Abstract
Background:
Suicidal Behaviors and Thoughts are a relevant public health issue that includes suicidal ideation, non-suicidal self-harm, attempted suicide, and failed suicides. Since there is a progression of suicidal behaviors, whereby suicide is more likely to be completed if there have already been previous behaviors or attempts to harm oneself, WHO has highlighted the need to detect early predictors of such suicidal behaviors, which can help identify individuals at risk, plan prevention strategies and implement specific therapeutic interventions, particularly in young people, thus reducing the number of deaths. This retrospective observational study aimed to identify early predictors of suicidal risk in 237 inpatients admitted for Suicidal Behaviors and Thoughts at Child and Adolescent Psychiatry Emergency Unit of the Meyer Children's Hospital, Florence, Italy.
Methods:
The study was subdivided into three phases: data collection, statistical analysis, and neural network. For each patient, we collected epidemiological and psychopathological data. We stratified the inpatients into two groups: “suicidal volition patients” and “suicidal motivation patients.”
Results:
The hospitalization rate for suicidal behaviors and thoughts showed a growing trend from 2016 to 2020 (27.69 to 45.28%). Under 12 years of age, diagnosis of disruptive, impulse-control and conduct disorder, previous specialist care, history of attempted suicide, and intoxication as methods of suicide were statistically correlated to an increased risk of suicidal behaviors. Artificial intelligence, with an accuracy of 86.7%, confirmed these risk factors.
Limitations:
The most important limitation of the study is its retrospective nature.
Conclusions:
Our study identifies new early predictors of suicidal risk: age less than 12, diagnosis of disruptive, impulse-control and conduct disorder. In addition, suicidal volition behavior emerges as an important and underestimated risk factor. The use of artificial intelligence methods could be supporting the clinician in assessing suicidal risk.
Keywords: Suicidal behaviors and thoughts, artificial intelligence, children and adolescents, risk of suicide and predictive factors
Highlights
Suicidal behaviors and thoughts are a relevant public health issue.
Artificial intelligence could support the clinician in assessing suicidal risk.
Aged less than 12, conduct disorders are new early predictors of suicidal risk.
Introduction
The World Health Organization 1 recognizes suicide as a critical public health issue. 1 Although suicide represents one of the main causes of death in all age groups, this phenomenon is of critical importance at developmental ages because the sharpest increase in the number of deaths due to suicide occurs in the transition between adolescence and early adulthood and because the onset of suicidal thoughts/behaviors occurs commonly before the age of 25, even in most of those subjects who carry out a suicide attempt later in life. 2 The prevalence of suicidal ideation and attempted suicide increases dramatically during adolescence 3 and it represents the second leading cause of death among youth of 10–19 years old. 4
There is still no consensus on the use of specific terms in the suicide literature. The most common trend is to indicate as suicidal behaviors and thoughts (SBTs) a range of phenomena with a continuum of symptom severity and sharing the same distal and proximal risk factors.3,5 SBTs are closely related to each other but differ in prevalence, strength of intention and lethality. Suicidal ideation represents a risk factor for subsequent suicidal behavior: the risk of committing an attempted suicide by 30 years of age is 12 times higher for people with previous suicidal ideation. 6 In any age group, suicides are to some extent preventable. Due to their multifactorial etiopathogenesis, prevention strategies require coordinated and integrated actions involving healthcare, education, politics, and mass media. 1
In the WHO Mental Health Action Plan 2013–2030, WHO Member States have committed themselves to working toward the global target of reducing the suicide rate in countries by one-third by 2030. 7 The WHO also highlighted the need to detect early predictors of suicidal behaviors, which can help to identify subjects at risk, plan prevention strategies and implement specific therapeutic interventions.1,7
In recent years, artificial intelligence proved to be an effective approach to automating the analysis of medical data and extracting new combinations of biomarkers useful for early diagnosis,8–11 and for the identification of suicidal behaviors among psychiatrically hospitalized adolescents. 12
In this scenario, identifying risk factors for progression from suicidal ideation to attempted suicide/failed suicide is one of the main challenges in suicidology. Self-injurious actions not intended to end in death must be distinguished from suicide. Such actions include, for example, courage tests and, relatively common among minors, nonsuicidal self-injury, which often serves to regulate emotional states of aversion. 13 Furthermore, in clinical practice, there is a widespread tendency to distinguish between attempted suicides and failed suicides. Attempted suicides correspond to those events which, even in the presence of a confirmed suicidal intention, do not determine a fatal outcome due to the unconscious use of low-cost method lethality, or because they are interrupted prematurely by the will of the subject. On the other hand, failed suicides are defined as events that do not determine a fatal outcome due to fortuitous causes, independent of the will of the subject (e.g. intervention by third parties), despite the confirmed suicidal intentionality and the choice of methods and high lethality. 14
Our study combined clinical evaluation, statistical analysis, and a neural network approach to investigate risk factors for SBTs and to evaluate the differences existing between suicidal ideation versus attempted suicide/failed suicide in children and adolescents admitted to the Child and Adolescent Psychiatry Emergency Unit (CAPEU) of the Meyer Children's Hospital in Florence. The heterogeneity detected in patients with SBTs might be used to train a multivariate model and a specific neural network approach is able to predict or classify a specific behavior. In this direction, one of the main objectives of this work is the creation of an instrument able to identify at-risk subjects and give a probabilistic indication of the characteristics of the suicidal event.
