Abstract
Background
There is no consensus established on postoperative rehabilitation after medial meniscus posterior root tear (MMPRT) repair, including when and how physicians can apply range of motion (ROM) exercise, weight-bearing (WB), brace use, and return to sports (RTS). The purpose of this study was to systematically review the literature on postoperative rehabilitation characteristics of MMPRT repair regarding ROM, WB, brace use, and RTS.
Methods
A literature search was performed using the Medline/PubMed, Cochrane Central Register of Controlled Trials, and Embase databases. The inclusion criteria were English language, human clinical studies, and studies describing rehabilitation protocols after MMPRT repair such as ROM, WB, brace use, and RTS. Abstracts, case reports, cohort studies, controlled laboratory studies, human cadaveric or animal studies, systematic reviews, and meta-analyses were excluded.
Results
Thirteen studies were included. Of the 12 ROM studies, ROM was started immediately within 1 or 2 days after operation in 6 studies and after 2 to 3 weeks of knee immobilization in the rest. Of the 13 WB studies, partial weight-bearing was initiated 1 to 4 weeks after operation in 8 studies and 6 weeks in the rest. Of the 9 brace studies, patients were immobilized by a splint for 2 weeks in 3 studies, and in the rest, a brace with full extension was applied for 3 to 6 weeks after several days of splint application. Of the 7 RTS studies, RTS was allowed at 6 months in 6 studies and 5 to 7 months in 1 study.
Conclusions
This systematic review revealed conservative rehabilitation protocols were more widely adapted as ROM and WB were restricted at certain degrees during postoperative periods in most protocols analyzed. However, it is impossible to identify a consensus on rehabilitation protocols as the protocols analyzed in this review were distinct each other and heterogeneous. In the future, a well-designed comparative study among different rehabilitation protocols is essential to establish a consensus.
Keywords: Medial meniscus, Rehabilitation, Systematic review, Tibial meniscus tear
The interest in medial meniscus posterior root tears (MMPRTs) has been growing. MMPRTs, which are defined as radial tears or avulsion injuries on bony attachments,1,2,3) result in decreased contact surface and increased peak pressure through a loss of hoop tension due to circumferential fiber disruption.4,5,6) MMPRTs can result in complications after total meniscectomy, with pathologic loads leading to degenerative arthritis. Recently, there has been an increasing interest in encouraging results of MMPRT repair accumulated over the last decade. MMPRT repair restores the hoop tension of the medial meniscus and its ability to dissipate forces, which can slow the progression of arthritis in most cases.7,8) Meta-analyses and systematic reviews reported that MMPRT repair showed satisfactory clinical and radiologic outcomes.9)
There is no consensus on MMPRT repair procedures in terms of the optimal surgical techniques, type of suture configurations, and stitch methods. Likewise, no agreement has been reached on postoperative rehabilitation, including when and how physicians can apply range of motion (ROM) exercise, weight-bearing (WB), brace use, and return to sports (RTS) periods. So far, no comprehensive systemic literature review has been conducted on postoperative rehabilitation after MMPRT repair. The purpose of this study was to systematically review literatures on the postoperative rehabilitation protocols after MMPRT repair regarding ROM, WB, brace use, and RTS and to determine whether the conservative or accelerated protocols are more widely adopted in MMPRT repair protocols.
METHODS
Search Strategy and Study Selection
Articles published until March 2021 were searched in Medline/PubMed, the Cochrane Central Register of Controlled Trials, and Embase databases. Each search was performed using “meniscal or meniscus” AND “root” AND “repair or fixation or refixation” as keywords. Articles were classified by applying the following inclusion criteria: (1) human clinical studies, (2) MMPRTs studies, (3) studies describing at least two of the following: ROM, WB, brace, and RTS, (4) studies showing significant clinical or functional improvement after surgery, (5) studies providing all original data, and (6) studies with levels of evidence from I to IV.10) The exclusion criteria were as follow: (1) treatment of lesions that expanded to the lateral or anterior meniscus, (2) combined concomitant multiple ligament injuries, (3) articles showing outcomes with less than a minimum of 24-month follow-up, (4) biomechanics, (5) radiological reports, (6) letters to the editor, (7) review articles, and (8) case reports. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline was followed in this systematic review.11) No other restrictions were applied, including language restrictions. All results were searched to select relevant articles.
Data Extraction
The titles and abstracts of all studies identified from the initial search were manually screened independently by two authors (JSK and MYC). The full text of all studies that passed the manual screening was further evaluated for eligibility by the two authors mentioned above and reviewed by the primary investigator (DHK). The first author reviewed the references of all selected articles to ensure that no relevant studies were overlooked in the initial search. The primary investigator gathered data used in the current study: first author, publication year, the number of participants, ROM, WB, brace use, RTS, suture material (ethibond, polydioxanone, Fiberwire, and Ultrabraid), repair technique (pullout repair or suture anchor repair). Protocols for each type of rehabilitation instructions were classified as follows: (1) ROM by the starting point and target angle increase by period, (2) WB by period and WB intensity (non-weight-bearing [NWB], toe-touch weight-bearing [TTWB], partial weight-bearing [PWB], and full weight-bearing [FWB]), (3) a brace by period of use and angle change, and (4) RTS by the starting point. The quality of all studies included was independently evaluated by two authors (MYC and JSK) using the Coleman methodology score.12) The study was exempted the Institutional Review Board approval by Inje University Seoul Paik Hospital (No. PAIK 2020-10-006).
