Abstract
Background
Because of a change of government, the Colombian Ministry of Health and Social Protection is in the process of presenting a structural reform for the General System of Social Security in Health (GSSSH), in order to implement a ‘preventive and predictive health model’. However, it will always be relevant to review and analyze the fiscal implications of any proposed public policy program, to protect financial sustainability and to promote the better functioning of the system in question.
Methods
To contribute to this topic, we have calculated, using a financial–actuarial approach, the loss ratio for the years 2017 to 2021 for the Capitation Payment Unit (CPU) for all the Health-Promoting Entities (HPE) for both contributory and subsidized schemes. This information, derived from public reports available on the official website of the National Health Superintendency, allows us to estimate the financial burden of the institutions that guarantee access to and provision of health services and technologies in Colombia.
Results
The study shows that close to half of the HPEs in Colombia (which represent 11.6 million affiliates) have CPU loss ratios of more than 100% for the year 2021, evidencing insufficient resources for the operation of health insurance.
Conclusions
Finally, we propose some policy recommendations regarding the strengthening of informed decision-making to allow the healthy financial sustainability of the Colombian GSSSH.
Keywords: General System of Social Security in Health, Health-Promoting Entities, Actuarial sciences, Loss ratio, Colombia, Capitation Payment Unit
Introduction
Colombia’s General System of Social Security in Health (GSSSH) was created by Law 100 of 1993 [1], and defines health insurance in article 14 of Law 1122 of 2007 as:
(…) financial risk management, health risk management, articulation of services that guarantee effective access, quality assurance in the provision of health services and the representation of the member before the provider and other actors without prejudice to the autonomy of the user [2].
In Colombia, the companies in charge of these functions are called Health Benefit Plan Administration Entities, and, within these, the Health-Promoting Entities (HPEs) stand out. These are the companies in charge of assuming the risk transferred by the user, guaranteeing the fundamental right to health [3], complying with all the legal provisions of the respective insurance, and having as their ultimate goal the constant improvement of the health of the entire affiliated population.1
Currently, there are two main mechanisms for the financing of the GSSSH and the operation of the HPEs, one ex-ante2 and the other ex-post. The former refers to the Capitation Payment Unit (CPU), an insurance premium that is defined annually by the Ministry of Health and Social Protection on the basis of the age, sex, and region of residence of each affiliate to the HPE, through a pricing method called the loss ratio [4]. This monetary amount is the amount that the GSSSH resource administrator gives to each HPE to guarantee the provision of health services and technologies (HSTs) financed by the CPU to its entire pool of risks [5]—all GSSSH affiliates are entitled to the same set of HSTs, regardless of their HPE. The ex-post mechanism is a zero-sum adjustment according to the results of the HPE risk management for the following health conditions: chronic kidney disease, arterial hypertension, diabetes mellitus, HIV, and cancer. This is done by the High Cost Account, which is the entity responsible for the calculation and application of this resource redistribution mechanism [6].3
By 2022, the HST charged to the CPU represented more than 84% of the total expenditure in the GSSSH, approximately 62.4 billion Colombian pesos [7]. Likewise, it is important to highlight that 96.9% of health procedures and 93.7% of medicines approved and available for use in the country are currently fully financed with CPU resources [5].
Within the framework of social health insurance, if the CPU is conceived of as an insurance premium, its financial sufficiency is vital for the sustainability of the GSSSH in the short, medium, and long term (given the aging of the population, the increase in life expectancy, pharmacological innovations, the updating of health benefit plans, etc.). Therefore, each year the Ministry of Health and Social Protection must estimate a rate consistent with the future demand for HST that allows, in a supportive and comprehensive manner, the fundamental right to health of all affiliates to be guaranteed.
According to article 23 of Law 1438 of 2011, an HPE’s administration expenses cannot exceed 8% or 10% of the CPU for subsidized4 (SS) or contributory5 (CS) schemes, respectively. Therefore, the loss ratio, actuarially conceptualized as the cost of the set of events that have already materialized and that are covered by the insurance, cannot be less than 92% in the SS and 90% in the CS [8]. Although having a claim rate close to or greater than 100% is not adequate for financial solvency, neither is having a very low claim rate, since health insurers must invest part of their premium in the promotion of the health and prevention of illness of their members, as well as improving the efficiency and quality of care [9]. This investment fosters a positive result from two perspectives: (i) the maintenance of the health of the population of interest, and (ii) the reduction of future avoidable health conditions, especially in the medium and long term.
In recent decades at the international level, the calculation methodology and the regulatory aspects of health loss ratios for insurers have been a topic of priority interest in public supervision policy [10, 11]. The region with the greatest scientific production in this regard is North America [9, 12–16], although work has also been done for European [17], Asian [18, 19], and African [20] nations. In countries like the United States, Israel, the Netherlands, Vietnam, South Africa, Germany, Denmark, and Spain, among others, the medical loss ratio is between 49% and 92%. These values represent a wide range, since most of the health insurance in these countries is private, differing from the conceptual framework for the CPU in Colombia of social insurance.
In Colombia, the Ministry of Health and Social Protection has, for more than two decades, published an annual sufficiency report for the CPU, in which an analysis of the loss ratio is shown; however, this analysis is not carried out for all the HPEs in the GSSSH but only for those selected at the discretion of the Ministry [21].6 Outside the governmental sphere, only two approaches to the calculation the loss ratio have been published. In 2021, the Colombian Association of Comprehensive Medicine Companies (ACEMI, by its Spanish acronym), one of the HPE's guilds, estimated the loss ratio for both schemes, but the technical development of this report is not publicly available, and nor is its methodology, meaning that it is not transparent or replicable but is merely a ‘black box’ [22]. Subsequently, in 2023 NUMERIS estimates the loss ratio only for the contributory scheme, and although they show the methodology in a very aggregated way, they did not specify the financial sub-accounts analysed for the calculation [23].
This research article calculates the CPU loss ratio for all HPEs in the country in the contributory and subsidized schemes, between 2017 and 2021, to provide empirical evidence on the current financial conditions of HPEs in Colombia, in such a way as can nourish the debate on the options for improvement in insurance finances in the Colombian health system.
