Abstract
Aims
To evaluate the effect of antibiotic prophylaxis(AP) in the prognosis of Post-neurosurgical meningitis(PNM) patients.
Methods
A cohort analysis was performed using the clinical database in Beijing Tiantan Hospital and Capital Medical University. Data were collected on patients with the diagnosis of PNM (n = 3931) during 2012.01 to 2022.04. The microbial distribution, types of AP, and 42 and 90 days survival analysis of AP patients were evaluated using probable statistical methods. Independent risk factors for mortality were established by constructing a logistic regression analysis.
Result
A total of 1,190 patients were included in this study, Klebsiella pneumoniae, Acinetobacter baumannii, and Staphylococcus aureus occupied the highest proportion. Of them, 929 cases received AP, cefuroxime and ceftriaxone are the most frequent used antibiotics. In addition, We found that PNM patients without AP significantly increased the 42 days and 90 days all-cause mortality rates. The use of different levels of AP did not improve patient outcomes, and ICU admission and assisted mechanical ventilation (AMV) were identified as independent mortality risk factors for PNM patient received AP.
Conclusions
AP plays an important role in the prognosis of PNM patients and has a significant function in improving prognosis. The prevention of PNM with antibiotics prior to neurosurgery should be emphasized in clinical practice, and appropriate selection of antibiotics is necessary to prevent the occurrence of infection and inhibit the emergence of antibiotic-resistant bacteria.
Keywords: Antibiotic prophylaxis, Post-neurosurgical meningitis, Survival analysis, Risk factor
Introduction
Post-neurosurgical meningitis (PNM) is a type of infection that commonly occurs in previously damaged or malformed areas of the brain, typically caused by bacterial contamination during or after neurosurgical procedures [1]. Treatment of PNM generally involves the use of antibiotics; however, the condition can be life-threatening and has a high mortality rate, with up to 30% of patients dying even with antibiotic treatment [2]. Therefore, effective prevention of PNM is crucial to reduce morbidity and mortality [3].
Antibiotic prophylaxis (AP) is a preventive measure used to decrease the incidence of bacterial infections after surgery, and it is an essential component of standard care in patients undergoing neurosurgical procedures [4]. AP has been shown to reduce the incidence of PNM to 10–20% [5–7]. However, despite its widespread use, many challenges still exist in the application of AP, including the high rates of PNM, which can be as high as 3–15% even with the administration of antibiotics [8, 9]. Furthermore, it is unclear if the use of 3rd, 4th generation cephalosporins or carbapenem antibiotics can improve the survival rates of PNM patients, which highlights the need for further investigation.
In this study, we conducted a clinical cohort involving more than 1000 PNM patients, aiming to evaluate the role of AP in the prognosis of PNM patients and to identify any associated risk factors. To the best of our knowledge, this is the first global analysis specifically investigating the impact of AP on the prognosis of PNM patients.
Methods
Study design and participants
This analytical descriptive cross-sectional study was carried out at Beijing Tiantan Hospital & Capital Medical University, which served as the largest neurosurgical center in northern China, between January 2012 and April 2022. All neurosurgical patients aged 18 years or older with at least one positive cerebrospinal fluid (CSF) culture were enrolled in the study after approval from the ethics committees of both institutions (KY-2021-079-02) with a waiver of informed consent.
Inclusion and exclusion criteria
Patients diagnosed with PNM were identified based on the classic diagnostic criteria recommended by the U.S. Centers for Disease Control and Prevention (CDC) and the Infectious Diseases Society of America (IDSA). The patients were required to have bacterial proliferation in their CSF and at least one sign of meningeal irritation, such as a headache, neck stiffness, or cranial nerve involvement. In addition, the patients had to exhibit at least one of the following features: raised protein and/or lowered glucose in their CSF, increased neutrophil count, positive Gram stain CSF culture, positive blood culture, positive antigen test in blood or CSF, or increased antibody titer against the pathogen.
The exclusion criteria used in this study involved: (1) neurosurgical patients with either brain abscesses or peritoneal shunt infections, (2) those with incomplete demographic or clinical information, (3) patients aged below 18 years, and (4) those who had died within 72 h of neurosurgery, as well as those with positive CSF cultures for coagulase-negative staphylococci (CoNS), Bacillus, and Propionibacterium. Additionally, patients were only included if they were admitted to the hospital 48 h or more after the onset of their illness and underwent a neurosurgical procedure.
The AP patients were required to meet two main criteria: firstly, they had to show no signs of infection or meningitis from the time of admission until the neurosurgery. Secondly, they had to receive antibiotics 0–4 h prior to the neurosurgical operation. Patients who met both criteria were classified as AP patients, while those that did not meet or only met one criterion were categorized as non-AP patients.
Procedures
The present study relied on data extracted from the PNM database, which includes over 6,000 cases of neurosurgical patients with positive CSF cultures. 63 parameters associated with each patient, including demographic data (such as name, age, and gender), medical history (including the presence of a tumor, length of hospitalization, etc.), and details of the neurosurgical operation (such as Craniotomy, Transsphenoidal approach, and antibiotic prophylaxis) were embedded in the database.
Originally designed for monitoring hospital-acquired infections and preventing PNM the database has been utilized by various researchers in a multitude of studies [10, 11]. These have included investigations into risk factors associated with PNM, as well as survival analysis of PNM resulting from multi-drug resistant organisms (MDROs) or Staphylococcus aureus infections. In this study, all patients that met the inclusion and exclusion criteria were selected from the database.
