Abstract
Background
Emotional support is key to improve older adults’ subjective health, and psychological, social and emotional well-being. However, many older adults living in the community lack emotional support, increasing the risk for loneliness, depression, anxiety, potentially avoidable healthcare use and costs, and premature death. Multiple intersecting factors may influence emotional support of older adults in the community, but these are poorly understood. Studies have focused on specific populations (e.g., older adults with depression, cancer). Although relevant, these studies may not capture modifiable factors for the wider and more diverse population of older adults living in the community. Our scoping review will address these important gaps. We will identify and synthesize the evidence on factors that influence emotional support of older adults in the community.
Methods
We will use the Johanna Briggs Institute updated methodological guidance for the conduct of scoping reviews to guide our review process. We will search MEDLINE, EMBASE, APA Psycinfo, CINAHL, Dissertations and Theses Global, and Scopus from inception. We will include studies published in English, examining factors influencing emotional support of older adults residing in community, without restrictions on the study design or year of publication. We will also include gray literature (dissertations and reports). Two independent reviewers will conduct title, abstract, and full-text screening, as well as risk of bias assessment, using validated quality appraisal tools based on study designs. Discrepancies will be resolved by consensus. The primary reviewer will extract the data from all studies, and the second reviewer will check the extractions of all the studies. We will use descriptive statistics and narrative synthesis for analysis. Family/friend caregivers and older adults involved as an advisory group will help with explaining the findings in terms of whether associations observed reflect their experiences and reality. We will analyze the discussion and generate themes, and summarize in a narrative form.
Discussion
This scoping review may identify factors that could be modified or mitigated to improve emotional support provision for older adults residing in community. The knowledge will inform the development of tailored interventions directed to older adults and their caregivers.
Systematic review registration
https://doi.org/10.17605/OSF.IO/4TAEB (associated project link: osf.io/6y48t).
Supplementary Information
The online version contains supplementary material available at 10.1186/s13643-023-02346-7.
Keywords: Emotional support, Older adults, Community, Public health
Background
Social support plays crucial role in older adults’ life (like younger individuals) [1–3]. Older adults who experience the death of friends or family members, functional and/or cognitive decline, reduced ability to attend social events, and loss of social contacts need support to cope with these losses [4–7]. Social support is referred as the interactive process in which person’s social networks (e.g., family, friends, neighbors, churches) or paid support services (e.g., physicians, nurses, therapists, and personal support workers) [8–13] provide assistance to the individual, including emotional (e.g., care, concern, love), material (e.g., services, goods, financial help, assistance), and informational (e.g., knowledge, advice) support [14, 15]. Emotional support, therefore, is one aspect of the broader concept social support.
Emotional support is crucial for the health and well-being of human beings (including older adults) [16]. Emotional support is defined as the expression of positive affect, empathetic understanding, and the encouragement of expressions of feelings, or the offering of advice, information, guidance or feedback [17]. It is a key process in close relationships, as well as an important determinant of satisfaction with these relationships [18]. Receipt of adequate emotional support is associated with improved subjective health [19], psychological, social and emotional well-being [20–23], and a reduced likelihood for depressive symptoms [24]. However, not all older adults receive sufficient emotional support. For example, between 20 and 48% older Atlantic Canadians (≥ 65 years) living in the community reported low emotional/informational support [25]. According to the Canadian Longitudinal Study on Aging (CLSA) [26], more than 17% of those aged 65 years and older felt like they did not have someone to confide in (measured as one of the sub-component of emotional/informational support) [26] which corresponds to almost 1.2 million older adults in Canada [27]. Lack of emotional support increases the risk of loneliness [28], anxiety [29], poor quality of life [28], and premature death [30].
Multiple intersecting factors may influence an older person’s emotional support. A body of evidence has identified common socio-demographic and health characteristics influencing older adults’ emotional support. Older adults who were widowed, divorced or were never married [7, 31, 32], those who had functional impairment [32], higher symptom burden [7], and those who lived alone [4] had lower levels of emotional support. Further, older adults with higher emotional support reported lower depression and chronic pain scores [31]. However, findings are inconsistent for increasing age, female sex, lower education, and lower income [6, 7, 31–34]. These inconsistencies may be attributed to the differences in sample characteristics and settings, and approaches to measuring emotional support across research studies. Research has also identified relationship-level factors that influence older adults’ emotional support. For instance, older adults with restricted social networks reported less emotional support [32], and those who had traumatic childhood experiences, such as emotional neglect, felt more emotionally isolated in old age [35]. Studies suggest that community-based support resources, such as the availability of community programs, are essential to develop and broaden the social network [36, 37]. The broader social networks provide opportunities to gain companionship and positive social interaction [32], and increase opportunities to receive various kind of support resources (e.g., instrumental, emotional) offered by their network members [38]. Further, racialized communities compared to white populations are reported to have higher levels of emotional and instrumental support [39–41]. However, these studies do not differentiate between emotional and instrumental support [39–41]. Age-related prejudices (ageism) promote social exclusion and limit social participation and thus lead to low social support [42, 43]. These studies do not indicate the types of social support measured [39–43]. Most studies on older adults’ emotional support have focused on specific populations, such as older adults with depression, cancer, diabetes, multiple illnesses, or disabilities [7, 44–47]. These studies are relevant. However, they may miss modifiable factors influencing emotional support for the wider and more diverse population of older adults.
