Abstract
Background
Amyloidosis of the bladder is a benign condition which can present with a multitude of symptoms including bladder mass, irritative voiding symptoms and haematuria.
Case presentation
We report on the investigation and management of a patient with recurrent localised amyloidosis of the bladder, which appears to have been managed fortuitously by concurrent methotrexate prescribed for another indication.
Conclusion
We provide further assessment and management with a focus on the possible benefit of methotrexate for management of localised bladder amyloidosis.
Keywords: Bladder tumour, Amyloidosis, Haematuria, Benign, Management, Methotrexate
List of abbreviations
- AL
Primary Amyloidosis
- AA
Secondary Amyloidosis
- ATTR
Inherited Transthyretin-related Amyloidosis
- CKD
Chronic Kidney Disease
- CIS
Carcinoma in Situ
- CT
Computed Tomography
- DMSO
Dimethyl Sulfoxide
- IHD
Ischaemic Heart Disease
- IVP
Intravenous Pyelogram
- LUTS
Lower Urinary Tract Symptoms
- TCC
Transitional Cell Carcinoma
- TTE
Transthoracic Echocardiogram
1. Introduction
The deposition of amyloid fibrils into the extracellular space leads to amyloidosis, a diverse disease that ranges from singular localised lesions with good prognosis to a morbid systemic condition.1 Common sites of localised amyloidosis are skin, lung, tongue, heart and larynx.1 Amyloidosis of the bladder is extremely rare, with only 349 cases reported in the literature, documented initially by Soloman in 1897 following a series of autopsies.1
Amyloidosis is classified into three subtypes based on chemistry profile; primary (AL), secondary (AA) and inherited transthyretin-related (ATTR) amyloidosis, the latter often associated with cardiomyopathy.2 Amyloidosis falls into two broad categories including systemic and localised. Amyloidosis can be localised where amyloid deposits are produced and deposited in one isolated part of the body, or systemic where amyloidogenic protein produced at a distant site circulates in the blood depositing amyloid in distant tissues and resulting in organ dysfunction.3
Amyloidosis of the bladder is a benign condition, and accounts for around 1–2% of all bladder tumour aetiology.3 It is primarily a disease of older males, presenting with haematuria or bladder mass, often requiring histological confirmation for diagnosis, with the use of a Congo red staining.2
We report a case of recurrent localised bladder amyloidosis, seen in a regional clinical setting. A fifty year old male presented with recurrent localised bladder amyloidosis. The patient was subsequently diagnosed with psoriatic arthritis requiring the initiation of systemic methotrexate. There is an emerging link between not only inflammatory arthropathy and amyloidosis but also treatment with disease modifying anti-rheumatic drugs such as methotrexate.2, 3, 4 We hypothesise that this patient's amyloidosis was incidentally controlled with methotrexate and there may be a role for methotrexate in the bladder amyloidosis treatment algorithm.
2. Case presentation
A male in his fifth decade of life presented for review of recurrent painless macroscopic haematuria. His past medical history included dyslipidaemia and psoriatic arthritis, eventually requiring systemic methotrexate. He did not have any known risk factors for bladder cancer.
Ten years prior the patient had been diagnosed with amyloidosis of the bladder. He had presented at that time with haematuria, and CT of the abdomen and pelvis noted bladder wall thickening. Cystoscopy revealed erythema of the left lateral wall and biopsy confirmed amyloidosis on Congo red stain and chronic cystitis. He was reviewed by a haematologist and underwent a bone marrow biopsy which was negative for amyloid deposition. His final diagnosis was of localised bladder amyloidosis. He did not undergo further cystoscopic surveillance.
He represented with recurrent macroscopic haematuria with CT IVP illustrating extensive bladder wall thickening, most marked at the left lateral aspect of the bladder with punctate calcifications (Fig. 1).
Fig. 1.
Cystoscopic View of Amyloidosis of the Bladder: A) Right B) Posterior and C) Left bladder walls D) Cystitis with Amyloid Deposition.
He underwent repeat cystoscopic investigation which revealed recurrence of a small erythematous patch of bladder wall with presence of small stone embedded into the bladder wall (Fig. 2). Histology confirmed recurrent amyloidosis with associated calcification in the stroma of the bladder with adjacent cystitis (Fig. 3).
Fig. 2.
Computed Tomography Intravenous Pyelogram (CT IVP) Images, Coronal Slices, Showing Bladder Wall Thickening and Calcifications. Non contrast (A) and contrast (B) imaging illustrating left bladder wall thickening with calcification present.
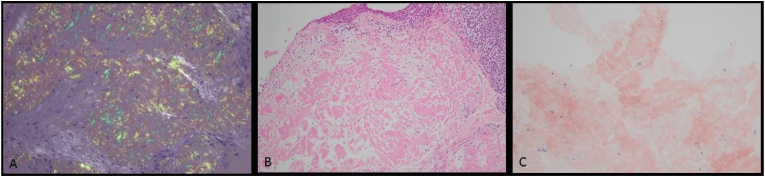
Fig. 3.
Histopathology microscopic sections. A) Apple green birefringence highlighting fibres of amyloid when viewed under polarized light. B) Heamatoxylin and eosin stain showing pale eosinophilic amorphous material C) Congo Red stain showing typical “salmon pink” amyloid.
The patient was reviewed again by a haematologist for further evaluation into his recurrent bladder amyloidosis, however there was no concern for systemic involvement. A 24 hour urine protein was elevated 0.39g/L (<0.12), however Bence Jones Proteins were not detected. Serum electrophoresis was unremarkable. Clinical examination did not reveal any features suggestive of systemic amyloidosis.
