To the Editor:
The critical care management of patients with pulmonary hypertension (PH) is challenging1 and is associated with high mortality.2, 3, 4, 5 Long-term outcomes of patients with PH who survive an episode of critical illness have not been characterized. Our study aimed to elucidate the clinical features, mortality, and predictors of long-term mortality after an admission to the medical ICU (MICU) in patients with PH.
We conducted a retrospective cohort study of adult groups of 1, 4, or 5 patients with PH enrolled in the Cleveland Clinic PH registry (institutional review board number 8097) admitted to the MICU between January 2009 and June 2011. We collected clinical, functional, hemodynamic, and laboratory data before MICU admission (considered baseline) and during MICU admission. Primary outcome was post-MICU discharge mortality. Study patients were compared with matched patients that did not have a MICU admission during the study period. Patients were matched to be within the same age categories defined by decade, gender, and year of diagnostic right heart catheterization.
Table 1 shows the baseline clinical features of the 63 study patients and the matched PH cohort without a MICU admission. The most common reason for admission was right heart failure (RHF), followed by septic shock. The MICU mortality rate was 22.2% (14/63). Eleven of 14 patients who died in the MICU were admitted for worsening RHF; the remaining three had sepsis. RHF was the cause of death in 64% (9/14).
Table 1.
Baseline Characteristics: Study Group (n = 63) and Matched Group (n = 58)
| Characteristic | Total, Study Group, % | Total, Matched Group, % | P Value |
|---|---|---|---|
| Age, y | 51 ± 15 | 52 ± 15 | .89 |
| Female | 48 (76.2) | 43 (74.1) | > .99 |
| PH categories | .37 | ||
| PAH | 51 (81)a | 47 (81.0.3)b | |
| CTEPH | 6 (9.5) | 6 (10.3) | |
| Miscellaneous | 6 (9.5)c | 4 (6.9)d | |
| 6MWD, m | 273 ± 135 (n = 48) | 286 ± 160 (n = 57) | .2 |
| NYHA class | .054 | ||
| I-II | 14 (33.3) | 16 (53.4) | |
| III-IV | 28 (66.7) | 14 (46.7) | |
| BNP, pg/mL (n = 42) | 451 ± 622 | 276 ± 433 | .045 |
| Pericardial effusion | 14/50 (28.0) | 13/55 (23.6) | .69 |
| Right heart catheterization | |||
| RAP, mm Hg | 12.2 ± 6.6 (n = 58) | 8.2 ± 6.5 | .001 |
| Mean PAP, mm Hg | 54.2 ± 12.5 (n = 60) | 42.2 ± 15.0 | < .001 |
| CI, L/min/m2 | 2.59 ± 1.05 (n = 57) | 2.11 ± 1.7 | .75 |
| PVR, Wood units | 10.0 ± 5.4 (n = 53) | 7.12 ± 5.0 (n = 53) | .003 |
| PAWP, mm Hg | 14.4 ± 9.7 (n = 57) | 11.7 ± 5.4 | .15 |
| PAH therapies | 52 (89.7) | 52 (89.7) | > .99 |
| Prostacyclin | 30 (51.7) | 11 (19.0) | < .001 |
| PDE5-inhibitor | 39 (67.2) | 23 (39.7) | .003 |
| ERA | 14 (24.1) | 18 (31) | .41 |
Data presented as mean ± SD unless otherwise indicated. 6MWD = 6-min walk distance; BNP = B-type natriuretic peptide; CI = cardiac index; CTEPH = chronic thromboembolic pulmonary hypertension; ERA = endothelin receptor antagonist; PAH = pulmonary arterial hypertension; PAWP = pulmonary artery wedge pressure; PAP = pulmonary artery pressure; PDE5 = phosphodiesterase; PVR = pulmonary vascular resistance; RAP = right atrial pressure.
16 idiopathic, 3 heritable, 1 hereditary hemorrhagic telangiectasia, 1 anorexygen, 15 connective tissue disease, 6 congenital heart disease, 7 portal hypertension, 2 pulmonary veno-occlusive disease.
13 idiopathic, 3 heritable, 1 COPD, 2 ILD, 1 diastolic dysfunction.
3 sarcoid, 1 pulmonary histiocytosis, 1 fibrosing mediastinitis, 1 chronic renal failure.
3 sarcoid, 1 pulmonary histiocytosis, 1 fibrosing mediastinitis, 1 chronic renal failure.
