Abstract
Background
Exposure to repetitive head impacts (RHI) in American football players can lead to cognitive impairment and dementia due to neurodegenerative disease, particularly chronic traumatic encephalopathy (CTE). The pathognomonic lesion of CTE consists of perivascular aggregates of hyper-phosphorylated tau in neurons at the depths of cortical sulci. However, it is unclear whether exposure to RHI accelerates amyloid-β (Aβ) plaque formation and increases the risk for Alzheimer’s disease (AD). Although the Aβ neuritic plaques characteristic of AD are observed in a minority of later-stage CTE cases, diffuse plaques are more common. This study examined whether former professional and college American football players, including those with cognitive impairment and dementia, have elevated neuritic Aβ plaque density, as measured by florbetapir PET. Regardless of cognitive and functional status, elevated levels of florbetapir uptake were not expected.
Methods
We examined 237 men ages 45–74, including 119 former professional (PRO) and 60 former college (COL) football players, with and without cognitive impairment and dementia, and 58 same-age men without a history of contact sports or TBI (unexposed; UE) and who denied cognitive or behavioral symptoms at telephone screening. Former players were categorized into four diagnostic groups: normal cognition, subjective memory impairment, mild cognitive impairment, and dementia. Positive florbetapir PET was defined by cortical-cerebellar average SUVR of ≥ 1.10. Multivariable linear regression and analysis of covariance (ANCOVA) compared florbetapir average SUVR across diagnostic and exposure groups. Multivariable logistic regression compared florbetapir positivity. Race, education, age, and APOE4 were covariates.
Results
There were no diagnostic group differences either in florbetapir average SUVR or the proportion of elevated florbetapir uptake. Average SUVR means also did not differ between exposure groups: PRO-COL (p = 0.94, 95% C.I. = [− 0.033, 0.025]), PRO-UE (p = 0.40, 95% C.I. = [− 0.010, 0.029]), COL-UE (p = 0.36, 95% CI = [0.0004, 0.039]). Florbetapir was not significantly associated with years of football exposure, cognition, or daily functioning.
Conclusions
Cognitive impairment in former American football players is not associated with PET imaging of neuritic Aβ plaque deposition. These findings are inconsistent with a neuropathological diagnosis of AD in individuals with substantial RHI exposure and have both clinical and medico-legal implications.
Trial registration
Supplementary Information
The online version contains supplementary material available at 10.1186/s13195-023-01315-5.
Keywords: American Football, Amyloid-β, Concussion, Alzheimer’s disease, Cognitive function, Chronic traumatic encephalopathy, Dementia, Florbetapir, Neurodegenerative disease, Positron emission tomography, Repetitive head impacts, Subconcussive trauma, Tau, Traumatic brain injury
Background
The routine play of American football involves exposure to repetitive head impacts (RHI), including those resulting in symptomatic concussions and the more common asymptomatic subconcussive trauma [1–3]. This RHI exposure can lead to cognitive impairment and dementia later in life [4–8], and to the neurodegenerative disease, chronic traumatic encephalopathy [9–13] (CTE). CTE is currently diagnosed through postmortem neuropathological evaluation, characterized by the perivascular deposition of hyper-phosphorylated tau (p-tau) in neurons (with or without astrocytic involvement) at the depths of the cortical sulci, with widespread p-tau deposition and neurodegeneration in later stages [9, 14–17]. CTE is a unique disease that is distinct from Alzheimer’s disease (AD) and other tauopathies; this distinction is based on the type and distribution of p-tau deposition [14, 18], molecular structure of the tau filament [19, 20], specific location and evolution of p-tau isoforms [21, 22], and tau phosphorylation sites [23].
Similar to AD and other neurodegenerative diseases [24–26], CTE often has concomitant neurodegenerative and aging-related pathologies [27–32]. Although amyloid-β (Aβ) diffuse plaques are present in 52% of post-mortem CTE cases [33], moderate-to-frequent Aβ neuritic plaques, a defining characteristic of AD, are found in only 14% of confirmed cases of CTE, predominantly in older individuals with later stage pathology [15]. Results of in vivo amyloid positron emission tomography (PET) have been reported in two small studies of cognitively impaired former football and other contact sport athletes and have not found significantly elevated tracer binding compared to asymptomatic controls [34, 35]. These preliminary studies had several limitations (e.g., small sample size, inconsistent sources and levels of RHI exposure, limited range of cognitive impairment), however, precluding conclusions as to whether cognitive impairment and dementia in former American football players are associated with Aβ neuritic plaque pathology.
Here, we report findings from the Diagnostics, Imaging, and Genetics Network for the Objective Study and Evaluation of Chronic Traumatic Encephalopathy (DIAGNOSE CTE) Research Project, a multi-center, 8-year study funded by the National Institute of Neurological Disorders and Stroke (NINDS). A detailed description of the study design, procedures, and sample (including detailed inclusion and exclusion criteria) has been previously reported [36]. The aim of the cross-sectional study reported herein was to assess neuritic amyloid plaque density, as measured by florbetapir PET, in former professional and college football players across the spectrum of cognitive functioning (unimpaired, subjective memory complaints, mild cognitive impairment [MCI], and dementia), and in same-age asymptomatic men without exposure to RHI. Based on results of previous small studies [34, 35], and because deposition of neuritic plaques is not a common or early neuropathological finding in American football players [15, 33]—even in those with memory impairment and mild dementia—we hypothesized that florbetapir uptake would not be elevated in the former players compared to unexposed controls and that florbetapir uptake would not be associated with length of RHI exposure or to cognitive impairment or dementia.
Methods
Sample
The DIAGNOSE CTE Research Project includes 120 former professional American football players (PRO), 60 former college football players (COL), and 60 same-age men without a history of playing football or other RHI exposure (i.e., unexposed [UE]). All participants were male and 45–74 years old. Three participants did not receive florbetapir PET due to dose failure at the manufacturer. Therefore, the sample for this study consisted of 237 men, including 119 PRO, 60 COL, and 58 asymptomatic UE. PRO participants played a minimum of 12 years of organized football, including ≥ 3 in college and > 3 seasons in the National Football League (NFL). COL participants played organized football for ≥ 6 years, with ≥3 years at the college level, and had no contact/collision sports involvement following college. UE participants had no history of participation in contact/collision sports or combat military service. At telephone screening, all UE participants denied cognitive, mood, or behavioral symptoms; functional dependence; history of concussion or traumatic brain injury (TBI); or preexisting psychiatric disorders. Data were collected between September 2016 and February 2020. All participants provided written informed consent.
Diagnostic classification
Specific tests, variables, and cutoff scores for this study were determined a priori to group participants into one of four categories: cognitively normal (CN), subjective memory complaints (SMC), mild cognitive impairment (MCI), and dementia (DEM) across the cognitive continuum [37]. The algorithm used for this categorization is detailed in the Supplementary Material (Additional File 1). Participants who did not fall within any of the four diagnoses (n = 18) were excluded from analyses involving diagnostic grouping but included in other analyses. The Test of Memory Malingering (TOMM) [38] was used to detect suboptimal effort on neurocognitive tests. For all analyses other than exposure group differences (i.e., PRO, COL, UE), participants with a TOMM trial 2 score ≤ 45 (n = 11, 1 missing) were excluded.
Florbetapir PET acquisition and evaluation
Florbetapir doses at the four DIAGNOSE performance evaluation sites were requested through and provided at no cost by Avid Radiopharmaceuticals (Philadelphia, PA, USA). Quality control and imaging calibration procedures were completed prior to study initiation by Invicro (Needham, MA, USA). PET imaging involved a 10-min acquisition (10 frames, 1 min in length each) following a 370 MBq (10 mCi) bolus injection of florbetapir. Fifty minutes after injection, a second 15-min scan was done (acquired in 3 × 5-min frames). Images were uploaded to Invicro for quality control checks. Cortical-cerebellar florbetapir standardized uptake value ratios (SUVR) were calculated as published elsewhere [39, 40]. A positive florbetapir PET scan was defined by an average cortical SUVR of 1.10 or greater (centiloid values > 24.3), equivalent to moderate-to-frequent neuritic Aβ plaques [41]. A negative PET scan was defined by an SUVR < 1.10, indicating sparse-to-no neuritic amyloid plaques.
Statistical analysis
Power calculations, based on reports of using florbetapir to assess amyloid burden in AD dementia, MCI, and normal aging [42], indicate that 35 participants per group would result in 80% power to detect a significant group difference in average SUVR of at least 0.15 (MCI and CN SUVR = 1.2 vs 1.05). For exposure analyses, the PRO and COL groups were combined. Multivariable linear regressions were conducted for comparison of florbetapir SUVR and its association with exposure. Multivariable logistic regressions were conducted for group comparisons of florbetapir positivity. For bivariate analyses, t-tests were used for florbetapir SUVR and chi-square tests for florbetapir positivity. The following variables were controlled for in all models: age, race, years of education, and APOE ε4 genotype (carrier vs. non-carrier). Statistical significance was set at a more liberal P < 0.05 to reduce type 2 error because of the hypothesized nonsignificant results. Statistical analyses were conducted using R version 4.00.
