Abstract
Introduction
Emergency medical service (EMS) resources are limited and should be reserved for incidents of appropriate acuity. Over-triage in dispatching of EMS resources is a global problem. Analysing patients that are not transported to hospital is valuable in contributing to decision-making models/algorithms to better inform dispatching of resources. The aim is to determine variables associated with patients receiving an emergency response but result in non-conveyance to hospital.
Methods
A retrospective cross-sectional study was performed on data for the period October 2018 to September 2019. EMS records were reviewed for instances where a patient received an emergency response but the patient was not transported to hospital. Data were subjected to univariate and multivariate regression analysis to determine variables predictive of non-transport to hospital.
Results
A total of 245 954 responses were analysed, 240 730 (97.88 %) were patients that were transported to hospital and 5 224 (2.12 %) were not transported. Of all patients that received an emergency response, 203 450 (82.72 %) patients did not receive any medical interventions. Notable variables predictive of non-transport were green (OR 4.33 (95 % CI: 3.55–5.28; p<0.01)) and yellow on-scene (OR 1.95 (95 % CI: 1.60–2.37; p<0.01).
Incident types most predictive of non-transport were electrocutions (OR 4.55 (95 % CI: 1.36–15.23; p=0.014)), diabetes (OR 2.978 (95 % CI: 2.10–3.68; p<0.01)), motor vehicle accidents (OR 1.92 (95 % CI: 1.51–2.43; p<0.01)), and unresponsive patients (OR 1.98 (95 % CI: 1.54–2.55; p<0.01)). The highest treatment predictors for non-transport of patients were nebulisation (OR 1.45 (95 % CI: 1.21–1.74; p<0.01)) and the administration of glucose (OR 4.47 (95 % CI: 3.11–6.41; p<0.01)).
Conclusion
This study provided factors that predict ambulance non-conveyance to hospital. The prediction of patients not transported to hospital may aid in the development of dispatch algorithms that reduce over-triage of patients, on-scene discharge protocols, and treat and refer guidelines in EMS.
Keywords: Prehospital, Emergency medical service, Emergency dispatch, Low acuity, Triage, Ambulance dispatch
African relevance
-
•
The EMD is the first point in the activation of the EMS system and is therefore critical in the dispatching of appropriate resources.
-
•
Improved efficiencies in triaging of emergency calls in the EMD will improve resource utilization both in the prehospital and in-hospital environment.
-
•
The EMD has the potential to influence the EMS system financially and economically which is required in a resource constrained environment.
-
•
Over utilization of EMS resources is a global problem that has greater effects on the low to middle income countries.
Introduction
EMS resources are limited, and efforts must be made to ensure they are dispatched to calls of appropriate patient acuity to ensure that patients who need emergency care can get it [1,2]. The most appropriate response also optimises availability of EMS resources for other emergency calls and patients that are experiencing true emergency cases [2,3]. It is estimated that the United States government could save in excess of $560 million dollars per annum by reducing unnecessary transport of patients by EMS to an emergency department (ED) [4]. There are no similar data published for low- to middle-income countries. Over-triage or overestimating the urgency of a patient's condition [5] is not a new problem in EMS and affects many countries globally, with a prevalence between 23.4 % and 78 % [2,[6], [7], [8], [9], [10]].
Consequently, over-triage in emergency medical dispatch (EMD) will result in an urgent response of emergency resources with lights and sirens that may be deemed as inappropriate. Over-triage limits EMS resource availability [2,[6], [7], [8], [9], [10]] which keeps EMS resources working harder for longer hours resulting in tiredness and fatigue of EMS personnel [11]. This study also reports that 48 % of paramedics have fallen off to sleep while driving, increasing the risk of motor vehicle accidents (MVA) and endangering both EMS staff and members of the public. The guideline for the field triage of injured patients from the American College of Surgeons Committee on Trauma (ASCOT) has recommended that over-triage should be less than 35 % [12]. In South Africa it is reported to be as high as 93.5 % [13]. Over-triage rates in the Western Cape EMS are reported to be approximately 67.6 % [14].
South Africa with a population of 59 million people has a target of one ambulance per 10 000 people, [15] - approximately 5 900 ambulances. Currently, there are less than 2 000 ambulances in operation [16] indicating the resource constraint. A South African study has shown that 58 % of emergency responses did not require any medical intervention: such mismatch of supply and demand of emergency resources is a contributing factor to the EMS system not meeting current demand for emergency care [17].
It is reported that the Western Cape EMS in South Africa receive at least 5 000 unnecessary callouts every month [18]. Another report states that 70 % of calls received are non-emergent in nature and range from headache to toothache [19]. Analysing patients that are not transported to hospital will be valuable in the development of evidence-based systems and mechanisms to improve emergency response not only in the context of South Africa but also in other lower- to middle-income countries (LMICs).
In this study we aim to seek variables inclusive of dispatch priority, triage and clinical information that predict the non-transport of patients to hospital by EMS.
Methods
Design
A retrospective cross-sectional study was performed. Electronic patient care records (ePCR) and the computer aided dispatch (CAD) system of a public EMS in the Western Cape Province of South Africa were reviewed for instances where an ambulance response was initiated but the patient was consequently not transported to hospital.
Setting
The EMS in the Western Cape province (130 000 km²) [20] is managed by the Western Cape Department of Health and serves a population of 6.94 million people [21]. EMS in the Western Cape is made up of four main components [22]: (1) Emergency Medical Dispatch or Control Centre (EMD), (2) EMS Rescue Services, (3) HealthNet for planned patient transport and (4) the ambulance service for emergency care and transport.
There are currently 253 ambulances and 1 633 operational personnel which attended to 618 352 emergency cases in 2021/2022 as per Western Cape Government (WCG) annual report [23]. Based on the 1/10 000 per capita ratio for EMS required, there exists a shortfall of 441 ambulances in the province. The private EMS sector is available for emergency response, however it caters primarily for people with medical insurance which is only 18 % of the population [24].
