Abstract
BACKGROUND
Adverse radiation effects (AREs) can occur after stereotactic radiosurgery (SRS), and symptomatic cases are often treated with corticosteroids, pentoxifylline, and vitamin E. The supplement 5-Loxin (Boswellia serrata) is an extract of Indian frankincense that inhibits vascular endothelial growth factor expression and has been shown to reduce perilesional edema in brain tumor patients undergoing fractionated radiation.
OBSERVATIONS
Three patients underwent SRS for meningioma or metastasis and developed symptomatic AREs at 4 to 8 months. They were initially treated with corticosteroids, pentoxifylline, and vitamin E with transient improvement followed by recurrent neurological symptoms and imaging findings as steroids were tapered off. All patients were rescued by the administration of 5-Loxin with resolution of neurological symptoms and imaging changes, discontinuation of steroids, and no medication side effects.
LESSONS
The author’s early experience with 5-Loxin has been encouraging, and this supplement has become the author’s first-line treatment for acute radiation effects after SRS. The author reserves bevacizumab for significant mass effect or failure of oral therapy. 5-Loxin has many advantages including low cost, ease of use, and patient tolerability. More experience is needed to confirm the role of 5-Loxin in the upfront treatment of AREs.
Keywords: stereotactic radiosurgery, adverse radiation effects, meningioma, brain metastasis, Boswellia serrata, pentoxifylline
ABBREVIATIONS: ARE = adverse radiation effects, AKBA = acetyl-11-keto-β-boswellic acid, FLAIR = fluid-attenuated inversion recovery, HBO = hyperbaric oxygen therapy, HIF = hypoxia-inducible factor, MRI = magnetic resonance imaging, SRS = stereotactic radiosurgery, VEGF = vascular endothelial growth factor
Stereotactic radiosurgery (SRS) is a widely accepted treatment for brain metastases, benign brain tumors, and vascular malformations. The major risk of SRS is the delayed onset of adverse radiation effects (AREs) in up to 14% of patients.1 Corticosteroids are commonly used to treat the perilesional edema associated with ARE but may cause long-term toxicity. Pentoxifylline and vitamin E have shown positive clinical and radiographic responses in patients who develop ARE after SRS.2 However, we lack a second-line oral agent for patients who do not tolerate this standard therapy or in whom it fails.
Boswellia serrata is an extract of Indian frankincense and contains at least six different boswellic acids including the main bioactive component acetyl-11-keto-β-boswellic acid (AKBA). AKBA is a potent inhibitor of hypoxia-inducible factor (HIF)-1α which results in downstream inhibition of vascular endothelial growth factor (VEGF) expression and reduction in brain edema.3 In this report, three patients are described who underwent SRS for brain tumors, who subsequently developed clinical and radiographic evidence of ARE, and in whom initial therapy with steroids, pentoxifylline, and vitamin E failed.
Patients were treated with 5-Loxin-AKBA Boswellia Extract (Vitacost), which provides 30% AKBA by weight. They were instructed to take 150 mg twice a day with a fatty snack (e.g., cheese, peanut butter) to enhance absorption. Patients were evaluated every 3 to 6 months with neurological examination and contrast-enhanced magnetic resonance imaging (MRI) including axial T1-weighted sequences with contrast and fluid-attenuated inversion recovery (FLAIR) sequences. Corticosteroid dose was adjusted based on neurological symptoms and extent of edema on the FLAIR sequence. 5-Loxin was continued until resolution of symptoms and edema.
We retrospectively performed manual quantitative image analysis utilizing the OsiriX MD software (Pixmeo). The enhancing tumor volume was contoured on the T1-weighted contrast sequence and perilesional edema was measured on the FLAIR sequence. A graph was generated for each patient correlating neurological symptoms, steroid dose, and volumetric data.