Results
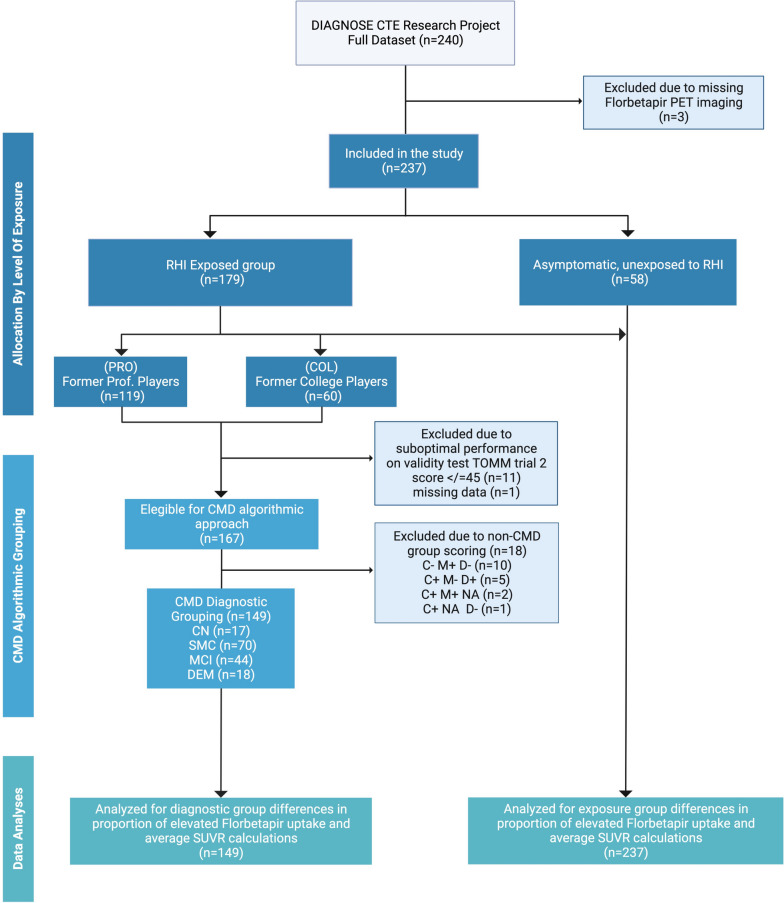
A flow diagram depicting the sampling of subjects, diagnostic status, and inclusion in data analyses is provided in Fig. 1. Participant characteristics by exposure group, including clinical ratings and cognitive test scores, APOE ε4 genotype, and florbetapir average SUVR and percent positive, are summarized in Table 1. There were no significant differences between the exposure groups in the proportion of positive amyloid PET scans or in the continuous florbetapir average SUVR by age range or exposure group (Supplementary Table 1, Additional File 1). Post hoc analysis comparing pairs of exposure groups found that the mean value of florbetapir average SUVR did not differ between PRO and COL (− 0.01 p = 0.95, 95% CI [− 0.033, 0.025]), PRO and UE (0.02 p = 0.41, 95% CI [− 0.010, 0.029]), and COL and UE (0.02 p = 0.36, 95% CI [0.0004, 0.039]) (Table 2). There was no significant association between florbetapir average SUVR and total years of football or with measures of cognition and daily functioning (Supplementary Table 2, Additional File 1).
Fig. 1.
Study flow chart illustrating participant recruitment and allocation to repetitive head impact exposure groups and diagnostic groups for data analyses. Abbreviations: RHI, repetitive head impacts; CMD, Complaints-Memory-Dementia algorithmic grouping; CN, cognitively normal; SMC, subjective memory complaint; MCI, mild cognitive impairment; DEM, dementia; SUVR, standard uptake value ratio; NA, not applicable; TOMM, Test of Memory Malingering, CMD algorithmic approach for diagnostic grouping: Presence or absence of subjective cognitive complaints, C ± (C + defined by Cognitive Complaint Index [memory items] self-report score > 16); presence or absence of objective memory impairment, M ± (M + defined by NAB List Learning Test Delayed Recall T score ≤ 35); presence or absence of dependence in daily functioning, D ± (D + defined as Functional Activities Questionnaire score ≥ 9)
Table 1.
Demographics and descriptive data
| Characteristic | Former professional football players (PRO) (n = 119) | Former college football players (COL) (n = 60) | Unexposed (UE) (n = 58) | P value |
|---|---|---|---|---|
| Age, mean (SD), years | 59.0 (7.8) | 53.5 (7.7) | 59.5 (8.3) | < 0.001a |
| Age by decade, n (%) within exposure group | ||||
| 45–54 | 42 (35.3) | 44 (73.3) | 22 (37.9) | < 0.01 |
| 55–64 | 46 (38.7) | 9 (15.0) | 14 (24.1) | |
| 65–74 | 31 (26.1) | 7 (11.7) | 22 (37.9) | |
| Body Mass Index, mean (SD) kg/m2 | 32.0 (4.5) | 33.8 (4.8) | 30.7 (4.4) | 0.001b |
| Education, mean (SD), years | 16.6 (1.1) | 17.1 (1.9) | 17.3 (3.5) | 0.07 |
| Racial Identity, No. (%) | ||||
| American Indian or Alaska Native | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0.003 |
| Black or African-American | 52 (43.7%) | 11 (18.3%) | 24 (41.5%) | |
| Native Hawaiian or Other Pacific Islander | 0 (0.0%) | 0 (0.0%) | 1 (1.7%) | |
| White | 65 (54.6%) | 48 (80.0%) | 33 (56.9) | |
| Multiracial | 2 (1.7%) | 1 (1.7%) | 0 (0.0%) | |
| Ethnicity, No. (%) | ||||
| Hispanic or Latino | 3 (2.5%) | 0 (0.0%) | 0 (0.0%) | 0.433 |
| Not Hispanic or Latino | 116 (97.5%) | 60 (100.0%) | 58 (100%) | |
| Total years of football, mean (SD), years | 18.0 (3.4) | 11.5 (2.5) | NA | < 0.001 |
| Years of NFL participation, mean (SD), years | 7.4 (2.7) | NA | NA | NA |
| Age of first exposure to football, mean (SD), years | 11.6 (2.8) | 10.2 (2.6) | NA | 0.002 |
| Yrs between end of football play and baseline, mean (SD), years | 28.8 (8.5) | 31.5 (8.1) | NA | 0.043 |
| MoCA total, mean (SD) T score | 39.3 (13.3) | 42.0 (12.5) | 49.0 (9.9) | < 0.001c |
| Cognitive Complaint Index, mean (SD) raw score | 32.8 (13.0) | 31.4 (12.8) | 13.7 (2.2) | < 0.001d |
| Cognitive Complaint Index above cut (> 16), No. (%) | 100 (84.0%) | 52 (86.7%) | 7 (12.1%) | < 0.001 |
| NAB List Learning Test Delayed Recall, mean (SD) T score | 36.1 (11.7) | 41.38 (13.7) | 45.6 (12.5) | < 0.001e |
| NAB List Learning Delayed Recall T score impaired (≤ 35), No. (%) | 63 (53.9%) | 21 (35.0%) | 13 (22.4%) | < 0.001 |
| Functional Activities Questionnaire -Informant, mean (SD) total score | 3.9 (5.7) | 2.97 (5.0) | 0.18 (0.5) | < 0.001d |
| ApoE ε4 genotype carriers, No. (%)f | 33 (28.6%) | 20 (33.9%) | 11 (20.4%) | 0.27 |
| Florbetapir average SUVR ≥ 1.10, No. (%) | 10 (8.4%) | 7 (11.7%) | 3 (5.2%) | 0.44 |
| Florbetapir mean (SD) average SUVR | 1.00 (0.09) | 0.99 (0.10) | 0.98 (0.09) | 0.30 |
Continuous variables compared with T-test or analysis of variance (for normally distributed data) or Mann–Whitney U or Kruskal–Wallis tests (for non-normally distributed data). Significant analysis of variance post-hoc pairwise group comparisons examined with Student–Newman–Keuls test. Categorical variables compared with chi-square or Fischer’s exact tests
Abbreviations: MoCA Montreal Cognitive Assessment, NAB Neuropsychological Assessment Battery, SUVR standardized uptake value ratio, NA not applicable
aPRO = UE > COL
bPRO = UE < COL
cPRO = COL < UE
dPRO = COL > UE
ePRO < COL < UE
fApoE genotyping unavailable for 10 participants (5 PRO, 1 COL, 4 UE)
Table 2.