For this analysis, we focused on the most extreme vital signs recorded within 24 h of the first positive CSF culture, including the highest body temperature. We also examined all microbiological information pertaining to the first positive CSF culture, including the type of microorganism present in the AP and non-AP groups. In this study, we classified 3rd or 4th generation cephalosporins and carbapenems into one group, and named to high grade antibiotics, which means that these antibiotics have strong bactericidal abilities. Other antibiotics, such as 1st, 2nd generation cephalosporins, Penicillin, Erythromycin were classified into low grade antibiotics, which means these antibiotics have slighter bactericidal abilities. All antibiotics administered to AP patients were evaluated.
The entire treatment plan consisted of two types of antibiotic usage, which were antibiotic empirical therapy (AET) and antibiotic definitive therapy (ADT). The two categories were described as follows: (1) PNM patients who underwent AET were administered antibiotics prior to obtaining the antimicrobial susceptibility testing result; (2) patients who underwent ADT were given antibiotic treatment based on antimicrobial susceptibility testing guidance.
Statistical analysis
The aim of this study was to investigate the impact of AP on PNM patients’ 42 days and 90 days mortality, as mortality beyond 90 days was deemed less likely to be related to PNM. As secondary outcomes, we evaluated the management of risk factors in patients with AP. Furthermore, all microbiological and clinical epidemic parameters were presented in this study.
Descriptive statistics were conducted using appropriate statistical tests such as the chi-squared or Fisher’s exact tests, t-tests, or Mann–Whitney U tests. To assess the relationship between AP and 42 days or 90 days all-cause mortality, we developed a logistic regression model where AP was treated as the dependent variable, and all potential predictors of infectious disease consultation or mortality were considered as independent variables.
In the second stage, we performed a Kaplan–Meier analysis to ascertain the effect of AP on 42 days and 90 days all-cause mortality. In this analysis, AP was treated as a time-dependent variable to adjust for the variability in the timing of consultation.
Result
During the course of the study, a total of 85,639 patients were admitted to the neurosurgery ward and underwent at least one neurosurgical procedure. Among these patients, 3,931 individuals displayed positive CSF cultures. Of the positive cases, 1, 970 patients were identified as being CoNS culture positive, 215 were Micrococcus positive, 145 were Bacillus positive, and 65 were positive for Propionibacterium acnes. A total of 347 cases were excluded from further analysis, 239 cases for having only a CSF ventriculo-peritoneal shunt, 41 for discharge within 24 h, and 67 for having incomplete clinical records. This left 1,190 patients for inclusion in the final analysis.
Microbiology
Table 1 presents a summary of the distribution of the 1,190 microorganisms that were isolated from the CSF of patients with PNM. Among the identified isolates, Klebsiella pneumoniae (12.4%), Acinetobacter baumannii (11.6%), and Staphylococcus aureus (11.3%) were the most frequently isolated microorganisms. Significant differences (P < 0.05) were observed in the distribution of S. aureus, Enterococcus faecalis, and Enterococcus faecium between the groups with and without AP.
Table 1.
Distribution of the microorganisms caused PNM
| Microorganism | AP (929) | Non-AP (261) | Total (1190) | P |
|---|---|---|---|---|
| Klebsiella pneumoniae | 119 (12.8%) | 28 (10.7%) | 147 (12.4%) | 0.395 |
| Acinetobacter baumannii | 110 (11.8%) | 28 (10.7%) | 138 (11.6%) | 0.663 |
| Staphylococcus aureus | 69 (7.4%) | 65 (24.9%) | 134 (11.3%) | < 0.001 |
| Enterococcus faecalis | 81 (8.7%) | 10 (3.8%) | 91 (7.6%) | 0.008 |
| Enterococcus faecium | 80 (8.6%) | 10 (3.8%) | 90 (7.6%) | 0.008 |
| Streptococcus viridans | 52 (5.6%) | 9 (3.4%) | 61 (5.1%) | 0.204 |
| Escherichia coli | 38 (4.1%) | 6 (2.3%) | 44 (3.7%) | 0.198 |
| Klebsiella aerogenes | 31 (3.3%) | 7 (2.7%) | 38 (3.2%) | 0.694 |
| Pseudomonas aeruginosa | 29 (3.1%) | 7 (2.7%) | 36 (3.0%) | 0.84 |
| Enterobacter cloacae | 21 (2.3%) | 5 (1.9%) | 26 (2.2%) | 0.999 |
| Serratia marcescens | 18 (1.9%) | 3 (1.1%) | 21 (1.8%) | 0.594 |
| Acinetobacter lwoffii | 18 (1.9%) | 2 (0.8%) | 20 (1.7%) | 0.277 |
| Others | 263 (28.3%) | 81 (31.0%) | 344 (28.9%) | 0.396 |
| Total | 929 (100%) | 261 (100%) | 1190 (100%) | – |
Of the AP PNM episodes, 98.0% (910/929) of patients received single antibiotics, with the highest percentage of low grade antibiotics at 63.0% (585/929) and cefuroxime at 61.7% (573/929). Among the high grade AP categories, ceftriaxone had the highest ratio, approximately 25.4% (236/929), and other antibiotics were applied in lower proportions, as shown in Table 2.
Table 2.
Distribution of AP in PNM patients
| Groups | Antibiotics | Numbers | Proportion (%) |
|---|---|---|---|
| High grade antibiotics | Ceftazidime | 50 | 5.4 |
| Meropenem | 37 | 4.0 | |
| Ceftriaxone | 236 | 25.4 | |
| Cefoperazone/Sulbactam | 2 | 0.2 | |
| Low grade antibiotics | Erythromycin | 7 | 0.8 |
| Piperacillin | 5 | 0.5 | |
| Cefuroxime | 573 | 61.7 | |
| Penicillin | 5 | 0.5 | |
| Moxalactam | 3 | 0.3 | |
| Others | 23 | 2.5 | |
Characteristics of PNM patients
The clinical characteristics of the 1,190 patients with PNM are summarized in Table 2. The median age was 42 (27, 54), and 679 (57.0%) were men. Of the PNM patients, 78.1% (929) had experienced AP, and 261 had not. The distribution of age, gender, and comorbidities was similar between groups, and all clinical laboratory tests showed no significant difference. In terms of clinical characteristics, patients who experienced traumatic brain injury, longer operation duration, reoperation, craniotomy, and coma were evenly distributed between patients with and without AP. There was no difference observed between the two groups in other items (Table 3).