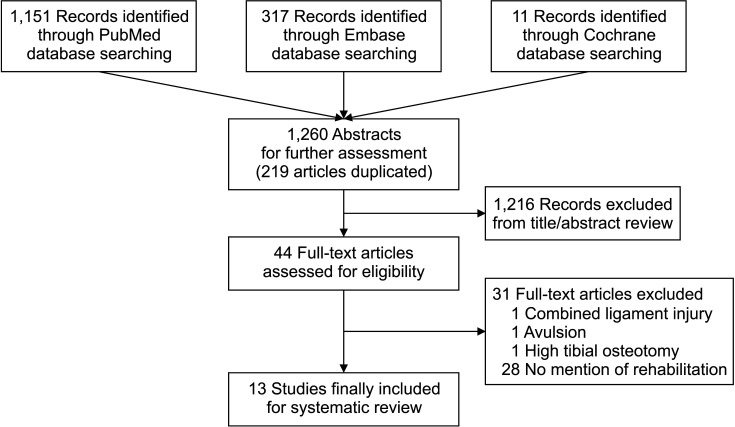
RESULTS
We identified 1,260 articles in the Medline/PubMed, Cochrane Central Register of Controlled Trials, and Embase database. Among 1,260 articles, 44 articles passed the initial screening and were further reviewed according to the inclusion criteria. As a result, a total of 13 studies were included for this systematic review (Fig. 1). Among the 13 studies, ROM was used in 12 studies, WB in 13 studies, a brace in 9 studies, and RTS in 7 studies.
Fig. 1. Flowchart of search strategy used for study identification and inclusion.
The characteristics of surgical techniques are shown in Table 1.7,13,14,15,16,17,18,19,20,21,22,23,24) Regarding surgical techniques, transtibial pullout repair was done in 9 studies and suture anchor repair was done in 3 studies. One study compared transtibial pullout repair and suture anchor repair. No.1 polydioxanone suture (PDS) was used in 6 studies, and No.1 PDS in combination with No.2 ethibond, 2-0 Fiberwire, and No.2 Ultrabraid was used in 1 study each. The mean score of quality assessment using the Coleman methodology score tool in all studies was 60.7 ± 8.11 (maximum, 100 points; range, 48–81 points).12) The following three categories had the lowest scores: (1) study size, (2) type of study, and (3) procedure for assessing outcome.
Table 1. General Characteristics of Included Studies.
| Study | Study design (level of evidence) | No. of patients | ROM | WB | Brace | RTS | Functional score |
|---|---|---|---|---|---|---|---|
| Chung et al. (2018)14) | Retrospective uncontrolled case series (IV) | 91 | Yes | Yes | Yes | - | Lysholm score |
| Chung et al. (2015)7) | Retrospective comparative study (III) | 57 | - | Yes | Yes | Yes | Lysholm score, IKDC subjective score |
| Lee et al. (2018)20) | Case series (IV) | 56 | Yes | Yes | Yes | Yes | Lysholm score, IKDC subjective score, HSS score |
| Lee et al. (2009)22) | Therapeutic case series (IV) | 20 | Yes | Yes | Yes | - | Lysholm score, HSS score |
| Kim et al. (2011)23) | Prospective therapeutic comparative study (III) | 45 | Yes | Yes | Yes | Yes | Lysholm score, IKDC subjective score, HSS score |
| Seo et al. (2011)21) | Case series (IV) | 21 | Yes | Yes | Yes | Yes | Lysholm score, HSS score |
| LaPrade et al. (2017)15) | Cohort study (III) | 31 | Yes | Yes | Yes | Yes | Lysholm score, WOMAC, SF-12, Tegner activity score |
| Jung et al. (2012)16) | Case series (IV) | 13 | Yes | Yes | - | - | Lysholm score, Tegner activity score |
| Kim et al. (2011)17) | Retrospective comparative study (III) | 30 | Yes | Yes | - | - | Lysholm score, IKDC subjective score |
| Lee et al. (2014)18) | Retrospective comparative study (III) | 25 | Yes | Yes | - | Yes | Lysholm score, IKDC subjective score, Tegner activity score |
| Furumatsu et al. (2019)19) | Retrospective comparative study (III) | 20 | Yes | Yes | - | - | KOOS, Lysholm score, IKDC subjective score, Tegner activity score |
| Kim et al. (2019)24) | Retrospective comparative study (III) | 45 | Yes | Yes | Yes | Yes | Lysholm score, IKDC subjective score, |
| Dragoo et al. (2020)13) | Cohort study (II) | 30 | Yes | Yes | Yes | - | KOOS, Lysholm score, Tegner activity score, VR-12 |
ROM: range of motion, WB: weight-bearing, RTS: return to sports, IKDC: International Knee Documentation Committee, HSS: Hospital for Special Surgery, WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index, SF-12: 12-Item Short Form Survey, KOOS: Knee injury and Osteoarthritis Outcome Score, VR-12: Veterans RAND 12-Item Health Survey.
Range of Motion
There were 12 studies that included ROM exercises in rehabilitation protocols (Table 2).13,14,15,16,17,18,19,20,21,22,23,24) ROM exercise protocols were very diverse in terms of the starting point of ROM exercise, exercise period, and angle limitation according to the period. In 6 studies, it was started immediately within 1 or 2 days after operation,13,14,15,16,17,18) whereas 5 studies and 1 study suggested immobilization of the knee for 2 weeks19,20,21,22,23) and 3 weeks, respectively.24) Four studies recommended ROM exercise without ROM restriction to a specific degree of flexion,14,16,17,18) whereas 8 studies suggested ROM restriction based on the period.13,15,19,20,21,22,23,24)
Table 2. Results of ROM.