An interesting note was made by the treating haematologist suggesting that perhaps his regular management for psoriatic arthritis with methotrexate may have been incidentally treating his amyloidosis with the drug modifying local amyloid deposition of the bladder.
3. Discussion
The aetiology of bladder amyloidosis is unknown.3 This rare benign condition, classically presents in males in their sixth decade of life.1 Haematuria, irritative voiding symptoms and abdominal pain traditionally thought to be the leading clinical presentations, were challenged in a recent publication by Sirohi et al. in which the 29 patient case series had 62% of patients present with a bladder mass.5
Typical investigation involves urine culture, cytology, and CT. Distribution of systemic compared to localised disease at the time of diagnosis is reported as 60% and 40% respectively, with no reported cases of progression to systemic disease after confirmation of localised bladder amyloidosis.5 Hence, initial evaluation for systemic amyloidosis is prudent, with echocardiogram, serum amyloid P scintigraphy, 24 hour protein electrophoresis, Bence Jones protein assessment and histology from abdominal subcutaneous fat, salivary gland or rectal mucosa.3
Diagnosis is required with histological assessment following transurethral resection of the tumour. 70% of tumours are found in the posterior bladder wall with a quarter found on the trigone.2 Congo Red Staining expresses an apple-green birefringence in polarised microscopy.3
Concurrent transitional cell carcinoma with amyloid of the bladder was originally thought to be rare, with only 3 reported cases in the literature.2 However, Sirohi et al. reported a retrospective 13-year case series in 2019 of 29 patients with amyloidosis of the bladder, showing 48% were associated with urothelial carcinoma.5 No correlation with amyloid chemical subtypes was noted, and on histological assessment the amyloid deposits were always adjacent to the urothelial carcinoma not integrated within them.
Clear guidelines for management are not in place but have been recently suggested by Pyrgidis et al.6 After initial resection and assessment and exclusion of systemic amyloidosis, a period of surveillance cystoscopy should be considered after initial resection at 3, 12 and 24 months.6 In cases of recurrent localised bladder amyloidosis which are asymptomatic, consideration of conservative management may be appropriate to reduce operative risks and excessive bladder scarring, with progression to transurethral resection of the bladder tumour when appropriate.6 Installation with dimethyl-sulfoxide is described in the literature but has not been widely adopted in treatment pathways.3,5
The patient has a history of psoriatic arthritis treated with low dose methotrexate. At the time of initial diagnosis, the patient was not taking methotrexate, the treatment was commenced in the ten-year period between presentations with macroscopic haematuria. Chronic autoimmune inflammatory diseases, such as rheumatoid and psoriatic arthritis, cause chronic inflammation by increasing production of pro-inflammatory molecules. The persistent inflammatory process is proposed as a cause of amyloidosis.2, 3, 4 Methotrexate inhibits the inflammatory properties of macrophages, endothelial cells and T-cells that mediate autoimmune inflammatory arthropathies and their complications, such as amyloidosis.4 There is limited evidence available on the treatment paradigms of this rare disease process, thus there is no current evidence available to support the theoretical benefit of methotrexate in psoriatic arthritis and bladder amyloid. Further high-quality research with randomised control trials are required to further explore potential treatment.
4. Conclusion
Localised amyloidosis of the bladder is a rare condition that is often managed with resection and fulguration. Initial assessment for systemic disease is essential, and ongoing surveillance is required for the high rate of local recurrence. Haematologist referral for consideration of methotrexate in severe, recurrent, or refractory cases may be warranted but more research is required.
Disclosure/conflict of interest
Nil.
Funding
Nil.
Written patient/MTDM consent
Yes.
References
- 1.Kaur S., Gupta A., Gulwani H. A clinicopathological and immunohistochemical study of non-urothelial bladder tumours. Indian J Cancer. 2019;56(3) doi: 10.4103/ijc.IJC_459_17. 254 -26. [DOI] [PubMed] [Google Scholar]
- 2.Schou-Jensen K., Dahl C., Pedersen Pilt A., Htum Azawi N. Amyloidosis in the bladder: three cases with different appearance. Scandinavian J Urol. 2014;48(5):489–492. doi: 10.3109/21681805.2014.920414. [DOI] [PubMed] [Google Scholar]
- 3.Gomha F.S., Smain A.M., Sohail N., Yousif A.A., Abdelrahman K.M., Amir E., et al. Primary localised amyloidosis of the urinary bladder: a recurrent and progressive disease. J Taibah Univ Med Sci. 2018 doi: 10.1016/j.jtumed.2018.02.003. JID - 101621911 PMC - PMC6694977 OTO - NOTNLM. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nakamura T. 2016. Developments in the Treatment of Amyloid A Amyloidosis Secondary to Rheumatoid Arthritis [Internet] Exploring New Findings on Amyloidosis. InTech. [DOI] [Google Scholar]
- 5.Sirohi D., Gandhi J., Amin M.B., Luthringer D.J. Amyloidosis of the bladder and association with urothelial carcinoma: report of 29 cases. Human Pathol. 2019 doi: 10.1016/j.humpath.2019.08.011. JID - 9421547. [DOI] [PubMed] [Google Scholar]
- 6.Pyrgidis N., Mykoniatis I., Pegios V.F., Sokolakis I., Hatzichristodoulou G., Bourdoumis A., et al. Amyloidosis of the urinary bladder: a systematic review and a proposed management algorithm. Urology. 2021 doi: 10.1016/j.urology.2021.07.013. JID - 0366151. [DOI] [PubMed] [Google Scholar]