Comparisons of florbetapir average SUVR between exposure groups
| Comparison by level of exposure | Estimate (95% CI) | Std. error | t valuea | P-value |
|---|---|---|---|---|
| PRO-COL | − 0.01 (− 0.033, 0.025) | 0.02 | − 0.31 | 0.95 |
| PRO-UE | 0.02 (− 0.010, 0.029) | 0.02 | 1.28 | 0.41 |
| COL-UE | 0.02 (0.0004, 0.039) | 0.02 | 1.36 | 0.36 |
Abbreviations: PRO former professional football players, COL former college football players, UE unexposed control group
aOne-way ANOVA, post hoc Tukey analysis based on the studentized range distribution. P-values were adjusted, controlling for age, education, race, and APOEe4 status
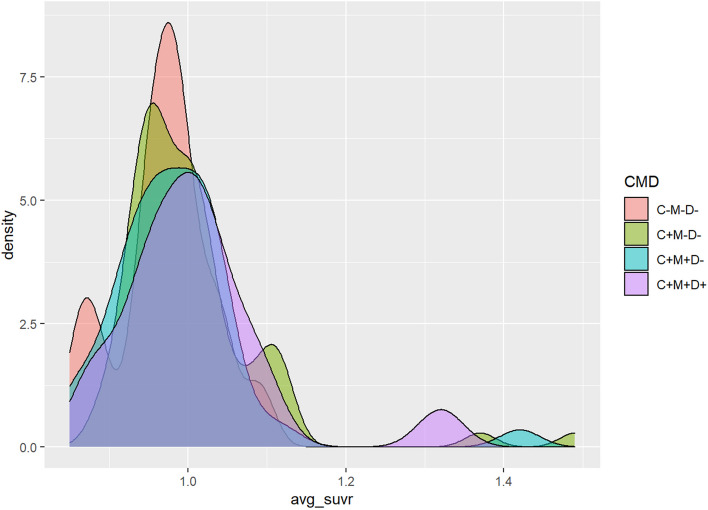
Among all former football players (with adequate TOMM performance), there were 17 CN, 70 SMC, 44 MCI, and 18 DEM. None of the CN group had an elevated florbetapir SUVR. There were 9 SMC (13%), 2 MCI (5%), and 2 DEM (11%) with elevated florbetapir SUVRs. Both participants in the DEM group with positive florbetapir scans were former college players though they differed in age and the number of years they played football. One was in the age range of 45 to 54 years and played for over a decade. The other was between 65 to 74 years old but played for less than one decade. Conversely, 16 of the 18 former football players in the DEM group did not have elevated florbetapir. Five of them were in the COL group and 11 in the PRO, across the age spectrum. Specific ages of participants are not reported to protect confidentiality. The smoothed density plot in Fig. 2 shows the scaled frequency distribution of florbetapir SUVR in each diagnostic group.
Fig. 2.
Density map of the mean florbetapir PET average SUVR in former American football players by diagnostic group. Diagnostic groups: C-M-D-, cognitively normal (CN); C + M-D-, subjective memory complaint (SMC); C + M + D-, mild cognitive impairment (MCI); C + M + D + , dementia (DEM). Y axis = number of subjects. X axis = average SUVR scores. Elevated florbetapir is defined by an average SUVR of 1.10 or greater
A one-way ANCOVA was conducted to estimate diagnostic group differences among football players (n = 149) on the continuous florbetapir average SUVR variable and found no significant between-group differences. Tukey post hoc comparisons found a global F-value of 0.94, p = 0.43 (Table 3).
Table 3.
Comparisons of differences in florbetapir average SUVRs between pairs of diagnostic groups in all former football players
| Group comparison | Coefficient | Sigma | T | P |
|---|---|---|---|---|
| CN-SMC | 0.05 | 0.03 | 1.86 | 0.24 |
| CN-MCI | 0.02 | 0.03 | 0.82 | 0.84 |
| CN-DEM | 0.05 | 0.03 | 1.69 | 0.33 |
| SMC-MCI | − 0.03 | 0.02 | − 1.50 | 0.43 |
| SMC-DEM | 0.01 | 0.02 | 0.25 | 0.99 |
| MCI-DEM | 0.03 | 0.03 | 1.27 | 0.57 |
One-way ANCOVA was performed to assess differences in the four diagnostic groups after controlling the linear effect of covariates by using regression analysis. F = 0.94, p = 0.43
Abbreviations: CN cognitively normal, SMC subjective memory complaints, MCI mild cognitive impairment, DEM dementia
Discussion
RHI exposure from American football has been associated with later-life cognitive impairment and dementia [4–8], and results of autopsy studies suggest that repetitive brain trauma causes, in part, the neurodegenerative disease, CTE [12, 43]. However, because there are currently no validated in vivo biomarkers for CTE pathology, and because the clinical presentation of CTE is often similar to that of AD, the differential diagnosis of individuals with substantial RHI exposure and later-life cognitive and functional impairment can be difficult [44]. Moderate-to-frequent Aβ neuritic plaques are scarce in CTE [15]. Florbetapir brain PET imaging is approved by the US Food and Drug Administration for estimating Aβ neuritic plaque density for cognitively impaired adult patients being evaluated for AD and other causes of cognitive decline [45]. A negative florbetapir PET indicates sparse-to-no neuritic plaques and is inconsistent with a neuropathological diagnosis of AD. The use of florbetapir and other amyloid PET imaging in clinical settings results in changes in the clinical management of patients, in general, and in changes in etiologic diagnosis from AD to non-AD in patients with negative scans [46, 47].
In this study, we found that most former professional and college football players, ages 45–74 years, with and without cognitive impairment or dementia, did not have in vivo amyloid PET evidence of AD. There were no exposure group differences nor cognitive impairment group differences in florbetapir average SUVR. Moreover, there were no differences between the three exposure groups (PRO, COL, UE) in the proportion of elevated SUVR. Finally, there were no significant associations between florbetapir average SUVR and total years of football or clinical measures. Our findings are consistent with previous preliminary studies [34, 35] and provide strong support that the cognitive impairment and dementia experienced by many former professional and college American football players are not associated with amyloid deposition typical of AD.
The percentage of former football players with positive amyloid PET in this study, across all cognitive impairment groups, was markedly lower than published prevalence estimates [48, 49]. In our CN, SMC, MCI, and DEM groups, the percentage of amyloid PET positivity was 0%, 13%, 5%, and 11%, respectively. In contrast, the most recent prevalence estimates of amyloid PET positivity for 60-year-old men (based on pooled data from 85 Amyloid Biomarker Study cohorts) are as follows: normal cognition = 17.6% (95% CI 13.8–22.3); subjective cognitive decline = 19.6% (95% CI 14.1–26.5); MCI = 39.2% (95% CI 32.5–46.4); and clinical AD dementia = 88.4% (95% CI 84.5–91.5) [48]. It is unclear why these former football players do not have amyloid PET evidence of AD, the most common cause of cognitive impairment and dementia in aging. That is, is there a potential mechanism that would reduce or prevent Aβ neuritic plaques in individuals with extensive RHI exposure? Animal models have shown that there is microglial activation with a sustained inflammatory response during and following repetitive mTBI [50–53], but before p-tau pathology [54]. In a postmortem study of young contact sport athletes, an increased number of activated microglia, positively associated with CTE severity, has been reported [55]. It is possible that such a primed inflammatory response has a differential effect on amyloid and tau aggregate formation, preventing or delaying the formation of Aβ neuritic plaque, but accelerating and promoting p-tau neurofibrillary inclusions. Additional research is needed to examine this and other potential mechanisms.
Strengths
This study has several advantages. Unlike previous reports, this study had a relatively large sample size and was well-powered to detect statistical differences if they existed. Our sample was not limited to former professional football players, but also included former college football athletes who never played professional football or any other contact sport after college. The sample of football players includes participants across the spectrum of cognitive impairment. Participants in the UE group had no history of playing contact sports, combat military experience, or concussion/TBI. Importantly, the sample of former NFL players includes 44% Black-identified participants, which is representative of the approximately 40% Black former players in this age group who played during the era our sample would have played (1967–1996). Moreover, the UE group had a similar representation of Black-identified participants (42%).