| Sub group | Study | Study design (level of evidence) | No. of patients | Suture | Surgical technique | ROM | Permitted ROM | |
|---|---|---|---|---|---|---|---|---|
| 90° | 130° | |||||||
| 1 | Chung et al. (2018)14) | Retrospective uncontrolled case series (IV) | 91 | No.1 PDS | Pullout repair | Progressive knee ROM exercises, using a CPM machine and isometric exercises, were initiated 2 days postoperatively. | - | - |
| 2 | Lee et al. (2018)20) | Case series (IV) | 56 | No.2 PDS | Pullout repair | Their knees were immobilized in fully extended cylinder leg splints for 2 weeks. ROM exercises were then initiated from 0° to 60° with a hinged brace and the patients increased their knee flexion by 15° per week. | 6 wk | - |
| 3 | Lee et al. (2009)22) | Therapeutic case series (IV) | 20 | No.5 Ethibond | Pullout repair | A long cylinder leg cast was applied for 2 weeks in a fully extended position. Passive motion after the first 2 weeks and active motion up to 90° after the first 4 weeks. Increased flexion by 10° a week until 8 weeks to allow an ROM of 130°. | 4 wk | 8 wk |
| 4-1 | Kim et al. (2011)23) | Prospective therapeutic comparative study (III) | 45 | No.0 PDS | Suture anchor repair | A long cylinder leg cast was applied in the fully extended position for 2 weeks. Flexion of the knee was allowed to 30° for the next 2 weeks. Increased flexion of the knee by 15° per week until 6 weeks to allow ROM of 90°. | 6 wk | - |
| 4-2 | Kim et al. (2011)23) | Prospective therapeutic comparative study (III) | 45 | No.2 Ethibond | Pullout repair | - | ||
| 5 | Seo et al. (2011)21) | Case series (IV) | 21 | No.1 PDS or No.2 Ethibond | Pullout repair | The knees were immobilized in a full extension brace for 2 weeks. ROM exercises were then gradually initiated to increase the knee flexion angle by 15° to 30° per week to achieve 90° of knee flexion within 6 weeks. | 6 wk | - |
| 6 | LaPrade et al. (2017)15) | Cohort study (III) | 31 | 2-0 Fiberwire | Pullout repair | On postoperative day 1, passive knee ROM exercises from 0° to 90° Increased ROM was allowed as tolerated 2 weeks postoperatively. | 2 wk | - |
| 7 | Jung et al. (2012)16) | Case series (IV) | 13 | No.1 PDS | Suture anchor repair | Active motion exercises were encouraged from 0 °to 120 °of flexion. | - | - |
| 8 | Kim et al. (2011)17) | Retrospective comparative study (III) | 30 | No.1 PDS | Pullout repair | Knee ROM exercises with a CPM machine began the day after surgery. | - | - |
| 9-1 | Lee et al. (2014)18) | Retrospective comparative study (III) | 25 | Mason-allen: No.1 PDS | Pullout repair | Knee ROM exercises using a CPM machine were initiated the day after surgery. | - | - |
| 9-2 | Lee et al. (2014)18) | Retrospective comparative study (III) | 25 | Simple stich: | Pullout repair | - | ||
| 10 | Furumatsu et al. (2019)19) | Retrospective comparative study (III) | 20 | No.2 Ultrabraid | Pullout repair | Use of knee immobilizer for 2 weeks. Between 2 and 4 weeks, knee flexion exercise was gradually increased up to 90°. Five or 6 weeks postoperatively, patients were allowed 120° of knee flexion. | 4 wk | 6 wk |
| 11 | Kim et al. (2019)24) | Retrospective comparative study (III) | 45 | No.1 PDS | Pullout repair | The knee joint was immobilized for 3 weeks. ROM was performed 3 weeks postoperatively. At 6 weeks, 0° to 90° flexion was allowed. At 12 weeks, 0° to 120° flexion was allowed. | 6 wk | 12 wk |
| 12 | Dragoo et al. (2020)13) | Cohort study (II) | 30 | - | Suture anchor repair | ROM from 0° to 90° of flexion was allowed for 6 weeks. ROM from 0° to 110° of flexion was allowed from weeks 6 to 12. | 6 wk | 12 wk |
ROM: range of motion, PDS: polydioxanone, CPM: continuous passive motion.
Weight-Bearing
There were 13 studies that included WB (Table 3).4,7,13,15,16,17,18,19,20,21,22,23,24) The starting period and methods of WB varied. Among the 13 studies, 2 studies had low-level PWB started 1 day after surgery with a gradual increase of WB intensity until 6 weeks,17,18) and PWB was started at postoperative 2 weeks, 4 weeks, and 6 weeks in remaining 2 studies,19,21) 1 study,20) and 6 studies,13,15,16,22,23,24) respectively. Regarding FWB, it was allowed at 6 weeks and 8 weeks postoperatively in 7 studies7,14,17,18,19,21,24) and 4 studies,16,20,22,23) respectively. One study suggested that PWB should be started after 6 weeks of the NWB period and gradually increased to FWB until there is no pain or swelling.15) Another study suggested TTWB should be initiated at postoperative 2 weeks and WB intensity should be gradually increased to 50% until postoperative 4 weeks.21)
Table 3. Results of WB.