Previous reviews have mainly focused on the influence of social support on morbidity, mortality, or healthcare service utilization [15, 48–51]. To the best of our knowledge, no review has comprehensively synthesized the available literature on factors that influence emotional support of older adults in general (rather than specific older adult populations), and that include all research designs. This scoping review will address this critical knowledge gap. With an aging population, maintaining older adults’ health, well-being and independence is a key public health priority around the globe [52–54]. To achieve this, a better understanding of factors influencing older adults’ emotional support is a prerequisite [16]. We will identify and synthesize the available evidence on factors that influence emotional support of older adults living in community.
Theoretical guidance
We will use the social-ecological model (Fig. 1) to inform this review. The socio-ecological model is an adaptation of the earlier concepts from Bronfenbrenner’s ecological theory [55–57]. The social-ecological perspective assumes that human beings are a product of their thoughts, interpersonal relationships, organizational entities, and the community structures, systems, and policies which they are embedded in [58, 59]. Further, the culmination of these factors influences and predicts, or explains, health and well-being outcomes [58]. This social-ecological model posits that there are multiple factors at three levels that influences older adults’ emotional support: (1) Individual (e.g., race/ethnicity), (2) relationship (e.g., social network), and (3) community (e.g., availability of community programs and events) and society (e.g., ageism) levels [2, 55, 58, 60, 61]. The model explicates how factors at one level are embedded within or influence factors at another level, offering a multifaceted way to capture the complex interplay among individual, relationship, community, and society factors that influences older adults’ emotional support. Further, it posits that receipt of adequate emotional support influences older adults’ emotional well-being. Emotional support is important for individuals to lessen distress, cope more effectively with problems, and to maintain a positive self-concept and positive outlook on their life [16]. Further, it supports an individual to express positive emotions and regulate negative emotions [62–66]. This helps to attain a sense of balance between pleasant and unpleasant emotions [67–69]. Experiencing more pleasant than unpleasant emotions is central to a person’s emotional well-being [70, 71]. The levels and factors specified in socio-ecological model will guide inclusion or exclusion of studies (i.e., studies will be included if they assess any of the factors mentioned in the socio-ecological model) and data extraction on factors associated with emotional support of older adults. Details on this process is provided in Data extraction and Analyses section.
Fig. 1.
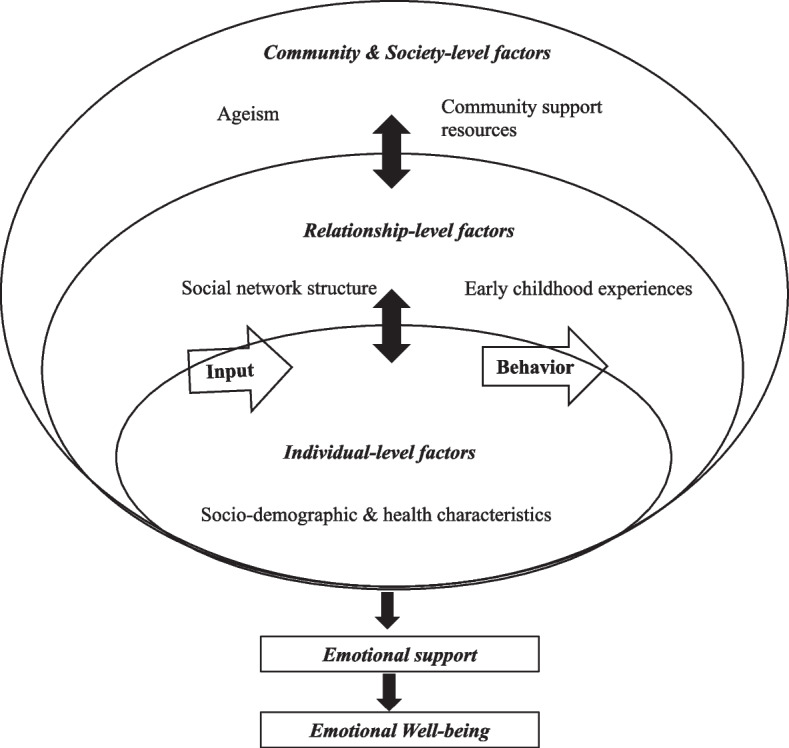
Socio-ecological model. Adapted from Bronfenbrenner, U. (1977) [57]. This model is inspired by Bronfenbrenner’s work on ecology of human development [57]. Thus, publication permission is not required (confirmed with American Psychologist Journal-the copyright holder of the original work)
Research question
What are the factors that influence emotional support of older adults living in community?
Methods/design
This is a protocol of a scoping review that aims to systematically map the literature available on factors influencing older adults’ emotional support. We used scoping review as it allows to capture the diverse literature and study designs on this topic. The Johanna Briggs Institute updated methodological guidance for the conduct of scoping reviews will guide the processes of this scoping review [72]. To facilitate complete and transparent reporting of the review process, we will report the results of the synthesis according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses–Scoping Review (PRISMA-ScR) reporting guideline (Additional file 1) [73]. The review protocol follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) 2015 statement (Additional file 2) [74]. We will involve people with lived experience (family/friend caregivers, and older adults) as an advisory group to further contextualize the review findings. Details are provided in Older adults and family engagement section.
Inclusion and exclusion criteria
We will use broad inclusion/exclusion criteria (Appendix Table 1) to obtain relevant papers published in the English language without any restrictions on the study design or year of publication. We will not systematically search for grey literature; however, we will only include those grey literature (i.e., dissertations and reports) identified during the database search.