Table 3.
Clinical characteristics of PNM patients received AP or not
| Characteristics | AP (929) | Non-AP (261) | Total (1190) | P |
|---|---|---|---|---|
| Age | 41 (27, 54) | 42 (27,54) | 42 (27, 54) | 0.846 |
| Gender | 524 (56.4%) | 154 (59.0%) | 679 (57.0%) | 0.48 |
| Diabetes | 44 (4.7%) | 15 (5.7%) | 59 (5.0%) | 0.519 |
| Hypertension | 146 (15.7%) | 49 (18.8%) | 195 (16.4%) | 0.256 |
| Tumour | 663 (71.4%) | 183 (70.1%) | 846 (71.1%) | 0.7 |
| Glioma | 230 (24.8%) | 62 (23.8%) | 292 (24.5%) | |
| Meningioma | 138 (14.9%) | 56 (21.5%) | 194 (16.3%) | |
| Pituitary tumor/craniopharyngioma | 158 (17.0%) | 31 (11.9%) | 189 (15.9%) | |
| Others | 137 (14.7%) | 34 (13.0%) | 171 (14.4%) | |
| Malignant tumor | 290 (31.2%) | 84 (32.2%) | 374 (31.4%) | 0.763 |
| Traumatic brain injury | 36 (3.9%) | 21 (8.0%) | 57 (4.8%) | 0.008 |
| Operation duration | 4.2 (3.0, 6.0) | 3.5 (2.0, 6.0) | 4.0 (2.8, 6.0) | 0.001 |
| Reoperation | 186 (20.0%) | 69 (26.4%) | 255 (21.4%) | 0.013 |
| Craniotomy | 664 (71.5%) | 161 (61.7%) | 825 (69.3%) | 0.003 |
| Type I incision | 478 (51.5%) | 124 (47.5%) | 602 (50.6%) | 0.263 |
| ICU admission | 378 (40.7%) | 111 (42.5%) | 489 (41.1%) | 0.618 |
| CSF Leakage | 129 (13.9%) | 44 (16.9%) | 173 (14.5%) | 0.234 |
| EVD(external ventricular drainage) | 311 (33.5%) | 103 (39.5%) | 414 (34.8%) | 0.078 |
| LD(lumbar drainage) | 250 (26.9%) | 79 (30.3%) | 329 (27.6%) | 0.309 |
| AMV(assisted mechanical ventilator) | 384 (41.3%) | 102 (39.1%) | 486 (40.8%) | 0.522 |
| Body temperature | 37.7 ± 0.9 | 37.6 ± 0.9 | 37.7 ± 0.9 | 0.807 |
| Coma | 49 (5.3%) | 57 (21.8%) | 106 (8.9%) | < 0.001 |
| Length of hospitalize | 22.0 (16.0, 34.0) | 23.0 (16.0, 32.0) | 22.0 (16.0. 34.0) | 0.576 |
| Cure time | 5.0 (2.0, 11.0) | 5.0 (3.0, 12.0) | 5.0 (2.0, 11.0) | 0.651 |
| Postoperative infection time | 7.0 (4.0, 12.0) | 7.0 (4.0, 13.0) | 7.0 (4.0, 12.0) | 0.983 |
| Fee | 71010.0 (50315.8, 119021.2) | 79160.5 (50704.7, 142460.0) | 72259.0 (50413.0, 123340.5) | 0.117 |
| All-cause mortality | 110 (11.8%) | 61 (23.4%) | 171 (14.4%) | < 0.001 |
Data are presented as means and standard deviations or median (Q1, Q3) for continuous variables and as frequencies and percentages for categorical variables
High grade and low grade AP in PNM patients
Out of the 929 AP patients, a total of 331 patients received high grade antibiotics, and 587 patients received low grade antibiotics. There were almost no significant differences between the two groups in terms of clinical operations and disease classification, except for some differences observed among patients who underwent postoperative EVD, where more patients received low grade antibiotics(Table 4).
Table 4.
