial # of Delphi Experts |
|||||
|---|---|---|---|---|---|---|
| Triage | Prehospital Life Support and Damage Control | Prehospital Processes | Triage | Prehospital Life Support and Damage Control | Prehospital Processes | |
| First Round | 19 | 23 | 23 | |||
| Second Round | 27 | 24 | 16/17 a | 27/19 = 1.42 b | 24/23 = 1.04 b | 16/23 = 0.69; 17/23 = 0.74 |
| Third Round | 21 | 23 | 20 | 21/19 = 1.10 c | 23/23 = 1 c | 20/23 = 0.87 |
This Round 1 expert offered their opinion on 5/17 statements of which five reached group consensus and 12 did not reach consensus.
More experts participated in the second round.
Some experts left the third round after participating in the second round.
Results
Sixty-two (62) international experts were recruited to participate in the modified Delphi study. Recruitment demographic characteristics of the recruited experts are presented in Table 1. The outcomes of the three modified Delphi expert rounds are illustrated in Table 2.
Table 1.
Demographic Characteristics of Delphi Experts
| Triage, n (%) 18 experts |
PHLSDC, n (%) 22 experts |
PHP, n (%) 22 experts |
|
|---|---|---|---|
| Years of Expertise in the Field: | |||
| Less < than 5 | 9 (50.0%) | 2 (9.1%) | 1 (4.5%) |
| Less < than 10 | 3 (16.7%) | 6 (27.3%) | 4 (18.2%) |
| Less < than 15 | 0 (0.0%) | 3 (13.6%) | 5 (22.7%) |
| Less < than 20 | 5 (27.7%) | 6 (27.3%) | 1 (4.5%) |
| Greater > than 20 | 1 (5.5%) | 2 (9.1%) | 10 (45.5%) |
| N/A | 0 (0.0%) | 3 (13.6%) | 1 (4.5%) |
| Location of Mass-Casualty Practice (World Bank Regions) | |||
| East Asia and Pacific | 2 (11.1%) | 2 (9.1%) | – |
| Europe and Central Asia | 11 (61.1%) | 13 (59.1%) | 14 (63.6%) |
| Middle East and North Africa | 1 (5.6%) | 3 (13.7%) | 5 (22.7%) |
| North America | 3 (16.7%) | 4 (18.2%) | 2 (9.1%) |
| Sub-Saharan Africa | 1 (5.6%) | – | 1 (4.5%) |
| Primary Employment | |||
| Governmental Organization | 7 (38.9%) | 11 (50.0%) | 9 (40.9%) |
| Nongovernmental Organization | 3 (16.7%) | 2 (9.1%) | 2 (9.1%) |
| Private Sector | 2 (11.1%) | 4 (18.2%) | 2 (9.1%) |
| University | 4 (22.2%) | 4 (18.2%) | 7 (31.8%) |
| Other | 2 (11.1%) | 1 (4.5%) | 2 (9.1%) |
| Current Profession (Multiple Choice Allowed) | |||
| Administration and Support | 3 | 4 | 4 |
| EMT/Paramedic | 2 | – | 3 |
| Education/Training | 9 | 15 | 2 |
| Fire Fighter | – | – | 2 |
| Nurse | – | – | 2 |
| Physician | 16 | 21 | 16 |
| Public Safety | – | 1 | 2 |
| Research | 7 | 8 | 14 |
| Response/Field Operations | 7 | 9 | 10 |
| Simulation Coder/Designer/Creator | 1 | 5 | 3 |
| Other | 3 | 1 | 2 |
Abbreviation: PHLSDC, prehospital life support and damage control interventions; PHP, prehospital processes; EMT, emergency medical technician.
Table 2.
Modified Delphi Statement Consensus Outcomes
| Modified Delphi Outcomes | ||||||
|---|---|---|---|---|---|---|
| Theme | Initial | Round 1 | Round 2 | Round 3 | Attained | Not Attained |
| Triage | 25 | 10 | 4 | 4 | 18 | 7 |
| Prehospital Life Support and Damage Control | 27 | 2 | 4 | 2 | 8 | 19 |
| Prehospital Processes | 28 | 11 | 11 | 1 | 23 | 5 |
| Total | 80 | 23 | 19 | 7 | 49 | 31 |
The consensus outcomes of this study were 18 mass-casualty incident triage, eight prehospital life support and damage control, and 23 prehospital process statements, as shown in Table 3.
Table 3.