Search strategy
A health sciences librarian (LD) developed searches for Medline (Ovid MEDLINE(R) ALL), Embase (Ovid interface), APA Psycinfo (Ovid Interface), CINAHL Plus with Full Text (EBSCOhost interface), Dissertations and Theses Global (Proquest Interface), and Scopus. These databases will be searched from the date of inception. The search combines an extensive list of terms for three concepts: emotional support AND family/friend caregivers or formal care providers AND older adults. Articles focused on nursing home and assisted living residents were removed from the search. Case reports and non-research articles were removed from the search where possible. No date, language, or study design limits were used. All the searches in six databases are included as an Additional file 3. We will conduct title/Abstract and full text screening in COVIDENCE. We will review the reference lists of included articles and reviews for additional studies.
Study selection and screening
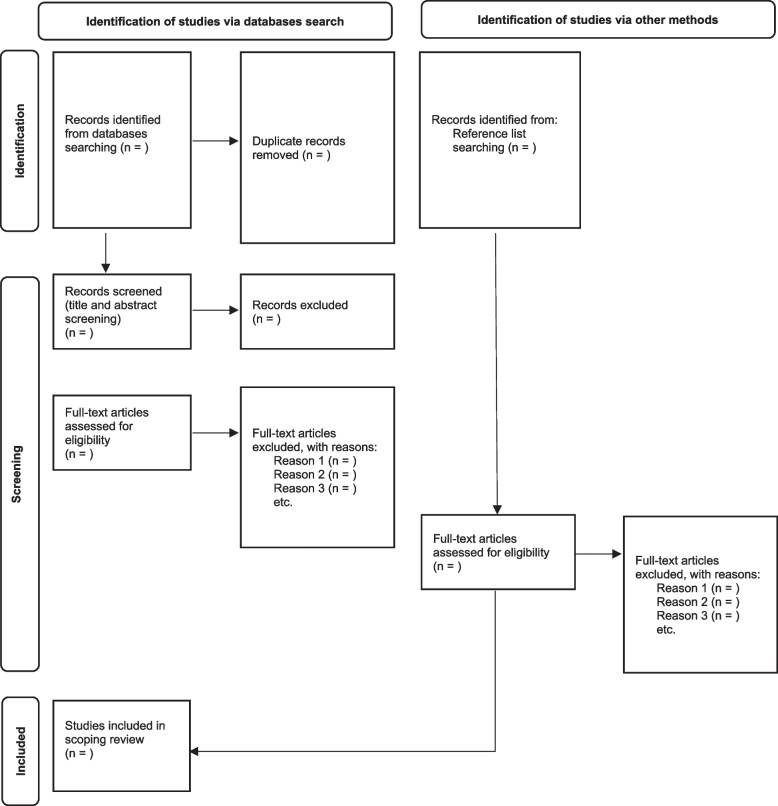
Two reviewers (RD and SS) will independently screen the titles and abstract of retrieved studies in batches, screening the first 100 articles [75] and then a consensus meeting follows to discuss issues and reconcile decisions. They will follow the same process for the remaining articles. Full-text screening of all references not definitely excluded in the previous step will follow a similar process. We will consult a third reviewer if two reviewers cannot agree upon the inclusion or exclusion of a study. We will use the PRISMA flow diagram (Appendix Fig. 2) to report the selection of articles during each phase with the rationale and to ensure the transparency of the selection of studies.
Data extraction
We developed a data extraction form (Google Form, Additional file 4) to document details of eligible studies. Categories include: (1) study characteristics: year of publication and data collection, publication type (e.g., journal, thesis, reports), country of origin of the study, research aim/question, (2) theoretical framework, (3) design/methods: study design, setting, sample and sampling methods, data collection methods, outcomes and measures used, types of emotional support assessed and measures used, analyses applied, and (4) main findings: factors found to influence older adults’ emotional support—categorized based on their correspondence with the factor levels—individual (e.g., age, sex, marital status, race/ethnicity, chronic conditions), relationship (e.g., social network, early childhood experiences), or community (e.g., availability of community programs and events) and society (e.g., ageism) of the socio-ecological model. We will pre-test the data extraction form using five randomly selected studies to ensure feasibility of the data extraction form [76]. Two reviewers (RD and SS) will independently extract data from the 10% of the studies, followed by a consensus meeting to calibrate extraction. Reviewers will discuss any discrepancies, come to consensus, and the update the form (if needed) before extracting data from the remaining studies. RD will extract the data from all remaining studies, and SS will check the extractions of all the studies. Any discrepancies will be solved through discussion, and if needed, a third reviewer will help to resolve the differences.
Quality appraisal
Quality appraisal is generally not recommended in scoping reviews [72]. However, we will conduct quality assessments to be able to speak to the quality of the studies and to increase the credibility of review findings. We will use five validated checklists to assess the methodological quality of the included studies after full text screening: (a) the Checklist for systematic reviews and research synthesis for systematic reviews, meta-analysis, scoping reviews, integrative reviews, and narrative reviews [77], (b) the Quality Assessment Tool for Quantitative Studies (QATQS) for randomized controlled trial (RCT), controlled trial (CT), pre-post [78, 79], (c) the Newcastle–Ottawa Scale (NOS) for any observational study (cohort study, cross-sectional study) [80], (d) the CASP for qualitative research studies [81], and (e) the Mixed Method Appraisal Tool (MMAT) for mixed method study designs [82, 83].