| Sup group | Study | Study design (level of evidence) | No. of patients | Suture | Surgical technique | WB | Starting period | ||
|---|---|---|---|---|---|---|---|---|---|
| TTWB | PWB | FWB | |||||||
| 1 | Chung et al.(2018)14) | Retrospective uncontrolled case series (IV) | 91 | No.1 PDS | Pullout repair | TTWB, the use of crutches for 3 weeks postoperatively. FWB at 6 weeks postoperatively | Immediately | 4 wk | 6 wk |
| 2 | Chung et al.(2015)7) | Retrospective comparative study (III) | 57 | No.1 PDS | Pullout repair | PWB exercise (i.e., toe touching and use of crutches) was carried out for 6 weeks postoperatively with the brace locked in full extension of the knee joint for the initial 3 weeks postoperatively. FWB was allowed at least 6 weeks after surgery. | Immediately | Immediately | 6 wk |
| 3 | Lee et al.(2018)20) | Case series (IV) | 56 | No.2 PDS | Pullout repair | PWB was allowed at 4 weeks postoperatively and FWB at 8 weeks postoperatively. | - | 4 wk | 8 wk |
| 4 | Lee et al. (2009)22) | Therapeutic case series (IV) | 20 | No.5 Ethibond | Pullout repair | PWB was allowed at 6 weeks postoperatively, followed by FWB at 8 weeks. | - | 6 wk | 8 wk |
| 5-1 | Kim et al. (2011)23) | Prospective therapeutic comparative study (III) | 45 | No.0 PDS | Suture anchor repair | PWB was allowed at 6 weeks postoperatively, followed by FWB at 8 weeks. | - | 6 wk | 8 wk |
| 5-2 | Kim et al.(2011)23) | Prospective therapeutic comparative study (III) | 45 | No.2 Ethibond | Pullout repair | - | - | - | - |
| 6 | Seo et al.(2011)21) | Case series (IV) | 21 | No.1 PDS or No.2 Ethibond | Pullout repair | Only TTWB during the first 2 weeks after the procedure and it was slowly advanced to bear 50% of body weight at 4 weeks and FWB at 6 weeks. | 2 wk | 4 wk | 6 wk |
| 7 | LaPrade et al. (2017)15) | Cohort study (III) | 31 | 2-0 Fiberwire | Pullout repair | NWB in a straight leg brace for the first 6 weeks after surgery. PWB began at week 7 and gradually increased to FWB as tolerated without pain or swelling. | - | 7 wk | Without pain or swelling |
| 8 | Jung et al.(2012)16) | Case series (IV) | 13 | No.1 PDS | Suture anchor repair | TTWB for 6 weeks was allowed without a knee immobilizer. After 6 weeks, WB progressed for 2 weeks, and FWB was permitted at 8 weeks. | Immediately | 6 wk | 8 wk |
| 9 | Kim et al.(2011)17) | Retrospective comparative study (III) | 30 | No.1 PDS | Pullout repair | PWB with the aid of crutches was continued for 6 weeks postoperatively. | - | Immediately | 6 wk |
| 10-1 | Lee et al.(2014)18) | Retrospective comparative study (III) | 25 | Mason-Allen: No.1 PDS | Pullout repair (Mason-Allen stitch) | PWB allowing toe touch using a crutch was continued for 6 weeks postoperatively. FWB was allowed at a minimum of 6 weeks after surgery. | Immediately | Immediately | 6 wk |
| 10-2 | Lee et al.(2014)18) | Retrospective comparative study (III) | 25 | Simple stich: No.1 PDS | Pullout repair (simple stitch) | - | - | - | - |
| 11 | Furumatsu et al. (2019)19) | Retrospective comparative study (III) | 20 | No.2 Ultrabraid | Pullout repair | NWB in the knee immobilizer for 2 weeks. Between 2 and 4 weeks, knee flexion exercise was gradually increased up to 90° under PWB condition. At 5 or 6 weeks postoperatively, patients were allowed FWB. | - | 2 wk | 5 or 6 wk |
| 12 | Kim et al. (2019)24) | Retrospective comparative study (III) | 45 | No.1 PDS | Pullout repair | TTWB with the use of a crutch was allowed for 6 weeks postoperatively. FWB was allowed 6 weeks postoperatively. | Immediately | Immediately | 6 wk |
| 13 | Dragoo et al. (2020)13) | Cohort study (II) | 30 | - | Suture anchor repair | TTWB for 4 days was followed for 6 weeks. ROM from 0° to 110° of flexion was allowed from weeks 6 to 12 along with non-restricted weight-bearing. | 4 day | 6 wk | 6 to 12 wk |
WB: weight-bearing, TTWB: toe-touch weight-bearing, PWB: partial weight-bearing, FWB: full weight-bearing, PDS: polydioxanone, NWB: non-weight-bearing, ROM: range of motion.
Brace
There were 9 studies that included brace protocols (Table 4). There were differences in the timing of brace wear, range of brace angle, and timing of brace removal. Three studies reported that the knee joint was immobilized by a splint for 2 weeks and then it was replaced with a brace.20,22,23) Three studies reported changing from a splint to a brace within several days and wearing a brace in full extension for 3 weeks.7,14,24) In 2 studies, although ROM exercise was performed immediately after surgery, the brace was fixed in full extension for 6 weeks in TTWB or NWB.13,15) Two studies reported that the brace angle must be adjusted according to the change of the knee flexion degree by ROM exercise.14,22) Chung et al.14) recommended that the brace should be removed by 6 weeks after surgery and his study was the only one referring to the timing of brace removal.
Table 4. Results of Brace Use.
| Sup group | Study | Study design (level of evidence) | No. of patients | Suture | Surgical technique | Brace |
|---|---|---|---|---|---|---|
| 1 | Chung et al. (2018)14) | Retrospective uncontrolled case series (IV) | 91 | No.1 PDS | Pullout repair | A knee brace locked in extension was required for 3 weeks postoperatively. The motion allowed within the brace was progressively increased starting at 3 weeks. Discontinued at 6 weeks. |
| 2 | Chung et al. (2015)7) | Retrospective comparative study (III) | 57 | No.1 PDS | Pullout repair | The brace locked in full extension of the knee joint for the initial 3 weeks postoperatively. |
| 3 | Lee et al. (2018)20) | Case series (IV) | 56 | No.2 PDS | Pullout repair | The knees were immobilized in fully extended cylinder leg splints for 2 weeks. ROM exercises were then initiated from 0° to 60° with a hinged brace and the patients increased their knee flexion by 15° per week. |
| 4 | Lee et al. (2009)22) | Therapeutic case series (IV) | 20 | No.5 Ethibond | Pullout repair | A limited motion brace was subsequently applied to control motion. |
| 5-1 | Kim et al. (2011)23) | Prospective therapeutic comparative study (III) | 45 | No.0 PDS | Suture anchor repair | At 2 weeks postoperatively, a hinged postoperative brace was applied. |
| 5-2 | Kim et al. (2011)23) | Prospective therapeutic comparative study (III) | 45 | No 2 Ethibond | Pullout repair | - |
| 6 | Seo et al. (2011)21) | Case series (IV) | 21 | No.1 PDS or No.2 Ethibond | Pullout repair | Immobilized in a full extension brace for 2 weeks. |
| 7 | LaPrade et al. (2017)15) | Cohort study (III) | 31 | 2-0 Fiberwire | Pullout repair | Patients maintained NWB in a straight leg brace for the first 6 weeks after surgery. |
| 8 | Kim et al. (2019)24) | Retrospective comparative study (III) | 45 | No.1 PDS | Pullout repair | The knee joint was immobilized with a hinged brace locked in full extension for 3 weeks postoperatively. |
| 9 | Dragoo et al. (2020)13) | Cohort study (II) | 30 | - | Suture anchor repair | Brace use was followed by the leg locked in full extension for 6 weeks. |
PDS: polydioxanone, ROM: range of motion, NWB: non-weight-bearing.
