Abstract
BACKGROUND
Short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing (SUNCT) is a rare headache disorder that has been associated with pituitary adenomas. Resection has been posited to be curative.
OBSERVATIONS
A 60-year-old female presented with a 10-year history of SUNCT, which had been medically refractory. Sellar magnetic resonance imaging (MRI) showed a 2 × 2 mm nodule in the right anterolateral aspect of the pituitary. Endoscopic endonasal transsphenoidal resection of the pituitary microadenoma with neuronavigation was performed. The patient felt immediate relief from the headaches. Postoperative MRI showed persistence of the pituitary microadenoma and the resection tract to be inferomedial to the lesion. The right middle and partial superior turbinectomy site was close to the sphenopalatine foramen (SPF). The patient was discharged on postoperative day 1 and remained headache-free without any medications at the 4-month follow-up.
LESSONS
Resection of pituitary lesions associated with SUNCT may not necessarily be the cause of SUNCT resolution. Manipulation of the middle and superior turbinate close to the SPF may lead to a pterygopalatine ganglion block. This may be the mechanism of cure for SUNCT in patients with related pituitary lesions who undergo endonasal resection.
Keywords: SUNCT, SUNHA, pituitary microadenoma, pterygopalatine ganglion block
ABBREVIATIONS: MRI = magnetic resonance imaging, PPG = pterygopalatine foramen, SPF = sphenopalatine foramen, SUNCT = short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing, SUNHA = short-lasting unilateral neuralgiform headache attack, TAC = trigeminal autonomic cephalgia
Short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing (SUNCT) syndrome is a rare headache entity characterized by brief, frequent, paroxysmal, severe unilateral pain. The symptoms occur in the distribution of the ophthalmic and maxillary divisions of the trigeminal nerve; accordingly, ipsilateral trigeminal autonomic phenomena are observed.1 The International Classification of Headache Disorders classifies SUNCT as a short-lasting unilateral neuralgiform headache attack (SUNHA), which falls under the trigeminal autonomic cephalalgias (TACs).2 SUNCT is typically considered a primary disorder; however, pituitary microadenomas have been suggested as an etiology.3 In these cases, the headaches occur ipsilateral to the pituitary lesion and have been cured with resection.3 Herein, we report the case of a patient with medically refractory SUNCT and an associated pituitary microadenoma who underwent failed resection of the lesion despite standard neuronavigation protocols. The patient’s long-standing headache symptoms resolved immediately following surgery.
Illustrative Case
A 60-year-old female presented with a 10-year history of right-sided neuralgiform headaches with associated eye redness and tearing that lasted 10 to 300 seconds each, occurring once to twice per hour. SUNCT was diagnosed. Her symptoms were refractory to medical treatment with carbamazepine and lamotrigine, and she experienced very minimal relief with topiramate, gabapentin, and tramadol. Dedicated sellar magnetic resonance imaging (MRI) revealed a 2 × 2 mm T1 hypointense, T2 hyperintense, noncontrast-enhancing nodule located at the superolateral right aspect of the pituitary gland (Fig. 1). In retrospect, this lesion was present on brain MRI that had been performed when she presented with SUNCT symptoms 7 years before her neurosurgical consultation. Her prolactin (11 ng/mL) and insulin-like growth factor 1 (152 ng/mL) levels were normal. Given her poor response to medical treatment, as well as previous reports of the successful treatment of pituitary microadenoma-associated SUNCT with adenoma resection,3 she was offered resection of the pituitary nodule with the objective of a headache cure. She underwent endoscopic transsphenoidal resection of her lesion with standard neuronavigation protocols. The right middle turbinate was infiltrated with 5 mL of 2% lidocaine, and a right middle and partial right superior turbinectomy was performed with the development of a vascularized nasoseptal flap using monopolar cauterization of the nasal mucosa. The dura was opened, and the lesion was resected using the pointer of the image guidance system and an angled curette. No definite adenomatous tissue was identified intraoperatively; however, the image guidance system confirmed the resection area cavity. No cerebrospinal fluid leaking occurred. Her headache symptoms immediately resolved after surgery. MRI on postsurgery day 1 revealed that the lesion was untouched, with the resection tract medial and inferior to the lesion (Fig. 2). Histopathology demonstrated normal pituitary tissue. She was discharged the day after surgery and has not required any of her pain medications since then. On follow-up after 4 months, she remained headache-free.