Methods
Selection of subjects
The study was approved by the Pediatric Ethics Committee of the Tuscany Region (number 112/2022). This was a single-center retrospective observational cohort study including 237 patients admitted for SBTs at the CAPEU of the Meyer Children's Hospital from January 1st, 2016, to June 30th, 2020. The selection bias was minimized by the consecutive enrollment of patients 15 Inclusion criteria were: (1) psychiatric diagnosis in accordance with the Diagnostic and Statistical Manual of Mental Disorders DSM-5 criteria 16 ; (2) subjects required inpatient treatment. Exclusion criteria were intellectual disability and moderate–severe neurological disorders. All subjects completed a study protocol consisting of a complete diagnostic evaluation to collect sociodemographic and psychopathological data. For each patient, we retrospectively collected from the medical records (software C7 medico), clinical data including sex, date of birth, age at first hospital admission, ethnicity, family characteristics, type of school, academic performance, method, previous treatments, the outcome of the hospitalizations and past stressful or traumatic events (STEs). An STE is a traumatic or stressful event, occurring in childhood or adolescence, with potential negative consequences on neurobiological or psychosocial development.17,18
We also stratified the sample into two different groups according to the reason for referral for admission. The first group comprised patients with low-damaging SBTs, which included patients with unstructured suicidal ideation, hereinafter referred to as “suicidal volition patients.” The second group included patients with suicidal intent with a high potential for injury, hereinafter referred to as “suicidal motivation patients,” hospitalized for failed suicide or attempted suicide. We recorded data in a Microsoft Excel database. All analyses (statistical and neural network approach) were related to this stratification. Psychiatric diagnosis was based on DSM-5 16 and the Kiddie Schedule for Affective Disorders and Schizophrenia-Present and Lifetime interview. 19 SBT phenomena were assessed using the Italian version of the Columbia-Suicide Severity Rating Scale (C-SSRS) administered to psychiatric residents in the first 2 days after admission to the psychiatric ward. Based on the C-SSRS scores, 20 we differentiated the presence of suicidal ideation, the intensity of ideation, self-injurious behaviors, and suicide attempts. The lethality of suicide attempts was based on actual mortality/medical harm and coded as follows:
0: No suicidal ideation or suicidal behavior with no damage.
Thoughts of death but not suicidal ideation and not suicidal behavior.
Sporadic unstructured suicidal ideation or minor suicidal behavior, such as superficial self-cutting with minor physical damage (slight bleeding, scratching, bruising).
Unplanned suicidal ideation or persistent thoughts of death or suicidal behavior with moderate physical damage, need for medical attention (e.g. second-degree burns, major vessel bleeding).
Active suicidal ideation with some intent to act, without specific plan or preparatory acts or behavior (anything beyond verbalization or thought, like assembling the specific method (e.g. buying pills or a gun) or preparing for death by suicide (e.g. giving things away, writing suicide notes).
Active suicidal ideation with a specific plan and intent or suicide attempt with minor physical damage and medical hospitalization required.
Repeated major self-injurious behaviors, suicide attempts with severe physical harm and repeated suicide attempts.
Statistical analysis
Statistical analysis envisaged the extraction of absolute and relative frequencies for the categorical variables and the evaluation of mean and standard deviation for the numerical variables. Pearson's chi-squared test (χ2) 21 was performed to assess the statistical significance of the observations. Specifically, the relationship or independence between available categorical data with respect to the variable referral reason for admission was evaluated. The test requires the creation of contingency tables between two variables, that is two-entry tables in which the cells defined by the intersection of rows and columns contain the number of cases with positive values of the two variables (joint frequencies). The χ2 test assumes as a null hypothesis that the two variables are statistically independent, whilst the alternative hypothesis is that there is a relationship between the two variables. The χ2 test uses the χ2 distribution to decide whether to reject the null hypothesis and is widely used to verify if the frequencies of the observed values fit the theoretical frequencies of a fixed probability distribution. The χ2 test makes it possible to establish, after setting the maximum permissible error, whether discrepancies between observed and theoretical frequencies are due entirely to chance or are justified by statistical dependence. The tolerated error was set at 5%. 22 To carry out this test, each variable of interest was transformed into a dichotomous variable (e.g. the variable “Presence/absence of previous specialist care” was analyzed as “Caretaking YES/ Caretaking NO”) and its dependence on the variable referral reason for admission was evaluated, which was also transformed into a dichotomous mode (“suicidal motivation patients” versus “suicidal volition patients”).