Clinical characteristics of PNM patients received high or low grade AP
| Characteristics | High grade antibiotics(331) | Low grade antibiotics(587) | P |
|---|---|---|---|
| Age | 41 (26, 53) | 42 (27,55) | 0.678 |
| Gender | 200 (60.4%) | 324 (55.2%) | 0.127 |
| Diabetes | 17 (5.1%) | 27 (4.6%) | 0.749 |
| Hypertension | 55 (16.6%) | 91 (15.5%) | 0.925 |
| Tumour | 228 (62.8%) | 435 (77.5%) | 0.092 |
| Glioma | 68 (20.5%) | 162 (27.6%) | |
| Meningioma | 35 (10.6%) | 83 (14.1%) | |
| Pituitary tumor/craniopharyngioma | 48 (14.5%) | 110 (18.7%) | |
| Others | 77 (23.3%) | 80 (13.6%) | |
| Malignant tumor | 95 (27.2%) | 195 (34.1%) | 0.161 |
| Traumatic brain injury | 19 (5.7%) | 17 (2.9%) | 0.05 |
| Operation duration | 4.0 (2.5, 5.5) | 4.5 (3.0,6.0) | 0.441 |
| Reoperation | 71 (21.5%) | 115 (19.6%) | 0.496 |
| Craniotomy | 236 (71.3%) | 428 (72.9%) | 0.645 |
| Type I incision | 179 (54.1%) | 299 (50.9%) | 0.372 |
| ICU admission | 132 (39.9%) | 246 (41.9%) | 0.577 |
| CSF Leakage | 45 (13.6%) | 84 (14.3%) | 0.843 |
| EVD(external ventricular drainage) | 33 (10.0%) | 179 (30.5%) | < 0.001 |
| LD(lumbar drainage) | 91 (27.5%) | 159 (27.1%) | 0.817 |
| AMV(assisted mechanical ventilator) | 130 (39.3%) | 254 (43.3%) | 0.265 |
| Body temperature | 37.7 ± 0.9 | 37.7 ± 0.9 | 0.845 |
| Coma | 14 (4.2%) | 35 (6.0%) | 0.288 |
| Length of hospitalize | 23.0 (17.0, 36.0) | 21.0 (16.0,33.0) | 0.229 |
| Cure time | 6.0 (3.0, 11.0) | 5.0 (2.0, 10.0) | 0.246 |
| Postoperative infection time | 8.0 (5.0,13.0) | 7.0 (4.0, 12.0) | 0.115 |
| Fee | 68992.0 (48682.0, 118003.0) | 72687.0 (50833.0, 119312.0) | 0.953 |
| All-cause mortality | 33 (10.0%) | 77 (13.1%) | 0.185 |
Data are presented as means and standard deviations or median(Q1, Q3) for continuous variables and as frequencies and percentages for categorical variables
Survival analysis
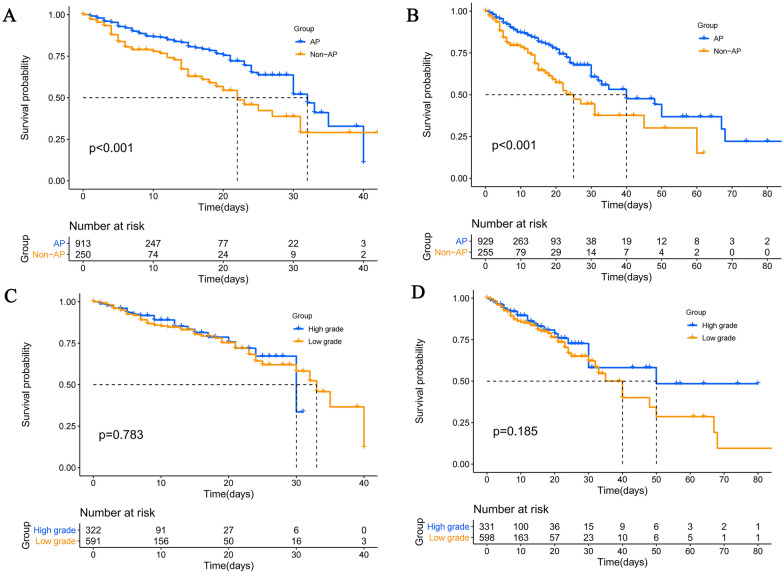
Survival analysis of PNM patients at 42 and 90 days mortality revealed a significant difference between patients who received AP and those who did not. However, there was no significant difference found between the two groups who received high-grade antibiotics for prophylaxis, as depicted in Fig. 1.
Fig. 1.
Kaplan–Meier analysis of PNM patients. A: 42 days analysis of PNM patients received AP. B: 90 days survival analysis of PNM patients received AP. C: 42 days survival analysis of PNM patients received high grade AP. D: 90 days survival analysis of PNM patients received high grade AP
Mortality risk factors
In univariate analysis, ten characteristics including traumatic brain injury, hypertension, operation duration, reoperation, ICU admission, LD, EVD, AMV, Body temperature, and coma were found to be statistically significantly different between the two groups. In multivariate regression analysis, ICU admission (OR 14.337, 95% CI 1.716–119.798, P = 0.014) and AMV (OR 2.841, 95% CI 1.078–7.492, P = 0.035) were identified as independent mortality risk factors (Table 5).
Table 5.
Univariate and multvariate analysis of clinical characteristics of AP patients
| Characteristics | Univariate analysis | Multivariate regression analysis | ||||
|---|---|---|---|---|---|---|
| Survivors (819) | Non-survivors (110) | P | OR | 95%C.I | P | |
| Age | 41 (27, 54) | 46 (28, 58) | ||||
| Gender | 454 (55.4%) | 72 (65.5%) | ||||
| Tumor | 581 (70.9%) | 82 (74.5%) | 0.443 | |||
| Malignant tumor | 250 (30.5%) | 40 (36.4%) | 0.200 | |||
| Traumatic brain injury | 26 (3.2%) | 10 (9.1%) | < 0.001 | 2.508 | 0.563–11.169 | 0.228 |
| Diabetes | 36 (4.4%) | 8 (7.3%) | 0.175 | |||
| Hypertension | 115 (14.0%) | 31 (28.2%) | < 0.001 | 1.329 | 0.509–3.471 | 0.561 |
| Operation duration | 4.0 (3.0, 6.0) | 5.0 (3.4, 7.5) | 0.008 | 1.120 | 0.963–1.304 | 0.142 |
| Reoperation | 143 (17.5%) | 43 (39.1%) | < 0.001 | 1.516 | 0.626–3.668 | 0.356 |
| Craniotomy | 581 (70.9%) | 83 (75.5%) | 0.212 | |||
| Type I incision | 421 (51.4%) | 57 (51.8%) | 0.970 | |||
| ICU admission | 293 (35.8%) | 85 (77.3%) | < 0.001 | 14.337 | 1.716–119.798 | 0.014 |
| CSF leakage | 108 (13.2%) | 21 (19.1%) | 0.095 | |||
|
EVD( external ventricular drainage) |
257 (31.4%) | 54 (49.1%) | < 0.001 | 1.093 | 0.452–2.643 | 0.843 |
| LD(lumbar drainage) | 203 (24.8%) | 47 (42.7%) | < 0.001 | 0.875 | 0.0369–2.076 | 0.763 |
| AMV(assisted mechanical ventilator) | 299 (36.5%) | 85 (77.3%) | < 0.001 | 2.841 | 1.078–7.492 | 0.035 |
| Body temperature | 37.6 ± 0.9 | 37.8 ± 1.0 | 0.017 | 1.287 | 0.599–1.323 | 0.565 |
| Coma | 34 (4.2%) | 37 (33.6%) | < 0.001 | 2.306 | 0.959–5.544 | 0.062 |
| Length of hospitalize | 21 (16, 32) | 31 (18, 46) | 0.840 | |||
| Cure time | 5 (2, 10) | 7 (3, 17) | < 0.001 | 1.004 | 0.973–1.037 | 0.792 |
Data are presented as means and standard deviations or median(Q1, Q3) for continuous variables and as frequencies and percentages for categorical variables
Therapy
In both the AP and Non-AP groups, a majority of patients with PNM received AET, with 851 (91.6%) and 231 (88.5%) patients, respectively. The most commonly administered antibiotic combination was Meropenem + Vancomycin, accounting for 45.7% in the AP group and 39.0% in the Non-AP group. Additionally, 776 (83.5%) and 213 (81.6%) PNM patients received ADT. Interestingly, our study found no significant difference between AET and ADT in terms of treatment outcomes. However, the use of Ceftazidime showed a statistically significant difference in ADT(Table 6).
