Abstract
Background
This study aimed to access the radiologic and clinical outcomes after arthroscopic reduction and internal fixation with screws in patients with posterior wall fractures of the acetabulum.
Methods
From May 2013 to December 2019, 13 patients (11 men and 2 women) with posterior wall fractures of the acetabulum were treated with arthroscopic reduction and internal fixation with screws at two medical centers. The mean age at the index operation was 39 years (range, 22–58 years). The mean duration of follow-up was 23 months (range, 12–46 months). Clinical assessment was performed using the modified Merle d'Aubigné and Postel functional scoring system. The maximum displacement of acetabular or femoral head fragments detected on radiographs was used as radiographic results. Secondary osteoarthritis, osteonecrosis, or heterotrophic ossification was assessed at the latest follow-up.
Results
Bony union was shown at 12 weeks of follow-up in all patients. The radiologic outcomes showed an anatomical reduction in 11 patients and a satisfactory reduction in 2 patients. The modified Merle d'Aubigné and Postel functional score was excellent in 7 patients, good in 5 patients, and fair in 1 patient. Two patients had transient pudendal nerve palsy after hip arthroscopy. However, no sciatic nerve palsy occurred. At the latest follow-up, there was no heterotopic ossification, osteonecrosis of the femoral head, or posttraumatic osteoarthritis.
Conclusions
Arthroscopic reduction and internal fixation with cannulated screws can be good alternative options with good radiographic and clinical outcomes, convenient removal of intra-articular loose body, and low complication rates.
Keywords: Arthroscopic reduction, Arthroscopic internal fixation, Acetabular posterior wall fracture, Hip arthroscopy
Acetabular posterior wall fractures are well known as the most common type among acetabular fractures and account for approximately one-quarter to one-third of acetabular fractures.1,2) Traditionally, the first option for treatment of acetabular posterior wall fracture is open reduction and internal fixation with pelvic reconstruction plates or in combination with implants such as spring plates.
Recently, arthroscopic reduction and internal fixations in intra-articular fractures are becoming popular due to successful results.3,4,5,6) Although several studies have reported the use of arthroscopic treatment for traumatic fractures of the hip joint,4,7,8) a case report showed that direct arthroscopic reduction and internal fixation were done on two young patients with a posterior wall or anterior column fracture of the acetabulum.5) Arthroscopic reduction and fixation for posterior wall fractures of the acetabulum have advantages including direct visualization of intra-articular fractures, accurate fracture reduction, repair of labral tears, management of ligamentum teres ruptures, joint lavage, and removal of loose fragments.
However, screw only fixations for posterior wall fractures of the acetabulum might not be as stable as plate and screw fixations. In addition, existing arthroscopic screw fixation devices were not enough to fix the fracture fragments of the acetabular posterior wall. Therefore, based on previous studies, we designed a retrospective study and reviewed patients with acetabular posterior wall fractures with intra-articular loose bodies. We developed fixation devices and adapted them as reduction guides for direct fracture fragments and flexible guides for flexible anchors.
The purpose of this study was to evaluate the radiologic and clinical results after arthroscopic reduction and fixation using screws in patients with posterior wall fractures of the acetabulum. We hypothesized that arthroscopic reduction and internal fixation for posterior wall fractures of the acetabulum with or without combined fractures would allow accurate, stable fracture reduction with minimal dissection and satisfactory clinical outcomes.
METHODS
This retrospective study was approved by the Institutional Review Board of Chungnam National University Hospital (No. CNUH 2018-08-008) and the requirement of written informed consent was waived.
From May 2013 to December 2019, 13 patients with posterior wall fractures of the acetabulum were treated with arthroscopic reduction and internal fixation using cannulated screws at two medical centers. Indications for operative treatment include a single fracture with an intra-articular displacement of more than 2 mm,9) the presence of intra-articular bony fragments, and/or marginal impaction injury. However, large fragments involving the acetabular dome, severely comminuted fractures, combined fractures, and increased risk of extravasation of the retroperitoneal area were excluded.