Artificial intelligence: Neural network approach
Statistical analysis evaluated the single variables independently and did not allow the creation of a predictive model that considers different factors at the same time and therefore predicts a possible suicidal event based on the available information. This failure could be overcome with the use of artificial neural networks, which had the advantage of not requiring the assumption of a linear relationship between values and could be used for modeling prediction problems that had several characteristics following undefined functions.23,24
A neural network is an interconnected system of perceptrons. The perceptron is a type of binary classifier that maps its inputs into an output value calculated with an activation function (χ) that evaluates the scalar product between the input vector (x) and a vector of weights (w) added to a constant bias value (b). The activation formula is therefore:
By modifying the vector of the weights w through a specific learning algorithm, it is possible to modulate the output of a perceptron, with the aim of obtaining learning properties. Several layers of perceptrons form a neural network.
Preparation of data
The preparation of data is a crucial step for the success of the system as it can strongly influence the results of the analysis and the simplicity of the data management. The dataset based on the medical records at the CAPEU of the Meyer Children's Hospital contains 53 variables, including numerical data (e.g. age) and categorical features (e.g. nationality), that is variables represented by labels with predefined values. In this work the pre-processing of data involved: (1) normalization of numerical data in the interval [-1-1], with the aim of avoiding features with wider ranges weighing more on the output; (2) one-hot encoding of categorical features (for each example all bits are set to 0 except one, which indicates the category to which it belongs) was applied to avoid the forced creation of ordinality relations where these do not exist; (3) dichotomous variables that assumed value 0–1 were remapped to −0.5–0.5 to avoid the risk of setting some weights to zero.
Feature selection
The size of the dataset after the above-mentioned preprocessing required a feature selection phase to reduce the network inputs. In general, feature reduction processes are applied to avoid resource consumption by weak features, optimize model performance by avoiding the noise generated by unnecessary fields, and generally identify the strongest predictors. A widely used technique for this task is recursive feature elimination (RFE). 25 Given an external estimator that assigns weights to features, and a desired number of features to select, the goal of feature selection is to select features by recursively considering smaller and smaller sets of features. The estimator chosen in this work is Random Forest Classifier 26 a machine learning method that generally works well with high-density problems and allows non-linear relationships between predictors. In our work, the desired number of features was fixed at 30. Minimizing the number of features is a practice generally executed to facilitate the learning process, but at the same time, it is necessary to avoid reducing the amount of input information too much. In the present study, the value of 30 features was empirically found, as the minimum number of features required by the network to maximize accuracy.
Model architecture
As mentioned above, a neural network is a multilayer system of perceptrons, the choice of the number of neurons in the hidden layers is a very important part of the decision on the overall architecture of the neural network. Using too few neurons in the hidden layers causes so-called underfitting, i.e. when there are too few neurons in the hidden layers to adequately detect signals in a complicated data set. Using too many neurons in the hidden layers can cause several problems. First, it can cause overfitting, i.e. when the neural network has such a high information processing capacity that the limited amount of information in the training set is not enough to train all the neurons in the hidden layers. An excessive number of neurons in the hidden layers may also increase the time required to train the network. A trade-off must be reached between too many and too few neurons in the hidden layers. There are many rules of thumb for determining the correct number of neurons to use in the hidden layers. 23 However, choosing an architecture for the neural network usually comes down to trial and error. The choice of the number of neurons during the neural network's trial and error process can be guided by some considerations regarding the network's ability to learn the complexity of the problem. Also, for the learning algorithm that defines the data model by changing the weights, an empirical procedure is generally used. 23
Iterative empirical tests were performed to identify the final and optimized configuration of the neural network by varying both the number of neurons per layer and the number of hidden layers. The best configuration consists of a single layer with 15 neurons and uses the Adam Optimizer. 27 In this research, neural networks were used as a tool to predict the type of suicidal behavior (“suicidal motivation patients” versus “suicidal volition patients”), and therefore the variable referral reason to admission was considered as the single variable in the output layer.
Model evaluation
The loss graph and the accuracy parameter were used to assess the learning ability and accuracy of the network. The loss value indicates the optimization error, so a gradual decrease in this function is to be expected. The accuracy of a model is usually determined after the model parameters are learned and fixed and no learning is taking place and indicates the percentage of the number of correct predictions. Often to evaluate the performance of a model and its generalization ability an approach involving dividing the data into three parts, Train, Validation and Test, is followed. However, this technique generally does not work well in cases where large datasets are not available. Thus, when limited datasets are available, as is the present case, splitting the dataset may result in some useful information being excluded from the training procedure and the model failing to learn the data distribution correctly. Therefore, after this first stage of model evaluation, the K-fold Cross-validation (CV) method was used to validate the network's generalization ability. In K-Fold CV, the “K” parameter decides the number of folds into which the dataset will be divided. Each fold has a chance to appear in the training set (K-1) times, which ensures that every observation appears in the dataset, thus allowing the model to better learn the distribution of the underlying data. The results of the K-fold test were also compared with the estimation obtained by leave-one-out cross-validation (LOOCV), a computationally expensive version of cross-validation in which K = N and N is the total number of examples in the training dataset. In other words, each sample in the training set is assigned an example to be used alone as the test evaluation dataset. This procedure is rarely used for large datasets because it is computationally expensive, but it can be used in the case presented in this article. Thus, a comparison could be made between the average classification accuracy for different values of K and the average classification accuracy of LOOCV on the same dataset.