Methodology and data
The CPU loss ratio , according to the context of the GSSSH and the definition used in the actuarial sciences [24–27], is understood as a measure of the proportion of each monetary unit received as income within the concept of the CPU that is used to pay for the HST incurred under the CPU.
In formal terms, it is calculated as: 7:
| 1 |
where is the year in the analysis and is the HPE of interest.
The data needed to calculate the of the different HPEs (both SS and CS), were extracted from the technical annex FT001—Financial information catalog for supervisory purposes [28], provided on the website of the National Health Superintendency, between 2017 and 2021. In Table 1 the different HPEs are presented by scheme and classification according to the International Financial Reporting Standards (IFRS) or Public Accounting Regime (PAR). The table shows that, for the different years, the HPEs analyzed in this study together cover—on average—99% of the population affiliated with the GSSSH (more than 44 million people, on average per year).
Table 1.
Number of affiliates per HPE (expressed in hundred thousand) according to scheme and IFRS/PAR classification, years 2017 to 2021
| Classification | Authorized/enabled scheme | HPE | 2017 | 2018 | 2019 | 2020 | 2021 |
|---|---|---|---|---|---|---|---|
| IFRS 1 | Contributory | Aliansalud | 2.05 (0.47%) | 2.11 (0.48%) | 2.25 (0.49%) | 2.34 (0.51%) | 2.40 (0.49%) |
| Compensar | 13.27 (3.03%) | 14.27 (3.22%) | 15.44 (3.38%) | 17.34 (3.76%) | 19.43 (3.96%) | ||
| Coomeva | 26.38 (6.02%) | 22.68 (5.12%) | 18.75 (4.1%) | 15.61 (3.38%) | 13.28 (2.71%) | ||
| Sanitas | 19.19 (4.38%) | 23.07 (5.2%) | 28.12 (6.15%) | 34.82 (7.54%) | 42.80 (8.73%) | ||
| Sura | 25.77 (5.88%) | 29.15 (6.58%) | 34.26 (7.49%) |
38.98 (8.44%) |
44.37 (9.05%) |
||
| Subsidized | CCF de Nariño–Comfamiliar Nariño | 1.84 (0.42%) | 1.83 (0.41%) | 1.85 (0.4%) | 1.82 (0.39%) | 1.71 (0.35%) | |
| CCF del Huila–Comfamiliar Huila | 5.24 (1.2%) | 5.73 (1.29%) | 5.71 (1.25%) | 5.58 (1.21%) | 5.50 (1.12%) | ||
| Mixed | Asociación Mutual Ser Empresa Solidaria de Salud–Mutual Ser | 14.78 (3.37%) | 15.90 (3.59%) | 18.82 (4.11%) | 21.10 (4.57%) | 23.19 (4.73%) | |
| IFRS 2 | Contributory | Comfenalco Valle | 2.41 (0.55%) | 2.34 (0.53%) | 2.31 (0.5%) | 2.39 (0.52%) | 2.57 (0.52%) |
| Cruz Blanca | 4.96 (1.13%) | 4.33 (0.98%) | 2.94 (0.64%) | 0 (0%) | 0 (0%) | ||
| Famisanar | 18.84 (4.3%) | 20.32 (4.58%) | 22.49 (4.92%) | 24.75 (5.36%) | 26.67 (5.44%) | ||
| Fundación Salud Mía | 0 (0%) | 0.04 (0.01%) | 0.17 (0.04%) | 0.35 (0.08%) | 0.47 (0.1%) | ||
| Salud Total | 24.69 (5.64%) | 26.68 (6.02%) | 29.63 (6.48%) | 34.17 (7.4%) | 38.88 (7.93%) | ||
| Servicio Occidental de Salud–S.O.S | 9.30 (2.12%) | 9.21 (2.08%) | 8.70 (1.90%) | 8.31 (1.80%) | 8.18 (1.67%) | ||
| Subsidized | Asociación Barrios Unidos de Quibdó—AMBUQ | 8.73 (1.99%) | 8.30 (1.87%) | 7.91 (1.73%) | 7.71 (1.67%) | 7.69 (1.57%) | |
| Asociación Mutual Empresa Solidaria de Salud de Nariño—EMSSANAR | 19.08 (4.35%) | 19.15 (4.32%) | 19.07 (4.17%) | 19.14 (4.15%) | 19.41 (3.96%) | ||
| Asociación Mutual la Esperanza—ASMET Salud | 19.30 (4.40%) | 19.02 (4.29%) | 18.86 (4.12%) | 18.92 (4.10%) | 19.37 (3.95%) | ||
| CCF Cajacopi Atlántico | 7.82 (1.79%) | 8.74 (1.97%) | 10.05 (2.20%) | 11.43 (2.48%) | 12.82 (2.62%) | ||
| CCF de Cartagena—Comfamiliar Cartagena | 1.96 (0.45%) | 1.73 (0.39%) | 1.52 (0.33%) | 1.38 (0.30%) | 0 (0%) | ||
| CCF de Córdoba—Comfacor | 5.77 (1.32%) | 5.51 (1.24%) | 5.39 (1.18%) | 0 (0%) | 0 (0%) | ||
| CCF de Cundinamarca—Comfacundi | 1.25 (0.29%) | 1.23 (0.28%) | 1.66 (0.36%) | 1.63 (0.35%) | 0 (0%) | ||
| CCF de la Guajira—Comfaguajira | 2.07 (0.47%) | 2.25 (0.51%) | 2.27 (0.50%) | 2.46 (0.53%) | 2.57 (0.52%) | ||
| CCF de Sucre—Comfasucre | 1.14 (0.26%) | 1.19 (0.27%) | 1.16 (0.25%) | 1.16 (0.25%) | 1.18 (0.24%) | ||
| CCF del Chocó—Comfachocó | 1.61 (0.37%) | 1.75 (0.39%) | 1.74 (0.38%) | 1.75 (0.38%) | 1.78 (0.36%) | ||
| CCF del Oriente Colombiano—Comfaoriente | 1.12 (0.26%) | 1.22 (0.28%) | 1.37 (0.30%) | 1.83 (0.40%) | 1.95 (0.40%) | ||
| Comparta | 17.79 (4.06%) | 17.39 (3.92%) | 16.21 (3.54%) | 15.37 (3.33%) | 15.25 (3.11%) | ||
| Ecoopsos | 2.97 (0.68%) | 3.03 (0.68%) | 3.23 (0.71%) | 3.27 (0.71%) | 3.32 (0.68%) | ||
| Empresa Mutual para el Desarrollo Integral de la Salud—Emdisalud | 4.62 (1.05%) | 4.59 (1.04%) | 4.06 (0.89%) | 0 (0%) | 0 (0%) | ||
| Mixed | Cooperativa de Salud y Desarrollo Integral Zona Sur Oriental de Cartagena—COOSALUD | 19.61 (4.47%) | 20.46 (4.62%) | 22.71 (4.97%) | 26.10 (5.66%) | 29.62 (6.04%) | |
| Medimás | 47.55 (10.85%) | 42.67 (9.62%) | 35.55 (7.77%) | 25.28 (5.48%) | 16.04 (3.27%) | ||
| Nueva EPS | 42.35 (9.66%) | 46.15 (10.41%) | 52.75 (11.53%) | 67.07 (14.53%) | 79.70 (16.26%) | ||
