Abstract
Objectives:
To evaluate whether information from CBCT changes the treatment plan for maxillary second and third molars and to examine clinical and radiographic parameters with an impact on treatment decision.
Methods:
This prospective study included 260 maxillary third molars with superimposition onto the second molar in panoramic images (170 patients; mean age 28 years, range 16–63). An initial treatment plan was based on clinical findings and panoramic images. After CBCT, a final treatment plan was decided. Treatment was undertaken based on the final treatment plan. Through logistic regression analyses, impact of clinical and radiographic parameters on change in treatment plan, removal of the third molar vs no treatment, and removal of the second vs third molar were evaluated.
Results:
The treatment plan changed in 82 cases (32%). Sixteen cases (6%) changed from removal of the third molar to removal of the second molar. Regression analyses showed that severe resorption in the second molar was significantly related to a change in treatment plan. Removal of a third molar was decided in 180 cases and regression analyses identified that mesioangulation of the third molar, marginal bone loss, superficial resorption, and age were significantly related to removal of the third molar vs no treatment. Thirty second molars were removed, and regression analyses showed that severe resorption was significantly related to removal of the second molar instead of the third molar.
Conclusions:
Parameters such as resorption evaluated in CBCT can modify the treatment decision, resulting in removal of the second and/or the third molar.
Keywords: Cone Beam Computed Tomography, Maxilla, Panoramic Radiography, Diagnostic Imaging, Third Molar
Introduction
Impaction of maxillary third molars is commonly seen. 1 Pathology related to an impacted maxillary third molar could be external root resorption (ERR) and marginal bone loss. 2 The first choice radiographic method to assess third molars is panoramic imaging to assist the clinical examination prior to treatment planning. 3 No guidelines concerning maxillary second and third molar exist stating when Cone Beam CT (CBCT) is indicated. This is in contrast to mandibular third molars where guidelines concerning the use of CBCT have been published after extensive investigation over the past decades. 4
Recently, a systematic review comparing panoramic imaging and CBCT for assessment of marginal bone loss and ERR of the second molar associated with a third molar impaction has been published. 5 The study concluded that more cases of ERR were diagnosed based on CBCT compared to panoramic imaging. A study by Hermann et al drew the same conclusion, but also revealed that severity of ERR was underestimated in panoramic images compared to CBCT. 6 Whether the additional information provided by CBCT, in comparison with panoramic images, changes the treatment plan for maxillary third molars has been investigated in a retrospective study. 7 It was found in 111 cases of maxillary third molars that findings in CBCT changed the treatment plan in 59% of the cases, and severe ERR in the second molar was identified as the main factor when deciding on whether to remove a second molar instead of a third molar. Removal of the second molar was performed in 19% of the cases.
Lately, Tao Qu et al performed the first prospective study in the area of ERR of maxillary second molars. 8 The study included 33 cases of maxillary second molars and assessed the prognosis of second molars with ERR observed in CBCT caused by an adjacent impacted third molar. The patients were followed for six months after third molar removal. The study concluded that asymptomatic second molars with ERR have a high probability of preserving normal vitality of the pulp after removal of the adjacent third molar. Increasing age of the patient and the presence of ERR affecting all roots of the second molar were significantly associated with poor prognosis of the second molar. The study did not evaluate other treatment possibilities but merely the short-term prognosis of the second molar. 8
In the presence of ERR of the maxillary second molar caused by the third molar, treatment options may include removal of the third molar with an expectation of arresting the progression of ERR, or removal of the second molar, if severe ERR is present and the long-term prognosis for tooth survival is considered to be poor. A further treatment option may be removal of both the second and the third molar if the prognosis of the second molar is poor and eruption of the third molar is unlikely, or if pathology is related to the third molar. Finally, no treatment and ensuing observation may also be an option, particularly when prognosis of the second molar is poor, and the patient is without symptoms. The Guidance on the Extraction of Wisdom Teeth published by the National Institute for Health and Care Excellence (NICE) only considers whether the third molar should be removed or not. 9
Conclusively, studies focusing on maxillary third molars are sparse, and few have examined whether CBCT has an impact on treatment planning. Therefore, the aim of this prospective study was to examine whether CBCT changed the treatment plan for maxillary second and third molars. Furthermore, this study aimed to evaluate the influence of relevant clinical and radiographic parameters on the choice of treatment decided for impacted maxillary third molars.
Methods and materials
Patients
In this prospective clinical study, 170 patients (107 females and 63 males), mean age 28 years (range 16 to 63 years), were included contributing 260 maxillary third molars (134 right side-and 126 left side-maxillary third molars). Eighty patients had one maxillary third molar (52 females and 28 males) and 90 patients had both maxillary third molars (55 females and 35 males) included in the study. The inclusion criterion was the presence of superimposition of the maxillary third molar onto the second molar observed in panoramic radiographic images.
The patients included in the study were initially examined as a result of specific problems with a third molar or for other pathologies not related to third molars, either at the Department of Dentistry and Oral Health, Aarhus University, private dental practices or community dental healthcare clinics in Denmark. If superimposition of the maxillary third and second molar was present, and consequently, ERR could be suspected, the patients were invited to participate in the study. Patients were consecutively enrolled in the study between 2019 and 2021. Participation in the study was without any economical expenses to the patients.
Clinical examination
The patients underwent a clinical examination performed by the primary investigator (LH). If a panoramic image was not available when the patient was included in study, a panoramic image was taken following the clinical examination to enable radiographic assessment of the maxillary second and third molars in question.