Illustrative Cases
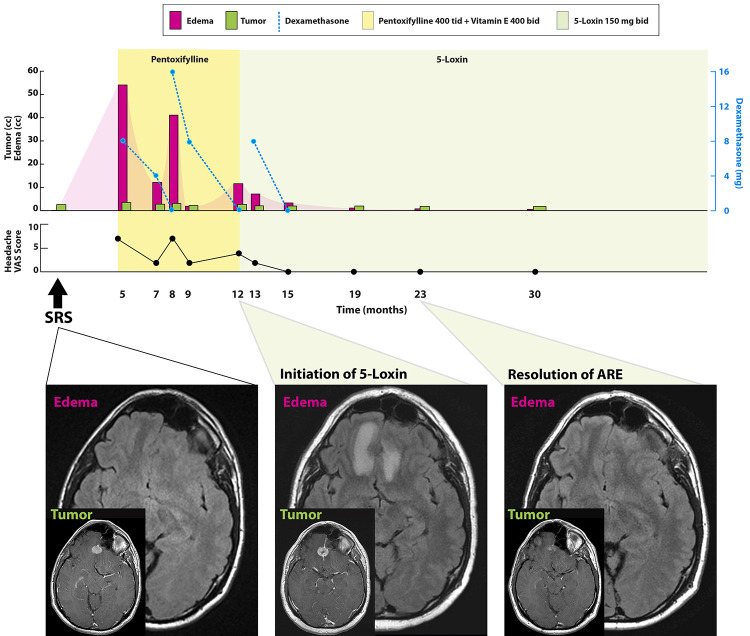
Case 1
A 33-year-old male with Proteus syndrome presented with multiple meningiomas. Serial MRI scans showed gradual enlargement of an anterior frontal falcine meningioma (1.8 cm maximal diameter). The patient underwent Novalis (Brainlab) single-fraction, frameless stereotactic radiosurgery (13 Gy prescription dose). Five months after SRS, the patient returned with frontal headaches, and repeat MRI showed a rim of parenchymal enhancement and significant bifrontal edema (Fig. 1). He was started on dexamethasone 4 mg four times a day, pentoxifylline 400 mg three times a day, and vitamin E 400 IU twice a day. His headaches and ARE imaging findings improved but then recurred after steroids were tapered off. Trimodal therapy was restarted with a similar result (i.e., recurrence after steroid taper). Pentoxifylline and vitamin E were considered to have failed since the patient remained dependent on steroids and his quality of life was limited by significant weight gain and fatigue. We discussed the option of resecting the falcine meningioma or initiating bevacizumab infusions but ultimately started 5-Loxin 150 mg twice a day. The patient was successfully tapered off steroids 3 months later without return of headaches. Follow-up MRI scans showed complete resolution of parenchymal enhancement and perilesional edema and 61% reduction in meningioma volume. The patient continued 5-Loxin for 28 months without adverse effects.
FIG. 1.
Case 1. Timeline of symptoms, imaging findings, and steroid dose according to treatment modality (upper). Axial T1-weighted sequences with contrast and FLAIR sequences at key time points (lower). Baseline MRI at the time of SRS (left) to a 1.8-cm falcine meningioma shows no edema. At 12 months (center), 5-Loxin was initiated after trimodal therapy failed to control AREs (imaging changes include central necrosis, rim of parenchymal enhancement, bifrontal edema). At 23 months (right), MRI shows resolution of the AREs (no perilesional edema, tumor volume decreased 61%). bid = twice a day; tid = three times a day; qid = four times a day; VAS = visual analog scale.
