Abstract
Postural assessment can help doctors and therapists identify risk factors for low back pain and determine appropriate follow-up treatment.
Postural alignment is not perfectly symmetrical, and small asymmetries can instead represent norms and criteria for postural evaluation.
It is necessary to comprehensively observe patients’ posture in all directions and analyze the factors related to posture evaluation.
The results of reliability show that in general intra-rater reliability is higher than inter-rater reliability, and inclinometers are being more reliable than other instrumentations.
Some common postural problems can cause lumbar discomfort, and prolonged poor posture is a potential risk factor for lumbar spine injuries.
On the basis of previous studies on posture evaluation, a unified standardized method for posture evaluation must be established in future research.
Keywords: posture assessment, low back pain, reliability, spinal posture
Introduction
Low back pain is a major cause of disability worldwide (1). Hartvigsen J et al. found that the rate of disability caused by low back pain increased by 54% from 1990 to 2015 due to the population explosion and increased aging (2). This condition also has a high recurrence rate, and the persistent pain brings great distress and economic burden to patients. Low back pain is a common public health problem, especially in low- and middle-income countries (2). Approximately 84% of people reported suffering from low back pain during their lifetime, and 23% eventually developed chronic low back pain (3).
From a clinical point of view, spinal problems are classified as structural and non-structural. Structural misalignment of the spine is defined as the presence of some morphological abnormality in the bones and soft tissues. Structural dislocation of the spine mainly includes some specific clinical disease types, such as idiopathic scoliosis, congenital scoliosis or kyphosis, neuromuscular scoliosis, neurofibroma, mesenchymal disease, malnutrition, and metabolic disorders combined with spinal malformations (4). Non-structural misalignment of the spine is mainly caused by poor posture, uneven muscle distribution, nerve root irritation, and certain inflammation (5). Due to the different characteristics of the two spinal deformities, this paper mainly discusses the postural assessment of non-structural spinal deformities.
Body posture is mainly described as the arrangement of various human body parts and their connections. Common postural abnormalities for low back pain include lordosis, sway-back, round back/kyphosis, flat back, and scoliosis. Poor posture can negatively affect the spinal posture and flexibility of white-collar workers, and chronic poor posture may be linked to chronic nonspecific low back pain (6).
In addition to the postural problems, radiating angle parameters of the spine pelvis and spinal deformity are also correlated (7). A controlled clinical trial comparing standing sagittal radiographs of healthy people and patients with chronic low back pain found that patients with low back pain had less distal segmental lordosis but more proximal lumbar lordosis and more vertical sacrum (8). In asymptomatic patients, the relationship between lumbar lordosis in standing position and pelvic tilt angle was weak (9). On the other hand, patients reported more pain and deformity in the lower lumbar stage than in the upper lumbar stage due to the greater degree of degeneration in the lower lumbar segment (10, 11, 12). In addition, the asymmetry of the pelvis and the abnormal position between the pelvis and the lumbar spine can lead to varying degrees of pain and spinal deformity and even have an adverse effect on the biological lines of the lower extremities, causing pain in other areas (13).
Many previous clinical studies have focused on postural and balance assessments to examine physical conditions in older adults (14). Some diseases can lead to abnormal posture, such as scoliosis and stroke. A quantitative functional assessment of movement in people with scoliosis was conducted using 3D biomechanical models (15). Abnormal postures may also have the opposite effects of causing pain and increasing the risk of sports injuries. For example, flat feet and high arches can alter the limb line and increase the risks (16). A cross-sectional study found that people who use computers on a daily basis reported more shoulder and neck pain and numbness than those who do not use computers (17). An abnormal patella position can lead to knee dysfunction and patella femoral imbalance, which eventually cause pain (18). Studies have used varying techniques and instruments to measure and evaluate different people’s postures. However, a review to confirm the consensus on the correct assessment of postures and the reliability of different assessment methods is still lacking. The current work aims to provide a review on correct posture, reliability of different assessments, and potential relationship between postural abnormalities and low back pain.
Key points of spinal posture assessment
In an upright position, the pressure on the body is evenly distributed across the joint surfaces. This position was named as standard posture. In this stance, the body can be divided into anterior, lateral, and posterior views, each with a specific standard posture.
Anterior view
The anterior view can easily identify some structural problems. A study designed a new evaluation method for anterior view imaging and analyzed its effectiveness to improve its detection level (19). In general, when viewed from the front, the head should be facing straight forward without rotation or side bending. The shoulders and locks on both sides should be at the same level. The navel should be squarely in the center without deviation to the left or right. The bilateral anterior superior iliac spine is equal in height, and the distance from the line of gravity of the body is equal. Both knees are of equal height, with the patella facing forward and of equal height. The femur and tibia are erect without internal or external rotation, and the muscles in both legs are similar in shape and size without muscle atrophy or swelling. Bilateral medial malleoli have equal height, and the foot sole faces slightly outward from the midline of the body (Fig. 1). A particular muscle appearing prominent may indicate a high muscle tone. Maintaining this stance for a long time may lead to pain in that area. Some patients with nonspecific low back pain may have a high muscle tone in the lower back.
Figure 1.
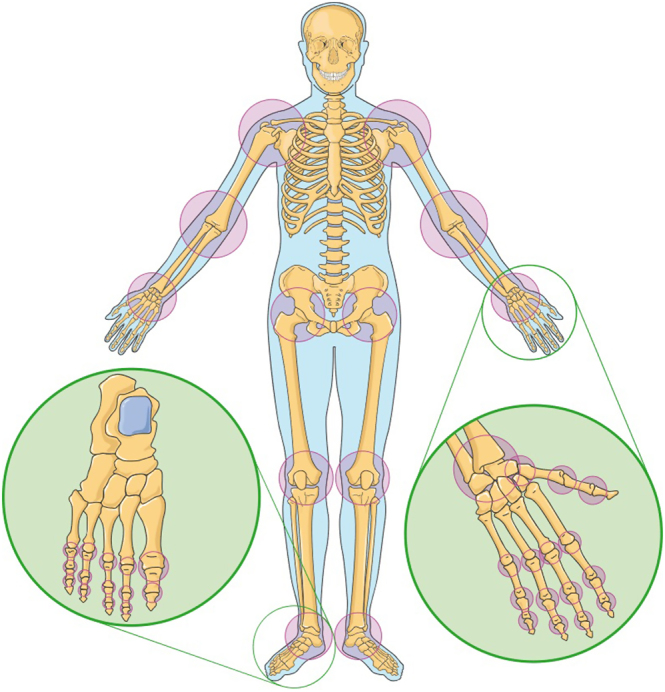
The anterior view of body.