From the clinical examination, the following parameters were registered in relation to the maxillary second and third molars: Anamnestic parameters: (1) experience of pain from the area of the maxillary second and/or third molar on the day of the clinical examination (no pain/pain) ; (2) self-reported oral hygiene related to the maxillary third molar (adequate oral hygiene/inadequate oral hygiene); Clinical parameters: (3) impaction state of the maxillary third molar (erupted/impacted) ; (4) periodontal status of the maxillary second molar (no periodontal pockets and no bleeding on probing/periodontal pockets ≥ 4 mm or bleeding on probing/periodontal pocket ≥4 mm and bleeding on probing); (5) caries in the maxillary second molar (no caries/caries); and (6) pain on percussion from the maxillary second molar (no pain/pain). Parameter (1) and (2) were patient-reported, whereas parameter (3) to (6) were examiner-reported. In case of the patient having two third molars included in the project, all the clinical parameters were scored individually for each second and third molar regions.
Radiographic examination
The panoramic image was obtained either from the referring dental practice or recorded at Section for Oral Radiology, Department of Dentistry and Oral Health, Aarhus, Denmark using a ProMax unit (Planmeca, Helsinki, Finland) with a CCD-based image receptor (68 kV, 12.5 mA, 11.3 s examination time). The panoramic images were taken by the primary investigator, trained by experienced staff members, or by a radiographer at the section. To reduce the radiation dose, the recordings were sectioned to expose only the area of the relevant maxillary second and third molar. After the clinical examination and panoramic imaging, the patient was referred for a CBCT. The CBCT examination was performed at Section for Oral Radiology using a 3Shape X1 3D unit (3Shape, Copenhagen, Denmark) with a 4 × 4 cm field of view (FOV) and 0.075 voxel resolution (90 kV, 12 mA, 11.7 s exposure time, 533 base projections). The FOV was centered at the maxillary third molar region. The CBCT was obtained the same day as the clinical examination and the panoramic image. An experienced staff member at the Section for Oral Radiology performed the CBCT.
Radiographic assessment
The primary investigator assessed the following radiographic parameters: (1) bony coverage of the maxillary third molar (no bony coverage/bony coverage); (2) apical root closure of the maxillary third molar (closed apices/open apices); (3) angulation of the maxillary third molar (vertical/mesioangulated/distoangulated/horizontal/transversal/inverted); (4) number of root(s) of the maxillary third molar (1/2/3/≥ 4); (5) enlarged follicular space ≥2 mm related to the maxillary third molar (no enlargement/enlargement); (6) marginal bone loss ≥4 mm of the distal surface of the maxillary second molar (no marginal bone loss/marginal bone loss ≥4 mm); (7) external root resorption of the maxillary second molar (no ERR/superficial ERR/ERR involving <halfway through dentin/ERR involving ≥halfway through dentin); 10 (8) bony separation between the sinus floor and the maxillary third molar (bony separation/no bony separation); and (9) inclination of the maxillary third molar in the coronal plane (no inclination/palatal inclination/buccal inclination). The radiographic parameters assessed were the same for the panoramic image and CBCT, except for parameter (8) and, (9) which were only assessed in the CBCT volume. The primary investigator was authorized to order and evaluate CBCT according to the Danish Radiation Protection authorities and had five years of experience in assessing CBCT. Moreover, in case of doubt on the radiographic assessment, an oral radiologist (LHM) with more than 15 years of experience in the area was consulted and diagnosis was established in consensus.
Treatment plans
Based on both the clinical examination and the panoramic image, an initial treatment plan was established deciding on: (1) no treatment or; (2) removal of the maxillary second molar or; (3) removal of the maxillary third molar or; (4) removal of both the maxillary second and third molars. Subsequently, the CBCT was assessed and the final treatment plan was decided including the same options as the initial treatment plan, and this plan was offered to the patient. The primary investigator did not evaluate the CBCT until after the initial treatment plan had been established. Both the initial and final treatment plans were established as a consensus among the primary investigator with little experience in oral surgery, an oral surgeon (PT) with more than 10 years of experience, and an oral and maxillofacial surgeon (SEN) with more than 20 years of experience. Findings from the clinical and radiographic examinations, the initial and final treatment plan, and the treatment were registered in separate documents as well as in the patient’s record.
Treatment
Treatment according to the final treatment plan was performed at Section for Oral and Maxillofacial Surgery and Oral Pathology, Department of Dentistry and Oral Health, Aarhus University, Denmark by the primary investigator, the oral and maxillofacial surgeon, or the oral surgeon who had participated in the treatment planning. The primary investigator performed most of the operations supervised by one of the two oral surgeons. If decided to be too difficult for the primary investigator, one of the oral surgeons performed the operation assisted by the primary investigator. If patients declined the offered treatment or for other reasons did not receive the planned treatment, this was registered in the patient’s records.
The study is considered a quality control study of the radiographic and treatment protocol used at IOOS to address the impact of CBCT on treatment of maxillary third molars. Since the study is a quality control study and treatment offered to the patients not chosen by randomization, approval of the study by ethical committees is not needed.
Data treatment
Data were recorded in Microsoft Office Excel® 2016 (Microsoft Corp., Redmond, WA) and imported to STATA® 2021 (StataCorp LLC, Santa Monica, CA) for statistical analysis. A change in treatment plan was registered when the initial treatment plan was not identical with the final treatment plan. The fact that some patients had more than one tooth included in the study has been taken into account in the statistical analyses, where the logistic regression with robust standard errors accounted for correlation between outcomes from the same patient. The estimates are calculated based on a generalized estimating equation approach.