Limitations
This study also has limitations. Due to a lack of power, it is possible that we are not detecting early focal amyloid deposits [56]. Hence, conceivably, a higher proportion of participants were unaccounted for progressive amyloid pathology. Longitudinal studies of cognitively unaffected participants and elevated amyloid accumulation have indicated that elevation in baseline amyloid level is associated with a risk for cognitive decline, suggesting a preclinical stage of Alzheimer’s disease [57, 58]. Because this is a cross-sectional study, evolving amyloid deposition indicating incipient AD neuropathologic changes cannot be estimated in individuals below the cut-off point. Future prospective cohort studies may benefit from optimal threshold corrections [59]. By design, in addition to no RHI exposure, the UE “control” group had no complaints of cognitive, mood, or behavioral impairment at telephone screening. Although the UE group may be appropriate for some analyses aimed at biomarker development and validation, its inclusion in other types of analyses may not be appropriate because of the inability to disentangle the exposure history from the clinical presentation [36]. Additionally, although histories of mood or sleep disorders could affect cognitive and functional measures, we did not include them in the diagnostic classification algorithm used in this study, nor were they included as covariates. The PRO group had a similar age and race composition as the UE group. However, the COL group was significantly younger and included fewer Black participants than either the PRO or UE groups. Although age and race were both used as covariates in all analyses, there still may have been an impact on the findings due to these differences. Similar to almost all research in this area, this study only involved men who played American football. Future studies should include women and individuals with other sources of RHI exposure (e.g., former soccer and rugby players, combat military veterans, and victims of intimate partner violence). The number of participants who met the criteria for the dementia classification was relatively small. Future studies may benefit from including a larger number of former football players with dementia. Finally, the classification of participants into the MCI and DEM groups is limited by being based solely on an algorithm using cutoff scores on specific tests, and not based on a clinical evaluation or adjudicated through a consensus diagnostic conference.
Clinical implications
CTE is a neuropathological diagnosis. Although other neurodegenerative diseases, such as AD, are also defined by their neuropathological characteristics, the development of sensitive and specific in vivo neuroimaging and fluid biomarkers over the past two decades has resulted in improved clinical diagnostic accuracy and early detection of underlying neuropathology [60, 61]. The clinical disorder associated with CTE is traumatic encephalopathy syndrome (TES). The NINDS consensus diagnostic criteria for TES include a provisional level of certainty for underlying CTE p-tau pathology [44]. However, biomarkers are not included in those criteria because biomarker development for CTE had not reached sufficient maturity to be included. Until there are sensitive and specific biomarkers for CTE pathophysiology, a clinical “diagnosis by exclusion”—similar to older diagnostic criteria for “Alzheimer’s disease” [62, 63]—may be appropriate in some, but not all, circumstances. For example, if a 65-year-old former NFL player presents with significant and progressive cognitive decline (including episodic memory impairment and executive dysfunction), no neuropsychiatric symptoms, and mild-moderate dementia, meeting all NINDS consensus criteria for TES with a probable level of certainty for CTE pathology [44]; has no evidence for another cause of his clinical presentation other than AD or CTE; and has a negative amyloid PET, it may be appropriate for the clinician to suspect that CTE is the underlying cause of the patient’s dementia. In this case, the negative biomarker for AD neuritic plaque would be used to inform the diagnosis by exclusion, as previously suggested [31].
A history of “head injury” is commonly included in lists of important risk factors for AD. Although earlier studies indicated a possible increased risk for dementia from a single moderate-to-severe TBI [64], more recent studies have not found postmortem evidence of AD pathology in individuals with previous TBI [65]. The lack of evidence of AD pathology following TBI has been demonstrated by in vivo amyloid PET studies of older community-dwelling volunteers [66] and cognitively impaired military veterans [67]. Additional studies have indicated that TBI history increases the risk for non-AD dementia [68] and is associated with non-AD pathologies at postmortem examination [65, 69, 70]. There is a clinical and pathological distinction between AD pathology and TBI-related neurodegeneration. Thus, patients with delayed cognitive and functional decline following a moderate-to-severe TBI may not have AD as the sole cause of their dementia [71, 72].
Medico-legal implications
There are potential medico-legal implications of the results of this study, including those associated with the highly publicized NFL “Concussion Settlement” [73]. This class action settlement provides substantially higher monetary compensation to former players with a diagnosis of AD than for players with similar cognitive impairment and dementia but without an AD diagnosis. For example, a 62-year-old former player who receives a DSM-5 diagnosis of Major Neurocognitive Disorder due to probable AD by a settlement-qualified neurologist who does not order a florbetapir PET would be eligible for compensation of $950,000 [73]. However, if the same patient were to have a florbetapir amyloid PET as part of the evaluation and the results were negative (i.e., inconsistent with a neuropathological diagnosis of AD [45]), the neurologist would likely not make the probable AD diagnosis, and therefore, the player would be eligible for compensation of only $290,000. That is, the retired player who was given the less precise diagnosis of probable AD made without the florbetapir PET would receive substantially more compensation. The compensation criteria for the NFL settlement may need to be modified based on new medical/scientific findings, including findings that cognitive impairment and dementia in many former NFL players may be caused by non-AD neuropathology.
Conclusion
In this study from the DIAGNOSE CTE Research Project, we did not find evidence of elevated Aβ neuritic plaque density as measured by florbetapir PET imaging in former professional and college football players, with and without cognitive and functional impairment. These findings suggest that AD is not the cause of the former players’ cognitive decline and dementia. Additional studies are needed to clarify the extent to which cognitive impairment in former football players and persons with a history of repetitive head impacts is related to other neuropathological changes, including CTE. Until sensitive and specific biomarkers for CTE p-tau pathology are available, a diagnosis of TES dementia “consistent with CTE” could be considered in older individuals with a substantial history of RHI exposure, progressive cognitive decline, and functional impairment who have negative amyloid PET imaging.
Supplementary Information
Additional file 1: Algorithm for Diagnostic Categorization. Supplementary Table 1. Proportion of Positive Amyloid PET Scans by Age within Exposure Group. Supplementary Table 2. Correlationsa of Florbetapir PET Average SUVR with Clinical Measures and Years of Football.
Acknowledgements
Avid Radiopharmaceuticals, Inc., a wholly-owned subsidiary of Eli Lilly and Company, provided the florbetapir tracer but did not provide direct funding and was not involved in data analysis or interpretation.
The DIAGNOSE CTE Research Project Current and Former Investigators and Key Personnel
Banner Alzheimer’s Institute
Investigators
Kewei Chen, Ph.D.
Hillary Protas, Ph.D.
Eric Reiman, M.D. (mPI).
Yi Su, Ph.D.
Non-Investigators
Connie Boker, M.B.A. (Director, Imaging Center Operations).
Boston University Chobanian & Avedisian School of Medicine
Investigators
Michael L. Alosco, Ph.D.
Rhoda Au, Ph.D.
Robert C. Cantu, Ph.D.
Lindsay Farrer, Ph.D.
Robert Helm, M.D. *
Douglas I. Katz, M.D.
Neil Kowall, M.D. *
Jesse Mez, M.D.
Gustavo Mercier, M.D., Ph.D. *
James Otis, M.D. *
Robert A. Stern, Ph.D. (mPI).
Jason Weller, M.D.
Trainees
Tahlia Bragg, Ph.D. (Postdoctoral Fellow).
Irene Simkin, M.S. (Lab Manager, Molecular Genetics Core Facility).
Diana Trujillo-Rodriguez, B.Sc., M.Sc. (Ph.D. Student).
Suzan van Amerongen, M.D. (Research Fellow).
Boston University Project Coordinating Center Staff
Alondra Andino, B.A. (Project Administrative Manager) *
Shannon Conneely, B.A. (Site Coordinator) *
Courtney Diamond, M.B.A. (Project Manager) *
Tessa Fagle, B.A. (Research Assistant).
Olivia Haller, B.A. (Recruitment Coordinator) *
Tennyson Hunt, M.B.A. (Project Administrative Manager) *
Nicole Gullotti, M.B.A. (Research Administrator) *
Bailey Kossow, B.S. (Research Assistant).
Carrie Kugelmass, B.A. (Research Assistant).
Megan Mariani, B.S., B.A. (Project Manager) *
Brian Mayville, B.S. (Site Coordinator) *
Kathleen McLaughlin, B.A. (Research Assistant) *
Mary Nanna, B.A. (Retention Coordinator) *
Marty DiPopolo, B.S. (Retention Coordinator).
Taylor Platt, M.P.H. (Recruitment Coordinator) *
Surya Pulukuri, B.A. (Research Assistant).
Fiona Rice, M.P.H. (Project Manager) *
Madison Sestak, B.S. (Assistant Recruitment Coordinator) *
Irene Simkin, M.S. (Lab Manager, Molecular Genetics Core Facility).
Boston University School of Public Health
Investigators
Michael McClean, Sc.D.
Yorghos Tripodis, Ph.D.
Data Team Staff
Douglas Annis, M.S. (Systems Analyst) *
Christine Chaisson, M.P.H. (Leader of Data Management Sub-team) *
Diane B. Dixon (Project Manager).
Carolyn Finney, B.A. (Data Manager).
Kerrin Gallagher, M.P.H. (Statistical Analyst) *
Kaitlin Hartlage, M.P.H. (Statistical Analyst).
Jun Lu, M.S. (Data Security and Technology Analyst).
Brett Martin, M.S. (Statistical Manager).
Emmanuel Ojo, M.P.H. (Statistical Analyst) *
Joseph N. Palmisano, M.A., M.P.H. (Leader of Data Management Sub-team).
Brittany Pine, B.A., B.S. (Statistical Analyst).
Janani Ramachandran, M.S. (Data Manager) *
Trainees
Zachary Baucom, Ph.D.