We will use the method developed by De Vet et al. [84] to score the overall quality of each study. For this, we will calculate the ratio of the obtained score to the maximum possible score (varies depending on the checklist used and the number of checklist items applicable) for each study (possible range 0–1). Each study will then be categorized as: weak (≤ 0.50), low moderate (0.51–0.66), high moderate (0.67–0.79), or strong (≥ 0.80). However, we will not exclude studies based on the methodological quality. RD and SS will independently appraise all the included studies. A consensus meeting will follow to solve any discrepancies after completing 10% of the appraisal of included studies (same process for the remaining appraisals). We will consult a third reviewer if needed to resolve any disagreements. We will report summary of quality of included studies. We will summarize and describe the key areas of strength and weakness for all studies within each type of research design.
Analyses
We will descriptively present the number and proportion of studies that represent each category (e.g., country of origin, study setting, design, risk of bias category) using figures and tables. We will use descriptive statistics and narrative synthesis to summarize review findings [85]. In this process, we will identify and categorize the factors influencing older adults’ emotional support identified in each study based on their correspondence with individual, relationship, or community, and society level factors of socio-ecological framework. For quantitative results, we will report the number and proportion of studies reporting statistically significant positive and negative associations and non-significant associations (vote counting) by factor category as informed by socio-ecological framework. For qualitative results, we will conduct a content analysis of the key themes and factors assessed and we will indicate if the content of these themes varied across studies. We will report each theme to illustrate similarities and differences in their relationships with older adults’ emotional support. We will then categorize them into either individual, relationship, or community and society level factors according to how these themes align with either of the factor levels of socio-ecological framework.
For narrative synthesis, after organizing the review findings under three factor levels (individual, relationship, community/society) of socio-ecological framework, we will explore the relationships within (characteristics of individual studies and their reported findings) and between (between findings of different studies) included studies [85]. Socio-ecological framework will guide in understanding the relationships between different factors identified and older adults’ emotional support. Finally, we will assess the strength of the evidence (based on methodological quality of the included studies) for drawing conclusions about the influence of factors on older adults’ emotional support. Further, we will present the list of factors descriptively in table format. The analysis process will be iterative, and depend on the concrete references retrieved. Therefore, we will refine the synthesis strategies as needed and transparently document and report the process and any decisions made.
Older adult and family engagement
We will involve family/friend caregivers from BC and Alberta, and older adults as an advisory group. While contacting advisory group members, we informed them about the objective of the review, their role in the research team, what is expected of them and their time commitments. We have presented a summary of the proposed review to this group in November 2021 and received their input on important issues (e.g., definition of emotional support) to guide the review. We will conduct one Zoom-based group discussion (approximately one hour in total) after data synthesis from the scoping review. Older adults and family members will assist with evaluating the findings. They will (a) help with explaining the patterns (e.g., associations)–if the associations reflect their experiences, if they agree or disagree with the findings, (b) assist in understanding if our findings include important gaps or if any additional focus is needed, and (c) provide their perspective on what can be done to emotionally support older adults in the community. We will obtain verbal informed consent from the respective patient-partners to participate in the focus group discussion. Two researchers will facilitate the recorded discussions. We will transcribe the focus group recordings verbatim. We will conduct thematic analysis. For this, two researchers will independently code texts, develop a preliminary coding categories (which we will discuss among the review team), discuss and reconcile coding categories, look for similarities and differences between the codes and then identify major themes and group them into similar themes [86]. We will present these findings in the results section separately in a narrative form [85]. We will integrate the advisors in planning and production (co-authorship, critical feedback) of the review output.
Dissemination
We intend to disseminate the review findings through peer-reviewed publication, policy briefs (to Public Health Agency of Canada, Health Canada, provincial and regional governments, and provincial and regional health authorities) and prepare lay summaries and presentations of the findings for older adults and family/friend caregivers. We will present the findings at conference on geriatrics or health services and policy (e.g., Canadian Gerontological Nursing Association, Canadian Association on Gerontology, International Association of Gerontology and Geriatrics). The review will provide recommendations for future research areas, health policy, and care practice.
Limitations
We are limited to studies published in English language and as a result, we might miss potential studies that are non-English. As we are not systematically searching for gray literature, we might miss out potential gray literature. Another limitation is that only primary reviewer will extract the data from all the studies. However, another independent reviewer will check the extraction of all the studies.
Discussion
The scoping review is an appropriate and valid review approach to map a body of literature on factors that determine older adults’ emotional support. The review may aid in identifying factors that can be modified or mitigated (e.g., availability of community programs or events, ageism, caregiver distress) to improve emotional support provision for older adults. This knowledge will inform the development of tailored services and interventions directed to improve the older adults’ emotional support, as well as, minimize older adults’ unmet emotional support needs. The involvement of stakeholders in evaluating the findings will ensure that the findings of this study are grounded, and impactful. Further, this will also provide opportunity for dissemination of findings to target audiences (i.e., through the networks of family/friend caregivers and older adults who will be involved as an advisory group in the review).
Identifying and understanding older adults’ emotional support has become one of the urgent public health priorities considering the growth in the aging population. To develop an effective solution to meet older adults’ emotional support needs, it is important first to understand the factors that influence older adults’ emotional support. We hope this scoping review, when conducted rigorously and systematically, will provide trustworthy evidence that contributes to the understanding of older peoples’ emotional support. We acknowledge that the scoping review is an iterative process, and any changes made to the plan will be made as transparent as possible.
Supplementary Information
Additional file 1. Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist.
Additional file 2. PRISMA-P 2015 Checklist.
Additional file 3. Preliminary search strategy.