Lateral view
Lateral observation can compensate for some of the problems missed in anterior and posterior observation and can be used to establish a sagittal plane model and a 3D model with anterior and posterior observation of human body posture (20). When viewed from the side, the head should be aligned with the chest, and the chin should be free of receding and lordosis. The cervical spine has normal physiological curvature without deformation and degeneration. Both shoulder joints have no internal or external rotation. The thoracic vertebra has a normal physiological curvature, and the double chest is naturally and comfortably erected. The lumbar spine has a normal lordosis without a flat back. The anterior superior iliac spine is at the same level as the pubic bone. The anterior superior iliac spine and the posterior superior iliac spine are equal in height. The pelvis does not lean forward and backward. No flexion or over-extension of the knee is visible in the standing position. The ankle joint has a normal dorsiflexion angle (Fig. 2). As shown from the side, a person spending a long time at the desk will develop a hunched posture over time. Long-term poor posture will also lead to shoulder and waist pain.
Figure 2.
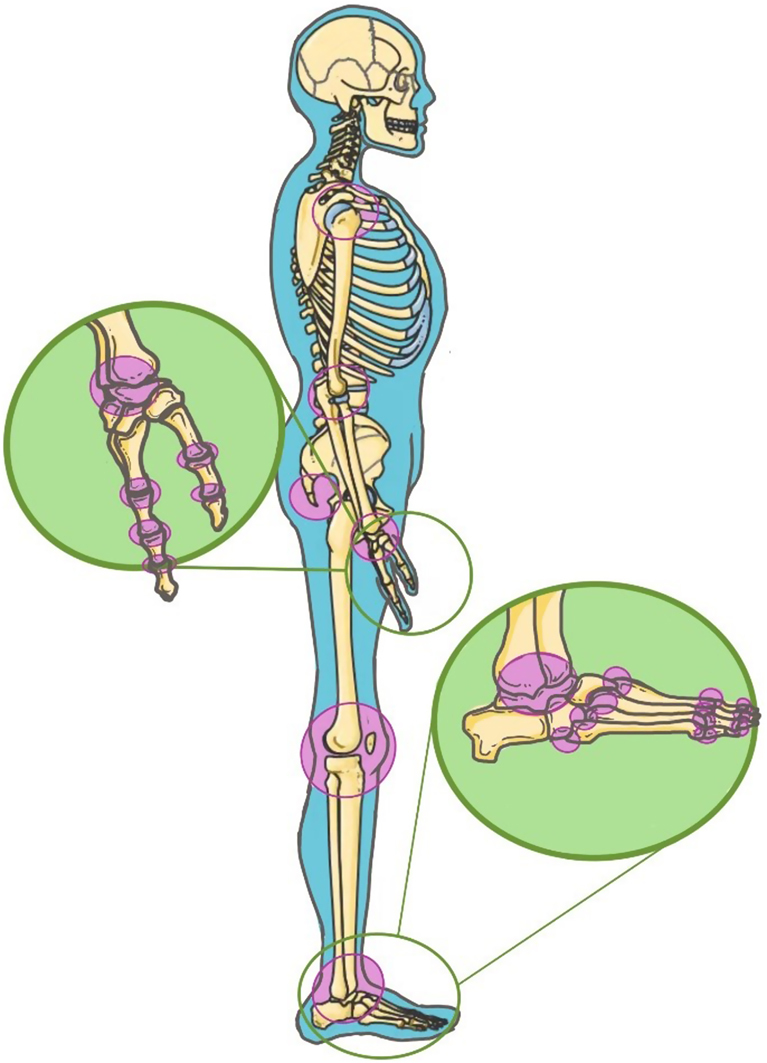
The lateral view of body.
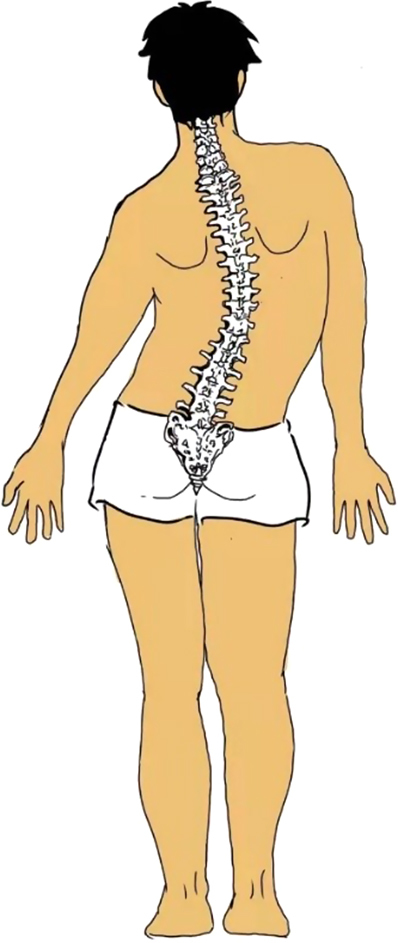
Posterior view
The posterior view is the gold standard for pelvic posture assessment (21). When viewed from behind, the head should be facing straight forward without rotation or side bending, and the neck should be upright without side bending. Shoulders should be about the same height on each side and may be slightly lower on the dominant side. The arms are naturally drooping on both sides and equidistant from the body, with elbows and wrists on both sides at equal height. Bilateral shoulder blades are equidistant from the spine, flat to the ribs, not sloping forward, and showing equal height at the subscapular angle without lifting, sinking, and rotation. The lumbar spine is straight without left and right bulges. The distance between the posterior and superior iliac spines of both sides and the midline of the body is equal. The greater trochanter of the femur is equal in height, and the gluteal line of both sides is equal in height. Both legs are erect and at an equal distance from the midline of the body without knee joint varus, and bilateral gastrocnemius muscles are similar in size and shape. The ankle is medial and lateral equal in height, the Achilles tendon and calcaneus are erect, and the sole of the foot is slightly everted (Fig. 3). Prolonged poor posture can lead to lumbar scoliosis, which can cause pain. Slight asymmetry in the pelvis and scapula showing up in the posterior view is normal (22).
Figure 3.
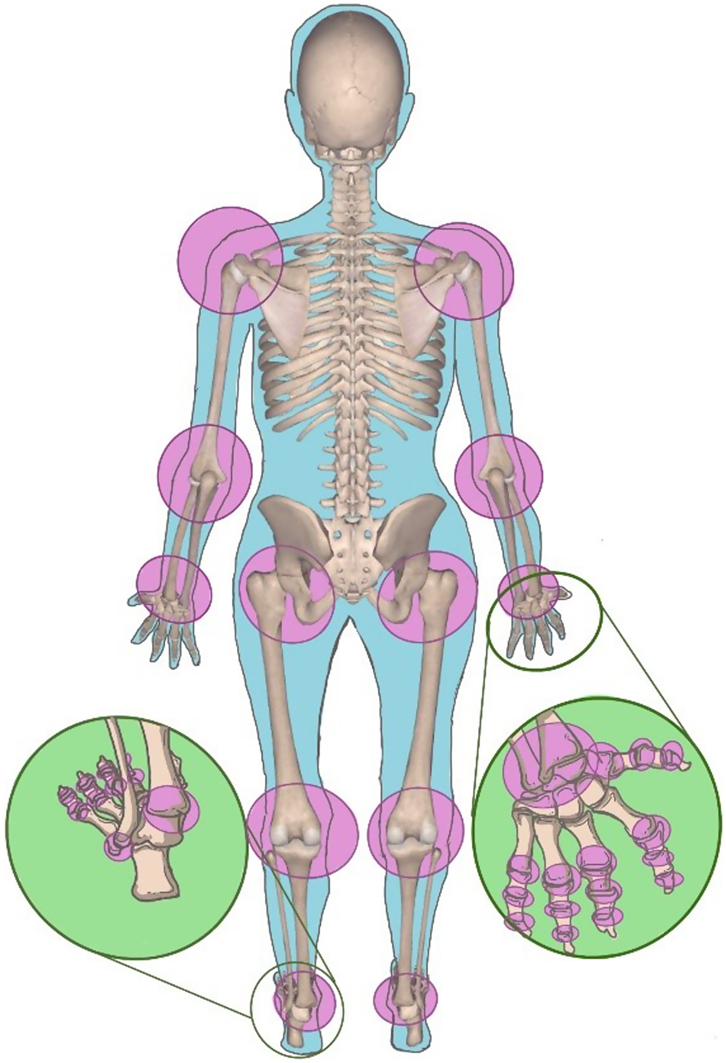
The posterior view of body.