Return to Sports
There were 7 studies referring to the timing of RTS (Table 5). Six studies suggested RTS should be allowed at postoperative 6 months7,18,20,21,23,24) and 1 study at postoperative 5 to 7 months.15) Some studies commented on the period of light running including RTS, and 3 studies reported that light running was allowed 3 months after surgery.7,18,23) Regarding when allowing full flexion or squat, 2 studies recommended 3 months after surgery16,21) and 2 studies recommended 6 months after surgery.22,23)
Table 5. Result of RTS.
| Sup group | Study | Study design (level of evidence) | No. of patients | Suture | Surgical technique | RTS |
|---|---|---|---|---|---|---|
| 1 | Chung et al. (2015)7) | Retrospective comparative study (III) | 57 | No.1 PDS | Pullout repair | Light running at 3 months; RTS at 6 months |
| 2 | Lee et al. (2018)20) | Case series (IV) | 56 | No.2 PDS | Pullout repair | RTS activity was permitted 6 months postoperatively. |
| 3-1 | Kim et al. (2011)23) | Prospective therapeutic comparative study (III) | 45 | No.0 PDS | Suture anchor repair | Further flexion, squatting, and RTS were allowed 6 months postoperatively. |
| 3-2 | Kim et al. (2011)23) | Prospective therapeutic comparative study (III) | 45 | No.2 Ethibond | Pullout repair | - |
| 4 | Seo et al. (2011)21) | Case series (IV) | 21 | No.1 PDS or No. 2 Ethibond | Pullout repair | Squatting and deep flexion were prohibited for at least 3 months. Return to previous sporting activities was permitted 6 months postoperatively. |
| 5 | LaPrade et al. (2017)15) | Cohort study (III) | 31 | 2-0 Fiberwire | Pullout repair | Normal activities with an average return to full activities at 5 to 7 months postoperatively. |
| 6-1 | Lee et al. (2014)18) | Retrospective comparative study (III) | 25 | Mason-Allen: No.1 PDS | Pullout repair (Mason-Allen stitch) | Light running was allowed at 3 months, and RTS was allowed at 6 months, although strenuous contact sports were prohibited. |
| 6-2 | Lee et al. (2014)18) | Retrospective comparative study (III) | 25 | Simple stich: No.1 PDS | Pullout repair (simple stitch) | - |
| 7 | Kim et al. (2019)24) | Retrospective comparative study (III) | 45 | No.1 PDS | Pullout repair | RTS was allowed at 6 months postoperaively. |
RTS: return to sports, PDS: polydioxanone.
DISCUSSION
The primary conclusions of this systematic review are as follows: (1) There are various rehabilitation protocols after MMPRT repair regarding ROM exercise, WB, brace use, and RTS. There was no study comparing clinical outcomes depending on the rehabilitation method, so it was difficult to suggest which protocol was superior and to identify a consensus on rehabilitation protocols. (2) Regarding the initiation of ROM exercise, half of the included studies suggested 1 or 2 days after surgery, whereas remaining studies recommended limited ROM exercise until about 2 or 3 weeks after surgery. (3) Two studies suggested starting careful PWB on postoperative day 1 and gradually increasing WB intensity by 6 weeks after surgery, whereas other studies recommended TTWB or NWB until 2 to 6 weeks after operation. (4) Most studies (9 of 13) suggested using a knee brace without comments on the timing of weaning from a brace. (5) About half of the studies (7 of 13) suggested allowing RTS at 5 or 6 months after surgery.
To our knowledge, there are few systemic reviews summarizing trends of rehabilitation protocols after meniscus root repair, unlike the general meniscus repair. The healing mechanism of meniscus root repair and general meniscus repair is different (root repair: bone to meniscus healing between bone bed and meniscus proper; meniscus repair: soft-tissue healing within meniscus proper). It is still debatable whether a complete healing can be achieved after root repair. A few studies reported complete healing with good tension would not be achieved after root repair from second-look arthroscopy,21,24) whereas complete and partial healing rates of simple meniscus repair were 74% and 10%, respectively, from second-look arthroscopy.25) Accelerated rehabilitation can have a negative effect on healing process after root repair, thus surgeons should be careful when applying rehabilitation after root repair. However, it was difficult to identify a consensus on rehabilitation protocols after root repair as there was little research comparing clinical outcomes of different rehabilitation methods. Thus, there is a need to investigate which protocol (conservative or accelerated) is more widely adopted although the rehabilitation protocol described in this study would be based on surgeons’ experiences and preferences. This systematic study reviewed and summarized rehabilitation protocols specifically with regard to ROM exercise, WB, brace use, and RTS after root repair.
Definition of accelerated or conservative rehabilitation protocol was based on a previous study26) that investigated outcomes with a free or a restricted rehabilitation regimen after isolated meniscus repair. According to Lind’s study,26) the free rehabilitation group (accelerated rehabilitation) was allowed ROM 0°–90° immediately while maintaining touch WB for 2 weeks, and WB as tolerated thereafter. The restricted rehabilitation (conservative protocol) group wore a hinged brace for 6 weeks and ROM was progressively increased to 90° for 6 weeks (0°–30° for 2 weeks, 0°–60° for 4 weeks). Touch WB was recommended for 4 weeks, and WB as tolerated thereafter. Thus, the accelerated rehabilitation group with early ROM and weight-bearing was regarded as the free rehabilitation group, whereas the conservative rehabilitation group with delayed ROM and weight-bearing was regarded as the restricted rehabilitation group.