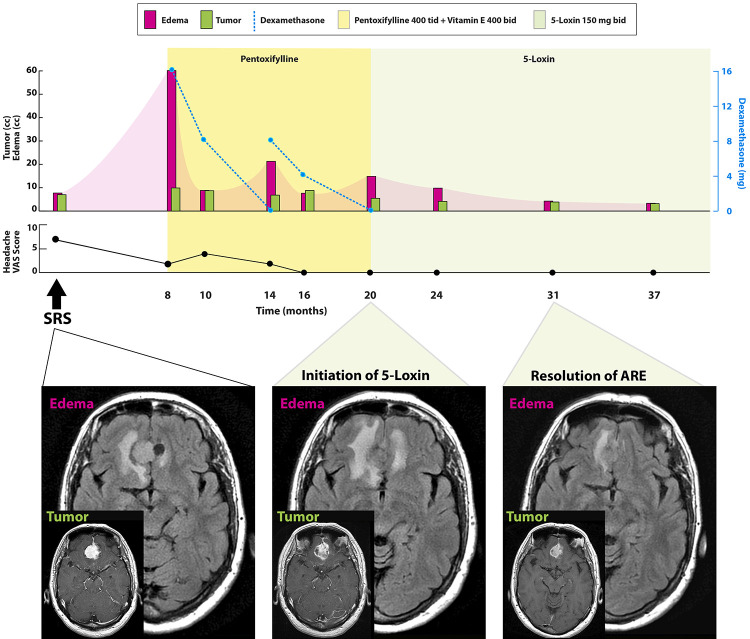
Case 2
A 59-year-old female presented with a gradually enlarging olfactory groove meningioma (2.5 cm maximal diameter). The patient underwent Novalis 5-fraction, frameless stereotactic radiosurgery (25 Gy total prescription dose). Eight months after SRS, the patient complained of frontal headaches and mild confusion. MRI showed irregular parenchymal enhancement and increased bifrontal edema with effacement of the right lateral ventricle (Fig. 2). She was started on dexamethasone 4 mg four times a day, pentoxifylline 400 mg three times a day, and vitamin E 400 IU twice a day. She initially responded to this therapy but her headaches and ARE imaging findings recrudesced as steroids were tapered off. Trimodal therapy was reinstituted with a similar beneficial response, but subsequent MRI showed increased perilesional edema when steroids were again discontinued. We judged pentoxifylline and vitamin E to have failed, as the patient remained steroid-dependent despite 12 months of treatment. We discussed surgery to resect the olfactory meningioma, hyperbaric oxygen therapy (HBO), or bevacizumab. After considering all options, the patient was started on 5-Loxin 150 mg twice a day without steroids. Follow-up MRI showed an 87% reduction in perilesional edema, resolution of mass effect, and 73% decrease in tumor volume. The patient continued 5-Loxin for a total of 17 months without side effects.
FIG. 2.
Case 2. Timeline of symptoms, imaging findings, and steroid dose according to treatment modality (upper). Axial T1-weighted sequences with contrast and axial FLAIR sequences at key time points (lower). Baseline MRI at the time of SRS (left) to a 2.5 cm partially cystic olfactory meningioma shows mild edema. At 20 months (center), 5-Loxin was initiated after patient failed trimodal therapy to control ARE (imaging changes including central necrosis, rim of parenchymal enhancement, increased bifrontal edema). At 31 months (right), MRI shows marked improvement of AREs (perilesional edema decreased 87%, tumor volume decreased 73%).
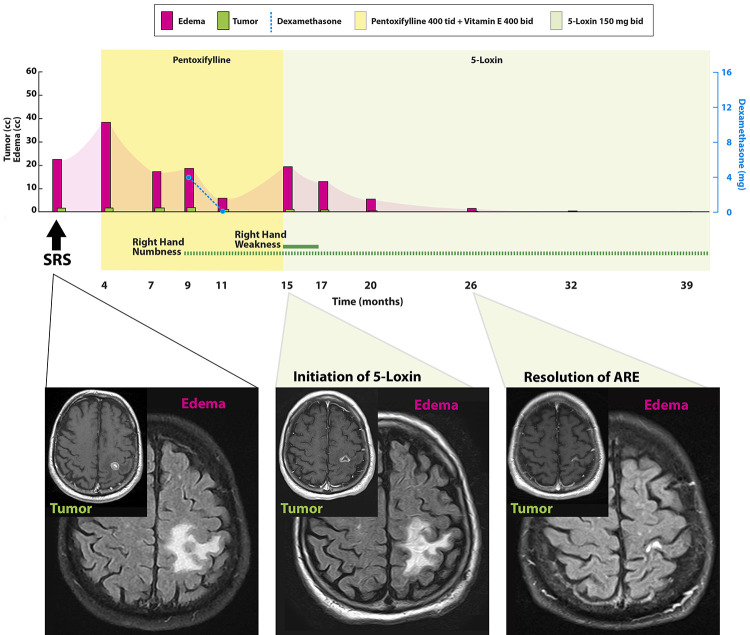
Case 3
A 74-year-old male with melanoma metastatic to the lung presented with right-sided hyperreflexia. MRI revealed a 1.5-cm left motor area metastasis, and the patient underwent Novalis single-fraction, frameless SRS (18 Gy prescription dose). MRI 4 months after SRS showed slight tumor enlargement with hazy enhancing borders and significantly increased perilesional edema (Fig. 3). The patient was started on pentoxifylline 400 mg three times a day and vitamin E 400 IU twice a day. At 9 months, he developed progressive right-hand numbness and began dexamethasone. MRI scans showed gradual improvement in AREs until 15 months after SRS when the patient developed right hand weakness and repeat MRI demonstrated increasing perilesional edema. Pentoxifylline was deemed to be a failure, and we discussed the options of HBO or bevacizumab (surgery was contraindicated based on location). The patient elected to start 5-Loxin 150 mg twice a day. He gradually returned to his neurological baseline and follow-up scans showed complete resolution of perilesional edema and minimal residual enhancement. The patient continued 5-Loxin for 24 months without side effects.