Triage, Prehospital Life Support and Damage Control, and Prehospital Process Statements that Achieved Consensus
| Theme | Statements | Mean Score |
Standard Deviation |
|---|---|---|---|
| Triage | Triage is an on-going and repetitive process throughout the continuum from the initial assessment through definitive care. | 6.6 | 0.7 |
| Each triage system should allow for dynamic triage decisions based on changes in available treatment and transportation resources. | 6.4 | 1.0 | |
| Each triage system should be inclusive of all populations. | 6.3 | 1.0 | |
| Each triage system should be simple, easy to remember, amenable to quick memory aids, and just-in-time training for trained first responders. | 6.7 | 0.7 | |
| Each triage system should be practical for use in an austere environment. | 6.5 | 0.7 | |
| Each triage system should require that the assigned triage category for each patient be visibly identifiable and/or by patients being sent to a specific assigned location as a group of similar triaged patients. | 6.3 | 0.9 | |
| It should be possible to perform the initial assessment without diagnostic equipment. | 6.5 | 0.8 | |
| Patients categorized or considered as expectant should be provided with treatment and/or transport as resources become available. | 6.6 | 0.7 | |
| Efficient use of transport assets may include mixing categories of patients and using alternate forms of transport. | 6.2 | 0.5 | |
| Use of ultrasound may be incorporated in the continuum of prehospital care. | 6.2 | 1.0 | |
| Each jurisdiction should require that all first response agencies utilize the same triage system for any mass-casualty incident response in that jurisdiction. | 6.5 | 0.9 | |
| Each triage system should allow for dynamic triage decisions based on changes in patient conditions. | 6.6 | 0.7 | |
| Each triage system should be inclusive of all ages. | 6.0 | 0.7 | |
| The field trauma score may be used to guide life-saving and damage control interventions. | 5.0 | 0.9 | |
| Each jurisdiction should develop clinical guidelines for priority transportation decisions to match the patient to the appropriate definitive health care facility. | 5.7 | 0.9 | |
| Each triage system should develop a continuum of repeated assessments of available vital signs. | 5.8 | 0.9 | |
| Each jurisdiction should develop clinical guidelines for priority life support and damage control intervention. | 5.4 | 1.0 | |
| Each first response agency should develop protocols for use of monitoring equipment. | 5.2 | 0.9 | |
| Prehospital Life Support and Damage Control | Pain management should be considered for the injured and when performing interventions. | 6.7 | 0.7 |
| Each jurisdiction should document life support and damage control intervention in a patient care record. | 6.3 | 0.6 | |
| Each medical first response agency should develop crush injury treatment guidelines, education, and training to achieve and maintain competencies. | 6.2 | 1.0 | |
| Each medical first response agency should develop clinical guidelines, education, and training to achieve and maintain competencies to utilize intraosseous access to achieve rapid vascular access. | 6.4 | 0.9 | |
| Each first response agency should utilize a formal evidence-based framework for post-incident evaluation that defines and assesses key performance indicators. | 6.0 | 1.0 | |
| Each jurisdiction should create guidelines to utilize spontaneous first providers/bystanders. | 5.6 | 0.9 | |
| Each medical first response agency should develop permissive hypotension clinical guidelines, education, and training to achieve and maintain competencies. | 5.9 | 1.0 | |
| After life-saving interventions are performed, the continued monitoring of the patient can be assigned to a provider of lesser training (ie, physician to paramedic or Emergency Medical Technician/EMT, paramedic to EMT or first responder with medical training). | 5.4 | 1.0 | |
| Prehospital Processes | Each jurisdiction’s prehospital processes should be inclusive of all populations. | 6.4 | 0.9 |
| Each jurisdiction should develop contingency plans for casualty collection points (ie, advanced medical posts, field hospitals, alternate care sites, repurposing health care facilities) to meet the demand of mass-casualty incident response. | 6.6 | 0.5 | |
| If available, each jurisdiction should apply technology to recognize and locate emergency response vehicles at all times. | 6.2 | 1.0 | |
| Transport information management systems enhance coordination of patient distribution. | 6.6 | 0.8 | |
| Information management systems enhance coordination of resources (ie, staff, stuff, structures). | 6.5 | 0.8 | |
| Each jurisdiction should have contingencies to manage transport disruption caused by a mass-casualty incident (ie, earthquake destroying road/rail). | 6.5 | 0.6 | |
| Each jurisdiction should apply evidence-based key performance indicators to evaluate and improve the mass-casualty incident response. | 6.4 | 0.8 | |
| The mass-casualty incident response plan should be based on the jurisdiction hazard vulnerability and risk analysis. | 6.3 | 1.0 | |
| Each jurisdiction mass-casualty incident response plan should include a structured debrief of the exercise or actual mass-casualty incident by all participating first response agencies, where possible. | 6.4 | 0.8 | |
| Each jurisdiction should ensure mass-casualty incident response plan education, training, and competencies are consistent across first response agencies. | 6.6 | 0.6 | |
| Assessment, observation, and monitoring technology and devices that have capacity for storing and transmitting data enhance mass-casualty incident response. | 5.9 | 0.8 | |
| Each jurisdiction should define mass-casualty incident response terminology utilized by all first response agencies in this jurisdiction. | 6.6 | 0.6 | |
| Each jurisdiction’s prehospital processes should be inclusive of all ages. | 6.5 | 0.7 | |
| Each jurisdiction should develop search and rescue guidelines. | 6.2 | 1.0 | |
| Each jurisdiction should develop search and rescue education, training, and competencies. | 6.2 | 1.0 | |
| Each jurisdiction should develop mass-casualty incident Chemical, Biological, Radiological, and Nuclear (CBRN) decontamination education, training, and competencies. | 6.2 | 0.9 | |
| Each jurisdiction should develop communication technology backup for all first response agencies in the jurisdiction. | 6.6 | 0.7 | |
| Each jurisdiction should develop a single patient identification method utilized across all first response agencies. | 6.3 | 1.0 | |
| Evaluation of an exercise or actual mass-casualty incident event should be completed by all participating first response agencies. | 6.5 | 0.6 | |
| Each jurisdiction mass-casualty incident plan should be designed to be consistent with the jurisdictional incident management system. | 6.8 | 0.4 | |
| Each jurisdiction mass-casualty incident response plan should be designed to be consistent with the jurisdictional health authority legislation and regulations. | 6.4 | 0.9 | |
| Unmanned aerial vehicle/UAV technology enhances mass-casualty incident response situational awareness. | 5.5 | 0.8 | |
| Unmanned aerial vehicle/UAV technology enhances mass-casualty incident response operations. | 5.7 | 0.9 |
Abbreviations: EMT, emergency medical technician; CBRN, Chemical, Biological, Radiological, and Nuclear; UAV, unmanned aerial vehicle.