Table 6.
Therapy of the PNM, including AET and ADT
| Therapy | AP(929) | Non-AP(261) | Total(1190) | P |
|---|---|---|---|---|
| AET | 851 (91.6%) | 231 (88.5%) | 1082 (90.9%) | 0.143 |
| Meropenem | 53 (6.2%) | 12 (5.2%) | 65 (6.0%) | 0.641 |
| Ceftazidime | 63 (7.4%) | 26 (11.3%) | 89 (8.2%) | 0.078 |
| Cefotaxime | 18 (2.1%) | 6 (2.6%) | 24 (2.2%) | 0.619 |
| Ceftriaxone | 81 (9.5%) | 17 (7.4%) | 98 (9.1%) | 0.366 |
| Vancomycin | 26 (3.1%) | 9 (3.9%) | 35 (3.2%) | 0.530 |
| Meropenem + Vancomycin | 389 (45.7%) | 90 (39.0%) | 479 (44.3%) | 0.073 |
| Ceftazidime + Vancomycin | 29 (3.4%) | 12 (5.2%) | 41 (3.8%) | 0.242 |
| Ceftriaxone + Vancomycin | 18 (2.1%) | 8 (3.5%) | 26 (2.4%) | 0.231 |
| Cefotaxime + Vancomycin | 27 (3.2%) | 12 (5.2%) | 39 (3.6%) | 0.162 |
| Sulbactam Sodium + Meropenem + Vancomycin | 12 (1.4%) | 6 (2.6%) | 18 (1.7%) | 0.234 |
| Others | 135 (15.9%) | 33 (14.3%) | 168 (15.5%) | 0.609 |
| ADT | 776 (83.5%) | 213 (81.6%) | 989 (83.1%) | 0.456 |
| Meropenem | 57 (7.3%) | 15 (7.0%) | 72 (7.3%) | 0.999 |
| Ceftazidime | 23 (3.0%) | 15 (7.0%) | 38 (3.8%) | 0.014 |
| Cefotaxime | 11 (1.4%) | 4 (1.9%) | 15 (1.5%) | 0.542 |
| Ceftriaxone | 22 (2.8%) | 7 (3.3%) | 29 (2.9%) | 0.654 |
| Vancomycin | 30 (3.9%) | 8 (3.8%) | 38 (3.8%) | 0.999 |
| Meropenem + Vancomycin | 370 (47.7%) | 96 (45.1%) | 466 (47.1%) | 0.536 |
| Ceftazidime + Vancomycin | 12 (1.5%) | 6 (2.8%) | 18 (1.8%) | 0.245 |
| Ceftriaxone + Vancomycin | 12 (1.5%) | 3 (1.4%) | 15 (1.5%) | 0.999 |
| Cefotaxime + Vancomycin | 14 (1.8%) | 5 (2.3%) | 19 (1.9%) | 0.578 |
| Sulbactam Sodium + Meropenem + Vancomycin | 10 (1.3%) | 6 (2.8%) | 16 (1.6%) | 0.128 |
| Others | 215 (27.7%) | 48 (22.5%) | 263 (26.6%) | 0.137 |
Discussion
Excessive use of antimicrobial agents has become an growing concern in public health [12]. In particular, after various surgical operations, AP plays a crucial role in infection control [13]. However, the overuse of antibiotics can lead to resistance, which hampers the effective treatment of bacterial infections. In this single-center cohort study conducted in China, we evaluated the microbiology and clinical epidemiology associated with PNM and identified risk factors for mortality in patients receiving AP.
This cohort study had a relatively large sample size, enrolling over 1000 cases. We observed that as many as 75% of patients received AP, while the proportion of PNM patients could reach 15% of all neurosurgical patients, irrespective of whether or not they were administered AP. Our study revealed that the use of AP significantly decreased the all-cause mortality of PNM patients at both the 42 days and 90 days follow-up periods. Interestingly, we did not observe improved patient outcomes when different types of antibiotics were used as prophylaxis. These results indicate that AP may not provide the intended benefits for neurosurgical patients with PNM. Additionaly, we identified independent mortality risk factors for PNM patients receiving AP, which included ICU admission and AMV. Increased attention should be paid to risk factors that may lead to mortality. To the best of our knowledge, this is the largest cohort study to explore the potential benefit of AP for PNM patients in the world. Our pragmatic and detailed clinical cohort design facilitated an investigation into the impact of prophylaxis independent of other factors that may lead to mortality. This study provides valuable insights that can inform the optimization of infection control strategies in neurosurgical practice.