Fatima Tuz-Zahra, M.S.
Eukyung Yhang, B.A.
Brigham and Women’s Hospital
Investigators
Sylvain Bouix, Ph.D.
Jennifer Fitzsimmons, M.D. *
Alexander P. Lin, Ph.D.
Inga K. Koerte, M.D., Ph.D.
Ofer Pasternak, Ph.D.
Martha E. Shenton, Ph.D. (mPI).
Non-Investigators
Hector Arciniega, Ph.D. (Postdoctoral Research Fellow).
Tashrif Billah, M.S. (Software Engineer).
Elena Bonke, M.S. (Ph.D. Student).
Katherine Breedlove, Ph.D. (Postdoctoral Research Fellow).
Holly Carrington, B.A. (Research Assistant).
Eduardo Coello, Ph.D. (Postdoctoral Research Fellow).
Michael J. Coleman, M.A. (Senior Scientist).
Omar John, B.S. (Research Assistant).
Leonard Jung, (Ph.D. Student).
Huijun Liao, B.S. (Study Coordinator).
Maria Loy, M.B.A., M.P.H. (Senior Program Coordinator).
Elizabeth Rizzoni, B.A. (Research Assistant).
Vivian Schultz, M.D. (Postdoctoral Research Fellow).
Annelise Silva, B.S. (Research Assistant) *
Brynn Vessey, B.S. (Research Assistant).
Tim L.T. Wiegand, (Ph.D. Student).
Cleveland Clinic Lou Ruvo Center for Brain Health
Investigators
Sarah Banks, Ph.D. (Now at University of California, San Diego).
Charles Bernick, M.D.
Jason Miller, Ph.D.
Aaron Ritter, M.D.
Marwan Sabbagh, M.D. * (Now at Barrow Institute).
Non-Investigators
Raelynn de la Cruz, (Psychometrician) *
Jan Durant, (Psychometrician) *
Morgan Golceker (Site Coordinator).
Nicolette Harmon, (Site Coordinator) *
Jaeson Kaylegian, (Psychometrician)*
Rachelle Long, (Site Coordinator) *
Christin Nance, (Psychometrician)*
Priscilla Sandoval (Site Coordinator) *
Miranda Staples, Ph.D. (Program Manager).
George Washington University School of Medicine and Health Sciences
Investigator
Robert W. Turner, Ph.D.
Non-Investigators
Emma F. Clark, B.A. (Research Assistant) *
Invicro (formerly Molecular NeuroImaging)
Investigator
Kenneth L. Marek, M.D.
Non-Investigator
Andrew Serrano, M.B.A.
Mayo Clinic Arizona
Investigators
Charles H. Adler, M.D., Ph.D.,
David W. Dodick, M.D. (Now at Atria Academy of Science and Medicine).
Yonas Geda, M.D., M.Sc. (Now at Barrow Neurological Institute).
Jennifer V. Wethe, Ph.D.
Non-Investigators
Amy Duffy, (Site Coordinator) *
Bryce Falk, R.N.
Marci Howard, (Psychometrician)*
Michelle Montague, (Psychometrician)*
Thomas Osgood, (Site Coordinator).
National Institute of Neurological Disorders and Stroke (NINDS)
Debra Babcock, M.D., Ph.D. (Scientific Program Official).
Patrick Bellgowan, Ph.D. (Administrative Program Official)*
New York University:
Investigators
Laura Balcer, M.D., M.S.C.E.
William Barr, Ph.D.
Judith Goldberg, Sc.D.
Binu Joseph, M.B.B.S.
Ivan Kirov, Ph.D.
Yvonne Lui, M.D.
Charles Marmar, M.D.
Thomas Wisniewski, M.D. *
Non-Investigators
Alhassan Al-Kharafi (Psychometrician) *
Allan George (Psychometrician) *
Lisena Hasanaj (Site Coordinator).
Sammie Martin (Psychometrician) *
Edward Riley (Psychometrician) *
William Runge (Psychometrician) *
Liliana Serrano.
University of Gothenburg, Sweden
Nicholas Ashton, Ph.D.
Henrik Zetterberg, M.D., Ph.D.
Kaj Blennow, M.D., Ph.D.
University of Nevada, Las Vegas
Jeffrey L. Cummings, M.D., ScD (mPI).
University of Washington and VA Puget Sound
Investigator
Jeffrey Iliff, Ph.D.
Gail Li, M.D., Ph.D.
Deidre Janssen, Ph.D.
James Meabon, Ph.D.
Elaine R. Peskind, M.D.
Juan Piantino, M.D.
Abigail Schindler, Ph.D.
Ronald Thomas, Ph.D
Non-Investigator
Elizabeth Colasurdo (Lab Manager).
Jane Shofer, M.S.
Washington University (CNDA)
Investigators
Daniel S. Marcus, Ph.D.
Non-Investigator
Jenny Gurney, M.S.
Consultants
Richard Greenwald, Ph.D. (Simbex)*
Keith A. Johnson, M.D. (Massachusetts General Hospital).
*No longer involved in the project.
Abbreviations
- Aβ
Amyloid-β
- ANCOVA
Analysis of covariance
- AD
Alzheimer’s disease
- CI
Confidence intervals
- CMD
Complaints-Memory-Dementia algorithmic grouping
- COL
Former college football players
- CN
Cognitively normal
- CTE
Chronic traumatic encephalopathy
- DEM
Dementia
- DIAGNOSE CTE
Diagnostics, Imaging, and Genetics Network for the Objective Study and Evaluation of Chronic Traumatic Encephalopathy
- MCI
Mild cognitive impairment
- MoCA
Montreal Cognitive Assessment
- NA
Not applicable
- NAB
Neuropsychological Assessment Battery
- NFL
National Football League
- PET
Positron emission tomography
- PRO
Former professional football players
- RHI
Repetitive head impacts
- SD
Standard deviation
- SMC
Subjective memory complaints
- SUVR
Standardized uptake value ratios
- TBI
Traumatic brain injury
- TOMM
Test of Memory Malingering
- UE
Unexposed
Authors’ contributions
RAS, JLC, MES, and EMR conceptualized and designed the study. RAS and DTR drafted the manuscript and substantively revised the work. YT, SVP, MLA, CHA, LJB, CB, KLM, TDS, JM, JLC, and EMR substantively contributed to revising the work and added valuable input. RAS, CHA, LJB, and CB were PIs of baseline evaluation sites and oversaw data acquisition. RAS, YT, MLA, KLM, MDM, KAJ, ACM, TDS, JM, JLC, MES, and EMR provided additional contributions to the interpretation of data. YT implemented biostatistical and data analytic plans. ZB analyzed data. JNP supervised data management and data sharing. All authors reviewed the manuscript.
Funding
This work was supported by grants from the National Institutes of Health (U01NS093334; R01NS078337; K23NS102399; K01AG054762; R01NS100952). The primary funding source is the National Institute of Neurological Disorders and Stroke (NINDS), through a U01 Research Project Cooperative Agreement (U01NS093334).
Availability of data and materials
Data from the DIAGNOSE CTE Research Project will be available to qualified investigators through the Federal Interagency Traumatic Brain Injury Research (FITBIR) Informatics System, through the National Institutes of Health Center for Information Technology: https://fitbir.nih.gov/content/access-data. DIAGNOSE CTE Research Project data, including those reported in this study, will also be available to qualified investigators through a project-specific data-sharing portal. Interested investigators should contact Dr. Robert A. Stern, bobstern@bu.edu.
Declarations
Ethics approval and consent to participate
All Participant Evaluation Sites received approval by their respective Institutional Review Boards.
◦ Boston University Medical Campus Institutional Review Board, #H-34799.
◦ Cleveland Clinic Institutional Review Board, #16–1694.
◦ Mayo Clinic Institutional Review Boards, #16–002662.
◦ NYU School of Medicine Institutional Review Board, #i16-01032 CR3.
◦ Partners Human Research Institutional Review Board, #2016P001359 and #2016P001328.
◦ Western Copernicus Group (WCG) Institutional Review Board (Banner Alzheimer’s Institute), #1168489.
All participants provided written informed consent during their baseline visits.
Consent for publication
Not applicable.
Competing interests
RAS is a member of the Board of Directors of King-Devick Technologies, Inc. (Chicago, IL, USA), and he receives royalties for published neuropsychological tests from Psychological Assessment Resources, Inc. (Lutz, FL, USA).
DTR: None to report.
YT None to report.
SVP None to report.
MLA None to report.
CHA None to report.
LJB is Editor-in-Chief of the Journal of Neuro-Ophthalmology.
CB receives research support from the Ultimate Fighting Championship, Top Rank promotions, and Haymon Boxing.ZB None to report.
KLM is a consultant for the Michael J Fox Foundation, GE Healthcare, Biohaven, Inhibikase, IRLabs, Roche, UCB, Denali, Calico, Biohaven, Neuron23, Aprinoia, Genentech, and Invicro.