Parameters from the clinical and radiographic examinations were used as independent variables in the initial logistic regression analyses. The independent variables were divided into: Clinical variables (pain from the area of the second and third molar, oral hygiene related to the third molar, periodontal status of the second molar, impaction state of the third molar, caries of the second molar, and pain on percussion of the second molar); panoramic variables (bony coverage of the third molar, apical root closure of the third molar, angulation of the third molar, root number of the third molar, degree of ERR of the second molar, and marginal bone loss at the distal surface of the second molar); and CBCT variables, which were the same as the panoramic variables together with the relation between the sinus floor and apex of the third molar and inclination of the third molar in the coronal plane.
To explore the impact of the parameters from the clinical and two radiographic examinations on a change in treatment plan, initial logistic regression analyses were performed for each variable with the outcome “change in treatment plan”, defined as any change between the initial and the final plan. Further, initial logistic regression analyses were performed for each variable to explore factors with an impact on the decision to remove the maxillary third molar (yes/no) and on the decision to remove the maxillary second molar (with or without the maxillary third molar) instead of only the maxillary third molar (yes/no).
After the initial analyses, variables with a significant impact (p < 0.05) were entered into multivariate logistic regression analyses together with gender and age. For all three outcomes, a multivariate logistic regression analysis was performed separately for the clinical, panoramic, and CBCT parameters.
Results
Clinical and radiographic findings
Impaction of the maxillary third molar was observed in the majority cases (74%). The low frequency of erupted third molars is also reflected in few cases reporting inadequate oral hygiene related to a maxillary third molar (6%). Pain on the day of the examination from the region of maxillary second and/or third molar was only reported in 5% of the cases, despite the fact that severe ERR was found in 17% of the cases. Table 1 displays the distribution of the clinical findings.
Table 1.
Distribution of the clinical parameters
| Clinical parameters | N (%) |
|---|---|
| Experience of pain from region of M2/M3 at clinical examination | |
| No Yes |
246 (94.6%) 14 (5.4%) |
| Reported inadequate oral hygiene related to M3 | |
| No Yes |
245 (94.2%) 15 (5.8%) |
| Impaction of M3 | |
| Not impacted Impacted |
67 (25.8%) 193 (74.2%) |
| Periodontal pockets and/or BOP of M2 | |
| No Yes |
71 (27.3%) 189 (72.7%) |
| Caries M2 | |
| No Yes |
247 (95.0%) 13 (5.0%) |
| Pain on percussion M2 | |
| No Yes |
235 (90.4%) 25 (9.6%) |
BOP, bleeding on probing.; M2, maxillary second molar; M3, maxillary third molar.
Mesioangulation was the most common position of the maxillary third molar identified in this study, followed by the vertical and distoangular position observed in both panoramic imaging and CBCT. Pathology related to either the maxillary second or third molar was often found. Marginal bone loss of the second molar was found in 80–88% of the cases. ERR independent of severity was diagnosed in 43–61% of the cases. Distribution of the findings in panoramic imaging and CBCT can be seen in Table 2.
Table 2.
Distribution of the radiographic findings seen in panoramic images and CBCT
| Radiographic parameters | Panoramic imaging N (%) | CBCT N (%) |
|---|---|---|
| Bony coverage of M3 | ||
| No | 228 (87.7%) | 256 (98.5%) |
| Yes | 32 (12.3%) | 4 (1.5%) |
| Apical root closure of M3 | ||
| No | 58 (22.3%) | 80 (30.8%) |
| Yes | 202 (77.7%) | 180 (69.2%) |
| Angulation M3 | ||
| Vertical | 57 (21.9%) | 58 (22.3%) |
| Mesioangulation | 174 (66.9%) | 175 (67.3%) |
| Distoangulation | 26 (10.0%) | 18 (6.9%) |
| Other | 3 (1.2%) | 9 (3.5%) |
| Number of root(s) M3 | ||
| 1 | 96 (36.9%) | 73 (28.1%) |
| 2 | 12 (4.6%) | 49 (18.9%) |
| 3 | 150 (57.7%) | 121 (46.5%) |
| 4 or more | 2 (0.8%) | 17 (6.5%) |
| Enlarged follicular space M3 | ||
| No | 191 (73.5%) | 166 (63.8%) |
| Yes | 69 (26.5%) | 94 (36.2%) |
| Marginal bone loss of M2 | ||
| No | 51 (19.6%) | 32 (12.3%) |
| Yes | 209 (80.4%) | 228 (87.7%) |
| External Root resorption of M2 | ||
| No | 149 (57.3%) | 101 (38.9%) |
| Superficial ERR | 21 (8.1%) | 44 (16.9%) |
| ERR involving < Halfway through dentin | 50 (19.2%) | 70 (26.9%) |
| ERR involving ≥ Halfway through dentin | 40 (15.4%) | 45 (17.3%) |
| Bony separation between the sinus floor and M3 | ||
| No | - | 178 (68.5%) |
| Yes | - | 82 (31.5%) |
| Inclination of M3 | ||
| No | - | 150 (57.7%) |
| Buccal | - | 58 (22.3%) |
| Palatal | - | 52 (20.0%) |
ERR, external root resorption.; M2, maxillary second molar; M3, maxillary third molar.