Results
Statistical analysis
The main description of our population is summarized in Table 1.
Table 1.
Summary of the clinical data of 237 patients in our study.
| Total patients (N = 237) | Suicidal motivation patients (N = 111) | Suicidal volition patients (CSITALICSTARTNCSITALICEND = 126) | ||
|---|---|---|---|---|
| N (%) | (%) | (%) | P-value** | |
| Patients 2016–2020 | 42.62 | 21.09 | 21.51 | .478 |
| Female | 74.69 | 33.76 | 40.93 | .386 |
| Age ≤ 12.5 | 6.3 | 4.64 | 1.68 | .034 |
| Italian | 57.38 | 26.16 | 31.22 | .655 |
| Resident in Florence | 31.64 | 12.23 | 19.41 | .086 |
| Parental divorce/death | 42.6 | 21.09 | 21.51 | .478 |
| Only child | 21.52 | 9.28 | 12.23 | .550 |
| Maternal PD | 33.75 | 15.19 | 18.56 | .686 |
| Paternal PD | 35.85 | 17.29 | 18.56 | .747 |
| Family history of SBTS | 8 | 3.79 | 4.21 | .961 |
| Poor school performance | 20.68 | 11.39 | 9.28 | .193 |
| School failure | 17.30 | 8.86 | 8.43 | .536 |
| Bullying | 38.40 | 17.29 | 2.09 | .665 |
| RCCI | 17.30 | 6.75 | 10.54 | .270 |
| Winter/spring ADM | 58.65 | 28.27 | 30.37 | .616 |
| School day ADM | 69.20 | 30.8 | 38.39 | .283 |
| Self-cutting | 41.34 | 4.21 | 37.13 | .000 |
| Intoxication | 27.43 | 24.47 | 2.95 | .000 |
| Previous IS | 83.54 | 39.24 | 44.3 | .926 |
| Previous AS | 23.62 | 14.34 | 9.28 | .017 |
| Previous specialist care | 83.54 | 35.86 | 47.67 | .007 |
| Drug | 61.60 | 27 | 34.60 | .241 |
| MD | 55.27 | 27 | 28.27 | .489 |
| DICCD | 8.01 | 6.33 | 1.69 | .003 |
| ID | 2.90 | 0.42 | 2.54 | .080 |
| Anxiety | 24.05 | 11.39 | 12.65 | .926 |
| ND | 12.23 | 7.17 | 5.06 | .175 |
| Substance abuse | 5.90 | 2.95 | 2.95 | .807 |
| RCCI after discharge | 24.05 | 13.08 | 10.97 | .190 |
*For each entry, the percentage of inpatients belonging to the category and the percentage of patients belonging to the category divided by admission reason: “suicidal motivation patients” (AS/FS) and “suicidal volition patients” (patients with low-damaging SBTs) are shown.
**The corresponding p-value is shown, whereby values below .05 indicate a dependence of the entry variable with the admission reason reporting the highest frequency value.
Note: adm = admission time; AS = attempted suicide; FS = failed suicides; DICCD = disruptive-impulse-control and conduct disorders; ID = intellectual disability; MD = mood disorder; ND = neurodevelopmental disorder; PD = psychiatric disorder; RCCI = Residential Child Care Institution; SBT = Suicidal Behaviors and Thoughts.
Our study included 237 hospitalizations per SBT and represented 33.86% of the total hospitalizations of the CAPEU. In addition, 14.77% of patients exhibited SBTs twice or three times during the study period. Regarding temporal trends, the hospitalization percentage for SBTs switched from 26.92% in 2016 to 52.83% in the first half of 2020. Specifically, hospitalizations are shown in Table 2.
Table 2.
Absolute annual distribution and percentage of hospitalizations per SBTs compared to the total annual hospitalizations at the CAPEU of the Meyer Children’s Hospital in Florence in the period 2016–2020.
| Year | SBTs N° | Total hospitalizations (N°) | SBTs/total hospitalizations (%) |
|---|---|---|---|
| 2016 | 35 | 130 | 26.92% |
| 2017 | 53 | 166 | 31.93% |
| 2018 | 45 | 162 | 27.78% |
| 2019 | 76 | 189 | 40.21% |
| 2020 | 28 | 53 | 52.83% |
| Total | 237 | 700 | 33.86% |
Note: CAPEU = Child and Adolescent Psychiatry Emergency Unit; N = number; SBTs = suicidal behaviors and thoughts.