Physicians would be particularly interested in early phase rehabilitation protocols; when to initiate ROM exercise and WB and how to progress according to timeline. ROM exercise can reduce the risk of scar tissue adhesions and restriction of joint mobility.27,28,29,30,31) There is also evidence that early passive ROM exercise does not cause knee damage.32) However, early ROM exercise and WB can cause damage on suture-meniscal tissue and bone-to-meniscus interface, which can result in unfavorable meniscal healing and loosening of fixation.
Among the 12 included studies, 6 studies maintained immobilization in full extension for 2–3 weeks. Restriction of ROM to 90° was applied for 6 weeks in 5 studies, for 4 weeks in 2 studies, and for 2 weeks in 1 study. Restriction of ROM to 130° was used for 12 weeks in 2 studies, for 8 weeks in 1 study, and for 6 weeks in 1 study. ROM protocols were very heterogeneous between studies included in this review and half of them restricted ROM in the early postoperative periods; thus, some surgeons appeared to be cautious about starting ROM exercises.
The concerns over potential harmful effect of immediate ROM exercise on the clinical outcome and fixation of torn roots have not been clearly substantiated with evidence from comparative studies.33) In an early phase, however, it is necessary to consider that minimal exercise is more desirable than lots of movement after operation to reduce excessive pressure on the meniscus and prevent meniscal extrusion after root repair.27)
WB is another important issue in rehabilitation after root repair. Early WB interferes with meniscus healing by damaging the meniscus and applying intolerable load to a fixed root after repair, which may cause meniscus extrusion. There are as divergent opinions about the WB period as ROM. WB can cause damage on suture-meniscal tissue and bone-to-meniscus interface, which can result in unfavorable meniscal healing and meniscal extrusion.27) However, excessive delays in WB can have a negative effect on the clinical outcome as some studies have confirmed that hoop stresses associated with WB actually facilitate meniscal healing in general meniscus repair.34)
In the current study, PWB was performed for 4–6 weeks after surgery in most of the included studies, and FWB was allowed at 6–8 weeks after surgery. Although ROM protocols were very heterogeneous between studies included in this review, most of them restricted WB a few weeks after surgery; thus, most surgeons were cautious about allowing WB. This means that most surgeons agree that excessive WB can cause excessive force and shear conditions interfering with the healing of meniscus repair site35) and protective and conservative WB protocols in the early phase can be helpful to achieve more favorable meniscal healing and extrusion.4) It was difficult to conclude what kind of WB protocol was superior in promoting recovery from MMPRTs due to the diversity of WB protocols, but in most studies, FWB was recommended 6 weeks postoperatively.7,14,17,18,19,21,24)
Most studies recommended wearing a brace for 4–6 weeks after surgery, although there were differences in the timing of brace wear, range of brace angle, and timing of brace removal. Some studies recommended using a splint for 2 weeks after surgery and then switch to a brace.20,22,23) Several studies recommended wearing a brace for 2 to 3 weeks in full extension immediately after surgery.7,14,20,21,24) Then, the brace angle was increased by 15° per week or adjusted to the same angle as the knee flexion degree.20)
The reason for wearing a brace is to prevent overloading the knee or to make it safer.36) In particular, a brace is essential to avoid pivoting imposed by the meniscus.37) However, if the period of brace use is long, muscle weakness will be accompanied.36) Therefore, it is important to take off the brace at appropriate timing as an extended use of a brace may interfere with recovery. The duration of brace use depends on the meniscus tear pattern. Wearing a brace for longitudinal tears allows PWB for 3 weeks and complex and radial tears for 6 to 8 weeks.38) Since root tears are similar to radial tears, a similar principle can be applied to both root tears and radial tears. Consequently, wearing a brace can be helpful during a rehabilitation period for protection.
Most studies reported that RTS can usually be allowed at postoperative 6 months. However, most MMPRTs are degenerative tears, which occur mostly in middle aged patients. Thus, in MMPRTs, returning to pre-activity levels is more important than RTS. Regarding functional rehabilitation protocol, the included studies recommended starting light running at 3 months after surgery7,18,23) and deep knee flexion and squatting at 3 to 6 months after surgery.21,23) Lee et al.18) recommended allowing light running at 3 months after surgery and RTS at 6 months after surgery, while prohibiting strenuous contact sports. Consequently, physicians can recommend functional rehabilitation following time schedule and according to patients’ condition.
Besides, many factors during rehabilitation will affect the healing of the meniscus root and meniscal extrusion, either positively or negatively. Early rehabilitation programs prevent muscle weakness and joint stiffness, whereas delayed rehabilitation programs prevent high compression, shear applications, and damage to the meniscus.38) As there are strengths and weaknesses of each program, physicians are responsible to identify and manage factors that can affect the recovery of a repaired meniscus.
There are several limitations in this study. First, this systematic review was based on studies with relatively low levels of evidence. Most studies included in this review were based on retrospective case series, which have limited clinical significance. However, this study conducted quality assessment using the Coleman methodology score.12) The quality of the studies analyzed in this review was overall quite high with an average Coleman methodology score of 60.7 ± 8.11. Quartile Coleman methodology score distribution was as follows: (1) first quartile (≥ 66), (2) second quartile (60–65), (3) third quartile (51–59), and (4) fourth quartile (≤ 50). Retrospective studies have traditionally received equal importance as prospective studies in scientific journals. Coleman’s score heavily penalizes retrospective studies by providing no score for its retrospective nature and hence the maximum score a retrospective study can obtain is only 65. Therefore, the authors believe the quality of the studies included in our systematic review is overall adequate. Second, it was impossible to conduct a study that compares clinical outcomes including clinical scores, progression of arthrosis, meniscal healing, and meniscus extrusion among distinct rehabilitation protocols since studies included in this review were retrospective case series, not comparative studies between distinct rehabilitation protocols, and other clinical parameters including participants, suture materials, surgical techniques, and follow-up periods were distinct among studies included. Comparing clinical outcomes among studies with different parameters would lead to a biased and inaccurate conclusion. Third, the current study included two surgical techniques (pullout repair and suture anchor repair), whereas studies using a meniscal fixator for side-to-side repair were not included. However, it would not be a serious problem because the main purpose of this study was to systematically review the literature on the postoperative rehabilitation protocols after MMPRT repair, not to compare clinical outcomes of the two surgical techniques. In the future, a well-organized comparative study among different rehabilitation protocols with a long-term follow-up and a larger sample size is required to properly evaluate the effects of each rehabilitation protocol after MMPRT repair. Fourth, it was impossible to conclude what kind of rehabilitation protocol was superior regarding ROM, WB, brace use, and RTS. In this systematic review, no discrete consensus on rehabilitation protocols after root repair could be found due to the heterogeneous nature of the data included in this study. However, it should be considered that the clinical relevance of this systematic review is to understand the trend of rehabilitation after root repair.