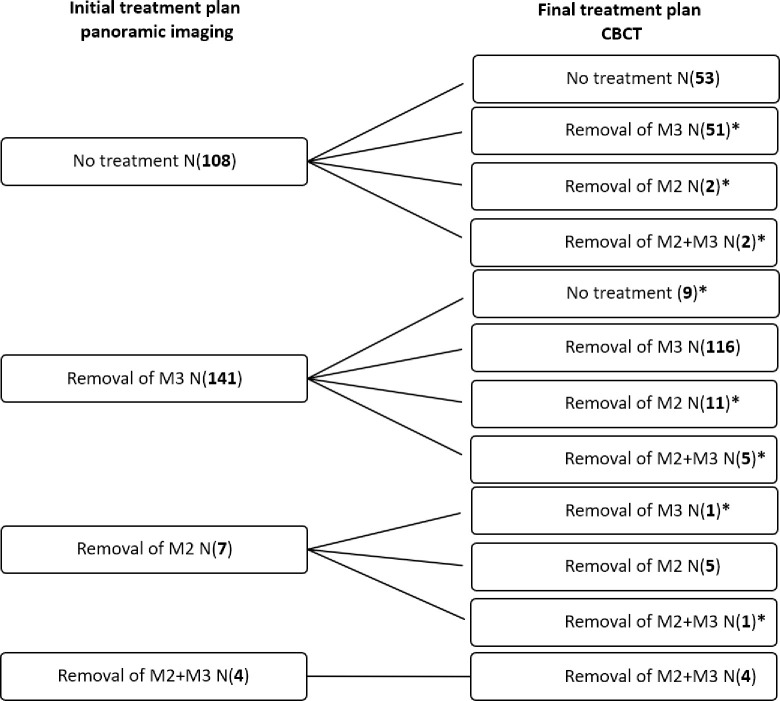
Treatment plans
For each of the 260 cases included in the study, both an initial and a final treatment plan were registered, and the distribution is shown in Figure 1. Removal of a third molar (54%) was the most commonly decided treatment based on the panoramic image followed by no treatment (42%), whereas removal of a second molar was rarely planned based on a panoramic image (4%). As for CBCT, removal of a third molar (64.6%) and no treatment (23.9%) were the most common treatment plans, although removal of a second molar (11.5%) was more often planned based on CBCT compared to panoramic images. When examining changes between the initial treatment plan and the final treatment plan, a change occurred in 82 cases (32%).
Figure 1.
Flowchart demonstrating the initial treatment plan based on a panoramic image and the final treatment plan based on CBCT for the 260 cases. *changes in treatment plan. M2, maxillary second molar; M3, maxillary third molar.
Parameters with an impact on a change in treatment plan
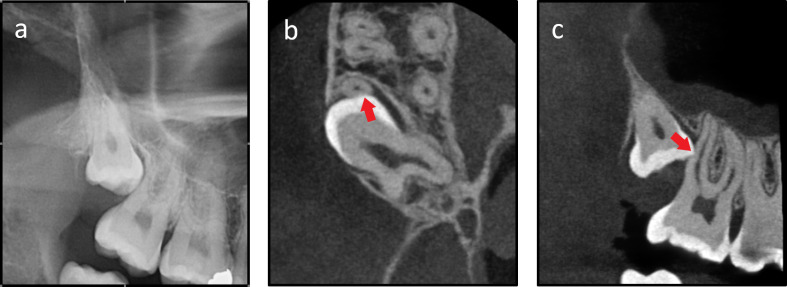
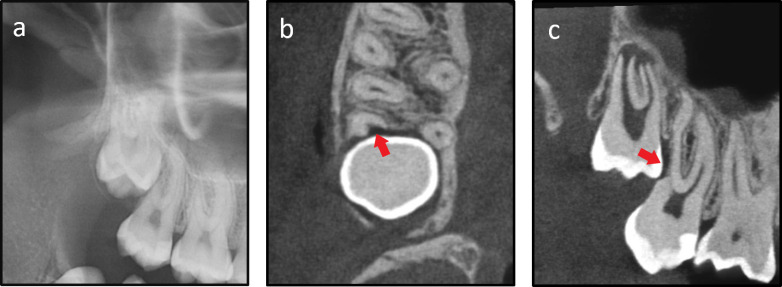
A change from no treatment to removal of either the second or the third molar or both occurred in 55 cases, whereas nine cases changed from removal of the third molar to no treatment. Sixteen cases changed from removal of the third molar to removal of the second molar or both. Only one case changed from removal of the second molar to removal of the third molar (Figure 1). Figure 2 shows a case where the treatment plan changed from no treatment to removal of the third molar after information from CBCT. On the other hand, Figure 3 shows a case were the treatment plan changed from removal of the third molar to removal of the second molar.
Figure 2.
A right side impacted maxillary third molar shown in the panoramic image (a); CBCT image in the axial plane (b); CBCT image in the sagittal plane, ERR is marked with an arrow (c). CBCT shows ERR in the middle portion of the distobuccal root of the second molar, ERR is marked with an arrow. ERR is seen less than halfway through dentin. ERR, external root resorption.
Figure 3.
A right side impacted maxillary third molar shown in the panoramic image (a); CBCT image in the axial plane (b); CBCT image in the sagittal plane, ERR is marked with an arrow (c). CBCT shows ERR in the middle portion of the distobuccal root of the second molar, ERR is marked with an arrow. ERR involves the pulp of the second molar. ERR, external root resorption.
The results from the initial logistic regression analyses showed that only severe ERR observed in CBCT and gender had a significant impact on a change in treatment plan. Based on the multivariate logistic regression analysis (Table 3), the presence of severe ERR observed in CBCT was associated with an almost three times higher chance that the treatment plan changed (p = 0.011). None of the parameters from the clinical examination or panoramic images showed a significant impact on a change in treatment plan.