| SaludVida | 12.87 (2.94%) | 12.17 (2.75%) | 11.55 (2.52%) | 0 (0%) | 0 (0%) | ||
| PAR 6 | Contributory | Empresas Públicas de Medellín—Departamento Médico | 0.10 (0.02%) | 0.10 (0.02%) | 0.09 (0.02%) | 0.09 (0.02%) | 0.08 (0.02%) |
| PAR 7 | Subsidized | Anas Wayuu (Indígena) | 1.72 (0.39%) | 1.85 (0.42%) | 1.94 (0.42%) | 2.07 (0.45%) | 2.17 (0.44%) |
| Asociación Indígena del Cauca—AIC (Indígena) | 4.66 (1.06%) | 4.78 (1.08%) | 5.01 (1.09%) | 5.34 (1.16%) | 5.43 (1.11%) | ||
| Asociación Indígena del Cesar y La Guajira Dusakawi (Indígena) | 1.97 (0.45%) | 2.08 (0.47%) | 2.26 (0.49%) | 2.37 (0.51%) | 2.50 (0.51%) | ||
| Capital Salud | 11.62 (2.65%) | 11.62 (2.62%) | 11.28 (2.47%) | 11.36 (2.46%) | 11.69 (2.38%) | ||
| Capresoca | 1.77 (0.40%) | 1.79 (0.40%) | 1.75 (0.38%) | 1.72 (0.37%) | 1.74 (0.35%) | ||
| Convida | 5.60 (1.28%) | 5.50 (1.24%) | 5.38 (1.18%) | 5.20 (1.13%) | 5.03 (1.03%) | ||
| Mallamás (Indígena) | 3.04 (0.69%) | 3.13 (0.71%) | 3.21 (0.70%) | 3.29 (0.71%) | 3.42 (0.70%) | ||
| Pijaos Salud (Indígena) | 0.80 (0.18%) | 0.84 (0.19%) | 0.88 (0.19%) | 0.94 (0.20%) | 0.99 (0.20%) | ||
| Savia Salud | 16.71 (3.81%) | 17.04 (3.84%) | 16.74 (3.66%) | 16.84 (3.65%) | 16.62 (3.39%) | ||
| PAR 8 | Contributory | Fondo de Pasivo Social de los Ferrocarriles Nacionales | 0.41 (0.09%) | 0.40 (0.09%) | 0.38 (0.08%) | 0.37 (0.08%) | 0.35 (0.07%) |
| Percentage of all people affiliated to the GSSSH | 93.79% | 100% | 100% | 100% | 100% | ||
CCF: Family Compensation Fund; (ii) a mixed scheme refers to an HPE that is qualified/authorized to operate in both schemes (CS and SS); (iii) in parentheses the percentage of affiliates to the total number affiliated to the GSSSH for that year is shown
Next, we proceed to explain in detail the construction of the factors of Eq. (1), based on the available financial information for the HPEs disclosed by the National Health Superintendency. In the first measure, for the numerator, the costs for health care financing with the CPU for the CS and SS are derived from the financial sub-accounts displayed in Tables 2 and 3 (segmented according to IFRS and PAR group by financial catalog FT001).
Table 2.
Financial sub-accounts of CPU costs for the contributory scheme according to IFRS or PAR group
| IFRS 1 and 2 | |||||||
|---|---|---|---|---|---|---|---|
| Financial sub-accounts | Cost of technical reservesa—Settled pending payment—Health services | Cost of technical reserves—Known unliquidated—Health services | Cost of technical reserves—Pending unknown—Health services | Contracts for promotion and prevention activities | Catastrophic illnesses and high-cost illnesses | Other reserves | Cost of provision of services from own providers |
| Financial catalog AT FT001 | 61020101 61020301 | 61020401 61020601 | 61021001 61021201 | 61021301 | 61021401 | 61021501 | 61050101 |
| PAR 6, 7 and 8 | |||||
|---|---|---|---|---|---|
| Public entities before resolution 427 of 2019 of the general accounting of the nation (years 2017 to 2019) | Public entities after resolution 427 of 2019 of the general accounting of the nation (the year 2020) | Public entities after resolution 223 of 2020 of the general accounting of the nation (the year 2021) | |||
| Capitation contracts—Contributory | 561301 | Capitation contracts—Contributory | 561301 | Promotion and prevention—Contributory | 561303 |
| Contracts by event and other modalities—Contributory | 561302 | Contracts by event and other modalities—Contributory | 561302 | Guarantee and quality system—Contributory | 561304 |
| Promotion and prevention—Contributory | 561303 | Promotion and prevention—Contributory | 561303 | High-cost disease reinsurance—Contributory | 561305 |
| Guarantee and quality system—Contributory | 561304 | Guarantee and quality system—Contributory | 561304 | Technical reserve for known unpaid health services and technologies, financed with the CPU | 537201 |
| High-cost disease reinsurance—Contributory | 561305 | High-cost disease reinsurance—Contributory | 561305 | Technical reserve for health services and technologies that have occurred and are not known | 537202 |
| Technical reserves for authorized health services | 561320 | Technical reserves for authorized health services | 537201 | Other provisions for health services and technologies | 537290 |
| Technical reserves for unknown health services occurred | 561321 | Technical reserves for unknown health services occurred | 537202 | ||
| Other technical reserves | 561323 | Other provisions for health services | 537290 | ||
aThe technical reserves can be understood as a provision that will guarantee the payment for the HST provided to the affiliates of the HPE, which is a legal requirement defined by the National Health Superintendency
Table 3.