The statements that did not reach consensus outcomes of this study were six triage statements, 17 prehospital life support and damage control statements, and five prehospital processes statements, as shown in Table 4.
Table 4.
Triage, Prehospital Life Support and Damage Control, and Prehospital Process Statements that Did Not Achieve Consensus with SD >1.0 after Three Delphi Expert Rounds
| Theme | Statements | Mean Score |
|---|---|---|
| Triage | 1. Patients should be assigned a triage category, as defined by the first response agency, according to their condition after any life-saving interventions. | 5.2 |
| 2. Each first response agency should develop specific education, training, and competencies for their specific jurisdiction triage system. | 5.8 | |
| 3. Each triage system should be based on the jurisdiction hazard vulnerability and risk analysis. | 4.7 | |
| 4. The shock index may be used to guide life-saving and damage control interventions. | 4.2 | |
| 5. The pulse pressure may be used to guide life-saving and damage control interventions. | 3.9 | |
| 6. The heart rate variability may be used to guide life-saving and damage control interventions. | 4.0 | |
| Prehospital Life Support and Damage Control | 1. Each first response agency should develop crush injury incident recognition guidelines, education, and training to achieve and maintain competencies. | 5.6 |
| 2. Materials for crush injury resuscitation should be included on every medical first response vehicle. | 5.2 | |
| 3. Each first response agency should develop life-threatening hemorrhage control guidelines, education, and training to achieve and maintain competencies. | 6.6 | |
| 4. Each first response agency should develop life-threatening hemorrhage first provider/bystander training and education programs that interface with the first response agency. | 5.7 | |
| 5. Each first response agency should develop CBRNE incident recognition, education, and training to achieve and maintain competencies. | 5.7 | |
| 6. Each first response agency should develop CBRNE incident clinical guidelines, education, and training to achieve and maintain competencies. | 5.1 | |
| 7. Each first response agency should develop an awareness of the need for specific CBRNE antidotes and to deliver these to the scene. | 4.6 | |
| 8. When feasible, the medical first response agency should develop blood product use clinical guidelines, education, and training to achieve and maintain competencies and to deliver these to the scene. | 4.9 | |
| 9. Each medical first agency should develop tranexamic acid (TXA) clinical guidelines, education, and training to achieve and maintain competencies. | 5.8 | |
| 10. Each first response agency should develop mass hypothermia monitoring and treatment guidelines. | 5.5 | |
| 11. First responders should only perform interventions within their scope of practice. | 6.0 | |
| 12. Each first response agency should develop smoke inhalation education and training to achieve and maintain competencies. | 5.7 | |
| 13. Each medical first response agency should develop clinical guidelines, education, and training to achieve and maintain competencies to treat the specific patient with hypotension due to hemorrhage and a declining level of consciousness without clear evidence of a head injury. | 6.5 | |
| 14. Each medical first response agency should develop blunt and penetrating chest trauma education and training to achieve and maintain competencies. | 6.3 | |
| 15. Deployable technology should employ evidence-based physiologic parameters and undergo clinical evaluation before utilization. | 5.8 | |
| 16. Each medical first response agency should evaluate the use of the motor Glasgow Coma Score (mGCS) in certain clinical scenarios in preference to the total Glasgow Coma Score (tGCS). | 4.1 | |
| 17. Each jurisdiction should utilize a patient consent process for interventions. | 4.3 | |
| Prehospital Processes | 1. Each jurisdiction should develop mass-casualty incident CBRNE decontamination guidelines. | 6.0 |
| 2. Each jurisdiction should define futility of care. | 5.0 | |
| 3. Each jurisdiction should develop community response education and training to active shooter. | 5.2 | |
| 4. Each jurisdiction should develop first responder plans, education training, and competencies for active shooter events. | 5.4 | |
| 5. Where possible, a jurisdiction should apply telemedicine technology and processes to support the mass-casualty incident event response. | 5.6 |
Abbreviation: CBRNE, Chemical, Biological, Radiological, Nuclear, and Explosives
This study produced nine statements that reached a consensus that referred to components of mass-casualty incident triage systems. Key themes of triage practices that the statements identified included the following:
A singular triage system should be consistently applied by the agency or agencies and be inclusive of all ages and populations.