All emergency calls in the EMD are received by a call taker and prioritised according to a two-tier system being priority 1 (P1) or priority 2 (P2) based on descriptive information of the emergency and signs and symptoms received from the caller [25]. A P1 patient is considered to be a higher priority (emergent) dispatch in the EMD relative to the P2 category dispatch [25]. On completion of receiving basic information on the emergency call from the caller, the appropriate response is then dispatched to the call. All information relating to the case in the EMD is captured into the CAD system and all case-related clinical information from the scene of the call is captured into the ePCR by the responding practitioners.
The WCG EMS also utilizes the South African Triage Scale (SATS) to determine the triage of patients which was developed for the resource constrained African setting [26]. SATS is composed of five colours representing various levels of severity of the patient with red being most severe and blue being the least.
Sample and sampling
Data for this study were obtained for the period 1 October 2018 to 30 September 2019 for all primary response cases by the WCG. This timeframe was chosen to overcome confounding factors from COVID-related service pressures and lockdown measures. The data files received from WCG were received separately for CAD and ePCR through Microsoft Excel® (Microsoft Corp. Washington, United States) spreadsheets which excluded any patient identifiable information. All patients that were transported through inter-facility transfers were excluded from the data.
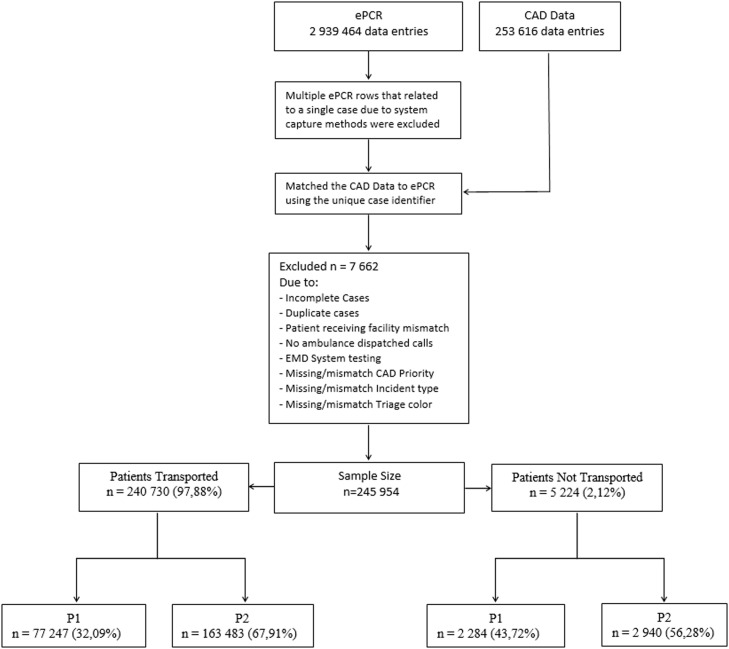
All cases received through the EMD were matched to their respective ePCR cases (Fig. 1). Matching of the data provided for holistic reviews of each case, including dispatch and on-scene information. The ePCR data entries included multiple entries for every time an intervention was administered to the patient such as vital signs monitoring, medical skills or drug administration. These data entries were reduced maintaining initial vital signs and all interventions administered to the patient. Cases were then excluded due to adjustments made for those entries that were duplicated, mismatched, missing data or cases where CAD system testing had been undertaken. Cases were considered non-conveyed if the patient refused transport and was not transported to any receiving facility using any EMS resource.
Fig. 1.
Area under ROC curve
Statistical analysis and procedure
Frequency and percentages are reported for categorical data while means and standard deviations are reported for the continuous variables. Univariate regression was initially conducted to determine purposive variables after which a multivariate logistic regression was performed to evaluate the effect of both clinical and non-clinical variables simultaneously on the likelihood of non-conveyance to hospital. Non-clinical variables (Table 1) included dispatch centre priority and final patient triage. The clinical details (Table 2) included the incident type, patient treatment and drugs administered. Only treatment and drug administration variables that were observed were included in the model.
Table 1.
Frequency and multivariate regression – non-clinical.
| Variables | Transported n=240 730 (97.88 %) | Not Transported n=5 224 (2.12 %) | Total n=245 954 (100 %) | Odds Ratio (95 % CI) | p-value |
|---|---|---|---|---|---|
| Dispatch Centre Priority | |||||
| Priority 1 (Ref. Category) | 77 247 (32.09 %) | 2 284 (43.72 %) | 79 531 (32.34 %) | - | - |
| Priority 2 | 163 483 (67.91 %) | 2 940 (56.28 %) | 166 423 (67.66 %) | 0.78 (0.72-0.84) | <0.001 |
| Final Patient Triage | |||||
| Red (Ref. Category) | 10 869 (4.52 %) | 116 (2.22 %) | 10 985 (4.47 %) | - | - |
| Blue | 3 381 (1.40 %) | 12 (0.23 %) | 3 393 (1.38 %) | 0.22 (0.12-0.40) | <0.001 |
| Orange | 42 910 (17.82 %) | 557 (10.66 %) | 43 467 (17.367 %) | 1.14 (0.93-1.40) | 0.056 |
| Yellow | 114 444 (47.54 %) | 2 084 (39.89 %) | 116 528 (47.38 %) | 1.95 (1.60-2.37) | <0.001 |
| Green | 69 126 (28.72 %) | 2 455 (46.99 %) | 71 581 (29.10 %) | 4.33 (3.55-5.28) | <0.001 |
Table 2.