This systematic review showed that there are various rehabilitation protocols after MMPRT repair regarding ROM exercise, WB, brace use, and RTS. According to the results of the current study, conservative rehabilitation protocols would be more widely accepted because most included studies had restricted ROM and WB according to postoperative periods. However, it was impossible to identify a consensus on rehabilitation protocols as the protocols analyzed in this review were distinct each other and heterogeneous. In the future, a well-organized comparative study on different rehabilitation protocols with a large volume is essential to reach a consensus on rehabilitation protocols.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Smigielski R, Becker R, Zdanowicz U, Ciszek B. Medial meniscus anatomy-from basic science to treatment. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):8–14. doi: 10.1007/s00167-014-3476-5. [DOI] [PubMed] [Google Scholar]
- 2.Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med. 2014;42(12):3016–3030. doi: 10.1177/0363546514524162. [DOI] [PubMed] [Google Scholar]
- 3.Furumatsu T, Hiranaka T, Kintaka K, et al. A characteristic MRI finding to diagnose a partial tear of the medial meniscus posterior root: an ocarina sign. Knee Surg Relat Res. 2021;33(1):38. doi: 10.1186/s43019-021-00120-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus: similar to total meniscectomy. J Bone Joint Surg Am. 2008;90(9):1922–1931. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 5.Kohli S, Schwenck J, Barlow I. Failure rates and clinical outcomes of synthetic meniscal implants following partial meniscectomy: a systematic review. Knee Surg Relat Res. 2022;34(1):27. doi: 10.1186/s43019-022-00155-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Matthews JR, Wang J, Zhao J, Kluczynski MA, Bisson LJ. The influence of suture materials on the biomechanical behavior of suture-meniscal specimens: a comparative study in a porcine model. Knee Surg Relat Res. 2020;32(1):42. doi: 10.1186/s43019-020-00053-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chung KS, Ha JK, Yeom CH, et al. Comparison of clinical and radiologic results between partial meniscectomy and refixation of medial meniscus posterior root tears: a minimum 5-year follow-up. Arthroscopy. 2015;31(10):1941–1950. doi: 10.1016/j.arthro.2015.03.035. [DOI] [PubMed] [Google Scholar]
- 8.Bernard CD, Kennedy NI, Tagliero AJ, et al. Medial meniscus posterior root tear treatment: a matched cohort comparison of nonoperative management, partial meniscectomy, and repair. Am J Sports Med. 2020;48(1):128–132. doi: 10.1177/0363546519888212. [DOI] [PubMed] [Google Scholar]
- 9.Feucht MJ, Kuhle J, Bode G, et al. Arthroscopic transtibial pullout repair for posterior medial meniscus root tears: a systematic review of clinical, radiographic, and second-look arthroscopic results. Arthroscopy. 2015;31(9):1808–1816. doi: 10.1016/j.arthro.2015.03.022. [DOI] [PubMed] [Google Scholar]
- 10.Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85(1):1–3. [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Scand J Med Sci Sports. 2000;10(1):2–11. doi: 10.1034/j.1600-0838.2000.010001002.x. [DOI] [PubMed] [Google Scholar]
- 13.Dragoo JL, Konopka JA, Guzman RA, Segovia N, Kandil A, Pappas GP. Outcomes of arthroscopic all-inside repair versus observation in older patients with meniscus root tears. Am J Sports Med. 2020;48(5):1127–1133. doi: 10.1177/0363546520909828. [DOI] [PubMed] [Google Scholar]
- 14.Chung KS, Noh JM, Ha JK, et al. Survivorship analysis and clinical outcomes of transtibial pullout repair for medial meniscus posterior root tears: a 5- to 10-year follow-up study. Arthroscopy. 2018;34(2):530–535. doi: 10.1016/j.arthro.2017.08.266. [DOI] [PubMed] [Google Scholar]
- 15.LaPrade RF, Matheny LM, Moulton SG, James EW, Dean CS. Posterior meniscal root repairs: outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017;45(4):884–891. doi: 10.1177/0363546516673996. [DOI] [PubMed] [Google Scholar]
- 16.Jung YH, Choi NH, Oh JS, Victoroff BN. All-inside repair for a root tear of the medial meniscus using a suture anchor. Am J Sports Med. 2012;40(6):1406–1411. doi: 10.1177/0363546512439181. [DOI] [PubMed] [Google Scholar]
- 17.Kim SB, Ha JK, Lee SW, et al. Medial meniscus root tear refixation: comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy. 2011;27(3):346–354. doi: 10.1016/j.arthro.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 18.Lee DW, Kim MK, Jang HS, Ha JK, Kim JG. Clinical and radiologic evaluation of arthroscopic medial meniscus root tear refixation: comparison of the modified Mason-Allen stitch and simple stitches. Arthroscopy. 2014;30(11):1439–1446. doi: 10.1016/j.arthro.2014.05.029. [DOI] [PubMed] [Google Scholar]
- 19.Furumatsu T, Miyazawa S, Fujii M, Tanaka T, Kodama Y, Ozaki T. Arthroscopic scoring system of meniscal healing following medial meniscus posterior root repair. Int Orthop. 2019;43(5):1239–1245. doi: 10.1007/s00264-018-4071-z. [DOI] [PubMed] [Google Scholar]