FIG. 3.
Case 3. Timeline of symptoms, imaging findings, and steroid dose according to treatment modality (upper). Axial T1-weighted sequences with contrast and axial FLAIR sequences at key time points (lower). Baseline MRI at the time of SRS (left) to a 1.5-cm melanoma metastasis shows significant edema. At 15 months (center), 5-Loxin was initiated after patient failed trimodal therapy to control ARE (imaging changes including irregular rim enhancement, central necrosis, increased edema compared to post-SRS scans). At 26 months (right), MRI shows resolution of AREs (minimal linear enhancement, no perilesional edema).
Discussion
Observations
In this report, three patients who underwent SRS for meningioma or brain metastasis complicated by symptomatic AREs at 4 to 8 months are described. They were initially treated with steroids, pentoxifylline, and vitamin E with transient improvement followed by recurrent neurological symptoms and imaging findings as steroids were tapered off. All patients were rescued by the administration of 5-Loxin (Boswellia serrata) with resolution of symptoms and imaging changes, discontinuation of steroids, and no medication side effects.
The incidence of ARE after radiosurgery is increasing due to several factors: (1) greater use of SRS for brain metastasis (nearly replacing whole brain radiation), (2) repeated courses of SRS in patients who are living longer with their primary cancer, and (3) negative synergy between SRS and immunotherapy. The treatment options for ARE have evolved over the last 2 decades. Half of these patients have neurological symptoms requiring initiation of corticosteroids. The duration of steroid use varies but many patients experience significant toxicity including immunosuppression, weight gain, hyperglycemia, hypertension, and osteoporosis. The oral combination of pentoxifylline and vitamin E has shown benefit in the treatment of ARE in extracranial soft tissues and in the setting of radiation necrosis after cranial SRS.2 Nonpharmacological interventions include surgery, laser-induced thermal therapy, and HBO.4
Several lines of evidence point to the role of VEGF in the formation of perilesional edema after SRS. Kan et al.5 demonstrated that VEGF expression in meningiomas was correlated with the development of peritumoral edema after radiosurgery. A subsequent study measured plasma VEGF levels in meningioma patients after SRS and noted elevated plasma VEGF levels in patients who developed perilesional edema.6 These and other studies support the causal role of VEGF secretion in the development of ARE through neovascularization, increased vascular permeability, and brain edema. Two randomized controlled trials and multiple retrospective studies have demonstrated the efficacy of bevacizumab for symptomatic brain radiation necrosis7,8 Overall, 91% of patients showed clinical improvement and 85% had a radiographic response. Adverse events occurred in 14% to 55% of patients and were mainly grade 1 or 2 (fatigue, hypertension, proteinuria) and less commonly grade 2 (cerebral ischemia, deep-vein thrombosis, pulmonary embolus). However, bevacizumab (Avastin) requires an implanted venous access device and is expensive ($5,000–$7,000 per injection). Therefore, there is a compelling need for an inexpensive, oral agent for the treatment of ARE in patients with brain tumors who have undergone SRS.