Frequency and multivariate regression – clinical.
| Variables | Transported n=240 730 (97.88 %) | Not Transported n=5 224 (2.12 %) | Total n=245 954 (100 %) | Odds ratio (95 % CI) | p-value |
|---|---|---|---|---|---|
| Incident Type | |||||
| Haemorrhage | 4 976 (2.07 %) | 110 (2.11 %) | 5 086 (2.07 %) | - | - |
| Abdominal pain | 13 145 (5.46 %) | 175 (3.35 %) | 13 320 (5.42 %) | 0.58 (0.45-0.74) | <0.001 |
| Domestic Injury | 6 817 (2.583 %) | 125 (2.39 %) | 6 942 (2.82 %) | 0.88 (0.68-1.15) | 0.352 |
| Industrial Injury | 935 (0.39 %) | 25 (0.48 %) | 960 (0.39 %) | 1.45 (0.93-2.25) | 0.102 |
| Sport Injury | 903 (0.38 %) | 31 (0.59 %) | 934 (0.38 %) | 1.71 (1.13-2.57) | 0.010 |
| Allergic reactions | 952 (0.40 %) | 12 (0.23 %) | 964 (0.39 %) | 0.47 (0.26-0.86) | 0.014 |
| Animal bites | 2 019 (0.84 %) | 53 (1.01 %) | 2 072 (0.84 %) | 1.02 (0.73-1.42) | 0.915 |
| Assault | 27 052 (11.24 %) | 801 (15.33 %) | 27 853 (11.32 %) | 1.33 (1.08-1.63) | 0.007 |
| Burns | 1 478 (0.61 %) | 35 (0.67 %) | 1 513 (0.62 %) | 1.06 (0.69-1.63) | 0.789 |
| Chest pain | 3 385 (1.41 %) | 84 (1.61 %) | 3 469 (1.41 %) | 1.35 (1.00-1.81) | 0.049 |
| Seizures | 10 668 (4.343 %) | 247 (4.73 %) | 10 915 (4.44 %) | 1.28 (1.01-1.62) | 0.042 |
| Diabetes | 2 175 (0.90 %) | 119 (2.28 %) | 2 294 (0.93 %) | 2.78 (2.10-3.68) | <0.001 |
| Submersion incidents | 95 (0.04 %) | 3 (0.06 %) | 98 (0.04 %) | 1.86 (0.57-6.01) | 0.303 |
| Electrocution | 44 (0.04 %) | 3 (0.06 %) | 47 (0.04 %) | 4.55 (1.36-15.23) | 0.014 |
| Heart related problems | 1 164 (0.48 %) | 39 (0.75 %) | 1 203 (0.49 %) | 1.80 (1.23-2.62) | 0.002 |
| Environmental Emergencies | 72 (0.03 %) | 4 (0.08 %) | 76 (0.03 %) | 2.40 (0.85-6.80) | 0.099 |
| Gynaecology | 3 558 (1.48 %) | 32 (0.61 %) | 3 590 (1.46 %) | 0.40 (0.27-0.59) | <0.001 |
| Obstetrics | 17 426 (8.24 %) | 73 (1.40 %) | 17 499 (7.11 %) | 0.18 (0.13-0.24) | <0.001 |
| Psychiatry | 1 225 (0.51 %) | 31 (0.59 %) | 1 256 (0.51 %) | 1.11 (0.74-1.67) | 0.604 |
| Motor vehicle accidents | 8 516 (3.54 %) | 287 (5.49 %) | 8 803 (3.58 %) | 1.92 (1.51-2.43) | <0.001 |
| Musculoskeletal Injuries | 8 494 (3.53 %) | 125 (2.39 %) | 8 619 (3.50 %) | 0.74 (0.57-0.96) | 0.022 |
| Neurological complaints | 12 830 (5.33 %) | 361 (6.91 %) | 13 191 (5.36 %) | 1.43 (1.15-1.77) | 0.001 |
| Respiratory complaints | 31 634 (13.14 %) | 1 103 (21.11 %) | 32 737 (13.31 %) | 1.46 (1.19-1.8) | <0.001 |
| Vomiting/Diarrhoea | 15 043 (6.25 %) | 171 (3.27 %) | 15 214 (6.19 %) | 0.53 (0.41-0.67) | <0.001 |
| Pain (non-cardiac) | 48 446 (20.12 %) | 743 (14.22 %) | 49 189 (20.00 %) | 0.70 (0.57-0.86) | 0.001 |
| Patient no response | 5 732 (2.38 %) | 181 (3.46 %) | 5 913 (2.40 %) | 1.98 (1.54-2.55) | <0.001 |
| Self-Harm | 4 285 (1.78 %) | 122 (2.34 %) | 4 407 (1.79 %) | 1.39 (1.06-1.81) | 0.015 |
| Fever | 6 039 (2.51 %) | 95 (1.82 %) | 6 134 (2.49 %) | 0.69 (0.52-0.91) | 0.009 |
| Other | 1 622 (0.67 %) | 34 (0.65 %) | 1 656 (0.67 %) | 2.01 (1.35-2.99) | 0.001 |
| Treatment | |||||
| No treatment | 199 062 (82.69 %) | 4 388 (84.00 %) | 203 450 (82.72 %) | - | - |
| Advanced Airway Procedure | 222 (0.09 %) | 1 (0.02 %) | 223 (0.29 %) | 0.60 (0.05-7.83) | 0.698 |
| Airway Other | 714 (0.30 %) | 9 (0.17 %) | 723 (0.29 %) | 0.71 (0.36-1.38) | 0.309 |
| Airway Suction | 387 (0.16 %) | 2 (0.04 %) | 389 (0.16 %) | 0.74 (0.16-3.39) | 0.702 |
| Basic Airway Manoeuvres | 1 301 (0.54 %) | 15 (0.29 %) | 1 316 (0.54 %) | 0.83 (0.50-1.41) | 0.498 |
| Basic Airway Procedure | 263 (0.11 %) | 2 (0.04 %) | 265 (0.11 %) | 1.98 (0.43-9.07) | 0.380 |