First responders’ initial triage should be simplified and done without the aid of diagnostic equipment, and it should produce a clear indicator of the patient triage category.
Mass-casualty incident triage is an on-going process clinically guided, and priority categories should be revised with frequent re-assessments guided by patient clinical status after response to life support and damage control interventions, which should change accordingly to the response to these interventions as more resources become available with the goal to achieve priority transportation.
Additionally, six triage statements met consensus with themes of triage application accuracy, first responder agency competency, and protocol to develop clinical triage key performance indicators. There was limited consensus of statements on practice related to prehospital life support and damage control theme. Of the 27 statements, only eight met consensus, of which respondents were in favor of guideline development for pain relief, documentation of care, rapid vascular access utilizing intraosseous access, hypotension management, scope of care, and outcomes measurement. Key areas of treatment guidance that did not meet statement consensus included first responder/first response agency hemorrhage treatment; Chemical, Biological, Radiological, Nuclear, and high yield Explosive (CBRNE) treatment; hypothermia treatment; and smoke inhalation treatment and monitoring.
Regarding the statements that attained consensus, the need for each first response agency to develop guidelines, education, and training on management of permissive hypotension, rapid vascular access, crush injury management, and pain relief were specifically related to treatment.
Prehospital processes refer to the organizational structures and operational management practices that coordinate deployment and utilization of resources, patient response, dispatch and transport, and non-clinical activities that organize prehospital capability to mass-casualty incident response. This study achieved consensus on 23 of the 28 statements that underwent modified Delphi review.
Discussion
The expert consensus triage, prehospital life support and damage control, and prehospital process statements produced in this modified Delphi study inform the development of toolkits and clinical guidelines to respond to mass-casualty incidents to meet the NIGHTINGALE project objectives.
Triage
Mass-casualty incident triage findings produced by this study are congruent with observed challenges or absence of validation of triage systems in mass-casualty incidents. Validation of triage practices has been predominantly informed by practice in daily care of traumatic patients rather than mass-casualty incidents. The challenge in doing so lies in the fact that the profile of daily practice circumstances is totally different. Delgado, et al have published findings of a triage system calculated from patients involved in a mass-casualty incident showing both sensitivity and specificity of tool accuracy. 19
Consensus of the participants of this modified Delphi study proposed advancement of the current concept of mass-casualty incident triage, from the initial sorting of injured patients into a static triage category to a dynamic continuum of care. Achieving this would require continuous sorting of mass-casualty incident casualties as the resources of staff, stuff, and structure necessary to meet demand are deployed. The goal of mass-casualty incident triage is to identify those patients requiring life support and damage control interventions during all the phases of the priority transport to definitive care.
The importance of standardizing and employing a consistency in practice related to the continuum of mass-casualty incident triage is relevant when considering the existing literature, from which multiple mass-casualty incident triage practices developed globally have emerged. Bazyar, et al identified 20 different triage practices employed world-wide used for the initial assessment of mass-casualty incident victims with variations in sensitivity and sensitivity. 20 Such variance creates a risk of the potential use of multiple or differing methods, which may result in suboptimal decision making and resource allocation. 20 Compounding this, initial triage inaccuracy has been reported in research conducted by Kahn, et al who examined outcomes of Simple Triage and Rapid Treatment (START). 21
In a mass-casualty incident with the mismatch between the demand of an unknown number of patients with unknown injuries and the dynamic accumulation of prehospital resources, the assignment of a triage category with re-assessments based on prehospital life support and damage control will change based on the treatment response and the volume of accumulating patients that are also undergoing treatment and re-assessments, which are competing for priority transport.
Priority transport decisions to various destinations in a mass-casualty incident are dynamic, as patients are not transported directly from the scene to the hospital. There are delays due to many factors with prehospital life support and damage control and other treatments to be administered in the field. The introduction of mass-casualty incident Key Performance Indicators, which examine the dynamic continuous sorting of patients to receive prehospital life support and damage control and priority transport, may enhance outcomes. Such practices have been considered; the findings of Gonzalos, et al resulted in the introduction of a “red surgical category,” which informs evacuation priority to the closest surgical hospital the respective patient may need. 22
The outcomes of a systematic review conducted by Marcussen, et al showed inconsistency in initial mass-casualty incident triage allocation and accuracy between system types SIEVE, 23 SMART Tag system, 24 and CareFlight. 25 The need for consistency in application is also supported by the accepted statement recommending triage education and training in this research. The application of resource-scarce mass-casualty incident triage is rarely a day-to-day skill of first responders; when required, staff should be conversant and skilled in its application to achieve the most significant outcome effect. Not having a robust education and training program risks inappropriate or inaccurate continuous triage, and as Kennedy, et al noted: “The disaster situation is not the time to try out a system for the first time.” 26 This finding is consistent with the outcomes of this study recommending that triage systems should be simple, easy to remember, amenable to quick memory aids, and just-in-time training for trained first responders. This encourages a jurisdiction to design or incorporate existing triage systems compatible with all first-responding agencies. The results of this modified Delphi study provide an opportunity to consider a nuanced approach to disaster triage that recognizes the context of population hazards and vulnerabilities. Further exploration of the efficacy in achieving and implementing this is warranted. Further insights on triage can be gathered by statements that did not achieve consensus. In particular, the modified Delphi participants did not reach consensus on statements related to monitoring. Given the focus of the NIGHTINGALE project technology developments, this finding is significant in the creation and development of any patient monitoring enhancements.