Preoperative assessments included a detailed physical examination of the sensorimotor function of the limb and vascular status in terms of dorsalis pedis and posterior tibialis artery pulses. For radiologic assessment, an anteroposterior view and two Judet 45° oblique views of the pelvis were obtained. Computed tomography (CT) scan of the pelvis with three-dimensional reconstruction was also done in the initial imaging assessment to obtain a more accurate diagnosis of the fracture. Posterior wall fractures of the acetabulum were classified into three types: a type I fracture is characterized by a single fracture line separating a single bone fragment from the remaining part of the posterior wall, a type II fracture involves several fragments of the posterior wall, and a type III fracture is a type I or type II fracture that is associated with a sunk cancellous area in the acetabular wall medial to the fracture line but is not affected by it because of the shear impact of the femoral head at the time of dislocation.10,11) Patients with combined femoral head fractures were classified by Pipkin.12) Arthroscopic treatment was performed as soon as the patient’s general medical condition permitted.
Surgical Techniques
Under general anesthesia, the patient was placed in the supine position using a specialized hip arthroscopic table with the injured lower extremity in traction and the opposite limb in 40° to 45° abduction. A C-arm image intensifier was used to provide an anteroposterior view of the fracture site. Appropriate traction was applied to the injured lower extremity to provide enough distraction forced by 10 to 12 mm at the hip joint. First, an anterolateral portal under fluoroscopic guidance as a viewing portal was made, and then 2 other portals (posterolateral and anterior) were made additionally. The fractured fragment of the posterior wall of the acetabulum was visualized after hematoma evacuation and displaced posteriorly. Using a straight or curved guide for the flexible all-suture anchor (Fig. 1), the fractured fragment was reduced into the intact acetabular side using long (more than 35 cm) 0.45-inch Kirschner-wires (K-wires) via the anterolateral and posterolateral portals, and the reduced fractured fragment was temporarily fixed by K-wires.
Fig. 1. Straight and curved guides for suture anchors and a long guide wire for cannulated screws.

After anatomical reduction of the fracture site was archived by arthroscopy, we used 4.0-mm-diameter or 5.0-mm-diameter cannulated titanium screws to secure the fragment under direct arthroscopic visualization (Fig. 2, Supplementary Video 1).
Fig. 2. (A) Judet 45° oblique radiograph of the pelvis in patient 5 showing a posterior wall fracture and a femoral head fracture (Pipkin type IV) of the right hip joint. (B) Anatomical reduction of the intra-articular fracture gap was confirmed by arthroscopy. (C) Postoperative pelvis in the anteroposterior view showing anatomic reduction of a displaced posterior wall fracture at 24 months of follow-up.
Rehabilitation
Postoperative protocols of rehabilitation were started as soon as the patient’s conditions permitted. For 6 to 8 weeks after the index surgery, patients were encouraged to walk with toe touch weight-bearing with the aid of two crutches. Subsequent progression to full weight-bearing was individualized for each patient.
Clinical and Radiologic Evaluation
Follow-up visitations were scheduled at 4 weeks, 2 months, 3 months, 6 months, 1 year, and annually thereafter. Patients who did not regularly return for their visiting schedules were contacted by telephone interview. Clinical and radiologic outcomes were evaluated during these follow-up visits. Two nurses and one doctor were assigned and visited non-responders. Clinical result was evaluated using the modified Merle d’Aubigne and Postel functional scoring system.13) The modified Merle d’Aubigne and Postel functional scoring system assigns a maximum score of 6 points to pain, gait, and range of motion. The scores are then summed up to obtain an overall clinical score and classified into excellent (18 points), very good (17 points), good (15 or 16 points), fair (13 or 14 points), or poor (< 13 points).
Postoperatively, three standard pelvic radiographic views and CT scans were done to evaluate the reduction status of the fracture fragments. The maximum displacement seen at any of the normal radiographic lines of the acetabulum or the femoral head was used to grade the reduction based on three categories: anatomical (0–1 mm), satisfactory (2–3 mm), or poor (more than 3 mm).13) All radiologic evaluations were performed by a single radiologist (STK) and two board-certified orthopedic surgeons (YCH and JMH) to enhance objectivity.