Additional file 4. Data Extraction Form-Emotional support.
Acknowledgements
Not applicable.
Appendix
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Study focus | • Studies examining factors that are associated with or influence older adults’ emotional support | • Studies only describing emotional support and/or assessing whether the emotional support needs are met but not assessing the association of any factors influencing older adults’ emotional support |
| Dependent variable | Emotional support, defined as a sole construct (expression of positive affect, empathetic understanding, and the encouragement of expressions of feelings) or in combination with informational support (offering of advice, information, guidance or feedback) | • Studies only assessing instrumental/tangible, positive social interaction, or affection social support without explicitly examining emotional support |
| Independent variables |
• Socio-demographic and health characteristics of older adults (e.g., age, sex, marital status, race/ethnicity, chronic conditions) • Relationship factors (e.g., social network, early childhood experiences) • Community factors (e.g., availability of community programs and events) • Society related factors (e.g., ageism) |
|
| Study design |
• Primary empirical quantitative studies regardless of the research design (e.g., randomized controlled trials, non-randomized trials with or without a control group, cohort studies, cross-sectional studies, time series or regression discontinuity designs) • Qualitative studies (e.g., qualitative interviews, focus groups, ethnographic observations, qualitative case studies) • Mixed-methods studies |
• Research protocols, case reports, editorials, opinion papers, comments, newspaper articles, historical articles, lecture notes, presentations, personal narratives |
| Setting | • Older adult’s private home, apartment, rented home | • Studies focusing on nursing homes (residential long-term care), daycare/centers, rehabilitation centers, assisted living settings, hospitals |
| Population |
• Studies that only include older adults age ≥ 65 •Studies that include older adults (≥ 65) and younger adults as long as results are reported separately for older adults |
• Studies including no participants aged ≥ 65 years • Studies including older adults but not reporting results specific to this sub-group |
Fig. 2.
PRISMA flow diagram for article selection process
Authors’ contributions
RD was responsible for concept development, review planning, and manuscript writing. MH and GC are co-supervisors and guided all aspects of the review, including protocol development, review planning, and manuscript writing. KH and CM are RD's supervisory committee members and were responsible for all major areas of protocol development, review planning, and manuscript writing. SS was involved in protocol development and provided manuscript edits. LD is a research librarian and helped develop the search strategy, wrote the search strategy section, and provided manuscript edits. All authors read and approved the final manuscript.
Funding
The patient-partner engagement activity is funded through Nursing Research to Practice Award received from the faculty of nursing at the University of Alberta, and the studentship award for patient engagement received from the Alberta SPOR Support Unit (AbSPORU). RD received both awards.
Availability of data and materials
We will include all data generated or analyzed in the published scoping review article. Upon request, other resources can be made available.
Declarations
Ethics approval and consent to participate
This study is a part of RD’s PhD project and have received ethical approval from Health Research Ethics Board, University of Alberta (Pro00106735).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rook KS, Charles ST. Close social ties and health in later life: strengths and vulnerabilities. Am Psychol. 2017;72(6):567–577. doi: 10.1037/amp0000104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holt-Lunstad J. Why social relationships are important for physical health: a systems approach to understanding and modifying risk and protection. Annu Rev Psychol. 2018;69(1):437–458. doi: 10.1146/annurev-psych-122216-011902. [DOI] [PubMed] [Google Scholar]
- 3.Rook KS. Gaps in social support resources in later life: an adaptational challenge in need of further research. J Soc Pers Relat. 2009;26(1):103–112. doi: 10.1177/0265407509105525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Årestedt K, Saveman BI, Johansson P, Blomqvist K. Social support and its association with health-related quality of life among older patients with chronic heart failure. Eur J Cardiovasc Nurs. 2012;12(1):69–77. doi: 10.1177/1474515111432997. [DOI] [PubMed] [Google Scholar]
- 5.Stevens A, Gillam S. Needs assessment: from theory to practice. Br Med J. 1998;316(7142):1448–1452. doi: 10.1136/bmj.316.7142.1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shin JK, Kim KW, Park JH, Lee JJ, Huh Y, Lee SB, et al. Impacts of poor social support on general health status in community-dwelling Korean elderly: the results from the Korean Longitudinal Study on Health and Aging. Psychiatry Investig. 2008;5(3):155–162. doi: 10.4306/pi.2008.5.3.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams GR, Pisu M, Rocque GB, Williams CP, Taylor RA, Kvale EA, et al. Unmet social support needs among older adults with cancer. Cancer. 2019;125(3):473–481. doi: 10.1002/cncr.31809. [DOI] [PubMed] [Google Scholar]
- 8.Government of Canada. Home and community health care. 2016 [Cited 16 June 2020]. Available from: https://www.canada.ca/en/health-canada/services/home-continuing-care/home-community-care.html.
- 9.Gilmour H. Formal home care use in Canada. Heal Reports. 2018;29(9):3–9. [PubMed] [Google Scholar]
- 10.Fast J, Eales J, Norah K. Informal caregiving: what are the financial costs for cargivers?. 2018. Available from: https://crdcn.org/sites/default/files/financial_costs_of_family_caregiving.pdf.
- 11.Stall N. We should care more about caregivers. CMAJ. 2019;191(9):E245–E246. doi: 10.1503/cmaj.190204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Keating NC, Fast JE, Lero DS, Lucas SJ, Eales J. A taxonomy of the economic costs of family care to adults. J Econ Ageing. 2014;3:11–20. [Google Scholar]
- 13.Health Council of Canada. Seniors in need , caregivers in distress : What are the home care. Toronto; 2012. Available from: https://healthcouncilcanada.ca/files/HCC_HomeCare_FA.pdf.