Table 3.
Parameters including gender and age that could influence a change in treatment plan (multivariate logistic regression analysis). Parameters with a p-value < 0.05 are marked with *
| Change in treatment plan (n = 82) vs no change (n = 178) | |||
|---|---|---|---|
| Parameter | OR | p-value | 95% CI |
| ERR seen in CBCT [No] | |||
| Superficial | 1.00 | 0.995 | 0.42–2.38 |
| < Halfway through dentin | 1.12 | 0.772 | 0.53–2.35 |
| ≥ Halfway through dentin | 2.80 | 0.011* | 1.27–6.18 |
| Gender [Male] | |||
| Female | 1.87 | 0.051 | 0.99–3.52 |
| Age [Ascending] | 0.99 | 0.607 | 0.96–1.02 |
CI, confidence interval; ERR, external root resorption; OR, odds ratio.
Group in [brackets] was the reference group.
Parameters with an impact on the decision to remove the maxillary third molar vs. no treatment
Removal of a maxillary third molar was planned based on CBCT for 180 cases (69%); however, 12 of these cases were also scheduled for removal of the second molar. It was decided not to treat in 62 cases (24%).
In the initial logistic regression analyses, none of the clinical parameters showed a significant impact on removal of a maxillary third molar. On the other hand, bony coverage of the third molar, angulation of the third molar, marginal bone loss at the second molar, and ERR observed in the panoramic image had a significant impact. Based on the multivariate analysis, mesio- and distoangulated third molars were more likely to be removed compared to third molars with a vertical position (Table 4). If a third molar was mesioangulated in the panoramic image, there was a nearly nine times higher chance that the third molar was removed (p < 0.001) instead of deciding on no treatment. Although removal of the third molar was less likely when distoangulated (p = 0.045) compared to mesioangulated. If marginal bone loss of the second molar was registered, the chance of removing the third molar instead of no treatment was almost four times higher (p = 0.024). Furthermore, age also had a significant impact (p = 0.004) meaning that the likelihood of having a third molar removed decreased 0.93 times for every year the patient’s age increases. Thereby, the surgeon would more likely remove a third molar in younger patients.
Table 4.
Radiographic parameters seen in panoramic images and CBCT together with gender and age that could influence removal of a third molar (multivariate logistic regression analysis). Parameters with a p-value < 0.05 are marked with *
| Parameter | Removal of a third molar (n = 180) vs no treatment (n = 62) | |||||
|---|---|---|---|---|---|---|
| Panoramic image | CBCT | |||||
| OR | p-value | 95% CI | OR | p-value | 95% CI | |
| Bony coverage [No] | ||||||
| Yes | 0.76 | 0.648 | 0.23–2.46 | - | - | - |
| Angulation [Vertical] | ||||||
| Mesioangulation | 8.80 | <0.001* | 3.53–21.95 | 6.54 | <0.001* | 2.54–16.86 |
| Distoangulation | 4.07 | 0.045* | 1.03–16.06 | 1.04 | 0.956 | 0.27–4.00 |
| Other | 3.08 | 0.298 | 0.37–25.52 | 2.66 | 0.311 | 0.40–17.62 |
| Marginal bone loss [No] | ||||||
| Yes | 3.90 | 0.024* | 1.20–12.76 | 3.49 | 0.012* | 1.31–9.29 |
| ERR [No] | ||||||
| Superficial | 1.36 | 0.632 | 0.39–4.80 | 10.23 | <0.001* | 2.55–41.02 |
| < Halfway through dentin | 2.19 | 0.183 | 0.69–6.92 | 2.16 | 0.133 | 0.79–5.88 |
| ≥ Halfway through dentin | 2.25 | 0.257 | 0.55–9.17 | 2.95 | 0.183 | 0.60–14.45 |
| Gender [Male] | ||||||
| Female | 0.72 | 0.443 | 0.31–1.68 | 0.70 | 0.432 | 0.29–1.69 |
| Age [Ascending] | 0.93 | 0.004* | 0.89–0.98 | 0.93 | 0.004* | 0.89–0.98 |
CI, confidence interval; ERR, external root resorption; OR, odds ratio.
Group in [brackets] was the reference group.
Parameters in CBCT with a significant impact in the initial analyses were angulation of the third molar, marginal bone loss of the second molar, and ERR. Results from the multivariate analysis (Table 4) showed that mesioangulated third molars had more than six times the chance to be removed compared to molars with a vertical position (p < 0.001). Marginal bone loss was also associated with a higher chance of having a third molar removed (p = 0.012). Furthermore, if superficial resorption of the second molar was present in CBCT, it was 10 times more likely that the third molar was removed instead of deciding on no treatment (p < 0.001). Similar to the initial treatment plan based on the panoramic image, age also had a significant impact in the multivariate analysis for CBCT (p = 0.004) meaning that younger patients had a higher chance of having a third molar removed instead of no treatment, compared to older patients. Removal of a third molar was more commonly performed in younger patients, in 74% of the cases with third molar removal, the patient was 27 years old or younger.
Parameters with an impact on the decision to remove the second maxillary molar vs. the third molar
The third analysis examined parameters influencing the decision to remove a second molar instead a third molar in the final treatment plan. Overall, 30 cases were scheduled for removal of a second molar based on CBCT, removal of both a second and a third molar comprised 12 out of the 30 cases. On the other hand, removal of a third molar was planned based on CBCT for 168 cases.