Complications
Final follow-up radiographs were graded according to Matta’s radiologic criteria, which showed arthritic changes in the hip joint. Evaluation of osteonecrosis of the femoral head or heterotrophic ossification14) was performed using these follow-up radiographs.
RESULTS
All 13 patients (11 men and 2 women) were diagnosed with simple posterior wall fractures of the acetabulum. Nine patients had dislocations. Of these patients, 5 were combined with head fractures and 6 patients had a loose body. The mean age of the patients was 39 years (range, 22–58 years). The time from injury to operation was an average of 5 days (range, 2–10 days). The mean follow-up period was 23 months (range, 12–46 months) (Table 1).
Table 1. Thirteen Patients with Acetabular Posterior Wall Fractures.
| Patient No. | Age (yr) | Sex | Side | Cause of injury | Combined injury | Time to surgery (day) | Surgical treatment | Clinical outcome* | Radiological outcome | Follow-up (mo) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 55 | Man | Left | TA | Dislocation, loose body | 4 | Fixation | Excellent (18) | Anatomical | 36 |
| 2 | 50 | Man | Left | TA | Dislocation, head fracture | 7 | Fixation | Good (15) | Anatomical | 36 |
| 3 | 22 | Man | Left | Fall | Dislocation, loose body | 2 | Fixation | Good (16) | Satisfactory | 36 |
| 4 | 57 | Man | Right | TA | Head fracture | 3 | Fixation | Fair (14) | Anatomical | 24 |
| 5 | 25 | Woman | Right | TA | Dislocation, head fracture | 4 | Fixation | Excellent (18) | Anatomical | 46 |
| 6 | 25 | Man | Right | TA | Head fracture | 4 | Excision, fixation | Good (16) | Anatomical | 24 |
| 7 | 57 | Man | Left | TA | Dislocation, head fracture | 3 | Excision, fixation | Good (16) | Anatomical | 18 |
| 8 | 58 | Man | Left | TA | Dislocation, loose body | 10 | Fixation | Excellent (18) | Satisfactory | 14 |
| 9 | 37 | Man | Left | TA | Dislocation, loose body | 7 | Fixation | Excellent (18) | Anatomical | 12 |
| 10 | 32 | Man | Right | Fall | Dislocation, loose body | 4 | Fixation | Good (16) | Anatomical | 18 |
| 11 | 28 | Woman | Right | TA | Dislocation, loose body | 3 | Fixation | Excellent (18) | Anatomical | 12 |
| 12 | 34 | Man | Left | Sports | Loose body | 8 | Fixation | Excellent (18) | Anatomical | 16 |
| 13 | 28 | Man | Right | Sports | Dislocation, loose body | 5 | Fixation | Excellent (18) | Anatomical | 12 |
TA: traffic accident, Excision: excision of fractured femoral head.
*Clinical outcome using modified Merle d’Aubigne scoring system.
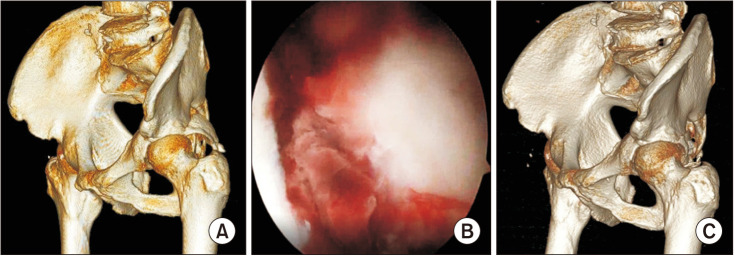
The mean operation time was 110 minutes (range, 80–145 minutes). During the operation, intra-articular loose bodies were removed and the posterior wall fractures were fixed using cannulated titanium screws (Fig. 3).
Fig. 3. (A) Preoperative three-dimensional (3D) reconstructed computed tomography in patient 8 showing a displaced fracture of the acetabular posterior wall on the right hip joint. (B) Satisfactory reduction of the intra-articular fracture gap was confirmed by arthroscopy. (C) Postoperative 3D reconstructed computed tomography showing fixation of the reduced fracture fragments using two cannulated screws.