MDM None to report.
KAJ
ACM None to report.
TDS
JM None to report.
JNP None to report.
JLC has provided consultation to Acadia, Actinogen, Acumen, AlphaCognition, Aprinoia, AriBio, Artery, Biogen, BioVie, Bristol-Myers Squib, Cassava, Cerecin, Diadem, EIP Pharma, Eisai, GemVax, Genentech, GAP Innovations, Janssen, Jocasta, Karuna, Lighthouse, Lilly, Lundbeck, LSP/EQT, Merck, NervGen, Novo Nordisk, Oligomerix, Optoceutics, Ono, Otsuka, PRODEO, Prothena, ReMYND, Roche, Sage Therapeutics, Signant Health, Simcere, Suven, SynapseBio, TrueBinding, Vaxxinity, and Wren pharmaceutical, assessment, and investment companies. He owns the copyright of the Neuropsychiatric Inventory.
MES None to report.
EMR is a compensated scientific advisor for Alkahest, Alzheon, AuralAnalytics, Denali, Green Valley, Retromer Therapeutics, and Vaxxinity, and a co-founder of ALZPath.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Robert A. Stern and Diana Trujillo-Rodriguez shared the first authorship.
Contributor Information
Robert A. Stern, Email: bobstern@bu.edu
for the DIAGNOSE CTE Research Project Investigators:
Kewei Chen, Hillary Protas, Yi Su, Connie Boker, Rhoda Au, Robert C. Cantu, Lindsay Farrer, Robert Helm, Douglas I. Katz, Neil Kowall, Gustavo Mercier, James Otis, Jason Weller, Tahlia Bragg, Irene Simkin, Suzan van Amerongen, Alondra Andino, Shannon Conneely, Courtney Diamond, Tessa Fagle, Olivia Haller, Tennyson Hunt, Nicole Gullotti, Bailey Kossow, Carrie Kugelmass, Megan Mariani, Brian Mayville, Kathleen McLaughlin, Mary Nanna, Marty DiPopolo, Taylor Platt, Fiona Rice, Madison Sestak, Douglas Annis, Christine Chaisson, Diane B. Dixon, Carolyn Finney, Kerrin Gallagher, Kaitlin Hartlage, Jun Lu, Brett Martin, Emmanuel Ojo, Brittany Pine, Janani Ramachandran, Fatima Tuz-Zahra, Eukyung Yhang, Sylvain Bouix, Jennifer Fitzsimmons, Alexander P. Lin, Inga K. Koerte, Ofer Pasternak, Hector Arciniega, Tashrif Billah, Elena Bonke, Katherine Breedlove, Holly Carrington, Eduardo Coello, Michael J. Coleman, Omar John, Leonard Jung, Huijun Liao, Maria Loy, Elizabeth Rizzoni, Vivian Schultz, Annelise Silva, Brynn Vessey, Tim L. T. Wiegand, Sarah Banks, Jason Miller, Aaron Ritter, Marwan Sabbagh, Raelynn de la Cruz, Jan Durant, Morgan Golceker, Nicolette Harmon, Jaeson Kaylegian, Rachelle Long, Christin Nance, Priscilla Sandoval, Miranda Staples, Robert W. Turner, Emma F. Clark, Andrew Serrano, David W. Dodick, Yonas Geda, Jennifer V. Wethe, Amy Duffy, Bryce Falk, Marci Howard, Michelle Montague, Thomas Osgood, Debra Babcock, Patrick Bellgowan, William Barr, Judith Goldberg, Binu Joseph, Ivan Kirov, Yvonne Lui, Charles Marmar, Thomas Wisniewski, Alhassan Al-Kharafi, Allan George, Lisena Hasanaj, Sammie Martin, Edward Riley, William Runge, Liliana Serrano, Nicholas Ashton, Henrik Zetterberg, Kaj Blennow, Jeffrey Iliff, Gail Li, Deidre Janssen, James Meabon, Elaine R. Peskind, Juan Piantino, Abigail Schindler, Ronald Thomas, Elizabeth Colasurdo, Jane Shofer, Daniel S. Marcus, Jenny Gurney, and Richard Greenwald
References
- 1.Belanger HG, Vanderploeg RD, McAllister T. Subconcussive blows to the head: a formative review of short-term clinical outcomes. J Head Trauma Rehabil. 2016;31(3):159–166. doi: 10.1097/HTR.0000000000000138. [DOI] [PubMed] [Google Scholar]
- 2.Walter AE, Wilkes JR, Arnett PA, Miller SJ, Sebastianelli W, Seidenberg P, et al. The accumulation of subconcussive impacts on cognitive, imaging, and biomarker outcomes in child and college-aged athletes: a systematic review. Brain Imaging Behav. 2022;16(1):503–517. doi: 10.1007/s11682-021-00489-6. [DOI] [PubMed] [Google Scholar]
- 3.Nathanson JT, Connolly JG, Yuk F, Gometz A, Rasouli J, Lovell M, et al. Concussion incidence in professional football: position-specific analysis with use of a novel metric. Orthop J Sports Med. 2016;4(1):2325967115622621. doi: 10.1177/2325967115622621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guskiewicz KM, Marshall SW, Bailes J, McCrea M, Cantu RC, Randolph C, et al. Association between recurrent concussion and late-life cognitive impairment in retired professional football players. Neurosurgery. 2005;57(4):719–726. doi: 10.1227/01.NEU.0000175725.75780.DD. [DOI] [PubMed] [Google Scholar]
- 5.Montenigro PH, Alosco ML, Martin BM, Daneshvar DH, Mez J, Chaisson CE, et al. Cumulative head impact exposure predicts later-life depression, apathy, executive dysfunction, and cognitive impairment in former high school and college football players. J Neurotrauma. 2017;34(2):328–40. [DOI] [PMC free article] [PubMed]
- 6.Lehman EJ. Epidemiology of neurodegeneration in American-style professional football players. Alzheimer's Res Ther. 2013;5(4):34. doi: 10.1186/alzrt188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Walton SR, Brett BL, Chandran A, Defreese JD, Mannix R, Echemendia RJ, et al. Mild Cognitive impairment and dementia reported by former professional football players over 50 yr of age: an NFL-LONG Study. Med Sci Sports Exerc. 2022;54(3):424–431. doi: 10.1249/MSS.0000000000002802. [DOI] [PubMed] [Google Scholar]
- 8.Randolph C, Karantzoulis S, Guskiewicz K. Prevalence and characterization of mild cognitive impairment in retired national football league players. J Int Neuropsychol Soc. 2013;19(8):873–880. doi: 10.1017/S1355617713000805. [DOI] [PubMed] [Google Scholar]
- 9.McKee AC, Stern RA, Nowinski CJ, Stein TD, Alvarez VE, Daneshvar DH, et al. The spectrum of disease in chronic traumatic encephalopathy. Brain. 2013;136:43–64. doi: 10.1093/brain/aws307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bieniek KF, Ross OA, Cormier KA, Walton RL, Soto-Ortolaza A, Johnston AE, et al. Chronic traumatic encephalopathy pathology in a neurodegenerative disorders brain bank. Acta Neuropathol. 2015;130(6):877–889. doi: 10.1007/s00401-015-1502-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mez J, Daneshvar DH, Abdolmohammadi B, Chua AS, Alosco ML, Kiernan PT, et al. Duration of American football play and chronic traumatic encephalopathy. Ann Neurol. 2020;87(1):116–131. doi: 10.1002/ana.25611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nowinski CJ, Bureau SC, Buckland ME, Curtis MA, Daneshvar DH, Faull RLM, et al. Applying the Bradford Hill criteria for causation to repetitive head impacts and chronic traumatic encephalopathy. Front Neurol. 2022;13:938163. 10.3389/fneur.2022.938163. [DOI] [PMC free article] [PubMed]
- 13.LeClair J, Weuve J, Fox MP, Mez J, Alosco ML, Nowinski C, et al. Selection bias analysis supports dose-response relationship between level of American football play and chronic traumatic encephalopathy diagnosis. Am J Epidemiol. 2022;191(8):1429–43. [DOI] [PMC free article] [PubMed]
- 14.Bieniek KF, Cairns NJ, Crary JF, Dickson DW, Folkerth RD, Keene CD, et al. The second NINDS/NIBIB consensus meeting to define neuropathological criteria for the diagnosis of chronic traumatic encephalopathy. J Neuropathol Exp Neurol. 2021;80(3):210–9. [DOI] [PMC free article] [PubMed]
