Abstract
A mouse model was developed to evaluate the efficacy of antibiotic treatment of pneumonic plague; streptomycin was compared to antibiotics with which there is little or no clinical experience. Infection was induced by inhalation of aerosolized Yersinia pestis organisms. Antibiotics were administered by intraperitoneal injection every 6 hours for 5 days, at doses that produced levels of drug in serum comparable to those observed in humans treated for other serious infections. These studies compared in vitro to in vivo activity and evaluated the efficacy of antibiotics started at different times after exposure. Early treatment (started 24 h after challenge, when 0 of 10 mice tested had positive blood cultures) with netilmicin, ciprofloxacin, ofloxacin, ceftriaxone, ceftazidime, aztreonam, ampicillin, and rifampin (but not cefazolin, cefotetan, or ceftizoxime) demonstrated efficacy comparable to streptomycin. Late treatment (started 42 h after exposure, when five of five mice tested had positive blood cultures) with netilmicin, ciprofloxacin, ofloxacin, and a high dose (20 mg/kg of body weight every 6 h) of gentamicin produced survival rates comparable to that with streptomycin, while all of the beta-lactam antibiotics (cefazolin, cefotetan, ceftriaxone, ceftazidime, aztreonam, and ampicillin) and rifampin were significantly inferior to streptomycin. In fact, all groups of mice treated late with beta-lactam antibiotics experienced accelerated mortality rates compared to normal-saline-treated control mice. These studies indicate that netilmicin, gentamicin, ciprofloxacin, and ofloxacin may be alternatives for the treatment of pneumonic plague in humans. However, the beta-lactam antibiotics are not recommended, based upon poor efficacy in this mouse model of pneumonic plague, particularly when pneumonic plague may be associated with bacteremia.
Human infection with Yersinia pestis is usually manifested as bubonic plague. However, pneumonic plague also occurs, either as a result of primary inhalation of aerosolized organisms from close contact with pneumonic plague in a human or animal or secondary to metastatic infection associated with bacteremic spread from a primary bubonic focus. Pneumonic plague remains a threat to human health in areas in which this disease is endemic, as exemplified by a recent case in the United States (7) and recent outbreaks in India (8) and Zambia (30). Pneumonic plague is particularly dangerous, with an incubation period of 3 to 5 days (44) and a mortality rate approaching 100% unless antibiotic treatment is initiated within 24 h of the onset of symptoms (31).
Since its introduction in 1948, streptomycin has been the antibiotic of choice for the treatment of most forms of plague (4). However, this drug is currently available in the United States only by specific request to the streptomycin distribution program of Pfizer, Inc., a circumstance which of necessity entails some delay in initiation of treatment. Besides streptomycin, there are a limited number of antibiotics with demonstrated efficacy for the treatment of plague in humans. Gentamicin and tetracyclines have been used with success (11, 23, 45), while trimethoprim-sulfamethoxazole has also been employed, with both success (32) and disappointing results (6). For the treatment of pneumonic plague, streptomycin, chloramphenicol, and the tetracyclines have demonstrated efficacy (11, 31).
There are a number of antibiotics, including the quinolones, cephalosporins, ampicillin, amoxicillin, and rifampin, which demonstrate in vitro activity against Y. pestis (19, 43), but there is little or no published human experience with these antibiotics for the treatment of plague in general and pneumonic plague in particular.
Studies of experimental bubonic plague in laboratory animals have demonstrated efficacy for a number of antibiotics, including quinolones, such as ciprofloxacin (25, 26, 35, 36) and ofloxacin (2, 25, 35); penicillins, such as ampicillin (5, 35) and amoxicillin (2); rifampin (28, 35); broad-spectrum cephalosporins, such as ceftriaxone (2, 37, 38), cefoperazone (38), cefotaxime (38), and ceftazidime (38); and other aminoglycosides, such as gentamicin (41) and netilmicin (35). However, none of these studies evaluated antibiotic efficacy for the treatment of pneumonic plague, and in all of them except one (5), antibiotic treatments were initiated within 24 h after challenge.
The purpose of these studies was to investigate the efficacy of a number of antibiotics, all with demonstrated in vitro efficacy against Y. pestis, for the treatment of pneumonic plague in a murine model of infection and to compare the efficacy of the tested drugs to streptomycin. For most studies, two antibiotic regimens were tested, one with early initiation (24 h after aerosol infection) and the other with late initiation (42 h after aerosol infection). This experimental design was used primarily to determine if any of the antibiotics tested were superior to streptomycin, particularly for the late treatment of pneumonic plague. In addition, this design provided for an assessment of differences in antibiotic efficacy for treatment of early, localized infection versus treatment of well-established, disseminated infection.
In order to investigate unexpected findings in the treatment of pneumonic plague, i.e., that late treatment with ceftriaxone appeared to accelerate mortality compared to normal-saline (NS)-treated control mice, the efficacy of streptomycin was also compared to ceftriaxone following subcutaneous infection with Y. pestis. These studies were performed to determine whether the problems observed with ceftriaxone therapy of pneumonic plague were unique to this form of the disease or if similar problems would also be observed in the treatment of bubonic plague with this antibiotic.
MATERIALS AND METHODS
Mice.
Adult female Hsd:ND4 mice, 6 to 8 weeks old and weighing 19 to 25 g, were obtained from Harlan-Sprague-Dawley, Indianapolis, Ind., and were used for all studies. The mice had free access to food and water throughout the course of the study. When it was determined that death was imminent within a few hours, moribund mice were humanely euthanatized by cervical dislocation or injection with a solution consisting of ketamine, xylazine, and acetylpromazine. Time of death was recorded as the time of euthanasia, and these mice were included in all analyses of outcome. Usually 15 to 25% of the total number of deaths were the result of euthanasia.