- 14.Jacobson DE. Types and Timing of Social Support. J Heal Soc Behav. 1986;27(3):250–264. [PubMed] [Google Scholar]
- 15.Bowling A. Social support and social networks: Their relationship to the successful and unsuccessful survival of elderly people in the community. an analysis of concepts and a review of the evidence. Fam Pract. 1991;8(1):68–83. doi: 10.1093/fampra/8.1.68. [DOI] [PubMed] [Google Scholar]
- 16.Burleson BR. The experience and effects of emotional support: what the study of cultural and gender differences can tell us about close relationships, emotion, and interpersonal communication. Pers Relatsh. 2003;10(1):1–23. [Google Scholar]
- 17.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 18.Cunningham MR, Barbee AP. Social support. In: Hendrick C, Hendrick SS, editors. Close relationships: a sourcebook. Thousand Oaks: SAGE Publications, Inc.; 2000. pp. 272–85. [Google Scholar]
- 19.White AM, Philogene GS, Fine L, Sinha S. Social support and self-reported health status of older adults in the United States. Am J Public Health. 2009;99(10):1872–1878. doi: 10.2105/AJPH.2008.146894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Port CL, Zimmerman S, Williams CS, Dobbs D, Preisser JS, Williams SW. Families filling the gap: comparing family involvement for assisted living and nursing home residents with dementia. Gerontologist. 2005;45(SPEC. ISS. 1):87–95. doi: 10.1093/geront/45.suppl_1.87. [DOI] [PubMed] [Google Scholar]
- 21.Thompson D, Weber JA, Juozapavicius K. Residents in assisted living facilities and visitation patterns. J Hous Elderly. 2001;15(1–2):31–42. [Google Scholar]
- 22.Whitaker A. Family involvement in the institutional eldercare context. Towards a new understanding. J Aging Stud. 2009;23(3):158–167. [Google Scholar]
- 23.Gaugler JE, Kane RL. Families and assisted living. Gerontologist. 2007;47(Suppl 1):83–99. [PubMed] [Google Scholar]
- 24.Chao SF. Assessing social support and depressive symptoms in older Chinese adults: a longitudinal perspective. Aging Ment Heal. 2011;15(6):765–774. doi: 10.1080/13607863.2011.562182. [DOI] [PubMed] [Google Scholar]
- 25.Mcinnis-perry G, Weeks LE, Stryhn H. Age and gender differences in emotional and informational social support insufficiency for older adults in Atlantic Canada. Can J Nurs Res. 2013;45(4):50–68. doi: 10.1177/084456211304500405. [DOI] [PubMed] [Google Scholar]
- 26.Kirkland SA, Griffith LE, Menec V, Wister A, Payette H, Wolfson C, et al. Canadian institutes of health research-institute of aging: profile: mining a unique Canadian resource: the Canadian longitudinal study on aging. Can J Aging. 2015;34(3):366–377. doi: 10.1017/S071498081500029X. [DOI] [PubMed] [Google Scholar]
- 27.Statistics Canada. Canada’s population estimates: Age and sex, July 1, 2020. 2020 [cited 17 Feb 2021]. Available from: https://www150.statcan.gc.ca/n1/en/daily-quotidien/200929/dq200929b-eng.pdf?st=Kx1YUSTG.
- 28.Kang HW, Park M, Wallace (Hernandez) JP. The impact of perceived social support, loneliness, and physical activity on quality of life in South Korean older adults. J Sport Heal Sci. 2018;7:237–244. doi: 10.1016/j.jshs.2016.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Santini ZI, Jose PE, York Cornwell E, Koyanagi A, Nielsen L, Hinrichsen C, et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Heal. 2020;5(1):e62–70. doi: 10.1016/S2468-2667(19)30230-0. [DOI] [PubMed] [Google Scholar]
- 30.Lyyra TM, Heikkinen RL. Perceived social support and mortality in older people. J Gerontol Ser B Psychol Sci Soc Sci. 2006;61(3):147–152. doi: 10.1093/geronb/61.3.s147. [DOI] [PubMed] [Google Scholar]
- 31.Conte KP, Schure MB, Goins RT. Correlates of social support in older American Indians: the native elder care study. Aging Ment Heal. 2015;19(9):835–843. doi: 10.1080/13607863.2014.967171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Harasemiw O, Newall N, Shooshtari S, Mackenzie C, Menec V. From social integration to social isolation: the relationship between social network types and perceived availability of social support in a national sample of older Canadians. Res Aging. 2018;40(8):715–739. doi: 10.1177/0164027517734587. [DOI] [PubMed] [Google Scholar]
- 33.Hoogendijk EO, Muntinga ME, van Leeuwen KM, van der Horst HE, Deeg DJH, Frijters DHM, et al. Self-perceived met and unmet care needs of frail older adults in primary care. Arch Gerontol Geriatr. 2014;58(1):37–42. doi: 10.1016/j.archger.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 34.Melchiorre MG, Chiatti C, Lamura G, Torres-Gonzales F, Stankunas M, Lindert J, et al. tankunas M, Lindert J, et al. Social support, socio-economic status, health and abuse among older peop. PLoS ONE. 2013;8(1):e54856. doi: 10.1371/journal.pone.0054856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wilson RS, Krueger KR, Arnold SE, Barnes LL, De LCFM, Bienias JL, et al. Childhood adversity and psychosocial adjustment in old age. Am J Geriatr Psychiatry. 