Prehospital Life Support and Damage Control
Of the three areas of practice investigated, prehospital life support and damage control achieved limited consensus on proposed statements comparative to triage and processes (eight statements versus 18 and 23, respectively). Where consensus was achieved related to treatment, it was confined to specific areas of practice (ie, crush and hypotension). Crush injury guidance in disasters has most often been examined in post-earthquake settings, resulting in the development of consensus statements to provide guidance. 27,28 The findings of this modified Delphi study underpin the need for responder education, training, and guidance in the management of crush injury as a possible consequence in all disaster types, as tornadoes, building collapses due to terrorism and asymmetric warfare, faulty construction, and other causes create a risk of crush injuries.
The consensus achieved on statements related to permissive hypotension and rapid vascular access using intraosseous access suggests that focused trauma management is specifically recommended by the modified Delphi experts. This is pertinent as the type, frequency, and impact of sudden-onset disasters are changing, placing risk in new areas that may not have been previously identified in hazard vulnerability analysis. Multiple scene mass-casualty incidents following a targeted terror attack or mass-shooting events of civilian populations and asymmetrical warfare create a need for improved capability of first responders and health care workers in trauma management. In a comprehensive review on permissive hypotension used to treat hemorrhagic shock following trauma, Albreiki, et al discovered that it is both practical and safe to use permissive hypotension to treat hemorrhagic shock in prehospital and in-hospital settings. 29 The study by Albreiki, et al recommended further trials to assess the effectiveness of this practice on survival rates, in conjunction with the statement from this study that achieved consensus research in field use for disaster response, is warranted. 29
The available research and evidence related to the provision of analgesia in disasters to inform practice is limited.
Whilst several conference proceedings and medical texts describing the current state of evidence in this area or proposing treatment practices exists, there is limited literature exploring pain relief practice after sudden-onset disasters. 30–36 Key areas of analgesia practice in contemporary research focus on use of nerve block interventions and ketamine as an analgesic agent in the field. 37–40 Stewart’s summary of potential options for consideration of field analgesia identifies need for further research and guidance on development of administration techniques suitable for field use and consideration of safe options of pain relief. 41 This modified Delphi study recognizes and underpins the need for provision of analgesia in mass-casualty incident response and furthers the call for research to describe best practice and novel administration in resource-scarce mass-casualty incidents after sudden-onset disasters.
The need for obtaining patient consent was also identified by the modified Delphi experts. In the setting of a mass-casualty incident after a sudden-onset disaster, this is of particular significance in guidance to domestic and international response teams to inform an ethical response framework for care. Disaster ethics have been previously considered by Geale, et al as requiring further development and maturity that considers the scope of practice of responders and ensuring that the rights of the patient, including consent to treatment, are upheld in events resulting in mass-casualty incidents. 42
Prehospital Processes
Mass-casualty incident response prehospital processes are undergoing rapid change due to new and emerging technologies. Identification and adaptation of such technology adopted in other industries offers potential enhancement of existing prehospital response processes. Technological developments in telemedicine, artificial intelligence, drone technology, active shooter response, diagnostic equipment, and live data feeds of resource systems offer additional or enhanced tools to disaster responders. Such enhancements can potentially enable more effective priority transportation of patients with efficient and effective hospital distribution to match the patient with the most capable facility. 43 Equally, the learning gained from active shooter mass-casualty incidents offers opportunities to update prehospital response plans and processes. 44
The use of mobile apps to support triage and patient assessment was explored in a systematic review by Montano, et al who found that the development of apps should ensure accessibility and continuity of care between prehospital and hospital providers and include treatment guidelines for responders. 45 Of note, the use of telemedicine to support mass-casualty incident response did not meet consensus as a proposed statement in this modified Delphi. It was also noted that proper testing should be conducted before field implementation when technology is to be introduced. Contemporary research shows that incidents of active armed offenders, particularly active shooter mass-casualty incidents, has consequences in some jurisdiction. 46 Despite this, consensus was not achieved on statements related to active armed offender practice.
There was a difference in prehospital process statements achieving consensus regarding guidance for patient treatment by medical first responders versus first responders/first response agencies. This outcome may be related to the higher proportion of physicians participating in the modified Delphi proportionate to first responder participants. Defining futility of care did not reach consensus, mirroring the discussions across jurisdictions in many nations based on religious, cultural, and legal considerations. Mass-casualty incident crisis standards of care after sudden-onset disasters and allocation of scarce resources in such settings remains challenging for prehospital staff. The ethical application of such decisions has resulted in recommendations of establishing frameworks of practice a priori to sudden-onset disaster occurrence. However, the practical establishment of such, including clarity of decision making, remains needed in many situations. 42,47–50
Whilst a Delphi review identifies where consensus is achieved, which subsequently informs guidance for practice, statements that did not achieve consensus may be equally informative. Statements that did not achieve consensus were thematically centered around clinical practices and patient care interventions. Given that a high proportion of Delphi participants were health care practitioners from across a diverse geographical area, a lack of consensus on care warrants further exploration such that common practices desired in care are articulated. The lack of prehospital life support and damage control consensus is a finding and suggests an urgent need for the undertaking of robust research to establish a more substantial evidence base to guide prehospital life support and damage control in the mass-casualty incident resource-scarce environment when the number of patients and their injuries is unknown.