| Burns Dressing | 684 (0.28 %) | 18 (0.34 %) | 702 (0.29 %) | 1.42 (0.81-2.47) | 0.222 |
| Direct Pressure | 3 850 (1.60 %) | 86 (1.65 %) | 3 936 (1.60 %) | 1.20 (0.92-1.56) | 0.187 |
| Dressing Application | 12 103 (5.03 %) | 254 (4.86 %) | 12 357 (5.02 %) | 0.80 (0.68-0.94) | 0.007 |
| Limb Splinting | 1 487 (0.62 %) | 6 (0.11 %) | 1 493 (0.61 %) | 0.31 (0.14-0.70) | 0.005 |
| Maternity Care | 2893 (0.12 %) | 1 (0.02 %) | 294 (0.12 %) | 0.85 (0.12-6.14) | 0.873 |
| Nebulization | 8 158 (3.39 %) | 407 (7.79 %) | 8 565 (3.48 %) | 1.45 (1.21-1.74) | <0.001 |
| Oxygen Administration | 20 038 (8.32 %) | 179 (3.43 %) | 20 217 (8.22 %) | 0.52 (0.44-0.61) | <0.001 |
| Pressure Dressing | 1 236 (0.51 %) | 32 (0.61 %) | 1 268 0.52 %) | 1.40 (0.96-2.03) | 0.082 |
| Spinal Immobilization | 3 800 (1.58 %) | 23 (0.44 %) | 3 823 (1.55 %) | 0.33 (0.22-0.51) | <0.001 |
| Tourniquet Application | 139 (0.06 %) | 1 (0.02 %) | 140 (0.06 %) | 0.49 (0.07-3.58) | 0.483 |
| Ventilator | 143 (0.06 %) | 1 (0.02 %) | 144 (0.06 %) | 1.89 (0.15-23.41) | 0.622 |
| Drugs | |||||
| No Drug Admin | 216 802 (90.06 %) | 4 624 (88.51 %) | 221 426 (90.03 %) | 1.49 (1.10-2.04) | 0.011 |
| Aspirin | 623 (0.26 %) | 3 (0.06 %) | 626 (0.25 %) | 0.62 (0.19-2.05) | 0.436 |
| Beta-2 Stimulants | 8 306 (3.45 %) | 430 (8.23 %) | 8 736 (3.55 %) | 2.30 (1.65-3.21) | < 0.001 |
| Activated Charcoal | 80 (0.03 %) | 4 (0.08 %) | 84 (0.03 %) | 2.92 (1.01-8.46) | 0.048 |
| Salbutamol and Ipratropium Bromide | 293 (0.12 %) | 11 (0.21 %)) | 304 (0.12 %) | 1.61 (0.84-3.10) | 0.152 |
| Corticosteroids | 646 (0.27 %) | 14 (0.27 %) | 660 (0.27 %) | 0.59 (0.33-1.06) | 0.079 |
| Diazepam | 682 (0.28 %) | 2 (0.04 %) | 684 (0.28 %) | 0.43 (0.10-1.78) | 0.245 |
| Glucose | 1 779 (0.74 %) | 93 (1.78 %) | 1 872 (0.76 %) | 4.47 (3.11-6.41) | < 0.001 |
| Ipratropium Bromide | 6292 (2.61 %) | 332 (6.36 %) | 6 624 (2.69 %) | 1.38 (1.12-1.72) | 0.003 |
| Isordil | 304 (0.13 %) | 1 (0.02 %) | 305 (0.12 %) | 0.43 (0.06-3.20) | 0.407 |
| IV Crystalloids | 12 357 (5.13 %) | 94 (1.80 %) | 12 451(5.06 %) | 0.47 (0.36-0.60) | < 0.001 |
| Ketamine | 142 (0.06 %) | 1 (0.02 %) | 143 (0.06 %) | 1.49 (0.18-12.41) | 0.712 |
| Magnesium Sulphate | 261 (0.11 %) | 3 (0.06 %) | 264 (0.11 %) | 0.47 (0.14-1.61) | 0.230 |
| Midazolam | 343 (0.14 %) | 3 (0.06 %) | 346 (0.14 %) | 1.56 (0.45-5.47) | 0.486 |
| Morphine Sulphate | 996 (0.41 %) | 6 (0.11 %) | 1 002 (0.41 %) | 0.81 (0.34-1.95) | 0.645 |
| Oxygen | 222 (0.09 %) | 2 (0.04 %) | 224 (0.09 %) | 0.67 (0.16-2.75) | 0.574 |
| Promethazine | 32 (0.01 %) | 1 (0.02 %) | 33 (0.01 %) | 2.98 (0.39-23.03) | 0.295 |
| Sodium Bicarbonate | 75 (0.03 %) | 5 (0.10 %) | 80 (0.03 %) | 1.47 (0.58-3.70) | 0.418 |
| Other Meds | 1 189 (0.49 %) | 7 (0.13 %) | 1 196 (0.49 %) | 0.59 (0.28-1.27) | 0.177 |
Reference categories used in the model were considered based on its exclusivity. In table 1, P1 and red code is used as the reference category as these indicate the severest variables in order to achieve reliable odds ratios (OR). In table 2, haemorrhage was designated as the reference category based on it being high acuity in a previous study [27]. No treatment and drugs administered was the reference category used denoting exclusivity in these variables. Multicollinearity was assessed using the variance inflation factor (VIF) and plots were inspected for influential observations. All data analysis was performed using Stata 17.0 (StataCorp., Texas, USA).
This study was approved by the Human Research Ethics Committee of the University of Cape Town (HREC Ref 546/2019).