2006;14(4):307–315. doi: 10.1097/01.JGP.0000196637.95869.d9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Giebel C, Hassan S, Harvey G, Devitt C, Harper L, Simmill-Binning C. Enabling middle-aged and older adults accessing community services to reduce social isolation: community connectors. Heal Soc Care Community. 2020;00:1–8. doi: 10.1111/hsc.13228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goll JC, Charlesworth G, Scior K, Stott J. Barriers to social participation among lonely older adults: the influence of social fears and identity. PLoS ONE. 2015;10(2):1–17. doi: 10.1371/journal.pone.0116664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ashida S, Sewell DK, Schafer EJ, Schroer A, Friberg J. Social network members who engage in activities with older adults: do they bring more social benefits than other members? Ageing Soc. 2019;39(5):1050–1069. doi: 10.1017/S0144686X17001490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Almeida J, Molnar BE, Kawachi I, Subramanian SV. Ethnicity and nativity status as determinants of perceived social support: testing the concept of familism. Soc Sci Med. 2009;68(10):1852–1858. doi: 10.1016/j.socscimed.2009.02.029. [DOI] [PubMed] [Google Scholar]
- 40.Chan B, Goldman LE, Sarkar U, Guzman D, Critchfield J, Saha S, et al. High perceived social support and hospital readmissions in an older multi-ethnic, limited English proficiency, safety-net population. BMC Health Serv Res. 2019;19(1):1–9. doi: 10.1186/s12913-019-4162-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hill TD, Uchino BN, Eckhardt JL, Angel JL. Perceived social support trajectories and the all-cause mortality risk of older Mexican American women and men. Res Aging. 2016;38(3):374–398. doi: 10.1177/0164027515620239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lee HS, Kim C. Structural equation modeling to assess discrimination, stress, social support, and depression among the elderly women in South Korea. Asian Nurs Res (Korean Soc Nurs Sci) 2016;10(3):182–188. doi: 10.1016/j.anr.2016.06.003. [DOI] [PubMed] [Google Scholar]
- 43.Ramírez L, Palacios-Espinosa X. Stereotypes about old age, social support, aging anxiety and evaluations of one’s own health. J Soc Issues. 2016;72(1):47–68. [Google Scholar]
- 44.Pejner MN, Ziegert K, Kihlgren A. Trying to cope with everyday life-Emotional support in municipal elderly care setting. Int J Qual Stud Health Well-being. 2012;7:1–7. doi: 10.3402/qhw.v7i0.19613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kapadia MR, Veenstra CM, Davis RE, Hawley ST, Morris AM. Unmet emotional support needs among diverse patients with colorectal cancer. Am Surg. 2020;86(6):695–702. doi: 10.1177/0003134820923318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shyu YIL, Tang WR, Tsai WC, Liang J, Chen MC. Emotional support levels can predict physical functioning and health related quality of life among elderly Taiwanese with hip fractures. Osteoporos Int. 2006;17(4):501–506. doi: 10.1007/s00198-005-0020-y. [DOI] [PubMed] [Google Scholar]
- 47.Warner LM, Schüz B, Wurm S, Ziegelmann JP, Tesch-Römer C. Giving and taking -differential effects of providing, receiving and anticipating emotional support on quality of life in adults with multiple illnesses. J Health Psychol. 2010;15(5):660–670. doi: 10.1177/1359105310368186. [DOI] [PubMed] [Google Scholar]
- 48.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Valtorta NK, Moore DC, Barron L, Stow D, Hanratty B. Older adults’ social relationships and health care utilization: a systematic review. Am J Public Health. 2018;108(4):e1–10. doi: 10.2105/AJPH.2017.304256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Spiers G, Matthews FE, Moffatt S, Barker RO, Jarvis H, Stow D, et al. Impact of social care supply on healthcare utilisation by older adults: a systematic review and meta-analysis. Age Ageing. 2019;48(1):57–66. doi: 10.1093/ageing/afy147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tajvar M, Fletcher A, Grundy E, Arab M. Social support and health of older people in Middle Eastern countries: a systematic review. Australas J Ageing. 2013;32(2):71–78. doi: 10.1111/j.1741-6612.2012.00639.x. [DOI] [PubMed] [Google Scholar]
- 52.World Health Organization. Global strategy and action plan on ageing and health. Geneva, Switzerland; 2017. Available from: http://apps.who.int/bookorders.%0A, http://www.who.int/ageing/WHO-GSAP-2017.pdf?ua=1.
- 53.Government of Canada. Government of Canada-action for seniors report. Ottawa, Canada; 2014. Available from: https://www.canada.ca/en/employment-social-development/programs/seniors-action-report.html.
- 54.Vlachantoni A. Unmet need for social care among older people. Ageing Soc. 2019;39(4):657–684. [Google Scholar]
- 55.Bronfenbrenner U. Ecology of the family as a context for human development. Dev Psychol. 1986;22(6):723–742. [Google Scholar]
- 56.Bronfenbrenner U. The ecology of human development experiments by nature and design. USA: President and Fellows of Harvard College; 1979. Available from: https://khoerulanwarbk.files.wordpress.com/2015/08/urie_bronfenbrenner_the_ecology_of_human_developbokos-z1.pdf.