Boswellia serrata is an extract of Indian frankincense and contains at least six different boswellic acids including the main bioactive component AKBA. AKBA is a potent inhibitor of HIF-1α, which results in downstream inhibition of VEGF expression.3 In a murine model of oxygen-induced retinopathy, AKBA inhibited VEGF expression and reduced pathologic neovascularization (endothelial cell proliferation, migration, and tube formation).9 Thus, AKBA was viewed as a potential agent for the prevention of the neovascularization and increased vascular permeability associated with radiation injury.
Kirste et al.10 performed a randomized, placebo-controlled, double-blind study of Boswellia serrata in malignant brain tumor patients undergoing fractionated radiation. Forty-four patients with glioblastoma or brain metastases were randomly assigned to radiotherapy plus either Boswellia serrata 4,200 mg/d or placebo. The primary endpoint was peritumoral edema on T2-weighted MRI scans. A reduction in brain edema of ≥75% was noted in 60% of patients receiving Boswellia serrata compared to 25% of patients receiving the placebo. Adverse events attributed to the study drug were limited to 6 of 20 patients who developed grade 1 to 2 diarrhea. A randomized placebo-controlled study of 5-Loxin for osteoarthritis of the knee established a favorable safety profile.11 Adverse events were limited to gastrointestinal symptoms including diarrhea (8%), nausea (10%), and abdominal pain (4%).
5-Loxin is a patented, standardized extract of Boswellia serrata that provides 30% AKBA by weight. 5-Loxin is readily available in the United States (Vitacost.com) and is inexpensive (approximately $20 per month). Boswellia serrata is lipophilic, and therefore, food intake has a significant effect on its absorption. Sterk et al.12 measured plasma levels of AKBA in healthy volunteers who received Boswellia serrata while fasting or after ingestion of a high-fat meal. The mean total area under the plasma concentration-time curve was 387% higher in patients with concomitant fatty food intake. The average time to peak plasma concentration was 3.0 hours and the half-life was 15.0 hours. AKBA has also been shown to cross the blood–brain barrier reaching concentrations similar to plasma levels after 3 hours.13
These emerging studies prompted us to prescribe 5-Loxin to three patients with adverse radiation effects in whom standard oral therapy with pentoxifylline and vitamin E had failed. All patients were successfully weaned off steroids and MRI scans confirmed resolution of ARE imaging changes. Radiation injury may spontaneously regress, and the impact of a pharmacological intervention may be difficult to determine. Cases 1 and 2 had each failed two courses of trimodal therapy and the patients remained steroid-dependent. Therefore, it is unlikely that the clinical and radiographic responses after initiation of 5-Loxin were spontaneous and coincidental. For case 3, we were encouraged by our initial experience and prescribed 5-Loxin after the first failure of pentoxifylline and vitamin E with similar beneficial results. None of our patients experienced any side effects while taking 5-Loxin, and overall, less than 10% of patients taking 5-Loxin will experience transient gastrointestinal side effects. The duration of 5-Loxin in our report (17–28 months) was largely a patient choice to prevent subsequent recurrence of ARE.
We now use 5-Loxin for patients who have MRI findings of ARE without mass effect. We reserve surgery and bevacizumab for patients who are either highly symptomatic or demonstrate mass effect. We hope to gain sufficient experience with 5-Loxin in the upfront treatment of ARE for a future report. We also envision the potential of 5-Loxin as a prophylactic agent to prevent ARE after SRS especially in patients undergoing SRS followed by immunotherapy.
Lessons
Our early experience with the supplement 5-Loxin has been encouraging and it has become our first-line treatment for acute radiation effects after SRS because of low cost, ease of use, and patient tolerability. We reserve bevacizumab for significant mass effect or failure of oral therapy. More experience is needed to confirm the role of 5-Loxin in the upfront treatment of ARE including timing and optimal dose.
Acknowledgments
We would like to thank Martha Headworth and Tonya Hines for illustration of the case infographics and Laura Mancini for medical editing.