Based on the initial analyses of the clinical parameters, the presence of periodontal pockets ≥ 4 mm and bleeding on probing together with caries in the second molar were entered in the multivariate logistic regression analysis. Only age had a significant impact in the analysis. Every time the patient’s age raised with one year, the chance of having a second molar removed instead of a third molar increased 1.07 times (p = 0.003).
For the radiographic parameters observed in the panoramic image, ERR was the only parameter with a significant impact in the initial analyses. Both severe ERR and age were significant parameters found in the multivariate analysis (Table 5). If severe ERR was observed in the second molar in the panoramic image, the chance of having the second molar planned for removal instead of the third molar was 13 times higher (p < 0.001). In the initial analyses for CBCT, ERR and dental status of the second molar both had a significant impact. As also seen for panoramic imaging, but with a higher odds ratio in CBCT (OR 51, p < 0.001), the presence of severe ERR highly influenced the decision to remove the second molar (Table 5). Age was significant in the multivariate analysis when treatment plan was based on the panoramic image (p = 0.002), increasing age raised the chance of having a second molar removed instead of a third molar. Age as well as dental status of the second molar was not significant in the multivariate analysis based on CBCT.
Table 5.
Radiographic parameters seen in panoramic images and CBCT together with gender and age that could influence removal of a second molar instead of a third molar (multivariate logistic regression analysis). Parameters with a p-value < 0.05 are marked with *
| Parameter | Removal of second molar (n = 30) vs third molar (n = 168) | |||||
|---|---|---|---|---|---|---|
| Panoramic image | CBCT | |||||
| OR | p-value | 95% CI | OR | p-value | 95% CI | |
| ERR [No] | ||||||
| Superficial | 1.02 | 0.986 | 0.12–8.89 | - | - | - |
| < Halfway through dentin | 1.70 | 0.432 | 0.45–6.36 | 0.97 | 0.977 | 0.16–5.85 |
| ≥ Halfway through dentin | 13.21 | <0.001* | 4.59–38.05 | 51.03 | <0.001* | 11.00–236.73 |
| Dental status [No filling, crown or root canal treatment] | ||||||
| Filling therapy, crown or root canal treatment | - | - | - | 2.18 | 0.391 | 0.37–12.94 |
| Gender [Male] | ||||||
| Female | 1.50 | 0.452 | 0.55–4.05 | 0.95 | 0.938 | 0.28–3.26 |
| Age [Ascending] | 1.07 | 0.002* | 1.03–1.12 | 1.06 | 0.112 | 0.99–1.15 |
CI, confidence interval; ERR, external root resorption; OR, odds ratio.
Treatment
Agreement between the final treatment plan based on CBCT and the actual treatment performed is visualized in Table 6. In general, the treatment performed was in accordance with the final treatment plan based on the findings seen in CBCT. In 11 cases (4%), another treatment or no treatment was carried out. Nine of these cases changed from removal of a third molar, second molar, or both to no treatment since the patients either declined the proposed treatment plan (two cases), did not have time to receive treatment (four cases), or did not show up for the scheduled appointment (three cases). One case changed from no treatment to removal of the third molar, since symptoms from the maxillary third molar occurred shortly after the final treatment plan. One case changed from removal of the second molar to removal of the third molar due to a misinterpretation of the final treatment plan by the dentist performing the treatment.
Table 6.
Agreement between the final treatment plan based on CBCT and the actual treatment performed.
|
Treatment Final treatment plan |
No treatment | Removal of a third molar |
Removal of a second molar | Removal of both a second and a third molar |
Total |
|---|---|---|---|---|---|
| No treatment | 61 | 1 a | 0 | 0 | 62 |
| Removal of a third molar | 6 a | 162 | 0 | 0 | 168 |
| Removal of a second molar | 1 a | 1 a | 16 | 0 | 18 |
| Removal of both a second and a third molar | 2 a | 0 | 0 | 10 | 12 |
| Total | 70 | 164 | 16 | 10 | 260 |
Eleven cases with inconsistency between the final treatment plan and the actual treatment performed
Discussion
To the best of the authors’ knowledge, this present prospective cohort study is the first to examine the impact of CBCT on treatment decision for maxillary third molars. Furthermore, this study aimed at identifying clinical and radiographic parameters influencing the treatment decision. It included a large number of patients, which allowed more precise estimates of odds ratios and confidence intervals. The study design ensured that all examinations and treatment plans were performed in a highly systematic set-up. Clinical and radiographic examinations of the patients were performed by the primary investigator and therefore patient records were uniform. The prospective study design ensured that parameters to be examined both clinically and radiographically were determined before inclusion of patients. Relevant parameters were discussed and agreed on in consensus among the authors of this article taking into consideration perspectives from both oral radiologists and oral surgeons. The initial treatment plan was always decided on before evaluation of the CBCT to make sure that findings in CBCT did not influence the initial treatment plan. This reflects the general daily clinical practice.