Postural alignment is not perfectly symmetrical, and small asymmetries can instead represent norms and criteria for postural evaluation (22). This assessment can be accomplished in a standing or sitting position. The assessed person must be observed on the spot where he or she usually works. A substantial change in the sitting posture might be noted at the beginning of the work and after a period of time.
Influencing factors of spinal posture
Understanding the factors that affect different postures can help distinguish which postures can be corrected with physical therapy, require long-term behavioral changes, or cannot be changed. Some common factors and examples that affect body posture are shown in Table 1.
Table 1.
The influencing factors of abnormal posture.
| Influencing factors | Examples |
|---|---|
| Structural or anatomical | Scoliosis; difference in bone length of upper limbs or lower limbs; proliferation of vertebral body or frame |
| Aging | Various degenerative changes; childhood postures are markedly different from postures of other ages |
| Physiological | There are temporary slight differences in posture between different states, such as being active and tired; we may adopt a position to relieve pain, but if we hold it for a long time, it can have long-lasting effects; physical changes during pregnancy are temporary, but sometimes lead to permanent compensatory changes |
| Pathological | Illness can change our posture, especially when it comes to bone and joint diseases; improper alignment of bone during fracture healing may result in changes in bone profile; some pathological changes in muscle tone may also contribute to postural changes |
| Occupational | There were significant differences between mental and manual workers and between high physical activity levels and sedentary jobs |
| Entertainment | People who enjoy different forms of entertainment also have certain posture differences |
| Environmental | People feel cold or warm feeling will present different posture |
| Social and cultural | Different living habits have different effects on posture |
| Emotional | Different emotions can cause different postures, and some pain in patients tend to take defensive postures |
Observing the different states of the patients and understanding the influencing factors related to posture assessment allow physical therapists to obtain useful information and give their own judgments for the convenience of subsequent treatment.
Reliability of measurements for spinal posture assessment
With its increasing importance, different methods have been developed for postural assessment. Table 2 describes the samples used in 18 articles and the instruments used for the assessment. Most of the studies discussed the reliability of different assessment and measurement methods in healthy populations and different disease populations. The results showed that the intra-rater reliability was higher than inter-rater reliability in the vast majority of tests (Table 3). A cross-sectional study validated the trunk appearance perception scale for physicians as a reliable and valid scale for assessing the severity of malformation in patients with idiopathic scoliosis (23). An Ovako work posture assessment system used observational assessment methods to identify work-related musculoskeletal disorders with good inter-rater reliability and found that upper extremity assessment is more reliable than lower extremity assessment (24). Another work investigated the measurement techniques used to assess thoracic dexterity. Inclinometer and manual assessments found strong intra-rater and inter-rater reliabilities, with intra-rater reliability being higher than inter-rater and inclinometers being more reliable than other instrumentations (25).
Table 2.
Sample description and instruments used in the different studies.
| Reference | Sample characteristics | Instrument methods | |
|---|---|---|---|
| Participants, n | Age, years | ||
| Yang et al. (52) | 60 asymptomatic adults | >45 | Three (standing, prone, and sitting) positions simple maximal isometric BES |
| Lee et al. (53) | 4 novice observers | ISPM method | |
| Cary et al. (54) | 20 HP (clinical experience: 2–42 years; mean: 16.7± 12.4) | View a pre-recorded video about six categories in sleep postures | |
| Gallego-Izquierdo et al. (55) | 44 | 23.30 ± 4.44 | Two experienced and trained physiotherapists assessing cervical posture using mobile application, forward head posture, and photogrammetry. |
| Mani et al. (56) | 11 with non-specific neck pain | Face-to-face and telerehabilitation methods | |
| Vieira et al. (57) | 60 (30 with and 30 without neck pain (Age: years)) | 27.8 | Photogrammetry: quantifying the static body posture alignments and angles |
| Visual inspection: indicate the presence of postural misalignment and neck pain | |||
| Lins et al. (24) | 20 volunteers | OWAS | |
| Takatalo et al. (25) | 32 (F: 16; M: 16) | 39 | Observation: TS posture |
| Tape measure: TS mobility | |||
| Inclinometer: mobility in a seated position and TS posture in sitting and standing positions | |||
| Hopkins et al. (58) | 50 asymptomatic males | 24.04 ± 1.81 | PSM iOS application compared with VICON 3D |
| Gardiner et al. (59) | 40 with axSpA | IMU sensors measure the maximum range of movement at the cervical and lumbar spine. | |
| Ruthard et al. (60) | 28 (girls: 10) children with cerebral palsy | 9.7 ± 3.1 | SM measure children with cerebral palsy |
| Yu et al. (61) | 28 healthy and 28 with non-specific chronic low back pain | 18–30 | GPS to assess pelvic asymmetry |
| Pimentel-Santos et al. (62) | 17 (M: 8) healthy | 18–50 | MTM (stiffness, elasticity, and tone) and ultrasound-based SWE (shear modulus) |
| Carvalho et al. (63) | 21 asymptomatic patients | Clinical measures related to forward shoulder posture | |
| Martinez et al. (64) | 42 volunteers | FPI | |
| Paraskevopoulos et al. (66) | 10 male asymptomatic professional volleyball players (BMI: 23.1 ± 0.32 kg/m2) | 30.5 ± 2.67 | Several evaluation methods of SA |
| Yeung et al. (65) | 33 preoperative AIS patients | 18.4 ± 4.2 | EOS was used to scan the whole thoracic spine at upright position |
| CT scan was used to evaluate the spine in prone position | |||
| The three-dimensional reconstruction of EOS and CT of the spine were then generated | |||
| Matamalas et al. (23) | 52 idiopathic scoliosis patients | 6.6 | TAPS-Phy |
BES, back extensor strength; F, females; FPI, Foot Posture Index; GPS, Global Postural System; HP, health professionals; ISPM, inertial measurement unit sensor-based posture-matching; M, males; MTM, Myotonometry; OWAS, Ovako Working Posture Assessment System; PSM, Posture Screen Mobile; SA, Scapular asymmetries; SM, Spinal Mouse®; SWE, shear-wave elastography; TAPS-Phy, Trunk appearance perception scale for physicians.