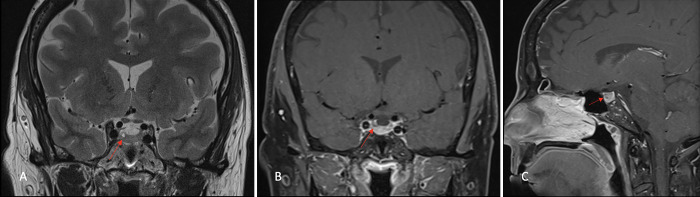
FIG. 1.
Preoperative sellar MRI showing a 2 × 2 mm, T1 hypointense, noncontrast-enhancing pituitary microadenoma located at the superolateral right aspect of the gland (red arrows). Coronal T2-weighted (A) and coronal (B) and sagittal (C) T1-weighted images with gadolinium.
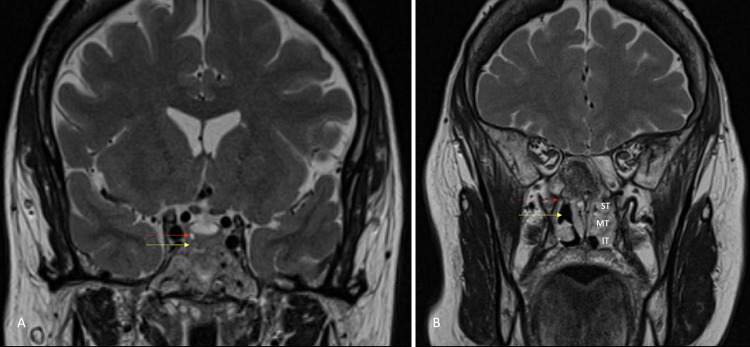
FIG. 2.
Postoperative coronal T2-weighted magnetic resonance image (A) showing the 2 × 2 mm hyperintense nodule (red arrow) and the resection tract, seen as a T2 hyperintensity, inferomedial to the nodule (yellow arrow). Coronal T2-weighted magnetic resonance image (B) at the level of the inferior orbital fissure showing the SPF (red arrow) adjacent to the site of the right middle and partial superior turbinectomy (yellow arrow). IT = inferior turbinate; MT = middle turbinate; ST = superior turbinate.
Discussion
SUNCT is a rare headache disorder without a defined pathophysiology.1 The most widely accepted theory is that an abnormality in the posterior hypothalamus precipitates activation of the trigeminal-autonomic reflex.4–6 Functional imaging and brain stimulation studies have identified activation of the posterior hypothalamic gray matter in TACs, which in turn leads to heightened sensitivity to noxious stimuli via the pain-modulating system of the trigemino-hypothalamic tract and the trigeminovascular system.4–6 These systems then stimulate internal trigger areas in the hypothalamus and trigeminal nucleus caudalis, which activate the superior salivatory nucleus. In turn, they send parasympathetic fibers through the facial (greater superficial petrosal nerve) and pterygopalatine ganglion (PPG; also known as the sphenopalatine ganglion).4–6 In the case of pituitary adenomas, it is suggested that dural stretching, increased intrasellar pressure secondary to large lesions, and cavernous sinus involvement by the tumor cause the activation of nociceptive receptors along the internal carotid artery walls. Direct trigeminal branch contact and hormonal release by the tumors also contribute to the pathomechanisms behind pain.3,7,8 The use of dopamine agonists for prolactinomas often exacerbates SUNCT symptoms.9 This is likely due to the shared properties of dopamine agonists and ergot alkaloids, which are known to affect the activity of the trigeminovascular system.9 These may explain SUNCT symptoms for patients with pituitary macroadenomas or prolactinomas; however, the connection between SUNCT and nonfunctioning pituitary microadenomas is less clear.