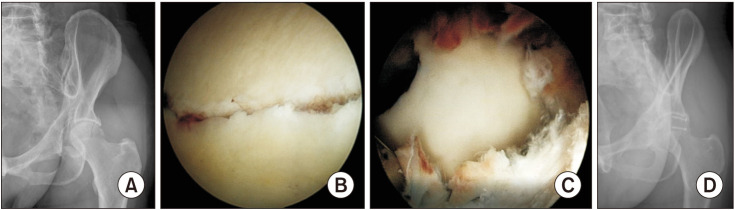
Out of the 5 patients who had combined fractures of the femoral head (Pipkins type IV), 3 patients underwent removal of small freely mobile loose bodies and the main fractured fragment of the femoral head remained without fixation because of minimal displacement and well containment after internal fixation of the posterior wall fracture. However, 2 of the patients with fractures of the femoral head had the fractured fragments of the femoral head removed because the fragments were inside out and irreducible with the possibility of interrupting motion (Fig. 4).
Fig. 4. (A) Judet 45° oblique radiograph of the pelvis in patient 7 showing a posterior wall fracture and an inside out femoral head fracture (Pipkin type IV) of the left hip joint. (B) Anatomical reduction of the intra-articular fracture gap was confirmed by arthroscopy. (C) During the reduction procedures, the cartilage of the fractured femoral head was damaged and irreducible because of the fractured femoral head fragments; hence, it was removed. (D) Postoperative pelvis in the anteroposterior view showing anatomic reduction of a displaced posterior wall fracture at 18 months follow-up.
The radiologic results showed anatomical reduction status in 11 patients and satisfactory reduction status in 2 patients using the criteria of Matta13) by postoperative CT and/or postoperative radiography. Union was achieved at 12 weeks of follow-up in all patients. The modified Merle d’Aubigne and Postel functional score13) was excellent in 7 patients, good in 5 of the other patients, and fair in 1 patient.
Two patients had transient pudendal nerve palsy after hip arthroscopy. However, no sciatic nerve palsy occurred. There was no heterotopic ossification, osteonecrosis of the femoral head, or posttraumatic osteoarthritis at the latest follow-up.
DISCUSSION
Although open reduction and internal fixation methods are considered for posterior wall fractures of the acetabulum, 13 patients with posterior wall single fractures in this study had complete healing after arthroscopic reduction and internal fixation using cannulated screws at the mean 23 months of follow-up. This study suggests that arthroscopic reduction and internal fixations using screws to treat acetabular posterior wall single fractures is a possible alternative treatment option.
According to the advancing hip arthroscopic technique, arthroscopy-assisted fracture fixations around the hip joint have been possible since the last decade. Although indications for hip arthroscopy after an acetabular posterior wall fracture have not yet been clearly defined, we consider that the ideal indication of arthroscopic fixation in patients with acetabular posterior wall fractures is single fragment (about 30% of posterior wall) with intra-articular loose body. Traditional open reduction and internal fixation requires extensive exposure, which may be complicated by infection, blood loss, wound healing problems, muscle weakness, sciatic nerve palsy, and heterotopic ossification.15) There is also the problem of intra-articular perforation of hardware.15,16) However, the hip arthroscopic technique has fewer complications than the open reduction technique described above and has the additional advantage of less invasive approach, joint washing, confirmation of reduction, and faster postoperative recovery.17)
Matsuda4) was the first to report the use of hip arthroscopic reduction and screw fixation in patients with femoral head fractures. Kim et al.5) also reported successful outcomes in patients with acetabular posterior wall fractures using hip arthroscopic reduction and screw fixation of acetabular fractures. Park et al.15) reported two successful cases of arthroscopic reduction and transportal screw fixation of acetabular posterior wall fractures using the curved guide of Jugger Knot (1.4 mm and 1.5 mm, curved reusable guide; Biomet Inc., Warsaw, IN, USA) for maintaining reduced fragments and being used as fixating guide wires. This technique was similar to ours. In the current study, the fractured fragment was reduced at the intact acetabulum and was fixed by long (more than 35 cm) K-wires via a straight or curved guide for flexible All-Suture anchors. A conventional cannulated screw guide for the fixation of reduced fracture fragments is short in length, which is not enough for obese patients and needs to be improved. This technique has two advantages. First, the straight or curved guide is helpful in maintaining the reduced fragments and stabilizing the fractured fragments using cannulated screws. Second, the curved guide is more suitable to use in curved acetabular shapes and makes it possible to use standard portals, such as anterolateral and posterolateral portals, which minimizes additional incisions for cannulated screws.