- 15.Alosco ML, Cherry JD, Huber BR, Tripodis Y, Baucom Z, Kowall NW, et al. Characterizing tau deposition in chronic traumatic encephalopathy (CTE): utility of the McKee CTE staging scheme. Acta Neuropathol. 2020;140(4):495–512. doi: 10.1007/s00401-020-02197-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mez J, Daneshvar DH, Kiernan PT, Abdolmohammadi B, Alvarez VE, Huber BR, et al. Clinicopathological evaluation of chronic traumatic encephalopathy in players of American football. JAMA. 2017;318(4):360–370. doi: 10.1001/jama.2017.8334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Butler M, Dixon E, Stein TD, Alvarez VE, Huber B, Buckland ME, et al. Tau pathology in chronic traumatic encephalopathy is primarily neuronal. J Neuropathol Exp Neurol. 2022;81(10):773–780. doi: 10.1093/jnen/nlac065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McKee AC, Cairns NJ, Dickson DW, Folkerth RD, Keene CD, Litvan I, et al. The first NINDS/NIBIB consensus meeting to define neuropathological criteria for the diagnosis of chronic traumatic encephalopathy. Acta Neuropathol. 2016;131(1):75–86. doi: 10.1007/s00401-015-1515-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Falcon B, Zivanov J, Zhang W, Murzin AG, Garringer HJ, Vidal R, et al. Novel tau filament fold in chronic traumatic encephalopathy encloses hydrophobic molecules. Nature. 2019;568(7752):420–423. doi: 10.1038/s41586-019-1026-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shi Y, Zhang W, Yang Y, Murzin AG, Falcon B, Kotecha A, et al. Structure-based classification of tauopathies. Nature. 2021;598(7880):359–363. doi: 10.1038/s41586-021-03911-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cherry JD, Esnault CD, Baucom ZH, Tripodis Y, Huber BR, Alvarez VE, et al. Tau isoforms are differentially expressed across the hippocampus in chronic traumatic encephalopathy and Alzheimer’s disease. Acta Neuropathol Commun. 2021;9(1):86. doi: 10.1186/s40478-021-01189-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cherry JD, Kim SH, Stein TD, Pothast MJ, Nicks R, Meng G, et al. Evolution of neuronal and glial tau isoforms in chronic traumatic encephalopathy. Brain Pathol. 2020;30(5):913–925. doi: 10.1111/bpa.12867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stathas S, Alvarez VE, Xia W, Nicks R, Meng G, Daley S, et al. Tau phosphorylation sites serine202 and serine396 are differently altered in chronic traumatic encephalopathy and Alzheimer’s disease. Alzheimers Dement. 2021;18(8):1511–1522. doi: 10.1002/alz.12502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.DeTure MA, Dickson DW. The neuropathological diagnosis of Alzheimer’s disease. Mol Neurodegener. 2019;14(1):32. doi: 10.1186/s13024-019-0333-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nelson PT, Brayne C, Flanagan ME, Abner EL, Agrawal S, Attems J, et al. Frequency of LATE neuropathologic change across the spectrum of Alzheimer’s disease neuropathology: combined data from 13 community-based or population-based autopsy cohorts. Acta Neuropathol. 2022;144(1):27–44. doi: 10.1007/s00401-022-02444-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Robinson JL, Lee EB, Xie SX, Rennert L, Suh E, Bredenberg C, et al. Neurodegenerative disease concomitant proteinopathies are prevalent, age-related and APOE4-associated. Brain. 2018;141(7):2181–2193. doi: 10.1093/brain/awy146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Adams JW, Alvarez VE, Mez J, Huber BR, Tripodis Y, Xia W, et al. Lewy body pathology and chronic traumatic encephalopathy associated with contact sports. J Neuropathol Exp Neurol. 2018;77(9):757–768. doi: 10.1093/jnen/nly065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Standring OJ, Friedberg J, Tripodis Y, Chua AS, Cherry JD, Alvarez VE, et al. Contact sport participation and chronic traumatic encephalopathy are associated with altered severity and distribution of cerebral amyloid angiopathy. Acta Neuropathol. 2019;138(3):401–413. doi: 10.1007/s00401-019-02031-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ling H, Morris HR, Neal JW, Lees AJ, Hardy J, Holton JL, et al. Mixed pathologies including chronic traumatic encephalopathy account for dementia in retired association football (soccer) players. Acta Neuropathol. 2017;133(3):337–352. doi: 10.1007/s00401-017-1680-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stein TD, Crary JF. Chronic traumatic encephalopathy and neuropathological comorbidities. Semin Neurol. 2020;40(4):384–393. doi: 10.1055/s-0040-1713628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mez J, Alosco ML, Daneshvar DH, Saltiel N, Baucom Z, Abdolmohammadi B, et al. Validity of the 2014 Traumatic Encephalopathy Syndrome criteria for CTE pathology. Alzheimers Dement. 2021;17(10):1709–24. [DOI] [PMC free article] [PubMed]
- 32.Nicks R, Clement NF, Alvarez VE, Tripodis Y, Baucom ZH, Huber BR, et al. Repetitive head impacts and chronic traumatic encephalopathy are associated with TDP-43 inclusions and hippocampal sclerosis. Acta Neuropathol. 2023;145(4):395–408. [DOI] [PMC free article] [PubMed]
- 33.Stein TD, Montenigro PH, Alvarez VE, Xia W, Crary JF, Tripodis Y, et al. Beta-amyloid deposition in chronic traumatic encephalopathy. Acta Neuropathol. 2015;130(1):21–34. doi: 10.1007/s00401-015-1435-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lesman-Segev OH, La Joie R, Stephens ML, Sonni I, Tsai R, Bourakova V, et al. Tau PET and multimodal brain imaging in patients at risk for chronic traumatic encephalopathy. Neuroimage Clin. 2019;24:102025. doi: 10.1016/j.nicl.2019.102025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stern RA, Adler CH, Chen K, Navitsky M, Luo J, Dodick DW, et al. Tau Positron-Emission Tomography in former National Football League players. N Engl J Med. 2019;380(18):1716–1725. doi: 10.1056/NEJMoa1900757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alosco ML, Mariani ML, Adler CH, Balcer LJ, Bernick C, Au R, et al. Developing methods to detect and diagnose chronic traumatic encephalopathy during life: rationale, design, and methodology for the DIAGNOSE CTE Research Project. Alzheimer's Res Ther. 2021;13(1):136. doi: 10.1186/s13195-021-00872-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jack CR, Jr, Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, et al. NIA-AA research framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 2018;14(4):535–562. doi: 10.1016/j.jalz.2018.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tombaugh TN. Test of memory malingering: TOMM: Multy-Health Systems. 1996. [Google Scholar]
- 39.Clark CM, Schneider JA, Bedell BJ, Beach TG, Bilker WB, Mintun MA, et al. Use of florbetapir-PET for imaging beta-amyloid pathology. JAMA. 2011;305(3):275–283. doi: 10.1001/jama.2010.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fleisher AS, Chen K, Liu X, Roontiva A, Thiyyagura P, Ayutyanont N, et al. Using positron emission tomography and florbetapir F18 to image cortical amyloid in patients with mild cognitive impairment or dementia due to Alzheimer disease. Arch Neurol. 2011;68(11):1404–1411. doi: 10.1001/archneurol.2011.150. [DOI] [PubMed] [Google Scholar]
- 41.Clark CM, Pontecorvo MJ, Beach TG, Bedell BJ, Coleman RE, Doraiswamy PM, et al. Cerebral PET with florbetapir compared with neuropathology at autopsy for detection of neuritic amyloid-β plaques: a prospective cohort study. Lancet Neurol. 2012;11(8):669–678. doi: 10.1016/S1474-4422(12)70142-4. [DOI] [PubMed] [Google Scholar]
- 42.Johnson KA, Sperling RA, Gidicsin CM, Carmasin JS, Maye JE, Coleman RE, et al. Florbetapir (F18-AV-45) PET to assess amyloid burden in Alzheimer’s disease dementia, mild cognitive impairment, and normal aging. Alzheimers Dement. 2013;9(5 Suppl):S72–83. doi: 10.1016/j.jalz.2012.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.NINDS. Focus on Traumatic Brain Injury Research: National Institutes of Health. In: Traumatic Brain Injury Research 2022 https://www.ninds.nih.gov/current-research/focus-disorders/focus-traumatic-brain-injury-research. Accessed 10 Nov 2022.
- 44.Katz DI, Bernick C, Dodick DW, Mez J, Mariani ML, Adler CH, et al. National Institute of Neurological Disorders and Stroke consensus diagnostic criteria for traumatic encephalopathy syndrome. Neurology. 2021;96(18):848–863. doi: 10.1212/WNL.0000000000011850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.U.S. Food and Drug Administration. Highlights of prescribing information: Amyvid (florbetapir F18 injection). Silver Spring: U.S. Food and Drug Administration; 2012. http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/202008s000lbl.pdf. Accessed 14 Nov 2022.