PNM is a significant complication of neurosurgery that may have a detrimental effect on patient outcomes [14]. The administration of antibiotics stands as a pivotal measure in mitigating patient mortality. In clinical practice, preventive and therapeutic approaches are available to improve the outcomes of PNM patients [15]. Therapeutic options encompass the utilization of antibiotics, anti-inflammatory steroids, and open wound management, among others [16, 17]. Nonetheless, patients afflicted with PNM may experience significantly longer hospitalization periods and heightened expenses compared to neurosurgery patients without meningitis, and their survival rates may be significantly lower. Therefore, prevention, besides AP, plays a crucial role in the clinical management of PNM.
The selection of antibiotics is primarily contingent upon the type of microorganism responsible for PNM. Our study findings demonstrate that the responsible microorganisms for PNM are common nosocomial pathogens [18]. Nevertheless, the role of CoNS in PNM remains enigmatic. Throughout the study's duration, CoNS constituted over half of the positive pathogen cultures. While prior research has suggested that CoNS can indeed induce PNM [19], particularly in cases involving meningitis related to ventricular peritoneal shunts [20], our own prior investigation revealed that 79% of CoNS isolates were classified as contaminants [21]. Hence, in this present study, CoNS was deliberately excluded from the cohort analysis. In the rest of cases, no significant disparities exist between the top two pathogens among patients who received or did not receive AP. However, there were significant differences in the isolation rates of the top three Gram-positive bacteria, mainly Staphylococcus aureus, which had a significantly lower proportion in the AP group than in the non-AP group. Probably reason target to this issue may be the choice of AP. Cephalosporins, such as cefuroxime and ceftriaxone, accounted for 87.1% of the whole antibiotic usage. Both of these antibiotics possess notable efficacy against Staphylococcus aureus,except the Methicillin-resistant Staphylococcus aureus [22]. However, neither had a high sensitivity rate to Enterococcus faecalis, and as we all know, antibiotics combination is the most preferred choice in Enterococcus infections [23]. Our findings suggest that AP has a greater impact on patients infected with Staphylococcus aureus, and the antibiotics used in AP are more effective against this Staphylococcus aureus than against Enterococcus spp.
Previous studies have predominantly concentrated on the reduction of infection incidence with AP. Despite guidelines advocating for the administration of antibiotics prior to neurosurgery, their impact on patient prognosis has not been reported [24, 25]. Our study reveals that AP patients exhibit significantly lower all-cause mortality rates at 42 and 90 days compared to Non-AP patients, indicating a positive effect on patient outcomes. While the optimal antimicrobial regimen for preventing PNM during the perioperative period remains uncertain, guidelines propose using a single β-lactam antibiotic for most surgical procedures [4]. Our findings align with this recommendation; however, the guidelines do not stipulate the specific antibiotic type to employ. Antibiotic management proposes utilizing different levels of antibiotics with varying application strategies in clinical practice.
With the escalation of antibiotic categorization, the emergence of antibiotic-resistant bacteria becomes increasingly evident in clinical settings.. We classified patients based on their use of high-level or low-level antibiotics and found no differences in survival indicators such as survival time, treatment costs, and the length of hospital stay. This investigation underscores that the utilization of high-grade antibiotics failed to yield enhanced patient outcomes and, conversely, could heighten the susceptibility to unfavorable reactions due to their robust bactericidal impacts. Literature reports suggest that the use of high-level antibiotics can easily lead to the emergence of drug-resistant bacteria, and vancomycin, in particular, is known to have significant adverse effects [26–28]. Additionally, the two primary antibiotics used in our study, ceftriaxone (a high grade antibiotic) and cefuroxime (a low grade antibiotic), have differing effects on Gram-negative bacteria. Third generation cephalosposin is always effective against Gram-negative bacteria but may induce bacterial resistance (e.g., by producing AmpC) [29], while cefuroxime does not have this effect or possess slighter side effects, and even much cheaper. Therefore, we recommend that cefuroxime should be the preferred antibiotic for prophylaxis as it may offer equal or better benefits to patients.
Mitigating patient mortality and enhancing prognosis in the context of PNM represents a pivotal research objective. In addition to AP, other factors that impact patient outcomes should not be overlooked, such as AMV and EVD. Thorough scrutiny of risk factors across all patients subjected to AP can serve to attenuate patient mortality during the initial phases. In our previous studies, a series of risk factors about to PNM have been evaluated, such as GCS scores [11], EVD [30], AMV[10], craniotomy and malignancy [9] and so on. This study evaluated two mortality risk factors, ICU admission and AMV. Both factors are known to have poor prognoses due to the severity of the underlying disease, making patients more susceptible to infection and leads to poor outcome.
In this investigation, we scrutinized two distinct treatment modalities for patients diagnosed with PNM. The initial approach involved AET, predominantly due to the delay in receiving antibiotic susceptibility test results. Consequently, a broad-spectrum antibiotic regimen was administered to ensure comprehensive coverage and mitigate any potential adverse consequences. Our findings revealed that the most frequently prescribed empirical antibiotic combination was Meropenem + Vancomycin, which may be associated with the severity of PNM and its higher propensity for unfavorable prognosis. The second approach entailed ADT, guided by the findings of antibiotic susceptibility testing. Similar to AET, the Meropenem + Vancomycin combination remained the predominant choice. This preference can be attributed to the widely accepted and efficacious nature of the Meropenem + Vancomycin clinical regimen for combating PNM. Additionally, a slightly lower proportion of patients received ADT compared to AET. This variation could be explained by the longer cultivation period (3–5 days) required for pathogen identification, allowing some PNM patients to recover within the timeframe of AET.