Financial sub-accounts of CPU costs for the subsidized scheme according to IFRS or PAR group
| IFRS 1 and 2 | |||||||
|---|---|---|---|---|---|---|---|
| Financial subaccounts | Cost of technical reserves—Settled pending payment—Health services | Cost of technical reserves—Known unliquidated—Health services | Technical reserve cost—Unknown pending—Health services | Contracts for promotion and prevention activities | Catastrophic illnesses and high-cost illnesses | Other reserves | Cost of provision of services from own providers |
| Financial catalog AT FT001 | 61020102 61020302 | 61020402 61020602 | 61021002 61021202 | 61021302 | 61021402 | 61021502 | 61050102 |
| PAR 6, 7 and 8a | |||||
|---|---|---|---|---|---|
| Public entities before Resolution 427 of 2019 of the General Accounting of the Nation (years 2017 to 2019) | Public entities after Resolution 427 of 2019 of the General Accounting of the Nation (the year 2020) | Public entities after Resolution 223 of 2020 of the General Accounting of the Nation (the year 2021) | |||
| Capitation contracts—Subsidized | 561307 | Capitation contracts—Subsidized | 561307 | Promotion and prevention—Subsidized | 561309 |
| Contracts by event and other modalities—Subsidized | 561308 | Contracts by event and other modalities–Subsidized | 561308 | Guarantee and quality system—Subsidized | 561310 |
| Promotion and prevention—Subsidized | 561309 | Promotion and prevention—Subsidized | 561309 | High-cost disease reinsurance—Subsidized | 561311 |
| Guarantee and quality system—Subsidized | 561310 | Guarantee and quality system—Subsidized | 561310 | Technical reserve for known unpaid health services and technologies, financed with the CPU | 537201 |
| High-cost disease reinsurance—Subsidized | 561311 | High-cost disease reinsurance—Subsidized | 561311 | Technical reserve for health services and technologies that have occurred and are not known | 537202 |
| Technical reserves for authorized health services | 561320 | Technical reserves for authorized health services | 537201 | Other provisions for health services and technologies | 537290 |
| Technical reserves for unknown health services occurred | 561321 | Technical reserves for unknown health services occurred | 537202 | Other expenses for the administration of social security in health | 561390 |
| Other technical reserves | 561323 | Other provisions for health services | 537290 | ||
| Other expenses for the administration of social security in health | 561390 | Other expenses for the administration of social security in health | 561390 | ||
aIn public catalogs (AT-FT001-06, AT-FT001-07, AT-FT001-08) it is not possible to determine, in the sub-accounts related to technical reserves, whether those are from the SS or the CS, and therefore this should be considered in accordance with the authorized/enabled regime of the study HPE
We consider that the release of reserves,8 although it is part of the income account (non-operational), should be read as a minor cost since it directly impacts technical reserves. Therefore, the sum of the costs must be subtracted from the monetary values consigned to the financial sub-accounts related to the release of technical reserves, so that for the HPEs in IFRS 1 and 2 the following three financial sub-accounts must be taken: (i) 410204 (‘Release of technical reserves—Pending and known obligations’), (ii) 410205 (‘Release of technical reserves—Unknown outstanding obligations’) and (iii) 410206 (‘Release of technical reserves—Other reserves’); while for the HPEs in IFRS 6, 7 and 8 this corresponds to the financial sub-account 435508 (‘Release of technical reserves’). These financial items should theoretically be used when reserves from previous periods are released instead but, in practice, they have been used in the current release, so that fact should be reflected as a lower cost and not as income.
Secondly, the denominator is the CPU income for the HPE resulting from the sum of the financial sub-accounts presented in Table 4, according to its IFRS or PAR group, and according to the financial catalog AT FT001.
Table 4.
CPU income financial sub-accounts for the contributory and subsidized schemes according to IFRS or PAR group
| Contributory scheme | |||||
|---|---|---|---|---|---|
| Financial catalog AT FT001 | Financial sub-accounts | ||||
| Capitation Payment Unit–CPU | Additional CPUa | Payment unit for promotion and prevention activities | Moderator fees | Copays | |
| IFRS 1 and 2 | 41020101 | 410202 | 410203 | 41020801 | 41020901 |
| PAR 6, 7 and 8 | 431101 | 431102 | 431122 | 431103 | 431104 |
| Subsidized scheme | ||
|---|---|---|
| Financial catalog AT FT001 |
Financial sub-accounts | |
| Capitation Payment Unit–CPU | Copays | |
| IFRS 1 and 2 | 41020102 | 41020902 |
| PAR 6, 7 and 8 | 431106 | 431107 |
aThis sub-account corresponds to an additional premium that is delivered to the HPE by affiliates residing in certain municipalities due to geographic dispersion and low population density, in order to cover cost overruns in health care
For the SS and CS, the financial sub-accounts related to disabilities, complementary care plans, and maximum budgets were excluded from the analysis, since these are not charged to the CPU.
On the other hand, the estimation takes into account what is referred to as mobility between schemes. This aspect is important for calculating the loss ratio due to the HPE in the GSSSH, because it impacts a particular financial fact: an HPE authorized/enabled to operate in the CS may have members of the SS, and therefore resources associated with this latter health scheme [29]. Likewise, an SS HPE may have CS affiliates, with their respective financial resources.
The foregoing follows the provisions of article 2.1.1.3 of Decree 780 of 2016, which defines ‘(…) the change of belonging to a scheme within the same HPE for affiliates in the General System of Social Security in Health focused on levels I and II of the SISBEN [Identification System for Potential Beneficiaries of Social Programs] and some special populations’ [30]. This mechanism allows continuity of insurance for vulnerable people, so that if, for example, a person belonging to the CS lost their ability to pay, they would move to the SS, but would continue to be affiliated with the same HPE.