Strengths
Strengths of this project included the engagement of a diverse and international panel of participants of health care practitioners to participate in Delphi statement assessment and review.
Limitations
This review is limited to study design and methodology. This modified Delphi study utilized pre-selected data informed by a PRISMA-ScR scoping review of prehospital triage, life support and damage control interventions, and the inherent processes to develop draft statements, in contrast to the more standard approach of an open questionnaire to collect such data from experts. The limitations of this process may not have captured relevant references to collect data to incorporate into the creation of the initial draft Delphi statements.
No standard minimum number of experts required for a Delphi study is known, however Franc, et al have described support for a minimum of five. 51 Furthermore, experts are often selected as a function of their availability to perform the Delphi process, the scope of the consultation, or their expertise in that field. 14 In addition, the selected number of experts needs to account for the fact that, from one round to another, the number of experts willing to participate can drop significantly. 52 Therefore, specific authors recommend the number of experts to be lower than 50, 53 while others consider larger values. 15
In this modified Delphi study, there was an improved triage expert response and consistent prehospital life support and damage control expert response, with an inference that this had no bearing on the round-to-round consensus, with the final consensus attained based on stability of the statements not reaching consensus after three rounds. There is no way to know of the varied prehospital process expert response impacted round-to-round consensus with the final consensus attained based on stability of the statements not reaching consensus after three rounds.
Consequently, several methodological decisions were required, including the number of Delphi rounds undertaken, the threshold for defining consensus, and the selection of the experts for Delphi round participation. A common practice for Delphi studies is to cease further rounds when consensus is reached. 52 The optimal number of rounds and the acceptable level of consensus can vary depending on the number of expert participants and the a priori target of the Delphi process undertaken. 52,54
Conclusion
This project provided guidance to enhance mass-casualty incident response triage, prehospital damage and life support, and prehospital processes through the modified Delphi scientific process. The consensus statements, in addition to the data collected in the scoping review, will be utilized to inform the creation of mass-casualty incident response toolkits and clinical guidelines in the NIGHTINGALE project.
Acknowledgments
The authors thank the User Partners of the NIGHTINGALE Consortium and the User Advisory Board Members who provided their valuable inputs during the different steps of the project methodology. The authors would like to sincerely acknowledge the time and dedication of the expert Delphi participants, the support of ESTES and the Nightingale project team, and the input of subject matter expertise of Itamar Ashkenazi, Maddalena D’Urso, and Yael Vias Gvirsman in the achievement of this research.
Conflicts of interest/funding
Jeffrey Michael Franc is the CEO and Founder of STAT59. All other authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. This study is supported by the NIGHTINGALE project ‘Novel InteGrated toolkit for enhanced prehospital life support and Triage IN challenging And Large Emergencies.’ This project has received funding from the European Union’s Horizon 2020 research and innovation program under grant agreement No 101021957.
References
- 1. Field CB. Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaption: Special Report of the Intergovernmental Panel on Climate Change. Cambridge, United Kingdom: Cambridge University Press; 2012:p582. [Google Scholar]
- 2. Burkle FM Jr. Future humanitarian crises: challenges for practice, policy, and public health. Prehosp Disaster Med. 2010;25(3):191–199. [DOI] [PubMed] [Google Scholar]
- 3. Palliyaguru R, Amaratunga D, Baldry D. Constructing a holistic approach to disaster risk reduction: the significance of focusing on vulnerability reduction. Disasters. 2014;38(1):45–61. [DOI] [PubMed] [Google Scholar]
- 4. Lavell A, Maskrey A. The future of disaster risk management. Environmental Hazards. 2014;13(4):267–280. [Google Scholar]
- 5. Caviglia M, Cuthbertson JL, Sdongos E, Faccincani R, Ragazzoni L, Weinstein ES. An application example of translational science in disaster medicine: from grant to deliverables. Int J Disaster Risk Reduction. 2023;85:103518. [Google Scholar]
- 6. Delgado RC, Gonzalez KA, Martinez JAC, Alvarez TC, Gonzalez PA. Top research priorities in prehospital care in Spain. Prehosp Disaster Med. 2023;38(1):81–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sendai Framework for Disaster Risk Reduction 2015-2030. UNDRR. https://www.undrr.org/publication/sendai-framework-disaster-risk-reduction-2015-2030. Accessed January 24, 2023.