Disclosures
The author reports no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
References
- 1. Sneed PK, Mendez J, Vemer-van den Hoek JG, et al. Adverse radiation effect after stereotactic radiosurgery for brain metastases: incidence, time course, and risk factors. J Neurosurg. 2015;123(2):373–386. doi: 10.3171/2014.10.JNS141610. [DOI] [PubMed] [Google Scholar]
- 2. Williamson R, Kondziolka D, Kanaan H, Lunsford LD, Flickinger JC. Adverse radiation effects after radiosurgery may benefit from oral vitamin E and pentoxifylline therapy: a pilot study. Stereotact Funct Neurosurg. 2008;86(6):359–366. doi: 10.1159/000163557. [DOI] [PubMed] [Google Scholar]
- 3. Lakka A, Mylonis I, Bonanou S, Simos G, Tsakalof A. Isolation of hypoxia-inducible factor 1 (HIF-1) inhibitors from frankincense using a molecularly imprinted polymer. Invest New Drugs. 2011;29(5):1081–1089. doi: 10.1007/s10637-010-9440-4. [DOI] [PubMed] [Google Scholar]
- 4. Chung C, Bryant A, Brown PD. Interventions for the treatment of brain radionecrosis after radiotherapy or radiosurgery. Cochrane Database Syst Rev. 2018;7(7):CD011492. doi: 10.1002/14651858.CD011492.pub2. (Review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kan P, Liu JK, Wendland MM, Shrieve D, Jensen RL. Peritumoral edema after stereotactic radiosurgery for intracranial meningiomas and molecular factors that predict its development. J Neurooncol. 2007;83(1):33–38. doi: 10.1007/s11060-006-9294-y. [DOI] [PubMed] [Google Scholar]
- 6. Park SH, Hwang JH, Hwang SK. Change in plasma vascular endothelial growth factor after gamma knife radiosurgery for meningioma: a preliminary study. J Korean Neurosurg Soc. 2015;57(2):77–81. doi: 10.3340/jkns.2015.57.2.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Levin VA, Bidaut L, Hou P, et al. Randomized double-blind placebo-controlled trial of bevacizumab therapy for radiation necrosis of the central nervous system. Int J Radiat Oncol Biol Phys. 2011;79(5):1487–1495. doi: 10.1016/j.ijrobp.2009.12.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Liao G, Khan M, Zhao Z, Arooj S, Yan M, Li X. Bevacizumab treatment of radiation-induced brain necrosis: a systematic review. Front Oncol. 2021;11:593449. doi: 10.3389/fonc.2021.593449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lulli M, Cammalleri M, Fornaciari I, Casini G, Dal Monte M. Acetyl-11-keto-β-boswellic acid reduces retinal angiogenesis in a mouse model of oxygen-induced retinopathy. Exp Eye Res. 2015;135:67–80. doi: 10.1016/j.exer.2015.04.011. [DOI] [PubMed] [Google Scholar]
- 10. Kirste S, Treier M, Wehrle SJ, et al. Boswellia serrata acts on cerebral edema in patients irradiated for brain tumors: a prospective, randomized, placebo-controlled, double-blind pilot trial. Cancer. 2011;117(16):3788–3795. doi: 10.1002/cncr.25945. [DOI] [PubMed] [Google Scholar]
- 11. Sengupta K, Alluri KV, Satish AR, et al. A double blind, randomized, placebo controlled study of the efficacy and safety of 5-Loxin for treatment of osteoarthritis of the knee. Arthritis Res Ther. 2008;10(4):R85. doi: 10.1186/ar2461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sterk V, Büchele B, Simmet T. Effect of food intake on the bioavailability of boswellic acids from a herbal preparation in healthy volunteers. Planta Med. 2004;70(12):1155–1160. doi: 10.1055/s-2004-835844. [DOI] [PubMed] [Google Scholar]
- 13. Reising K, Meins J, Bastian B, et al. Determination of boswellic acids in brain and plasma by high-performance liquid chromatography/tandem mass spectrometry. Anal Chem. 2005;77(20):6640–6645. doi: 10.1021/ac0506478. [DOI] [PubMed] [Google Scholar]