Therefore, Eq. (1) is redefined as follows:
| 2 |
In this way, it is possible to consolidate the financial information9 necessary to properly calculate the
Results
For the HPEs in the IFRS 1 and IFRS 2 categories, more than 80% of the costs are associated with ‘Cost of technical reserves—Settled pending payment—Health services’ (71.41% annual average) and ‘Catastrophic illnesses and high-cost illnesses’ (9.50% annual average), which have been increasing during the analysis period. In monetary terms, the two sub-accounts with the highest growth rates between 2017 and 2021 are ‘Technical reserve cost—Unknown pending—Health services’ and ‘Cost of technical reserves—Known unliquidated—Health services’, which have increased10 by 280.05% and 201.13%, respectively. The ‘Other reserves’ sub-account is, from 2020, one of the ones with the lowest participation in costs and the only one that has decreased, going from $2.06 trillion in 2017 to $240 billion Colombian pesos in 2021.
On the other hand, for the HPEs in the PAR 6, PAR 7, and PAR 8 categories, between 2017 and 2020 close to 80% of the costs were concentrated in ‘Contracts per event and other modalities’ (55.90% annual average) and ‘Capitation contracts’ (32.19% annual average); however, in 2021 there was a change, with ‘Other expenses for the administration of social security in health’ being the highest cost, going from a share of 7.48% of total costs in 2017 to 72.10% in 2021. The account with the greatest variation is the ‘Guarantee and quality system’, which increased its monetary amount by more than 50 times in the analysis period, going from $4.86 billion in 2017 to $363.33 billion Colombian pesos in 2021.
Regarding the income related to the CPU, both for the HPEs in the IFRS 1 and 2 categories and those in the PAR 6, 7, and 8 categories, about 97% of the income corresponds to the ‘Capitation Payment Unit—CPU’, which is foreseeable given the logic of this financial item. Regarding the release of reserves, the results identify that this is done only by HPEs in the IFRS 1 and IFRS 2 categories, with the sub-account ‘Release technical reserves—Pending and known obligations’ being the one with the highest share of the total releases (85.42% annual average). These releases represent, on average, 2.73% of the costs.
The GSSSH of Colombia has a decrease in its loss ratio between 2018 and 2020, going from 97.59% to 93.82%; however, in 2021 there is an increase of 5.25 percentage points (p.p.), with the ratio reaching 99.07%. When estimating the aggregate CPU11 loss ratio by the scheme, the SS shows a decrease of 11.79 p.p., going from 102.70% in 2017 to 90.91% in 2020; however, this trend is reversed in 2021, when there is an increase of 6.44 p.p. to a loss ratio of 97.35%. For its part, the CPU claims ratio of the CS, in general, has increased over the period, from 90.51% in 2017 to 100.54% in 202112, which implies an increase of 10.03 p.p. It is noteworthy that, except for the CS in 2017, the estimated here has been higher than the minimum value regulated by the Ministry of Health and Social Protection (Fig. 1).
Fig. 1.
CPU loss ratio by scheme, 2017–2021. CPU Capitation Payment Unit, CS Contributory scheme, SS Subsidized scheme, GSSSH General System of Social Security in Health
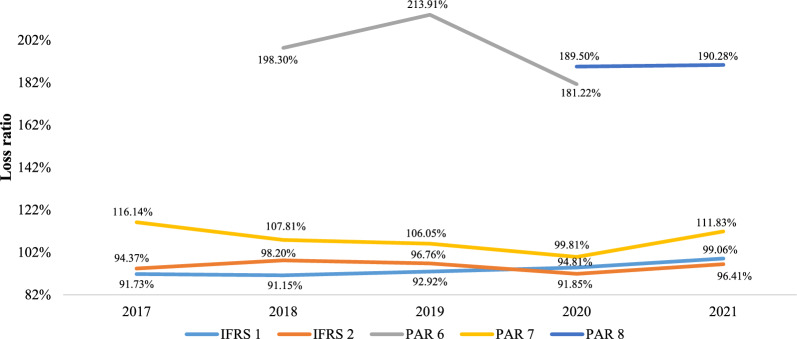
According to the type of accounting that is carried out, and taking into account the nature of the HPEs, it can be observed that the loss ratio of the HPEs of the PAR 6, PAR 7, and PAR 8 categories is, throughout the analysis period, superior to the rest, and in some cases, is almost double the index for the HPEs of the IFRS 1 and IFRS 2 categories (Fig. 2). This difference is because the HPEs that belong to the PAR 6 and PAR 8 categories, EPM Empresa Pública de Medellín and Fondo de Pasivo Social de los Ferrocarriles Nacionales, respectively, are institutions whose corporate purpose is not health insurance (they are so-called adapted health entities), so that only their own workers and beneficiaries are affiliates, they have a regressive population pyramid (a high proportion of people in old age), and they have high capitalization and operation costs and financial insolvency [31].
Fig. 2.
CPU loss ratio by IFRS and PAR category, 2017–2021. IFRS International Financial Reporting Standards, PAR Public Accounting Regime
Table 5 shows the calculation of the for each entity for the different years of study (2017–2021), from which one can observe that, on average, the loss ratio of 44.19% of the insurance entities analyzed exceed 100%. Given the previously mentioned characteristics of EPM Empresa Pública de Medellín and Fondo de Pasivo Social de los Ferrocarriles Nacionales, it is evident that these two companies have the highest loss ratios. It should be noted that all the companies whose affiliates are original indigenous populations had, at least one moment of the analysis period, indices above 100%. Likewise, firms whose loss ratio has presented greater variations between 2017 and 2021 are authorized/enabled to operate in the SS (Emdisalud, Savia Salud, Comfamiliar Nariño, Pijaos Salud and Comfacundi).
Table 5.
CPU loss ratio (%) by HPE (including mobility), 2017–2021
Red: higher than 100%; green: between the legal minimum according to the scheme (90% for HPE operating in the CS and 92% for HPE operating in the SS and mixed) and 100%; grey: lower than the imposed legal minimum; orange: no information (N.I.) – either because the HPE’s information report is inconsistent or because it is in liquidation
1Available information as of September 2021
2Available information as of September 2020
3Available information as of September 2020
4Available information as of March 2021
Discussion and conclusions
Every health system must have, as its most important premise, the maximization and improvement of the health results of the general population, and thus must be aiming for the financial sustainability of the different actors (patients, government, providers, insurers, pharmaceutical companies, etc.) in a way that allows a sustainable, relevant, and orderly performance within clear institutional rules.