Generally, clinical and radiologic outcomes in patients with acetabular posterior wall fractures are related to several factors such as older age,18) the status of the femoral head,19) intra-articular impaction of fracture fragments,20) the quality of reduction,21,22) and the associated injuries.23) In this study, all 13 patients were completely healed without major complications. The reason for these results might be related to the accuracy of anatomical reduction.21,22) Matta13) reported poorer outcomes in patients with more than 3 mm of displacement as compared to anatomical reduction. In addition, the indication for arthroscopic surgery in patients with acetabular posterior wall fractures is a single fragment without severe comminution. Therefore, simple comparisons between studies have inevitable limitations due to different patient conditions and fracture types.
In this study, 5 patients had femoral head fractures (Pipkin type IV) and 2 patients had femoral head fractures that should be removed because the fractured fragments of the femoral head were inside out (Fig. 4). During the reduction procedures, the cartilage of the fractured femoral head was damaged; hence, it was removed. Kekatpure et al.8) reported successful arthroscopic reduction and internal fixation of Pipkin type I femoral head fractures. Although the removal of fractured fragments of the femoral head in this study had similar clinical and radiologic outcomes at the latest follow-up, long-term follow-up is still mandatory.
This study has several limitations. First, this study is retrospective in design. Therefore, it might be inevitable to have selection bias for arthroscopic surgery. Second, the sample size was small. The indications for arthroscopic surgery in patients with acetabular posterior wall fractures are relatively rare. In the two centers, only 13 patients were available for the 6-year study period. Third, the cannulated screw has relatively weak fixation power compared to the conventional screw and plate. Therefore, this is a main causal factor of narrow surgical indications of acetabular posterior wall fractures. Finally, an agreement for academic use of information such as the type of treatment might be mandatory to obtain patient’s consent. We acquired agreement regarding arthroscopic treatment during preoperative consultation with the patients.
In conclusion, arthroscopic reduction and internal fixation with cannulated screws in patients with posterior wall single fractures of the acetabulum can be a good alternative option because of good radiologic and clinical outcomes, easy intra-articular loose body removal, and low complication rates.
ACKNOWLEDGEMENTS
The authors would like to thank Dr. Soon-Tae Kwon, MD, Department of Radiology, Chungnam National University Hospital, for performing the radiologic evaluations.
Footnotes
CONFLICT OF INTEREST: Yong-Chan Ha is an editorial board member of the journal but was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
SUPPLEMENTARY MATERIAL
Supplementary material is available in the electronic version of this paper at the CiOS website, www.ecios.org
References
- 1.Moed BR, Kregor PJ, Reilly MC, Stover MD, Vrahas MS. Current management of posterior wall fractures of the acetabulum. Instr Course Lect. 2015;64:139–159. [PubMed] [Google Scholar]
- 2.Baumgaertner MR. Fractures of the posterior wall of the acetabulum. J Am Acad Orthop Surg. 1999;7(1):54–65. doi: 10.5435/00124635-199901000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Del Pinal F. Technical tips for (dry) arthroscopic reduction and internal fixation of distal radius fractures. J Hand Surg Am. 2011;36(10):1694–1705. doi: 10.1016/j.jhsa.2011.07.021. [DOI] [PubMed] [Google Scholar]
- 4.Matsuda DK. A rare fracture, an even rarer treatment: the arthroscopic reduction and internal fixation of an isolated femoral head fracture. Arthroscopy. 2009;25(4):408–412. doi: 10.1016/j.arthro.2009.01.011. [DOI] [PubMed] [Google Scholar]