There are no evidence-based guidelines that state when a CBCT is indicated for evaluation of maxillary third molars, which leaves the usage of CBCT to be based on “good clinical practice” alone. Before guidelines on CBCT related to maxillary third molars can be developed, studies thoroughly examining the topic is needed. Studies on all six levels in the hierarchical model of efficacy for new radiographic modalities suggested by Fryback and Thornbury have to be performed. 11 Studies related to risk factors mainly adds to Level three in the model, whereas studies examining whether the imaging modality changes the treatment plan adds to Level 4. The present study is seen as a Level-4 study. Studies at all six levels examining the usage of CBCT related to impacted maxillary third molars are important to secure that the patient benefits from a CBCT examination since it is coherent with additional radiation to the patient and also economical costs. 11
Treatment plan
The results demonstrated that a CBCT examination supplementing the panoramic image of an impacted maxillary third molar changed the treatment plan in 32% of the cases. In a previous retrospective study, a change in treatment plan was registered in 59% of the cases.7 The studies are not directly comparable, and differences may be related to the fact that the rate of change in treatment plan in the retrospective study could be overestimated, since data was extracted from patient files and not collected in a systematic clinical set-up. Overestimation may occur in cases where the patient file did not clearly state the initial treatment plan based on panoramic imaging, which as a consequence was interpreted as “no treatment”. As such, the plan often changed after CBCT. However, the difference in change could also be related to the fact that the treatment plan was decided by two surgeons in the present study, whereas the retrospective study represented several dentists’/surgeons’ opinions. Furthermore, it was not necessarily the same dentist/surgeon deciding on the initial and the final treatment plan in the retrospective study. Since no guidelines exist on which treatment will benefit the patient best, one could speculate that more surgeons could result in more changes, since their personal experience is different.
When deciding on removal of a third molar compared to no treatment, several parameters seen in panoramic images had a significant impact. Both mesio- and distoangulation of the third molar, presence of marginal bone loss of the second molar together with younger age were all parameters associated with the decision to remove the third molar. Mesioangulation of the third molar has previously been shown to be a risk factor for presence of ERR. 12 This could explain why patients with a mesioangulated third molar were offered removal of the molar to prevent ERR or to arrest superficial ERR of the second molar. Distoangulation has not previously been considered a risk factor. Also presence of marginal bone loss of second molars was associated with removal of a third molar. Marginal bone loss of the second molar adjacent to an impacted third molar could possibly influence the prognosis of the second molar. If the third molar is not removed the marginal bone loss may progress. Within this consideration, removal of third molars causing marginal bone loss seems relevant, although the NICE guidelines do not explicitly mention marginal bone loss of the second molar as an indication for removal of third molars. 9 Superficial ERR seen in CBCT was also a factor that led to the decision to remove a third molar. An explanation for this finding could be that removal of an impacted third molar is presumed to arrest the progression of ERR and thereby improve the long-term prognosis of the second molar. Age, likewise had a significant impact when deciding on removal of a third molar vs no removal. This could be related to the fact that early removal of a third molar is believed to avoid pathology such as ERR, when risk factors such as mesioangulation is present. Furthermore, removal at younger age also favors bony healing after removal the third molar in addition with less occurrence of complications and shorter recovery time. 13,14 However, the NICE guidelines do not state the age group in which third molar removal is most optimal. Removal at older age could be due to symptoms from the area or inflammation in the area caused by insufficient oral hygiene of a partly erupted third molar.
When deciding on removal of the second molar instead of the third molar, this was significantly associated with presence of severe ERR. Severe ERR may affect the long term prognosis of the second molar, 15 therefore removal of the second molar either alone or together with the third molar may be considered. In the present study, the clinicians were 13 times more likely to remove the maxillary second molar instead of the third molar based on ERR findings in a panoramic image and 51 times more likely based on ERR finding in CBCT. This is in accordance with results from a retrospective study where the chance for removal of a maxillary second molar instead of a third molar was almost 17 times as high when severe ERR was present. 7 In addition, a change in treatment plan after CBCT led to removal of the second molar, either together with or without the third molar in 30 cases. Increasing age also had an impact on the initial treatment based on panoramic imaging. In the previous retrospective study, age was not found to be a significant parameter when deciding on removal of the second molar. 7
Treatment
In the majority of cases, the treatment was performed according to the final treatment plan. According to the NICE guidelines, surgical intervention is indicated when ERR is present, since ERR is considered irreversible pathology. 9 Removal of a third molar causing the ERR is believed to arrest the progression of ERR, and no alternatives are suggested in the NICE guidelines regardless of the severity of ERR. A recent prospective study with a limited number of patients investigated the prognosis of the second molar after third molar removal in case of ERR of the second molar.8 They found that second molars with ERR had a high probability of remaining normal pulp vitality after removal of the adjacent third molar. The outcome was not the same as for this study, and therefore results were not comparable since it did not consider alternative treatment options or no treatment in case of ERR. Furthermore, the study did not handle the issue whether CBCT changed the treatment decision or not.
Limitations
There was a strict inclusion criterion in the present study, which was superimposition of the maxillary third molar and second molar with a suspicion of ERR. Therefore, the frequency of ERR in this selected patient population cannot be interpreted as a prevalence of ERR in the general population. Prevalence of ERR related to maxillary third molars still needs to be investigated.
One of the limitations of the present study was the fact, that both radiographic evaluation and treatment planning were performed based on individual experience and preference among the clinicians. Lack of evidence in this area may be one of the reasons why no surgical protocol for maxillary third molars exists. In addition, radiographic assessment was performed by one observer to mimic the daily clinical setting, where a treatment decision needs to be taken for the patient. It is therefore outside the scope of this study to evaluate inter observer reproducibility of the radiographic assessments, but observer variation of the parameters examined in both panoramic images and CBCT can be found in a previous retrospective study. 6
In the future, higher levels in the hierarchy of evidence could be reached through randomized controlled trials (RCT) to evaluate different treatment options in cases with severe ERR. Since this study is not randomized, we cannot provide evidence on which treatment would be the most beneficial to the patient on a long-term basis. It is still uncertain whether the cases that changed treatment based on CBCT have an improved prognosis compared with the initial treatment plan. RCTs with long-term follow-up is needed for further clarification. Before such studies can be put into practice, more information is needed on which radiographic method is to be used, which treatment options should be considered, and which follow-up parameters are meaningful for a given outcome.