This research article estimated the loss ratios, considering the CPU concept, for more than 40 HPEs of the GSSSH of Colombia in the five years between 2017 and 2021. The results obtained in this investigation show that in the most recent year analyzed, a large proportion of the HPEs (with 66.60% of the affiliated population as of 2021) had a CPU loss ratio greater than 95%, leaving little room for administrative expenses and, in some periods, income for their proper operation that was insufficient to guarantee the fundamental right to health (as was the case for the CS added for the year 2021). In addition, it was found that the COVID-19 pandemic had a downward impact on the behavior of the index for SS in 2020, due to the dispersion and natural physical distance in scattered rural areas [32].
On the other hand, several HPEs exhibit CPU loss ratios greater than 100%, with the maximum values being obtained in the SS. As the two schemes have populations with completely different risk profiles [33], there is an urgent need to use this information for an actuarial estimation of the CPU of the SS (to which more than 24 million people belong), since the Ministry of Health and Social Protection has generally made decisions regarding its growth based on whatever happens with the behavior of the CS, as was the case in 2023.
The heterogeneity of the loss ratios may reflect divergences in the efficiency of risk management due to socio-demographic differences in their population groups, different contracting models with their network of health service providers, and inequities in the structure and availability in the supply of health services, among other systematic factors. That is why, for any new reform to the GSSSH that may be proposed, it will be essential to consider the future fiscal impact of the new health care models, as well as strengthening the supervision systems, in order to determine the effects of spending on the population health outcomes. The National Health Superintendency must play a fundamental and active role in monitoring HPE risks, a mission that up to now it has not been able to fulfill completely [34].
Likewise, it will be key that, in the debate on the future reform of the GSSSH, such important issues are addressed as the maximum value of the margin of administration by the HPE (depending on different parameters, such as size, among other characteristics), the maximum limit of 30% of the health expense of an HPE of the CS in its network of providers (Art. 15 of Law 1122 of 2007) [2], and the obligation for an SS HPE to contract a minimum of 60% of its health expenses with public providers (Art. 16 of Law 1122 of 2007) [2], among others. All these thresholds are established in the legislation of the health sector in Colombia, and impact in one way or another the comprehensive risk management of the HPE and therefore the financial sustainability of the GSSSH, and they will have to be reformulated based on scientific studies and evidence from the real contexts of these entities.
The findings set out above require caution in their reading, since they approximate a methodological proposal that provides empirical evidence on HPE loss ratios but are not the only way in which these could be calculated. The interpretation of these results must be framed under the limitations given by Robinson [35] in calculating loss ratios in health, which include: (i) these ratios are subject to somewhat arbitrary accounting conventions 13; (ii) these ratios are not the only valid measure of financial performance; (iii) low or high values are not necessarily good or bad, since the conclusion depends on the nature of the insurer and the context of the health system, and (iv) the loss ratio alone does not indicate the quality of health care.
In this way, for example, the fact that the financial policies for the accrual of health spending by CPU may vary from one HPE to another in Colombia should be taken into account. In future, the Ministry of Health and Social Protection and the National Health Superintendency could strengthen the calculation of this index through joint work with the HPEs, allowing the estimation of technical reserves and their impact on the calculated loss ratio to be homologated in a certain way. Likewise, the Ministry of Health and Social Protection should work to develop better methodological proposals for CPU pricing (for example, including health conditions or improving the accuracy of demographic forecasts) that allow a minimum financial sufficiency and avoid indebtedness and an unsustainable increase in portfolio for the health insurers. Finally, as a future line of research, the authors consider that the minimum solvency requirements required for HPEs should be studied; this is a path recently started by National Health Superintendency, but there is a long way to the horizon.
Acknowledgements
The authors thank Wynand van de Ven, Cristina Gutiérrez, Fernando Mesquida, Daniel Pinzón, Mery Bolívar, Johnattan García, Mauricio Martínez, Gabriela Puentes, Juan Vargas, Ana Cipagauta and Lorena Mesa, as well as officials and former officials (both managers and technicians) of the Ministry of Health and Social Protection, the National Health Superintendency, Health-Promoting Entities of the contributory and subsidized schemes, guilds, and other health sector entities, for their valuable and useful comments on previous versions of this research document. In addition, Oscar Espinosa thanks several members of the Society of Actuaries for their feedback on this document, including Greg Herrle, Josh Collins, Merideth Randles, and Jorge Torres.
Abbreviations
- CPU
Capitation Payment Unit
- CS
Contributory scheme
- GSSSH
General System of Social Security in Health
- HPE
Health-Promoting Entities
- IFRS
International Financial Reporting Standards
- PAR
Public Accounting Regime
- SS
Subsidized scheme
Author contributions
OE: conception and design of the work, data collection, data analysis and interpretation, drafting the article, critical revision of the article, final approval of the version to be submitted. JR: data collection, data analysis and interpretation, drafting the article, critical revision of the article, final approval of the version to be submitted. BPU, PLDN, EV: data analysis and interpretation, drafting the article, critical revision of the article, final approval of the version to be submitted. AS, MLA, TC, SF: drafting the article, critical revision of the article, final approval of the version to be submitted.
Funding
None.
Availability of data and materials
The datasets and programming codes used, generated, and analyzed during the current study are available in https://github.com/Jonavier/Loss_Ratio_CPU.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors agree with the content of this manuscript.
Competing interests
None.
Footnotes
The results obtained in this research are the sole responsibility of the authors and not of the institutions with which they are linked.
There is another ex-ante mechanism called maximum budgets, through which health services and technologies not covered by the CPU are financed. However, in terms of health expenses for 2022, these represented less than 5% of the total GSSSH.
The transfers received by the High Cost Account from the HPEs originate in the CPU, and the HPEs that benefit from these resources record these entries as operating income [29].