- 57.Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol. 1977;32(7):513–531. [Google Scholar]
- 58.McLeroy K, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 59.Brown V. Using the social ecological model to inform community needs assessments. J Fam Consum Sci. 2015;107(1):45–51. [Google Scholar]
- 60.Centers for Disease Control and Prevention. The social-ecological model: a framework for prevention. 2015. Available from: https://www.cdc.gov/violenceprevention/overview/social-ecologicalmodel.html.
- 61.World Health Organization. The ecological framework. 2017. Available from: http://www.who.int/violenceprevention/approach/ecology/en/.
- 62.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–357. [PubMed] [Google Scholar]
- 63.Hofmann SG. Interpersonal emotion regulation model of mood and anxiety disorders. Cognit Ther Res. 2014;38(5):483–492. doi: 10.1007/s10608-014-9620-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Marroquín B. Interpersonal emotion regulation as a mechanism of social support in depression. Clin Psychol Rev. 2011;31(8):1276–1290. doi: 10.1016/j.cpr.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 65.Schwarzer R, Knoll N. Functional roles of social support within the stress and coping process: a theoretical and empirical overview. Int J Psychol. 2007;42(4):243–252. [Google Scholar]
- 66.Zaki J, Craig WW. Interpersonal emotion regulation. Emotion. 2013;13(5):803–810. doi: 10.1037/a0033839. [DOI] [PubMed] [Google Scholar]
- 67.Fredrickson BL. The broaden-and-build theory of positive emotions. Philos Trans R Soc B Biol Sci. 2004;359(1449):1367–1377. doi: 10.1098/rstb.2004.1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fredrickson BL, Mancuso RA, Branigan C, Tugade MM. The undoing effect of positive emotions. Motiv Emot. 2000;24(4):237–258. doi: 10.1023/a:1010796329158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fredrickson BL, Joiner T. Positive emotions trigger upward spirals toward emotional well-being. Psychol Sci. 2002;13(2):172–175. doi: 10.1111/1467-9280.00431. [DOI] [PubMed] [Google Scholar]
- 70.Diener E, Larsen RJ. The experience of emotional well-being. In: Lewis M, Haviland JM, editors. Handbook of emotions. The Guilford Press; 1993. pp. 405–415. [Google Scholar]
- 71.Diener E, Lucas RE. Subjective emotional well-being. In: Lewis M, Haviland M, editors. Handbook of emotions. 2. New York: Guilford; 2000. pp. 325–337. [Google Scholar]
- 72.Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18(10):2119–2126. doi: 10.11124/JBIES-20-00167. [DOI] [PubMed] [Google Scholar]
- 73.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 74.Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015: Elaboration and explanation. BMJ. 2015;349(January):1–25. doi: 10.1136/bmj.g7647. [DOI] [PubMed] [Google Scholar]
- 75.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):1–9. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Long L. Routine piloting in systematic reviews-a modified approach? Syst Rev. 2014;3(1):1–5. doi: 10.1186/2046-4053-3-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Aromataris E, Fernandez R, Godfrey C, Holly C, Kahlil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc. 2015;13(3):132–140. doi: 10.1097/XEB.0000000000000055. [DOI] [PubMed] [Google Scholar]
- 78.Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evidence-Based Nurs. 2004;1(3):176–184. doi: 10.1111/j.1524-475X.2004.04006.x. [DOI] [PubMed] [Google Scholar]
- 79.Armijo-Olivo S, Stiles CR, Hagen NA, Biondo PD, Cummings GG. Assessment of study quality for systematic reviews: a comparison of the Cochrane collaboration risk of bias tool and the effective public health practice project quality assessment tool: methodological research. J Eval Clin Pract. 2012;18(1):12–18. doi: 10.1111/j.1365-2753.2010.01516.x. [DOI] [PubMed] [Google Scholar]
- 80.Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2013. [Google Scholar]
- 81.Critical Appraisal Skills Program. CASP (Qualitative Checklist). 2018. Available from: https://casp-uk.net/casp-tools-checklists/.
- 82.Pace R, Pluye P, Bartlett G, Macaulay AC, Salsberg J, Jagosh J, et al. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. Int J Nurs Stud. 2012;49(1):47–53. doi: 10.1016/j.ijnurstu.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 83.Souto RQ, Khanassov V, Hong QN, Bush PL, Vedel I, Pluye P. Systematic mixed studies reviews: Updating results on the reliability and efficiency of the mixed methods appraisal tool. Int J Nurs Stud. 2015;52(1):500–501. doi: 10.1016/j.ijnurstu.2014.08.010. [DOI] [PubMed] [Google Scholar]
- 84.De Vet HCW, De Bie RA, Van Der Heijden GJMG, Verhagen AP, Sijpkes P, Knipschild PG. Systematic reviews on the basis of methodological criteria. Physiotherapy. 1997;83(6):284–289. [Google Scholar]
- 85.Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the conduct of narrative synthesis in systematic reviews. a product from the a product from the ESRC methods programme. Bailrigg; 2006. Available from: https://www.researchgate.net/publication/233866356_Guidance_on_the_conduct_of_narrative_synthesis_in_systematic_reviews_A_product_from_the_ESRC_Methods_Programme?channel=doi&linkId=02e7e5231e8f3a6183000000&showFulltext=true%0Ahttps://www.researchgate.net/.
- 86.Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8:1–10. doi: 10.1186/1471-2288-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist.
Additional file 2. PRISMA-P 2015 Checklist.
Additional file 3. Preliminary search strategy.
Additional file 4. Data Extraction Form-Emotional support.
Data Availability Statement
We will include all data generated or analyzed in the published scoping review article. Upon request, other resources can be made available.