Conclusion
The overall conclusion from the present study was that additional information from CBCT changed the treatment plan for maxillary third molar in 32% of cases. Generally, presence of severe ERR had an impact on the final treatment plan. Specific clinical and radiographic findings had an impact on the treatment decision, both for panoramic imaging and CBCT:
Younger age, marginal bone loss of the second molar and third molar mesioangulation, both when seen in panoramic images and CBCT, had an impact on deciding on removal of a maxillary third molar, and moreover superficial ERR seen in CBCT also contributed to this decision.
Severe ERR, both when seen in panoramic images and CBCT, and older age, had an impact on removal of the maxillary second molar instead of, or together with, the third molar. The chance for deciding to remove the second molar, based on the presence of severe ERR, was much higher when this was found in CBCT compared to a panoramic image.
Contributor Information
Louise Hermann, Email: lhp@dent.au.dk.
Sven Erik Nørholt, Email: sven.erik.noerholt@dent.au.dk.
Ann Wenzel, Email: AWENZEL@dent.au.dk.
Pankaj Taneja, Email: pantaneja@dent.au.dk.
Louise Hauge Matzen, Email: louise.hauge.matzen@dent.au.dk.
REFERENCES
- 1. Ventä I, Vehkalahti MM, Huumonen S, Suominen AL. Signs of disease occur in the majority of third molars in an adult population. Int J Oral Maxillofac Surg 2017; 46: 1635–40. doi: 10.1016/j.ijom.2017.06.023 [DOI] [PubMed] [Google Scholar]
- 2. Sarica I, Derindag G, Kurtuldu E, Naralan ME, Caglayan F. A retrospective study: do all impacted teeth cause pathology Niger J Clin Pract 2019; 22: 527–33. doi: 10.4103/njcp.njcp_563_18 [DOI] [PubMed] [Google Scholar]
- 3. European Commision . European guidelines on radiation protection in dental radiology: The safe use of radiographs in dental practice . In: Radiation protection. European Commision; 2004. [Google Scholar]
- 4. Matzen LH, Berkhout E. Cone beam CT imaging of the Mandibular third molar: A position paper prepared by the European Academy of Dentomaxillofacial Radiology (EADMFR). Dentomaxillofac Radiol 2019; 48(): 20190039. doi: 10.1259/dmfr.20190039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Moreira-Souza L, Butini Oliveira L, Gaêta-Araujo H, Almeida-Marques M, Asprino L, Oenning AC. Comparison of Cbct and panoramic radiography for the assessment of bone loss and root Resorption on the second molar associated with third molar Impaction: A systematic review. Dentomaxillofac Radiol 2022; 51(): 20210217. doi: 10.1259/dmfr.20210217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hermann L, Wenzel A, Schropp L, Matzen LH. Marginal bone loss and Resorption of second molars related to Maxillary third molars in panoramic images compared with Cbct. Dentomaxillofac Radiol 2019; 48(): 20180313. doi: 10.1259/dmfr.20180313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hermann L, Wenzel A, Schropp L, Matzen LH. Impact of Cbct on treatment decision related to surgical removal of impacted Maxillary third molars: does Cbct change the surgical approach. Dentomaxillofac Radiol 2019; 48(): 20190209. doi: 10.1259/dmfr.20190209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Qu T, Lai Y, Luo Y, Pan W, Liu C, Cao Y, et al. Prognosis of second molars with external root Resorption caused by adjacent embedded third molars. J Endod 2022; 48: 1113–20. doi: 10.1016/j.joen.2022.06.008 [DOI] [PubMed] [Google Scholar]
- 9. National Institute of Clinical Excellence . Guidance on the extraction of wisdom teeth. London: NICE; 2000. [Google Scholar]
- 10. Ericson S, Kurol PJ. Resorption of Incisors after ectopic eruption of Maxillary Canines: A ct study. Angle Orthod 2000; 70: 415–23. doi: [DOI] [PubMed] [Google Scholar]
- 11. Fryback DG, Thornbury JR. The efficacy of diagnostic imaging. Med Decis Making 1991; 11: 88–94. doi: 10.1177/0272989X9101100203 [DOI] [PubMed] [Google Scholar]
- 12. Ma Y, Mu D, Li X. Risk factors for root Resorption of second molars with impacted third molars: A meta-analysis of Cbct studies. Acta Odontol Scand 2023; 81: 18–28. doi: 10.1080/00016357.2022.2077982 [DOI] [PubMed] [Google Scholar]
- 13. Haug RH, Perrott DH, Gonzalez ML, Talwar RM. The American Association of oral and Maxillofacial Surgeons age-related third molar study. J Oral Maxillofac Surg 2005; 63: 1106–14. doi: 10.1016/j.joms.2005.04.022 [DOI] [PubMed] [Google Scholar]
- 14. Phillips C, Gelesko S, Proffit WR, White RP. Recovery after third-molar surgery: the effects of age and sex. Am J Orthod Dentofacial Orthop 2010; 138: 700. doi: 10.1016/j.ajodo.2010.06.013 [DOI] [PubMed] [Google Scholar]
- 15. Wang HY. Root Resorption associated with impacted Maxillary third molar. Oral Surg Oral Med Oral Pathol 1992; 73: 765–66. doi: 10.1016/0030-4220(92)90025-l [DOI] [PubMed] [Google Scholar]