The subsidized scheme is the mechanism through which the most socio-economically vulnerable members of the population have access to health services based on subsidies offered by the state [36].
The contributory scheme is the mechanism through which individuals access the GSSSH through the payment of an individual and family contribution, or a previous economic contribution financed directly by the affiliate or by agreement between the latter and their employer [37].
For more details, see the website of the Ministry of Health and Social Protection, where it is possible to review the different studies developed on HPE spending, under the subsection ‘Estudio de Suficiencia’, since 2006.
This, framed from an approach of incurred claims, technically determines the sum of paid claims plus the constitution of reserves.
In public catalogs it is not possible to determine, in the sub-accounts related to release of reserves, whether those are from the SS or the CS, and therefore this should be considered in accordance with the authorized/enabled regime of the study HPE. In the case of mixed HPEs, the distribution of the reserve release amount for each of the regimes is based on the distribution of the number of affiliates in each regime for the HPE of interest.
The data used were those reported by the HPE in the financial catalog FT001, and no adjustment was made to homogenize the applied measurement bases. The authors consider this topic an important opportunity for improvement that should be addressed by the Ministry of Health and Social Protection and the National Health Superintendency in relation to accounting standardization throughout the health insurance sector in the country.
Variations are calculated with deflated monetary amounts at 2021 prices.
For this case, the sub-accounts belonging to the SS (Table 3) of all HPEs are added, regardless of whether or not the entities are authorized/enabled to operate in the SS. The same reasoning applies in the case of the aggregate CPU loss ratio of the CS.
This provides evidence that, on average and according to the figures reported by the National Health Superintendency, the costs for the HPEs, once the release of reserves is excluded, are growing more quickly than their income with regard to the set of HSTs financed by the CPU.
In recent years, some authors have studied the impact of this type of potential bias in financial reporting, for more details see Fang et al. and Samuels et al. [38, 39].
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Congreso de la República de Colombia. Ley 100 de 1993 “Por la cual se crea el sistema de seguridad social integral y se dictan otras disposiciones”. Bogotá, D.C; 1993. https://www.funcionpublica.gov.co/eva/gestornormativo/norma.php?i=5248
- 2.Congreso de la República de Colombia. Ley 1122 de 2007 “Por la cual se hacen algunas modificaciones en el Sistema General de Seguridad Social en Salud y se dictan otras disposiciones”. Bogotá, D.C.; 2007. https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/DIJ/ley-1122-de-2007.pdf
- 3.Congreso de la República de Colombia. Ley Estatutaria de Salud 1751 de 2015 “Por medio de la cual se regula el derecho fundamental a la salud y se dictan otras disposiciones” [Internet]. Bogotá, D.C.; 2015. https://www.minsalud.gov.co/Normatividad_Nuevo/Ley1751de2015.pdf
- 4.Ministerio de Salud y Protección Social. Estudio de suficiencia y de los mecanismos de ajuste del riesgo para el cálculo de la Unidad de Pago por Capitación del año 2022. Bogotá, D.C. Ministerio de Salud y Protección Social; 2021. https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VP/DOA/estudio-suficienciaupc2022.pdf
- 5.Ministerio de Salud y Protección Social. 2022 Informe al Congreso de la República 2021/2022. Bogotá, D.C. Ministerio de Salud y Protección Social.
- 6.Cuenta de Alto Costo (CAC). Líneas de acción. 2022. https://cuentadealtocosto.org/site/quienes-somos/lineas-de-accion/. Accessed Dec 28 2022.
- 7.Administradora de los Recursos del Sistema General de Seguridad Social en Salud. Unidad de recursos administrados (URA). https://www.adres.gov.co/nuestra-entidad/informacion-financiera/unidad-de-recursos-administrados-ura/presupuesto. Accessed 18 Dec 2022.
- 8.Congreso de la República de Colombia. Ley 1438 de 2011 “Por medio de la cual se reforma el Sistema General de Seguridad Social en Salud y se dictan otras disposiciones”. Bogotá, D.C.; 2011. https://www.minsalud.gov.co/Normatividad_Nuevo/LEY%201438%20DE%202011.pdf.
- 9.Brockett P, Golden L, Wei P, Yang C. Medicare advantage, medical loss ratio, service efficiency, and efficiently positive health outcomes. North Am Actuar J. 2023;27(3):493–507. doi: 10.1080/10920277.2022.2099425. [DOI] [Google Scholar]
- 10.Haberkorn J. Medical loss ratios. Health Aff. 2010. https://www.healthaffairs.org/do/10.1377/hpb20101112.449011/full/. Accessed 28 Jan 2023.
- 11.Natsis A. A summary of the updated medical loss ratio methodology and historical results. Schaumburg. 2019. https://www.soa.org/4b023f/globalassets/assets/files/resources/research-report/2019/mimimum-mlr-analysis.pdf. Accessed 28 Jan 2023.
- 12.Abraham J, Karaca-Mandic P. Regulating the medical loss ratio: implications for the individual market. Am J Manag Care. 2011;17(3):211–218. [PubMed] [Google Scholar]
- 13.Brockett P, Golden L, Yang C, Young D. Medicaid managed care: efficiency, medical loss ratio, and quality of care. North Am Actuar J. 2021;25(1):1–16. doi: 10.1080/10920277.2019.1678044. [DOI] [Google Scholar]
- 14.Harrington S. Medical loss ratio regulation under the affordable care act. Inq J Heal Care Organ Provision, Financ. 2013;50(1):9–26. doi: 10.5034/inquiryjrnl_50.01.05. [DOI] [PubMed] [Google Scholar]
- 15.Karaca-Mandic P, Abraham J, Simon K. Is the medical loss ratio a good target measure for regulation in the individual market for health insurance? Health Econ. 2015;24(1):55–74. doi: 10.1002/hec.3002. [DOI] [PubMed] [Google Scholar]
- 16.Belina H, Surysekar K, Weismann M. On the medical loss ratio (MLR) and sticky selling general and administrative costs: evidence from health insurers. J Account Public Policy. 2019;38(1):53–61. doi: 10.1016/j.jaccpubpol.2019.01.004. [DOI] [Google Scholar]
- 17.Mossialos E, Thomson S, editors. Voluntary health insurance in the European Union. 1. Brussels: European Observatory on Health Systems and Policies; 2004. [Google Scholar]
- 18.Thu-Cúc N. Socialist Republic of Viet Nam: strengthening the policy and institutional framework of social health insurance. Hanoi; 2021. https://www.adb.org/sites/default/files/project-documents/50139/50139-002-tacr-en_0.pdf. Accessed 25 Jan 2023.