Results
After matching the CAD data to the ePCR data, a final data set of n=245 954 responses were eligible for analysis. Of these patients, 97.88 % (n=240 730) were conveyed to hospital while only 2.12 % (n=5 224) of patients were not. Fig 2 outlines the sampling process and case exclusion. The patients transported and not transported to hospital were further split into P1 and P2 based on dispatch priority in the EMD (CAD Data).
Fig. 2.
Process flow of data
Of all patients transported to hospital, 67.91 % (n=163 483) of cases were dispatched as P2. Of patients not transported to hospital, 43.72 % (n=2 284) were dispatched as P1. Final patient triage indicates that majority of patients attended to by EMS were yellow code (47.38 % (n= 116 528)) while 29.10 % (n=71 581) of patients were triaged green code. The single regression model displayed across Tables 1 and 2 shows the non-clinical and clinical characteristics of the sample and their relation to conveyance of the patient. The tables also show the risk adjusted results from the multivariate logistic regression for both the clinical and non-clinical variables.
In the prediction model, Fig. 1, the area under the receiver operating characteristic curve (ROC) is noted at 0.72 indicating and acceptable diagnostic accuracy of the variables with all VIFs reported <10 indicating no multicollinearity in the model.
Following multivariate regression analysis, notable variables of non-clinical predictors of patients not being transported to hospital (table 1) are: green (OR 4.33 (95 % CI: 3.55–5.28; p<0.01)) or yellow triage (OR 1.95 (95 % CI: 1.60–2.37; p<0.01)).
In table 2, the most common incident types of EMS responses were non-cardiac chest pain (n=49 189; 20.00 %), respiratory complaints (n=32 737; 13.31 %), assault (n=27 853; 11.32 %), obstetrics (n=17 499:7.11 %) and abdominal pain (n=13 320 (5.42 %).
Of all patients that were transported to hospital, 82.69 % (n=199 062) of these patients received no treatment. Conversely, of all patients not transported to hospital, 84.00 % (n=4 388) also did not receive any treatment. Of all patients in the sample that received no drug administration (90.03 % (n=221 426)), almost all (97.9 %; (n=216 802) were transported to hospital.
Following multivariate regression, notable incident types that were predictive of non-transport were electrocutions ((OR 4.55 (95 % CI: 1.36–15.23; p=0.014)), diabetes ((OR 2.78 (95 % CI: 2.10–3.68; p<0.01)), motor vehicle accidents ((OR 1.92 (95 % CI: 1.51–2.43; p<0.01)), unresponsive/unconscious patients ((OR 1.98 (95 % CI: 1.54–2.55; p<0.01)), heart-related problems ((OR 1.80 (95 % CI: 1.23–2.62; p=0.002)), sports injuries ((OR 1.71 (95 % CI: 1.13–2.57; p=0.010)) and respiratory complaints ((OR 1.46 (95 % CI: 1.19–1.80; p<0.001)). Incident type other (OR 2.01 (95 % CI: 1.35–2.99; p=0.001)) includes emergency response to call outs such as aviation incidents, high angle incidents, search and rescue, train and railway incidents.
Substantial treatment predictors for non-transport of patients to hospital were nebulisation ((OR 1.45 (95 % CI: 1.21–1.74; p<0.01)) and administration of glucose (OR 4.47 (95 % CI: 3.11–6.41; p<0.01)).
Discussion
The aim of this study was to determine which variables were predictive of non-conveyance of patients to hospital by EMS, in a cohort of patients from the Western Cape province of South Africa. Following univariate and multivariate regression, we found triage, incident and treatment variables predictive of non-conveyance to hospital.
The rate of non-conveyance of patients to hospital (n=5 224, 2.12 %) in this study is low in comparison to an international systematic review that reported non-conveyance rates of between 3.7 % and 93.7 % globally [28]. The increased conveyance of patients to hospital and overcrowding of Emergency Departments (ED) has been highlighted in a previous study in South Africa recommending the introduction of on scene discharge by EMS in resolving the problem [29].
Previous studies in the same setting have dichotomised green and yellow codes as being lower acuity [25,30]. Most EMS responses in this study were triaged as green and yellow and were predictors of patients not transported to hospital. Over-triage in the EMD is noted as the safer alternative in dispatching resources to emergencies within WCG [22,25]. It is reported by EMD staff and their management in WCG that “if they don't over prioritise, then the patient might die.”[25]. Although 67.66 % of patients were dispatched as P2 or non-emergent, unexpectedly, P1 or emergent dispatch of resources resulted in higher odds of patients being non-conveyed to hospital. This result supports the evidence of over-triage in the EMD and the reason why 82.69 % of all patients transported to hospital received no treatment with 90.06 % of all patients transported receiving no emergency medications. These results might indicate that most patients used EMS as mere transportation to hospital which contributes to high patient numbers in the ED thus placing greater strain on already constrained resources [29]. The introduction of treat and refer guidelines, on scene discharge or alternative transport pathways to a primary healthcare network using dispatch algorithms in such cases is recommended in optimising resource utilisation.
A mixed methods study by Alshehri et al [25] provided evidence of EMD staff choosing to dispatch emergency resources with intentional over-triage to be safe, resulting in ‘misuse’ of EMS resources. Incident types of MVAs and abdominal emergencies were identified as most over-triaged in Alshehri's study [25]. It is reported that MVAs (46.7 %) and abdominal complaints (36.4 %) are the highest trauma and medical cases being discharged from the ED for patients transported by EMS to the hospital in South Africa [29]. Just these two incident types make up 62.4 % of all patients being discharged from the ED. MVAs in this study indicated that the odds of non-conveyance of patients to hospital is OR 1.92 (95 % CI: 1.51-2.43; p<0.01). This result corroborates with the over triage of MVAs in the EMD [31]. It is however reasonable to consider that patients requiring spinal immobilisation must be transported to hospital with OR 0.33 (95 % CI: 0.22-0.51; p<0.01); yet it isn't clear whether there was a true indication for spinal immobilisation.