Table 3.
Reliability of spinal postural assessments in different studies.
| Reference | Reliability, ICC | |
|---|---|---|
| Inter-rater | Intra-rater | |
| Yang et al. (52) | No | Repeated after 1 week |
| Standing posture | 0.92 | |
| Prone posture | 0.93 | |
| Sitting posture | 0.90 | |
| Lee et al. (53) | No | |
| Shoulder and elbow | κ = 0.41, κ w= 0.52, ks = 0.89 | |
| Wrist | κ = 0.20, κ w = 0.26, ks = 0.52 | |
| Trunk | κ = 0.89, κw = 0.89, ks = 0.26 | |
| Cary et al. (54) | Repeated after 2 days | |
| Fleiss Kappa | 0.83 (95% CI: 0.82–0.84) | |
| Cohen’s Kappa | 0.93 (95% CI: 0.80–1.0) | |
| Gallego-Izquierdo et al. (55) | 0.85 | 0.88 |
| Mani et al. (56) | Repeated after 1 h | |
| 0.96–0.99 | 0.93–0.99 | |
| Vieira et al. (57) | ||
| Photogrammetry | ||
| Hip angle | 0.564 | 0.502 |
| Ankle angle | 0.996 | |
| Head vertical alignment | 0.995 | |
| Visual inspection | −0.002 (−0.036; 0.014)* | |
| Lins et al. (24) | No | |
| Arms | 98%, ks = 0.98 | |
| Legs | 66–97%, ks = 0.85 | |
| Upper body | 80–96%, ks = 0.85 | |
| Takatalo et al. (25) | Repeated after 1 day | |
| Inclinometer measurements | ||
| sitting | 0.85 | 0.84 |
| standing | 0.81 | 0.86 |
| Tape measurements | 0.74 | 0.86 |
| Hopkins et al. (58) | ||
| Sagittal plane hip shift | 0.74 ± 0.05 | |
| Frontal plane hip shift | 0.23 ± 0.08 | |
| Gardiner et al. (59) | ||
| IMU test | No | 0.94–0.97 |
| Ruthard et al. (60) | No | Repeated after 2 days |
| Sagittal and frontal plane | 0.69–0.99 | |
| Yu et al. (61) | Repeated after 1 week | |
| Height of the ASIS from the platform left | 0.96; s.e.m.= 1.35; MDD95= 3.74 | 0.99; s.e.m . = 0.79; MDD95= 2.20 |
| Pimentel-Santos et al. (62) | No | |
| MTM | ≥0.90 | |
| SWE | ≥0.85 | |
| Carvalho et al. (63) | ||
| AWI, ATI, and TC | 0.82–0.85 | 0.77–0.94† |
| Martinez et al. (64) | ||
| Dominant lower limb | 0.91 | 0.90 |
| Nondominant lower limb | 0.94 | 0.92 |
| Paraskevopoulos et al. (66) | ||
| First and second methods | 0.90–0.97;s.e.m.= 0.17–0.16 | 0.90–0.98; s.e.m. = 0.16–0.13 |
| Third method | 0.84–0.92; s.e.m. : 0.23–0.13 | 0.84–0.92; s.e.m.: 0.23–0.13 |
| Last two methods | 0.70–0.68; S.E.M. = 0.23–0.27 | 0.66–0.77; S.E.M. = 0.20 |
| Yeung et al. (65) | ||
| EOS (uprightposition) | 0.903 | 0.969 |
| CT (prone position) | 0.961 | 0.985 |
| Matamalas et al. (23) | ||
| Cronbach’s alpha coefficient | 0.84 | |
| κw | 0.14–0.63 | 0.35–0.99 |
*Value is from Janson and Olsson’s iota (95% CI); †includes PMI and SI.
AIS, adolescent idiopathic scoliosis; ATI, acromion to the treatment table index; AWI, acromion to the wall index; CT, computed tomography; EOS, biplanar stereoradiography; ICC, intraclass correlation coefficient; IMU, inertial measurement unit; κ, Fleiss kappa; κ w, Conger-weighted kappa coefficients; k s, kappa scores; κ L, light’s kappa; I=; axSpA, axial spondyloarthritis; PMI, pectoralis minor index; SD, standard deviation; SI, scapular index; TC, thoracic curvature.
Common spinal poor posture for low back pain
Some common postural problems can cause lumbar discomfort, and prolonged poor posture is a potential risk factor for lumbar spine injuries. Lumbar discomfort and injury can compensatively increase the number of postural problems, such as lack of muscle strength, poor stability of deep muscle core, holding the same position for a long time, and poor muscle flexibility. Poor posture increases mechanical stress in the lower back, which can lead to low back pain (26). Common bad postures for low back pain include lumbar lordosis, sway-back, round back, flat back, and scoliosis (Fig. 4). A PubMed search was conducted to obtain articles on the above five lumbar diseases related to bad posture.
Figure 4.
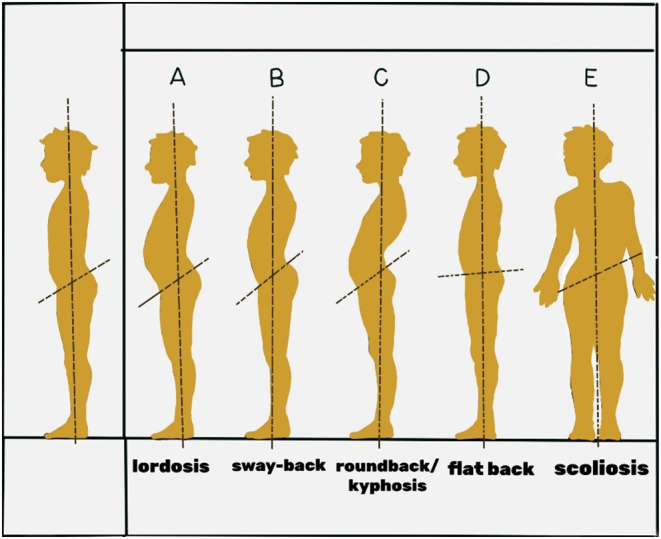
Common bad posture.
Lordosis
Lordosis is characterized by the excessive forward tilt of the pelvis and increased lordosis of the lumbar spine and is accompanied by the forward movement of the spine and tilt of the pelvis (Fig. 5) (27). Lumbar lordosis curvature (LLC) is a unique structural feature of the normal adult human spine and is yet to be described in some clinical areas as the root cause of low back pain (28). Several studies have discussed the relationship between lumbar lordotic curvature and low back pain. In general, lumbar lordosis is less common in the lumbar lordotic angle than in the general healthy population, and low back pain due to lumbar disc herniation is strongly associated with lumbar lordotic angle loss in certain diseases (28). For lumbar lordosis, the Williams back exercises and the McKenzie stretching exercises can improve lumbar mobility and strengthen hip and abdominal muscles. McKenzie emphasizes lumbar stretching exercises, and Williams focuses on waist flexion exercises and core stability exercises. Table 4 summarizes some physiological changes due to lordosis, including body position, muscle changes, and affected joints.