- 8. Stratton SJ. Is there a scientific basis for disaster health and medicine? Prehosp Disaster Med. 2014;29(3):221–222. [DOI] [PubMed] [Google Scholar]
- 9. Stratton SJ. Data sampling strategies for disaster and emergency health research. Prehosp Disaster Med. 2019;34(3):227–229. [DOI] [PubMed] [Google Scholar]
- 10. Weinstein ES, Cuthbertson JL, Herbert TL, et al. Advancing the scientific study of prehospital mass-casualty response through a translational science process: the T1 scoping literature review stage. Eur J Trauma Emerg Surg. 2023. Epub ahead of print. [DOI] [PMC free article] [PubMed]
- 11. Hsu CC, Sandford BA. The Delphi Technique: making sense of consensus. Practical Assessment, Research, and Evaluation. 2007;12:10. [Google Scholar]
- 12. Delbecq A, Van de Ven A, Gustafson DH. Group Techniques for Program Planning a Guide to Nominal Group and Delphi Processes. Michigan USA: University of Michigan; 1975. [Google Scholar]
- 13. Williams PL, Webb C. The Delphi technique: a methodological discussion. J Adv Nurs. 1994;19(1):180–186. [DOI] [PubMed] [Google Scholar]
- 14. Alshehri SA, Rezgui Y, Li H. Delphi-based consensus study into a framework of community resilience to disaster. Nat Hazards. 2015;75:2221–2245. [Google Scholar]
- 15. McGowan J, Straus S, Moher D, et al. Reporting scoping reviews-PRISMA ScR extension. J Clin Epidemiol. 2020;123:177–179. [DOI] [PubMed] [Google Scholar]
- 16. Weinstein ES, Cuthbertson JL, Ragazzoni L, Verde M. A T2 translational science modified Delphi study: spinal motion restriction in a resource-scarce environment. Prehosp Disaster Med. 2020;35(5):538–545. [DOI] [PubMed] [Google Scholar]
- 17. Office for Human Research Protections (OHRP). Exemptions (2018 requirements). HHS.gov. https://www.hhs.gov/ohrp/regulations-and-policy/regulations/45-cfr-46/common-rule-subpart-a-46104/index.html. Published December 15, 2021. Accessed January 24, 2023.
- 18. Bazyar J, Farrokhi M, Khankeh H. Triage systems in mass-casualty incidents and disasters: a review study with a world-wide approach. Open Access Maced J Med Sci. 2019;7(3):482–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Delgado RC, Gan RK, García VC, González PA. Sensitivity and specificity of Spanish Prehospital Advanced Triage Method (META). Prehosp Disaster Med. 2022;37(3):321–326. [DOI] [PubMed] [Google Scholar]
- 20. Kahn CA, Schultz CH, Miller KT, Anderson CL. Does START triage work? An outcomes assessment after a disaster. Ann Emerg Med. 2009;54(3):424–430.e1. [DOI] [PubMed] [Google Scholar]
- 21. Cuttance G, Dansie K, Rayner T. Paramedic application of a triage sieve: a paper-based exercise. Prehosp Disaster Med. 2017;32(1):3–13. [DOI] [PubMed] [Google Scholar]
- 22. González PA, Delgado RC, Álvarez TC, et al. Ten years using the advanced triage model for out-of-hospital emergencies (META): the 2020 version. Emergencias. 2021;33(5):387–391. [PubMed] [Google Scholar]
- 23. Cone DC, Serra J, Kurland L. Comparison of the SALT and Smart triage systems using a virtual reality simulator with paramedic students. Eur J Emerg Med. 2011;18(6):314–321. [DOI] [PubMed] [Google Scholar]
- 24. Marcussen CE, Bräuner KB, Alstrøm H, Møller AM. Accuracy of prehospital triage systems for mass-casualty incidents in trauma register studies - a systematic review and meta-analysis of diagnostic test accuracy studies. Injury. 2022;53(8):2725–2733. [DOI] [PubMed] [Google Scholar]
- 25. Kennedy K, Aghababian RV, Gans L, Lewis CP. Triage: techniques and applications in decision making. Ann Emerg Med. 1996;28(2):136–144. [DOI] [PubMed] [Google Scholar]
- 26. Lerner EB, Schwartz RB, Coule PL, et al. Mass-casualty triage: an evaluation of the data and development of a proposed national guideline. Disaster Med Public Health Prep. 2008;2 Suppl 1:S25–S34. [DOI] [PubMed] [Google Scholar]
- 27. Li W, Qian J, Liu X, et al. Management of severe crush injury in a front-line tent ICU after 2008 Wenchuan earthquake in China: an experience with 32 cases. Crit Care. 2009;13(6):R178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gibney RT, Sever MS, Vanholder RC. Disaster nephrology: crush injury and beyond. Kidney Int. 2014;85(5):1049–1057. [DOI] [PubMed] [Google Scholar]
- 29. Albreiki M, Voegeli D. Permissive hypotensive resuscitation in adult patients with traumatic hemorrhagic shock: a systematic review. Eur J Trauma Emerg Surg. 2018;44(2):191–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Zorab J. Relief of Pain and Suffering in Disaster Situations. In: Resuscitation and Life Support in Disasters Relief of Pain and Suffering in Disaster Situations. Berlin, West Germany: Springer; 1980:p63–65. [Google Scholar]