A government hospital in South Africa has reported 60.4 % of trauma patients coming into the ED via EMS are discharged from hospital [29]. With all the patients being discharged, MVAs make up 46.7 %. These results imply that approximately half of all patients with spinal immobilization transported to the hospital ED will be discharged. Internationally, only 0.71 % of entrapped patients had spinal cord injuries (SCI) which represent the more serious patient in MVAs [32]. Hospital admissions for spinal injuries in the Western Cape however are approximately 185 cases per month taken from a study detailing spinal injuries over a period of 11 years [33]. For MVAs, spinal immobilisation is not absolute because the rate of SCI is low and therefore require guidelines to support safe identification of those with SCI and that "might" benefit from movement minimisation. Following from this, and to minimise unnecessary transport and ED crowding, there is also a need for on-scene discharge guidelines in MVAs to avoid risk.
Despite abdominal emergencies being over-triaged [25,31], these patients have higher odds of being transported to hospital by EMS. The conveyance of these patients may be out of concern as it is noted that abdominal complaints is a major descriptor of potential sepsis [34]. A Delphi study conducted among EMS experts in South Africa [27] had indicated that these incidents (MVAs and abdominal emergencies) may be classified as low acuity specifically at dispatch level using defined descriptors. These descriptors can be used in the development of dispatch algorithms to reduce unnecessary dispatch of EMS to cases of low acuity or contribute to the development of time critical response protocols for incident types like abdominal emergencies. This is exactly the type of supportive tools highlighted in the global systematic review to improve the non-conveyance of patients to hospital [28].
The Delphi study [27] also indicated that any form of respiratory distress cannot be deemed as low acuity at dispatch level, however the results of this study indicate contrary. Respiratory complaints are the highest incident type of patients not transported (21.11 %) with odds of 46 % non-conveyance to hospital. These types of cases would typically be categorised as “P1” in the EMD and therefore warrants a lights and sirens response [25]. Over triage of respiratory complaints in the EMD is known to be 58.21 % [31] however, South Africa is facing a problem of growing rates of asthma (18.5 per 100 000) ranking in the top five globally for mortality rates [35,36]. Making the situation worse is that there is a lack of appropriate diagnosis, treatment, and access to medical care for these patients, [36] hence leaving the patient no alternative but to initiate an EMS response. South Africa also ranks among the top thirty Tuberculosis burdened countries (500 per 100 000) [37] with one of highest prevalence of Chronic Obstructive Pulmonary Disease (COPD) in the world [38]. Burden of disease data indicate that Tuberculosis is a leading cause of natural death in South Africa with 23.8 % of all deaths taking place at home. [39] Such high rates of serious respiratory disease make it difficult for the EMD not to initiate an emergency response and therefore supports the argument of dispatching emergency resources with intentional over-triage to improve patient safety [25].
Given the high prevalence of asthma, it is interesting to note that on-scene nebulisation was predictive of non-transport. This may indicate a role of EMS providers to treat and discharge patients with acute asthma exacerbation with onward referral to further management, especially after hours. Conversely, oxygen administration was not predictive of non-transport, which may be explained by oxygen administration as standard practice for all critically ill or injured patients, especially those presenting with respiratory distress.[32]
Similar to respiratory complaints, experts in South Africa have also indicated that chest pain cannot be regarded as low acuity in the EMD [27]; however, our results indicate that 35 % of chest pain patients are not being transported to hospital after receiving an emergency response. Chest pain has also been highlighted as incidents with high rates of deliberate over triage, thus contributing to the non-conveyance of patients to hospital [25]. Emergency calls in the EMD for acute myocardial infarctions, although found to have a consistent set of descriptors that is used by callers [40], requires further evidence in telephonic recognition and development of appropriate dispatch algorithms.
The administration of glucose in this study shows 347 % odds of not being transported to hospital. This may indicate that EMS provide treatment for hypoglycaemia, whereafter patients refuse or do not require transport. Similarly, the incident type “Diabetes” was also predictive of non-transport in this study. Hospitals in the Western Cape have a high prevalence of diabetic emergencies, of which 64 % are brought in by EMS [41]. More than half (51 %) of patients presenting with diabetic emergencies return to the ED presenting with a diabetic emergency within 6 months of discharge [41]. EMS is confronted with similar figures where more than half of patients treated and discharged on scene for hypoglycaemia reactivating EMS within 7 days [42]. These high rates of presentation, discharge, and re-presentation within the emergency service exposes gaps in screening and prevention, patient education, adequate discharge instructions, and follow-up or referral to primary care. Fig. 2
Variables that is predictive of non-conveyance pf patients to hospital have been highlighted. The development of guidelines to support on-scene discharge and referral within the broader healthcare system may prove beneficial [36]. Further resolutions based on international recommendations include additional training and implementation of supportive tools such as non-conveyance guidelines in improving the rate of non-conveyance of patients to hospital [28]. Such mechanisms are required in South Africa not only within ambulance operations but in the EMD as well.
Limitations
The data are extracted from the WCG and may not be externally valid. This study should therefore be repeated in other settings across the country. It is possible that instances where patients were not transported had a higher likelihood of an ePCR not being completed. This may result in a falsely lowered prevalence of non-conveyance also affecting the variables that were found to be predictive. Only 2.12 % of the total data used in this study were patients that were non-conveyed to hospital. Despite this being a small proportion of the entire data set, 82.69 % of the patients that were transported to hospital have indicated no treatment which may influence the non-transportation of patients to hospital. Lastly, no assessments were made as to whether non-conveyance or lack of emergency interventions in this cohort were appropriate, justified, or safe. Unfortunately, follow ups with these patients were not possible due to resource constraints, the high number of patients and patient confidentiality, therefore, patient outcomes could not be measured. Future research should take these factors into consideration to enhance the current body of knowledge.