Figure 5.

Lordosis.
Table 4.
Physiological changes according to lordosis, kyphosis, flat back, and scoliosis.
| Changes according to | ||||
|---|---|---|---|---|
| Lordosis | Kyphosis | Flat back | Scoliosis | |
| Body alignment position | Lumbar lordosis, pelvis forward tilt, pelvic angle may increase to 40° (normal pelvic angle is about 30°). | Kyphosis is described as an abnormal round back flexion. In adolescents, the normal thoracic kyphosis angle is 20–40°, and more than 45° can be clinically diagnosed as kyphosis. | Lumbar lordosis is reduced, the hip joints are straight, the knee joints are slightly bent, and the pelvis is about 20° backward. | The spine is skewed to one side and the horizontal angle (Cobb angle) of the segment of the skewed vertebral body is more than 10° [35]. When there is a difference in the length of the legs, the lumbar spine and pelvis tilt to compensate for the balance of the shoulders, and functional scoliosis is prone to occur. |
| Elongated and weakened muscles | Abdominal muscles (rectus abdominis, internal and external oblique), neck extensors, erector spine of the upper back, deep core stabilizers of lumbar spine (transverse abdominis, multifidus). | Cervical flexors (Scalenus, sternocleidomastoid), rhomboids, middle and lower trapezius, paravertebral muscles. | The muscle degeneration of the lumbar and dorsal extensor groups is serious (latissimus dorsi, rhomboid, erector spinae, trapezius, etc.). Hip flexion group (iliopsoas, quadriceps femoris, sartorius, etc.). | The muscles on the bulging side of the back and gluteal abductor on the concave side in scoliosis are lower in strength and more relaxed, resulting in lower overall back strength. |
| Shorter and stronger muscles | Lumbar stretch muscles (erector spinae, trapezius, etc.), hip flexors (iliopsoas, rectus femoris, sartorius, etc.), neck extensors, hamstring muscles. | Cervical extensors (trapezius, semispinalis capitis, etc.), hip flexors (iliopsoas, quadriceps femoris, sartorius, etc.), abdominal muscles. | Abdominal muscles are in a state of contraction and tension (such as rectus abdominis, transverse abdominis, internal and external oblique muscles); hip stretch muscles (gluteus maximus, biceps femoris, semitendinosus, semimembranosus, etc.). | The gluteal adductor group on the concave and convex side of the back has a higher degree of muscle tone and stiffness. |
| Affected joints | The cervix–thoracic joint and lumbosacral joint appeared in a slump position. Lumbar lordosis is closely related to degenerative joint diseases of the lumbar spine. | The thoracic and shoulder blade joints flexion, and the lumbar joint pressure increases. | The lumbar lordosis angle was reduced, the hip joint was straight, the knee was slightly flexion, and the cervical spine was slightly forward. | The deviation of the spine to one side, the elevation of the pelvis on the side of the thoracic or lumbar spine, the asymmetry of the lumbosacral joints, and excessive joint movement are risk factors for idiopathic scoliosis. |
Sway-back
Sway-back is one of the common types of non-structural misalignments of body posture (5). This position is passive because it relies on passive structures such as ligaments to maintain an upright position against its own gravity (29). Only a few articles related to sway-back and low back pain were available, and only one document was retrieved. The review assessed the evidence for spinal function and low back pain based on lower limb biomechanical data (30). The main features of a sway-back are forward movement of the head, elongated cervical vertebrae, flattening of the lower lumbar region, waist curvature and flattening, slight backward tilt of the pelvis, and hip joint accompanied by forward pelvic movement (Fig. 6) (5, 30, 31). Here, the hamstring and upper oblique muscles contract and strengthen, and the single-joint hip flexors, external oblique muscles, upper back extensors, and neck flexors are stretched and weakened. The erector spine muscle contracts isometrically. The sway-back position compensates for abdominal and back muscle weakness by swinging the torso and pelvis, including bending the hips, knees, and ankles (30).
Figure 6.

Sway-back.
Round back/kyphosis
Postural round back is one of the most common abnormal postural conditions (Fig. 7). Most patients have no clinical symptoms, but the pathological kyphosis caused by rickets require clinical intervention (32). Scheuermann Kyphosis is a common cause of excessive kyphosis in adolescents and affects between 1% and 8% of the population (33). A systematic review and meta-analysis of the improvement of yoga in a range of bone and joint diseases found remarkable clinical improvements in the function of clinical indicators of low back pain and fibromyalgia and a favorable enhancement on kyphosis trends (34). A randomized controlled trial presented good results for a technique developed through motion imaging that enhances muscle tissue control combined with flexibility and strength training to improve kyphosis angles and relieve low back pain symptoms (35). Table 4 summarizes some physiological changes due to kyphosis, including body position, muscle changes, and affected joints.
Figure 7.

Round back/kyphosis.
Flat back
The flat back position reduces lumbar lordosis and adversely affects the sagittal balance of the spine (36). This posture is mainly manifested by a reduction in lumbar lordosis angle straightened hip joint, backward tilt of the pelvis, and instability of the lumbar spine. Incorrect standing and sitting posture and excessive lumbar flexion are the underlying factors of flat back posture. This position is a potential source of lower back pain while standing and sitting (Fig. 8) (37, 38). A study examined the effects of an inclined treadmill on pelvic forward angle, hamstring length, and back muscle endurance in patients with flat back and found an increase in pelvic forward angle, knee extension angle, and extensor dorsi endurance after the intervention (39). Table 4 summarizes some physiological changes due to flat back, including body position, muscle changes, and affected joints.
Figure 8.

Flat back.
Scoliosis
Scoliosis is a common musculoskeletal disorder with a rotational component and is generally divided into idiopathic and non-idiopathic (40). Most scoliosis is idiopathic scoliosis, and non-idiopathic scoliosis accounts for only a small proportion, mainly including congenital and neuromuscular scoliosis, mesenchymal disorders, non-structural scoliosis, juvenile kyphosis, and Scheuermann’s disease (41). Severe scoliosis can lead to deformity and places heavy physical and mental burdens on patients (Fig. 9) (42, 43). Idiopathic scoliosis in adolescents is rare and affects 2–3% of the population. This illness usually starts before the age of 10 years and can affect the whole life (44). Idiopathic scoliosis refers to a scoliosis angle (Cobb angle) greater than 10° without any underlying congenital or muscular abnormality (45). Neuromuscular scoliosis may involve the entire thoracolumbar spine and even cause pelvic deformity and thus require complicated treatment and involve a high risk of complications; the incidence of diseases related to the neuromuscular system even can be as high as 90% (43, 46, 47). Scoliosis is often caused by multiple factors including genetic factors and skeletal muscle nerve abnormalities. In addition to surgical treatment, conservative therapies are available, such as exercise therapy and physical manipulation therapy (48, 49). In general, the Cobb angle is between 10° and 25°, and kinesitherapy and manipulative therapy can be considered. Support should be installed for auxiliary treatment between 25° and 50°, and >50° requires surgery (48). Table 4 summarizes the relevant muscles and joints affected by scoliosis.