The female/male ratio among our population was 2.9:1 (177 females and 60 males), whilst the age ranged between 7.4 and 17.9 years (mean 15.44 ± 1.67). Age-related stratification showed that 43.04% (102 patients) of SBTs occurred in 16 to 18-year-old patients, followed by 14 to 16-year-olds (37.13%; 88 patients), 12 to 14-year-olds (16.88%; 40 patients) and those less than 12 years old (2.95%; 7 patients). We detected a female prevalence in patients older than 12 years old (75.65%; 173 females) and a male prevalence (57.14%; 4 males) in subjects younger than 12 years old.
The most common referral reasons were, in order of frequency, suicidal ideation (53.16%; 126 patients), followed by attempted suicide (32.07%; 76 patients) and failed suicide (14.77%; 35 patients). Forty-eight-point-five percent of the entire population (105/237) showed a family history of neuropsychiatric disorders, 5.5% of them (13 patients) having a family history of suicidal behaviors. In our study, 81.01% (191 patients) of the population reported one or more STEs during their life. Previous suicidal behaviors were a common finding and 64.98% (154 patients) revealed a lifelong history of nonsuicidal self-injury.
The most frequent diagnosis at discharge was mood disorder (55.27%; 131 of patients), with a significant prevalence in females (70.99%), followed by feeding and eating disorders (11.81%; 28 of patients) and trauma and stress-related disorders (9.70%; 23 of patients). Considering all patients, 162 (68.35%) showed comorbidities: anxiety disorder (16.88%; 40 patients), multimorbidity (14.77%; 35 patients) and neurodevelopmental disorder (6.33%; 15 patients). Sixty-one-point six percent (146 patients) already had a drug prescription in mono and polytherapy including atypical antipsychotics (39.24%), mood stabilizers (33.76%), antidepressants (29.96%), and anxiolytics (21.52%). Most patients (83.54%; 197 patients), when admitted, were already on psychiatric or psychological care.
“Suicidal volition patients” versus “suicidal motivation patients”
Comparing patients admitted for “suicidal volition” (53.16%; 126/237) and subjects hospitalized for “suicidal motivation” (46.84%; 111/237), we found statistically significant differences in the method of suicide and previous specialist care (see Table 1). Furthermore, a correlation between people admitted for “suicidal motivation” and aged younger than 12.5 years old, χ2(1, N = 237) = 4.516, p = .034, previously attempted suicide, χ2(1, N = 237) = 5.672, p = .017, intoxication, χ2(1, N = 237) = 64.651, p < .01, and disruptive, impulse-control or conduct disorder diagnosis, χ2(1, N = 237) = 8.554, p = .003, was demonstrated. A higher risk in the group of “suicidal volition,” instead, was demonstrated for self-cutting behavior, χ2(1, N = 237) = 90.047, p < .01, and previous specialist care, χ2(1, N = 237) = 7.373, p = .007) (see Table 1).
Artificial intelligence: Neural network approach
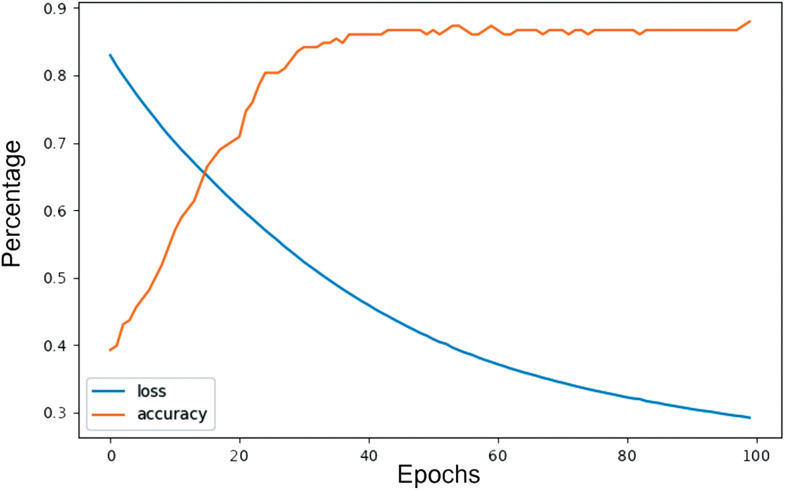
The dataset, consisting of 237 subjects, was divided into a train set (166 cases, equivalent to 70% of the total) and a test set (71 cases, equivalent to 30% of the total) to train and test the implemented network. The number of epochs fixed at 100 allows us to avoid the phenomenon of data overfitting. This phenomenon occurs when the weight model follows the test set too specifically and cannot adapt to other examples, which leads to a loss of accuracy. The network described achieved a final accuracy of 86.7% (Figure 1).
Figure 1.
Neural network approach: Graph showing loss (mean squared error) and accuracy versus number of training epochs. It achieved an 89% accuracy.