In conducting the research described in this report, the investigators adhered to the “Guide for the Care and Use of Laboratory Animals,” prepared by the Committee on Care and Use of Laboratory Animals of the Institute of Laboratory Animal Resources Commission of Life Sciences-National Research Council. The facilities are fully accredited by the American Association for Accreditation of Laboratory Animal Care.
Preparation of the Y. pestis challenge strain for aerosolization and subcutaneous injection.
Y. pestis CO92 (kindly provided by T. Quan, Centers for Disease Control and Prevention, Fort Collins, Colo.) was originally isolated in 1992 from a fatal human case of pneumonic plague (16). The 50% lethal dose (LD50) in mice for this strain is 1.9 CFU when administered by subcutaneous injection (46) and 2.3 × 104 CFU inhaled when administered by aerosolization (20).
The inoculum for aerosol challenge was prepared as previously described (1). The suspension of Y. pestis was diluted to the appropriate aerosol challenge dose, and the exact concentration was determined by preparing 10-fold dilutions in heart infusion broth and plating aliquots on sheep blood agar plates (SBAP). The plates were then incubated for 2 days at room temperature, and the colonies were counted.
Aerosol infection.
Inhaled doses of 100 ± 50 LD50s of Y. pestis were administered to mice by nose-only aerosol exposure as previously described (1). The aerosol was generated by a 3-Jet Collison nebulizer (29) and sampled continuously during the 10-min exposure (6 liters/min) with an all-glass impinger containing 10 ml of heart infusion broth. The aerosol concentrations were determined by plating dilutions of the sampled aerosol on SBAP and counting the colonies. The inhaled dose (CFU/mouse) was estimated by using Guyton’s formula (22).
Subcutaneous infection.
Doses of 1 × 104 to 1.5 × 104 LD50s of Y. pestis CO92 were administered in a volume of 0.2 ml by subcutaneous injection in the interscapular area of the back.
In vitro antibiotic susceptibility testing.
MIC determinations of the test strain of Y. pestis were performed at 35°C by an automated microdilution technique (Microscan; Baxter Diagnostics, Deerfield, Ill.), except for streptomycin. Because streptomycin was not available on a microdilution plate at the concentration required, the MIC was determined by broth macrodilution in Mueller-Hinton broth (39). Y. pestis microdilution panels and broth macrodilution tubes were incubated for 48 h prior to MIC determinations.
Antibiotics.
Intravenous preparations of the following antibiotics were obtained from the manufacturers, either in solution or reconstituted according to the manufacturers’ directions: streptomycin (Pfizer, New York, N.Y.), ciprofloxacin (Miles, West Haven, Conn.), ofloxacin (Ortho Pharmaceutical, Raritan, N.J.), gentamicin (Lyphomed, Deerfield, Ill.), netilmicin (Schering, Kenilworth, N.J.), ceftriaxone (Roche Laboratories, Nutley, N.J.), ampicillin (Apothecon; Bristol-Myers Squibb, Princeton, N.J.), cefazolin (SmithKline Beecham, Philadelphia, Pa.), cefotetan (Stuart, Wilmington, Del.), ceftazidime (Glaxo, Research Triangle Park, N.C.), ceftizoxime (Fujisawa, Deerfield, Ill.), aztreonam (Bristol-Myers Squibb), and rifampin (Marion Merrill Dow; Kansas City, Mo.). Streptomycin in solution, obtained from Pfizer, was used for MIC determinations.
All antibiotics, or NS, were administered by intraperitoneal injection in a volume of 0.2 ml every 6 h (q6h) for 5 days, unless the mouse died during the antibiotic treatment course.
Assessment of antibiotic efficacy.
Mice exposed to Y. pestis by aerosolization and subcutaneous injection were evaluated in groups of 15 to 20 (usually 20). For groups of 20 mice, the statistical power of detecting a difference in efficacy of 50% for one antibiotic versus 90% for another is 0.81. Mortality was assessed and recorded every 6 h during antibiotic administration and daily for a minimum of 2 weeks after completion of the antibiotic course. Results from similar treatment groups were pooled for statistical analysis.
Antibiotic pharmacokinetics.
Four to seven mice were terminally bled after being subjected to deep anesthesia with a solution containing ketamine, xylazine, and acetylpromazine at each time point specified (usually 15, 30, 60, 90, and 120 min after injection). Log-linear regression of the terminal elimination phase concentration data was used to calculate the elimination half-life (t1/2 = ln 2/kel, where kel is the elimination rate constant for each antibiotic) (21). The time above MIC was calculated by the formula −ln (MIC/a)/kel, where a is the y intercept of the time-concentration curve.
The antibiotic levels were determined according to a modified microbiological assay (18) by Microbiology Reference Laboratory, Cypress, Calif.
Quantitative blood cultures.
Untreated Y. pestis-infected mice were used for quantitative blood culture determinations. Following anesthesia with a mixture of ketamine, acetylpromazine, and xylazine, 200 μl of blood was obtained by intracardiac puncture. The blood was immediately diluted in 800 μl of cold NS and then stored on ice, followed by serial 10-fold dilutions within 60 min. One hundred microliters from each dilution tube was spread on SBAP, in duplicate, and CFU were counted after incubation at room temperature for 48 h.
Pathology.
Postmortem tissue samples of all major organs were collected from approximately 50% of the dead (including the euthanatized) animals during all studies, including antibiotic-treated mice and NS-treated mice. Tissue samples were fixed in 10% neutral buffered formalin and then routinely processed, embedded in paraffin, and sectioned (5- to 6-μm-thick sections) for hematoxylin and eosin staining as previously described (13). Selected replicate tissue sections were Giemsa stained and immunohistochemically evaluated for reactivity with polyclonal monospecific rabbit anti-fraction 1 (F1) capsule antiserum as previously described (13).