Observations
Sixteen cases of SUNCT associated with pituitary adenoma are reported in the literature, and only three of these are nonfunctioning microadenomas.3,7,10 In the three cases reported, two were cured with transsphenoidal resective surgery and one was cured medically, suggesting the role of resection in treating SUNCT that is associated with pituitary microadenomas.3,7 However, in our case, the SUNCT symptoms resolved without resection of the lesion. This brings the connection between SUNCT and pituitary microadenomas into question. During endoscopic endonasal transsphenoidal surgery, the middle turbinate is infiltrated with lidocaine and removed, or at least maximally laterally reflected, to gain access to the keel of the vomer and subsequently the sphenoid sinus. The sphenopalatine foramen (SPF) is the connection between the pterygopalatine fossa and the nasal cavity, and it is located just deep to the attachment of the middle turbinate.11 The pterygopalatine fossa houses the PPG.11 The SPF is also used as a landmark to determine the vascular supply of a nasoseptal flap as the sphenopalatine artery exits through it.11 This foramen is the target when performing transnasal PPG blocks, a common office procedure performed for TACs and other headache disorders.12 The nasal portion of endoscopic transsphenoidal surgery is therefore a PPG block under direct visualization. In our case, this was likely the SUNCT cure. The technique of identification, lidocaine infiltration, and manipulation of the middle turbinate in proximity to the SPF is standard in endoscopic transsphenoidal surgery; therefore, we posit that this adds to the therapeutic effect for SUNCT.
SUNCT is generally medically refractory, which compels the search for alternative treatment paradigms.5 Though direct PPG block with lidocaine has been reported to acutely resolve symptoms in a patient with SUNCT,12 a systematic review on the use of PPG blockade for headache syndromes did not demonstrate a cure for the two SUNCT cases that were included.13 Pulsed radiofrequency of the PPG has been explored as a possible treatment for SUNCT, and this resulted in symptom resolution in seven out of nine cases.14 Gamma Knife radiosurgery of the PPG and trigeminal nerve has also been performed in SUNCT patients, with varying degrees of success.15 Because of the rarity of SUNCT,1 there are no large-sample studies on treatment paradigms for medically refractory SUNCT, and most available data are from case reports and case series. Our case adds to the body of literature on the use of PPG blockade for the treatment of SUNCT. A limitation of our report is the short follow-up duration; however, this surgical treatment was the first in 10 years to afford the patient lasting relief of her SUNCT symptoms.
Lessons
The resection of pituitary adenomas in patients with SUNCT may not necessarily be the cause of cure. The endonasal route with subsequent middle and superior turbinate manipulation may be associated with a PPG block during the procedure owing to the proximity of the SPF to the turbinates. This may be the mechanism behind symptom improvement in other reported cases of endonasal pituitary lesion resection in SUNCT patients.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: Pascual, de Lotbiniere-Bassett, Ignacio, Clark, Starreveld. Acquisition of data: Pascual, Clark, Starreveld. Analysis and interpretation of data: Pascual, Ignacio, Ben-Israel, Clark. Drafting the article: Pascual, de Lotbiniere-Bassett, Ignacio, Clark. Critically revising the article: de Lotbiniere-Bassett, Ignacio, Ben-Israel, Clark. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript on behalf of all authors: Pascual. Administrative/technical/material support: Ignacio, Starreveld. Study supervision: Starreveld.