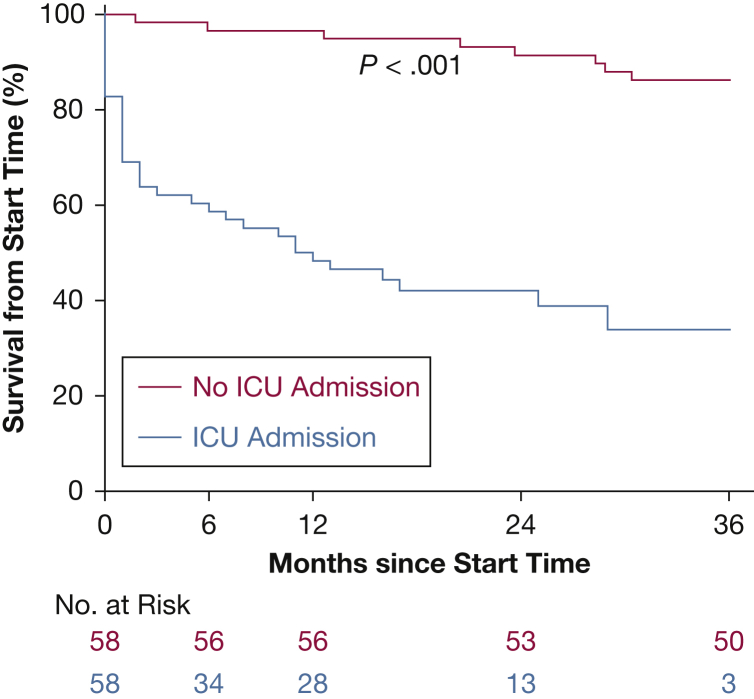
Mortality rates 6, 12, and 24 months after discharge were 26.5%, 40.8%, and 45.8%, respectively. In the postdischarge period, 85% (17/20) died of RHF. Independent factors that predicted post-MICU discharge mortality were age (hazard ratio [HR], 1.66; 95% CI, 1.13-2.43), baseline mean right atrial pressure (HR, 1.43. 95% CI, 0.98-2.09), and platelet count (HR, 1.37. 95% CI, 0.99-1.90) at time of MICU admission. Compared with matched patients (n = 58), those admitted to the MICU had reduced survival since the date of PH diagnosis (Fig 1).
Figure 1.
Post-MICU discharge survival in our cohort compared with matched patients without MICU admission during the study period. Patients admitted to the MICU had a 1- and 2-year survival rates of 48.3% and 42.0%, respectively, compared with 96.5% and 91.31% (hazard ratio, 7.79; 95% CI, 3.68-16.49). MICU = medical ICU.
The main finding of our study is that a MICU admission for PH is associated with poor survival after discharge. Older age, baseline RHF, and severity of organ dysfunction while in the MICU were independent predictors of long-term mortality. Close monitoring and aggressive therapy are warranted for patients with PH who survive an episode of critical illness.
Footnotes
FINANCIAL/NONFINANCIAL DISCLOSURES: See earlier cited article for author conflicts of interest.
References
- 1.Hoeper M.M., Granton J. Intensive care unit management of patients with severe pulmonary hypertension and right heart failure. Am J Respir Crit Care Med. 2011;184(10):1114–1124. doi: 10.1164/rccm.201104-0662CI. [DOI] [PubMed] [Google Scholar]
- 2.Sztrymf B., Souza R., Bertoletti L., et al. Prognostic factors of acute heart failure in patients with pulmonary arterial hypertension. Eur Respir J. 2010;35(6):1286–1293. doi: 10.1183/09031936.00070209. [DOI] [PubMed] [Google Scholar]
- 3.Campos A., Mathai S.C., Le Pavec J., et al. Outcomes of hospitalisation for right heart failure in pulmonary arterial hypertension. Eur Respir J. 2011;38(2):359–367. doi: 10.1183/09031936.00148310. [DOI] [PubMed] [Google Scholar]
- 4.Huynh T.N., Weigt S.S., Sugar C.A., Shapiro S., Kleerup E.C. Prognostic factors and outcomes of patients with pulmonary hypertension admitted to the intensive care unit. J Crit Care. 2012;27(6):739. doi: 10.1016/j.jcrc.2012.08.006. [DOI] [PubMed] [Google Scholar]
- 5.Tonelli A.R., Arelli V., Minai O.A., et al. Causes and circumstances of death in pulmonary arterial hypertension. Am J Respir Crit Care Med. 2013;188(3):365–369. doi: 10.1164/rccm.201209-1640OC. [DOI] [PMC free article] [PubMed] [Google Scholar]