K-fold CV and LOOCV generally produce a less biased model than other methods as they ensure that every observation in the original dataset has a chance to appear in the training set and the test set. Sometimes the value obtained with LOOCV is considered to be the “ideal” value achievable by the model despite the fact that in general LOOCV can be subject to high variance (so that very different estimates would be obtained if the estimation were repeated with different initial samples of data from the same distribution) or overfitting since the model is being provided with almost all of the training data to learn and only a single observation to evaluate. In the present case, for K = 5 the model obtains an average accuracy of 84%, which is consistent with the ideal line obtained with LOOCV, i.e. indicating the model's stability in predicting with this accuracy value, which is slightly lower than that obtained in the previous test.
Discussion
Overall, out of 700 inpatients admitted to CAPEU between January 2016 and June 2020, 33.86% were for STBs with a significant increase over the years and hospitalization for SBTs switched from 26.92% in 2016 to 52.83% in the first half of 2020. More than 75% of patients were female, except for subjects younger than 12 years old, who showed a male/female ratio of 1.3:1. Male prevalence in younger patients seems to be related to the common finding of Disruptive, Impulse-control and Conduct-Disorders, which are known to have a male-prevalence. 28
The greatest incidence of SBTs is observed in spring and winter (56.96% of cases), probably due to the potentially stressful role of school. This data, already highlighted by the international literature, 29 is confirmed by the higher incidence of SBTs during weekdays (69.20%) compared to weekends and school holidays (30.8%). In addition, school difficulties are the second leading cause of triggering SBTs (8.44). More than 14% of our patients had a second or third re-hospitalization for SBTs. Determining the rate of rehospitalization with a diagnosis of suicidal ideation or attempted suicide within a year could be useful for the implementation of preventive measures. The presence of psychiatric disorders in 99.58% of patients could be related to their enrollment in an emergency department of a mental health third-level center. Additionally, mood disorders are the most frequent diagnosis at discharge, often associated with anxiety, behavior and eating disorders. In our sample, 68.35% of patients had one or more psychiatric comorbidities confirming that suicidal risk is strictly connected with the number of psychiatric diagnoses. 30
Suicidal ideation was the main reason for hospitalization in our series (45.15%), followed by suicide attempts (32.07%). Patients with suicide attempts/failed suicide did not show an increased presence of suicidal behaviors such as previous ideation or self-cutting, unlike patients with suicidal ideation. Furthermore, suicide attempts in the group of patients hospitalized for attempted suicide occurred mostly through intoxication (voluntary drug ingestion), and this figure is also consistent with that of other studies. 31
However, it appears that more patients with “suicidal volition” than those with “suicidal motivation” have greater access to previous specialist treatments. This datum is coherent and explicable with the fact that in many psychiatric illnesses with developmental onset and in particular, depressive disorder and bipolar disorder, acute psychotic disorder, posttraumatic stress disorder, eating disorders, anxiety, personality disorders with high impulsivity, and chronic or repetitive suicide may be a component of the syndrome. 32
Our observation of a strong correlation between age <12.5 years and a higher risk of “suicidal motivation” is scarcely observed in the literature. Consistent with this finding, a few other studies have identified a similar prevalence of suicidal ideation in boys and girls through age 12 and a higher prevalence of suicide attempts in boys than in girls in this age group. 33 It may be related to a higher rate of diagnoses of Disruptive, Impulse Control and Conduct Disorders and underreporting of thoughts of death and suicidal ideation in this age group.
Children with these conditions may have a diminished view of their emotions and an understanding of their own frustration, which can lead them to internalize their difficulties and experience self-harming thoughts and impulsive behaviors. This may be related to their difficulty recognizing or communicating their distressing thoughts and sometimes referral adults and clinicians may have difficulty assessing the nature and intent of their behavior. Accurate estimation of suicidal risk remains one of the most difficult and most important tasks that clinicians face. Estimation of suicidal risk also requires taking into consideration specific factors associated with the progression from suicidal ideation to attempted suicide.
Finally, the information collected in the database for each patient has proved to be relevant for the creation of a predictive model using machine learning tools. Although it is not possible to trace the characteristics of greatest impact clearly and directly after RFE, we can state that the information used to train the model is significant, as it yields an accuracy ranging between about 84 and 86%, on a relatively small input case study, proving to be a reliable monitoring and prediction tool. This work has, therefore, allowed the development of a key instrument able to predict, with good reliability, a suicidal event, giving the possibility to define a new intervention strategy, thus preventing and reducing the risk of suicide.
Conclusions
Our study reveals a significant increase in the hospitalization rate for SBTs among females aged 16–18 years old at the CAPEU of the Meyer Children's Hospital. Risk factors include males under 12 years with disruptive, impulse control and conduct disorder, individuals using intoxication as a suicide method, those with previous suicide attempts, and those with prior specialist care. Early identification of suicide risk factors during childhood and adolescence is crucial. This study contributes to knowledge and prevention efforts, utilizing machine learning techniques.
The limitation of the study is the retrospective nature of the study; however, it is a single-center recruitment, and all patients have been investigated with a standardized protocol.
Future work to improve the study is needed for further exploration, and it will have to consider a greater number of subjects in order to improve the performance of artificial intelligence.
Acknowledgments
The authors declare there are no acknowledgements to be reported for this article.