- 20.Lee SS, Ahn JH, Kim JH, Kyung BS, Wang JH. Evaluation of healing after medial meniscal root repair using second-look arthroscopy, clinical, and radiological criteria. Am J Sports Med. 2018;46(11):2661–2668. doi: 10.1177/0363546518788064. [DOI] [PubMed] [Google Scholar]
- 21.Seo HS, Lee SC, Jung KA. Second-look arthroscopic findings after repairs of posterior root tears of the medial meniscus. Am J Sports Med. 2011;39(1):99–107. doi: 10.1177/0363546510382225. [DOI] [PubMed] [Google Scholar]
- 22.Lee JH, Lim YJ, Kim KB, Kim KH, Song JH. Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: radiographic and clinical results with a 2-year follow-up. Arthroscopy. 2009;25(9):951–958. doi: 10.1016/j.arthro.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 23.Kim JH, Chung JH, Lee DH, Lee YS, Kim JR, Ryu KJ. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: a prospective comparison study. Arthroscopy. 2011;27(12):1644–1653. doi: 10.1016/j.arthro.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 24.Kim CW, Lee CR, Gwak HC, et al. Clinical and radiologic outcomes of patients with lax healing after medial meniscal root repair: comparison with subtotal meniscectomy. Arthroscopy. 2019;35(11):3079–3086. doi: 10.1016/j.arthro.2019.05.051. [DOI] [PubMed] [Google Scholar]
- 25.Dai W, Leng X, Wang J, Hu X, Ao Y. Second-look arthroscopic evaluation of healing rates after arthroscopic repair of meniscal tears: a systematic review and meta-analysis. Orthop J Sports Med. 2021;9(10):23259671211038289. doi: 10.1177/23259671211038289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lind M, Nielsen T, Fauno P, Lund B, Christiansen SE. Free rehabilitation is safe after isolated meniscus repair: a prospective randomized trial comparing free with restricted rehabilitation regimens. Am J Sports Med. 2013;41(12):2753–2758. doi: 10.1177/0363546513505079. [DOI] [PubMed] [Google Scholar]
- 27.Mueller BT, Moulton SG, O’Brien L, LaPrade RF. Rehabilitation following meniscal root repair: a clinical commentary. J Orthop Sports Phys Ther. 2016;46(2):104–113. doi: 10.2519/jospt.2016.6219. [DOI] [PubMed] [Google Scholar]
- 28.Hiranaka T, Furuhashi R, Takashiba K, et al. Agreement and accuracy of radiographic assessment using a decision aid for medial Oxford partial knee replacement: multicentre study. Knee Surg Relat Res. 2022;34(1):13. doi: 10.1186/s43019-022-00140-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Matthews JR, Brutico J, Heard J, Chauhan K, Tucker B, Freedman KB. Comparison of clinical outcomes following osteochondral allograft transplantation for osteochondral versus chondral defects in the knee. Knee Surg Relat Res. 2022;34(1):23. doi: 10.1186/s43019-022-00149-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Helito CP, da Silva AG, Guimaraes TM, Sobrado MF, Pecora JR, Camanho GL. Functional results of multiple revision anterior cruciate ligament with anterolateral tibial tunnel associated with anterolateral ligament reconstruction. Knee Surg Relat Res. 2022;34(1):24. doi: 10.1186/s43019-022-00153-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Asif N, Khan MJ, Haris KP, Waliullah S, Sharma A, Firoz D. A prospective randomized study of arthroscopic ACL reconstruction with adjustable-versus fixed-loop device for femoral side fixation. Knee Surg Relat Res. 2021;33(1):42. doi: 10.1186/s43019-021-00124-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hill PF, Vedi V, Williams A, Iwaki H, Pinskerova V, Freeman MA. Tibiofemoral movement 2: the loaded and unloaded living knee studied by MRI. J Bone Joint Surg Br. 2000;82(8):1196–1198. doi: 10.1302/0301-620x.82b8.10716. [DOI] [PubMed] [Google Scholar]
- 33.Feucht MJ, Grande E, Brunhuber J, Burgkart R, Imhoff AB, Braun S. Biomechanical evaluation of different suture techniques for arthroscopic transtibial pull-out repair of posterior medial meniscus root tears. Am J Sports Med. 2013;41(12):2784–2790. doi: 10.1177/0363546513502464. [DOI] [PubMed] [Google Scholar]
- 34.Vascellari A, Rebuzzi E, Schiavetti S, Coletti N. All-inside meniscal repair using the FasT-Fix meniscal repair system: is still needed to avoid weight bearing? A systematic review. Musculoskelet Surg. 2012;96(3):149–154. doi: 10.1007/s12306-012-0209-0. [DOI] [PubMed] [Google Scholar]
- 35.Noyes FR, Heckmann TP, Barber-Westin SD. Meniscus repair and transplantation: a comprehensive update. J Orthop Sports Phys Ther. 2012;42(3):274–290. doi: 10.2519/jospt.2012.3588. [DOI] [PubMed] [Google Scholar]
- 36.Styf J. The effects of functional knee bracing on muscle function and performance. Sports Med. 1999;28(2):77–81. doi: 10.2165/00007256-199928020-00002. [DOI] [PubMed] [Google Scholar]
- 37.Henriksson M, Rockborn P, Good L. Range of motion training in brace vs. plaster immobilization after anterior cruciate ligament reconstruction: a prospective randomized comparison with a 2-year follow-up. Scand J Med Sci Sports. 2002;12(2):73–80. doi: 10.1034/j.1600-0838.2002.120203.x. [DOI] [PubMed] [Google Scholar]
- 38.Spang Iii RC, Nasr MC, Mohamadi A, DeAngelis JP, Nazarian A, Ramappa AJ. Rehabilitation following meniscal repair: a systematic review. BMJ Open Sport Exerc Med. 2018;4(1):e000212. doi: 10.1136/bmjsem-2016-000212. [DOI] [PMC free article] [PubMed] [Google Scholar]