Statistical analysis.
Antibiotic efficacy for treatment groups was compared to that of streptomycin by Fisher’s exact two-tailed test. In mice infected with aerosolized Y. pestis, the survival associated with late beta-lactam treatment was compared to treatment with NS by the LIFETEST Procedure, (Statistical Analysis System) (40).
RESULTS
In vitro susceptibility tests.
The test strain of Y. pestis, CO92, was susceptible to all of the antibiotics studied (Table 1).
TABLE 1.
Antibiotic MICs (for Y. pestis CO92), t1/2 in serum, and doses (for Hsd:ND4 mice), calculated antibiotic time above MIC, peak antibiotic levels, and calculated antibiotic peak/MIC ratio
| Antibiotic | MIC (μg/ml)a | t1/2 in serum (min) | Dose q6h (mg/kg) | Time above MIC (min) | Peak level (μg/ml)b | Peak level/MICc |
|---|---|---|---|---|---|---|
| Streptomycin | 4 | 16.7 | 40 | 63 | 40.7–84.2 | 10.2–21.0 |
| Netilmicin | <2 | 13.2 | 12 | 55 | 9.8–22.4 | 9.8–22.4 |
| Gentamicin | ||||||
| Low dose | 2 | 11.5 | 12 | 57 | 12–14.4 | 6–7.2 |
| High dose | NDd | 20 | ND | 45.5 | 22.7 | |
| Ciprofloxacin | <1 | 23.6 | 30 | 106 | 7.4–9.8 | 14.8–19.6 |
| Ofloxacin | <2 | 20.7 | 30 | 58 | 8.5 | 8.5 |
| Cefazolin | 4 | 23.5 | 333 | 193 | 522–532 | 130.5–133 |
| Cefotetan | <4 | 18.8 | 333 | 151 | 607 | 303.5 |
| Ceftriaxone | <2 | 65 | 250 | 453 | 240–246 | 240–246 |
| Ceftazidime | <1 | 41.9 | 333 | 351 | 120 | 240 |
| Ceftizoxime | <2 | 15.2 | 333 | 148 | 625 | 625 |
| Aztreonam | <1 | 34.1 | 333 | 305 | 156–398 | 312–796 |
| Ampicillin | <1 | 13.8 | 333 | 123 | 165–239 | 330–478 |
| Rifampin | <1 | 377 | 50 | 2,135 | 26.9 | 53.8 |
After 48 h of incubation.
Each value represents either the mean of three to five separate specimens or the result obtained from three to five pooled specimens.
When the MIC obtained was less than the lowest dilution used, the peak/MIC ratio was calculated based on the next lower dilution.
ND, not done.
Pharmacokinetics.
The peak levels of antibiotics in serum achieved in mice were equal to or greater than those achievable with therapeutic doses used for the treatment of other diseases in humans (Table 1). Gentamicin was evaluated at two different doses: a low dose, which produced levels comparable to those observed in humans with administration every 8 to 12 h, and a high dose, which produced levels comparable to those obtained with once-daily administration (14).
The t1/2 varied from 11 to 17 min for the aminoglycosides to 377 min for rifampin (Table 1). In addition, five trough levels for ceftriaxone (obtained 6 h after injection, immediately prior to the next scheduled injection) were all ≥2 μg/ml, indicating that the levels of this antibiotic in serum were above the MIC for the test organism for most of the time during the course of treatment.
Establishment of the streptomycin treatment model.
Preliminary studies indicated that streptomycin administration, initiated 24 or 42 h after exposure and then administered q6h for 5 days, resulted in apparent cure of the infection in surviving mice. That is, in mice that survived the complete 5-day course of streptomycin, there were no deaths attributed to relapse of plague infection during the subsequent observation period. In contrast, when mice were treated with streptomycin administered q6h for 3 days, a substantial number of deaths due to pneumonic plague occurred after the antibiotic treatment course had been completed, indicating that the Y. pestis infection had not been cured. Since the 5-day course of streptomycin was effective, and because the 5-day treatment course required the same number of antibiotic doses (i.e., 20) as the standard 10-day treatment course for human plague infection, all other antibiotics were compared to the 5-day streptomycin regimen.
Antibiotic efficacy against experimental pneumonic plague.
Early treatment of pneumonic plague with streptomycin resulted in 100% survival, as did treatment with ciprofloxacin, ofloxacin, ceftriaxone, and netilmicin (Table 2). Treatment with aztreonam, ampicillin, ceftazidime, and rifampin resulted in lower survival rates than treatment with streptomycin, but the differences were not statistically significant. Cefazolin, cefotetan, and ceftizoxime were significantly less effective than streptomycin.
TABLE 2.
Effectiveness of early antibiotic treatment in mice with pneumonic plaguea
| Antibiotic | No. of survivors/total (%) | Pb |
|---|---|---|
| Streptomycin | 20/20 (100) | |
| Netilmicin | 20/20 (100) | 1.000 |
| Gentamicin | ||
| 12 mg/kg | 32/40 (80) | 0.043 |
| 20 mg/kg | 16/20 (80) | 0.016 |
| Ciprofloxacin | 35/35 (100) | 1.000 |
| Ofloxacin | 20/20 (100) | 1.000 |
| Cefazolin | 5/20 (25) | <0.00001 |
| Cefotetan | 14/20 (70) | 0.002 |
| Ceftriaxone | 20/20 (100) | 1.000 |
| Ceftazidime | 17/20 (85) | 0.231 |
| Ceftizoxime | 11/20 (55) | 0.00123 |
| Aztreonam | 17/20 (85) | 0.231 |
| Ampicillin | 17/20 (85) | 0.231 |
| Rifampin | 18/20 (90) | 0.487 |
Treatment was initiated 24 h after aerosol infection of Hsd:ND4 mice with 100 ± 50 LD50s of Y. pestis CO92.