Figure 9.
Scoliosis.
Conclusion and prospect
Low back pain is one of the most common disorders associated with postural imbalance (50). Spinal postural assessment plays an important role in the assessment of low back pain, and abnormal postural behavior is often a potential risk factor for low back pain and lumbar injury. Many studies have evaluated different postures to determine the best sitting and standing posture. Although consensus on the best posture has not been achieved, erect lordosis is considered a healthy posture (51). Current research on the reliability of posture assessment has focused on healthy people and those with related diseases. In general, the internal reliability is higher than the inter-test reliability, and the measurement reliability of the inclinometer is higher than that of other test instruments (25).
Various methods have been developed for human posture evaluation, and different institutions have varying evaluation standards. Existing low back pain rehabilitation evaluation and exercise rehabilitation treatment methods lack reliability and validity tests and efficacy proof. In addition to postural problems, other studies showed that BMI also has an impact on local lumbar load (10), and future studies can also focus on the impact of weight on postural problems. Academic circles have not established a unified standard to evaluate the posture impairment degree of patients with low back pain. In the future research, a unified and effective posture assessment standard must be developed and popularized to all levels of health care.
ICMJE conflict of interest statement
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding Statement
This work was supported by the Emerging and Cross-Disciplines of Pudong New Area Health Committee Discipline Construction Plan (PWXx2020-02); Featured Clinical Discipline Project of Pudong New Area Health Commission (PWYts2021-10); Talent Development Fund of Shanghai Municipal (2021081); Shanghai Clinical Research Center for Rehabilitation Medicine (21MC1930200).
Data availability
All data included in this study are available upon request from the corresponding author.
References
- 1.Traeger AC Buchbinder R Elshaug AG Croft PR & Maher CG. Care for low back pain: can health systems deliver? Bulletin of the World Health Organization 201997423–433. ( 10.2471/BLT.18.226050) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, Hoy D, Karppinen J, Pransky G, Sieper J, et al. What low back pain is and why we need to pay attention. Lancet 20183912356–2367. ( 10.1016/S0140-6736(1830480-X) [DOI] [PubMed] [Google Scholar]
- 3.Sadler SG Spink MJ Ho A De Jonge XJ & Chuter VH. Restriction in lateral bending range of motion, lumbar lordosis, and hamstring flexibility predicts the development of low back pain: a systematic review of prospective cohort studies. BMC Musculoskeletal Disorders 201718179. ( 10.1186/s12891-017-1534-0) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O'Leary SA Paschos NK Link JM Klineberg EO Hu JC & Athanasiou KA. Facet joints of the spine: structure-function relationships, problems and treatments, and the potential for regeneration. Annual Review of Biomedical Engineering 201820145–170. ( 10.1146/annurev-bioeng-062117-120924) [DOI] [PubMed] [Google Scholar]
- 5.Czaprowski D Stoliński Ł Tyrakowski M Kozinoga M & Kotwicki T. Non-structural misalignments of body posture in the sagittal plane. Scoliosis and Spinal Disorders 2018136. ( 10.1186/s13013-018-0151-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Csuhai ÉA Nagy AC Váradi Z & Veres-Balajti I. Functional analysis of the spine with the Idiag SpinalMouse system among sedentary workers affected by non-specific low back pain. International Journal of Environmental Research and Public Health 202017. ( 10.3390/ijerph17249259) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Evcik D & Yücel A. Lumbar lordosis in acute and chronic low back pain patients. Rheumatology International 200323163–165. ( 10.1007/s00296-002-0268-x) [DOI] [PubMed] [Google Scholar]
- 8.Jackson RP & McManus AC. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size: a prospective controlled clinical study. Spine 1994191611–1618. ( 10.1097/00007632-199407001-00010) [DOI] [PubMed] [Google Scholar]
- 9.Walker ML Rothstein JM Finucane SD & Lamb RL. Relationships between lumbar lordosis, pelvic tilt, and abdominal muscle performance. Physical Therapy 198767512–516. ( 10.1093/ptj/67.4.512) [DOI] [PubMed] [Google Scholar]
- 10.Beattie PF Meyers SP Stratford P Millard RW & Hollenberg GM. Associations between patient report of symptoms and anatomic impairment visible on lumbar magnetic resonance imaging. Spine 200025819–828. ( 10.1097/00007632-200004010-00010) [DOI] [PubMed] [Google Scholar]
- 11.Mitchell T O'Sullivan PB Burnett AF Straker L & Smith A. Regional differences in lumbar spinal posture and the influence of low back pain. BMC Musculoskeletal Disorders 20089152. ( 10.1186/1471-2474-9-152) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Quack C Schenk P Laeubli T Spillmann S Hodler J Michel BA & Klipstein A. Do MRI findings correlate with mobility tests? An explorative analysis of the test validity with regard to structure. European Spine Journal 200716803–812. ( 10.1007/s00586-006-0264-z) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.In TS Jung JH Jung KS & Cho HY. Spinal and pelvic alignment of sitting posture associated with smartphone use in adolescents with low back pain. International Journal of Environmental Research and Public Health 202118. ( 10.3390/ijerph18168369) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jorgensen MG Rathleff MS Laessoe U Caserotti P Nielsen OB & Aagaard P. Time-of-day influences postural balance in older adults. Gait and Posture 201235653–657. ( 10.1016/j.gaitpost.2011.12.018) [DOI] [PubMed] [Google Scholar]
- 15.Kinel E D'Amico M & Roncoletta P. 3D quantitative evaluation of posture and spine proprioceptive perception through instinctive self-correction maneuver in adolescent idiopathic scoliosis. Frontiers in Bioengineering and Biotechnology 20219663394. ( 10.3389/fbioe.2021.663394) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dickerson LC & Queen RM. Foot posture and plantar loading with ankle bracing. Journal of Athletic Training 202156461–472. ( 10.4085/1062-6050-164-20) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Korpinen L Pääkkönen R & Gobba F. White-collar workers' self-reported physical symptoms associated with using computers. International Journal of Occupational Safety and Ergonomics 201218137–147. ( 10.1080/10803548.2012.11076921) [DOI] [PubMed] [Google Scholar]