Insufficient investigation has been conducted regarding AP in the context of PNM. Firstly, single-center studies possess inherent limitations, and even with a sample size of over 1000 cases, single-center studies are less reliable than multi-center studies in terms of overall credibility. Secondly, the primary diseases causing PNM were not classified in detail, and only neurosurgical operations were analyzed as a category of disease. Lastly, the antibiotics used for AP at our center were limited, so we were only able to group them according to high level and low level antibiotics, which had certain limitations.
In summary, AP emerges as a pivotal determinant in the prognosis of PNM patients, exhibiting the potential to markedly enhance outcomes. Variations in antibiotic types exhibit negligible influence on patient mortality rates, thereby providing insights for antibiotic selection in clinical practice. Among all PNM patients receiving AP, ICU admission and AMV are independent risk factors for patient death, highlighting the need for vigilance in managing these factors by clinicians.
Acknowledgements
We would like to thank Ms. Yumeng Cai, Capital medical University, who had given the help to draw the relevant figures.
Abbreviations
- AP
Antibiotic prophylaxis
- PNM
Post-neurosurgical meningitis
- CSF
Cerebrospinal fluid
- CDC
Centers for Disease Control and Prevention
- IDSA
Infectious Diseases Society of America
- CoNS
Coagulase-negative staphylococci
- MDROs
Multi-drug resistant organisms
- EVD
External ventricular drainage
- LD
Lumbar drainage
- AMV
Assisted mechanical ventilator
Author contributions
GHZ, YJS, and JLS wrote original Draft; SQW and XL did calculate and editing job; HL and GJZ conduct the whole study. All authors approved the final version of the paper.
Funding
This work was supported by the Beijing Hospital Authority Clinical Medicine Development of Special Funding (Grant No. ZYLX202108), Beijing Municipal Administration of Hospitals Incubating Program (Grant No. PX2022021) and Medical Talent Program for High-throughput Sequencing Technology in Infectious Diseases, China (Grant No. MTP2022A011).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the Ethics Committee of Beijing tianta hospital & Capital medical university (Approved NO.: KY-2021-079-02). Permission was obtained to use ICSQ from the original authors. Informed written or oral consent was taken from the participants before carrying out the survey.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hussein K, Bitterman R, Shofty B, Paul M, Neuberger A. Management of post-neurosurgical meningitis: narrative review. Clin Microbiol Infect. 2017;23(9):621–628. doi: 10.1016/j.cmi.2017.05.013. [DOI] [PubMed] [Google Scholar]
- 2.Pintado V, Pazos R, Jiménez-Mejías ME, et al. Staphylococcus aureus meningitis in adults: a comparative cohort study of infections caused by meticillin-resistant and meticillin-susceptible strains. J Hosp Infect. 2019;102(1):108–115. doi: 10.1016/j.jhin.2018.11.008. [DOI] [PubMed] [Google Scholar]
- 3.Karvouniaris M, Brotis A, Tsiakos K, Palli E, Koulenti D. Current perspectives on the diagnosis and management of healthcare-associated ventriculitis and meningitis. Infect Drug Resist. 2022;15:697–721. doi: 10.2147/IDR.S326456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ratilal BO, Costa J, Pappamikail L, Sampaio C. Antibiotic prophylaxis for preventing meningitis in patients with basilar skull fractures. Cochrane Database Syst Rev. 2015;4:CD004884. doi: 10.1002/14651858.CD004884.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bernard B, Grangé JD, Khac EN, Amiot X, Opolon P, Poynard T. Antibiotic prophylaxis for the prevention of bacterial infections in cirrhotic patients with gastrointestinal bleeding: a meta-analysis. Hepatology. 1999;29(6):1655–1661. doi: 10.1002/hep.510290608. [DOI] [PubMed] [Google Scholar]
- 6.Chavez-Tapia NC, Barrientos-Gutierrez T, Tellez-Avila FI, Soares-Weiser K, Uribe M. 2010 Antibiotic prophylaxis for cirrhotic patients with upper gastrointestinal bleeding. Cochrane Database Syst Rev. 2010;9:CD002907. doi: 10.1002/14651858.CD002907.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chavez-Tapia NC, Barrientos-Gutierrez T, Tellez-Avila F, et al. Meta-analysis: antibiotic prophylaxis for cirrhotic patients with upper gastrointestinal bleeding - an updated Cochrane review. Aliment Pharmacol Ther. 2011;34(5):509–518. doi: 10.1111/j.1365-2036.2011.04746.x. [DOI] [PubMed] [Google Scholar]
- 8.Valentini LG, Casali C, Chatenoud L, Chiaffarino F, Uberti-Foppa C, Broggi G. Surgical site infections after elective neurosurgery: a survey of 1747 patients. Neurosurgery. 2008;62(1):88–95. doi: 10.1227/01.NEU.0000311065.95496.C5. [DOI] [PubMed] [Google Scholar]