Values obtained by Fisher’s exact two-tailed test comparing survival of various antibiotic treatment groups to survival with streptomycin.
Early treatment with both low and high doses of gentamicin demonstrated some efficacy, with survival rates of 80% for both doses, but there was a significant difference between these outcomes and survival with streptomycin. The failures associated with gentamicin appeared to represent the inability of this antibiotic to completely eradicate the challenge organism with a 5-day treatment course; i.e., all of the deaths occurred more than 72 h after completion of the 5-day course of gentamicin. Additionally, histologic examination revealed numerous bacteria that were morphologically and immunohistochemically compatible with Y. pestis, without histologic evidence of gentamicin-induced renal lesions.
Late treatment with streptomycin, netilmicin, ciprofloxacin, and ofloxacin all resulted in similar survival rates (Table 3). High-dose gentamicin (20 mg/kg of body weight) resulted in significantly better survival than did streptomycin.
TABLE 3.
Effectiveness of late antibiotic treatment in mice with pneumonic plaguea
| Antibiotic | No. of survivors/total (%) | Pb |
|---|---|---|
| Streptomycin | 50/85 (59) | |
| Netilmicin | 24/40 (60) | 1.000 |
| Gentamicin | ||
| 12 mg/kg | 12/38 (32) | 0.006 |
| 20 mg/kg | 17/20 (85) | 0.038 |
| Ciprofloxacin | 28/45 (62) | 0.851 |
| Ofloxacin | 12/20 (60) | 1.000 |
| Cefazolin | 2/18 (11) | 0.00021 |
| Cefotetan | 0/19 (0) | <0.00001 |
| Ceftriaxone | 1/40 (2.5) | <0.00001 |
| Ceftazidime | 0/20 (0) | <0.00001 |
| Aztreonam | 0/19 (0) | <0.00001 |
| Ampicillin | 1/19 (5) | 0.000016 |
| Rifampin | 4/20 (20) | 0.0024 |
Treatment was initiated 42 h after aerosol infection of Hsd:ND4 mice with 100 ± 50 LD50s of Y. pestis CO92.
Values obtained by Fisher’s exact two-tailed test comparing survival of various antibiotic treatment groups to survival with streptomycin.
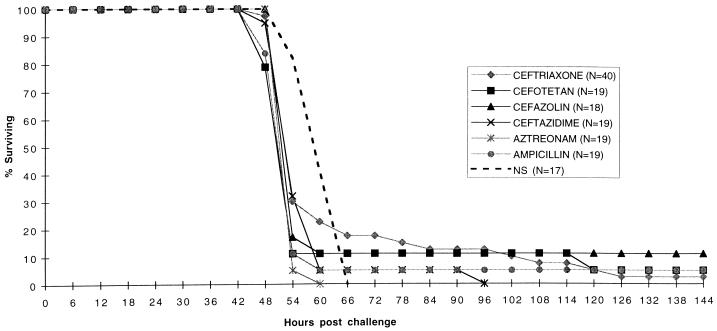
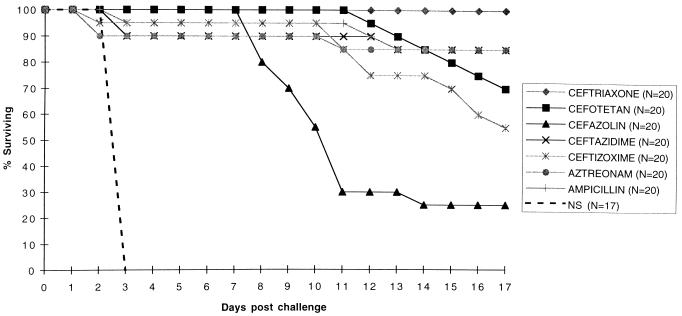
Late treatment with all of the beta-lactam antibiotics tested resulted in very poor survival. In fact, late treatment with these antibiotics (Fig. 1) resulted in accelerated early mortality compared to concurrent NS-treated mice (P was <0.02 [Wilcoxon] for all beta-lactam antibiotics compared to NS). In comparison, survival following early treatment with beta-lactam antibiotics is illustrated in Fig. 2. Note that survival is recorded by days, not hours as in Fig. 1. As shown, most of the deaths associated with early treatment with beta-lactam antibiotics occurred after the course of the antibiotic had been completed.
FIG. 1.
Survival with late treatment of pneumonic plague: six beta-lactam antibiotics compared to NS. The percentage of surviving mice was recorded every 6 h at the times specified. Treatment was initiated 42 h after aerosol infection of Hsd:ND4 mice with 100 ± 50 LD50s of Y. pestis CO92. Results of three studies were pooled. P was <0.02 (Wilcoxon) for all beta-lactam antibiotics compared to NS.
FIG. 2.
Survival with early treatment of pneumonic plague: seven beta-lactam antibiotics compared to NS. The percentage of surviving mice is indicated daily. Treatment was initiated 24 h after aerosol infection of Hsd:ND4 mice with 100 ± 50 LD50s of Y. pestis CO92. Antibiotic treatment was completed on day 6.
Late treatment with rifampin was also ineffective compared to streptomycin.
Antibiotic efficacy against experimental bubonic plague.