References
- 1. Sjaastad O, Saunte C, Salvesen R, et al. Shortlasting unilateral neuralgiform headache attacks with conjunctival injection, tearing, sweating, and rhinorrhea. Cephalalgia. 1989;9(2):147–156. doi: 10.1046/j.1468-2982.1989.0902147.x. [DOI] [PubMed] [Google Scholar]
- 2. Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders. Cephalalgia. (3rd edition) 2018;38(1):1–211. doi: 10.1177/0333102417738202. [DOI] [PubMed] [Google Scholar]
- 3. Chitsantikul P, Becker WJ. SUNCT, SUNA and pituitary tumors: clinical characteristics and treatment. Cephalalgia. 2013;33(3):160–170. doi: 10.1177/0333102412468672. [DOI] [PubMed] [Google Scholar]
- 4. Leone M, Bussone G. Pathophysiology of trigeminal autonomic cephalalgias. Lancet Neurol. 2009;8(8):755–764. doi: 10.1016/S1474-4422(09)70133-4. [DOI] [PubMed] [Google Scholar]
- 5. Cesaroni CA, Pruccoli J, Bergonzini L, et al. SUNCT/SUNA in pediatric age: a review of pathophysiology and therapeutic options. Brain Sci. 2021;11(9):1252. doi: 10.3390/brainsci11091252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Stubberud A, Tronvik E, Matharu M. Treatment of SUNCT/SUNA, paroxysmal hemicrania, and hemicrania continua: an update including single-arm meta-analyses. Curr Treat Options Neurol. 2020;22(12):42. [Google Scholar]
- 7. Bosco D, Labate A, Mungari P, Vero S, Fava A. SUNCT and high nocturnal prolactin levels: some new unusual characteristics. J Headache Pain. 2007;8(2):114–118. doi: 10.1007/s10194-007-0370-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Arafah BM, Prunty D, Ybarra J, Hlavin ML, Selman WR. The dominant role of increased intrasellar pressure in the pathogenesis of hypopituitarism, hyperprolactinemia, and headaches in patients with pituitary adenomas. J Clin Endocrinol Metab. 2000;85(5):1789–1793. doi: 10.1210/jcem.85.5.6611. [DOI] [PubMed] [Google Scholar]
- 9. Jiménez Caballero PE. SUNCT syndrome in a patient with prolactinoma and cabergoline-induced attacks. Cephalalgia. 2007;27(1):76–78. doi: 10.1111/j.1468-2982.2007.01229.x. [DOI] [PubMed] [Google Scholar]
- 10. Adamo MA, Drazin D, Popp AJ. Short-lasting, unilateral neuralgiform headache attacks with conjunctival injection and tearing syndrome treated successfully with transsphenoidal resection of a growth hormone-secreting pituitary adenoma. J Neurosurg. 2008;109(1):123–125. doi: 10.3171/JNS/2008/109/7/0123. [DOI] [PubMed] [Google Scholar]
- 11. Nalavenkata S, Meller C, Novakovic D, Forer M, Patel NP. Sphenopalatine foramen: endoscopic approach with bony landmarks. J Laryngol Otol. 2015;129(suppl 3):S47–S52. doi: 10.1017/S0022215115000766. [DOI] [PubMed] [Google Scholar]
- 12. Kocatürk M, Kocatürk Ö. Acute effect of sphenopalatine ganglion block with lidocaine in a patient with SUNCT. Ideggyogy Sz. 2020;73(9-10):345–348. doi: 10.18071/isz.73.0345. [DOI] [PubMed] [Google Scholar]
- 13. Ho KWD, Przkora R, Kumar S. Sphenopalatine ganglion: block, radiofrequency ablation and neurostimulation: a systematic review. J Headache Pain. 2017;18(1):118. doi: 10.1186/s10194-017-0826-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ornello R, Palmisani S, Murphy M, Sacco S, Al-Kaisy A, Lambru G. Sphenopalatine ganglion pulsed radiofrequency for the treatment of refractory chronic SUNCT and SUNA: a prospective case series. Headache. 2020;60(5):938–945. doi: 10.1111/head.13788. [DOI] [PubMed] [Google Scholar]
- 15. Zaed I, Attuati L, Tommasino C, et al. Gamma knife radiosurgery for short unilateral neuralgiform headache attacks with conjunctival injection and tearing (SUNCT) syndrome: targeting the trigeminal nerve and the sphenopalatine ganglion. Case report and literature review. World Neurosurg. 2020;133:167–171. doi: 10.1016/j.wneu.2019.10.016. [DOI] [PubMed] [Google Scholar]