- 31. Frey R, Safar P. Resuscitation and Life Support in Disasters. In: Relief of Pain and Suffering in Disaster Situations: Proceedings of the International Congress on Disaster Medicine. Mainz 1977, Part II. Berlin, West Germany: Springer-Verlag; 1980. [Google Scholar]
- 32. Buckenmaier CC. Acute pain management in field and disaster situations. In: Clinical Pain Management: Acute Pain. London, United Kingdom: CRC Press; 2008:p374–388. [Google Scholar]
- 33. McIssac J, McQueen K, Kucik C. In: McIssac J, (ed). Essentials of Disaster Anesthesia. Cambridge, United Kingdom: Cambridge University Press; 2020. [Google Scholar]
- 34. Jackson T, Pena M, McQueen K, Kucik C. Pain in Disasters. In: McIsaac J, (ed). Essentials of Disaster Anesthesia. Cambridge, United Kingdom: Cambridge University Press; 2020:143–156. [Google Scholar]
- 35. Theodosopoulou P, Moutafi M, Kalogridaki M, et al. Acute pain management in the emergency and disaster setting, a narrative review of the literature. Regional Anesthesia Pain Medicine. 2022;47:A112–A113. [Google Scholar]
- 36. Malchow RJ, Black IH. The evolution of pain management in the critically ill trauma patient: emerging concepts from the global war on terrorism. Crit Care Med. 2008;36(7 Suppl):S346–S357. [DOI] [PubMed] [Google Scholar]
- 37. Lippert SC, Nagdev A, Stone MB, Herring A, Norris R. Pain control in disaster settings: a role for ultrasound-guided nerve blocks. Ann Emerg Med. 2013;61(6):690–696. [DOI] [PubMed] [Google Scholar]
- 38. Visser E, Schug SA. The role of ketamine in pain management. Biomed Pharmacother. 2006;60(7):341–348. [DOI] [PubMed] [Google Scholar]
- 39. Levine AC, Teicher C, Aluisio AR, et al. Regional Anesthesia for Painful Injuries after Disasters (RAPID): study protocol for a randomized controlled trial. Trials. 2016;17(1):542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Stewart RD. Analgesia in the field. Prehosp Disaster Med. 1989;4(1):31–34. [Google Scholar]
- 41. Geale SK. The ethics of disaster management. Disaster Prevention and Management. 2012;21(4)445–462. [Google Scholar]
- 42. Chou C-C, Chiang W-C, Chen AY. Emergency medical response in mass-casualty incidents considering the traffic congestions in proximity on-site and hospital delays. Transport Res Part E Logist Transport Rev. 2022;158:102591. [Google Scholar]
- 43. Aylwin CJ, König TC, Brennan NW, et al. Reduction in critical mortality in urban mass-casualty incidents: analysis of triage, surge, and resource use after the London bombings on July 7, 2005. Lancet. 2006;368(9554):2219–2225. [DOI] [PubMed] [Google Scholar]
- 44. Montano IH, de la Torre Díez I, López-Izquierdo R, Villamor MAC, Martín-Rodríguez F. Mobile triage applications: a systematic review in literature and play store. J Med Syst. 2021;45(9):86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Blair JP, Schwieit KW. A study of active shooter incidents in the United States between 2000 and 2013. US Department of Justice; 2014. https://www.fbi.gov/file-repository/active-shooter-study-2000-2013-1.pdf/view. Accessed January 24, 2023.
- 46. Mariaselvam S, Gopichandran V. The Chennai floods of 2015: urgent need for ethical disaster management guidelines. Indian J Med Ethics. 2016;1(2):91–95. [DOI] [PubMed] [Google Scholar]
- 47. Dean M, Payne D. Disaster management: an ethical review and approach. International Journal of Emergency Management. 2013;9:(2)113–126. [Google Scholar]
- 48. Leider JP, DeBruin D, Reynolds N, Koch A, Seaberg J. Ethical guidance for disaster response, specifically around crisis standards of care: a systematic review. Am J Public Health. 2017;107(9):e1–e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Committee on Guidance for Establishing Crisis Standards of Care for Use in Disaster Situations; Institute of Medicine. Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response. Washington, DC USA: National Academies Press; 2012. [PubMed] [Google Scholar]
- 50. Cere G, Rezgui Y, Zhao W. Urban-scale framework for assessing the resilience of buildings informed by a Delphi expert consultation. Int J Disaster Risk Reduct. 2019;36:101079. [Google Scholar]
- 51. Franc JM, Hung KK, Pirisi A, Weinstein ES. Analysis of Delphi study 7-point linear scale data by parametric methods: use of the mean and standard deviation. Methodological Innovations. 2023. Epub ahead of print.
- 52. Witkin, BR , Altschuld JW. Planning and Conducting Needs Assessments: A Practical Guide. Thousand Oaks, California USA: Sage Publications; 1996. [Google Scholar]
- 53. Dalkey N. An experimental study of group opinion: the Delphi method. Futures. 1969;1(5):408–426. [Google Scholar]
- 54. Cyphert F, Grant W. The Delphi technique: a case study. Phi Delta Kappan. 1971;42:272–273. [Google Scholar]