For experimental plague initiated by subcutaneous injection of Y. pestis organisms, early treatment with ceftriaxone (initiated 24 h after infection) produced an inferior result compared to early treatment with streptomycin (Table 4). Late treatment with ceftriaxone (initiated ≥42 h after infection) resulted in a dismal outcome, with no survivors for any of the treatment groups. However, ceftriaxone-treated mice experienced a more prolonged mean time to death than the NS-treated mice, in contrast to the accelerated mortality observed with late treatment of pneumonic plague with ceftriaxone.
TABLE 4.
Effectiveness of ceftriaxone versus streptomycin for the treatment of experimental plague infection following subcutaneous injection
| Antibiotic | Time to start of treatment (h postchallenge)a | No. of survivors/total (%) | Time to death (h postchallenge)b | Pc |
|---|---|---|---|---|
| Streptomycin | 24 | 20/20 (100) | ||
| 42 | 14/20 (70) | 296 ± 19.5 | ||
| 48 | 5/20 (25) | 209 ± 24.4 | ||
| 54 | 9/20 (45) | 226 ± 25.8 | ||
| Ceftriaxone | 24 | 14/20 (70) | 272 ± 25.4 | 0.0086 |
| 42 | 0/20 (0) | 152 ± 8.7 | <0.00001 | |
| 48 | 0/20 (0) | 110 ± 9.1 | 0.0005 | |
| 54 | 0/20 (0) | 119 ± 11.8 | 0.0006 | |
| NS | 24 | 0/10 (0) | 65 ± 3.7 | <0.0001 |
| 48 | 0/20 (0) | 72 ± 2.8 | <0.0001 |
Treatment after subcutaneous infection of Hsd:ND4 mice with 1.0 × 104 to 1.5 × 104 LD50s of Y. pestis CO92.
Values are means ± standard errors.
Values obtained by Fisher’s exact two-tailed test comparing survival of various antibiotic treatment groups to survival with streptomycin initiated at the same time postinfection.
Quantitative blood cultures.
All blood cultures were performed on untreated, Y. pestis-infected mice. None of the blood cultures obtained 24 h after either aerosol (0 of 10) or subcutaneous (0 of 8) infection were positive. Forty-two hours after aerosol infection, 100% (five of five) of the blood cultures were positive. Following subcutaneous infection, blood cultures obtained 42, 48, and 54 h after challenge were positive in 50% (5 of 10), 55% (5 of 9), and 37.5% (3 of 8) of the surviving animals, respectively. When positive, quantitative blood cultures demonstrated a broad range, from 102 to 107 CFU/ml (lower limit of detection, 50 CFU/ml), regardless of the time elapsed since challenge or whether the infection was initiated by aerosolization or subcutaneous injection.
Pathology.
Histological examination of the necropsy specimens confirmed the diagnosis of plague as the cause of death in all animals. In the tissues of mice that died during the 5-day antibiotic treatment period, the numbers of Y. pestis organisms observed, particularly in the blood, spleen, or liver, were often diminished compared to NS-treated mice. Microscopic examination of infected tissue also revealed filamentous Y. pestis organisms, up to 24 times their normal length, in mice treated with certain beta-lactam antibiotics (ceftazidime, aztreonam, and ampicillin), as previously reported (13).
DISCUSSION
Of the antibiotics tested in this mouse model of experimental pneumonic plague, the most effective overall, compared to streptomycin, were ciprofloxacin, ofloxacin, and netilmicin. These antibiotics were equivalent to streptomycin for treatment initiated both early and late in the course of infection, and they may offer promise as alternatives to streptomycin for the treatment of pneumonic plague in humans or for prophylaxis against aerosol exposure.
Gentamicin is already used as an alternative to streptomycin for the treatment of human plague. This antibiotic demonstrated efficacy that was superior to streptomycin in this model of pneumonic plague when the high dose was used for late (but not early) treatment. Rifampin was effective when used for early but not for late treatment, so the use of this antibiotic might be limited to prophylaxis or treatment of an infection early in the course of human disease.
Although some of the beta-lactam antibiotics tested (ceftriaxone, ceftazidime, aztreonam, and ampicillin) demonstrated efficacy when started early, late treatment with all beta-lactam antibiotics produced very low survival rates. In fact, late treatment of pneumonic plague with all six of the beta-lactam antibiotics tested was associated with earlier death than with NS treatment. Although this acceleration of mortality associated with late beta-lactam treatment did not occur with experimental plague induced by subcutaneous injection and treated with ceftriaxone, the outcome with respect to overall survival was just as poor.
The paradoxical performance of the beta-lactam antibiotics, i.e., some were effective when started early but none were effective when started late, may be related to different factors. Beta-lactam efficacy is believed to correlate with the total time that levels of the antibiotic in serum are maintained above the MIC for the offending pathogen (17). In these studies, for early treatment, effective cephalosporins and aztreonam all had t1/2 of >30 min and times above MIC of >300 min, while ineffective cephalosporins had t1/2 of 15 to 23 min and times above MIC of <200 min. Hence, efficacy of the beta-lactam antibiotics may follow predictions based on current knowledge of this class of antibiotics when the organism load is low, i.e., early in the course of infection. The exception was ampicillin, which demonstrated efficacy in spite of the shortest t1/2 of the beta-lactam antibiotics tested, and this result remains inexplicable if antibiotic pharmacokinetics are used to explain the outcomes.
The poor performance of the beta-lactam antibiotics for late treatment of infection may well have been due to endotoxin release from organisms as a result of antibiotic effect, a topic which has attracted discussion and controversy in the past (24, 34). Beta-lactam antibiotics have been associated with the release of greater amounts of endotoxin from gram-negative organisms, both in vitro and in vivo, than other classes of antibiotics, including aminoglycosides and quinolones (10, 12, 15, 33, 42). Gentamicin, in fact, has been shown to inhibit the release of endotoxin (27).