- 5.Kim H, Baek JH, Park SM, Ha YC. Arthroscopic reduction and internal fixation of acetabular fractures. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):867–870. doi: 10.1007/s00167-013-2799-y. [DOI] [PubMed] [Google Scholar]
- 6.Atesok K, Doral MN, Whipple T, et al. Arthroscopy-assisted fracture fixation. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):320–329. doi: 10.1007/s00167-010-1298-7. [DOI] [PubMed] [Google Scholar]
- 7.Park MS, Yoon SJ, Choi SM. Arthroscopic reduction and internal fixation of femoral head fractures. J Orthop Trauma. 2014;28(7):e164–e168. doi: 10.1097/BOT.0000000000000048. [DOI] [PubMed] [Google Scholar]
- 8.Kekatpure A, Ahn T, Lee SJ, Jeong MY, Chang JS, Yoon PW. Arthroscopic reduction and internal fixation for pipkin type I femoral head fracture: technical note. Arthrosc Tech. 2016;5(5):e997–e1000. doi: 10.1016/j.eats.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. Preliminary report. J Bone Joint Surg Am. 1964;46:1615–1646. [PubMed] [Google Scholar]
- 10.Letournel E. Acetabulum fractures: classification and management. Clin Orthop Relat Res. 1980;(151):81–106. [PubMed] [Google Scholar]
- 11.Pascarella R, Cerbasi S, Politano R, et al. Surgical results and factors influencing outcome in patients with posterior wall acetabular fracture. Injury. 2017;48(8):1819–1824. doi: 10.1016/j.injury.2017.05.039. [DOI] [PubMed] [Google Scholar]
- 12.Pipkin G. Treatment of grade IV fracture-dislocation of the hip. J Bone Joint Surg Am. 1957;39(5):1027–1197. [PubMed] [Google Scholar]
- 13.Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78(11):1632–1645. [PubMed] [Google Scholar]
- 14.Brooker AF, Bowerman JW, Robinson RA, Riley LH., Jr Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55(8):1629–1632. [PubMed] [Google Scholar]
- 15.Park JY, Chung WC, Kim CK, Huh SH, Kim SJ, Jung BH. Arthroscopic reduction and transportal screw fixation of acetabular posterior wall fracture: technical note. Hip Pelvis. 2016;28(2):120–126. doi: 10.5371/hp.2016.28.2.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jang JH, Moon NH, Park KY. Arthroscopic management of intraarticular screw perforation after surgical treatment of an acetabular posterior wall fracture: a case report. Hip Pelvis. 2018;30(1):60–64. doi: 10.5371/hp.2018.30.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vale J, Diniz S, Leite PS, Soares D. Surgical treatment of acetabular posterior wall fracture with hip arthroscopy: a case report. Hip Pelvis. 2022;34(1):62–67. doi: 10.5371/hp.2022.34.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moed BR, WillsonCarr SE, Watson JT. Results of operative treatment of fractures of the posterior wall of the acetabulum. J Bone Joint Surg Am. 2002;84(5):752–758. doi: 10.2106/00004623-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 19.Zha GC, Sun JY, Dong SJ. Predictors of clinical outcomes after surgical treatment of displaced acetabular fractures in the elderly. J Orthop Res. 2013;31(4):588–595. doi: 10.1002/jor.22279. [DOI] [PubMed] [Google Scholar]
- 20.de Palma L, Santucci A, Verdenelli A, Bugatti MG, Meco L, Marinelli M. Outcome of unstable isolated fractures of the posterior acetabular wall associated with hip dislocation. Eur J Orthop Surg Traumatol. 2014;24(3):341–346. doi: 10.1007/s00590-013-1200-7. [DOI] [PubMed] [Google Scholar]
- 21.Pantazopoulos T, Nicolopoulos CS, Babis GC, Theodoropoulos T. Surgical treatment of acetabular posterior wall fractures. Injury. 1993;24(5):319–323. doi: 10.1016/0020-1383(93)90055-b. [DOI] [PubMed] [Google Scholar]
- 22.Giannoudis PV, Grotz MR, Papakostidis C, Dinopoulos H. Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Joint Surg Br. 2005;87(1):2–9. [PubMed] [Google Scholar]
- 23.Magu NK, Gogna P, Singh A, et al. Long term results after surgical management of posterior wall acetabular fractures. J Orthop Traumatol. 2014;15(3):173–179. doi: 10.1007/s10195-014-0297-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.