Conclusion
In one of the first and largest retrospective studies completed in Africa, this study provided variables that were predictive of ambulance non-conveyance. Further analysis and investigation into this predictive model together with established descriptors of low acuity will provide key evidence into the development of dispatch algorithms that reduce over-triage of patients, development of on scene discharge protocols as well as treat and refer guidelines in EMS.
Dissemination of results
The results of this study is shared with the WCG as this is where the data was sourced. This study is also part of a PhD project at the University of Cape Town where the results will be included into the original thesis.
Authors’ contribution
Authors contributed as follow to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: FB contributed 45 %, AH 20 %, WS 20 % and LW 15 %. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Declaration of Competing Interest
At the time of peer review, Dr Willem Stassen and Prof Lee Wallis were editors of the African Journal of Emergency Medicine. Both Dr Stassen and Prof Wallis were not involved in the editorial workflow for this manuscript. The African Journal of Emergency Medicine applies a double blinded process for all manuscript peer reviews. The authors declared no further conflict of interest.
References
- 1.Snooks H, Kearsley N, Dale J, Halter M, Redhead J, Cheung WY. Towards primary care for non-serious 999 callers: results of a controlled study of “‘Treat and Refer’” protocols for ambulance crews. Qual Saf Health Care. 2004;13:435–443. doi: 10.1136/qshc.2003.007658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dami F, Golay C, Pasquier M, Fuchs V, Carron PN, Hugli O. Prehospital triage accuracy in a criteria based dispatch centre. BMC Emerg Med. 2015;15:32. doi: 10.1186/s12873-015-0058-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Palumbo L, Kubincanek J, Emerman C, Jouriles N, Cydulka R, Shade B. Performance of a system to determine EMS dispatch priorities. Am J Emerg Med. 1996;14:388–390. doi: 10.1016/S0735-6757(96)90056-X. [DOI] [PubMed] [Google Scholar]
- 4.Alpert A, Morganti KG, Margolis GS, Wasserman J, Kellermann AL. Giving EMS flexibility in transporting low-acuity patients could generate substantial medicare savings. Health Aff. 2013;32:2142–2148. doi: 10.1377/hlthaff.2013.0741. [DOI] [PubMed] [Google Scholar]
- 5.Overtriage | definition of overtriage by Medical dictionary n.d. https://medical-dictionary.thefreedictionary.com/overtriage (accessed August 12, 2023).
- 6.Khorram-Manesh A, Montán KL, Hedelin A, Kihlgren M, Örtenwall P. Prehospital triage, discrepancy in priority-setting between emergency medical dispatch centre and ambulance crews. Eur J Trauma Emerg Surg. 2011;37:73–78. doi: 10.1007/s00068-010-0022-0. [DOI] [PubMed] [Google Scholar]
- 7.Lu TC, Chen YT, Ko PCI, Lin CH, Shih FY, Yen ZS, et al. The demand for prehospital advanced life support and the appropriateness of dispatch in Taipei. Resuscitation. 2006;71:171–179. doi: 10.1016/j.resuscitation.2006.03.016. [DOI] [PubMed] [Google Scholar]
- 8.Neely KW, Eldurkar JA, Drake MER. Do emergency medical services dispatch nature and severity codes agree with paramedic field findings? Acad Emerg Med. 2000;7:174–180. doi: 10.1111/j.1553-2712.2000.tb00523.x. [DOI] [PubMed] [Google Scholar]
- 9.Feldman MJ, Verbeek PR, Lyons DG, Chad SJ, Craig AM, Schwartz B. Comparison of the medical priority dispatch system to an out-of-hospital patient acuity score. Acad Emerg Med. 2006;13:954–960. doi: 10.1197/j.aem.2006.04.018. [DOI] [PubMed] [Google Scholar]
- 10.Hoikka M, Länkimäki S, Silfvast T, Ala-Kokko TI. Medical priority dispatch codes-comparison with national early warning score. Scand J Trauma Resusc Emerg Med. 2016;24:142. doi: 10.1186/s13049-016-0336-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sofianopoulos S, Williams B, Archer F, Thompson B. The exploration of physical fatigue, sleep and depression in paramedics: a pilot study. J Emerg Primary Health Care. 2011;9:1–33. doi: 10.1017/CBO9781107415324.004. [DOI] [Google Scholar]
- 12.Newgard CD, Fischer PE, Gestring M, Michaels HN, Jurkovich GJ, Lerner EB, et al. National Guideline for the Field Triage of Injured Patients: Recommendations of the National Expert Panel on Field Triage, 2021. ItraumaOrg n.d. https://doi.org/10.1097/TA.0000000000003627. [DOI] [PMC free article] [PubMed]
- 13.Newton PR. AN EVALUATION OF THE APPROPRIATENESS OF EMERGENCY MEDICAL SERVICE (EMS) RESPONSES IN THE ETHEKWINI HEALTH DISTRICT OF KWAZULU - NATAL. 2014. [DOI] [PubMed]
- 14.Alshehri MF, Pigoga JL, Wallis LA. Dispatcher triage accuracy in the western cape government emergency medical services system, Cape Town, South Africa. Prehosp Disaster Med. 2020;35:638–644. doi: 10.1017/S1049023X20001041. [DOI] [PubMed] [Google Scholar]
- 15.Annual Reports - KZN Department of Health n.d. http://www.kznhealth.gov.za/reports.htm (accessed July 9, 2020).
- 16.Graphic of the day: Where are South Africa's ambulances? – Bhekisisa n.d. https://bhekisisa.org/article/2018-12-19-00-graphic-of-the-day-where-are-south-africas-ambulances/(accessed June 15, 2020).