The adverse effects associated with the initiation of beta-lactam antibiotic therapy have been reported to be more pronounced with a higher burden of organisms (3), and we observed a similar phenomenon in our studies. As noted, none of the untreated animals tested were bacteremic 24 h after initiation of infection, but all animals were bacteremic 42 hours after aerosol exposure to Y. pestis when the adverse effects attributed to the beta-lactam antibiotics were noted.
Effective late treatment of experimental bubonic plague in mice with a beta-lactam antibiotic has been reported in one previous study, by Butler, in which ampicillin administration initiated 48 h after infection produced survival rates comparable to streptomycin, although the ampicillin-treated mice appeared more ill than the streptomycin-treated mice (5). In contrast, in our studies late treatment with ceftriaxone, starting 42, 48, or 54 h following subcutaneous infection, produced no survivors. This discrepancy in antibiotic efficacy may be explained by the larger number of organisms, 104 CFU, used for subcutaneous challenge in our studies (which resulted in 100% mortality in NS-treated control mice), than the 103 CFU in Butler’s studies (which resulted in 40 to 80% mortality in similarly treated control mice). Presumably, this difference in challenge inocula resulted in a larger burden of Y. pestis organisms in our studies at the time antibiotic treatment was initiated, with an associated decrease in efficacy of ceftriaxone compared to streptomycin.
The relevance of our observations of beta-lactam antibiotic therapy in this murine model of pneumonic plague to human pneumonic plague is not known. However, rapid clinical deterioration following initiation of treatment with beta-lactam antibiotics for pneumonic plague has been reported for one patient treated with ceftazidime (16), two patients treated with ampicillin (30), and one patient treated with ceftriaxone (9).
Other areas of potential discordance between this model and human disease include the different pharmacokinetic properties of the antibiotics in mice and humans and the fact that all of these studies were performed with a single test strain of Y. pestis. With respect to the first consideration, it should be noted that the antibiotic peak levels in mice are all achievable in humans with the same antibiotics. The differences in pharmacokinetics in mice, manifested primarily by shorter t1/2 and more rapid elimination of antibiotics, would tend to bias these studies towards antibiotic failure in this model. It would not be expected that improved pharmacokinetic properties in humans with the antibiotics tested would result in clinical failures of therapy when successful outcomes were observed in this mouse model. For the beta-lactam antibiotics, the failure of late treatment was certainly not the result of different pharmacokinetics in mice, because, as discussed previously, success associated with early treatment with this class of antibiotics correlated with an accepted pharmacokinetic parameter of beta-lactam therapy, the time above MIC. For the aminoglycosides, the shorter t1/2 dictated that doses be increased to produce levels in serum comparable to those observed in humans treated with once-daily dosing. Success comparable to streptomycin was observed when this was done, even though ideally the aminoglycosides would have been administered more frequently than q6h. For the quinolones, regardless of pharmacokinetic properties, efficacy comparable to streptomycin was observed. Thus, the results of these studies are believed to be relevant to the treatment of human disease.
Regarding the use of a single strain of Y. pestis for all studies, although it is theoretically possible that different strains would produce different results in this model of plague, we know of no evidence to suggest that Y. pestis CO92 responds differently to antibiotics than other strains of plague previously used in animal models.
In summary, compared to streptomycin, the most effective of the antibiotics tested in this murine model of pneumonic plague were ciprofloxacin, ofloxacin, and netilmicin. These three antibiotics were equivalent to streptomycin for both early (initiated 24 h after infection) and late (initiated 42 h after infection) treatment. Gentamicin was superior to streptomycin in a single instance, but only when the high dose was used for late treatment. The beta-lactam antibiotics exhibited paradoxical efficacy, as some were effective when started early but none were effective when started late. Based upon these studies, ciprofloxacin, ofloxacin, netilmicin, and gentamicin offer promise as alternatives to streptomycin for the treatment of human pneumonic plague, while the penicillins, cephalosporins, and the monocyclic beta-lactam aztreonam cannot be recommended.
ACKNOWLEDGMENTS
We thank Ralph Tamariello for performance of the aerosol studies and Paul Gibbs for statistical assistance. We also thank the Veterinary Medicine Division for outstanding support for the animal studies.
This work was supported by Department of Defense funds managed by the U.S. Army Medical Research and Materiel Command under the Medical Biological Defense Research Program.