- 18.Analan PD & Ozdemir H. The effect of patellar height by using Insall Salvati index on pain, function, muscle strength and postural stability in patients with primary knee osteoarthritis. Current Medical Imaging 202117532–538. ( 10.2174/1573405616999200817172649) [DOI] [PubMed] [Google Scholar]
- 19.Ichihara H Onoguchi M Hiyoshi K Saitou T & Abe T. Usefulness of imaging posture using anterior view of the half supine position for sentinel lymphscintigraphy in patients with breast cancer. Nihon Hoshasen Gijutsu Gakkai Zasshi 201268461–467. ( 10.6009/jjrt.2012_jsrt_68.4.461) [DOI] [PubMed] [Google Scholar]
- 20.Huynh PP, Ishii M, Juarez M, Liao D, Darrach HM, Fung N, Nellis JC, Byrne PJ, Boahene KDO, Papel ID, et al. Normal gaze patterns of the face in lateral view. Facial Plastic Surgery and Aesthetic Medicine 20202280–85. ( 10.1089/fpsam.2019.29019.huy) [DOI] [PubMed] [Google Scholar]
- 21.Lazennec JY Brusson A & Rousseau MA. Lumbar-pelvic-femoral balance on sitting and standing lateral radiographs. Orthopaedics and Traumatology, Surgery and Research 201399(1) S87–S103. ( 10.1016/j.otsr.2012.12.003) [DOI] [PubMed] [Google Scholar]
- 22.Ferreira EA Duarte M Maldonado EP Bersanetti AA & Marques AP. Quantitative assessment of postural alignment in young adults based on photographs of anterior, posterior, and lateral views. Journal of Manipulative and Physiological Therapeutics 201134371–380. ( 10.1016/j.jmpt.2011.05.018) [DOI] [PubMed] [Google Scholar]
- 23.Matamalas A D'Agata E Sanchez-Raya J & Bago J. Trunk appearance perception scale for physicians (TAPS-Phy) - a valid and reliable tool to rate trunk deformity in idiopathic scoliosis. Scoliosis and Spinal Disorders 20161124. ( 10.1186/s13013-016-0085-8) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lins C Fudickar S & Hein A. OWAS inter-rater reliability. Applied Ergonomics 202193103357. ( 10.1016/j.apergo.2021.103357) [DOI] [PubMed] [Google Scholar]
- 25.Takatalo J Ylinen J Pienimäki T & Häkkinen A. Intra- and inter-rater reliability of thoracic spine mobility and posture assessments in subjects with thoracic spine pain. BMC Musculoskeletal Disorders 202021529. ( 10.1186/s12891-020-03551-4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hasegawa T Katsuhira J Oka H Fujii T & Matsudaira K. Association of low back load with low back pain during static standing. PLoS One 201813e0208877. ( 10.1371/journal.pone.0208877) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Russell BS Muhlenkamp KA Hoiriis KT & Desimone CM. Measurement of lumbar lordosis in static standing posture with and without high-heeled shoes. Journal of Chiropractic Medicine 201211145–153. ( 10.1016/j.jcm.2012.02.002) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chun SW Lim CY Kim K Hwang J & Chung SG. The relationships between low back pain and lumbar lordosis: a systematic review and meta-analysis. Spine Journal 2017171180–1191. ( 10.1016/j.spinee.2017.04.034) [DOI] [PubMed] [Google Scholar]
- 29.Pezolato A de Vasconcelos EE Defino HL & Nogueira-Barbosa MH. Fat infiltration in the lumbar multifidus and erector spinae muscles in subjects with sway-back posture. European Spine Journal 2012212158–2164. ( 10.1007/s00586-012-2286-z) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McGregor AH & Hukins DW. Lower limb involvement in spinal function and low back pain. Journal of Back and Musculoskeletal Rehabilitation 200922219–222. ( 10.3233/BMR-2009-0239) [DOI] [PubMed] [Google Scholar]
- 31.Roussouly P & Pinheiro-Franco JL. Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. European Spine Journal 201120(Supplement 5) 609–618. ( 10.1007/s00586-011-1928-x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Garoflid N Fragnière B & Dutoit M. "Round back” in children and adolescents. Revue Médicale de la Suisse Romande 2000120815–820. [PubMed] [Google Scholar]
- 33.Huq S Ehresman J Cottrill E Ahmed AK Pennington Z Westbroek EM & Sciubba DM. Treatment approaches for Scheuermann kyphosis: a systematic review of historic and current management. Journal of Neurosurgery. Spine 201932235–247. ( 10.3171/2019.8.SPINE19500) [DOI] [PubMed] [Google Scholar]
- 34.Ward L Stebbings S Cherkin D & Baxter GD. Yoga for functional ability, pain and psychosocial outcomes in musculoskeletal conditions: a systematic review and meta-analysis. Musculoskeletal Care 201311203–217. ( 10.1002/msc.1042) [DOI] [PubMed] [Google Scholar]
- 35.Fairweather MM & Sidaway B. Ideokinetic imagery as a postural development technique. Research Quarterly for Exercise and Sport 199364385–392. ( 10.1080/02701367.1993.10607591) [DOI] [PubMed] [Google Scholar]
- 36.Yoo WG. Effect of individual strengthening exercises for anterior pelvic tilt muscles on back pain, pelvic angle, and lumbar ROMs of a LBP patient with flat back. Journal of Physical Therapy Science 2013251357–1358. ( 10.1589/jpts.25.1357) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gold PM Albright B Anani S & Toner H. Straight Back Syndrome: positive response to spinal manipulation and adjunctive therapy: a case report. Journal of the Canadian Chiropractic Association 201357143–149. [PMC free article] [PubMed] [Google Scholar]
- 38.Shin SS & Yoo WG. Differences in regional and global lumbar angle during slumped sitting and upright sitting among global three subgroups. Journal of Back and Musculoskeletal Rehabilitation 202134877–885. ( 10.3233/BMR-200087) [DOI] [PubMed] [Google Scholar]
- 39.Kim MH & Yoo WG. Effects of inclined treadmill walking on pelvic anterior tilt angle, hamstring muscle length, and trunk muscle endurance of seated workers with flat-back syndrome. Journal of Physical Therapy Science 201426855–856. ( 10.1589/jpts.26.855) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Van Goethem J Van Campenhout A van den Hauwe L & Parizel PM. Scoliosis. Neuroimaging Clinics of North America 200717105–115. ( 10.1016/j.nic.2006.12.001) [DOI] [PubMed] [Google Scholar]
- 41.Viviani GR. Scoliosis screening and treatment. Canadian Family Physician Medecin de Famille Canadien 198531529–533. [PMC free article] [PubMed] [Google Scholar]
- 42.Negrini S Minozzi S Bettany-Saltikov J Chockalingam N Grivas TB Kotwicki T Maruyama T Romano M & Zaina F. Braces for idiopathic scoliosis in adolescents. Cochrane Database of Systematic Reviews 2015Cd006850. ( 10.1002/14651858.CD006850.pub3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vialle R Thévenin-Lemoine C & Mary P. Neuromuscular scoliosis. Orthopaedics and Traumatology, Surgery and Research 201399(1) S124–S139. ( 10.1016/j.otsr.2012.11.002) [DOI] [PubMed] [Google Scholar]