- 19.Simon-Tuval T, Horev T, Kaplan G. Medical loss ratio as a potential regulatory tool in the Israeli healthcare system. Isr J Health Policy Res. 2015;4(1):21. doi: 10.1186/s13584-015-0009-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alhassan A. Financial health of medical schemes in South Africa. Financ Res Lett. 2023;51:103403. doi: 10.1016/j.frl.2022.103403. [DOI] [Google Scholar]
- 21.Ministerio de Salud y Protección Social. Unidad de pago por capitación (UPC) [Internet]. 2023 https://www.minsalud.gov.co/salud/POS/Paginas/unidad-de-pago-por-capitacion-upc.aspx. Accessed 13 Jan 2023.
- 22.Asociación Colombiana de Empresas de Medicina Integral (ACEMI). Cifras e indicadores. Conexxion. 2021;9(26):26.
- 23.NUMERIS. Análisis de siniestralidad y backtesting de UPC del régimen contributivo de salud. Bogotá, D.C. 2023. https://acemi.org.co/wp-content/uploads/2023/07/Estudio-de-Siniestralidad-y-Backtesting-UPC-VF.pdf. Accessed 30 Aug 2023.
- 24.Werner G, Modlin C. Basic ratemaking. 5. San Antonio: Casualty Actuarial Society; 2016. [Google Scholar]
- 25.Babcock N, Loss ratio. In: Encyclopedia of actuarial science. 1. Chichester: John Wiley & Sons Ltd; 2004. [Google Scholar]
- 26.Klugman S, Panjer H, Gordon W. Loss models. From data to decisions. 5. Hoboken: John Wiley & Sons; 2019. [Google Scholar]
- 27.Bugg W, Jay B, Lippai S, Moore B, Sky D, Sutton H, et al. Loss ratios and health coverages [Internet]. Washington, D.C. 1998. https://www.actuary.org/sites/default/files/files/publications/lossratios%201198.pdf. Accessed 3 Jan 2023.
- 28.Superintendencia Nacional de Salud. Información financiera EPS, EMP, SAP, Regímenes de Excepción y Especiales. 2022. https://www.supersalud.gov.co/es-co/Paginas/Delegada%20Supervision%20de%20Riesgos/informacion-financiera-EPS-EMP-SAP-regimenes-de-excepcion-y-especiales.aspx. Accessed 18 Jan 2023.
- 29.Basto S, Bejarano V, Do Nascimento P, Espinosa O, Estrada K, Higuera S, et al. Producto 3. Estimación actuarial de la UPC del régimen subsidiado. Convenio Interadministrativo IETS-MinHacienda N°. 7008-2021, Bogotá, D.C; 2021.
- 30.Ministerio de Salud y Protección Social. Decreto 780 de 2016 “Por medio del cual se expide el Decreto Único Reglamentario del Sector Salud y Protección Social”. Bogotá, D.C. 2016. https://www.minsalud.gov.co/Normatividad_Nuevo/Decreto%200780%20de%202016.pdf.
- 31.Londoño K. EPM explicó las razones por las que su Entidad Adaptada de Salud entra en un proceso de liquidación. Blue Radio. 2022 Dec. https://www.bluradio.com/blu360/antioquia/epm-explico-las-razones-por-las-que-su-entidad-adaptada-de-salud-entra-en-un-proceso-de-liquidacion-rg10. Accessed 20 Jan 2023
- 32.Ministerio de Salud y Protección Social. MinSalud hizo balance del sistema en la ruralidad frente al covid-19. 2020 https://www.minsalud.gov.co/Paginas/Minsalud-hizo-balance-del-sistema-en-la-ruralidad-frente-al-covid-19.aspx. Accessed 20 Jan 2023
- 33.Mora-Moreo L, Estrada-Orozco K, Espinosa O, Mesa-Melgarejo L. Characterization of the population affiliated to the subsidized health insurance scheme in Colombia: a systematic review and meta-analysis. Int J Equity Health. 2023;22(1):28. doi: 10.1186/s12939-022-01818-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Espinosa O, Estrada K, Franco O, Cepeda M, Rodríguez P, Chicaiza L, et al. El fortalecimiento de la Superintendencia Nacional de Salud (SUPERSALUD) es prioritario para garantizar el derecho fundamental a la salud. Medicina (B Aires) 2022;44(3):433–439. doi: 10.56050/01205498.2188. [DOI] [Google Scholar]
- 35.Robinson J. Marketwatch: use and abuse of the medical loss ratio to measure health plan performance. Health Aff. 1997;16(4):176–187. doi: 10.1377/hlthaff.16.4.176. [DOI] [PubMed] [Google Scholar]
- 36.Ministerio de Salud y Protección Social. Régimen Subsidiado. 2013. https://www.minsalud.gov.co/salud/Paginas/R%C3%A9gimenSubsidiado.aspx#:~:text=El%20R%C3%A9gimen%20Subsidiado%20es%20el,subsidio%20que%20ofrece%20el%20Estado.
- 37.Ministerio de Salud y Protección Social. Régimen Contributivo. 2013. https://www.minsalud.gov.co/proteccionsocial/Regimencontributivo/Paginas/regimen-contributivo.aspx#:~:text=El%20r%C3%A9gimen%20contributivo%20es%20un,por%20el%20afiliado%20o%20en.
- 38.Samuels D, Taylor D, Verrecchia R. The economics of misreporting and the role of public scrutiny. J Account Econ. 2021;71(1):101340. doi: 10.1016/j.jacceco.2020.101340. [DOI] [Google Scholar]
- 39.Fang V, Huang A, Wang W. Imperfect accounting and reporting bias. J Account Res. 2017;55(4):919–962. doi: 10.1111/1475-679X.12170. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets and programming codes used, generated, and analyzed during the current study are available in https://github.com/Jonavier/Loss_Ratio_CPU.