REFERENCES
- 1.Anderson G W, Jr, Leary S E C, Williamson E D, Titball R W, Welkos S L, Worsham P L, Friedlander A M. Recombinant V antigen protects mice against pneumonic and bubonic plague caused by F1-capsule-positive and -negative strains of Yersinia pestis. Infect Immun. 1996;64:4580–4585. doi: 10.1128/iai.64.11.4580-4585.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bonacorsi S P, Scavizzi M R, Guiyoule A, Amouroux J H, Carniel E. Assessment of a fluoroquinolone, three β-lactams, and a cycline in treatment of murine Yersinia pestis infection. Antimicrob Agents Chemother. 1994;38:481–486. doi: 10.1128/aac.38.3.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bucklin S E, Lake P, Lögdberg L, Morrison D C. Therapeutic efficacy of a polymyxin B-dextran 70 conjugate in experimental model of endotoxemia. Antimicrob Agents Chemother. 1995;39:1462–1466. doi: 10.1128/aac.39.7.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Butler T. Yersinia species (including plague) In: Mandell G L, Bennett J E, Dolin R, editors. Mandell, Douglas, and Bennett’s principles and practice of infectious diseases. 4th ed. New York, N.Y: Churchill Livingstone; 1995. p. 2075. [Google Scholar]
- 5.Butler T. Plague and other Yersinia infections. In: Greenough III W S, Merigan T C, editors. Current topics in infectious disease. 1st ed. New York, N.Y: Plenum Publishing Corporation; 1983. pp. 178–182. [Google Scholar]
- 6.Butler T, Levin J, Linh N N, Chau D M, Adickman M, Arnold K. Yersinia pestis infection in Vietnam. II. Quantitative blood cultures and detection of endotoxin in the cerebrospinal fluid of patients with meningitis. J Infect Dis. 1967;133:493–499. doi: 10.1093/infdis/133.5.493. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Pneumonic plague—Arizona. Morbid Mortal Weekly Rep. 1992;41:737–739. [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Update: human plague—India. Morbid Mortal Weekly Rep. 1994;43:761–762. [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Fatal human plague—Arizona and Colorado, 1996. Morbid Mortal Weekly Rep. 1997;46:617–620. [PubMed] [Google Scholar]
- 10.Christ W J, Asano O, Robidoux A L C, et al. E5531, a pure endotoxin antagonist of high potency. Science. 1995;268:80–83. doi: 10.1126/science.7701344. [DOI] [PubMed] [Google Scholar]
- 11.Crook L D, Tempest B. Plague: a clinical review of 27 cases. Arch Intern Med. 1992;152:1253–1256. doi: 10.1001/archinte.152.6.1253. [DOI] [PubMed] [Google Scholar]
- 12.Crosby H A, Bion J F, Penn C W, Elliott T S. Antibiotic-induced release of endotoxin from bacteria in vitro. J Med Microbiol. 1994;40:23–30. doi: 10.1099/00222615-40-1-23. [DOI] [PubMed] [Google Scholar]
- 13.Davis, K. J., P. Vogel, D. L. Fritz, et al. Bacterial filamentation of Yersinia pestis by beta-lactam antibiotics in experimentally infected mice. Arch. Pathol. Lab. Med., in press. [PubMed]
- 14.Demczar D J, Nafziger A N, Bertino J S., Jr Pharmacokinetics of gentamicin at traditional versus high doses: implications for once-daily aminoglycoside dosing. Antimicrob Agents Chemother. 1997;41:1115–1119. doi: 10.1128/aac.41.5.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dofferhoff A S M, Nuland J H, de Vries-Hospers H G, Mulder P O M, Weits J, Bom V J J. Effects of different types and combinations of antimicrobial agents on endotoxin release from Gram-negative bacteria: an in-vitro and in-vivo study. Scand J Infect Dis. 1991;23:745–754. doi: 10.3109/00365549109024303. [DOI] [PubMed] [Google Scholar]
- 16.Doll J M, Zeitz P S, Ettestad P, Bucholz A L, Davis T, Gage K. Cat-transmitted fatal pneumonic plague in a person who traveled from Colorado to Arizona. Am J Trop Med Hyg. 1994;51:109–114. doi: 10.4269/ajtmh.1994.51.109. [DOI] [PubMed] [Google Scholar]
- 17.Drusano G L. Pharmacocology of anti-infective agents. In: Mandell G L, Bennett J E, Dolin R, editors. Mandell, Douglas, and Bennett’s principles and practice of infectious diseases. 4th ed. New York, N.Y: Churchill Livingstone; 1995. pp. 225–233. [Google Scholar]
- 18.Edberg S C. The measurement of antibiotics in human body fluids: techniques and significance. In: Lorian V, editor. Antibiotics in laboratory medicine. 2nd ed. Baltimore, Md: Williams and Wilkins; 1986. pp. 382–399. [Google Scholar]
- 19.Frean J A, Arntzen L, Capper T, Bryskier A, Klugman K P. In vitro activities of 14 antibiotics against 100 human isolates of Yersinia pestis from a southern African plague focus. Antimicrob Agents Chemother. 1996;40:2646–2647. doi: 10.1128/aac.40.11.2646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Friedlander, A. M., S. L. Welkos, P. L. Worsham, et al. 1995. Relationship between virulence and immunity as revealed in recent studies of the F1 capsule of Yersinia pestis. Clin. Infect. Dis. 21(Suppl.):5178–5181. [DOI] [PubMed]
- 21.Gibaldi M, Perrier D. Pharmacokinetics. 2nd ed. New York, N.Y: Marcel Dekker; 1982. pp. 1–44. [Google Scholar]
- 22.Guyton A C. Measurement of the respiratory volumes of laboratory animals. Am J Physiol. 1947;150:70–77. doi: 10.1152/ajplegacy.1947.150.1.70. [DOI] [PubMed] [Google Scholar]
- 23.Hull H F, Montes J M, Mann J M. Septicemic plague in New Mexico. J Infect Dis. 1987;155:113–118. doi: 10.1093/infdis/155.1.113. [DOI] [PubMed] [Google Scholar]