- 46.Rabinovici GD, Gatsonis C, Apgar C, Chaudhary K, Gareen I, Hanna L, et al. Association of Amyloid positron emission tomography with subsequent change in clinical management among medicare beneficiaries with mild cognitive impairment or dementia. JAMA. 2019;321(13):1286–1294. doi: 10.1001/jama.2019.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vives-Rodriguez AL, Schiloski KA, Marin A, Wang R, Hajos GP, Powsner R, et al. Impact of amyloid PET in the clinical care of veterans in a tertiary memory disorders clinic. Alzheimer's Dement: Transl Res Clin Interv. 2022;8(1):e12320. doi: 10.1002/trc2.12320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jansen WJ, Janssen O, Tijms BM, Vos SJB, Ossenkoppele R, Visser PJ, et al. Prevalence estimates of amyloid abnormality across the Alzheimer disease clinical spectrum. JAMA Neurol. 2022;79(3):228–243. doi: 10.1001/jamaneurol.2021.5216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ossenkoppele R, Jansen WJ, Rabinovici GD, Knol DL, van der Flier WM, van Berckel BN, et al. Prevalence of amyloid PET positivity in dementia syndromes: a meta-analysis. JAMA. 2015;313(19):1939–1949. doi: 10.1001/jama.2015.4669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ponomarenko A, Tyrtyshnaia A, Ivashkevich D, Manzhulo I. Mild traumatic brain injury contributes to the development of delayed neuroinflammation. NeuroImmunoModulation. 2022;29(2):135–142. doi: 10.1159/000519011. [DOI] [PubMed] [Google Scholar]
- 51.Broussard JI, Acion L, De Jesús-Cortés H, Yin T, Britt JK, Salas R, et al. Repeated mild traumatic brain injury produces neuroinflammation, anxiety-like behaviour and impaired spatial memory in mice. Brain Inj. 2018;32(1):113–122. doi: 10.1080/02699052.2017.1380228. [DOI] [PubMed] [Google Scholar]
- 52.Wofford KL, Harris JP, Browne KD, Brown DP, Grovola MR, Mietus CJ, et al. Rapid neuroinflammatory response localized to injured neurons after diffuse traumatic brain injury in swine. Exp Neurol. 2017;290:85–94. doi: 10.1016/j.expneurol.2017.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shitaka Y, Tran HT, Bennett RE, Sanchez L, Levy MA, Dikranian K, et al. Repetitive closed-skull traumatic brain injury in mice causes persistent multifocal axonal injury and microglial reactivity. J Neuropathol Exp Neurol. 2011;70(7):551–567. doi: 10.1097/NEN.0b013e31821f891f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Izzy S, Brown-Whalen A, Yahya T, Sarro-Schwartz A, Jin G, Chung JY, et al. Repetitive traumatic brain injury causes neuroinflammation before tau pathology in adolescent P301S mice. Int J Mol Sci. 2021;22(2):907. 10.3390/ijms22020907. [DOI] [PMC free article] [PubMed]
- 55.Cherry JD, Tripodis Y, Alvarez VE, Huber B, Kiernan PT, Daneshvar DH, et al. Microglial neuroinflammation contributes to tau accumulation in chronic traumatic encephalopathy. Acta Neuropathol Commun. 2016;4(1):112. doi: 10.1186/s40478-016-0382-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Grothe MJ, Barthel H, Sepulcre J, Dyrba M, Sabri O, Teipel SJ. Alzheimer's Disease Neuroimaging Initiative. In vivo staging of regional amyloid deposition. Neurology. 2017;89(20):2031–2038. doi: 10.1212/WNL.0000000000004643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Donohue MC, Sperling RA, Petersen R, Sun CK, Weiner MW, Aisen PS. Alzheimer’s Disease Neuroimaging Initiative. Association between elevated brain amyloid and subsequent cognitive decline among cognitively normal persons. JAMA. 2017;317(22):2305–2316. doi: 10.1001/jama.2017.6669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sperling RA, Donohue MC, Raman R, Rafii MS, Johnson K, Masters CL, van Dyck CH, Iwatsubo T, Marshall GA, Yaari R, Mancini M, Holdridge KC, Case M, Sims JR, Aisen PS, A4 Study Team Trial of Solanezumab in preclinical Alzheimer's Disease. N Engl J Med. 2023;10:1056. doi: 10.1056/NEJMoa2305032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Amadoru S, Doré V, McLean CA, et al. Comparison of amyloid PET measured in Centiloid units with neuropathological findings in Alzheimer’s disease. Alzheimer's Res Ther. 2020;12:22. doi: 10.1186/s13195-020-00587-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang J, Jin C, Zhou J, Zhou R, Tian M, Lee HJ, et al. PET molecular imaging for pathophysiological visualization in Alzheimer’s disease. Eur J Nucl Med Mol Imaging. 2022;50:765–783. doi: 10.1007/s00259-022-05999-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Karikari TK, Ashton NJ, Brinkmalm G, Brum WS, Benedet AL, Montoliu-Gaya L, et al. Blood phospho-tau in Alzheimer disease: analysis, interpretation, and clinical utility. Nat Rev Neurol. 2022;18(7):400–418. doi: 10.1038/s41582-022-00665-2. [DOI] [PubMed] [Google Scholar]
- 62.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease. Report of the NINCDS‐ADRDA Work Group* under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984;34(7):939–44. [DOI] [PubMed]
- 63.McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR, Jr, Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7(3):263–269. doi: 10.1016/j.jalz.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Li Y, Li Y, Li X, Zhang S, Zhao J, Zhu X, et al. Head injury as a risk factor for dementia and Alzheimer’s disease: a systematic review and meta-analysis of 32 observational studies. PLoS ONE. 2017;12(1):e0169650. doi: 10.1371/journal.pone.0169650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sugarman MA, McKee AC, Stein TD, Tripodis Y, Besser LM, Martin B, et al. Failure to detect an association between self-reported traumatic brain injury and Alzheimer’s disease neuropathology and dementia. Alzheimers Dement. 2019;15(5):686–698. doi: 10.1016/j.jalz.2018.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hicks AJ, Ponsford JL, Spitz G, Dore V, Krishnadas N, Roberts C, et al. β-Amyloid and Tau imaging in chronic traumatic brain injury: a cross-sectional study. Neurology. 2022;99(11):e1131–e1141. doi: 10.1212/WNL.0000000000200857. [DOI] [PubMed] [Google Scholar]
- 67.Weiner MW, Harvey D, Hayes J, Landau SM, Aisen PS, Petersen RC, et al. Effects of traumatic brain injury and posttraumatic stress disorder on development of Alzheimer’s disease in Vietnam veterans using the Alzheimer's Disease Neuroimaging Initiative: Preliminary report. Alzheimers Dement. 2017;3(2):177–188. doi: 10.1016/j.trci.2017.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Plassman BL, Chanti-Ketterl M, Pieper CF, Yaffe K. Traumatic brain injury and dementia risk in male veteran older twins controlling for genetic and early life non-genetic factors. Alzheimers Dement. 2022;18(11):2234–2242. doi: 10.1002/alz.12571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Crane PK, Gibbons LE, Dams-O'Connor K, Trittschuh E, Leverenz JB, Keene CD, et al. Association of traumatic brain injury with late-life neurodegenerative conditions and neuropathologic findings. JAMA Neurol. 2016;73(9):1062–1069. doi: 10.1001/jamaneurol.2016.1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Brett BL, Gardner RC, Godbout J, Dams-O’Connor K, Keene CD. Traumatic brain injury and risk of neurodegenerative disorder. Biol Psychiatry. 2022;91(5):498–507. doi: 10.1016/j.biopsych.2021.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dams-O'Connor K, Guetta G, Hahn-Ketter AE, Fedor A. Traumatic brain injury as a risk factor for Alzheimer’s disease: current knowledge and future directions. Neurodegener Dis Manag. 2016;6(5):417–429. doi: 10.2217/nmt-2016-0017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Weiner MW, Crane PK, Montine TJ, Bennett DA, Veitch DP. Traumatic brain injury may not increase the risk of Alzheimer disease. Neurology. 2017;89(18):1923–1925. doi: 10.1212/WNL.0000000000004608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.United States District Court EDoP. National Football League players' concussion injury litigation, MDL 2323, Class Action Settlement Agreement 2015. In: Case 2:12-md-02323-AB Document 6481–1 https://www.nflconcussionsettlement.com/Docs/Amended%20Class%20Action.pdf. Accessed 11 Nov 2022
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Algorithm for Diagnostic Categorization. Supplementary Table 1. Proportion of Positive Amyloid PET Scans by Age within Exposure Group. Supplementary Table 2. Correlationsa of Florbetapir PET Average SUVR with Clinical Measures and Years of Football.
Data Availability Statement
Data from the DIAGNOSE CTE Research Project will be available to qualified investigators through the Federal Interagency Traumatic Brain Injury Research (FITBIR) Informatics System, through the National Institutes of Health Center for Information Technology: https://fitbir.nih.gov/content/access-data. DIAGNOSE CTE Research Project data, including those reported in this study, will also be available to qualified investigators through a project-specific data-sharing portal. Interested investigators should contact Dr. Robert A. Stern, bobstern@bu.edu.