- 44.Romano M Minozzi S Bettany-Saltikov J Zaina F Chockalingam N Kotwicki T Maier-Hennes A & Negrini S. Exercises for adolescent idiopathic scoliosis. Cochrane Database of Systematic Reviews 20122012CD007837. ( 10.1002/14651858.CD007837.pub2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kuznia AL Hernandez AK & Lee LU. Adolescent idiopathic scoliosis: common questions and answers. American Family Physician 202010119–23. [PubMed] [Google Scholar]
- 46.Putzier M Groß C Zahn RK Pumberger M & Strube P. Characteristics of neuromuscular scoliosis. Der Orthopade 201645500–508. ( 10.1007/s00132-016-3272-7) [DOI] [PubMed] [Google Scholar]
- 47.Shao ZX Fang X Lv QB Hu ZC Shao SY Hu YB Wu AM & Wang XY. Comparison of combined anterior-posterior approach versus posterior-only approach in neuromuscular scoliosis: a systematic review and meta-analysis. European Spine Journal 2018272213–2222. ( 10.1007/s00586-018-5702-1) [DOI] [PubMed] [Google Scholar]
- 48.Cassella MC & Hall JE. Current treatment approaches in the nonoperative and operative management of adolescent idiopathic scoliosis. Physical Therapy 199171897–909. ( 10.1093/ptj/71.12.897) [DOI] [PubMed] [Google Scholar]
- 49.Shakil H Iqbal ZA & Al-Ghadir AH. Scoliosis: review of types of curves, etiological theories and conservative treatment. Journal of Back and Musculoskeletal Rehabilitation 201427111–115. ( 10.3233/BMR-130438) [DOI] [PubMed] [Google Scholar]
- 50.Tüzün Ç Yorulmaz İ Cindaş A & Vatan A. Low back pain and posture. Clinical Rheumatology 199918308–312. ( 10.1007/s100670050107) [DOI] [PubMed] [Google Scholar]
- 51.Korakakis V O'Sullivan K O'Sullivan PB Evagelinou V Sotiralis Y Sideris A Sakellariou K Karanasios S & Giakas G. Physiotherapist perceptions of optimal sitting and standing posture. Musculoskeletal Science and Practice 20193924–31. ( 10.1016/j.msksp.2018.11.004) [DOI] [PubMed] [Google Scholar]
- 52.Yang S Wu W Zhang C Wang D Chen C Tang Y Li K Xu J & Luo F. Reliability and validity of three isometric back extensor strength assessments with different test postures. Journal of International Medical Research 202048300060519885268. ( 10.1177/0300060519885268) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lee W Lin J-H & Bao S. Inter-rater reliability of an inertial measurement unit sensor-based posture-matching method: a pilot study. International Journal of Industrial Ergonomics 202080. ( 10.1016/j.ergon.2020.103025) [DOI] [Google Scholar]
- 54.Cary D Collinson R Sterling M & Briffa K. Examining the validity and reliability of a portable sleep posture assessment protocol, using infrared cameras, under a variety of light and bed cover situations in the home environment. Work 201963291–298. ( 10.3233/WOR-192930) [DOI] [PubMed] [Google Scholar]
- 55.Gallego-Izquierdo T Arroba-Díaz E García-Ascoz G Val-Cano MDA Pecos-Martin D & Cano-de-la-Cuerda R. Psychometric proprieties of a mobile application to measure the craniovertebral angle a validation and reliability study. International Journal of Environmental Research and Public Health 202017. ( 10.3390/ijerph17186521) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mani S Sharma S & Singh DK. Concurrent validity and reliability of telerehabilitation-based physiotherapy assessment of cervical spine in adults with non-specific neck pain. Journal of Telemedicine and Telecare 20212788–97. ( 10.1177/1357633X19861802) [DOI] [PubMed] [Google Scholar]
- 57.Vieira ÉCN Meziat-Filho NAM & Ferreira AS. Photogrammetric variables used by physical therapists to detect neck pain and to refer for physiotherapeutic intervention: a cross-sectional study. Journal of Manipulative and Physiological Therapeutics 201942254–266. ( 10.1016/j.jmpt.2018.11.014) [DOI] [PubMed] [Google Scholar]
- 58.Hopkins BB Vehrs PR Fellingham GW George JD Hager R & Ridge ST. Validity and reliability of standing posture measurements using a mobile application. Journal of Manipulative and Physiological Therapeutics 201942132–140. ( 10.1016/j.jmpt.2019.02.003) [DOI] [PubMed] [Google Scholar]
- 59.Gardiner PV Small D Muñoz-Esquivel K Condell J Cuesta-Vargas A Williams J Machado PM & Garrido-Castro JL. Validity and reliability of a sensor-based electronic spinal mobility index for axial spondyloarthritis. Rheumatology 2020593415–3423. ( 10.1093/rheumatology/keaa122) [DOI] [PubMed] [Google Scholar]
- 60.Ruthard K Raabe-Oetker A Ruthard J Oppermann T Duran I & Schönau E. Reliability of a radiation-free, noninvasive and computer-assisted assessment of the spine in children with cerebral palsy. European Spine Journal 202029937–942. ( 10.1007/s00586-020-06328-4) [DOI] [PubMed] [Google Scholar]
- 61.Yu Q Huang H Zhang Z Hu X Li W Li L Chen M Liang Z Lo WLA & Wang C. The association between pelvic asymmetry and non-specific chronic low back pain as assessed by the global postural system. BMC Musculoskeletal Disorders 202021596. ( 10.1186/s12891-020-03617-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pimentel-Santos F, Rodrigues Manica S, Masi AT, Lagoas-Gomes J, Santos MB, Ramiro S, Sepriano A, Nair K, Gomes-Alves P, Costa J, et al. Lumbar myofascial physical properties in healthy adults: myotonometry vs. shear wave elastography measurements. Acta Reumatológica Portuguesa 202146110–119. [PubMed] [Google Scholar]
- 63.Carvalho LACM Aquino CF Souza TR Anjos MTS Lima DBM & Fonseca ST. Clinical measures related to forward shoulder posture: a reliability and correlational study. Journal of Manipulative and Physiological Therapeutics 201942141–147. ( 10.1016/j.jmpt.2019.03.006) [DOI] [PubMed] [Google Scholar]
- 64.Martinez BR Oliveira JC Vieira K & Yi LC. Translation, cross-cultural adaptation, and reliability of the Foot Posture Index (FPI-6) - Brazilian version. Physiotherapy Theory and Practice 202137218–223. ( 10.1080/09593985.2019.1587800) [DOI] [PubMed] [Google Scholar]
- 65.Yeung KH Man GCW Lam TP Ng BKW Cheng JCY & Chu WCW. Accuracy on the preoperative assessment of patients with adolescent idiopathic scoliosis using biplanar low-dose stereoradiography: a comparison with computed tomography. BMC Musculoskeletal Disorders 202021558. ( 10.1186/s12891-020-03561-2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Paraskevopoulos E Sasati D & Papandreou M. Intra-rater and inter-rater reliability of scapular asymmetry measurements in male professional volleyball players. Medicina Dello Sport 201972404–421. ( 10.23736/S0025-7826.19.03523-3) [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data included in this study are available upon request from the corresponding author.



 This work is licensed under a
This work is licensed under a