- 24.Hurley J C. Antibiotic-induced release of endotoxin: a reappraisal. Clin Infect Dis. 1992;15:840–854. doi: 10.1093/clind/15.5.840. [DOI] [PubMed] [Google Scholar]
- 25.Kalininskiy N T, Vasil’yev N T, Yudin S M. Effectiveness of quinolones against Y. pestis. Antibiot Khimioter. 1989;34:521–523. [PubMed] [Google Scholar]
- 26.Kasatkina I V, Shcherbanyuk A I, Makarovskaya L N, Padeiskaya E N. Efficacy of the new quinolones—ciprofloxacin and pefloxacin—in experimental plague. Antibiot Khimioter. 1993;38:42–45. [PubMed] [Google Scholar]
- 27.Kusser W C, Ishiguro E E. Effects of aminoglycosides and spectinomycin on the synthesis and release of lipopolysaccharide by Escherichia coli. Antimicrob Agents Chemother. 1988;32:1247–1250. doi: 10.1128/aac.32.8.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Makarovskaya L N, Ryzhkova V V, Zurbayan V A, Bugayeva O K, Pasyukov V V, Fomina I P, Navashin S M. Comparative efficacy of parenteral and oral use of rifampicin to treat experimental plague in albino mice. Antibiot Khimioter. 1995;40:37–39. [PubMed] [Google Scholar]
- 29.May K R. The Collison nebulizer: description, performance and applications. J Aerosol Sci. 1973;4:235–243. [Google Scholar]
- 30.McClean K L. An outbreak of plague in northwestern province, Zambia. Clin Infect Dis. 1995;21:650–652. doi: 10.1093/clinids/21.3.650. [DOI] [PubMed] [Google Scholar]
- 31.McCrumb F R, Mercier S, Robic J, Bouillat M, Smadel J E, Woodward T E, Goodner K. Chloramphenicol and terramycin in the treatment of pneumonic plague. Am J Med. 1953;14:284–293. doi: 10.1016/0002-9343(53)90040-0. [DOI] [PubMed] [Google Scholar]
- 32.Nguyen V-A, Nguyen D-H, Pham V-D, Nguyen V-L. Co-trimoxazole in bubonic plague. Br Med J. 1973;iv:108–109. doi: 10.1136/bmj.4.5884.108-c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nitsche D, Schulze C, Oesser S, Dalhoff A, Sack M. Impact of different classes of antimicrobial agents on plasma endotoxin activity. Arch Surg. 1996;131:192–199. doi: 10.1001/archsurg.1996.01430140082022. [DOI] [PubMed] [Google Scholar]
- 34.Prins J M, van Deventer S J, Kuijper E J, Speelman P. Clinical relevance of antibiotic-induced endotoxin release. Antimicrob Agents Chemother. 1994;38:1211–1218. doi: 10.1128/aac.38.6.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Romanov V E, Vasil’yev N T, Shabalin B A, Kozhemyako A V, Zhivov I V, Yezhov A V. Methods of estimating rapid efficacy of chemotherapeutic preparations promising in special prevention and treatment of plague. Antibiot Khimioter. 1995;40:31–36. [PubMed] [Google Scholar]
- 36.Russell P, Eley S M, Bell D L, Manchee R J, Titball R W. Doxycycline or ciprofloxacin prophylaxis and therapy against experimental Yersinia pestis infection in mice. J Antimicrob Chemother. 1996;37:769–774. doi: 10.1093/jac/37.4.769. [DOI] [PubMed] [Google Scholar]
- 37.Ryzhko I P, Samokhodkina E D, Zhigalova T A. Ceftriaxone in the prophylaxis and treatment of experimental plague infection. Antibiot Khimioter. 1993;38:39–42. [PubMed] [Google Scholar]
- 38.Ryzhko I V, Tsuraeva R I, Pasyukov V V, Samokhodkina E D, Shcherbanyuk A I. Third generation cephalosporins (cefoperazone, cefotaxime, ceftazidime, and ceftriaxone) in the prophylaxis and treatment of experimental plague in albino mice. Antibiot Khimioter. 1996;41:35–38. [PubMed] [Google Scholar]
- 39.Sahm D F, Washington J A., II . Antibacterial susceptibility tests: dilution methods. In: Balows A, Hausler W J Jr, Herrmann K L, Isenberg H D, Shadomy H J, editors. Manual of Clinical Microbiology. 5th ed. Washington, D.C: American Society for Microbiology; 1991. pp. 1105–1116. [Google Scholar]
- 40.SAS Institute. Statistical analysis system, version G. SAS Institute, Cary, N.C.
- 41.Shcherbanyuk A I, Makarovskaya L N, Bugayeva O K, Kasatkina I V. Antibiotics of the aminoglycoside group (gentamicin, sisomicin, and amikacin) in the prevention and treatment of experimental plague infection. Antibiot Khimioter. 1992;37:30–31. [PubMed] [Google Scholar]
- 42.Shenep J L, Barton R P, Mogan K A. Role of antibiotic class in the rate of liberation of endotoxin during therapy for experimental Gram-negative bacterial sepsis. J Infect Dis. 1985;151:1012–1018. doi: 10.1093/infdis/151.6.1012. [DOI] [PubMed] [Google Scholar]
- 43.Smith M D, Vinh D X, Hoa N T T, Wain J, Thung D, White N J. In vitro susceptibilities of strains of Yersinia pestis. Antimicrob Agents Chemother. 1995;39:2153–2154. doi: 10.1128/aac.39.9.2153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tieh T H, Landauer E, Miyagawa F, Kobayashi G, Okayasu G. Primary pneumonic plague in Mukden, 1946, and report of 39 cases with 3 recoveries. J Infect Dis. 1948;82:52–58. doi: 10.1093/infdis/82.1.52. [DOI] [PubMed] [Google Scholar]
- 45.Von Reyn C F, Barnes A M, Weber N S, Quan T, Dean W F. Bubonic plague from direct exposure to a naturally infected coyote. Am J Trop Med Hyg. 1976;25:626–629. doi: 10.4269/ajtmh.1976.25.626. [DOI] [PubMed] [Google Scholar]
- 46.Welkos S L, Davis K M, Pitt L M, Worsham P L, Friedlander A M. Studies on the contribution of the F1 capsule-associated plasmid pFra to the virulence of Yersinia pestis. Contrib Microbiol Immunol. 1995;13:299–305. [PubMed] [Google Scholar]