Author biographies
Michaela Servi (PhD) is researcher at the Department of Industrial Engineering, University of Florence (Italy). Her research work is addressed to 3D modeling, image processing and computer vision, software design, biomedical applications, human-computer interaction, and reverse engineering.
Silvia Chiaro is a child and adolescent psychiatrist who is licensed to practice cognitive-behavior psychotherapy and conducts professional activities in the territory of Florence (Italy). His research interests include prevention, diagnosis, and treatment of adolescent psychopathology (anxiety, mood, behavior, and nutrition disorders)
Elisa Mussi (PhD) is researcher at the Department of Industrial Engineering, University of Florence (Italy). Her research interests include the application of reverse engineering techniques and additive manufacturing technologies to design and manufacture advanced medical task trainers and patient-specific medical devices.
Giovanni Castellini is an associate professor of Psychiatry at the School of Medicine, Department of Health Sciences of the University of Florence (Italy). She works at the Day Hospital for eating disorders of the Psychiatry Unit and at the Andrology, Female Endocrinology and Gender Incongruence unit of the Careggi Polyclinic in Florence. He teaches Psychiatry at the Degree Course in Medicine, Psychology, at the Degree Course in Professional Education, Nursing and in the specialization School of Psychiatry, Neurology and Endocrinology.
Alberta Mereu is a child and adolescent psychiatrist and cognitive psychotherapist. He conducts professional activity at the Maggiore Hospital in Bologna (Italy). His clinical and research interests include the prevention, diagnosis, and treatment of adolescent psychopathology (anxiety, mood, behavioral, and nutritional disorders)
Yary Volpe is an associate professor at the Department of Industrial Engineering, University of Florence (Italy). His research interests include 3D modeling, mechanical design, computational geometry, human-computer interaction, and reverse engineering.
Tiziana Pisano is a medical doctor specialized in child neuropsychiatry, in charge of the Child and Adolescent Psychiatric Unit of the Children's Hospital Meyer IRCCS, Florence (Italy). Her research field concerns pediatric neurology, specifically epilepsy and the mental health of children and adolescents, with a particular focus on emergency treatments.
Footnotes
Author contributions: All authors contributed to the study conception and design. Material preparation and data collection were performed by Silvia Chiaro. The first draft of the manuscript was written by Michaela Servi, Silvia Chiaro, Elisa Mussi, and Tiziana Pisano all authors commented on previous versions of the manuscript. Conceptualization, review, supervision, and editing Tiziana Pisano, Giovanni Castellini, Alberta Mereu, and Yary Volpe. Statistical analysis and artificial intelligence were performed by Michaela Servi, Yary Volpe, and Elisa Mussi. All authors read and approved the final manuscript.
Consent to participate: Written informed consent was obtained from the parents.
The authors take full responsibility for the data, the analyses and interpretation, and the conduct of the research. I have full access to all the data. I have the right to publish all data separately and apart from any sponsor. None of the authors has a financial interest in this publication.
Data availability: The dataset generated during the current study are available from the corresponding author on reasonable request.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics approval: This study was performed in line with the principles of the Declaration of Helsinki. The study was approved by the Paediatric Ethics Committee of the Tuscany Region. 19th April 2022/N°112/2022.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Alberta Mereu https://orcid.org/0000-0003-1079-8581
References
- 1.World Health Organization. Preventing suicide: A global imperative. Geneva, Switzerland: World Health Organization, 2014. [Google Scholar]
- 2.Cha CB, Franz PJ, M Guzmán E, et al. Annual research review: suicide among youth - epidemiology, (potential) etiology, and treatment. J Child Psychol Psychiatry 2018; 59: 460–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andover MS, Morris BW, Wren Aet al. et al. The co-occurrence of non-suicidal self-injury and attempted suicide among adolescents: distinguishing risk factors and psychosocial correlates. Child Adolesc Psychiatry Ment Health 2012; 6: 11. Published 2012 Mar 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention [CDC]. https://www.cdc.gov/index.htm (2018).
- 5.Naghavi M; Global Burden of Disease Self-Harm Collaborators. Global, regional, and national burden of suicide mortality 1990 to 2016: systematic analysis for the Global Burden of Disease Study 2016. Br Med J 2019; 364: l94. Published 2019 Feb 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harmer B, Lee S, Duong TVHet al. et al. Suicidal ideation. In: StatPearls. Treasure Island, FL: StatPearls Publishing, April 24, 2023. PMID: 33351435. Bookshelf ID: NBK565877. [Google Scholar]
- 7.World Health Organization. Comprehensive mental health action plan 2013–2030. https://apps.who.int/iris/bitstream/handle/10665/345301/9789240031029-eng.pdf (2021).