- 9.Zheng G, Cao Y, Liu C, et al. Phenotype, molecular characterisation and risk factors for postoperative meningitis caused by ESBL-producing-Enterobacteriaceae: a six years multi-Centre comparative cohort study. BMC Infect Dis. 2021;21(1):85. doi: 10.1186/s12879-021-05784-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zheng G, Wang S, Lv H, Zhang G. Nomogram analysis of clinical characteristics and mortality risk factor of non-fermentative gram-negative bacteria-induced post-neurosurgical meningitis. Infect Drug Resist. 2022;15:6379–6389. doi: 10.2147/IDR.S385502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shi YJ, Zheng GH, Qian LY, Qsman RA, Li GG, Zhang GJ. Longitudinal analysis of risk factors for clinical outcomes of enterobacteriaceae meningitis/encephalitis in post-neurosurgical patients: a comparative cohort study during 2014–2019. Infect Drug Resist. 2020;13:2161–2170. doi: 10.2147/IDR.S252331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.El-Dalati S, Cronin D, Shea M, et al. Clinical practice update on infectious endocarditis. Am J Med. 2020;133(1):44–49. doi: 10.1016/j.amjmed.2019.08.022. [DOI] [PubMed] [Google Scholar]
- 13.Sastry RA, Wang EJ, Mermel LA. Antibiotic prophylaxis practices in neurosurgery: a Society for Healthcare Epidemiology of America (SHEA) survey. Infect Control Hosp Epidemiol. 2022;43(5):662–664. doi: 10.1017/ice.2021.488. [DOI] [PubMed] [Google Scholar]
- 14.Tan T, Lee H, Huang MS, et al. Prophylactic postoperative measures to minimize surgical site infections in spine surgery: systematic review and evidence summary. Spine J. 2020;20(3):435–447. doi: 10.1016/j.spinee.2019.09.013. [DOI] [PubMed] [Google Scholar]
- 15.Nau R, Djukic M, Spreer A, Eiffert H. Bacterial meningitis: new therapeutic approaches. Expert Rev Anti Infect Ther. 2013;11(10):1079–1095. doi: 10.1586/14787210.2013.839381. [DOI] [PubMed] [Google Scholar]
- 16.Lee BJ, Vu BN, Seddon AN, Hodgson HA, Wang SK. Treatment considerations for CNS infections caused by vancomycin-resistant Enterococcus faecium: a focused review of linezolid and daptomycin. Ann Pharmacother. 2020;54(12):1243–1251. doi: 10.1177/1060028020932513. [DOI] [PubMed] [Google Scholar]
- 17.Suthar R, Sankhyan N. Bacterial infections of the central nervous system. Indian J Pediatr. 2019;86(1):60–69. doi: 10.1007/s12098-017-2477-z. [DOI] [PubMed] [Google Scholar]
- 18.Facciolà A, Pellicanò GF, Visalli G, et al. The role of the hospital environment in the healthcare-associated infections: a general review of the literature. Eur Rev Med Pharmacol Sci. 2019;23(3):1266–1278. doi: 10.26355/eurrev_201902_17020. [DOI] [PubMed] [Google Scholar]
- 19.Huang CR, Lu CH, Wu JJ, Chang HW, Chien CC, Lei CB, Chang WN. Coagulase-negative staphylococcal meningitis in adults: clinical characteristics and therapeutic outcomes. Infection. 2005;33:56–60. doi: 10.1007/s15010-005-4083-7. [DOI] [PubMed] [Google Scholar]
- 20.Khan FY. Adult coagulase-negative staphylococcal meningitis in Qatar: clinical characteristics and therapeutic outcomes. Asian J Neurosurg. 2021;16:714–718. doi: 10.4103/ajns.AJNS_144_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zheng G, Zhang G, Li F, Zhang Y, Tang M, Kang X. Determination and clinical significance of the diagnostic value of Coagulase-negative Staphylococci true infection in cerebrospinal fluid cultures of post-neurosurgical patients. Chin J Lab Med. 2017;40(4):707–710. [Google Scholar]
- 22.Gudiol C, Cuervo G, Shaw E, Pujol M, Carratalà J. Pharmacotherapeutic options for treating Staphylococcus aureus bacteremia. Expert Opin Pharmacother. 2017;18(18):1947–1963. doi: 10.1080/14656566.2017.1403585. [DOI] [PubMed] [Google Scholar]
- 23.Beganovic M, Luther MK, Rice LB, Arias CA, Rybak MJ, LaPlante KL. A review of combination antimicrobial therapy for Enterococcus faecalis bloodstream infections and infective endocarditis. Clin Infect Dis. 2018;67(2):303–309. doi: 10.1093/cid/ciy064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goff DA, Mangino JE, Glassman AH, Goff D, Larsen P, Scheetz R. Review of guidelines for dental antibiotic prophylaxis for prevention of endocarditis and prosthetic joint infections and need for dental stewardship. Clin Infect Dis. 2020;71(2):455–462. doi: 10.1093/cid/ciz1118. [DOI] [PubMed] [Google Scholar]
- 25.Bratzler DW, Dellinger EP, Olsen KM, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg Infect (Larchmt) 2013;14(1):73–156. doi: 10.1089/sur.2013.9999. [DOI] [PubMed] [Google Scholar]
- 26.McEwen SA, Collignon PJ. Antimicrobial resistance: a one health perspective. Microbiol Spectr. 2018 doi: 10.1128/microbiolspec.ARBA-0009-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ferri M, Ranucci E, Romagnoli P, Giaccone V. Antimicrobial resistance: a global emerging threat to public health systems. Crit Rev Food Sci Nutr. 2017;57(13):2857–2876. doi: 10.1080/10408398.2015.1077192. [DOI] [PubMed] [Google Scholar]
- 28.Bruniera FR, Ferreira FM, Saviolli LR, et al. The use of vancomycin with its therapeutic and adverse effects: a review. Eur Rev Med Pharmacol Sci. 2015;19(4):694–700. [PubMed] [Google Scholar]
- 29.Jacoby GA. AmpC beta-lactamases. Clin Microbiol Rev. 2009;22(1):161–82. doi: 10.1128/CMR.00036-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zheng G, Shi Y, Cao Y, et al. clinical feature, therapy, antimicrobial resistance gene distribution, and outcome of nosocomial meningitis induced by multidrug-resistant enterobacteriaceae-a longitudinal cohort study from two neurosurgical centers in Northern China. Front Cell Infect Microbiol. 2022;12:839257. doi: 10.3389/fcimb.2022.839257. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.