- 17.Western Cape Emergency Medical Services-Improving emergency response times and patient services through innovative communications and a mobility solution. 2016.
- 18.WC ambulance service ‘stretched’ n.d. https://ewn.co.za/2014/07/02/Ambulance-services-severely-stretched (accessed August 31, 2019).
- 19.Department of Health and Wellness - Annual Reports: 2019 | Western Cape Government n.d. https://www.westerncape.gov.za/dept/health/documents/annual_reports/2019 (accessed August 12, 2023).
- 20.Western Cape | province, South Africa | Britannica.com n.d.
- 21.Department of Statistics South Africa. Mid-year population estimates P0302 2000. 2019.
- 22.Gleby F. Ambulance in Red Zones in Cape Town, South Africa: Waiting time for patients when ambulance requires armed escort 2018.
- 23.Department of Health: Western Cape Government. Annual Report 2021_2022 2022.
- 24.Statistics South Africa. Statistics South Africa. The Fieldworker 2016;2:People-Labour market. https://doi.org/10.1787/aeo-2012-53-en.
- 25.Alshehri MF, Pigoga JL, Wallis LA. A mixed methods investigation of emergency communications centre triage in the government emergency medical services system, Cape Town, South Africa. Afr J Emerg Med. 2020;10:S12–S17. doi: 10.1016/j.afjem.2020.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gottschalk SB, Wood D, Devries S, Wallis LA, Bruijns S. The cape triage score: A new triage system South Africa. Proposal from the cape triage group. Emerg Med J. 2006;23 doi: 10.1136/emj.2005.028332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Binks F, Wallis LA, Stassen W. The development of consensus-based descriptors for low-acuity emergency medical services cases for the South African setting. Prehosp Disaster Med. 2021:1–8. doi: 10.1017/S1049023X21000169. [DOI] [PubMed] [Google Scholar]
- 28.Ebben RHA, Vloet LCM, Speijers RF, Tönjes NW, Loef J, Pelgrim T, et al. A patient-safety and professional perspective on non-conveyance in ambulance care: a systematic review. Scand J Trauma Resusc Emerg Med. 2017;25:1–20. doi: 10.1186/S13049-017-0409-6/TABLES/4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goldstein LN, Sibanyoni S, Vincent-Lambert C. On-scene discharge by emergency care practitioners – a viable option for South Africa? S Afr J Pre-Hospital Emerg Care. 2020;1:3–8. doi: 10.24213/1-1-3330. [DOI] [Google Scholar]
- 30.Pettke A, Stassen W, Laflamme L, Wallis LA, Hasselberg M. Changes in trauma-related emergency medical services during the COVID-19 lockdown in the Western Cape, South Africa. BMC Emerg Med. 2023;23:1–9. doi: 10.1186/S12873-023-00840-8/TABLES/3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mcalpine D, Hodkinson P, Fleming J. “The rates of pre-hospital over-triage and the reasons behind them in a Cape Town setting” 2021.
- 32.Nutbeam T, Fenwick R, Smith J, Bouamra O, Wallis L, Stassen W. A comparison of the demographics, injury patterns and outcome data for patients injured in motor vehicle collisions who are trapped compared to those patients who are not trapped. Scand J Trauma Resusc Emerg Med. 2021;29:1–7. doi: 10.1186/S13049-020-00818-6/TABLES/4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sothmann J, Stander J, Kruger N, Dunn R. Epidemiology of acute spinal cord injuries in the Groote Schuur hospital acute spinal cord injury (GSH ASCI) unit, Cape Town, South Africa, over the past 11 years. S Afr Med J. 2015;105 doi: 10.7196/SAMJnew.8072. [DOI] [PubMed] [Google Scholar]
- 34.Stassen W, Larsson E, Wood C, Kurland L. Telephonic description of sepsis among callers to an emergency dispatch centre in South Africa. Afr J Emerg Med. 2020 doi: 10.1016/j.afjem.2020.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gray CL, Levin ME, Zar HJ, Potter PC, Khumalo NP, Volkwyn L, et al. Food allergy in South African children with atopic dermatitis. Pediatr Allergy Immunol. 2014;25 doi: 10.1111/pai.12270. [DOI] [PubMed] [Google Scholar]
- 36.Masekela R, Gray CL, Green RJ, Manjra AI, Kritzinger FE, Levin M, et al. The increasing burden of asthma in South African children: a call to action. S Afr Med J. 2018;108 doi: 10.7196/SAMJ.2018.v108i7.13162. [DOI] [Google Scholar]
- 37.Global Tuberculosis Report 2022 n.d. https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2022 (accessed October 30, 2022).
- 38.Blanco I, Diego I, … PB-E, 2019 undefined. Geographic distribution of COPD prevalence in the world displayed by Geographic Information System maps. Eur Respiratory Soc n.d. https://doi.org/10.1183/13993003.00610-2019. [DOI] [PubMed]
- 39.Department of Statistics South Africa. P0309.3 - Mortality and causes of death in South Africa: Findings from death notification, 2018. 2021.
- 40.Buma C, Saunders C, Watermeyer J, Stassen W. An analysis of the descriptors of acute myocardial infarction used by South Africans when calling for an ambulance from a private emergency call centre. Afr J Emerg Med. 2020 doi: 10.1016/j.afjem.2020.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lotter N, Lahri S, van Hoving DJ. The burden of diabetic emergencies on the resuscitation area of a district-level public hospital in Cape Town. Afr J Emerg Med. 2021;11:416–421. doi: 10.1016/J.AFJEM.2021.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ridhaa Booley M, Welzel T. A cross-sectional analysis of the short-term outcomes of patients receiving prehospital treatment for symptomatic hypoglycaemia in Cape Town. Afr J Emerg Med. 2015;5:159–164. doi: 10.1016/J.AFJEM.2015.03.003. [DOI] [Google Scholar]