- 8.Navarro MC, Ouellet-Morin I, Geoffroy MC, et al. Machine learning assessment of early life factors predicting suicide attempt in adolescence or young adulthood. JAMA Netw Open 2021; 4: e211450. Published 2021 Mar 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.George A, Johnson D, Carenini G, et al. Applications of aspect-based sentiment analysis on psychiatric clinical notes to study suicide in youth. AMIA Jt Summits Transl Sci Proc 2021; 2021: 229–237. Published 2021 May 17. [PMC free article] [PubMed] [Google Scholar]
- 10.Fortuna LR. Editorial: disrupting pathways to self-harm in adolescence: machine learning as an opportunity. J Am Acad Child Adolesc Psychiatry 2021; 60: 1459–1460. [DOI] [PubMed] [Google Scholar]
- 11.Nordin N, Zainol Z, Mohd Noor MHet al. et al. Suicidal behaviour prediction models using machine learning techniques: a systematic review. Artif Intell Med 2022; 132: 102395. [DOI] [PubMed] [Google Scholar]
- 12.Carson NJ, Mullin B, Sanchez MJ, et al. Identification of suicidal behavior among psychiatrically hospitalized adolescents using natural language processing and machine learning of electronic health records. PLoS One 2019; 14: e0211116. Published 2019 Feb 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Plener PL, Kaess M, Schmahl C, et al. Nonsuicidal self-injury in adolescents. Dtsch Arztebl Int 2018; 115: 23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sarkar P, Sattar FA, Gode Net al. et al. Failed suicide and deliberate self-harm: a need for specific nomenclature. Indian J Psychiatry 2006; 48: 78–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. Br Med J 2016; 355: i4919. Published 2016 Oct 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Association, 2013. https://doi.org/10.1176/appi.books.9780890425596 [Google Scholar]
- 17.Herzog JI, Schmahl C. Adverse childhood experiences and the consequences on neurobiological, psychosocial, and somatic conditions across the lifespan. Front Psychiatry 2018; 9: 420. Published 2018 Sep 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pisano T, Gori S, De Luca L, et al. Peer victimization and developmental psychopathology in childhood and adolescence Italian psychiatric emergency unit. A single center retrospective observational study. Psychol Health Med 2023; 28: 2147–2155. [DOI] [PubMed] [Google Scholar]
- 19.Kaufman J. K-SADS-PL DMS-5. Yale: Yale University. Trad. it. K-SADS-PL DMS-5. Trento: Edizioni Centro Studi Erikson, 2018. [Google Scholar]
- 20.Posner K, Brown GK, Stanley B, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry 2011; 168: 1266–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McHugh ML. The chi-square test of independence. Biochem Med (Zagreb) 2013; 23: 143–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shih JH, Fay MP. Pearson's chi-square test and rank correlation inferences for clustered data. Biometrics 2017; 73: 822–834. [DOI] [PubMed] [Google Scholar]
- 23.Ayat S, Farahani HA, Aghamohamadi M, et al. A comparison of artificial neural networks learning algorithms in predicting tendency for suicide. Neural Comput Appl 2013; 23: 1381–1386. [Google Scholar]
- 24.Rojas R. The backpropagation algorithm. In: Neural networks. Berlin, Heidelberg: Springer, 1996, pp.149–182. [Google Scholar]
- 25.Granitto PM, Furlanello C, Biasioli F, et al. Recursive feature elimination with random forest for PTR-MS analysis of agroindustrial products. Chemom Intell Lab Syst 2006; 83: 83–90. [Google Scholar]
- 26.Pal M. Random forest classifier for remote sensing classification. Int J Remote Sens 2005; 26: 217–222. [Google Scholar]
- 27.Zhang Z. Improved adam optimizer for deep neural networks. 2018 IEEE/ACM 26th international symposium on quality of service (IWQoS). IEEE, 2018.
- 28.Garrett AR, Bazaco SL, Clausen SS, et al. Epidemiology of impulse control disorders and association with dopamine agonist exposure, active component, U.S. Armed Forces, 2014-2018. MSMR 2019; 26: 10–16. [PubMed] [Google Scholar]
- 29.Martin G, Richardson AS, Bergen HA, et al. Perceived academic performance, self-esteem and locus of control as indicators of need for assessment of adolescent suicide risk: implications for teachers. J Adolesc 2005; 28: 75–87. [DOI] [PubMed] [Google Scholar]
- 30.Brådvik L. Suicide risk and mental disorders. Int J Environ Res Public Health 2018; 15: 2028. Published 2018 Sep 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cibis A, Mergl R, Bramesfeld A, et al. Preference of lethal methods is not the only cause for higher suicide rates in males. J Affect Disord 2012; 136: 9–16. [DOI] [PubMed] [Google Scholar]
- 32.Miché M, Hofer PD, Voss C, et al. Mental disorders and the risk for the subsequent first suicide attempt: results of a community study on adolescents and young adults. Eur Child Adolesc Psychiatry 2018; 27: 839–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Haavisto A, Sourander A, Ellilä H, et al. Suicidal ideation and suicide attempts among child and adolescent psychiatric inpatients in Finland. J Affect Disord 2003; 76: 211–221. [DOI] [PubMed] [Google Scholar]